Summary
Telemedicine is extremely useful when distance could hinder diagnostic procedures, disease management, or when severe side-effects may occur in patients not within easy reach of medical care and requiring prompt action and specific therapies. Telemedicine has been successfully adopted in the management of chronic patients, particularly in those with cardiologic or oncologic diseases. In the treatment of differentiated thyroid cancer, requiring long-term check-ups and visits as well as administration of high doses of levothyroxine (TSH – thyroid-stimulating hormone – suppression), also in elderly patients, telemedicine seems particularly indicated. Moreover, these distant monitoring techniques could not only reduce long-term management costs but also considerably decrease cardiovascular risks associated with these patients. The present review aims to provide some general information on telemedicine and its possible fields of action with regard to distant monitoring of patients with differentiated thyroid carcinoma.
Keywords: Telemedicine, Thyroid cancer, Heart disease and hyperthyroidism
Riassunto
La telemedicina è di grande utilità ogni volta in cui le distanze possano costituire un ostacolo alle procedure diagnostiche o alla programmazione dell’iter terapeutico, oppure quando si prospetti la necessità di fronteggiare effetti collaterali improvvisi alle terapie somministrate. L’uso della telemedicina si è già dimostrato vantaggioso nella gestione di pazienti cronici, in particolare pazienti con patologie cardiache o oncologiche. Nel trattamento dei carcinomi differenziati della tiroide, che prevede periodici controlli per moltissimi anni e utilizzo di L-tiroxina a dosi sovrafisiologiche (TSH-soppressione) anche in pazienti anziani, l’utilizzo delle tecniche di telemedicina sembra particolarmente indicato e potrebbe ridurre i costi della gestione a lungo termine di questi pazienti, oltre a ridurre notevolmente i rischi delle emergenze cardiologiche. In questa breve review sono riassunte le indicazioni generali della telemedicina e i possibili campi di utilizzo nel controllo a distanza di pazienti con neoplasie differenziate della tiroide.
Introduction
Treatment of differentiated thyroid cancer includes surgery, radioiodine therapy and pharmacological suppression of thyroid stimulating hormone (TSH) activity with levothyroxine (L-T4) administration.
Patients often have co-morbidities. Coronary artery disease and hypertensive heart disease are fairly common; furthermore, thyroid hormones, used as suppressive therapy, have many important cardiovascular effects.
The possibilities offered by telemedicine in cancer patient care have been reviewed in recent studies 1 2. In this review, thyroid hormones/heart interactions in thyroid cancer patients have been taken into consideration and the possible use of distant monitoring by means of telemedicine techniques is suggested as a further contribution to the management of such a combination of health problems which are not at all rare.
Potentials of telemedicine
Telemedicine in chronic diseases
Telemedicine can be used to directly communicate with patients, their relatives, and/or the nursing staff, in order to transmit biological data and images, data collection (Table I). The use of biological data transmission and telephone conversations with patients for counselling is referred to as telemonitoring.
Table I. Menu of telemedicine.
| Conference calls for case discussion |
| On line images and sounds sharing (videoconference) |
| – Pathology slides |
| – Digitised images from imaging diagnostic methods (CT, MRI, US) |
| – Laboratory data and medical database always available |
| Easily retrievable multi–language medical files |
| Telesurgery |
| Phone calls with patients on symptoms and real time transfer of data: |
| – ECGs heart rate blood pressure |
| – SpO2 (Pulse oximetry) respiratory rate peak expiratory flow |
| – Body temperature and weight |
Chronic diseases can derive enormous benefits from telemedicine, even when patients are severely ill or elderly.
The issue of managing chronic diseases is more and more important as age, multiple pathological conditions and technology increasingly contribute to increases in health care costs. Not surprisingly, great health care organisations have initiated tele home projects 3. For example, the Kaiser Permanent Center in California set up a project involving newly referred patients diagnosed as having congestive heart failure, chronic obstructive pulmonary disease, cerebral vascular accident, cancer, diabetes, anxiety, or in need of wound care. Eligible patients were randomly assigned to a telemonitoring (n = 102) or usual monitoring (control) (n = 110) group. Both control and telemonitoring groups received routine home health care (home visits and telephone contacts). The telemonitoring group also had access to a remote video system that allowed nurses and patients to interact in real time. The video system included peripheral equipment to assess cardiopulmonary status. No differences in the quality indicators, patient satisfaction, or use were observed. Remote video technology, in the home health care setting, has proven effective, well received and appreciated by patients, able to maintain quality of care, and potentially cost saving.
Various models of telemonitoring have been proven useful in different situations. Some examples include: home care of severe respiratory diseases 4, high risk infant nursing 5, open angle glaucoma follow-up 6, blood pressure monitoring 7 8, asthma 9 and chronic obstructive pulmonary disease control 10, chest pain first aid 11, home cardiac rehabilitation 12, early detection of silent atrial fibrillation 13.
Heart failure is an extremely good example of the use, as well as effectiveness, of telemedicine, and a large number of studies have been published on this topic. A recent meta-analysis 14 has been carried out to determine whether remote monitoring (structured telephone support or telemonitoring) without regular clinic or home visits improves outcomes in patients with chronic heart failure. Remote monitoring programmes have reduced hospital admission rates for chronic heart failure by 21%, as well as all-cause mortality by 20%. Healthcare costs have also benefited from structured telephone support.
According to the data obtained, these programmes for chronic heart failure, using remote monitoring, have been shown to have a positive effect on clinical outcome in community-dwelling patients with chronic heart failure.
It should be stressed that, while evaluating quality of life and costs, careful attention should be paid to the study model and to the complexity and costs of the devices employed (video camera and electronic scales as opposed to simple telephonic support).
Research is underway on the use of psychotherapy in terminally ill cancer patients. The condition of patients who have difficulty in moving due to the disease and distance is, indeed, an important issue. Passik et al. 15, reported results of a pilot study on dignity psychotherapy delivered via telemedicine. They reported overall benefits from the intervention as well as high-level satisfaction of the patients. Psychotherapeutic support can be scheduled with very few technical difficulties. Telemedicine can extend the benefits of dignity psychotherapy by “delivering” it to those patients who are too ill to move or live in rural areas. This could be a feasible way to offer them concrete help.
Telemedicine in training and consultation
Training patients with diabetes is of the utmost importance for the management of this disease, and can be implemented by means of distant communication with audio-visual devices. This activity has been shown to be equivalent to personal visits and less costly 16.
Multidisciplinary consultation is common with chronic diseases, such as chronic obstructive pulmonary disease and cancer care. Telemedicine allows easy distant visualisation of digitised images and simultaneous phone or e-mail contacts which are extremely useful for these diseases. Possible benefits include improved referral coordination, a reduction not only in patient transfers but also in delay of treatment 17–19. More recently, Norum & Jordhoy 20. used e-mail and videoconferences to link a University Oncology Department with a remote palliative care unit in Bodö, Norway. During a 12-month period, 23 breast and colorectal cancers were diagnosed in 20 patients. Most cases were treated locally. Although some videoconferences failed, due to telecommunication and/or user problems, videoconferencing was still held to be a success in the updating of oncologists in this remote area.
Telemedicine in oncological diagnosis and management
Telemedicine in oncology has been shown to be a very useful tool both in distant diagnosis and in distant confirmation of previously made and uncertain diagnoses 2. This can be employed not only in less fortunate geographical areas or where skilled specialists are not available, but also in technologically advanced areas where telemedicine allows a multidisciplinary approach in cases of uncertain or complex diagnoses 2 21 22. Moreover, the re-evaluation of radiologic images or histologic specimens through telemedicine leads to the reduction of diagnostic costs and time, increasing sensitivity provided that senior and experienced trainees are involved – as recommended.
Telemedicine techniques allow a joint approach to appropriate decision making with regard to treatment procedures, also in centres where medical staff and the number of patients seem too low to guarantee qualified team work.
Last but not least, telemedicine has been found to be particularly useful in distant monitoring and/or follow-up in less fortunate areas or where the continuous presence of a specialist could not be assured. This applies above all for rather infrequent tumours or for those tumours requiring long-term follow-up.
And what about thyroid cancer?
When dealing with thyroid cancer, the above-mentioned theories regarding cancer management are certainly valid. Moreover, two further issues which would greatly benefit from telemonitoring should be taken into due consideration.
In most cases, differentiated thyroid cancer treatment requires L-T4 administration at high doses to reach a subclinical hyperthyroid status. This can sometimes lead to cardiovascular risk, while in other cases it does not jeopardise the patient but places him/her in a state of anxiety and discomfort. On the other hand, forced hypothyroidism due to L-T4 deprivation before radioiodine treatment represents a further heart challenge, particularly for elderly patients 23.
Biological characteristics of thyroid cancer: low aggressiveness and possible recurrence several years after the initial treatment result in the need for long-term follow-up. For these reasons, the physician must often face the patients’ ambivalence as far as concerns compliance to monitoring and therapy. Due to long-term disease-free survival, sometimes leading to late recurrences, patients seem either to disregard treatment, as well as monitoring, because they tend to deny their status, or to exceed in monitoring, consulting and testing to soothe their anxiety. In such circumstances, telemonitoring could offer further advantages in thyroid cancer management.
Long-term cardiovascular effects of levothyroxine in TSH suppression
Prolonged administration of L-T4 for TSH suppression displays some different effects from overt clinical hyperthyroidism 24. Long-term TSH suppression affects both arterial and left ventricle walls 25 26 (Table II). This exposes patients to a greater likelihood of hypertension, cardiac ischaemia, heart failure and arrhythmias. Of these, diastolic left ventricular dysfunction is reversible after treatment withdrawal 23 27. In some studies, these unfavourable effects were shown to be reduced by tailoring the L-T4 dose. Thus, the TSH value is maintained in the range of > 0.1 mcU/ml 24. However, other researchers did not find any significant difference 28. Beta-blockade with atenolol has been shown to reduce and partially revert these alterations 28. Addition of the cardioselective beta-blocker bisoprolol to L-T4 treatment for 6 months significantly reduced the occurrence of supraventricular arrhythmias, average heart rate, and left ventricular mass with improvement of diastolic function at rest and systolic performance during exercise 29 30.
Table II. Telemedicine can be usefully adopted in the different steps of chronic diseases, from diagnosis to palliative care.
| Telemedicine | ||||
| Diagnosis | Treatment | Follow–up | Education & Training | Palliative & home assistance |
| – Imaging consulting (CT, MRI, US, scintigraphy) | – Multidisciplinary | – Imaging | – Patient’s training | – Therapy assessment for chronic disease |
| – Specimens | – Decision making | – Blood tests | – Videoconference | – Home counselling for disabled or severely ill patients |
| – Patient’s images | – Telesurgery | – Symptoms | – Counselling by skilled professionals | – Dignity psycotherapy |
| – Dose adjustment/assessment | – Side effects | |||
| – Dose adjustment | ||||
However, these data have not been supported by any large trials, and it would appear impossible to collect supporting data in the near future due the relatively small number of L-T4 treated patients.
Hyperthyroidism has a pro-arrhythmic action per se 31 that increases supraventricular ectopic activity in patients with normal hearts by the activation of arrhythmogenic foci. This may well be an important link between hyperthyroidism and atrial fibrillation. As is well known, the rapid heart action of atrial fibrillation can precipitate ischaemia and heart failure in the presence of reduced coronary reserve or systolic and even diastolic dysfunction.
Interestingly, it has recently been demonstrated that during thyroid hormone suppressive treatment, in thyroid cancer patients, some pro-coagulant protein levels (prothrombin fragment 1-2, fibrinogen, protein S, antithrombin, tPA, PAI-1, and PAI-1/tPA) were significantly higher than in healthy controls and in the same patients when hypothyroid for radioiodine whole-body scanning. Thus, the majority of patients treated with thyroid suppressive treatment should be considered as having a prothrombotic profile 32.
As for thyroid diseases, the menu of telemedicine (Table I) comprises: multidisciplinary consultation, telemonitoring for heart rate, arrhythmias, body temperature, body weight, blood pressure. These can be used for monitor treatment and for patient counselling, particularly for patients affected by synchronous diseases and/or advanced cancer.
Some examples from the literature are outlined below.
Table III. Long-term cardiovascular effects of thyroid cancer treatment.
| 1. Hyperthyroidism in TSH suppression |
| - Decreased small and large artery elasticity |
| - Left ventricular hypertrophy and diastolic dysfunction |
| - Increased left ventricular volumes and mass index |
| - Decreased effort tolerance (maximal work load and aerobic threshold) |
| - Night time systolic blood pressure increase (stimulation of renin angiotensin system) |
| - Prothrombotic profile |
| 2. Hypothyroidism in L-T4 deprivation |
| - Diastolic function worsening |
| - Increased systemic vascular resistance |
| - Systolic and diastolic hypertension |
| - Decreased creatinine clearance |
Yokota et al. 33, from the Atomic Bomb Disease Institute, Nagasaki, Japan, used a telemedicine system to connect Nagasaki University School of Medicine (Japan) and Gomel Regional Specialized Dispensary (Belarus) via satellite communication and the international ISDN, for management of patients’ data and research, including thyroid ultrasound images, cytology specimens. Information regarding patients was sent from Gomel to Nagasaki once a week in the event of doubtful diagnoses. Thyroid specialists at Nagasaki University School of Medicine double-checked the diagnoses and sent their comments to Gomel. Diagnoses were in agreement for only ~50% of these cases. The use of telemedicine proved useful in improving diagnostic skills.
Beta-blockers are administered to reduce and revert the alterations due to thyroid hormone suppressive treatment 28 30. In elderly or very sick outpatients, rapid and safe adjusting of doses of beta-blockers can be an issue due to possible side-effects and logistical difficulties. Spaeder et al. 34 from Johns Hopkins University, Baltimore, USA used telemonitoring to rapidly titrate carvedilol in outpatients with left ventricular systolic dysfunction. Patients were randomized to clinic-only (CO) carvedilol titration or titrations which combined clinic visits with telemonitoring. According to Spaeder et al., remote monitoring with an automated telemedicine system can be usefully employed in the titration of beta-blockers in outpatients with congestive heart failure.
Electrocardiography (ECG) telemonitoring can easily detect and diagnose arrhythmias, and simple single channel recorders are sufficient for diagnosis in most cases. In thyroid cancer patients on suppressive therapy, atrial fibrillation is highly prevalent and risky as the rapid heart rate can lead to heart failure or ischaemia. Should tachycardia continue for several days, cardiomyopathy may occur. Many trials have confirmed that atrial fibrillation has a three-fold higher incidence in hyperthyroid patients 35–37.
Moreover, subclinical hyperthyroidism was found to be an independent risk factor for atrial fibrillation in patients with other pre-existing cardiac risk factors (e.g. coronary heart disease, valvular defects, hypertension) 38. Page et al. 13 demonstrated that ECG telemonitoring promptly detected even asymptomatic atrial fibrillation in patients under bradycardic treatment.
Conclusions
Data on the effectiveness of telemedicine in thyroid cancer patients are fairly clear, such as telemonitoring in arrhythmias, drug dose adjustment, disabled and/or advanced disease patients. Telemedicine is also useful as a support for patients’ psychological aspects, to allow distant multidisciplinary discussion with visualisation of data and images, and to access real-time multi-language data bases. Obviously, telemedicine cannot replace the physicians, but it can play an important role in making their work easier, improving patient management, and the patient’s quality of life.
All of us who used to keep contacts with patients and colleagues by e-mail, feel the need for real time, or at least very fast, access to more and more information, particularly for seriously ill patients.
Cost benefit and cost efficacy data are lacking, in particular, those comparing complex models (i.e., use of high technology) versus simple models (i.e., simple phone scheduled follow-up plus calls from patients to integrate conventional visits). Legal issues should be evaluated locally. Institutional Ethics Committees should evaluate the implementation of telemedicine protocols. An important issue concerns telemonitoring in critical patients which should not to be intended as a substitute for conventional visit but rather a way by which to understand in advance whether a non-scheduled intervention is needed.
Finally, we should bear in mind that both the patient’s and the physician’s physical absence requires some adjustments in the usual human relationship. Phone counselling and/or videoconferencing are completely different from conventional visits since interactions are not direct but occur via a technological system. This system offers an unusual form of physical interaction that may be more or less realistic depending upon the technology employed 39. Patients seem satisfied with the possibility of adopting telemedicine, while doctors felt hampered by the communication barriers 40. For this reason, training programmes are needed for doctors to develop and improve communication skills as well as the ability to express empathy during telemedicine counselling.
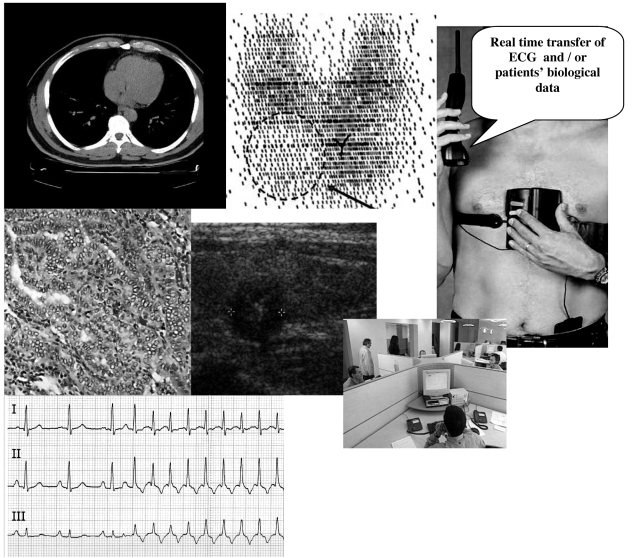
Fig. 1.
Use of telemedicine. Telemedicine can be usefully adopted in various steps of chronic diseases, from diagnosis to palliative care.
Acknowledgments
Authors are grateful to Mrs Lucia Zigliani for kind support in preparation of manuscript.
References
- 1.Wysockia WM, Komorowskia AL, Aapro AS. The new dimension of oncology. Teleoncology ante portas. Crit Rev Oncol Hematol 2005;53:95-100. [DOI] [PubMed] [Google Scholar]
- 2.Kunkler IH, Prescott RJ, Lee RJ, Brebner JA, Cairns JA, Fielding RG, et al. TELEMAM: a cluster randomised trial to assess the use of telemedicine in multi-disciplinary breast cancer decision making. Eur J Cancer 2007;43:2506-14. [DOI] [PubMed] [Google Scholar]
- 3.Johnston B, Wheeler L, Deuser J, Sousa KH. Outcomes of the Kaiser Permanente Tele-Home Health Research Project. Arch Fam Med 2000;9:40-5. [DOI] [PubMed] [Google Scholar]
- 4.Maiolo C, Mohamed EI, Fiorani CM, De Lorenzo A. Home telemonitoring for patients with severe respiratory illness: the Italian experience. J Telemed Telecare 2003;9:67-71. [DOI] [PubMed] [Google Scholar]
- 5.Gray JE, Safran C, Davis RB, Pompilio-Weitzner G, Stewart JE, Zaccagnini L, et al. Baby Care Link: using the internet and telemedicine to improve care for high-risk infants. Pediatrics 2000;106:1318-24. [DOI] [PubMed] [Google Scholar]
- 6.Michelson G, Striebel W, Prihoda W, Schmidt V. Telemedicine in the control of intra-ocular pressure. J Telemed Telecare 2000;6(Suppl 1):S126-8. [DOI] [PubMed] [Google Scholar]
- 7.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ 2004;329:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madsen LB, Kirkegaard P, Pedersen EB. Blood pressure control during telemonitoring of home blood pressure. A randomized controlled trial during 6 months. Blood Press 2008;17:78-86. [DOI] [PubMed] [Google Scholar]
- 9.Willems DC, Joore MA, Hendriks JJ, van Duurling RA, Wouters EF, Severens JL. Process evaluation of a nurse-led telemonitoring programme for patients with asthma. J Telemed Telecare 2007;13:310-7. [DOI] [PubMed] [Google Scholar]
- 10.Trappenburg JC, Niesink A, de Weert-van Oene GH, van der Zeijden H, van Snippenburg R, Peters A, et al. Effects of telemonitoring in patients with chronic obstructive pulmonary disease. Telemed J E-Health 2008;14:138-46. [DOI] [PubMed] [Google Scholar]
- 11.Scalvini S, Zanelli E, Conti C, Volterrani M, Pollina R, Giordano A, et al. Assessment of prehospital chest pain using telecardiology. J Telemed Telecare 2002;8:231-6. [DOI] [PubMed] [Google Scholar]
- 12.Ades PA, Pashkow FJ, Fletcher G, Pina IL, Zohman LR, Nestor JR. A controlled trial of cardiac rehabilitation in the home setting using electrocardiographic and voice transtelephonic monitoring. Am Heart J 2000;139:543-8. [DOI] [PubMed] [Google Scholar]
- 13.Page RL, Tilsch TW, Connolly SJ, Schnell DJ, Marcello SR, Wilkinson WE, et al. Asymptomatic or “Silent” atrial fibrillation frequency in untreated patients and patients receiving Azimilide. Circulation 2003;107:1141-5. [DOI] [PubMed] [Google Scholar]
- 14.Clark RA, Inglis SC, McAlister FA, Cleland JGF, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334:942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Passik SD, Kirsh KL, Leibee S, Kaplan LS, Love C, Napier E, et al. A feasibility study of dignity psychotherapy delivered via telemedicine. Palliat Support Care 2004;2:149-55. [DOI] [PubMed] [Google Scholar]
- 16.Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS, et al. A diabetes education administered through telemedicine versus in person. Diabetes Care 2003;26:1002-7. [DOI] [PubMed] [Google Scholar]
- 17.Duplaga M, Soja J, Cala J, Leszczuk M, Wasowski D, Sladek K, et al. The impact of teleconsultations at a referential centre on the management of pulmonary patients. Stud Health Technol Inform 2004;105:92-9. [PubMed] [Google Scholar]
- 18.Axford AT. Virtual multidisciplinary teams for cancer care. J Telemed Telecare 2002;8(Suppl 2):3-4. [DOI] [PubMed] [Google Scholar]
- 19.Billingleys KG. The development of a telemedical cancer center within the Veterans Affairs Health Care System: a report of preliminary clinical results. Telemed J E Health 2002;8:123-30. [DOI] [PubMed] [Google Scholar]
- 20.Norum J, Jordhoy MS. A university oncology department and a remote palliative care unit linked together by email and videoconferencing. J Telemed Telecare 2006;12:92-6. [DOI] [PubMed] [Google Scholar]
- 21.Kerr SE, Bellizzi AM, Stelow EB, Frierson HF Jr, Policarpio-Nicolas ML. Initial assessment of fine-needle aspiration specimens by telepathology: validation for use in pathology resident-faculty consultations. Am J Clin Pathol 2008;130:409-13. [DOI] [PubMed] [Google Scholar]
- 22.Liakhouski V, Rylkov S, Lushchyk M, Tuzikov A. Teleconsultation and image analysis system in radiation induced thyroid cancer. AMIA Ann Symp Proc 2005;2005:1028. [PMC free article] [PubMed] [Google Scholar]
- 23.Botella-Carretero JI, Gómez-Bueno M, Barrios V, Caballero C, García-Robles R, Sancho J, et al. Chronic thyrotropin-suppressive therapy with levothyroxine and short-term overt hypothyroidism after thyroxine withdrawal are associated with undesirable cardiovascular effects in patients with differentiated thyroid carcinoma. Endocr Relat Cancer 2004;11:345-56. [DOI] [PubMed] [Google Scholar]
- 24.Mercuro G, Panzuto MG, Bina A, Leo M, Cabula R, Petrini L, et al. Cardiac function, physical exercise capacity, and quality of life during long-term thyrotropin-suppressive therapy with levothyroxine: effect of individual dose tailoring. J Clin Endocrinol Metab 2000;85:159-64. [DOI] [PubMed] [Google Scholar]
- 25.Shargorodsky M, Serov S, Gavish D, Leibovitz E, Harpaz D, Zimlichman R. Long-term thyrotropin-suppressive therapy with levothyroxine impairs small and large artery elasticity and increases left ventricular mass in patients with thyroid carcinoma. Thyroid 2006;16:381-6. [DOI] [PubMed] [Google Scholar]
- 26.Biondi B, Palmieri, Klain M, Schlumberger M, Filetti S, Lombardi G. Subclinical hyperthyroidism: clinical features and treatment options. Eur J Endocrinol 2005;152:1-9. [DOI] [PubMed] [Google Scholar]
- 27.Smit JW, Eustatia-Rutten CF, Corssmit EP, Pereira AM, Frolich M, Bleeker GB, et al. Reversible diastolic dysfunction after long-term exogenous subclinical hyperthyroidism: a randomized, placebo-controlled study. J Clin Endocrinol Metab 2005;90:6041-7. [DOI] [PubMed] [Google Scholar]
- 28.Gullu S, Altuntas F, Dincer I, Erol C, Kamel N. Effects of TSH-suppressive therapy on cardiac morphology and function: beneficial effects of addition of beta-blockade on diastolic dysfunction. Eur J Endocrinol 2004;150:655-61. [DOI] [PubMed] [Google Scholar]
- 29.Biondi B, Fazio S, Carella C, Sabatini D, Amato G, Cittadini A, et al. Control of adrenergic overactivity by β-blockade improves quality of life in patients receiving long term suppressive therapy with levothyroxine. J Clin Endocrinol Metab 1994;78:1028-33. [DOI] [PubMed] [Google Scholar]
- 30.Biondi B, Fazio S, Cuocolo A, Sabatini D, Nicolai E, Lombardi G, et al. Impaired cardiac reserve and exercise capacity in patients receiving long-term thyrotropin suppressive therapy with levothyroxine. J Clin Endocrinol Metab 1996;1:4224-8. [DOI] [PubMed] [Google Scholar]
- 31.Wustmann K, Kucera JP, Zanchi A, Burow A, Stuber T, Chappuis B, et al. Activation of electrical triggers of atrial fibrillation in hyperthyroidism. J Clin Endocrinol Metab 2008;93:2104-8. [DOI] [PubMed] [Google Scholar]
- 32.Horne MK 3rd, Singh KK, Rosenfeld KG, Wesley R, Skarulis MC, Merryman PK, et al. Is thyroid hormone suppression therapy prothrombotic? J Clin Endocrinol Metab 2004;89:4469-73. [DOI] [PubMed] [Google Scholar]
- 33.Yokota K, Takamura N, Shibata Y, Yamashita S, Mine M, Tomonaga M, et al. Evaluation of a telemedicine system for supporting thyroid disease diagnosis. Medinfo 2001;10:866-9. [PubMed] [Google Scholar]
- 34.Spaeder J, Najjar SS, Gerstenblith G, Hefter G, Palmer JG, Gottlieb SH, et al. Rapid titration of carvedilol in patients with congestive heart failure: a randomized trial of automated telemedicine versus frequent outpatient clinic visits. Am Heart J 2006;151:844. [DOI] [PubMed] [Google Scholar]
- 35.Tenerz A, Forberg R, Jansson R. Is a more active attitude warranted in patients with subclinical thyrotoxicosis? J Intern Med 1999;228:229-33. [DOI] [PubMed] [Google Scholar]
- 36.Sawin CT, Geller A, Wolf PA, Belanger AJ, Baker E, Bacharach P, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. New Engl J Med 1994;331:1249-52. [DOI] [PubMed] [Google Scholar]
- 37.Auer JA, Scheibner P, Mische T, Langsteger W, Eber O, Eber B. Subclinical hyperthyroidism as a risk factor for atrial fibrillation. Am Heart J 2001;142:838-42. [DOI] [PubMed] [Google Scholar]
- 38.Hammer J, Johanningmann K, Schatz H, Pfeilschifter J. Subclinical hyperthyroidism is an independent risk factor for atrial fibrillation in patients with preexisting cardiac disease. Experimental and Clinical Endocrinology and Diabetes 2001;S37:109-12. [Google Scholar]
- 39.Onor ML, Misan S. The clinical interview and the doctor-patient relationship in telemedicine. Telemed J E Health 2005;11:102-5. [DOI] [PubMed] [Google Scholar]
- 40.Liu X, Sawada Y, Takizawa T, Sato H, Sato M, Sakamoto H, et al. Doctor-patient communication: a comparison between telemedicine consultation and face-to-face consultation. Intern Med 2007;46:227-32. [DOI] [PubMed] [Google Scholar]