Summary
Congenital preauricular sinus is a malformation of the preauricular soft tissues with an incidence ranging between 0.1 and 0.9% in Europe and the United States. It presents a high risk of recurrence when treated by a standard surgical technique (simple sinectomy), the incidence of which is reported to be between 19% and 40%. The supra-auricular approach, proposed by Prasad et al. in 1990, is easier to perform and presents a lower recurrence risk. Personal experience is presented in the treatment of congenital preauricular sinus with the supra-auricular approach as first choice or in the case of recurrence following previous standard surgery. This report includes a short review of the literature in order not only to focus on the supra-auricular approach and check the efficacy as far as concerns reduction of recurrence risk but also to contribute to a more widespread use of this method.
Keywords: Auricular malformations, Congenital preauricular sinus, Surgical treatment, Supra-auricular approach
Riassunto
La fistola preauricolare congenita è una malformazione dei tessuti preauricolari e presenta un’incidenza che va da 0,1 a 0,9% in Europa e negli Stati Uniti. Quando indicato, il trattamento chirurgico standard è gravato da un’alta percentuale di recidive la cui incidenza viene riportata tra il 19% e il 40%. L’approccio sopra-auricolare è caratterizzato da minore rischio di recidiva a fronte di limitate difficoltà di tecnica. Nel presente lavoro viene presentata la nostra esperienza nel trattamento della fistola preauricolare congenita con la tecnica chirurgica sopra-auricolare sia come opzione di prima scelta che in caso di trattamento di recidive di precedenti trattamenti con chirurgia standard. Allo stesso tempo questo lavoro è l’occasione per una revisione della letteratura, per incrementare l’esperienza nell’approccio sopra-auricolare e per contribuire ad una più ampia diffusione della metodica.
Introduction
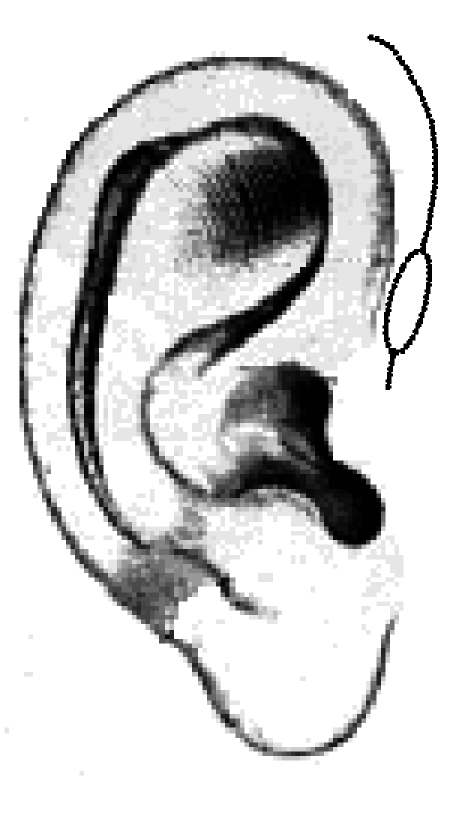
Congenital preauricular sinus is a malformation of the preauricular soft tissues the incidence of which is between 0.1 and 0.9% in Europe and the United States, 2.5% in Taiwan and reaches 10% in some African regions 1 2. Preauricular sinus is more often unilateral, only occasionally are bilateral forms inherited. The right side appears to be more often involved and females more than males 1 3. The embryological basis of this malformation is associated with a defect in the development of the first branchial arch during the sixth week of gestation 4. This alteration is probably due to incomplete fusion of the six auditory hillocks of His. Another hypothesis, less accredited, is that the sinus develops during embryonal auricular development from an isolated ectodermal folding 2. From a clinical point of view, preauricular sinus is an occasional finding and most frequently appears like a small pit close to the anterior margin of the first ascending portion of the helix. In some cases, it is associated with a subcutaneous cyst in close proximity to the pit (Fig. 1) related to the tragal cartilage and the anterior crus of the helix. The sinus course, in preauricular subcutaneous tissues, is not constant, often tortuous, with many ramifications, upwards and medially 5. Topographically, the sinus is located more superficially than the temporalis fascia, laterally and superiorly from the parotid gland and facial nerve and the terminal cutaneous portion is very near, and often adhering to, the cartilage of the first portion of the helix 2. Most sinuses are clinically silent. The eventual, however not rare, appearance of symptoms is related to an infectious process. The most common pathogens causing infection are Staphylococcal species and, less frequently, Proteus, Streptococcus and Peptococcus 12. In this case, the tendency to recurrences requires surgical treatment. In the literature, associations have been described with renal or inner ear anomalies 6 7 and there is a number of syndromes in which the preauricular sinus is only one of the clinical features 8 9.
Fig. 1.

Cyst and right preauricular sinus.
There is some agreement regarding surgical indication that is usually suggested after at least two subsequent infections 5 10 11. The real problem is the high risk of recurrence that weighs on a standard surgical technique, the incidence reported to be between 19 and 40% 11–14. In the literature, apart from a few technical variants, a standard technique has been described (simple sinectomy) that provides an elliptic skin excision around the sinus opening and the dissection of its ramifications in the subcutaneous tissues under visual or palpatory guidance 5 10. There are many suggestions for correct identification of the sinus tracts: the use of a small lachrimal probe 15, methylene blue intra-operative injection 5 16 17, or, pre-operative sonographic imaging or pre-operative sinograms aimed at grossly evaluating the sinus course 2. Each technical variant has limitations: the lacrimal probe trauma may cause a false course and it is unable to follow small ramifications; methylene blue has a vital diffusion in tissues thus making correct identification of the smallest ramifications difficult. Fistulography needs experienced hands, far from acute infectious episodes, and offers only approximate indications regarding the sinus length and direction and no suggestion concerning its depth 5. These issues are likely responsible for insufficient surgical radicality and consequently the high recurrence rate. Moreover, another aspect that appears to play an important role in the recurrence rate is the type of anaesthesia; in our experience, in agreement with Yeo et al. 14, surgery performed under local infiltrative anaesthesia has a higher rate of recurrence than cases receiving general anaesthesia. The reasons are probably related to patient’s limited compliance with surgical manoeuvres and to confounding factors that infiltration itself represents. In 1990, Prasad et al. 13, for the first time, described a new surgical approach defined supra-auricular which was based upon the theory that a fistula is, almost always, included in subcutaneous tissues between the temporalis fascia and perichondrium of the helix cartilage. Therefore, these Authors proposed that the elliptical incision of the standard technique be extended higher upward to the pre- and supra-auricular temporal region (Figs. 2, 3). This allows better surgical vision without adverse aesthetic consequences. Dissection proceeds identifying the temporalis fascia medially to the sinus area. It is only this fascia that represents a medial and deep limit of dissection that continues in a medium lateral direction until reaching the helix cartilage (Fig. 4). At this level, dissection is made below the perichondral layer and, at the point of maximum adherence of the fistula, excision of a small portion of the cartilage is advisable (Fig. 5). The surgeon, during dissection, does not follow the fistula but, being aware of the space in which it develops, removes all subcutaneous tissue comprised between the temporalis fascia and the helix perichondrium (Fig. 6). In this tissue, the sinus is certainly present with its ramifications and the eventual cyst.
Fig. 2.
Incision line.
Fig. 3.

Skin incision.
Fig. 4.

Temporalis fascia dissection.
Fig. 5.

Under perichondral dissection (medial-lateral vision).
Fig. 6.

Excision concluded.
Few papers related to this technique appeared in the Literature until 2001 when Lam et al. 5 reported on a comparison between the two techniques, standard and supra-auricular, in two groups of patients (25 treated with the standard technique and 27 with the supra-auricular) demonstrating how the latter presents a lower recurrence rate (3.7% vs. 32% with the standard technique) and concluding on the greater efficacy of supra-auricular, compared with the standard technique in preauricular sinus treatment. Aim of the present report is to contribute, with our limited experience, to increase the knowledge of the supra-auricular approach, checking the real efficacy in recurrence risk reduction and to contribute to more widespread use of this method.
Patients and methods
Between March 2005 and June 2007, 6 consecutive cases of congenital preauricular sinus, 5 on the right side, one on the left, were treated. The patients, 4 females and 2 males, had a mean age of 21.3 years, (range: 14-44) (Table I).
Table I. Patients, recurrence and follow-up times.
| Sex | Age (yrs) | Previous surgery | Recurrence (mos) | Follow-up (mos) |
| M | 44 | No | – | 7 |
| F | 16 | Yes (2 interventions) | 8 | 12 |
| F | 14 | Yes | 6 | 14 |
| F | 21 | Yes | 8 | 26 |
| M | 16 | No | – | 31 |
| F | 17 | No | – | 34 |
The first patient, a 44-year-old male, had a left preauricular sinus, present for some years but never submitted to surgery. Over the last two years, he had three episodes of infection with classical signs and symptoms: pain, erythema, discharge from pit, each time treated with antibiotics and steroids. The other male patient, 17 years old, underwent surgery for the first time after two infectious episodes. Of the 4 females, 3 had already been treated with standard surgery, two in our hospitals and one elsewhere. A 16-year-old girl presenting a right preauricular sinus, had been treated twice for recurrence, 8 months after the previous intervention. In this case, the clinical examination showed a subcutaneous cyst near the pit, partially adhering to the upper skin. All these cases underwent surgical treatment with the supra-auricular technique according Prasad and Lam 5 13, preceded by fistulography, only in the first two. At present, follow-up is between 7 and 34 months (median 20 months) and no recurrence has been detected. Aesthetic results are very good (Fig. 7).
Fig. 7.

Aesthetic result (7 months).
Discussion
The real problem in the surgical treatment of preauricular sinus is the high recurrence rate following standard techniques due to the high variability of the sinus ramifications, particularly of the terminal ramifications which are difficult for the surgeon to follow. Furthermore, infectious episodes, possibly with abscess, can produce scares that further alter the sinus route. The pre- and intra-operatory precautions, aimed to reduce this trend, are often not sufficient to guarantee absence of pathological recurrence. Data in the literature confirm the limited efficacy of the standard technique and our own experience is in agreement with this conclusion. Therefore, based upon evidence from the literature and on the convincing rationale proposed for the supra-auricular technique, we decided to adopt this approach in all cases of preauricular sinus whether first surgical approach or recurrence following previous surgery. The supra-auricular approach offers fewer execution difficulties since it is not mandatory to isolate and to follow the sinus ramifications as in the standard technique but simply to identify a surgical plane, clearly defined and easy to dissect, such as the temporalis fascia. Moreover, it carries a low recurrence risk: at present (minimum follow-up: 7 months) none of our cases has shown evidence of recurrence; furthermore, it does not result in untoward aesthetic aspects or further pathological conditions for the patients. Last but not least, since this kind of surgery is often performed by not very experienced surgeons, the supra-auricular approach may represent a further guarantee for prevention of recurrences. In conclusion, we are clearly in favour of the supra-auricular technique as first choice treatment not only in recurrence but also in cases never before submitted to surgery.
References
- 1.Scheinfeld NS, Silverberg NB, Weinberg JM, Nozad V. The preauricular sinus: a review of its clinical presentation, treatment, and associations. Pediatr Dermatol 2004;21:191-6. [DOI] [PubMed] [Google Scholar]
- 2.Tan T, Constantinides H, Mitchell TE. The preauricular sinus: a review of its aetiology, clinical presentation and management. Int J Pediatr Otorhinolaryngol 2005;69:1469-74. [DOI] [PubMed] [Google Scholar]
- 3.Paulozzi LJ, Lary JM. Laterality patterns in infants with external birth defects. Teratology 1999;60:265-71. [DOI] [PubMed] [Google Scholar]
- 4.Nofsinger YC, Tom LWC, La Rossa D, Wetmore RF, Handler SD. Periauricular cysts and sinuses. Laryngoscope 1997;107:883-7. [DOI] [PubMed] [Google Scholar]
- 5.Lam HCW, Soo G, Wormald PJ, Van Hasselt CA. Excision of the preauricular sinus: a comparison of two surgical techniques. Laryngoscope 2001;111:317-9. [DOI] [PubMed] [Google Scholar]
- 6.Leung AKC, Robson WLM. Association of the preauricular sinuses and renal anomalies. Urology 1992;40:259-61. [DOI] [PubMed] [Google Scholar]
- 7.Wang RY, Earl DL, Ruder RO, Graham JM. Syndromic ear anomalies and renal ultrasound. Pediatrics 2001;108:e32. [DOI] [PubMed] [Google Scholar]
- 8.Huang XY, Tay GS, Wansaicheong GK, Low WK. Preauricular sinus: clinical course and associations. Arch Otolaryngol Head Neck Surg 2007;133:65-8. [DOI] [PubMed] [Google Scholar]
- 9.Smith PG, Dyches TJ, Loomis RA. Clinical aspects of the brachio-oto-renal syndrome. Otolaryngol Head Neck Surg 1984;92:468-75. [DOI] [PubMed] [Google Scholar]
- 10.Baatenburg de Jong R. A new surgical technique for treatment of preauricular sinus. Surgery 2005;137:567-70. [DOI] [PubMed] [Google Scholar]
- 11.Currie AR, King WWK, Vlantis AC. Pitfalls in the management of preauricular sinuses. Br J Surg 1996;83:1722-4. [DOI] [PubMed] [Google Scholar]
- 12.Gur E, Yeung A, Al-Azzawi M. The excised preauricular sinus in 14 years of experience: is there a problem? Plast Reconstr Surg 1998;102:1405-8. [DOI] [PubMed] [Google Scholar]
- 13.Prasad S, Grundfast K, Milmore G. Management of congenital preauricular pit and sinus tract in children. Laryngoscope 1990;100:320-1. [DOI] [PubMed] [Google Scholar]
- 14.Yeo S, Jun B, Park S, Lee J, Song C, Chang K, et al. The preauricular sinus: factors contributing to recurrence after surgery. Am J Otolaryngol 2006:27:396-400. [DOI] [PubMed] [Google Scholar]
- 15.Coatesworth AP, Patmore H, Jose J. Management of an infected preauricular sinus, using a lacrimal probe. J Laryngol Otol 2003;117:983-4. [DOI] [PubMed] [Google Scholar]
- 16.Martín-Granizo R, Pérez-Herrero MC, Sánchez-Cuéllar. A methylene blue staining and probing for fistula resection: application in a case of bilateral congenital preauricular fistulas. Int J Oral Maxillofac Surg 2002;31:439-41. [DOI] [PubMed] [Google Scholar]
- 17.Tang IP, Shashinder S, Kuljit S, Gopala KG. Outcome of patients presenting with preauricular sinus in a tertiary centre – a five year experience. Med J Malaysia 2007;62:53-5. [PubMed] [Google Scholar]


