Abstract
A sensitive and specific method for extraction and quantification of Δ9-tetrahydrocannabinol (THC), 11-hydroxy-Δ9-tetrahydrocannabinol (11-OH-THC), and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THCCOOH) in human urine was developed and fully validated. To ensure complete hydrolysis of conjugates and capture of total analyte content, urine samples were hydrolyzed by two methods in series. Initial hydrolysis was with Escherichia coli β-glucuronidase (Type IX–A) followed by a second hydrolysis utilizing 10N NaOH. Specimens were adjusted to pH 5−6.5, treated with acetonitrile to precipitate protein, and centrifuged, and the supernatants were subjected to solid-phase extraction. Extracted analytes were derivatized with BSTFA and quantified by gas chromatography–mass spectrometry with electron impact ionization. Standard curves were linear from 2.5 to 300 ng/mL. Extraction efficiencies were 57.0−59.3% for THC, 68.3−75.5% for 11-OH-THC, and 71.5−79.7% for THCCOOH. Intra- and interassay precision across the linear range of the assay ranged from 0.1 to 4.3% and 2.6 to 7.4%, respectively. Accuracy was within 15% of target concentrations. This method was applied to the analysis of urine specimens collected from individuals participating in controlled administration cannabis studies, and it may be a useful analytical procedure for determining recency of cannabis use in forensic toxicology applications.
Introduction
Cannabis (marijuana, hashish) obtained from the complex Cannabis sativa plant is the most widely used illicit drug in the world. Self administered for its mood-altering properties, cannabis dependence and tolerance can develop. Euphoria, relaxation, altered-time perception, lack of concentration, and impaired learning and memory characterize its unique spectrum of behavioral effects (1). There also is increasing interest in therapeutic effects of cannabinoids and in development of potential cannabinoid medications (2,3). Cannabinoids are being investigated for treatment of chronic pain, muscle spasticity, nausea, AIDS wasting disease, and other conditions (4–7). Because of the prevalence of illicit use and increasing interest in cannabinoid chemistry and toxicology, development of accurate and sensitive analytical methods for quantification of cannabinoids in biological fluids is required. Procedures capable of quantifying Δ9-tetrahydrocannabinol (THC), the major psychoactive component of cannabis, and other cannabinoids are necessary to determine concentration-effect relationships (8).
Measurement of urine cannabinoid concentrations is necessary for pharmacokinetic studies, drug treatment, workplace drug testing, drug impaired driving investigations, and for evaluating recency of cannabis use (9–11). Urine specimens have the advantage of relative ease of collection and adequate volume for testing. Detailed urine collection procedures with comprehensive chain-of-custody documentation have been developed for forensic applications.
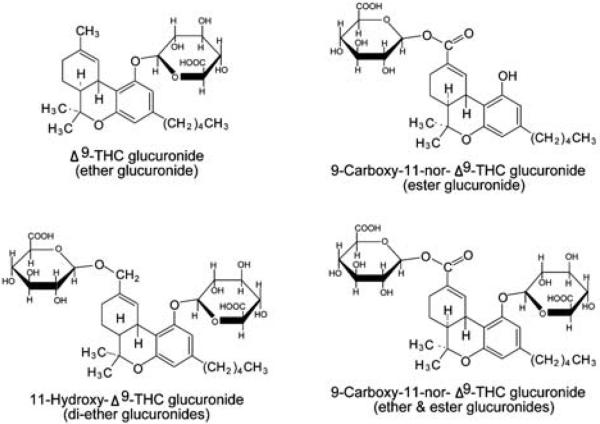
Initially, it was thought that THC and 11-hydroxy-Δ9-tetrahydrocannabinol (11-OH-THC) were not significantly excreted in urine (12). However, THC and its hydroxylated and carboxylated metabolites are conjugated prior to urinary excretion. Urine cannabinoid conjugates can be quantified by liquid chromatography–mass spectrometry (LC–MS and LC–MS–MS) techniques (13–16), but widely used gas chromatography–mass spectrometry (GC–MS) methods require hydrolysis of urine conjugates prior to extraction and analysis to capture total analyte concentration. Cannabinoids are rapidly and extensively metabolized by hepatic enzymes (17–19). The major pathway involves hydroxylation to 11-OH-THC, a psychoactive metabolite, followed by further oxidation to inactive 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THCCOOH). THC and its metabolites subsequently undergo phase II biotransformation to glucuronide conjugates. Glucuronide conjugates have enhanced water solubility facilitating urinary excretion (17). THC and its hydroxylated metabolites are conjugated through ether bonds between the hydroxyl moiety of the phenolic ring and also C-11 for 11-OH-THC and glucuronic acid (10). THCCOOH metabolite forms this ether bond as well, but predominately forms an ester bond between the glucuronide and carboxyl moiety at C-11 (10). The chemical structures of THC, 11-OH-THC, and THCCOOH glucuronides are presented in Figure 1. Two different numbering systems, the dibenzopyran (Δ9) and the monoterpene (Δ1), are used in the literature to describe THC. The dibenzopyran system will be used throughout this manuscript.
Figure 1.
Chemical structures of THC, 11-OH-THC, and THCCOOH glucuronides.
An effective method to measure THC and 11-OH-THC in urine is needed to test the hypothesis that THC and/or 11-OH-THC in this matrix are reliable markers for recent cannabis use. Kemp et al. (10) first proposed that the presence of these cannabinoids in urine indicated recent cannabis use. Manno et al. (9) later suggested that urinary THC concentrations > 2 ng/mL, following enzymatic hydrolysis with E. coli β-glucuronidase, were indicative of cannabis exposure within 8 h of specimen collection. However, the work of both investigators only extended for 8 h after controlled drug administration. Predicting the recency of cannabis consumption is important for estimating the potential impairing effects of the drug, and determining its contributions to accident causation.
The purpose of this study was to develop and validate a sensitive and specific procedure for simultaneous extraction and quantification of THC, 11-OH-THC, and THCCOOH in human urine. Additionally, evaluation of β-glucuronidase enzyme and alkaline hydrolysis, and the benefits of tandem enzyme-alkaline hydrolysis for optimal recovery of THC, 11-OH, and THCCOOH was conducted. Solid-phase extraction (SPE) was optimized to isolate the three cannabinoid analytes from urine in a single eluent. Separation and specific quantification was accomplished by GC–MS operated in selected ion monitoring mode. This procedure was applied to the analysis of urine specimens collected in a controlled drug administration paradigm.
Experimental
Standards and reagents
THC, 11-OH-THC, THCCOOH, THC-d3, 11-OH-THC-d3, and THCCOOH-d3 standards and interferants were purchased from Cerilliant (Austin, TX). Stock Δ9-THC-glucuronide was obtained from ElSohly Laboratories (Oxford, MS). β-Glucuronidase (E. coli, type IX-A) was from Sigma (St. Louis, MO), and N,O-bis(trimethylsilyl)trifluoroacetamide (BSTFA) containing 1% trimethylchlorosilane (TMCS) was from Pierce Chemical (Rockford, IL). Solvents were HPLC grade and obtained from Mallinckrodt Baker (Phillipsburg, NJ). Ammonium hydroxide, glacial acetic acid, hydrochloric acid, dibasic potassium phosphate, monobasic potassium phosphate, sodium acetate, and sodium hydroxide were ACS reagent grade and purchased from Mallinckrodt Baker (Phillipsburg, NJ). SPE columns (Clean Screen ZSTHC020) and vacuum manifolds were obtained from United Chemical Technologies (Bristol, PA). Drug free urine was obtained from volunteers and evaluated by GC–MS to ensure absence of cannabinoids.
Calibrators and controls
Three intermediate standards at concentrations of 200, 2000, and 10,000 ng/mL, each containing THC, 11-OH-THC, and THCCOOH, were prepared in methanol by diluting 1.0 mg/mL stock standards. Different lots of Cerilliant stock standards were used to prepare quality control samples at the same concentrations. Working calibrators (2.5, 5, 10, 50, 150, and 300 ng/mL THC, 11-OH-THC, and THCCOOH) were made daily by fortifying blank urine. Low, medium, and high quality control samples also were prepared daily in blank urine at concentrations of 7.5, 75, and 250 ng/mL for all analytes.
Working deuterated internal standard solution containing 1000 ng/mL each of THC-d3, 11-OH-THC-d3, and THCCOOH-d3 was prepared in methanol. Fifty microliters of working internal standard was added to each sample prior to extraction, giving a final concentration of 25 ng/mL THC-d3, 11-OH-THC-d3, and THCCOOH-d3. Standard solutions were stored at −20°C when not in use.
In-house hydrolysis quality control was prepared by pooling human urine specimens from study subjects. The combined pool was aliquotted and stored at −20°C.
Preparation of working enzyme solution
One million Fishman units stock β-glucuronidase were diluted to 50 mL with 0.1M potassium phosphate buffer (pH 6.8) to prepare working enzyme solution. Five-hundred microliters working enzyme solution was added to each 2-mL urine sample (5000 units/mL urine).
Specimen preparation
Working calibrators and quality control samples were prepared in 16 × 100-mm screw-top glass culture tubes by the addition of 2 mL blank urine, appropriate amount of calibrator or quality control solution, and 50 μL of working internal standard. Two milliliters of 0.1M potassium phosphate buffer (pH 6.8) and 0.5 mL of working β-glucuronidase were added. Tubes were capped, vortex mixed gently, and incubated for 16 h at 37°C in a shaking water bath. After allowing specimens to cool to room temperature, 80 μL 10N sodium hydroxide was added (specimen pH > 10). Tubes were capped, vortex mixed, and hydrolyzed in a dry heating block for 20 min at 60°C. After cooling to room temperature, 50 μL concentrated glacial acetic acid, 2 mL acetonitrile, and 2 mL 2N sodium acetate buffer pH 4.0 were added, and tubes were vortex mixed and centrifuged for 10 min at 1800 × g.
The extraction procedure was a modification of a published application (20). SPE columns were conditioned by sequential addition of 3 mL methanol, 3 mL deionized water, and 2 mL 0.1N acetic acid. Supernatants were applied to conditioned SPE columns under low vacuum. Columns were washed with 3 mL deionized water and 2 mL 0.1N hydrochloric acid/acetonitrile (70:30, v/v) and dried by full vacuum for 10 min. After priming the sorbent bed with 0.2 mL hexane, analytes were eluted with 5 mL elution solvent (hexane/ethyl acetate 80:20, v/v) into 15-mL centrifuge tubes containing 0.5 mL ethanol. Eluates were evaporated under nitrogen at 40°C in a Zymark Turbovap® LV Evaporator, reconstituted with 25 μL acetonitrile, vortex mixed, and centrifuged for 5 min at 1800 × g. Concentrated extracts were transferred to autosampler vials, and 20 μL BSTFA containing 1% TMCS was added. Vials were capped and derivatized at 85°C for 30 min.
GC–MS
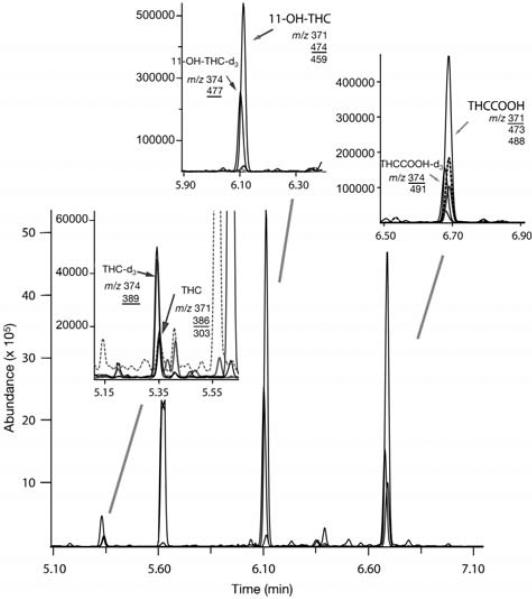
GC–MS analysis was performed using an Agilent 6890 GC interfaced to an Agilent 5973 mass selective detector. The GC was equipped with a 15-m × 0.32-mm i.d., 0.25-μm film thickness DB-35MS capillary column. Helium was used as carrier gas at a constant pressure of 2.0 psi. Two microliters of derivatized extract was injected with a split ratio of 2:1. The injection port and transfer line temperatures were 250°C and 280°C, respectively. The initial column temperature of 100°C was held for 1 min, followed by temperature ramps of 35°C/min to 200°C, 23°C/min to 250°C, and 20°C/min to 325°C held for 1 min. Total separation run time was 10.8 min with a 0.5 min postrun hold at 300°C. The ion source was maintained at 230°C and quadrupole at 150°C. Selected ion monitoring mode was used with a dwell time of 10 ms. Three ions for each analyte and two for each deuterated internal standard were monitored (quantification ions are underlined): THC-d0, m/z 386, 371, 303; THC-d3, m/z 389, 374; 11-OH-THC-d0, m/z 474, 371, 459; 11-OH-THC-d3, m/z 477, 374; THCCOOH-d0, m/z 371, 488, 473; and THCCOOH-d3, m/z 374, 491
Data analysis
Data were acquired and analyzed using Agilent Enhanced ChemStation G1701DA software. Analytes were identified by comparing retention time (± 2%) and relative abundance of qualifier ions. Qualifier ion ratios were required to be ± 20% of the average ion ratios of all calibrators assayed in the same run. Quantification was based upon ratios of target ion peak areas of native analyte to corresponding deuterated internal standard.
Calibration with internal standardization was performed with linear regression curve fitting with a weighting factor of 1/x. Working calibrators at 2.5, 5, 10, 50, 150, and 300 ng/mL were assayed with each batch.
Validation
Linearity
Method linearity was investigated by evaluation of the regression line and expressed by coefficient of determination (r2). Six calibrators were included in each curve and were required to meet all qualitative identification and quantification criteria. Each calibrator was calculated against the linear regression curve. Quantitative accuracy was required to be ± 20% of target. Linearity was achieved with a minimal r2 of 0.990.
Sensitivity
Method sensitivity was evaluated by determining limits of detection (LOD) and quantification (LOQ) for each compound. LOD was defined as lowest concentration for which analyte ion signal-to-noise ratio (determined by peak height) was ≥ 3:1 with satisfactory chromatography (peak shape and resolution), acceptable retention time (± 2% of average calibrator retention time), and qualifier ion ratios within ± 20% of the average of six calibrators. LOQ was defined as lowest concentration that met LOD criteria and had a measured concentration within ± 20% of target in six replicates.
Recovery
Extraction efficiency for each analyte was assessed by adding (d0) analyte to one set (n = 6) of low, medium, and high control samples before SPE and to a second set after SPE, but prior to evaporation. Extraction efficiency (%) was calculated by dividing analyte peak area responses of samples with analyte added before SPE by analyte peak area of samples with analyte added after SPE.
Hydrolysis recovery
Recoveries of glucuronide conjugated THC, 11-OH-THC, and THCCOOH from human urine after different hydrolysis conditions were compared. An in-house quality control pool, containing conjugated analytes, and blank urine fortified with Δ9-THC-glucuronide were assayed without hydrolysis, with enzyme hydrolysis only, 10N NaOH (alkaline) hydrolysis only, and tandem enzyme-alkaline hydrolysis.
Accuracy and precision
Validation samples (n = 6) at three concentrations (7.5, 75, and 300 ng/mL) were analyzed with independent calibration curves on each of five days. Method accuracy, expressed as percentage, was calculated by comparing mean calculated concentrations of THC, 11-OH-THC, and THCCOOH in validation samples to target concentrations. Interassay precision was assessed by calculating percent relative standard deviation (%RSD) of six replicates over six independently calibrated runs (n = 36). Interassay variability also was evaluated using analysis of variance (ANOVA). Intra-assay precision was assessed by calculation of %RSD from data within one run (n = 6). Intra-assay and interassay %RSD were calculated for each concentration.
Selectivity
To evaluate interference and method selectivity, 12 different blank (no analyte or IS added) and negative (IS added) urine specimens were evaluated for co-eluting chromatographic peaks that might interfere with detection of cannabinoid analytes or deuterated internal standards. Internal standard materials also were tested for presence of native analyte ions. To assess possible interference from other commonly available drugs, low quality control samples were spiked individually to contain 10,000 ng/mL of 6-acetylmorphine, acetaminophen, acetylsalicylic acid, benzoylecgonine, brompheniramine, caffeine, chlorpheniramine, dextromethorphan, ephedrine, ibuprofen, methadone, methamphetamine, morphine, nicotine, phencyclidine, phenylpropanolamine, pseudoephedrine, cannabinol, and cannabidiol (CBD). Acceptance criteria required adequate resolution and peak shape and analyte quantification within 20% of target.
Stability
Studies were performed to determine THC, 11-OH-THC, and THCCOOH stability in urine under different conditions. Temperature stability studies were performed on three sets of control samples spiked at 7.5, 75 and 250 ng/mL for each analyte. One set of control samples (n = 6) was stored at −20°C for 72 h and subjected to three freeze/thaw cycles. The second set of samples (n = 6) was maintained at room temperature for 24 h prior to analysis and the third set of samples (n = 6) was refrigerated for 72 h before analysis. Concentrations of analytes were calculated and compared with freshly prepared control samples.
Stability of derivatized extracts maintained at ambient temperature was evaluated after 72 h. Extracted low, medium, and high quality control samples (n = 6) were analyzed immediately after extraction along with calibrators, and reinjected and analyzed after 72 h. All samples were quantified using initial calibration curves.
Clinical specimens
A within-subject, placebo-controlled, double-blind, randomized smoked cannabis administration study was approved by the NIDA Institutional Review Board, and subjects provided written informed consent. Individuals with a history of chronic cannabis use, substantiated with a positive biological test, resided on the secure clinical research unit throughout the study. Urine specimens were collected and stored at −20°C until analysis.
Results
Calibration, LOD, LOQ, and linearity
A total of six assay calibration curves were prepared and evaluated for THC, 11-OH-THC, and THCCOOH. Calculated concentrations of each calibrator were compared to target and were within ± 20%. LOD for each analyte was established by extraction of urine samples containing decreasing concentrations of THC, 11-OH-THC, and THCCOOH, with acceptance criteria as described in the Experimental section. LOD for THC was 1.0 ng/mL and for 11-OH-THC and THCCOOH 2.5 ng/mL. LOQ for all three analytes was 2.5 ng/mL. Quantification failures (not within 20% of target) were exhibited at 0.5 ng/mL for all three analytes. Target ion retention times and S/N ratios for 11-OH-THC and THCCOOH in the 1.0 ng/mL standard were acceptable; however, other LOD criteria, peak shape and qualifier ion ratio, were not consistently met. A summary of calibration data is presented in Table I.
Table I.
Validation Parameters for Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-Δ9-Tetrahydrocannabinol (11-OH-THC), and 11-nor-9-Carboxy-Δ9-Tetrahydrocannabinol (THCCOOH) in Urine by Gas Chromatography–Electron Impact-Mass Spectrometry
| Analyte | LOD (ng/mL) | LOQ (ng/mL) | Linearity (ng/mL) | Regression Equation*Calibration Curves (n = 6) | r2 (mean) |
|---|---|---|---|---|---|
| THC | 1.0 | 2.5 | 300 | y = 0.0348(0.0010)x + 0.0219(0.0914) | 0.999 |
| 11-OH-THC | 2.5 | 2.5 | 300 | y = 0.0341(0.0013)x + 0.0494(0.0312) | 0.995 |
| THCCOOH |
2.5 |
2.5 |
300 |
y = 0.0371(0.0089)x + 0.0211(0.0030) | 0.999 |
Mean value (standard deviation).
Each analyte was adequately resolved (≥ 90% by peak height) from matrix and tested interferants with the chromatographic parameters described. Representative chromatography of blank urine fortified with THC, 11-OH-THC, and THCCOOH at LOQ concentration (2.5 ng/mL) is displayed in Figure 2. Linearity for all analytes was 300 ng/mL and individual calibration curves for all analytes exhibited r2 values ranging from 0.990 to 1.000 (Table I). Negative quality control samples were analyzed after linearity samples to evaluate potential carry-over. No detectable carry-over occurred following samples spiked at the linearity limit (300 ng/mL). Chromatographic resolution of THC, 11-OH-THC, and THCCOOH from a clinical sample containing 8.2 ng/mL THC, 54.2 ng/mL 11-OH-THC, and 83.4 ng/mL THCOOH is shown in Figure 3.
Figure 2.
Extracted ion chromatograms for Δ9-tetrahydrocannabinol-d0 (THC) [m/z 386, 371, 303], 11-hydroxy-Δ9-tetrahydrocannabinol (11-OH-THC) [m/z 474, 371, 459], and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THCCOOH) [m/z 371, 473, 488] in human urine fortified at the limit of quantification (LOQ) for each analyte. LOQ were 2.5 ng/mL for THC, 11-OH-THC, and THCCOOH (A). Quantification ions are underlined. MSD combined ion chromatogram (B).
Figure 3.
Merged ion chromatograms demonstrating separation of -d0 and -d3 Δ9-tetrahydrocannabinol (THC) [m/z 386, 371, 303; 389, 374], 11-hydroxy-Δ9-tetrahydrocannabinol (11-OH-THC) [m/z 371, 474, 459; 374, 477], and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THCCOOH) [m/z 371, 473, 488; 374, 491] from a participant urine specimen containing 8.2 ng/mL THC, 54.2 ng/mL 11-OH-THC, and 83.4 ng/mL THCCOOH. Quantification ions are underlined.
Recovery
Mean extraction efficiencies of THC, 11-OH-THC, and THCCOOH were calculated from six replicates of 7.5, 75, and 250 ng/mL quality control samples. Recoveries for THC, 11-OH-THC and THCCOOH ranged from 57.0 to 59.3%, 68.3 to 75.5%, and 71.5 to 79.7%, respectively.
Hydrolysis recovery
Hydrolysis recovery is shown in Tables II and III. Table II includes results of different hydrolysis conditions with in-house human urine control containing substantial amounts of glucuronide conjugated 11-OH-THC and THCCOOH. THC glucuronide concentrations in the in-house quality control material were below the LOQ for THC. Preliminary data indicate that THC glucuronide generally is found in urine only a few hours after drug administration. If THC was present in a few specimens collected shortly after cannabis smoking, pooling of specimens reduced the average concentration below the LOQ. These hydrolysis results demonstrate that 11-OH-THC was equally recovered by β-glucuronidase enzyme hydrolysis and by enzyme plus alkaline hydrolysis. As previously reported (21), 11-OH-THC and THC ether glucuronide linkages are effectively hydrolyzed with E. coli β-glucuronidase. 11-OH-THC was not recovered from the in-house pool with alkaline hydrolysis. THCCOOH was partially recovered from in-house control with no hydrolysis and enzyme only hydrolysis. Ester bonded THCCOOH glucuronide was effectively recovered following alkaline hydrolysis. The greatest recovery of THC, 11-OH-THC, and THCCOOH was accomplished with enzyme and alkaline hydrolysis.
Table II.
Comparison Recovery of Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-Δ9-Tetrahydrocannabinol (11-OH-THC), and 11-nor-9-Carboxy-Δ9-Tetrahydrocannabinol (THCCOOH) from Inhouse Pool without Hydrolysis, with Enzyme Hydrolysis, with Alkaline Hydrolysis, and with Tandem Hydrolysis (Enzyme and Alkaline)
| Types of Hydrolysis | THC (ng/mL) | 11-OH-THC (ng/mL) | THCCOOH (ng/mL) |
|---|---|---|---|
| No hydrolysis | 0 | 0 | 19.0 |
| 0 | 0 | 19.7 | |
| 0 | 0 | 19.6 | |
| 0 | 0 | 19.3 | |
| 0 | 0 | 19.6 | |
| 0 | 0 | 19.3 | |
| Enzyme hydrolysis | 0 | 21.2 | 28.2 |
| 5000 U/mL | 0 | 21.7 | 28.2 |
| β-glucuronidase | 0 | 21.8 | 28.4 |
| 37°C, 16 h | 0 | 20.4 | 28.2 |
| 0 | 20.4 | 28.5 | |
| Alkaline hydrolysis | 0 | 0 | 81.3 |
| 80 μL 10N NaOH | 0 | 0 | 80.7 |
| 60°C, 20 min | 0 | 0 | 90.6 |
| 0 | 0 | 86.2 | |
| 0 | 0 | 85.6 | |
| 0 | 0 | 86.7 | |
| Enzyme and alkaline (tandem) hydrolysis | 0 | 21.7 | 83.0 |
| 0 | 21.7 | 84.0 | |
| 0 | 21.8 | 83.3 | |
| 0 | 21.4 | 87.5 | |
| 0 | 19.9 | 87.5 | |
| 0 | 21.1 | 81.3 |
Table III.
Comparison of Recoveries of THC from Urine Fortified with Δ9-THC-Glucuronide
| THC Concentration (ng/mL) |
||
|---|---|---|
| Target | Observed* | |
| No Hydrolysis | 20 | 0.0 |
| Enzyme Hydrolysis | 20 | 20.4 ± 0.4 |
| 5000 U/mL β-glucuronidase; 37°C, 16 h | 40 | 41.9 ± 0.7 |
| Alkaline Hydrolysis | 20 | 0.0 |
| Enzyme and Alkaline (Tandem) Hydrolysis | 20 | 20.3 ± 0.2 |
| |
40 | 41.1 ± 0.7 |
Observed concentration: mean ± standard deviation (n = 5).
Urine fortified with Δ9-THC-glucuronide was utilized to evaluate enzyme and alkaline hydrolysis. As shown in Table III, THC ether glucuronide linkages were effectively hydrolyzed with E. coli β-glucuronidase. Results demonstrated that the most effective recovery of all three analytes was achieved with tandem hydrolysis by enzyme and base.
Precision and accuracy
Precision and accuracy were evaluated at three concentrations (7.5, 75, and 250 ng/mL) across the linear dynamic range and are presented in Tables IV and V. Six replicates at each concentration were assayed to determine intra-assay accuracy and precision. Within-run %RSD for all analytes was ≤ 2.4%. Accuracy, calculated as percentage of target concentrations, ranged from 92.0 to 112.5% (Table IV). Interassay precision, determined at the same concentrations, for six batches with six replicates per batch (n = 36) ranged from 2.6 to 7.4% (%RSD). Accuracy, calculated as percent of target, ranged from 101.1 to 113.7% for all analytes at all concentrations. Evaluation of interassay variability using analysis of variance (One-way ANOVA) demonstrated significant differences between days (p ≤ 0.05); however, differences in daily mean analyte concentrations for all controls were less than 14% and were clinically insignificant. Results of interassay precision are shown in Table V.
Table IV.
Intra-assay Precision and Accuracy for Determination of Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-Δ9-Tetrahydrocannabinol (11-OH-THC), and 11-nor-9-Carboxy-Δ9-Tetrahydrocannabinol (THCCOOH) in Human Urine (n = 6)
| Analyte | Expected Concentration (ng/mL) | Observed Concentration (mean ± SD) | Precision (%RSD) | Accuracy (% of target) |
|---|---|---|---|---|
| THC | 7.5 | 8.1 ± 0.2 | 2.0 | 108.0 |
| 75 | 83.2 ± 0.7 | 0.9 | 110.9 | |
| 250 | 258.9 ± 4.6 | 1.8 | 103.6 | |
| 11-OH-THC | 7.5 | 6.9 ± 0.2 | 2.4 | 92.0 |
| 75 | 84.4 ± 0.6 | 0.7 | 112.5 | |
| 250 | 241.5 ± 2.8 | 1.6 | 96.6 | |
| THCCOOH | 7.5 | 8.1 ± 0.1 | 0.8 | 108.0 |
| 75 | 84.3 ± 0.5 | 0.6 | 112.4 | |
| 250 | 264.6 ± 4.3 | 1.6 | 105.8 |
Specificity
Twelve different blank urine specimens were analyzed to evaluate chromatographic interference. No interferences with native or deuterated analyte peaks were detected. Absence of analyte ions in blank urines fortified with internal standards demonstrated that internal standards did not contain relevant amounts of native drug.
Low quality control samples (7.5 ng/mL) containing 10000 ng/mL of potential interferant were assayed to assess exogenous interference. No interference was detected in the drugs tested (n = 19), with the exception of CBD. An increase (> 20% of 7.5 ng/mL target) in THC concentration was observed when CBD was spiked at concentrations greater than 250 ng/mL. Low quality control samples spiked with 50, 100, and 250 ng/mL CBD quantified within ± 20% of target (7.5 ng/mL). Further evaluation was conducted by assaying blank urine samples fortified with 50, 100, 250, or 500 ng/mL CBD. THC was not detectable (> LOD) in any of these CBD-fortified urine samples (n = 3). Blank urine spiked with 500 ng/mL of CBD demonstrated an average of 8.4 ng/mL of THC (n = 3). Conversion of CBD to THC under acid conditions has been previously reported (22,23); the SPE procedure in the present study was conducted at a pH of 4.0.
Stability
Stability of THC, 11-OH-THC, and THCCOOH at low, medium and high quality control concentrations (n = 6) was evaluated after three freeze/thaw cycles, 72 h at 4°C, and 24 h at room temperature (Table VI). Quantification of all quality control samples was within 10% of target following stability challenges.
Table VI.
Stability Data for Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-Δ9-Tetrahydrocannabinol (11-OH-THC), and 11-nor-9-Carboxy-Δ9-Tetrahydrocannabinol (THCCOOH) in Human Urine (n = 6) and Stability of Derivatized Extracts
| Stability in Urine |
Derivatized Extracts |
||||
|---|---|---|---|---|---|
| Analyte | Expected Concentration (ng/mL) | 72 h at −20°C, 3 Freeze/thaw cycles (% of target) | 72 h at 4°C (% of target) | 24 h at Room temperature (% of target) | 72 h at Room temperature (% of target) |
| THC | 7.5 | 99.4 | 102.8 | 97.7 | 99.9 |
| 75 | 101.6 | 101.2 | 96.2 | 100.2 | |
| 250 | 99.9 | 99.0 | 96.2 | 100.4 | |
| 11-OH-THC | 7.5 | 101.3 | 101.6 | 94.3 | 98.7 |
| 75 | 100.3 | 99.3 | 96.0 | 100.7 | |
| 250 | 98.8 | 96.6 | 97.7 | 99.9 | |
| THCCOOH | 7.5 | 99.2 | 98.6 | 98.6 | 100.4 |
| 75 | 99.0 | 96.3 | 96.3 | 100.1 | |
| 250 | 99.4 | 97.7 | 97.7 | 97.9 | |
Stability of analytes after derivatization also was examined. Autosampler vials containing derivatized low, medium and high validation samples were stored at ambient temperature for 72 h following initial analysis. Concentrations of analytes in stored vials were compared to samples analyzed immediately after extraction and derivatization. All analytes were stable, differing from sample injected immediately by less than 3%.
Discussion
The objective of this study was to develop and validate a robust, efficient, and sensitive analytical method for quantification of THC, 11-OH-THC, and THCCOOH in urine. The method had to be adequately sensitive to characterize terminal elimination half-lives of cannabinoid analytes in urine and to test the hypothesis that the presence of THC and/or 11-OH-THC in urine predicted the recency of cannabis use. The goal was to efficiently recover all three analytes in one eluent and to identify and quantify THC, 11-OH-THC and THCCOOH in one GC–MS injection. The method also required a suitable dynamic range for analytes, particularly THCCOOH, which can be present in high concentrations. In addition, it was important to evaluate and optimize hydrolysis of ether and ester glucuronide conjugates. Recovery varies depending on the method of hydrolysis and it is necessary to effectively hydrolyze conjugates to provide optimal analyte recovery.
Cleavage of the ester-linked glucuronide bond of THCCOOH (10,24) can be accomplished under alkaline conditions (25), or enzymatically, using β-glucuronidase (26–29). THC and hydroxylated metabolites such as 11-OH-THC form ether bonds with glucuronic acid, which are not susceptible to cleavage under alkaline conditions (21). Kemp et al. (10) also demonstrated that glucuronidase activity varies with source of enzyme. Enzyme hydrolysis with β-glucuronidase preparations from E. coli recovered significantly greater concentrations of total THC (> 50% increase) and 11-OH-THC (75% increase) compared to Helix pomatia β-glucuronidase (21). Based on these results, β-glucuronidase from E. coli was utilized for hydrolysis of ether-linked conjugates of THC and 11-OH-THC in the present study.
As expected, THC and 11-OH-THC were recovered by enzyme hydrolysis but not by alkaline hydrolysis or when no hydrolysis was performed. As shown in Table III, 20 and 40 ng/mL Δ9-THC-glucuronide were quantitatively recovered with E.coli β-glucuronidase. Our results confirm the previously reported effectiveness of E. coli β-glucuronidase in recovery of THC and 11-OH-THC. Alkaline hydrolysis with 10N NaOH provided more effective recovery of THCCOOH than enzyme, and the tandem enzyme-alkaline hydrolysis procedure demonstrated the most complete recovery of analytes. Combining enzyme and alkaline hydrolysis in sequence enabled efficient recovery of THC, 11-OH-THC, and THCCOOH conjugates. Subsequent SPE provided rapid and efficient extraction of the three analytes in a single elution step.
A simultaneous assay for multiple THC components has been difficult to achieve because of the different physiochemical properties of THC and its more polar metabolites. Several previous methods to extract cannabinoids have required liquid–liquid extraction, preparation of two separate extracts, and two separate GC–MS injections in order to analyze acidic (THCCOOH) and nonacidic (THC and 11-OH-THC) cannabinoids in urine (10,11). Advances in SPE chemistry eliminate the need for liquid–liquid extractions and allow simultaneous extraction of THC, 11-OH-THC, and THCCOOH. Analytical procedures for quantification of THC and THCCOOH, but not 11-OH-THC, in serum, plasma, and blood have been published (30–35). Several recent methods include SPE extraction and quantification of 11-OH-THC with THC and THCCOOH from plasma, serum, or meconium (26,36–38), but not in urine.
THC, 11-OH-THC, and THCCOOH were effectively resolved from matrix in 11.3 min. The three analytes were quantified simultaneously with dynamic ranges of 2.5 to 300 ng/mL. Upper limits of linearity of 300 ng/mL provided effective quantification of most THCCOOH peak concentration clinical samples, although urinary concentrations may exceed this value. Trimethylsilyl derivatization was rapid and reliable and derivatized analytes were stable in the final extract for up to 72 h, enabling repeat chromatographic analysis if necessary.
Production of small amounts of THC from high concentrations of CBD greater than 250 ng/mL) in urine during hydrolysis/extraction was an interesting finding. Blank urines spiked with CBD at 250 ng/mL or less did not have detectable THC; however, blank urine fortified with 500 ng/mL of CBD prior to hydrolysis and extraction demonstrated 8.4 ng/mL THC. CBD concentrations greater than 250 ng/mL are unlikely to be encountered in urine specimens based on reported CBD concentrations of less than 3 ng/mL found in plasma after CBD administration. Guy and Robson (39) evaluated pharmacokinetics of THC, 11-OH-THC and CBD after sublingual, buccal, oro-pharyngeal, and oral administration of 10 mg THC and 10 mg CBD from a cannabis-based medicinal extract. Low plasma concentrations of CBD and THC were always observed. Mean plasma maximal concentrations (Cmax) for THC, CBD, and 11-OH-THC were less than 5, 2, and 7 ng/mL, respectively, across all administration routes (39). In a separate study comparing sublingual administration of 10 mg THC and 10 mg CBD to 10 mg THC in a cannabis-based medicinal extract, Guy and Robson (40) reported that THC's pharmacokinetic properties were not affected by CBD, except for a slight slowing of metabolism of 11-OH-THC to THCCOOH. Mean plasma Cmax concentrations for THC, CBD, and 11-OH-THC were less than 5, 3, and 4 ng/mL, respectively, in this second study. To our knowledge, reports of urine CBD concentrations are not available and should be studied because of the probable future availability of cannabis-based medicinal extracts. In general, cannabis used for recreational use, contains low concentrations of CBD (41).
Conclusions
A validated method for simultaneous detection and quantification of THC, 11-OH-THC, and THCCOOH in human urine is presented. The method employs a tandem enzyme-alkaline hydrolysis step, rapid and economical SPE, and utilizes readily available single-quadrupole GC–MS instrumentation. Acceptable assay characteristics and detection limits were achieved. This assay will be used to test the hypothesis that THC and/or 11-OH-THC in urine predicts recent use of cannabis within 8 h of specimen collection.
Table V.
Interassay Precision and Accuracy for Determination of Δ9-Tetrahydrocannabinol (THC), 11-Hydroxy-Δ9-Tetrahydrocannabinol (11-OH-THC), and 11-nor-9-Carboxy-Δ9-Tetrahydrocannabinol (THCCOOH) in Human Urine (n = 36)
| Analyte | Expected Concentration (ng/mL) | Observed Concentration (mean ± SD) | Precision (%RSD) | Accuracy (% of target) |
|---|---|---|---|---|
| THC | 7.5 | 8.2 ± 0.4 | 4.6 | 109.3 |
| 75 | 85.3 ± 2.9 | 3.4 | 113.7 | |
| 250 | 270.2 ± 9.1 | 3.4 | 108.1 | |
| 11-OH-THC | 7.5 | 7.9 ± 0.6 | 7.4 | 106.8 |
| 75 | 86.7 ± 2.8 | 3.3 | 115.6 | |
| 250 | 247.3 ± 6.9 | 2.8 | 101.1 | |
| THCCOOH | 7.5 | 8.1 ± 0.4 | 4.7 | 108.0 |
| 75 | 82.1 ± 2.1 | 2.6 | 109.5 | |
| 250 | 256.4 ± 7.0 | 2.7 | 102.6 |
Acknowledgment
This research was supported by the Intramural Research Program of the National Institute on Drug Abuse, National Institutes of Health. The authors would like to acknowledge Allan J. Barnes and Karl B. Scheidweiler of NIDA for their technical assistance.
References
- 1.Gorelick DA, Heishman SJ. Methods for clinical research involving cannabis administration. In: Onaivi ES, editor. Methods in Molecular Medicine: Marijuana and Cannabinoid Research. Humana Press; Totowa, NJ: 2005. pp. 235–253. [DOI] [PubMed] [Google Scholar]
- 2.Guy GW, Whittle BA, Robson PJ. The Medicinal Uses of Cannabis and Cannabinoids. Pharmaceutical Press; London, U.K.: 2004. [Google Scholar]
- 3.Blake DR, Robson P, Ho M, Jubb RW, McCabe CS. Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology (Oxford) 2006;45(1):50–52. doi: 10.1093/rheumatology/kei183. [DOI] [PubMed] [Google Scholar]
- 4.Notcutt W, Price M, Miller R, Newport S, Phillips C, Simmons S, Sansom C. Initial experiences with medicinal extracts of cannabis for chronic pain: results from 34 ‘N of 1’ studies. Anaesthesia. 2004;59:440–452. doi: 10.1111/j.1365-2044.2004.03674.x. [DOI] [PubMed] [Google Scholar]
- 5.Wade DT, Makela P, Robson P, House H, Bateman C. Do cannabis-based medicinal extracts have general or specific effects on symptoms in multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult. Scler. 2004;10:434–441. doi: 10.1191/1352458504ms1082oa. [DOI] [PubMed] [Google Scholar]
- 6.Wade DT, Makela PM, House H, Bateman C, Robson P. Long-term use of a cannabis-based medicine in the treatment of spasticity and other symptoms in multiple sclerosis. Mult. Scler. 2006;12:639–645. doi: 10.1177/1352458505070618. [DOI] [PubMed] [Google Scholar]
- 7.Mechoulam R, Hanu L. The cannabinoids: an overview. Therapeutic implications in vomiting and nausea after cancer chemotherapy, in appetite promotion, in multiple sclerosis and in neuroprotection. Pain Res. Manag. 2001;6:67–73. doi: 10.1155/2001/183057. [DOI] [PubMed] [Google Scholar]
- 8.Huestis MA. Pharmacokinetics and metabolism of the plant cannabinoids, Δ9-tetrahydrocannabinol, cannabidiol and cannabinol. In: Pertwee RG, editor. Cannabinoids (Handbook of Experimental Pharmacology) Vol. 168. Springer-Verlag; Heidelberg, Germany: 2005. pp. 657–690. [DOI] [PubMed] [Google Scholar]
- 9.Manno JE, Manno BR, Kemp PM, Alford DD, Abukhalaf IK, McWilliams ME, Hagaman FN, Fitzgerald MJ. Temporal indication of marijuana use can be estimated from plasma and urine concentrations of Δ9-tetrahydrocannabinol, 11-hydroxy-Δ9-tetrahydrocannabinol, and 11-nor-Δ9-tetrahydrocannabinol-9-carboxylic acid. J. Anal. Toxicol. 2001;25:538–549. doi: 10.1093/jat/25.7.538. [DOI] [PubMed] [Google Scholar]
- 10.Kemp PM, Abukhalaf IK, Manno JE, Manno BR, Alford DD, Abusada GA. Cannabinoids in humans. I. Analysis of delta-9-tetrahydrocannabinol and six metabolites in plasma and urine using GC–MS. J. Anal. Toxicol. 1995;19:285–291. doi: 10.1093/jat/19.5.285. [DOI] [PubMed] [Google Scholar]
- 11.Foltz RL, McGinnis KM, Chinn DM. Quantitative measurement of delta-9-tetrahydrocannabinol and two major metabolites in physiological specimens using capillary column gas chromatography negative ion chemical ionization mass spectrometry. Biomed. Mass Spectrom. 1983;10:316–323. doi: 10.1002/bms.1200100503. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Reyes M, Lipton MA, Timmons MC, Wall ME, Brine DR, Davis KH. Pharmacology of orally administered delta-9-tetrahydrocannabinol. Clin. Pharmacol. Ther. 1973;14:48–55. doi: 10.1002/cpt197314148. [DOI] [PubMed] [Google Scholar]
- 13.Franski R, Tezyk A, Wachowiak R, Schroeder G. Influence of mobile phase composition on the high-performance liquid chromatographic/electrospray ionization mass spectro-metric analysis of 11-nor-9-carboxy-delta9-tetrahydrocannabinol (THC-COOH) and its glucuronide in urine. J. Mass Spectrom. 2004;39:458–460. doi: 10.1002/jms.588. [DOI] [PubMed] [Google Scholar]
- 14.Skopp G, Potsch L. An investigation of the stability of free and glucuronidated 11-nor-Δ9-tetrahydrocannabinol-9-carboxylic acid in authentic urine samples. J. Anal. Toxicol. 2004;28:35–40. doi: 10.1093/jat/28.1.35. [DOI] [PubMed] [Google Scholar]
- 15.Skopp G, Potsch L. Stability of 11-nor-Δ9-carboxytetrahydrocannabinol glucuronide in plasma and urine assessed by liquid chromatography-tandem mass spectrometry. Clin. Chem. 2002;48:301–306. [PubMed] [Google Scholar]
- 16.Weinmann W, Vogt S, Goerke R, Muller C, Bromberger A. Simultaneous determination of THC-COOH and THC-COOH-glucuronide in urine samples by LC/MS/MS. Forensic Sci. Int. 2000;113:381–387. doi: 10.1016/s0379-0738(00)00210-3. [DOI] [PubMed] [Google Scholar]
- 17.Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. II. Models for the prediction of time of marijuana exposure from plasma concentrations of delta-9-tetrahydrocannabinol (THC) and 11-nor-9-carboxy-delta-9-tetrahydrocannabinol (THCCOOH). J. Anal. Toxicol. 1992;16:283–290. doi: 10.1093/jat/16.5.283. [DOI] [PubMed] [Google Scholar]
- 18.Peat MA. Distribution of delta-9-tetrahydrocannabinol and its metabolites. In: Baselt RC, editor. Advances in Analytical Toxicology II. Year Book Medical; Chicago, IL: 1989. pp. 186–217. [Google Scholar]
- 19.Agurell S, Halldin M, Lindgren JE, Ohlsson A, Widman M, Gillespie H, Hollister L. Pharmacokinetics and metabolism of delta-tetrahydrocannabinol and other cannabinoids with emphasis on man. Pharmacol. Rev. 1986;38:21–43. [PubMed] [Google Scholar]
- 20.United Chemical Technologies . Application Manual. Vol. 3.5. Bristol, PA: 2007. p. 33. [Google Scholar]
- 21.Kemp PM, Abukhalaf IK, Manno JE, Manno BR, Alford DD, McWilliams ME, Nixon FE, Fitzgerald MJ, Reeves RR, Wood MJ. Cannabinoids in humans. II. The influence of three methods of hydrolysis on the concentration of THC and two metabolites in urine. J. Anal. Toxicol. 1995;19:292–298. doi: 10.1093/jat/19.5.292. [DOI] [PubMed] [Google Scholar]
- 22.Adams R, Pease DC, Cain CK, Clark JH. Structure of cannabidiol. VI. Isomerization of cannabidiol to tetrahydrocannabinol, a physiologically active product. Conversion of cannabidiol to cannabinol. J. Am. Chem. Soc. 1940;62:2402–2405. [Google Scholar]
- 23.Gaoni Y, Mechoulam R. Hashish-VII. The isomerization of cannabidiol to tetrahydrocannabinols. Tetrahedron Lett. 1966;22:1481–1488. [Google Scholar]
- 24.Weinmann W, Vigt S, Goerke R, Muller C, Bromberger A. Simultaneous determination of THC-COOH and THC-COOH-glucuronide in urine samples by LC/MS/MS. Forensic Sci. Int. 2000;113:381–387. doi: 10.1016/s0379-0738(00)00210-3. [DOI] [PubMed] [Google Scholar]
- 25.Meatherall RC, Garriott JC. A sensitive thin-layer chromatographic procedure for the detection of urinary 11-nor-delta 9-tetrahydrocannabinol-9-carboxylic acid. J. Anal. Toxicol. 1988;12:136–140. doi: 10.1093/jat/12.3.136. [DOI] [PubMed] [Google Scholar]
- 26.Gustafson RA, Moolchan ET, Barnes A, Levine B, Huestis MA. Validated method for the simultaneous determination of delta-9-tetrahydrocannabinol (THC), 11-hydroxy-THC and 11-nor-9-carboxy-THC in human plasma using solid phase extraction and gas chromatography–mass spectrometry with positive chemical ionization. J. Chromatogr. B. 2003;798:145–154. doi: 10.1016/j.jchromb.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 27.Langen MCJ, de Bijl GA, Egberts ACG. Automated extraction of 11-nor-Δ9-tetrahydrocannabinol carboxylic acid from urine samples using the ASPEC XL solid-phase extraction system. J. Anal. Toxicol. 2000;24:433–437. doi: 10.1093/jat/24.6.433. [DOI] [PubMed] [Google Scholar]
- 28.Feng S, ElSohly MA, Salamone S, Salem MY. Simultaneous analysis of Δ9-THC and its major metabolites in urine, plasma, and meconium by GC–MS using an immunoaffinity extraction procedure. J. Anal. Toxicol. 2000;24:395–402. doi: 10.1093/jat/24.6.395. [DOI] [PubMed] [Google Scholar]
- 29.ElSohly M, Feng S. Δ9-THC metabolites in meconium: identification of 11-OH-Δ9-THC, 8β, 11-diOH-Δ9-THC, and 11-nor-Δ9-THC-9-COOH as major metabolites of Δ9-THC. J. Anal. Toxicol. 1998;22:329–335. doi: 10.1093/jat/22.4.329. [DOI] [PubMed] [Google Scholar]
- 30.Moeller MR, Doerr G, Warth S. Simultaneous quantitation of delta-9-tetrahydrocannabinol (THC) and 11-nor-9-carboxy-delta-9-tetrahydrocannabinol (THC-COOH) in serum by GC/MS using deuterated internal standards and its application to a smoking study and forensic cases. J. Forensic Sci. 1992;37:969–983. [PubMed] [Google Scholar]
- 31.Kelly P, Jones RT. Metabolism of tetrahydrocannabinol in frequent and infrequent marijuana users. J. Anal. Toxicol. 1992;16:228–235. doi: 10.1093/jat/16.4.228. [DOI] [PubMed] [Google Scholar]
- 32.Huang W, Moody DE, Andrenyak DM, Smith EK, Foltz RL, Huestis MA, Newton JF. Simultaneous determination of Δ9-tetrahydrocannabinol and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol in human plasma by solid phase extraction and gas chromatography–negative ion chemical ionization-mass spec-trometry. J. Anal. Toxicol. 2001;25:531–537. doi: 10.1093/jat/25.7.531. [DOI] [PubMed] [Google Scholar]
- 33.D'Asaro JA. An automated and simultaneous solid-phase extraction of Δ9-tetrahydrocannabinol and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol from whole blood using the Zymark RapidTrace with confirmation and quantitation by GC–EI-MS. J. Anal. Toxicol. 2000;24:289–295. doi: 10.1093/jat/24.4.289. [DOI] [PubMed] [Google Scholar]
- 34.Scurlock RD, Ohlson GB, Worthen DK. The detection of Δ9-tetrahydrocannabinol (THC) and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THCA) in whole blood using two-dimensional gas chromatography and EI-mass spectrometry. J. Anal. Toxicol. 2006;30:262–266. doi: 10.1093/jat/30.4.262. [DOI] [PubMed] [Google Scholar]
- 35.Felgate PD, Dinan AC. The determination of Δ9-tetrahydrocannabinol and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol in whole blood using solvent extraction combined with polar solid-phase extraction. J. Anal. Toxicol. 2000;23:127–132. doi: 10.1093/jat/24.2.127. [DOI] [PubMed] [Google Scholar]
- 36.Steinmeyer S, Bregel D, Warth S, Kraemer T, Moeller MR. Improved and validated method for the determination of Δ9-tetrahydrocannabinol (THC), 11-hydroxy-THC and 11-nor-9-carboxy-THC in serum, and in human liver microsomal preparations using gas chromatography–mass spectrometry. J. Chromatogr. B. 2002;772:239–248. doi: 10.1016/s1570-0232(02)00102-2. [DOI] [PubMed] [Google Scholar]
- 37.Nadulski T, Sporkert F, Schnelle M, Stadelmann AM, Roser P, Schefter T, Pragst F. Simultaneous and sensitive analysis of THC, 11-OH-THC, THC-COOH, CBD, and CBN by GC–MS in plasma after oral application of small doses of THC and cannabis extract. J. Anal. Toxicol. 2005;29:782–789. doi: 10.1093/jat/29.8.782. [DOI] [PubMed] [Google Scholar]
- 38.Coles R, Clements TT, Nelson GJ, McMillin GA, Urry FM. Simultaneous analysis of the Δ9-THC metabolites 11-nor-9-carboxy-Δ9-THC and 11-hydroxy-Δ9-THC in meconium by GC–MS. J. Anal. Toxicol. 2005;29:522–527. doi: 10.1093/jat/29.6.522. [DOI] [PubMed] [Google Scholar]
- 39.Guy GW, Robson PJ. A Phase I, open label, four-way crossover study to compare the pharmacokinetic profiles of a single dose of 20 mg of a cannabis based medicine extract (CBME) administered on 3 different areas of the buccal mucosa and to investigate the pharmacokinetics of CBME per oral in healthy male and female volunteers (GWPK0112). J. Cannabis Ther. 2004;3:79–120. [Google Scholar]
- 40.Guy GW, Robson PJ. A phase I, double blind, three-way crossover study to assess the pharmacokinetic profile of cannabis based medicine extract (CBME) administered sublingually in variant cannabinoid ratios in normal healthy male volunteers (GWPK0215). J. Cannabis Ther. 2004;3:121–152. [Google Scholar]
- 41.Nadulski T, Pragst F, Weinberg G, Roser P, Schnelle M, Fronk EM, Stadelmann AM. Randomized, double-blind, placebo-controlled study about the effects of cannabidiol (CBD) on the pharmacokinetics of Δ9-tetrahydrocannabinol (THC) after oral application of THC verses standardized cannabis extract. Ther. Drug Monit. 2005;27:799–810. doi: 10.1097/01.ftd.0000177223.19294.5c. [DOI] [PubMed] [Google Scholar]