Summary
Cartilage is the grafting material of choice in advanced disorders of the middle ear while the indications for its routine use remain controversial due to the possible detrimental effect on post-operative hearing. Aim of the present study was to report personal experience with “tragal cartilage shield” tympanoplasty. The study focused on 306 adult patients (236 primary procedures and 70 revisions from January 2003 to June 2007). Mean post-operative follow-up was 37 months (range 1-66). The following parameters were evaluated: graft take, change between the pre- and post-operative pure-tone average air-bone gap (PTA-ABG), post-operative complications. Graft take was achieved in 304 patients (99.35%) and there were no immediate post-operative complications. The overall average pre-operative pure-tone average air-bone gap was 43.79 ± 7.07 dB, whereas the post-operative (1 year after surgery) pure-tone average air-bone gap was 10.43 ± 5.25 dB (p < 0.0001). Statistically significant improvement was observed up to 5 years after surgery. This study reveals that tragal cartilage shield tympanoplasty is a reliable technique, in fact it has a high degree of graft take and hearing results are satisfactory. Furthermore, the cartilage is a satisfactory grafting material because it is easily accessible, easy to adapt, resistant to negative middle ear pressures, stable, elastic, well tolerated by the middle ear, resistant to resorption. Therefore, we also recommend its use in less severe middle ear disorders, in which the functional outcome is more essential.
Keywords: Middle ear, Chronic otitis, Tympanoplasty, Tragal cartilage, Shield
Riassunto
La cartilagine rappresenta l’innesto di scelta nelle patologie complicate dell’orecchio medio, mentre le indicazioni per un suo utilizzo di routine rimangono ancora controverse a causa dei presunti effetti negativi sui risultati uditivi. In questo studio riferiamo la nostra esperienza nella timpanoplastica con cartilagine del trago modellata a scudo (Cartilage Shield). Viene riportata la nostra esperienza su 306 pazienti (236 procedure primarie e 70 revisioni, da gennaio 2003 a giugno 2007). Il follow-up post-operatorio medio è stato di 37 mesi (range, 1-66 mesi). Abbiamo valutato i seguenti parametri: attecchimento dell’innesto, modifiche del gap medio via aerea-via ossea prima e dopo l’intervento, complicanze postoperatorie. L’attecchimento dell’innesto è stato ottenuto in 304 pazienti (99,35%) e non si sono registrate complicanze postoperatorie immediate. Il gap medio complessivo via aerea-via ossea prima e ad un anno dopo l’intervento è stato rispettivamente di 43,79 ± 7,07 dB e di 10,43 ± 5,25 dB (p < 0,0001). Miglioramenti significativi sono stati osservati fino a 5 anni dopo l’intervento. Questo studio dimostra che la tecnica della timpanoplastica con cartilagine del trago modellata a scudo è affidabile sia per l’alto tasso di attecchimento dell’innesto sia per i soddisfacenti risultati uditivi. Inoltre la cartilagine si è rivelata un adeguato materiale di innesto perché è facilmente accessibile, adatta al modellamento, resistente alle pressioni negative dell’orecchio medio, stabile, elastica, ben tollerata, resistente al riassorbimento. Per tutti questi motivi raccomandiamo l’utilizzo della cartilagine anche nelle patologie meno severe dell’orecchio medio, laddove l’aspettativa di un buon risultato funzionale è maggiore.
Introduction
The long-term aim of tympanoplasty is to reconstruct the tympanic membrane and the sound conducting mechanism.
Since the introduction of tympanoplasty, in the fifties, by Zoellner 1 and Wullstein 2, numerous graft materials have been used for the closure of the defective membrane: skin, fascia lata, temporalis fascia, vein, perichondrium, dura mater 3–5.
To date, temporalis fascia remains the most commonly employed material for tympanic membrane reconstruction with a success rate of 93-97% in primary tympanoplasties 6.
In certain situations, such as recurrent perforation following myringoplasty, severe attical and/or posterior uncontrolled retraction pockets with cholesteatomatous formation, atelectasis of the tympanic membrane, fascia and perichondrium have been shown to undergo atrophy and subsequent failure, regardless of the placement technique used 7.
In these cases, many surgeons have used cartilage as a grafting material on account of its increased stability and resistance to negative middle ear pressure, even in cases with chronic Eustachian tube dysfunction 8.
It has been shown, both in experimental and clinical studies, that cartilage is well tolerated by the middle ear and shows long-term survival 9 10.
However, acceptance of routine reconstruction of the tympanic membrane with cartilage has been hampered by its reputation of sacrificing maximum hearing improvement, although various Authors have shown that the hearing results are good, regardless of the thickness of the grafts 11–14.
Aim of this study was to report personal experience with “cartilage shield” tympanoplasty. The importance of this research is the large number of patients (306 cases) and the long-term follow-up (up to 66 months).
Material and methods
Patient population and evaluation
From January 2003 to June 2007, tympanoplasty was performed, using tragal cartilage, in 306 patients (127 male, 179 female, age range 18-79 years).
Overall, 236 cases were primary procedures and 70 were revisions in patients operated upon in other Centres.
Of the 236 primary procedures, 124 (52.5%) were for chronic suppurative otitis media (without cholesteatoma) and 112 (47.5%) for cholesteatoma.
Of the 70 revision procedures, 49 (70%) were for recurrence of perforation, 19 (27.1%) for recurrence of cholesteatoma and 2 (2.9%) for lateralized graft.
All patients with cholesteatoma had a second-stage procedure, within 9 to 12 months, for detection of possible recurrence.
Five types of tympanoplasties were performed: Type I (intact ossicular chain, 100 cases (32.7%)), Type III (cartilage graft on stapedial capitulum, 110 cases (35.9%)), Type III (cartilage graft and Partial Ossicular Reconstruction Prosthesis (PORP), 40 cases (13.1%)), Type III (cartilage graft in oval window, 20 cases (6.5%)), Type III (cartilage graft and Total Ossicular Reconstruction Prosthesis (TORP), 36 cases (11.8%)).
The following parameters were evaluated: graft take, change between the pre- and post-operative pure-tone average air-bone gap (PTA-ABG), post-operative complications.
Successful graft take was defined as having no perforation, retraction or lateralization.
The PTA-ABG for each audiogram was evaluated by calculating the mean air-bone gap at 500, 1,000, 2,000 and 4,000 Hz 15. Pre- and post-operative PTA-ABG were compared using Student’s t test.
Post-operative complications included: graft failures, reperforation, sensorineural hearing loss, retraction pockets, prosthesis extrusion, facial nerve injury, recurrent cholesteatoma.
Institutional Review Board approval and patients’ consent were obtained.
Surgical procedure
All procedures were performed by the senior author (M.I.) according to the well-established principles of ear surgery: the ear must be free of disease before the reconstruction of the hearing mechanism.
A post-auricular approach was used under general anaesthesia supplemented with local infiltration of 2% lidocaine with 1:100,000 epinephrine.
The edges of the perforation are scrupulously denuded to promote good capillary blood flow. All tympanic membrane remnants with tympanosclerosis are removed. The middle ear is explored and any pathological material is removed. Of the 112 patients with cholesteatoma, 17 had tympanoplasty with canal wall down mastoidectomy. A cut through the skin and cartilage is made on the medial side of the tragus, leaving 2 mm of cartilage in the dome of the tragus for cosmesis.
The tragal cartilage is harvested together with the perichondrium. This cartilage is ideal since it is thin, flat and in sufficient quantities to permit reconstruction of the entire tympanic membrane. Typically, the piece of cartilage is 15 mm in length and 10 mm in width in children and somewhat larger in adults.
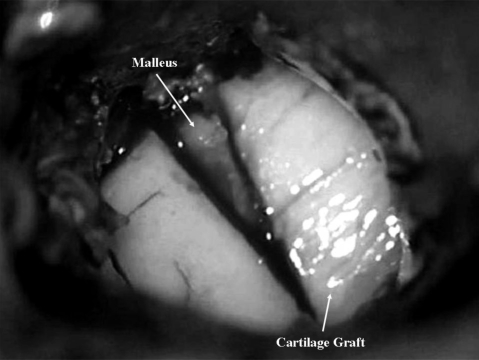
The perichondrium is dissected from both sides and is thinned with a hand press while the cartilage is sized and shaped properly to entirely replace the tympanic membrane. A V-shaped notch is removed from the cartilage shield to accommodate the malleus handle, when present (Fig. 1). The cartilage graft is placed on the same plane as the manubrium of the malleus and medial to tympanic membrane remnants or the fibrous annulus. It has been shown that incorporation of the malleus, in the graft, offers an acoustic gain 16.
Fig. 1.
V-shaped notch removed from cartilage shield to accommodate intact malleus handle.
No space is left between the posterior canal wall (when present) and the reconstructed tympanic membrane to prevent cholesteatoma or retraction pocket recurrence.
Once more experience was gained, this part of the procedure could be accomplished within 10 minutes.
Ossicular reconstruction is performed for cases with ossicular chain defects. The distance between the stapes footplate or superstructure and the medial side of the cartilage graft is measured and a titanium prosthesis (PORP or TORP) or a piece of cartilage is cut to the appropriate length.
The tragal perichondrium is placed lateral to the cartilage and medial to the edges of the perforation and extended posteriorly onto the canal wall, when present (underlay technique).
Pledgets of Spongostan® (Johnson & Johnson Medical S.p.A., Langhorne, PA, USA) are placed over the graft for stabilization. The post-auricular incision is closed in two layers and two Pope wicks impregnated in antibiotic ointment are placed in the ear canal.
Post-operative care
Patients are given water precautions and cautioned against vigorous nose blowing. Sutures were removed one week after surgery and the Spongostan® was suctioned from the ear canal 3 weeks post-operatively. Antibiotic steroid-containing drops are used for a further 2 weeks to clear the ear of residual Spongostan®, which can lead to granulation and fibrous tissue formation if not completely removed from the tympanic membrane.
An audiogram is performed 2 months after surgery and the tympanic membrane is examined. If the hearing result is good and the tympanic membrane is clear, the ear is examined at 6 months and, thereafter, every year. If effusion is detected, nasal steroids are added and the ear is examined every 2 weeks.
Results
Patients’ ages ranged from 18 to 79 years (mean 44.22). Mean post-operative follow-up was 37 months (range 1-66).
Graft-take was achieved in 304 patients (99.35%). In the two failures (revision surgery), a marginal perforation and a lateralization of the graft occurred.
There were no immediate post-operative complications. such as wound infection, haematoma, sensorineural hearing loss or facial nerve injury.
At follow-up, of the 131 patients, 11 (8.4%) who underwent a second-stage procedure for cholesteatoma were found to have limited residual disease, which was treated successfully. Recurrent cholesteatoma was observed in 3 cases (0.98% of total, 2.29% of cholesteatoma cases).
The overall mean pre-operative PTA-ABG was 43.79 ± 7.07 dB, whereas the post-operative (1 year after surgery) PTA-ABG was 10.43 ± 5.25 dB (p < 0.0001). A statistically significant improvement was observed up to 5 years after surgery.
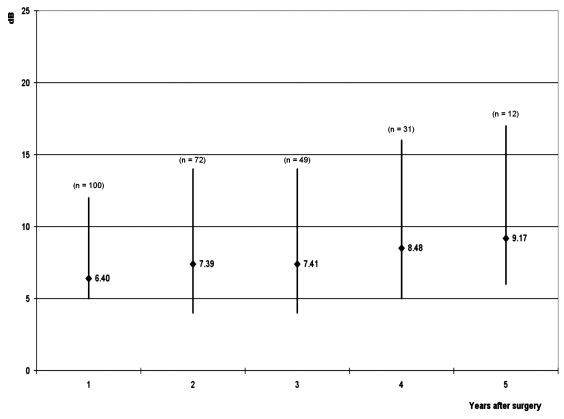
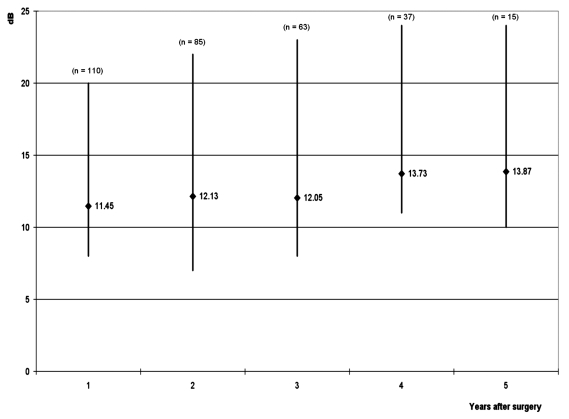
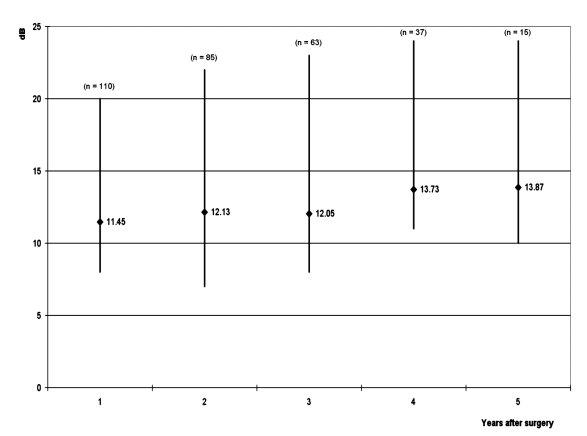
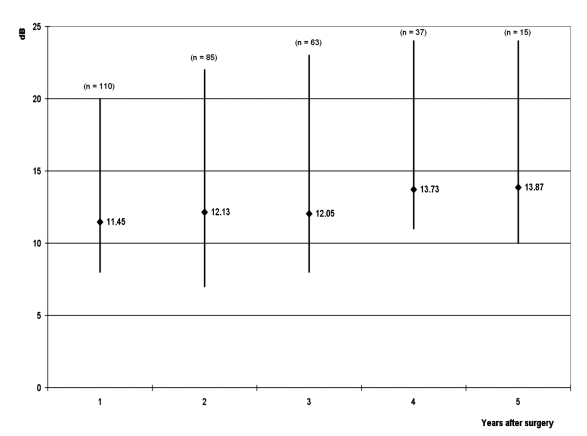
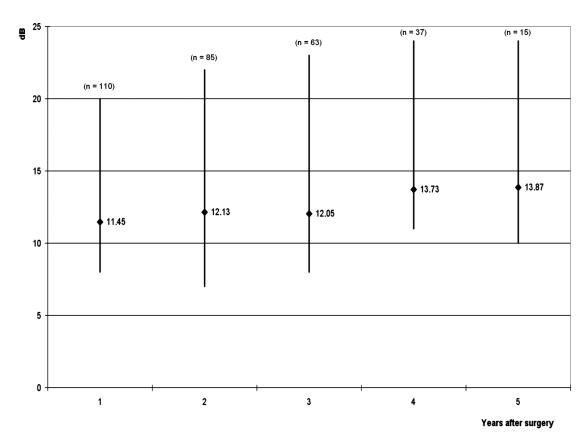
The hearing results, classified for tympanoplasty type and for year, are shown in Tables I– II and in Figures 2– 6.
Table I. Pre- and post-operative (1 year after surgery) PTA-ABG * for different types of tympanoplasty.
| Type of tympanoplasty | n. | PTA-ABG (dB) | P | |
| Pre-operative | Post-operative | |||
| Type I (ossicular chain intact) | 100 | 36.80 ± 1.94 | 6.40 ± 2.20 | < 0.0001 |
| Type III (cartilage graft on the stapedial capitulum) | 110 | 44.55 ± 4.98 | 11.45 ± 3.50 | < 0.0001 |
| Type III(cartilage graft and titanium-PORP) | 40 | 45.00 ± 5.06 | 11.60 ± 3.97 | < 0.0001 |
| Type III(cartilage graft in oval window) | 20 | 54.00 ± 2.05 | 15.80 ± 8.06 | < 0.0001 |
| Type III(cartilage graft and titanium-TORP) | 36 | 53.89 ± 3.19 | 14.25 ± 7.27 | < 0.0001 |
Pure-tone average air-bone gap.
Table II. Post-operative (1 year after surgery) hearing results for different types of Tympanoplasty.
| Type of tympanoplasty | n. | ≤10 dB % |
| Type I (ossicular chain intact) | 100 | 90.0 |
| Type III (cartilage graft on the stapedial capitulum) | 110 | 72.7 |
| Type III(cartilage graft and titanium-PORP) | 40 | 75.0 |
| Type III(cartilage graft in oval window) | 20 | 60.0 |
| Type III(cartilage graft and titanium-TORP) | 36 | 69.4 |
Fig. 2.
Type I Tympanoplasty (ossicular chain intact): Pure-Tone Average Air-Bone Gap at different follow-up times.
Fig. 6.
Type III (cartilage graft and titanium-TORP) Tympanoplasty: Pure-Tone Average Air-Bone Gap at different follow-up times.
Discussion
The use of cartilage in middle ear surgery is not a new concept, but the last decade has shown a renewed interest in this material. It was introduced in middle ear surgery in 1959 17 and has been described for the limited management of retraction pockets 18 19 and, more recently, for the reconstruction of the tympanic membrane in cases of recurrent perforation 8 11 20 21.
The indications for routine use of this more rigid material in tympanoplasty, however, remain somewhat controversial, and the impact on hearing remains to be fully elucidated.
The overall graft take rate of 99.35% (100% in primary tympanoplasties) suggests that cartilage shield tympanoplasty is a reliable technique, which is in agreement with the results of other Authors 8 13 21–23. In fact, the cartilage is nourished mostly by diffusion and becomes well incorporated in the tympanic membrane 18. The thickness of the cartilage creates stiffness that is more resistant than the fascia to the anatomic deformation caused by negative middle ear pressure, thus improving long-term integrity.
The tragal cartilage is typically slightly less than 1 mm thick and therefore is used as a full-thickness graft. Using the Doppler interferometer, Zahnert et al. 24 suggested a slight acoustic benefit by thinning the cartilage to 0.5 mm, but this advantage is offset by the curling of the graft. Therefore, since our hearing results have been good, we recommend full-thickness grafts for cartilage reconstruction of the eardrum.
In fact, an additional advantage of this technique might be considered the good hearing results 8 11–14. Overall, hearing results, in our study, showed a significant improvement as well as stability of the post-operative PTA-ABG. These results were related to the type of tympanoplasty: type I showed better hearing results, the post-operative PTA-ABG (1 year after surgery) improved to 6.4 ± 2.2 dB (90% of the patients in this group had their PTA-ABG reduced to 10 dB or less).
In type III tympanoplasties, no significant differences, based on presence or absence of superstructure of the stapes, were reported. Moreover, the use of prosthesis in comparison to the cartilage alone did not determine significant differences in the hearing threshold.
Further analysis of the patient data revealed that sex and age, at the time of surgery, had no impact on post-operative hearing results.
Various Authors have shown that the audiologic results, following cartilage tympanoplasty are comparable to those after perichondrium 12 or fascia grafting 13 25.
The publication comparing perichondrium and cartilage 12, in revision type I tympanoplasty, showed, in both the groups, an ABG of less than 10 dB. Assuming that replacing a large portion of the tympanic membrane with cartilage would add stiffness and mass, Gerber et al. 13 compared the cartilage to fascia in a frequency-specific manner and again no significant difference was observed. Thus, post-operative hearing loss is probably due to the post-operative changes in the middle ear structures, rather than to the material used for reconstruction.
As far as concerns cholesteatoma, our recurrence rate (2.29%) was quite low as this technique allows excellent approximation between the canal wall and reconstructed tympanic membrane to prevent retraction pocket recurrence.
The results of the present study suggest that cartilage is a good grafting material, in fact it is easily accessible, easy to fashion, resistant to negative middle ear pressures, stable (particularly in cases lacking fibrous annulus), sufficiently elastic for good sound conduction, well tolerated, resistant to resorption. Furthermore, cartilage prevents extrusion of the prosthesis, when this is used for ossicular reconstruction, and, above all, it does not involve additional costs.
A potential drawback of this procedure is the graft opacity, as it may be more difficult to detect eventual residual/recurrent cholesteatoma. However, also the fascia is often not transparent.
Conclusions
Use of tragal cartilage has resulted in a significant improvement in the tympanic membrane reconstruction procedure. Graft take of cartilage shield tympanoplasty has been excellent, hearing results are satisfactory and complications are minimal.
Thanks to its resistance, cartilage is the grafting material of choice in more advanced pathological conditions, such as recurrent perforation after myringoplasty, severe attical and/or posterior uncontrolled retraction pocket with cholesteatomatous formation, atelectasis of the tympanic membrane.
On the other hand, on account of its acoustic properties, comparable to those of fascia, we recommend its use in less severe middle ear disorders, in which the functional outcome is more essential.
Fig. 3.
Type III (cartilage graft on stapedial capitulum) Tympanoplasty: Pure-Tone Average Air-Bone Gap at different follow-up times.
Fig. 4.
Type III (cartilage graft and titanium-PORP) Tympanoplasty: Pure-Tone Average Air-Bone Gap at different follow-up times.
Fig. 5.
Type III (cartilage graft in oval window) Tympanoplasty: Pure-Tone Average Air-Bone Gap at different follow-up times.
References
- 1.Zoellner F. The principles of plastic surgery of the sound-conducting apparatus. J Laryngol Otol 1955;69:567-9. [PubMed] [Google Scholar]
- 2.Wullstein HL. Functional operations in the middle ear with split-thickness skin graft. Arch Otorhinolaryngol 1952;161:422-35. [Google Scholar]
- 3.Heermann H. Tympanic membrane plastic with temporal fascia. Hals Nas Ohren 1960;9:136-9. [Google Scholar]
- 4.Shea JJ. Vein graft closure of eardrum perforations. J Laryngol Otol 1960;74:358-62. [DOI] [PubMed] [Google Scholar]
- 5.Preobrazhenski TB, Rugov AA. The employment of preserved dura mater graft in tympanoplasty. Vestn Otorinolaringol 1965;5:38-42. [PubMed] [Google Scholar]
- 6.Sheehy JL, Anderson RG. Myringoplasty. A review of 472 cases. Ann Otol Rhinol Laryngol 1980;89:331-4. [DOI] [PubMed] [Google Scholar]
- 7.Buckingham RA. Fascia and perichondrium atrophy in tympanoplasty and recurrent middle ear atelectasis. Ann Otol Rhinol Laryngol 1992;101:755-8. [DOI] [PubMed] [Google Scholar]
- 8.Duckert LG, Muller J, Makielski KH, Helms J. Composite autograft “shield” reconstruction of remnant tympanic membranes. Am J Otol 1995;16:21-6. [PubMed] [Google Scholar]
- 9.Yamamoto E, Iwanaga M, Fukumoto M. Histologic study of homograft cartilage implanted in the middle ear. Otolaryngol Head Neck Surg 1988;98:546-51. [DOI] [PubMed] [Google Scholar]
- 10.Hamed M, Samir M, El Bigermy M. Fate of cartilage material used in middle ear surgery light and electron microscopy study. Auris Nasus Larynx 1999;26:257-62. [DOI] [PubMed] [Google Scholar]
- 11.Amedee RG, Mann WJ, Riechelmann H. Cartilage palisade tympanoplasty. Am J Otol 1989;10:447-50. [DOI] [PubMed] [Google Scholar]
- 12.Dornhoffer JL. Hearing results with cartilage tympanoplasty. Laryngoscope 1997;107:1094-9. [DOI] [PubMed] [Google Scholar]
- 13.Gerber MJ, Mason JC, Lambert PR. Hearing results after primary cartilage tympanoplasty. Laryngoscope 2000;110:1994-9. [DOI] [PubMed] [Google Scholar]
- 14.Heermann J. Autograft tragal and conchal palisade cartilage and perichondrium in tympanomastoid reconstruction. Ear Nose Throat J 1992;71:344-9. [PubMed] [Google Scholar]
- 15.Monsell EM. Results and outcomes in ossiculoplasty. Otolaryngol Clin North Am 1994;27:835-40. [PubMed] [Google Scholar]
- 16.Dornhoffer JL, Gardner EK. Prognostic factors in ossiculoplasty: a statistical staging system. Otol Neurotol 2001;22:299-304. [DOI] [PubMed] [Google Scholar]
- 17.Utech H. Tympanotomy in disorders of sound conduction; its diagnostic and therapeutic possibilities. Laryngol Rhinol Otol 1959;38:212-21. [PubMed] [Google Scholar]
- 18.Levinson RM. Cartilage-perichondrial composite graft tympanoplasty in the treatment of posterior marginal and attic retraction pockets. Laryngoscope 1987;97:1069-74. [DOI] [PubMed] [Google Scholar]
- 19.Eviatar A. Tragal perichondrium and cartilage in reconstructive ear surgery. Laryngoscope 1978;88(S11):1-23. [DOI] [PubMed] [Google Scholar]
- 20.Milewski C. Composite graft tympanoplasty in the treatment of ears with advanced middle ear pathology. Laryngoscope 1993;103:1352-6. [DOI] [PubMed] [Google Scholar]
- 21.Dornhoffer J. Cartilage tympanoplasty: indications, techniques, and outcomes in a 1,000-patient series. Laryngoscope 2003;113:1844-56. [DOI] [PubMed] [Google Scholar]
- 22.Aidonis I, Robertson TC, Sismanis A. Cartilage shield tympanoplasty: a reliable technique. Otol Neurotol 2005;26:838-41. [DOI] [PubMed] [Google Scholar]
- 23.Puls T. Tympanoplasty using conchal cartilage. Acta Oto-Rhino-Laryngol Belg 2003;57:187-91. [PubMed] [Google Scholar]
- 24.Zahnert T, Huttenbrink KB, Murbe D, Bornitz M. Experimental investigations of the use of cartilage in tympanic membrane reconstruction. Am J Otol 2000;21:322-8. [DOI] [PubMed] [Google Scholar]
- 25.Kirazli T, Bilgen C, Midilli R, Ogut F. Hearing results after primary cartilage tympanoplasty with island technique. Otolaryngol Head Neck Surg 2005;132:933-7. [DOI] [PubMed] [Google Scholar]