Abstract
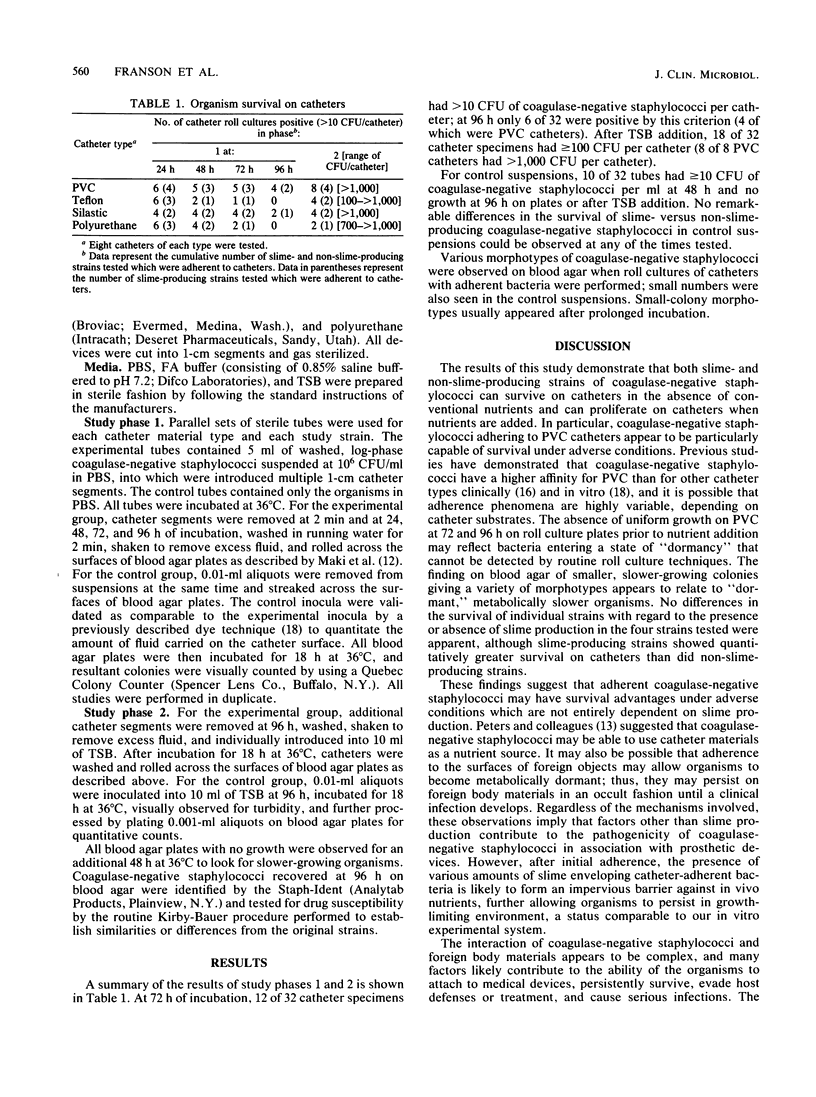
The in vitro survival of coagulase-negative staphylococci in media devoid of routine nutritional supplementation was assessed in the presence and absence of catheter materials to evaluate bacterium-device interactions. Strains of slime- and non-slime-producing coagulase-negative staphylococci were suspended in phosphate-buffered saline together with multiple segments of polyvinyl chloride (PVC), Teflon, Silastic, and polyurethane catheters and in control suspensions without catheters. Catheters were removed at 2 min and 24, 48, 72, and 96 h of incubation and washed thoroughly, and semiquantitative roll cultures were performed on blood agar. In addition, after 96 h catheters were introduced into tryptic soy broth (TSB), and roll cultures were performed after 18 h of incubation. Results demonstrated that after 96 h, 6 of 32 catheter specimens (4 PVC) had greater than 10 CFU of coagulase-negative staphylococci per catheter; after TSB addition, 18 of 32 catheter specimens had greater than or equal to 100 CFU per catheter (8 of 8 PVC catheters had greater than 1,000 CFU per catheter). In control suspensions, no growth was seen at 96 h or after TSB addition. No differences in the survival of slime- versus non-slime-producing strains were observed in control or catheter studies. These findings suggest that both slime- and non-slime-producing coagulase-negative staphylococci survive in vitro on catheters (especially PVC) in the absence of conventional nutrients and can proliferate on catheters when nutrients are added. Catheter-adherent coagulase-negative staphylococci appear to possess survival mechanisms under adverse conditions which may relate to the genesis of occult foreign-body-associated infections.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bandyk D. F., Berni G. A., Thiele B. L., Towne J. B. Aortofemoral graft infection due to Staphylococcus epidermidis. Arch Surg. 1984 Jan;119(1):102–108. doi: 10.1001/archsurg.1984.01390130084015. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Bisno A. L., Parisi J. T., McLaughlin B., Hester M. G., Luther R. W. Nosocomial septicemia due to multiply antibiotic-resistant Staphylococcus epidermidis. Ann Intern Med. 1982 Jan;96(1):1–10. doi: 10.7326/0003-4819-96-1-1. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Parisi J. T., Bisno A. L., Simpson W. A., Beachey E. H. Characterization of clinically significant strains of coagulase-negative staphylococci. J Clin Microbiol. 1983 Aug;18(2):258–269. doi: 10.1128/jcm.18.2.258-269.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982 Jul;37(1):318–326. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald R. H., Jr, Nolan D. R., Ilstrup D. M., Van Scoy R. E., Washington J. A., 2nd, Coventry M. B. Deep wound sepsis following total hip arthroplasty. J Bone Joint Surg Am. 1977 Oct;59(7):847–855. [PubMed] [Google Scholar]
- Gray E. D., Peters G., Verstegen M., Regelmann W. E. Effect of extracellular slime substance from Staphylococcus epidermidis on the human cellular immune response. Lancet. 1984 Feb 18;1(8373):365–367. doi: 10.1016/s0140-6736(84)90413-6. [DOI] [PubMed] [Google Scholar]
- Gristina A. G., Costerton J. W. Bacterial adherence and the glycocalyx and their role in musculoskeletal infection. Orthop Clin North Am. 1984 Jul;15(3):517–535. [PubMed] [Google Scholar]
- James H. E., Walsh J. W., Wilson H. D., Connor J. D., Bean J. R., Tibbs P. A. Prospective randomized study of therapy in cerebrospinal fluid shunt infection. Neurosurgery. 1980 Nov;7(5):459–463. doi: 10.1227/00006123-198011000-00006. [DOI] [PubMed] [Google Scholar]
- Karchmer A. W., Archer G. L., Dismukes W. E. Staphylococcus epidermidis causing prosthetic valve endocarditis: microbiologic and clinical observations as guides to therapy. Ann Intern Med. 1983 Apr;98(4):447–455. doi: 10.7326/0003-4819-98-4-447. [DOI] [PubMed] [Google Scholar]
- Lowy F. D., Hammer S. M. Staphylococcus epidermidis infections. Ann Intern Med. 1983 Dec;99(6):834–839. doi: 10.7326/0003-4819-99-6-834. [DOI] [PubMed] [Google Scholar]
- Maki D. G. Nosocomial bacteremia. An epidemiologic overview. Am J Med. 1981 Mar;70(3):719–732. doi: 10.1016/0002-9343(81)90603-3. [DOI] [PubMed] [Google Scholar]
- Maki D. G., Weise C. E., Sarafin H. W. A semiquantitative culture method for identifying intravenous-catheter-related infection. N Engl J Med. 1977 Jun 9;296(23):1305–1309. doi: 10.1056/NEJM197706092962301. [DOI] [PubMed] [Google Scholar]
- Peters G., Locci R., Pulverer G. Adherence and growth of coagulase-negative staphylococci on surfaces of intravenous catheters. J Infect Dis. 1982 Oct;146(4):479–482. doi: 10.1093/infdis/146.4.479. [DOI] [PubMed] [Google Scholar]
- Sattler F. R., Foderaro J. B., Aber R. C. Staphylococcus epidermidis bacteremia associated with vascular catheters: an important cause of febrile morbidity in hospitalized patients. Infect Control. 1984 Jun;5(6):279–283. doi: 10.1017/s0195941700060331. [DOI] [PubMed] [Google Scholar]
- Schoenbaum S. C., Gardner P., Shillito J. Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis. 1975 May;131(5):543–552. doi: 10.1093/infdis/131.5.543. [DOI] [PubMed] [Google Scholar]
- Sheth N. K., Franson T. R., Rose H. D., Buckmire F. L., Cooper J. A., Sohnle P. G. Colonization of bacteria on polyvinyl chloride and Teflon intravascular catheters in hospitalized patients. J Clin Microbiol. 1983 Nov;18(5):1061–1063. doi: 10.1128/jcm.18.5.1061-1063.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheth N. K., Franson T. R., Sohnle P. G. Influence of bacterial adherence to intravascular catheters on in-vitro antibiotic susceptibility. Lancet. 1985 Dec 7;2(8467):1266–1268. doi: 10.1016/s0140-6736(85)91552-1. [DOI] [PubMed] [Google Scholar]
- Sheth N. K., Rose H. D., Franson T. R., Buckmire F. L., Sohnle P. G. In vitro quantitative adherence of bacteria to intravascular catheters. J Surg Res. 1983 Mar;34(3):213–218. doi: 10.1016/0022-4804(83)90062-8. [DOI] [PubMed] [Google Scholar]



