Mature teratomas (benign cystic teratomas or dermoid cysts) are among the most common ovarian tumours; however, teratomas of the omentum and mesentery are extremely rare.1 The first omental dermoid cyst was described by Lebert in 1734.2 To date, only 29 cases of teratoma of the greater omentum (TGO) have been published. The etiology of these teratomas is not well understood. They are more frequently found in women,1 suggesting a possible association with the female reproductive organs. We describe the case of a woman with TGO.
Case report
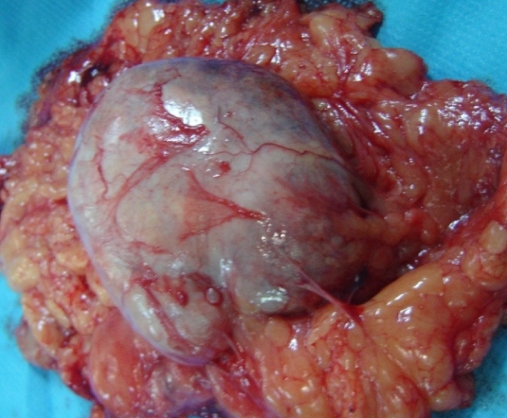
A 55-year-old woman was admitted to hospital for umbilical abdominal pain of a few months’ duration. She had not undergone any surgery or had any gynecologic illness. On admission, physical examination revealed a palpable umbilical mass. Ultrasound and computed tomography (CT) scans (Fig. 1) showed a cystic mass containing small areas of calcification behind the anterior abdominal wall. Preoperative laboratory test results were normal. Pre-operative tumour marker tests revealed no elevation of cancer antigen (CA125, CA19–9, carcinoembryonic antigen and α-fetoprotein). On laparoscopy, we found found a cystic mass measuring 3 × 3 cm attached to the greater omentum. The mass was well defined, and we were able to excise it almost completely from the omentum (Fig. 2). Hair discovered in the tumour suggested that it was a teratoma. Pathological examination of the excised tumour confirmed a typical pattern of benign mature cystic teratoma. The patient recovered well.
Fig. 1.
Computed tomography scan showing a cystic mass with areas of calcification.
Fig. 2.
Teratoma excised from the greater omentum.
Discussion
It is generally accepted that teratomas arise from germ cells that originate in the mature gonads. During early fetal development, germ cells from the yolk sac migrate along the hindgut (route of the mesentery) toward the genital ridge (primitive gonad). These totipotential cells may give rise to a variety of tissues originating from the 3 primitive embryonic layers.3 Migration along the hindgut explains how teratomas may develop in multiple locations.
Teratomas of the greater omentum have been reported more frequently in women. They are typically found in women of reproductive age, but may also appear in young girls and in older women. Mumley and colleagues,1 in 1928, reported a 16.7% occurrence rate of these tumours in men.
The etiology of omental teratomas is poorly understood, but 3 main theories have been proposed to explain their location:
Primary teratomas of the omentum may originate from displaced germ cells.
Teratomas may develop in a supernumerary ovary of the omentum.
Teratomas may result from autoamputation of an ovarian dermoid cyst with secondary implantation into the greater omentum.1,2
For the first theory, no pathological evidence for omental ectopic germ cells has ever been found. The weakness of the second hypothesis is the fact that no case of a normally structured ovary of the greater omentum has ever been reported. The third hypothesis seems to be the most plausible according to most cases, because of the association between mature teratoma of the greater omentum and pathological evidence of ovarian stroma, coexistent unilateral teratoma in the ovary (in 9 cases) or absent ovary (in 9 cases).4 Today, all 3 hypotheses should be considered.
It is difficult to establish a diagnosis preoperatively. The definitive diagnostic finding is the presence of fat and calcification, so CT is the diagnostic modality of choice. In our patient, the discovery of hair in the excised tumour certainly suggested the diagnosis of teratoma. The differential diagnosis of a cystic mesenteric mass includes duplication cysts, cystic mesothelioma, cystic lymphangioma and liposarcoma. Pathological examination must differentiate between mature and immature teratoma. Teratomas of the greater omentum are benign lesions, but malignant transformation of mature cystic teratomas has been described.5
Finally, the management may be easy in cases of mature, localized teratomas. Surgical removal is always necessary, and laparoscopy is the best approach. Immature teratomas are potentially malignant, so the patient may require chemotherapy and radiotherapy.
Footnotes
Competing interests: None declared.
References
- 1.Mumley N. Dermoid cysts of the great omentum. Am J Surg. 1928;5:56. [Google Scholar]
- 2.Lazarus JA, Rosenthal AA. Synchronous dermoid cyst of great omentum and ovary. Ann Surg. 1931;93:1269. [Google Scholar]
- 3.Printz JL, Choate JW, Townes PL, et al. The embryology of supernumerary ovaries. Obstet Gynecol. 1973;41:246–52. [PubMed] [Google Scholar]
- 4.Ushakov FB, Meirow D, Prus D, et al. Parasitic ovarian dermoid tumor of the omentum. A review of the literature and report of two new cases. Eur J Obstet Gynecol Reprod Biol. 1998;81:77–82. doi: 10.1016/s0301-2115(98)00144-4. [DOI] [PubMed] [Google Scholar]
- 5.Kubosawa H, Iwasaki H, Kuzuta N, et al. Adenocarcinoma with peritoneal dissemination secondary to multiple mature teratomas of the omentum. Gynecol Oncol. 2006;101:534–6. doi: 10.1016/j.ygyno.2005.12.041. [DOI] [PubMed] [Google Scholar]