Osteopetrosis refers to a group of disorders characterized by severe impairment of osteoclast-mediated bone resorption. Other terms that are often used for this disease are marble bone disease, which describes the solid radiographic appearance of the involved skeleton, and Albers–Schonberg disease, which refers to the milder, adult form of osteopetrosis, or autosomal dominant osteopetrosis type 2. The major types of osteopetrosis include malignant (severe, infantile, autosomal recessive) osteopetrosis and benign (adult, autosomal dominant) osteopetrosis types I and II. A third form is a rare autosomal recessive type characterized by a carbonic anhydrase II deficiency; it is associated with renal tubular acidosis and cerebral calcification.1 Radiographically, there is a generalized, symmetric increase in bone mass with thickening of both cortical and trabecular bone. Despite the excess bone formation, osteopetrosis bone tends to be brittle in nature.2 There is presently no cure for the disease, but bone marrow transplant is an option for some children.1
Osteoarthritis and periarticular nonunions are indications for joint-replacement surgery in these patients. Most reports of hip-replacement surgery performed in this population focus on total hip arthroplasty (THA) for osteoarthritis.3–9 One previous report discusses THA for femoral neck nonunion with retained hardware.9 Most authors recommend the use of cemented femoral fixation and uncemented acetabular fixation. There are no reports of bipolar hemiarthroplasty in osteopetrosis patients.
We describe a case of cemented bipolar hemiarthroplasty as a salvage option for failed femoral neck fixation with retained hardware, despite end-stage acetabular cartilage degeneration.
Case report
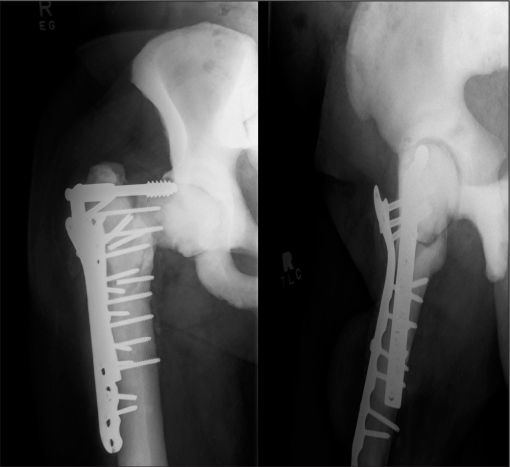
A 58-year-old man sustained a subtrochantric fracture of his right hip in 2005, and this was successfully fixed with a plate and screw construct. In 2006, he fell, causing a right femoral neck fracture that was primarily treated with a dynamic condylar screw and plate. The femoral neck fracture then went on to a nonunion, with failure of the hardware. He presented for consultation to our hospital in September 2007, as he was only able to walk using crutches and was experiencing severe pain in his right hip. Radiographs demonstrated that the femoral neck had collapsed into varus with substantial shortening of the leg. There was generalized bony sclerosis throughout the entire pelvis and right femur with virtually no intramedullary canal secondary to his osteopetrosis. There was a 90° dynamic condylar screw plate and a periarticular plate on the proximal femur. The lag screw was no longer in the femoral head, and there were multiple broken screws in the intramedullary canal of the femur (Fig. 1). The patient was deaf secondary to osteopetrosis involvement of the middle ear bones.
Fig. 1.
Anteroposterior and lateral preoperative radiographs showing failure of fracture fixation with nonunion of the femoral neck fracture.
Anticipating significant blood loss with the surgery, we had the patient cross-matched for 9 units of blood preoperatively. We also used the cell saver10 as a technique of blood salvage for autologous blood transfusion.
For removal of the screws, we had a crown drill set available, as well as carbide-tip burrs. The crown drills were not effective and were dulled by the hard, sclerotic cortical bone. We used the carbide burrs to open the intramedullary canal, as it was very sclerotic.
The acetabulum had substantial cartilage degeneration. We serially reamed the acetabulum to accept a 48-mm bipolar shell with a 28-mm head.
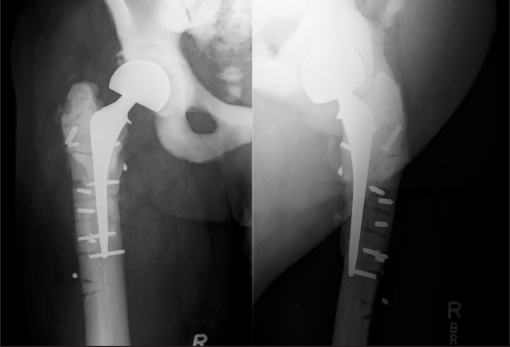
Our femoral implant of choice was a cemented Genesis IV stem (Smith and Nephew) with a bipolar head. We used Simplex T tobramycin-impregnated cement (Stryker) to fill a large defect in the superolateral femoral metaphysis. There was no need for a canal plug, as there was no intramedullary canal past what we created (Fig. 2).
Fig. 2.
Anteroposterior and lateral postoperative radiographs showing cemented bipolar hemiarthroplasty with retention of broken hardware.
At his 6-month follow-up, the patient’s Western Ontario McMaster University Osteoarthritis Index pain and total scores were 1 and 19, respectively.11
Discussion
There are few published articles about total hip arthroplasty in patients with osteopetrosis,3–9 and there is little information on the early and longer-term results, complications and technical difficulties in operating on these patients. There is one other report of hip arthroplasty for failed femoral neck fixation, and those authors performed a THA.9 To our knowledge, we report the first case of bipolar hemiarthroplasty for salvage of femoral neck nonunion with excellent function and pain relief. We elected to not use an acetabular shell to avoid the difficulty of reaming the dense, sclerotic bone and also having to drill holes for screws to fix the cup. The alternative option would be to cement an acetabular cup; however, we were quite concerned about cement interdigitation and the quality of long-term fixation in the marble bone.
Reviewing the literature, the use of cemented femoral stems4–7,9 is more common than uncemented ones.8 All authors encountered the same challenges of narrow femoral canals. In 2 cases, they had prepared a shortened femoral stem,4,5 and in 2 other cases they had to cut stems during surgery.6,7 Different methods have been used to prepare the femoral canal. Ashby4 and Janecki and Nelson6 used both hand reamers and power drills; Matsumo and Katayama5 used high-speed burrs. Jones and Hung8 used drill bits first and then a power reamer, whereas Ramiah9 used tungsten carbide drill bits over a guide wire under radiological guidance. We found using carbide-tip burrs to be effective at both opening the canal and removing broken screws.
In the case of femoral neck nonunion with retained hardware, we report good relief of pain and improvement in function with cemented bipolar hemiarthroplasty in osteopetrosis. Longer-term follow-up will be useful to ensure that our patient will have sustained pain relief despite us not having resurfaced the acetabulum.
Footnotes
Competing interests: None declared for Dr. Salehi. Drs. Gandhi and Davey have received speaker fees and travel assistance from Stryker. Dr. Davey is a paid consultant for both Stryker and Biomet, and has also received speaker fees and travel assistance from Biomet.
References
- 1.Kasper DL, Braunwald E, Fauci AS, et al. Harrison’s principles of internal medicine. 16th ed. New York (NY): McGraw Hill; 2005. [Google Scholar]
- 2.Landa J, Margolis N, Di Cesare P. Orthopedic management of the patient with osteopetrosis. J Am Acad Orthop Surg. 2007;15:654–62. doi: 10.5435/00124635-200711000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Benichou OD. Type 2 autosomal dominant osteopetrosis: clinical and radiological manifestations in 42 patients. Bone. 2000;26:87–93. doi: 10.1016/s8756-3282(99)00244-6. [DOI] [PubMed] [Google Scholar]
- 4.Ashby ME. Total hip arthroplasty in osteopetrosis. Clin Orthop Relat Res. 1992;276:214–21. [PubMed] [Google Scholar]
- 5.Matsuno T, Katayama N. Osteopetrosis and total hip arthroplasty. Report of two cases. Int Orthop. 1997;21:409–11. doi: 10.1007/s002640050196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janecki CJ, Nelson CL. Osteoarthritis associated with osteopetrosis treated by total hip replacement arthroplasty: report of a case. Cleve Clin Q. 1971;38:169–77. doi: 10.3949/ccjm.38.4.169. [DOI] [PubMed] [Google Scholar]
- 7.Cameron HU, Dewar FP. Degenerative osteoarthritis associated with osteopetrosis. CIin Orthop Relat Res. 1977;127:148–9. [PubMed] [Google Scholar]
- 8.Jones DPG, Hung NA. Bilateral, uncemented total hip arthroplasty in osteopetrosis. J Bone Joint Surg Br. 2004;86:276–8. doi: 10.1302/0301-620x.86b2.14354. [DOI] [PubMed] [Google Scholar]
- 9.Ramiah RD. Conversion of failed proximal femoral internal fixation to total hip arthroplasty in osteopetrotic bone. J Arthroplasty. 2006;21:1200–2. doi: 10.1016/j.arth.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 10.Napier JA, Bruce M, Chapman J, et al. Guidelines for autologous transfusion. II. Perioperative haemodilution and cell salvage. British Committee for Standards in Haematology Blood Transfusion Task Force. Autologous Transfusion Working Party. Br J Anaesth. 1997;78:768–71. doi: 10.1093/bja/78.6.768. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]