Mediastinal tumours tend to occur in particular subregions (superior, anterior, middle and posterior), according to their histology, and tumour location is considered to be an important differentiating criterion.1 Tumours in the anterior mediastinum include extragonadal teratomas.2 Teratomas are classified as germ-cell tumours that are composed of ectopic tissues from 2 or 3 germ layers, including mature, immature or malignant components.2 We present the case of a patient with a rare, mature cystic teratoma arising in the posterior mediastinum.
Case report
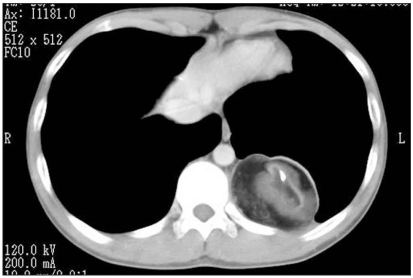
An 18-year-old otherwise healthy man was admitted to the Japan Self-Defense Forces Hospital in Yokosuka, Japan, with dull left subcostal pain. Radiographs, computed tomography scans and magnetic resonance images of the chest demonstrated a unilocular cystic tumour with a sharply defined contour located in the left posterior mediastinum (Fig. 1). The thick wall of the tumour showed heterogeneous densities, suggesting the presence of calcification and fat tissues. Preoperatively, we diagnosed teratoma. The patient did not show signs or symptoms of a testicular tumour or Klinefelter syndrome. Laboratory data were not remarkable, and there was only slight elevation of the serum amylase value.
Fig. 1.
A computed tomography scan of the chest demonstrates a typical mature cystic teratoma in the left posterior mediastinum.
On thoracoscopic examination, we found the tumour to be paravertebral, its surface covered with mediastinal pleura. Aspirated fluid from the tumour was oily. During surgery, we easily detached the tumour from the diaphragm but found that it involved the proximal portion of the left intercostal nerves Th-10 and Th-11 and accompanying vessels. After carefully detaching it from the left sympathetic nerve trunk, we resected the tumour along with the adherent nerves and vessels.
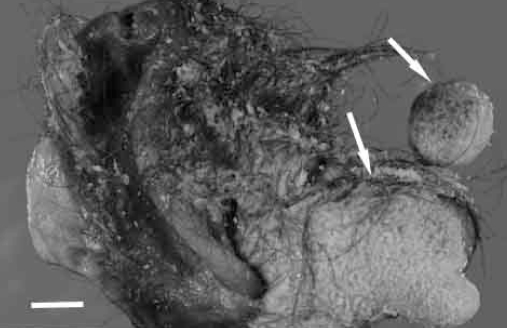
The resected specimen was a unilocular cystic tumour measuring 7.5 × 6.5 × 4.8 cm and weighing 98 g. The cystic cavity was filled with oily and grumous materials containing hair (Fig. 2). We also found a luminal protrusion, called a Rokitansky protuberance, and a tooth. Microscopic examination demonstrated ectopic mature tissues, derived from 3 germ layers, including skin with appendages, fat tissue, glial tissue (ectodermal origin), bone, cartilage (mesodermal origin), salivary gland and intestinal proper muscle layers (endodermal origin). We diagnosed a mature cystic teratoma. Although the tumour had adhered to nerves and vessels, we did not find any on microscopic examination of the specimen. After surgery, the patient recovered well throughout his postoperative and follow-up period.
Fig. 2.
The cut surface of the tumour shows hairs filling the cystic space and a so-called Rokitansky protuberance. Scale bar indicates 1 cm.
Discussion
Teratomas usually occur along the midline of the body, which is the route of germ cell migration during embryogenesis. These migrating germ cells may become “misplaced” en route to their appropriate organs, leading to the development of tumours later in life.3 It has also been suggested that thymic primitive cells lead to anterior mediastinal teratomas;2 however, the “misplacement” theory is more likely because posterior mediastinal teratomas have been reported to comprise 3%–8% of all mediastinal teratomas,4 even though thymic tissue does not usually exist at that site.
In our patient’s case, the preoperative differential diagnosis included neurogenic tumours, because they account for 19%–39% of mediastinal tumours and occur most frequently in the posterior mediastinum.3 These tumours arise from sympathetic ganglia, paraganglia and peripheral nerves, and a variety of neurogenic tumours occur, both benign and malignant, in other parts of the body. Some neurogenic tumours are accompanied by cystic change.5 Furthermore, enteric cysts are included in the differential diagnosis of posterior mediastinal tumour.3 Without typical radiologic findings or awareness of posterior mediastinal teratoma, a correct preoperative diagnosis can be difficult to establish. We recommend preoperative needle aspiration or intraoperative cytology and frozen section examination for posterior mediastinal cystic tumours, as we performed in this patient’s case.
Posterior mediastinal teratoma is a rare entity that can present diagnostic difficulty. Teratomas should be considered in the differential diagnosis of posterior mediastinal tumours.
Footnotes
This work was presented at the 69th annual congress of the Japanese Surgeon’s Association in Yokohama, Japan, on Nov. 29, 2007.
Competing interests: None declared.
References
- 1.Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. 2005;128:2893–909. doi: 10.1378/chest.128.4.2893. [DOI] [PubMed] [Google Scholar]
- 2.Rosai J. Mediastinum. In: Rosai J, editor. Rosai and Ackerman’s surgical pathology. 9th ed. Philadelphia (PA): Mosby; 2004. pp. 459–513. [Google Scholar]
- 3.Shimosato Y, Mukai K. Tumors of the mediastinum. In: Rosai J, editor. Atlas of tumor pathology. Washington (DC): Armed Forces Institute of Pathology; 1997. [Google Scholar]
- 4.Kurosaki Y, Tanaka YO, Itai Y. Mature teratoma of the posterior chest. Eur Radiol. 1998;8:100–2. doi: 10.1007/s003300050347. [DOI] [PubMed] [Google Scholar]
- 5.Scheithauer BW, Woodruff JM, Erlandson RA. Tumors of the peripheral nervous system. In: Rosai J, editor. Atlas of tumor pathology. Washington (DC): Armed Forces Institute of Pathology; 1999. pp. 105–76. [Google Scholar]