Abstract
Background
Outpatient surgery benefits patients and surgeons alike, as it is convenient, safe and cost-effective. We sought to assess the safety and feasibility of outpatient thyroid surgery (OTS) at an ambulatory site affiliated with a teaching hospital.
Methods
We performed a retrospective chart review of patients who underwent hemithyroidectomy, subtotal thyroidectomy, total thyroidectomy or completion thyroidectomy between 2002 and 2004 at the Riverside campus of The Ottawa Hospital. We analyzed patient outcomes based on hospital admission and readmission rates as well as complication rates.
Results
Two hundred and thirty-two patients met our inclusion criteria. Most patients were women (84%) with a mean age of 47 years. Of these patients, 43 had total thyroidectomies, 75 had subtotal thyroidectomies, 42 had left hemithyroidectomies, 57 had right hemithyroidectomies and 18 had completion thyroidectomies; 26% of these procedures were performed to treat cancer. Other pathologies included multinodular goitre (37%), adenoma (21%), nodular hyperplasia (12%) and Hashimoto thyroiditis (4%). The mean duration of surgery was 87 (range 50–150) minutes. No patients died or underwent reoperation. Complications included hypocalcaemia in 6 patients, hematoma in 1 patient, vocal cord injury in 1 patient and wound infection in 2 patients. All patients but 1 were discharged within 10 hours of surgery; the hospital admission rate was 0.4%. Four patients were readmitted within 1 week of surgery (2 for hypocalcemia, 1 for wound infection and 1 for pain control).
Conclusion
Outpatient thyroid surgery is safe and is associated with a low complication rate.
Abstract
Contexte
La chirurgie d’un jour comporte des avantages, tant pour les patients que pour les chirurgiens, car elle est pratique, sécuritaire et économique. Nous avons voulu vérifier la sécurité et la faisabilité des chirurgies d’un jour pour la thyroïde dans un centre de soins ambulatoires affilié à un hôpital universitaire.
Méthodes
Nous avons procédé à une analyse rétrospective des dossiers de patients devant subir une hémithyroïdectomie, une thyroïdectomie partielle, une thyroïdectomie totale ou une totalisation secondaire de thyroïdectomie entre 2002 et 2004, au campus Riverside de l’Hôpital d’Ottawa. Nous avons analysé les résultats obtenus chez les patients sur la base des taux d’hospitalisation, de réadmission et de complications.
Résultats
Deux cent trente-deux patients répondaient à nos critères d’admissibilité. La majorité des patients étaient des femmes (84 %) dont l’âge moyen était de 47 ans. Parmi ces patients, 43 avaient subi une thyroïdectomie totale, 75, une thyroïdectomie partielle, 42, une hémithyroïdectomie gauche, 57, une hémithyroïdectomie droite et 18, une totalisation secondaire de thyroïdectomie; 26 % de ces interventions avaient le cancer pour indication. Les autres pathologies incluaient le goitre multinodulaire (37 %), l’adénome (21 %), l’hyperplasie nodulaire (12 %) et la thyroïdite de Hashimoto (4 %). La chirurgie a duré en moyenne 87 (entre 50 et 150) minutes. Aucun patient n’est décédé ni n’a été réopéré. Parmi les complications survenues, mentionnons l’hypocalcémie chez 6 patients, un hématome chez 1 patient, une lésion des cordes vocales chez 1 patient et l’infection de la plaie chez 2 patients. Tous les patients, sauf 1, ont reçu leur congé 10 heures après l’intervention; le taux d’admission a été de 0,4 %. Quatre patients ont été réadmis dans la semaine suivant leur chirurgie (2 pour hypocalcémie, 1 pour une infection de la plaie et 1 pour contrôle de la douleur).
Conclusion
La chirurgie d’un jour pour la thyroïde est sécuritaire et le taux de complications qui y est associé est faible.
The advent and betterment of outpatient surgery has dramatically changed the landscape of the profession. Just as other innovations such as antibiotics and improved anesthetics have led to better outcomes for surgical patients, outpatient surgery has undoubtedly benefited patients and surgeons alike, as it is convenient, safe and cost-effective. Over the past decade the number of day surgeries performed in Canada has increased by 30%, and the number of procedures requiring hospital admission has dropped by almost 17%.1 However, many surgeons and institutions are hesitant to perform day surgery for some procedures. There are scant reports of outpatient thyroid surgeries (OTS) in the literature. Many of the published studies on this topic have a small cohort of patients; others are highly selective and exclude total thyroidectomies or procedures performed to treat cancer. Finally, in several studies, the procedures are being performed in 23-hour stay units.
Is it safe to discharge patients on the same day as these procedures are performed? We sought to review the outcomes of patients who underwent thyroidectomies in an ambulatory centre affiliated with a teaching hospital. The procedures were performed to treat benign diseases and cancer and included hemithyroidectomies, subtotal thyroidectomies, completion thyroidectomies and total thyroidectomies.
Methods
We conducted a retrospective chart review of OTS performed at the Riverside campus of The Ottawa Hospital between 2002 and 2004. The Riverside campus is an ambulatory centre that is part of The Ottawa Hospital university centre, and its hours of operation are 7:00 am to 7:00 pm. Three general surgeons (S.T., V.M., P.B.) with experience in the field but who did not have exclusive head and neck practices performed the operations. Inclusion criteria for our study are outlined in Box 1. The Ethics Committee of The Ottawa Hospital approved our study.
Box 1.
Inclusion criteria
Patient resides in Ottawa (or will stay in town, within a 1-hour drive from the hospital, for at least 48 hours)
Patient seen in preadmission assessment clinic (by an anesthesiologist) and cleared for day surgery
Patient has adequate support at home (remains in the presence of a second adult for 48 hours)
Patient was observed in the surgical day care unit for at least 4 hours
Hemithyroidectomies and subtotal thyroidectomies completed by 1:00 pm to allow adequate time to monitor
Total thyroidectomies scheduled as the first procedure of the day
Patients considered for this venue saw an anesthesiologist in the preoperative clinic and we asked them to remain in the city (within a 1-hour drive from the hospital) for 48 hours after the operation. We also requested that they remain in the presence of a second adult for the same period of time. We scheduled procedures in the morning, and all completion and total procedures had to be finished by 1:00 pm to allow for adequate observation. The intent was to discharge all of the patients at the end of the observation period, which was a maximum of 10 hours as the ambulatory centre is only accessible until 7:00 pm.
We dedicated substantial time to patient education. Specifically, we provided verbal and written instructions regarding the signs and symptoms of potential complications. Each patient received counselling in the office during the preoperative visit and a pamphlet that stated specific signs and symptoms that would mandate a visit to the emergency department. Patients received a follow-up telephone call from a nurse the day after the procedure. At the time of discharge, patients who underwent completion and total thyroidectomies received prescriptions for calcium replacement (500 mg 4 times/day) to prevent transient hypocalcemia. Finally, follow-up visists took place in clinic 2 weeks after the operation, at which time we measured their serum ionized calcium levels. If the calcium was normal, we advised patients to decrease their calcium doses by half for a total of 2 weeks. After 2 weeks, we repeated the ionized calcium measurement in clinic before discontinuing the calcium replacements altogether. Patients were then followed by their primary care physicians.
If the surgeons or anesthesiologist felt that a patient could not be discharged home, arrangements were made for admission at one of the inpatient campuses of The Ottawa Hospital.
We analyzed patient outcomes with an emphasis on admission and readmission rates as well as complications related to the procedures. We did not analyze patient satisfaction with the day surgery experience.
Results
A total of 232 patients underwent 235 procedures during our study period. Most patients were women (84%) with a a mean age of 47 years. The mean age of the men undergoing thyroid surgery was 50 years. Most patients had American Society of Anesthesia (ASA) scores of 1 or 2; scores were not recorded for some patients (Table 1).
Table 1.
Demographic characteristics and ASA scores of 232 patients who underwent thyroidectomies at The Ottawa Hospital, Riverside campus, from 2002 to 2004
| Characteristic | Measure |
|---|---|
| Women, no. (%) | 195 (84) |
| Age, mean (range) yr | |
| Women | 47 (20–85) |
| Men | 50 (25–68) |
| ASA score, % | |
| 1 | 33 |
| 2 | 55 |
| 3 | 5 |
| Not recorded | 7 |
ASA = American Society of Anesthesia.
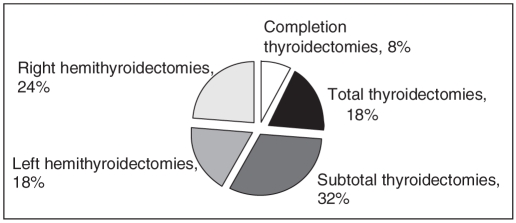
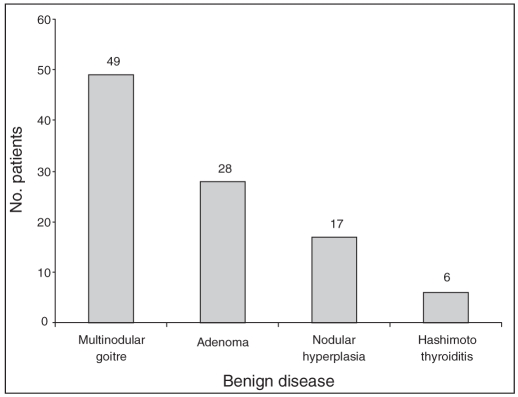
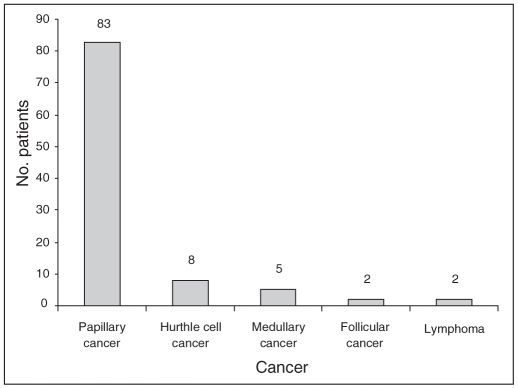
The mean duration of surgery was 87 minutes. The series included 43 total thyroidectomies, 75 subtotal thyroidectomies, 42 left hemithyroidectomies, 57 right hemithyroidectomies and 18 completion thyroidectomies (Fig. 1). We performed 74% of procedures to treat benign disease, including multinodular goiter, adenoma, nodular hyperplasia and Hashimoto thyroiditis (Fig. 2). Cancer accounted for 26% of the procedures and included papillary cancer, Hurthle cell cancer, follicular cancer, medullary cancer and lymphoma (Fig. 3). Patients with medullary thyroid cancer underwent central neck dissections.
Fig. 1.
Breakdown of thyroid procedures performed at The Ottawa Hospital, Riverside campus from 2002 to 2004.
Fig. 2.
Breakdown of patients who underwent thyroidectomies at The Ottawa Hospital, Riverside campus, from 2002 to 2004 to treat benign disease.
Fig. 3.
Breakdown of patients who underwent thyroidectomies at The Ottawa Hospital, Riverside campus, from 2002 to 2004 to treat cancer.
Overall, we discharged 99.6% of patients as planned on the day of the operation. Only 1 patient required admission to the inpatient hospital because of stridor that resolved spontaneously with administration of oxygen. She was admitted after a report of noisy breathing in the recovery room, was observed overnight at an inpatient centre and was subsequently discharged home the next morning with no subsequent complications. No patients died or underwent reoperation.
A nurse contacted patients by telephone the day after their surgeries (or the following Monday if the surgery was completed on a Friday). There were no records of follow-up telephone calls on the charts of 45 patients, and 2 others apparently had given incorrect coordinates and did not receive a call; there were documented follow-up calls in the charts of 187 patients. Of these, 69 calls were unanswered or were received by an answering service. Of the patients we contacted, 63% were able to provide an update on their postoperative condition either directly or through a friend or family member. All but 2 of these patients reported feeling well with minor nausea or discomfort around the incision. The 2 remaining patients reported visiting emergency departments owing to tingling in the fingertips. They both received intravenous calcium and were discharged home with no complications. Presumably, they had documented hypocalcemia on serum analysis, but we did not have access to this information as they were both seen at other hospitals in the region. One of these patients had a subtotal thyroidectomy and was seen on the day of surgery, whereas the other was seen a few days after her surgery and subsequently required admission to our hospital for treatment of transient hypocalcemia. She underwent a total thyroidectomy with reimplantation of the parathyroids into the sternocleidomastoid muscle.
We readmitted 4 patients to hospital, a readmission rate of 1.7%. We readmitted 2 patients for treatment of hypocalcemia. One of them had a total thyroidectomy with reimplantation of the parathyroid glands and was admitted 3 days after her procedure and stayed for a total of 3 days. The other had a subtotal thyroidectomy and was admitted on postoperative day 2 and discharged 4 days later. We readmitted 1 patient with a history of necrotizing fasciitis 2 days after her surgery with suspected wound infection. We kept her for observation for 24 hours and then discharged her with no further issues. Finally, we readmitted 1 patient for pain control. He presented the day after his procedure, and we treated him as an inpatient with oral analgesics and subsequently discharged him.
Postoperative complications included hypocalcemia, hematoma, vocal cord injury, wound infection and postoperative pain (Table 2). Six patients experienced hypocalcemia, as evidenced by symptoms of tingling. No symptoms were permanent, and no patients had serious symptoms such as convulsions or tetany. Of the 4 patients with hypocalcemia who were not admitted, 3 people had undergone total thyroidectomies and 1 had undergone a subtotal thyroidectomy. All 4 of these patients had minor symptoms treated with intravenous calcium in the emergency department and were discharged home with instructions to continue their oral calcium replacement. One patient experienced a hematoma 2 days after a right hemithyroidectomy. The hematoma was drained in the emergency department, and the patient was discharged home in stable condition. One patient experienced left vocal cord injury following subtotal thyroidectomy. She experienced some hoarseness that did not seem to resolve and was subsequently referred to an otolaryngologist. Her airway was never compromised. She continued to have residual hoarseness despite 5 months of therapy. Two patients had wound infections. One had a suspected infection with no objective evidence and was previously described. The other underwent a completion thyroidectomy and required reincision and drainage of an infected neck incision 1 week after surgery.
Table 2.
Complications and readmission rates among 232 patients who underwent thyroidectomies at The Ottawa Hospital, Riverside campus, from 2002 to 2004
| Complication | Total no. (no. admitted) n = 232 | Complication rate, % |
|---|---|---|
| Hypocalcemia | 6 (2) | 2.5 |
| Hematoma | 1 (0) | 0.4 |
| Vocal cord injury | 1 (0) | 0.4 |
| Wound infection | 2 (1) | 0.9 |
| Pain | 1 (1) | 0.4 |
Overall, the admission rate was 0.4%, the readmission rate was 1.7% and mortality was 0%. The incidence of postoperative hypocalcemia was 2.5%, hematoma 0.4%, wound infection 0.9% and vocal cord injury 0.4%.
Discussion
Even though OTS has been performed since the early 1980s,2 it remains a controversial topic with 2 distinct schools of thought. Most of the controversy revolves around the length of time patients should be observed for life-threatening complications following the procedure. Many agree that this depends on the type of thyroid surgery performed, as procedures performed to treat cancer, completion or total thyroidectomies have a greater potential for complications given the extensive dissection involved.3–5
The existing literature on short-stay thyroid surgery exhibits a great deal of variability in definitions, inclusion criteria and results. Some authors define same-day surgery as discharge at hour 23,6–8 whereas others admit patients before their surgeries for optimization.9,10 Other authors exclude patients with cancer2,11–13 because of the theoretical implications of greater complications related to more extensive dissection. Surprisingly, the admission rates in some studies where the intent was to discharge patients home on the same day as surgery were quite high; some authors reported that 14%–100% of their patients were admitted to an inpatient centre because of surgeon or patient preference.2,9,14–17 This may explain the low readmission rates in these studies; most report a readmission rate of 0% compared with our rate of 1.7%. The rate of readmission will naturally be lower if most patients are admitted for observation after surgery. Finally, a large study from the Philippines did not include total thyroidectomies.11
Airway compromise due to hematoma formation is an immediately life-threatening complication that requires close monitoring. These situations may require immediate evacuation of the hematoma and sometimes a second operation to obtain hemostasis. This complication typically occurs early in the postoperative period, and it did not occur in our study, suggesting that an observation period ranging from 4 to 10 hours is appropriate.
Hypocalcemia is more common,4,18 usually occurring within 14–72 hours after surgery. Hypocalcemia rates are reported to range from 6% to 30%.3,5,18–24 Most of the higher rates have been observed in patients who had total thyroidectomies. Many authors report on methods used to predict which patients will experience hypocalcemia.19–22,25–31 Despite useful predictors of hypocalcemia such as measurement of parathyroid hormone that permit early discharge of certain groups of patients, most methods are expensive, time-consuming and not readily available in all centres. In our study, we prescribed oral calcium therapy for patients undergoing subtotal or total thyroidectomy. Furthermore, we instructed patients to document and report symptoms of paraesthesia, which is indicative of hypocalcemia. The incidence of hypocalcemia in our series was 2.5%. A subanalysis of patients undergoing total thyroidectomies shows that hypocalcemia in this group approaches 9%, which is substantially lower than in other series.5,22 No patients experienced permanent hypocalcemia.
The telephone follow-up, although well intended, could have yielded better results. A call from a health professional once the patient has been discharged is a crucial added step that allows same-day discharge of patients undergoing OTS. Not only does it confirm that the patient is not experiencing ill effects as a result of the procedure, it also offers an added level of comfort to the patients and their caregivers. The call-back response rate at our centre would benefit from more stringent follow-up and more detailed documentation on the patients’ charts.
We did not examine the potential financial benefits of OTS. As with other types of outpatient surgeries, hospital costs are reduced when patients are safely discharged home on the day of their surgeries. Outpatient thyroid surgeries are no exception. In fact, many studies have shown financial benefits to OTS.2,6,9,14 Some American studies have shown a savings of as much as 22%–56% compared with the same procedures performed on an inpatient basis. It is unclear what the cost benefit would be in a Canadian centre.
Conclusion
Our review of OTS demonstrates that a short period of observation (4–10 h) is safe and that thyroid surgery can be performed as an outpatient procedure with an acceptable complication rate. However, due diligence is essential as it will undoubtedly serve to establish quality controls and safeguards to potential complications, which in turn will improve the safety of such procedures. Patient education is an essential first step in establishing such a program. Careful patient selection and preoperative assessment provides important safeguards. A follow-up call or appointment, a supportive caregiver and accessible emergency services are also critical for such procedures. Further studies assessing patient satisfaction with day surgery will reinforce the benefits of this approach.
Acknowledgements
We would like to acknowledge the assistance of Melanie Matton, RN, from The Ottawa Hospital, Civic campus, Ottawa, Ont.
Footnotes
Presented in poster format at the Canadian Surgery Forum, Sept. 7–10, 2006, in Calgary, Alta.
Competing interests: None declared.
Contributors: Drs. Trottier and Tadros designed the study. Drs. Tadros, Moonje and Barron acquired the data, which Dr. Trottier analyzed. Drs. Trottier and Tadros wrote the article, which all authors reviewed and approved for publication.
References
- 1.Canadian Institute for Health Information. Trends in acute inpatient hospitalizations and day surgery visits in Canada, 1995–1996 to 2005–2006 [database] Ottawa (ON): The Institute; 2007. [(accessed 2007 January 10)]. Available: http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=bl_hmdb_3jan2007_e. [Google Scholar]
- 2.Steckler RM. Outpatient thyroidectomy: a feasibility study. Am J Surg. 1986;152:417–9. doi: 10.1016/0002-9610(86)90315-6. [DOI] [PubMed] [Google Scholar]
- 3.Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28:271–6. doi: 10.1007/s00268-003-6903-1. [DOI] [PubMed] [Google Scholar]
- 4.Ozbas S, Kocak S, Aydintug S, et al. Comparison of the complications of subtotal, near total and total thyroidectomy in the surgical management of multinodular goiter. Endocr J. 2005;52:199–205. doi: 10.1507/endocrj.52.199. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya N, Fried MP. Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg. 2002;128:389–92. doi: 10.1001/archotol.128.4.389. [DOI] [PubMed] [Google Scholar]
- 6.McHenry CR. “Same-day” thyroid surgery: an analysis of safety, cost savings, and outcome. Am Surg. 1997;63:586–9. [PubMed] [Google Scholar]
- 7.Marohn MR, LaCivita KA. Evaluation of total/near-total thyroidectomy in a short-stay hospitalization: safe and cost-effective. Surgery. 1995;118:943–7. doi: 10.1016/s0039-6060(05)80098-4. [DOI] [PubMed] [Google Scholar]
- 8.Testini M, Nacchiero M, Miniello S, et al. One-day vs standard thyroidectomy. A perspective study of feasibility. Minerva Endocrinol. 2002;27:225–9. [PubMed] [Google Scholar]
- 9.Lo Gerfo P, Gates R, Gazetas P. Outpatient and short-stay thyroid surgery. Head Neck. 1991;13:97–101. doi: 10.1002/hed.2880130203. [DOI] [PubMed] [Google Scholar]
- 10.Matthews TW, Lampe HB, LeBlanc S. Same-day admission thyroidectomy programme: quality assurance study. J Otolaryngol. 1996;25:290–5. [PubMed] [Google Scholar]
- 11.Samson PS, Reyes FR, Saludares WN, et al. Outpatient thyroidectomy. Am J Surg. 1997;173:499–503. doi: 10.1016/s0002-9610(97)00019-6. [DOI] [PubMed] [Google Scholar]
- 12.Cannizzaro MA, Caruso L, Costanzo M, et al. Surgery of thyroid pathologies in one-day surgery. Ann Ital Chir. 2002;73:501–4. [PubMed] [Google Scholar]
- 13.Sahai A, Symes A, Jeddy T. Short-stay thyroid surgery. Br J Surg. 2005;92:58–9. doi: 10.1002/bjs.4746. [DOI] [PubMed] [Google Scholar]
- 14.Mowschenson PM, Hodin RA. Outpatient thyroid and parathyroid surgery: a prospective study of feasibility, safety, and costs. Surgery. 1995;118:1051–3. doi: 10.1016/s0039-6060(05)80113-8. [DOI] [PubMed] [Google Scholar]
- 15.Lo Gerfo P. Outpatient thyroid surgery. J Clin Endocrinol Metab. 1998;83:1097–100. doi: 10.1210/jcem.83.4.4740-1. [DOI] [PubMed] [Google Scholar]
- 16.Spanknebel K, Chabot JA, DiGiorgi M, et al. Thyroidectomy using monitored local or conventional general anesthesia: an analysis of out-patient surgery, outcome and cost in 1,194 consecutive cases. World J Surg. 2006;30:813–24. doi: 10.1007/s00268-005-0384-3. [DOI] [PubMed] [Google Scholar]
- 17.Lo Gerfo P. Local/regional anesthesia for thyroidectomy: evaluation as an outpatient procedure. Surgery. 1998;124:975–8. [PubMed] [Google Scholar]
- 18.Bergamaschi R, Becouarn G, Ronceray J, et al. Morbidity of thyroid surgery. Am J Surg. 1998;176:71–5. doi: 10.1016/s0002-9610(98)00099-3. [DOI] [PubMed] [Google Scholar]
- 19.Payne RJ, Tewfik MA, Hier MP, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. Otolaryngol Head Neck Surg. 2005;133:386–90. doi: 10.1016/j.otohns.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 20.Payne RJ, Hier MP, Tamilia M, et al. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck. 2005;27:1–7. doi: 10.1002/hed.20103. [DOI] [PubMed] [Google Scholar]
- 21.Gulluoglu BM, Manukyan MN, Cingi A, et al. Early prediction of normocalcemia after thyroid surgery. World J Surg. 2005;29:1288–93. doi: 10.1007/s00268-005-0057-2. [DOI] [PubMed] [Google Scholar]
- 22.Chia SH, Weisman RA, Tieu D, et al. Prospective study of perioperative factors predicting hypocalcemia after thyroid and parathyroid surgery. Arch Otolaryngol Head Neck Surg. 2006;132:41–5. doi: 10.1001/archotol.132.1.41. [DOI] [PubMed] [Google Scholar]
- 23.Szubin L, Kacker A, Kakani R, et al. The management of post-thyroidectomy hypocalcemia. Ear Nose Throat J. 1996;75:612–4. [PubMed] [Google Scholar]
- 24.Flyyn MB, Lyons KJ, Tarter JW, et al. Local complications after surgical resection of thyroid carcinoma. Am J Surg. 1994;168:404–7. doi: 10.1016/s0002-9610(05)80085-6. [DOI] [PubMed] [Google Scholar]
- 25.Nahas ZS, Farrag TY, Lin FR, et al. A safe and cost-effective short hospital stay protocol to identify patients at low risk for the development of significant hypocalcemia after total thyroidectomy. Laryngoscope. 2006;116:906–10. doi: 10.1097/01.mlg.0000217536.83395.37. [DOI] [PubMed] [Google Scholar]
- 26.Richards ML, Bingener-Casey J, Pierce D, et al. Intraoperative parathyroid hormone assay: an accurate predictor of symptomatic hypocalcemia following thyroidectomy. Arch Surg. 2003;138:632–6. doi: 10.1001/archsurg.138.6.632. [DOI] [PubMed] [Google Scholar]
- 27.Bellantone R, Lombardi CP, Raffaelli M, et al. Is routine supplementation therapy (calcium and vitamin D) useful after total thyroidectomy. Surgery. 2002;132:1109–12. doi: 10.1067/msy.2002.128617. [DOI] [PubMed] [Google Scholar]
- 28.Husein M, Hier MP, Al-Abdulhadi K, et al. Predicting calcium status post thyroidectomy with early calcium levels. Otolaryngol Head Neck Surg. 2002;127:289–93. doi: 10.1067/mhn.2002.127891. [DOI] [PubMed] [Google Scholar]
- 29.Lam A, Kerr PD. Parathyroid hormone: an early predictor of post-thyroidectomy hypocalcemia. Laryngoscope. 2003;113:2196–200. doi: 10.1097/00005537-200312000-00029. [DOI] [PubMed] [Google Scholar]
- 30.Del Rio P, Arcuri MF, Ferreri G, et al. The utility of serum PTH assessment 24 hours after total thyroidectomy. Otolaryngol Head Neck Surg. 2005;132:584–6. doi: 10.1016/j.otohns.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 31.Tartaglia F, Giuliani A, Sgueglia M, et al. Randomized study on oral administration of calcitriol to prevent symptomatic hypocalcemia after total thyroidectomy. Am J Surg. 2005;190:424–9. doi: 10.1016/j.amjsurg.2005.04.017. [DOI] [PubMed] [Google Scholar]