Careless of censure, nor too fond of fame, Still pleased to praise, yet not afraid to blame, Averse alike to flatter or offend, Not free from faults, nor yet too vain to mend.
Alexander Pope (1711) on the ideal critic
Starting roughly a quarter century ago, American medicine began a dramatic transformation from a system dominated by clinicians’ decision making and professional norms to one in which medical care is expected to reflect the preferences and choices of individual consumers. This growing aspiration toward “medical consumerism” began during the 1970s with a set of popular social movements devoted to giving patients more control over their own treatment and a more informed choice of their physicians (Rodwin 1994). Although the seeds of consumerism were only haphazardly sown and incompletely germinated (Hibbard and Weeks 1987), by the end of the decade they had grown into a noticeable presence in the health care system (Haug and Lavin 1981). During the 1980s, these shifts in popular attitudes were reinforced by public policies and private practices intended to give consumers greater incentives to learn more about their medical choices and to exercise these choices in a cost-conscious manner (Arnould, Rich, and White 1993).
In many ways, the emergence of managed competition seems like the apotheosis of health care consumerism. Its proponents saw the model as a means so “that informed consumers can improve the performance not only of health care markets but of delivery systems as well” (Sofaer 1993, p. 76). The role of the consumer was seen as essential to these new arrangements:
Our society needs to make cost/quality trade-off judgments. These should be made by consumers who are using their own money at the margin … managed competition is compatible with strong American cultural preferences … for limited government, voluntary action, decentralized decision making, individual choice, multiple competitive approaches, pluralism, and personal and local responsibility.
(Enthoven 1993, pp. 40, 46)
Although universal reforms based on managed competition faltered with the rejection of the Clinton administration's Health Security Act in 1994, its principles and major practices have grown increasingly common among large employers (Maxwell, Briscoe, Davidson, et al. 1998), state-administered Medicaid programs (Schlesinger 1997), and, most recently, reforms of the Medicare program (Oberlander 2000). The gospel of medical consumerism is now proclaimed by apostles along a varied ideological spectrum (Herzlinger 1997;Rodwin 1999). Its broad acceptance is reflected in the widespread adoption of report cards measuring the performance of health plans (GAO 1994;Hibbard, Harris-Kojetin, Mullin, et al. 2000), as well as in state regulations intended to protect consumers’ autonomy in choosing among these plans (Miller 1997).
Implicit in all models of market-based reform, and in managed competition reforms in particular, is the notion that consumers respond to unsatisfactory treatment in effective ways. Hirschmann (1970) described two possible responses to dissatisfaction: “exit” (switching to another health plan) and “voice” (complaining to plan administrators to induce them to alter their practices). The first alternative is often quite circumscribed in practice, as employees have little opportunity for exit when their employers contract with a single plan (Davis, Collins, Schoen, et al. 1995) and may not want to change plans if this requires them to end their relationships with their current clinicians (Schlesinger, Druss, Thomas, et al. 1999). As a result, there is growing interest in consumer empowerment by “voicing” concerns about health care (Rodwin 1997, 1999). State regulations are intended to facilitate voice by requiring standardized grievance procedures within plans, third-party arbitration of disputes over coverage, members’ “hot lines” to report complaints about a health plan, and various forms of ombuds programs (Perkins, Olson, and Rivera 1998; Pollitz, Dallek, and Tapay 1998; Tapay, Feder, and Dallek 1998). Most of these approaches make a formal complaint to the health plan the first step in the grievance process.
Ironically, one of the core features of managed competition may discourage, rather than encourage, active consumerism. In theory, consumers assess the performance of their health plan based on their own experience and the standardized information allowing them to compare their plan with available alternatives. Proponents of managed competition argue that it is easier for consumers to assess plans “during the annual enrollment, when they have information, choices, and time for consideration” (Enthoven 1993, p. 29) than to choose among providers when they are sick and actually need treatment. But the introduction of managed care complicates these decisions in ways that may undermine their responses to unsatisfactory treatment, by muddling the process of “blaming” or “blame attribution.”
These terms may not be familiar to most readers, because the role of blaming in health care has rarely been acknowledged and almost never applied to an understanding of medical consumerism in health care.1 Indeed, a search of articles cited in MEDLINE since 1966 identified 1,506 that examined the role of markets and consumer behavior in health care. But only five of these referred to issues of blame, and none actually related to the process of consumer choice, grievance, or other kinds of dissatisfaction with health plans. The only article that considers the role of blame in the context of consumer protection was about a study of ombuds programs in the British National Health Service.
Why, then, are we convinced that blaming plays such a crucial and overlooked role in the American context? Consider how consumers actually assess their health care. Most recognize the trade-off between quality and cost of care (Hibbard et al. 2000). But how do they judge these two aspects of a plan's performance? At least some aspects of cost are readily observed or easily predicted. Consumers are told the premiums when choosing among health plans, and if they get sick, they will soon discover the cost-sharing requirements imposed when they actually seek treatment. As most of the members recognize, each of these cost-related policies is part of the health plan (Mechanic 1989).
The quality of medical care is more difficult to discern, even after the fact. Consumers experience episodes of care and outcomes that are associated with that care, from which they must infer the quality of treatment. To do this, they must have some sense of why those outcomes resulted and who bears responsibility for them (Felsteiner, Abel, and Sarat 1980–81). Then, when problems emerge, they must decide who is to blame. They can avoid parties that have acted in a blameworthy manner and so reduce future risks. In this sense, blaming helps consumers both assess their situation and decide on the most appropriate response.
The positive functions of blaming depend on how accurately the blame is attributed. The more complex the situation is—that is, the greater the number of relevant factors and actors—the more difficult it will be for patients to make accurate attributions. In the past, patients have made sense of the causes of health and illness largely by dividing the responsibility among their own actions, those of their physician, and outside factors (e.g., luck, divine Providence) (Sonuga-Barke and Balding 1993). During the 1990s, however, a growing number of Americans discovered that managed care plans had the capacity to influence the quality of their health care (Jacobs and Shapiro 1999). Therefore, consumers must somehow take this into account, which complicates their attributions of responsibility and subsequent allocations of blame. If consumers become confused about whom to hold responsible for the outcomes of their medical care, they may be less willing or able to act effectively in response to problematic experiences, and the behaviors on which managed competition is predicated may become muted or distorted.
This article examines some of the attributional processes crucial to medical consumerism. We begin by exploring the nature of blame in this context. To do so, we develop a conceptual framework for understanding blaming in settings in which multiple actors, professional decision makers, and organizations intervene to shape treatment practices. From this framework we derive two sets of hypotheses. The first identifies some of the factors shaping blame attribution, and the second lists those factors that mediate the ways in which blame is translated into consumers’ voicing of dissatisfaction. We suggest ways in which managed care practices can affect both the attitudinal origins of blame and its behavioral consequences. Using data from a survey of people with serious mental illness and their families, we tested these hypotheses. We found that the attribution of blame follows certain predictable patterns and has significant influences on consumers’ voices. As the first exploration of this new conceptual terrain, our analyses are necessarily partial and incomplete. Nonetheless, we believe that even these preliminary analyses can highlight certain factors that have been omitted in past research. They also may discover ways of refining public policies intended to protect consumer interests or otherwise improve the performance of markets for medical services.
Conceptual Framework and Hypotheses
To develop hypotheses relating consumer behavior to blame, we had to consider how consumers respond to problems experienced while they were being treated. Despite the paucity of research on this question, a number of studies have explored how patients and their families attribute responsibility or blame for their illnesses (Collins 1990;Phares, Ehrbar, and Lum 1996;Sonuga-Barke and Balding 1993). In such cases, blame may be assigned to God, the environment, poor self-care, or no one at all. But we still know little about how blame attribution for the emergence of the disease relates to attitudes or perceptions associated with the treatment of the illness.
Without an established conceptual framework for thinking about the role of blame in health care markets, we must begin by creating a conceptual foundation. Because it is the first exploration of these issues, our goal is to identify a few of the potentially most salient relationships rather than to articulate a comprehensive theory.
Even this more modest objective requires two separate theory-building tasks. First, we must consider the factors that plausibly shape the assignment of blame. In this case we can use as a starting point models that have been previously developed in social psychology, most notably by Shaver (1985). These models must then be adapted to reflect certain distinctive features of interactions in contemporary American medicine. Our second theoretical task is identifying the ways in which blame attribution might influence consumer behavior. Contemporary economic theory of consumers offers little theoretical purchase for attributional assessments like blaming. Consequently, as a theoretical starting point we draw on the older conceptual framework developed by Hirschmann (1970). Although Hirschmann's work is more a taxonomy of institutional arrangements and individual responses than a full-fledged theory of consumer behavior, it is an adequate foundation for our exploratory development of hypotheses. We focus in particular on the linkages that can be established between blaming and one aspect of consumer behavior, the expression of dissatisfaction with the organization responsible for those services, which Hirschmann referred to as the consumer's “voice.”
Blame and Its Role in Human Behavior
To determine the origins and implications of blame attribution, we need to clarify our use of “blaming.” In common usage, the term sometimes conflates the formation of a judgment—how much a particular person is to blame for a given harmful event—and the expression of that judgment to either that person or a third party. For our analytic purposes, it is important to separate these two phenomena. When we refer to “blaming” here, we are describing the formation of an attitude. The first half of our conceptual model focuses on the factors that shape such attitudes. The expression of blame is incorporated into a second process of giving “voice” to grievances.
What gives rise to blame? In the aftermath of an injury, blame may represent an emotional response, the voicing of blame a cathartic release of expressed pain. In addition, an extensive literature in social and political psychology suggests that blame may have an important cognitive dimension. Deciding whom to blame is an important part of making sense of a complex, often unnerving, situation (Lane 2000;McGraw 1990;Shaver 1985;Stone 1989;Weiner 1995). The importance of blaming as a source of understanding and a motive for particular behavior was made evident in recent events, as the American public struggled to comprehend the motives for the terrorism directed at their buildings and public institutions (Cohen 2001;Sapinwall and Seitz 2001).
This search for understanding is a basic human motive, which is labeled by some sociologists as a quest for “ontological security” (Giddens 1991). It is particularly important to those people with serious and chronic medical conditions, since these can have consequential and life-defining implications (Thorne 1993). Blame attribution can also condition the ways in which people respond to problems. Events that are blameworthy motivate particular types of remedial action. Deciding that someone should be blamed for a problem may also have a predictive value, helping the victim assess motives or capacities should he or she encounter the perpetrator in the future.
Consequently, when people suffer episodes of ill health, deal with the symptoms and functional losses caused by injury or disease, receive medical care, and review its impact, we assume that they are simultaneously trying to make sense of the situation, to deal with its consequences, and to form strategies for avoiding similar problems in the future. Consumerism in medical care is thus a complex process of assessment, reaction, and prediction. Blame attribution can facilitate these processes by serving as a sort of decision heuristic, simplifying the challenge of understanding or taking effective action.
Factors Hypothesized to Influence the Attribution of Blame
We begin, as did Shaver, by considering attributions of blame in situations in which two actors of equal status interact with each other. For example, imagine that the drivers of two relatively expensive new cars, otherwise strangers to each other, are discussing a recent accident involving their two vehicles. Driver A was slightly injured in the accident, which was caused by the second driver pulling partially into her lane of traffic. Under what circumstances does driver A blame her injuries on driver B?
Social psychologists theorize that in such short-term dyadic relationships, blame attribution depends largely on assessments of responsibility and the acceptance of explanations (Lane 2000;McGraw 1990;Shaver 1985;Weiner 1995). Psychologists hypothesize that perceptions of responsibility are shaped by four considerations: knowledge of the outcome, capacity to assess its consequences, the objective of the action, and the voluntariness of the action. This process is represented schematically in figure 1. The extent to which driver B is held responsible for driver A's injuries depends on which of these four criteria for controllability apply to this case. Driver B would be viewed as less responsible if he (1) were unaware that he had crossed into driver A's lane; (2) had thought her lane was wider, so that she could easily avoid hitting his car; (3) had accidentally pulled into her lane; or (4) had been forced to pull into her lane because his tire had blown out.
FIG. 1.
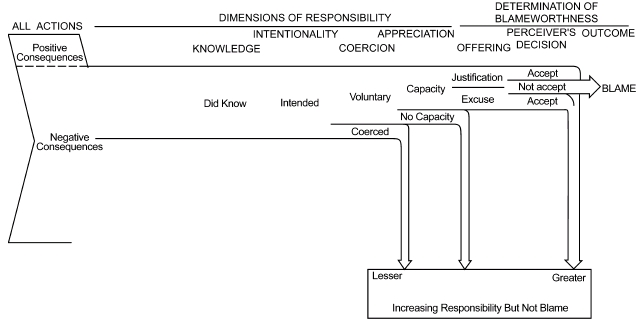
Simplified sequential model of the attribution of blame (after Shaver 1985).
In this conceptual framework, driver A will blame driver B for her injuries only if (1) driver B meets all the criteria for responsibility for the accident and (2) he can offer no exculpatory justification. The reasoning runs like this: If driver B is not responsible for the accident because it was caused by some factor outside his control, say a defectively manufactured tire, driver A will be more likely to blame the tire company than the other driver. Even if the accident was indisputably caused by driver B's actions, he would not be blamed if he could offer an acceptable justification, for example, that he had swerved into oncoming traffic to avoid a small child playing in the road.
This schematic presentation may give the impression that blame is always the outcome of an extended process of cognition and assessment, that it is quite difficult to assign blame, and that blaming would be observed only by the most sophisticated thinkers. But these apparent connotations do not match our understanding of blame. As we suggested earlier, blame often is an immediate, visceral, emotion-laden reaction to a set of events that does not depend on careful or extended reflection. It is only when making sense of blame (by either the affected party or an outside observer) that the stages of the attributional model become relevant. In this sense, the immediate reaction of blame creates a preliminary response, which is then tested against notions of responsibility and the justifications offered by the party being blamed. It establishes some implicit thresholds that must be reached in order for blame to be defused and thus guides the affected party through an otherwise complex set of causal assessments.
The Simple Dyadic Model Applied to Medical Care
Extrapolating this reasoning to medical care, we would expect blame attribution for adverse health outcomes to follow a similar reasoning process. Patients will blame their physician for problematic health outcomes only if (1) they see their doctor as responsible for the adverse event and (2) she cannot offer a compelling excuse (e.g., care for the patient was delayed in order to treat another patient with more pressing problems). Not all bad outcomes will be seen as under the physician's control, and not all physicians will be able to offer compelling excuses, particularly if they are judged to be less than fully competent (much as “bad drivers” have a harder time justifying their actions to forestall blame for an accident). This leads to two testable hypotheses.
Hypothesis 1: Responsibility and Problem Type. Patients are more likely to hold their providers responsible—and thus to blame them—for problems related to treatment than for problems related to payment for services or other issues unrelated to treatment.
Hypothesis 2: Competence and Justification. Health care providers who are viewed as incompetent are less able to offer convincing justification for adverse outcomes and thus are more likely to be blamed for them.
Adapting the Conventional Model: Medical Professionals as Objects of Blame
Relationships between clients and professionals are different from those between laypersons, and these differences affect blame attribution in health care in three ways. First, there are significant asymmetries of technical knowledge between professional and client. Less informed consumers have more difficulty evaluating the justifications offered by health care providers. In the extreme, the conventional “sick role” is played by patients who are willing to grant complete authority to their providers, thereby making these providers less subject to blame (Parsons 1951;Roter and Hall 1992). This deference tends to be most pronounced in those patients most debilitated by the symptoms of their illness or most concerned about the consequences of a “bad” decision (Hibbard and Weeks 1985;Roter and Hall 1992).
In the last quarter of the twentieth century, a movement to empower patients began (Haug and Lavin 1983). This “consumerist” movement encourages patients to draw on independent sources of information when evaluating their treatment and to challenge more readily the decisions of medical professionals (Rodwin 1994). These attitudes would make patients more likely to blame providers for adverse outcomes. But these changing norms have only partially altered the American public's prevailing attitudes (Hibbard and Weeks 1987). The evidence suggests that consumerist attitudes are most pronounced among patients with chronic illnesses, because their extended experience with and greater knowledge of their condition enables them to judge more independently and effectively (Thorne 1993). From these observations, we derive two additional testable hypotheses related to blame attribution:
Hypothesis 3: Knowledge and Duration of Illness. Patients or their families who have had a longer time to learn about a chronic condition are, all else being equal, more likely to challenge professional authority and to blame medical providers for adverse events.
Hypothesis 4: Autonomy and Severity of Illness. Patients or their families who experience more debilitating symptoms are more likely to defer to the authority of health care providers and thus are less likely to blame them for problematic experiences.
In addition to information asymmetries, two other features of professional-client relationships may affect blame attribution. The ethical codes of all professions hold their practitioners responsible for acting in the best interests of their clients (Kultgen 1988). This responsibility to act as a reliable agent is particularly pronounced in medical care, emphasized in both the Hippocratic oath and other contemporary codes of ethics propounded by various medical associations and societies (Emanuel and Brett 1993;Hart 1968;Woodward and Warren-Boulton 1984). Health care providers who are judged to have the greatest fidelity to these professional obligations are more trusted by patients and less subject to blame for adverse events (Mechanic 1996). The belief that one's physicians are acting in one's best interest implicitly exonerates their actions, defusing blame even without an explicit justification of their behavior.
Professional training does more than establish norms of conduct; it also creates social distance between health care providers and their patients who are less educated or otherwise have a lower social status. Because these status differences affect the professional-client relationship in many ways, they have an ambiguous predicted impact on blame attribution. On the one hand, high-status patients report having better communication with their physicians (Coates and Penrod 1980–81), giving these doctors more opportunities to justify bad outcomes and thus to deflect blame (Levinson, Roter, Mullooly, et al. 1997). Patterns of this sort have been documented in studies of medical malpractice suits. One study found that a quarter of those filing malpractice actions did so because they felt that their doctor had not been fully honest, and another 35 percent cited their doctor's failure to provide sufficient information (Hickson, Clayton, Githens, et al. 1992). May and Stengel (1990) found that patients were more likely to initiate malpractice actions when their physicians had not communicated a sense of caring.
On the other hand, patients of a lower social status are more likely to defer to medical authority (Hibbard and Weeks 1987), which would suggest that they would be less likely to blame medical professionals for adverse outcomes. It is not clear which of these status effects has the greater influence on blame attribution. These considerations lead to two more testable hypotheses.
Hypothesis 5: Agency and Trust. Medical professionals who are seen by patients or families to be acting in the best interests of their patients are less often blamed for adverse events.
Hypothesis 6: Social Distance and Deference. Social distance has a theoretically ambiguous impact on the propensity to blame. If communication dominates, then the patients’ status will be negatively related to their propensity to blame health care professionals. If deference dominates, status will be positively related to blaming.
Adapting the Conventional Model: Managed Care Plans as Objects of Blame
Although various forms of managed care were common by the end of the 1980s (Hoy, Curtis, and Rice 1991), the American public was slow to recognize its growth or implications (Miller and Horowitz 2000). Nonetheless, by the mid-1990s, most Americans had begun to realize that managed care practices had the potential to affect their medical care and had begun to form rather negative impressions of these consequences (Jacobs and Shapiro 1999). This growing awareness of managed care had several important implications for blame attribution.
First, as the public recognized that managed care plans had their own distinctive goals and methods for shaping medical care, it introduced a different type of actor into considerations related to blame. Unlike the dyadic relationship between equals or the relationship between clients and professionals, Americans deal with managed care plans as individuals confronting large organizations. This raises a number of questions about how individuals perceive organizational actors and how these perceptions affect attributions of blame.
We might expect that in at least certain ways, managed care plans would be treated like individuals in the assessment of blame, because people tend to invest organizations with some of the qualities of their interactions with other individuals (Coleman 1982). Indeed, we would predict that the first four hypotheses that we identified would apply to members’ judgments about whether their health plan was to blame for adverse health events. More specifically, this suggests that (1) plans are more likely to be held responsible for problems that are seen to be in their immediate domain of responsibility, such as questions about coverage or timely payment for treatment 2; (2) justifications by plans that are seen to perform their core functions more capably or competently are more readily accepted, and thus are less subject to blame, than are those by plans whose practices are seen as haphazard or inept; (3) consumers who have had longer to learn about their illness and health needs are more likely to challenge justifications and blame plans than are those who have less information; and (4) more severely debilitated patients are more apt to defer judgment and less often to consider plans blameworthy for adverse outcomes.
Although we predict that corporate actors will be treated in some senses similarly to individuals in regard to blame attribution, we also expect some differences to emerge. Previous research suggests, for example, that corporate actors are viewed by the public serving on juries as having certain qualities that make them more vulnerable to tort claims. These perceptions may involve notions of “deep pockets”—that is, corporations can more readily afford to compensate injured parties—doubts about corporate motives, or perceptions that corporate actors can more easily control their external environment and thus are more blameworthy for bad events.
These distinctive perceptions of corporate actors may make our fifth and sixth hypotheses less applicable to managed care plans than to health care professionals. It may be difficult for members to think of health plans as acting in the members’ fiduciary interests. The reason is in part that individuals are less likely to establish emotional bonds with a health plan than they are with a health care provider, and these depersonalized relationships may make it more difficult for them to trust the health plan (Mechanic and Schlesinger 1996). Members may also consider the objectives of most health plans to be inconsistent with fiduciary responsibility. Most Americans, for example, recognize that the majority of health plans operate under the auspices of large for-profit corporations (Kaiser Family Foundation 1998). The idea that health plans act as agents for their members may be difficult for members to accept when they see plans as motivated primarily by the pursuit of profits. Each of these factors would make perceptions of agency less salient to attributing blame to health plans than to health care professionals.
The impact of social distance is more difficult to determine because it is not clear how individuals assign social status to an organizational actor. On the one hand, large corporations might be seen as powerful entities that induce deference, particularly by respondents of low social status. But it seems to us more likely that corporations are assigned status according to their public “face,” that is, the characteristics of the individuals through whom they are represented in dealings with plan members. These interactions typically involve questions of coverage or paperwork and often require dealing with clerks or relatively low level administrators. We would therefore predict that the patient's social status would have less consequence for blaming health plans, because they would regard the effective social distance as shorter than for interactions involving health care professionals.
We would thus hypothesize that the process of blaming health plans that use managed care techniques is in some ways similar but in other ways different from the attribution of blame to health care professionals. These similarities and differences are summarized in the first six hypotheses listed in Table 1. The introduction of managed care also complicates assessments of blame in another way.
TABLE 1.
Summary of Hypotheses Related to Blame Attribution
| Applied to Blame Attribution for: | ||
|---|---|---|
| Specified Hypotheses | Health Care Professionals | Health Plans |
| Hypotheses Related to Blame Attribution for Single Actors | ||
| Hypothesis 1: Responsibility and Problem Type | Providers blamed for care-related problems | Plans blamed for payment-related problems |
| Hypothesis 2: Competence and Justification | Incompetent providers more often blamed | Incompetent plans more often blamed |
| Hypothesis 3: Knowledge and Duration of Illness | Duration of illness increases blaming | Duration of illness increases blaming |
| Hypothesis 4: Autonomy and Severity of Illness | Severity of illness decreases blaming | Severity of illness decreases blaming |
| Hypothesis 5: Agency and Trust | Providers seen as good agents less often blamed | Agency less relevant to blaming health plans |
| Hypothesis 6: Social Distance and Deference | Social status ambiguously linked to blame | No relationship between blame and social status |
| Hypotheses Related to Blame Allocation among Multiple Actors | ||
| Hypothesis 7: Hydraulic Allocation of Blame | Increased blame for one actor decreases propensity to blame other actors | |
| Hypothesis 8: Independence of Blame Attribution | Blame attribution for one actor has no impact on blaming other actors | |
| Hypothesis 9: Managed Care as Magnet for Blame | Perception that plan uses managed care decreases propensity to blame provider | Perception that plan uses managed care increases blame, whatever the plan's practices |
Multiple Parties: From Blame Attribution to Blame Allocation
Public recognition that managed care plans can directly alter the delivery of medical care increases the complexity of blame attribution by introducing a third actor into what had previously been a dyadic relationship. The injured party must now determine not only how blameworthy the actions of each of the other parties are, but how the actions of each affect the amount of blame that should be accorded the other. This must be done in a context in which each of the potentially blameworthy parties has a strategic interest in shifting blame to the other actor. In other words, the process of blame attribution in dyads becomes a matter of blame allocation in a triadic relationship. This requires that we extend the existing theoretical models to address these more complex circumstances.
Drawing on past studies of the social psychology of attribution (Heider 1958;Hewstone 1983;Jones and Davis 1965;Kelley 1967) and the social theory of triadic groups (Simmel 1950), we theorize that when there are multiple parties, the process of blaming has two stages of reasoning. In the first stage, each party is assigned a provisional level of blame, following the logic described in previous sections of this article. Once provisional assessments of blame are made for each actor, the second stage “balances” the blame among these different parties, following one of the possible heuristics described next.
Previous research has documented a similar multistage process in attributions of responsibility for a variety of problems involving multiple actors. For example, Pottick and Davis (2001) found that in determining who was responsible for addressing children's behavior problems in school, both parents and counselors first identified the extent to which the child (or other actors) were responsible for causing the problem. This first stage of assessment shaped the allocation of responsibility for treatment in the second stage of decision making. Similar patterns have been documented by political psychologists in citizens’ judgments of who in American society is responsible for dealing with various social problems (Iyengar 1990;Skitka and Tetlock 1993).
We theorize that a similar process occurs in the allocation of blame. Having made a provisional attribution for each actor, the injured party then must “balance” these attributions against one another in making a final judgment about blame. We have no a priori intuitions about how this balance is struck. At least three plausible alternatives can be identified from the general literature on legal grievances (e.g., tort actions) or the more specific literature on managed health care.
The first possibility involves what social psychologists label a “hydraulic process.” This implicitly assumes that a fixed magnitude of “blame” is assigned to each adverse event. Under these circumstances, increasing the attribution of blame to any one actor proportionally decreases the blame borne by the other actors (Heider 1958). Lane, for example, notes that the malign influences of one's peers are often invoked as “a mitigating circumstance reducing the blameworthiness of the offending person's later delinquent act” (2000, p. 51). In tort actions related to accidents, responsibility for damages is frequently determined by notions of “comparative negligence” that balance the blameworthiness of the various parties involved (Calabresi 1970).
Hydraulic processes are not the only observed form of blame allocation. Under some circumstances, blaming a particular actor appears to have more to do with whether he exercised an acceptable minimum of due diligence. Actors who fail to meet this threshold are judged blameworthy, whatever the role of others in producing the adverse outcome. This pattern has been identified for certain political misadventures (McGraw 1990) as well as for determinations of medical malpractice (Werth 1998). It corresponds to a standard of tort judgment referred to as “contributory negligence,” once common but now somewhat out of favor in most jurisdictions (Brown, Sukys, and Anderson 1988).
Finally, the process of blame allocation may be affected by systematic errors or misperceptions. In health care, because causal relationships are complicated and difficult to discern, the most likely forms of misperception are an overattribution of responsibility to those actors whose roles have been given the greatest recent publicity, whether or not their actions could have had much influence on the outcomes in question (Immerwahr, Johnson, and Kernan-Schloss 1992). Lane identified a second bias in blame allocation. He observed that uncommon actions, for example, isolating a patient who is thought to have a rare and highly contagious tropical disease, invite causal attributions that increase the likelihood of blaming, even though “this practice seems quite unfair, for the degree of negligence or the contribution to the harm should not vary with whether the offending act is frequently or infrequently performed” (2000, p. 49).
A spate of negative media coverage in the late 1990s may have created just this sort of negative public image of managed care plans (Blendon, Brodie, Benson, et al. 1998; Enthoven and Singer 1998; Jacobs and Shapiro 1999).Mechanic (1997, 2000) has argued that the resulting widespread public distrust has made managed care plans magnets for blame, held responsible for problems in American medicine that predate their birth and are not causally related to any form of managed care intervention. “Different from the past is the growing ease of attributing dissatisfactions and perceived failures to clearly identifiable targets (indeed an entire industry)…. The culprit is now more easily definable and each observable misdemeanor is a signal for what is wrong with managed care” (Mechanic 1997, p. 1810). A recent study of consumer attitudes lends some support to this claim: members’ fears of mistreatment were related as much to the belief that they were enrolled in a managed care plan as they were to their actual enrollment; almost a quarter misreported whether their insurance was a managed care plan (Reschovsky and Hargraves 2000).
The notion that the notoriety of managed care plans has made them magnets for blame suggests that plans will be blamed for adverse outcomes that they could not plausibly have caused. The implications for blaming health care professionals are less apparent. If the hydraulic hypothesis holds, then the increased blame on plans necessarily decreases the blame on providers. More complex connections may be at work as well. Precisely because many Americans only vaguely understand managed care, some may fear that managed care practices have compromised the willingness or ability of health care professionals to act in the interests of their patients (Mechanic and Schlesinger 1996). Some studies have shown, for example, that the belief that health care providers receive financial incentives from the plans with which they are affiliated decreases patients’ trust in their physicians (Kao, Green, Zaslavsky, et al. 1998;Miller and Horowitz, 2000).
These three alternatives provide our final three testable hypotheses regarding blame attribution:
Hypothesis 7: Hydraulic Processes of Blame Allocation. Increased blame on health plans decreases blame on health care professionals, and vice versa.
Hypothesis 8: Thresholds of Blame. The blame assigned to any one actor is not related to the blame assigned to other actors.
Hypothesis 9: Managed Care as a Magnet for Blame. Negative publicity of managed care practices causes health plans to be blamed for problems that they could not have created. The impact on blaming health care professionals is ambiguous.
Unlike the hypotheses presented earlier, not all those related to blame allocation can be valid simultaneously. In particular, the seventh and eighth hypotheses are mutually exclusive. But the ninth hypothesis may be compatible with either of the other two; indeed, it could be valid even if neither of the other two hypotheses holds true.
Linking Blame Attribution to Consumer Voice
The formation of blame in the attitudinal sense often leads to the expression of blame. But like any other behavior, voicing a grievance is costly in that it requires time, effort, and various material resources. It therefore is shaped by considerations and constraints quite different from those that affect the attribution of blame. We identify some of these additional factors next.
In principle, an aggrieved patient could express her dissatisfaction to either her health plan, her clinicians, or both. For several reasons, we direct our analysis to the study of voice to the plan. First, voice to health plans has been the primary focus of public policy, in the form of state regulations requiring grievance procedures, third-party arbitration, or other procedural arrangements to guarantee due process for the aggrieved party (Noble and Brennan 1999). Second, it would prove empirically difficult to separate the voicing of grievances to health care professionals from the more conventional aspects of patient-provider relationships, which often involve reporting symptoms or other concerns. Nonetheless, because providers are an alternative avenue for expressing dissatisfaction, we must take this into account in both our conceptual model and our hypothesis testing.
Exploring the impact of blaming on consumers’ actions requires a behavioral model with assumptions that are different from those of conventional neoclassical economic theory. Most important, whereas neoclassical theory assumes that consumer choices and actions can be made without cost, a plausible model of consumerism in health care must begin with the assumption that consumer decision making has considerable costs. They may be high partly because many consumers are not well informed about their health care choices, and acquiring more adequate information may require much time and effort (Cunningham, Denk, and Sinclair 2001;Hibbard et al. 2000). Even when consumers are well informed, switching among health plans may entail substantial costs (Schlesinger 1997).
Because it is predicated on notions of costly consumer action, Hirschmann's theory of consumer behavior (1970) is a promising starting point for exploring the role of blame in health care. Hirschmann argued that consumers react to unsatisfactory experiences (such as a decline in the quality of a good or service) by weighing the relative costs and benefits of two possible responses: (1) “exit,” switching to another supplier of goods or services, and (2) “voice,” complaining to their existing supplier in hopes of improving the quality of the service.3 Consumers are more inclined to switch suppliers when the costs of this transition are relatively low and the odds of finding a higher-quality supplier are relatively good. Consumers rely more on complaints when the cost of exit is high, when the cost of filing a complaint is modest, when they feel that the supplier will respond to their grievances, or when they can at least learn enough from going through the grievance process that they can better avoid the problem in the future.
If the costs for both strategies are high relative to the expected benefits, the best course for the consumer is to do nothing. Recent evidence on consumer behavior in health care suggests that this passive response is often seen as the one preferred. A 1990 study of patients found that 12 percent had a serious problem with their medical care (May and Stengel 1990). Roughly a quarter of these respondents had done nothing in response. Because of the difficulties of learning to use a health plan and the disruptions in continuity of care, only 25 to 40 percent of the most dissatisfied members of managed care plans actually leave them, with even lower rates of exit—12 to 35 percent—for members who have been seriously ill (Schlesinger et al. 1999). A recent Kaiser Family Foundation survey asked respondents whether they had had a problem with their health insurance plan in the previous year. Of the 51 percent who had, a little more than half had contacted someone at their health plan to seek recourse (Kaiser Family Foundation 2000).
This same body of research suggests that voice is a much more common response to dissatisfaction with one's health plan than exit is. Because a majority of Americans who receive their health insurance through work cannot choose their plan, the only way that they can switch health plans is to find another job (Davis et al. 1995;Long and Marquis 1998). As we noted earlier, even those who have a choice are often unwilling to switch plans if it means disrupting relationships with physicians or other health care professionals. As a result, although 54 percent of respondents reporting problems with insurance indicated that they had complained to their plan, only 5 percent had changed their health plan in response (6 percent changed their provider) (Kaiser Family Foundation 2000). This makes voice five times as common as exit as a response to problematic experiences with one's health plan.
Accordingly, we explore in this article the theoretical and empirical linkage between blaming and voice, taking into account the relationship between voice and exit. In principle, one can imagine aggrieved consumers complaining to a variety of different parties, including public officials and state regulators. In practice, however, most grievances are directed to the health plan itself (Kaiser Family Foundation 2000). Indeed, most states that have established third-party arbitration for managed care disputes require that plan members first exhaust their grievance options within the plan (Tapay et al. 1998). We thus concentrate on the voicing of dissatisfaction directly to the health plan.
A Model of the Influence of Blaming on Consumer Voice
Paralleling our conceptual treatment of blame attribution, we theorize that the voicing of grievances emerges from a multistage behavioral process. More specifically, these behaviors are presumed to emerge from three stages of reasoning (see figure 2). Assume that a consumer has experienced an adverse event while receiving medical care. Her initial decision is a strategic one: should she actively respond to this unfortunate event and, if so, how? Her response will depend in part on whether she believes that the medical care itself caused, exacerbated, or ameliorated the problem in question (Lau, Bernard, and Hartman 1989). But other factors will also come into play.
FIG. 2.
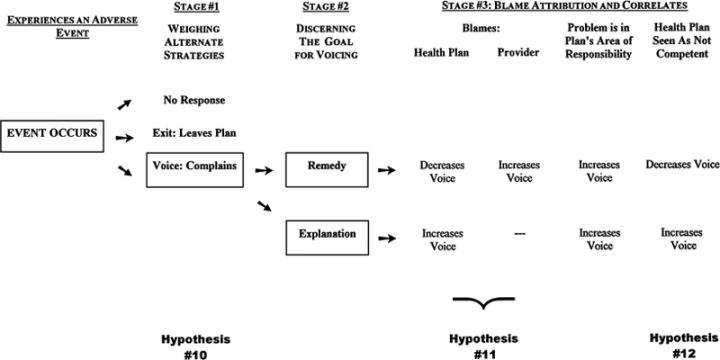
A three-stage model linking voicing and blame attribution.
Following Hirschmann, we hypothesize that this consumer makes her choice by balancing the perceived costs and benefits of each alternative, including doing nothing at all. Compared with a passive response, voicing appears more appropriate the more serious the problem is. For minor inconveniences or affronts, most consumers judge the effort of filing a formal grievance or even voicing an informal complaint to be too great to merit taking action. For more serious concerns, however, some action is justified either to remedy the problem or to reduce the odds of its recurring in the future. Compared with exit, the voice strategy is favored when either (1) the costs of complaining are relatively low or (2) the plan is expected to respond constructively to a grievance. This leads to our first testable hypothesis involving consumer voice:
Hypothesis 10: Strategic Balancing of Costs and Benefits. Plan members are more likely to voice complaints to health plans when they (a) have experienced more severe problems, (b) can complain at relatively low cost, and (c) expect the plan to respond constructively to their grievances.
The second stage in our model is discerning the objective of the complaint. According to the literature on torts, including medical malpractice, aggrieved parties are usually motivated to voice their concerns in order to achieve one or more of three goals. First, they may want to remedy a problematic situation. For example, members who have been denied coverage for procedures deemed “experimental” have filed grievances or gone to court to induce their health plan to pay for these treatments. Second, the injured party may complain primarily to get an explanation for why an adverse event occurred. In this case, the goal may be to obtain an apology from the culpable party, to understand the processes involved so that the problem can be avoided in the future, or simply to reach an emotional closure, to come to terms with the injury. In the managed care context, this might be extracting an acknowledgment that the health plan's practices did adversely affect the treatment of its members (Schlesinger 1997). Third, the injured party might voice a complaint as a prelude to seeking monetary compensation. This third motive has less relevance to health plans, which remain relatively insulated from legal action related to medical malpractice or other adverse outcomes (Bloche 2000). We therefore examine the first two of these three motives.
The predicted influence of blame attribution on consumer voice depends very much on the relative importance of these two objectives. Consider first the case of the member who complains in order to remedy a problem. Here the predictive aspect of blaming comes into play, as it makes sense only to seek a remedy from those parties that can be expected to be concerned about the patient's well-being. If the patient believes that the health plan is blameworthy for the initial problem, this belief will color his views of the plan's motives. If all else is equal, this belief will discourage the patient from complaining to the plan, because the complaint will seem less likely to yield an effective remedy. But if the patient blames primarily the health care provider for the problem, it may be quite sensible to complain to the health plan in order to remedy the situation. Under these circumstances, the adverse event cannot be indirectly related to the motives of the plan, so the plan can still be seen as acting in its members’ interests.
The situation is quite different if the complainant is seeking an explanation, as opposed to a remedy. Under these circumstances, the blameworthy party is exactly the actor that should be addressed by the grievance, since it is from that party that one must obtain an accounting or an apology. So if explanation is the motive, then the more blameworthy the plan is, the more likely the patient will complain to that organization. By parallel reasoning, if the primary blame is assigned to the clinician, this should reduce the likelihood that the patient will complain to the plan, since it has nothing to offer. This reasoning generates our next testable hypothesis (the middle columns in figure 2):
Hypothesis 11: Motive, Blame, and Voice. If plan members are seeking a remedy for a problem, one would expect them to complain more frequently to a health plan if they blame the health care providers for an adverse event but less frequently if they blame the plan itself. Alternatively, if the members are seeking an explanation, they will more frequently complain if they regard the plan as blameworthy.
Although we would expect that blame would influence the propensity to voice complaints, past research suggests that only a few of the events that are judged blameworthy evoke a response from consumers (Brennan, Leape, Laird, et al. 1991;May and Stengel 1990). Our exploration of blame attribution found that blaming is a function of notions about responsibility and causality. But these determinants of blaming may exert an independent influence over the voicing process. In order to discern the impact of blame on voice, we need to identify and control for these related considerations. As we pointed out earlier, the scope of responsibility in health care appears to be defined largely by the nature of the problem, with issues associated with treatment seen as the domain of health care professionals and issues associated with coverage or payment as the domain of the health plan. Whether the motivation is remedy or explanation, we would expect the plan to receive more complaints about those issues for which that plan is judged primarily responsible.
The influence of perceived control on voicing behavior again depends on the objective of the complaint. We observed earlier that the perceived competence of the health plan affects its ability to justify its action and policies and thus to shield itself against blame. But perceived competence can also be expected have an independent effect on voicing. The more incompetent that a plan is perceived as being, the less likely its members will complain to the plan to obtain a remedy. That is, if the plan “messed up” in the first instance, one would not necessarily expect anything better if it addressed the problem a second time. But perceptions of incompetence should increase the propensity to complain if one is seeking an explanation (or compensation) (see figure 2). Indeed, this is precisely what one finds in the literature on torts and other legal grievances: that providers that are judged to be incompetent are the most likely to be the targets of legal action, no matter how much they are blamed for the adverse event. This provides our final testable hypothesis:
Hypothesis 12: Competence and Voice. If complaints are motivated by a desire for remedy, the less competent the health plan is, the less frequently dissatisfaction with it will be voiced. But if grievances reflect primarily a search for explanation (or compensation), then perceptions of incompetence will increase the propensity to complain to the health plan.
Other Influences on Voice and Blame
We have developed a conceptual framework for understanding blame attribution in a health care system characterized by managed care, as well as the linkages between blaming and consumers’ expression of dissatisfaction to the administrators who run these plans. To test these hypotheses, we need to measure the prevalence of these factors and their relationships with one another. We also need to control for other characteristics of individuals that may affect their propensity to blame or express dissatisfaction.
An Exploratory Empirical Study of Blame Attribution and Managed Care
Despite the many large surveys of consumer attitudes and experiences with managed care, none has collected the sort of information required to assess the process of blame attribution. We therefore used data from a small exploratory survey that we conducted to examine the treatment of people with serious mental illness. This is a promising test population precisely because the norms of appropriate treatment remain in dispute and the application of managed care has been a matter of considerable controversy (Mechanic, Schlesinger, and McAlpine 1995). In this section, we describe the survey and the measures for each of our hypotheses.
Data Sources
The data for this study are from a survey that we fielded between August 1995 and May 1996. The sampling frame was the national membership list of the National Alliance for the Mentally Ill (NAMI). NAMI members are primarily family members of people who have a serious mental or emotional disorder (henceforth referred to as “clients”). To maximize the probability that respondents were members of managed care plans (unusual when the survey was fielded), we surveyed NAMI members living in 21 states in which managed care was commonly used for behavioral health care.
The survey had two parts. In the first, we contacted the NAMI members and asked them to participate in the study. Of the total of 467 families, 382 agreed to participate in the study, a response rate of 82 percent. The respondents were representative of the American public in most of their sociodemographic characteristics, although they were somewhat better educated and less likely to be members of a racial or ethnic minority group. We collected information about how the clients paid for their mental health services, as well as the family members’ assessment of the clients’ treatment, if they felt capable of judging the treatment process (74 percent did).
For the second part of the survey, we asked the family members to provide ways of contacting the client to whom they were related. Two-thirds agree to do so; most who did not reported that the client was too dysfunctional to respond to a telephone interview. Of 243 referrals to clients, 9 percent refused to participate in the study, and another 14.4 percent could not be reached with the information that we had; in all, 167 clients participated in this study.
Both the family and client parts of the survey obtained extensive information on the level of client function, the quality of mental health services, the impact of client well-being on burdens for family, the availability of grievance mechanisms if a problem emerged in treatment or in dealings with the insurance plan, as well as various sociodemographic characteristics of the respondents. Most relevant to this article, both stages of the survey collected information about “critical events” in the care of the client. These included (1) disagreements between the client and his or her primary mental health care provider over the appropriate treatment and other problems in the delivery of services, (2) disputes with the insurance plan over coverage for services, and (3) episodes in which the client's level of mental or emotional function had markedly declined. Sixty-eight percent of the respondents reported one such critical event in the past year; of this group, 59 percent also reported a second event during the year.
We constructed our data set using these potentially blameworthy problems, or “critical events,” as the unit of analysis. This combines responses from both family members and consumers. For this reason, in the following presentation we use the term “respondent” to refer to either the consumer or the family member who reported on the problem.
In regard to the critical events identified in this manner, we asked the respondents (1) how severe the implications were for the client; (2) which actors (including the client and “the illness”) were blameworthy in the episode; (3) how the client and/or the family responded to these events—in particular, whom they contacted for information or assistance; (4) if they had not contacted either the provider or the insurance plan, then why they had not contacted them; and (5) how successfully the problem was resolved. We extensively pilot-tested these questions, along with the more conventional measures cited earlier, to ensure that both family members and clients would understand them and respond to them coherently.
Dependent Variables: Measures of Blaming and Voice
In accordance with our conceptual discussion, our analysis has two stages. In the first, we explore the determinants of blame attribution, and in the second, we examine the extent to which blame, along with other factors, can influence voice, that is, the expression of dissatisfaction to the health plan paying for treatment. The dependent variables for the first stage are therefore the extent of blame assigned to either the provider or the plan. Blame was reported on a four-point scale: “none,” “some,” “most,” and “all.” We asked the respondents about the extent to which they blamed the client's primary therapist, the insurance plan, the client, the illness, and any other party they named.
To analyze consumer voice, we asked the respondents whether they had talked to a variety of parties in order to address the problem in question. These parties included the therapist, the insurance plan, some other health care provider, friends and family, a lawyer, the local chapter of AMI (Alliance for the Mentally Ill), a government agency, or any other party the respondent named. Our primary variable for analysis was any contact with the health plan (which could have been either a formal grievance or an informal complaint). We incorporated the information about contacts with other parties into the explanatory variables for this model, as described next.
Explanatory Variables and Methods Related to Blame Attribution
We tested each of the half dozen hypotheses related to blame attribution with a distinct explanatory variable. We then identified a set of additional independent variables to control for other influences on members’ satisfaction that might otherwise introduce spurious findings into the regression models.
Hypothesis 1: Responsibility and Problem Type
We divided the critical events being studied into three categories: problems with treatment (e.g., inadequate or ineffective services), problems with payment (e.g., an inability to have needed services paid for), and problems with condition (e.g., side effects of medication, unstable symptoms). Among the respondents who cited critical events, 32 percent cited treatment problems; 17 percent cited payment or services problems; and 51 percent cited problems with a worsening condition. In accord with this hypothesis, we would expect providers to be blamed most often for problems related to treatment and plans to be blamed for problems related to payment or service coverage. (We used problems related to deteriorating condition as the omitted comparison category in the regression models).
Hypothesis 2: Competence and Justification
We hypothesized that perceived competence would mediate the ability of both health care professionals and health plans to justify their actions and thus influence their ability to shield themselves from blame. We asked the respondents to assess the actions of both actors. The relevant interpretation of “competence” clearly is different for each actor, since each has a different domain of primary responsibility. We measured competence for the provider according to his or her assessed ability to “get to the heart of the client's problems.” Fifty-eight percent of the respondents reported having a high degree of trust in the provider's competence. For the plan, we measured competence by the extent of financial security that it provides. Eighty percent of our respondents gave the health plan high marks for this. Assessments of each role are on a five-point scale, and Table 2 gives the specific wording of the questions.
TABLE 2.
Specific Questions about Plan and Provider Behavior
| Dimension of Behavior | ||
|---|---|---|
| Measured Behavior of: | Competence | Agency |
| Primary Mental Health Care Provider | Respondent was asked about the quality of mental health care provided over the past year by this provider. Measures included helping the client “get to the heart of his/her problems.” (Scale: poor, fair, good, very good, excellent) | Respondent was asked whether the provider could be counted on to “choose the best treatments even if they required more time and effort.” (Scale: five-point agreement-disagreement) |
| Health Plan | Respondent was asked how often the client “decided not to seek mental health care out of a concern that the services would cost too much.” (Scale: never, rarely, sometimes, often, always) | If the respondents had complaints, they were asked whether they could “count on the plan to try to respond to them.” (Scale: five-point agreement-disagreement) |
Hypothesis 3: Knowledge and Duration of Illness, and Hypothesis 4: Autonomy and Severity of Illness
The respondents’ willingness and ability to challenge independently the claims of health care professionals and health plans is hypothesized to be linked to the duration and severity of the patients’ illness. We measured experience with mental illness by the number of years that had passed since the client was first diagnosed with a mental illness. For this sample, an average of 17 years had passed between the initial diagnosis and the response to the survey; 4 percent had less than five years of experience. We measured the current severity of the illness by an index of problematic behaviors reported by the clients’ families. Table 3 lists half a dozen problems and their reported frequency. The average client was reported to have had problems in the past year in slightly more than two of these categories.
TABLE 3.
Frequency of Behavioral Problems Reported for Clients in Past Year
| Frequency with Which Problem Was Reported (%) | ||||
|---|---|---|---|---|
| Type of Problem Behavior | Often | Sometimes | Seldom | Never |
| Arguments or verbal abuse of others | 11.0 | 22.8 | 16.4 | 49.7 |
| Physical threats or harm to others | 2.4 | 3.8 | 10.8 | 83.1 |
| Drunk or high on drugs | 5.1 | 9.9 | 8.3 | 76.6 |
| Discussion of or attempt to commit suicide | 0.8 | 9.9 | 11.3 | 78.0 |
| Incoherent speech or hearing of voices | 19.6 | 30.6 | 16.7 | 33.1 |
| Extreme withdrawal | 19.1 | 24.2 | 13.4 | 43.3 |
Hypothesis 5: Agency and Trust
We predicted that health care professionals who are seen to be acting in the best interests of their patients would be less likely to be blamed for adverse events. We measured agency among health care providers by the perceived willingness of the primary therapist to select treatments that benefited the patient, even if they imposed costs on the provider. Table 2 gives the specific wording of the question and response scale.
Recall that we expected agency to be less important to blaming the health plan. Nonetheless, because it still may prove consequential, we attempted to measure the respondents’ perceptions of agency on the part of the plan. Again, because the plans have different domains of primary responsibility, we had to direct the question to a different aspect of performance than was asked of health care professionals. More specifically, we asked about the perceived willingness of the plan to respond to its members’ concerns (the specific wording is presented in Table 2). Sixty-six percent believed that the client's primary therapist was a good agent, and 52 percent viewed the plan as a good agent for the client. It is important to recognize that these questions assess only one of many possible dimensions of agency behavior, that they only partially capture the ways in which these actions might affect blame attribution.
Hypothesis 6: Social Distance and Deference
Social distance has a theoretically ambiguous impact on the propensity to blame and likely has a smaller role in blaming plans than in blaming health care professionals. Nonetheless, it is important to measure and control for the influence of status. Because many people with serious mental illness do not work and because many of our family respondents were retired or homemakers, occupational status was not appropriate. We instead relied on educational attainment as a marker for social status and found that 52 percent of respondents had at least a college degree.
Controlling for Other Factors That May Affect Satisfaction
Our goal was to identify the factors shaping blame attribution. But it is likely that in practice, blame is negatively correlated with more general notions of satisfaction with health care and health care financing. Consequently, we introduced into the regression models some additional variables known to be related to satisfaction in managed care settings (Schlesinger et al. 1999). Past studies have found that satisfaction with both health plans and health care is affected by (1) the types of health care needs that the plan must address (those with more immediate and extensive needs report lower satisfaction) and (2) members’ understanding of the plan's administrative requirements. We controlled for differences in health care experiences by asking whether the respondents had had one or more episodes requiring “urgent” care (often related to threats of suicide by the client). Fifty-seven percent of the clients had urgently needed care in the previous year. Because clients and families might have interpreted treatment experiences differently, we controlled for the type of respondent with a separate dichotomous variable.
We measured the respondents’ knowledge of the plan's administrative practices by two variables. The first asked them about their understanding of the plan's grievance procedures, whether the plan had a grievance process and, if so, whether it applied to five different situations, including (1) “confused about insurance benefits,” (2) “the therapist is not providing effective treatments,” (3) “medication is not effective,” (4) “disagreements between patients and their therapists,” and (5) “your insurance does not cover the treatment proposed by your therapist.” Thirty-seven percent of the respondents were aware that their plan had a grievance mechanism, but only 5 percent knew all the circumstances under which this mechanism could be used. Our second measure of knowledge pertained to the client's ability to understand the administrative procedures required in order to obtain services. Twenty-four percent of the families reported that the client was “always” or “often” confused about this sort of paperwork. By contrast, 59 percent reported that the client was never confused by these requirements.
Although exposure and knowledge are likely to be related to satisfaction (and thus correlated with expressed blame) for both providers and plans, one additional variable has been shown in past research to uniquely affect satisfaction with the health plan itself. This is the length of time that an individual has been enrolled in the plan (Ross, Wheaton, and Duff 1981;Schlesinger et al. 1999). Those enrolled for a longer period in a plan may be more familiar with its requirements or better adapted to its expectations. Alternatively, individuals whose needs or preferences clash with the plan's priorities may leave, reducing the potential for conflict and blame. Whatever the causal mechanism, it is important to control for this effect. Although the average client in this sample had been covered by the same insurance plan for the past 12.6 years, there was considerable variation in this dimension of experience. Twenty-two percent of the clients had had their current insurance coverage for five years or less. Fourteen percent had been in the same coverage for 20 years or more.
Explanatory Variables and Methods Related to Blame Allocation
Recall that we identified three additional hypotheses regarding the relationship between blame on health plans and blame on health care providers.
We assessed the ninth hypothesis, that managed care plans have become a “magnet” for blame, by including measures of respondents’ perceptions of whether the client was or was not enrolled in a managed care plan. Because we also asked for the name of the clients’ health plan, we were able to determine independently whether or not they were enrolled in managed care. Based on these measures, 53 percent of clients were in some form of managed health plan, although 38 percent of the respondents were not aware of this. Three percent of the respondents falsely perceived the client to be in managed care, even though he or she was not in a managed health plan. This distinction between actual and perceived enrollment became a means of testing the ninth hypothesis (Reschovsky and Hargraves 2000). More specifically, if managed care is being unfairly blamed for adverse events, we should see plans being blamed more often when respondents think they involve managed care but actually do not. We can also test to find out whether health care professionals suffer from a sort of “guilt by association,” thus increasing the propensity to blame providers who are incorrectly perceived to be affiliated with managed care.
Testing the hydraulic hypothesis (hypothesis 7) is more challenging, as we could do it in several different ways. We could incorporate certain variables thought to be correlated with plan blame (e.g., plan competence) into the model predicting the allocation of blame to the provider, and vice versa. A more formal version of this approach is estimating a two-stage least squares model, in which blaming the provider is included as an explanatory variable in the regression predicting blame for the plan. Using this two-stage model, blaming the plan also becomes an explanatory variable in the model predicting blame for the provider. Each model is identified by having some variables that uniquely predict each allocation of blame (e.g., trust and types of problem). The predicted value for blame on the plan from the first-stage regression is then incorporated as the explanatory variable in the model predicting blame on the provider (and vice versa). We report the results from this more complex model after presenting our findings from the single-stage models of blame allocation.
Hypothesis 8, predicting that blame on the provider and the plan are not related to each other, becomes the default hypothesis. If we observe no findings consistent with either the hydraulic or the blame magnet hypothesis, we have validated this hypothesis.
Explanatory Variables and Methods Relating Blame to Consumer Voice
Recall that we identified three primary hypotheses related to voice. Next we discuss the measures that we used to test each hypothesis and the additional explanatory variables we introduced into the models as statistical controls.
Hypothesis 10: Strategic Balancing of Costs and Benefit
In the first stage of our model, plan members are expected to weigh the costs and benefits of voice, as reflected in their assessment that they (a) have had relatively severe problems, (b) can complain at relatively low cost, and (c) expect the plan to respond positively to their grievances.
The severity of the critical event's consequences was reported directly by the respondents on a four-point scale, ranging from “not very serious at all” to “extremely serious.” Of the events reported in this survey, 48 percent were described as extremely serious, 24 percent as moderately serious, 13 percent as somewhat serious, and the remainder as not very serious at all. We would expect that the greater the severity was, the more frequently the respondents would voice their concerns to the health plan.
We have two measures of the cost of exercising voice. Past studies have found that most Americans make sense of their health insurance arrangements by asking family and friends for advice (Isaacs 1996). Those respondents with a broader social support network can be expected to make sense more readily of their problems and to construct remedies. Consequently, the availability of social support reduces the cost of expressing grievances, and family members may also help as advocates in dealing with the plan. We measured social support by whether the respondents reported that they had talked about the problem with “family or friends.” Half the respondents reported that they had social support for dealing with the problem. Our second measure of the cost of complaints is the respondents’ knowledge of the grievance process, as described earlier. Those who understand the grievance process should find it easier to express their concerns when they are dissatisfied with some experience or aspect of care.
The benefits of voicing a grievance depend on the plan's willingness to respond positively. Recall that the variable that we used to measure plan agency in the blame attribution models asks specifically about this. All being else equal, we would expect respondents to voice their concerns more readily when they perceive that the plan will respond to their concerns (see Table 2).
Hypothesis 11: Motive, Blame, and Voice
Recall that our predictions relating blame to voice depend on the motives for voicing dissatisfaction. If the goal is to remedy a problem, we would expect voice to be negatively related to plan blame (but positively related to provider blame). Conversely, if the goal is explanation or compensation, then we should observe a positive relationship between blaming the plan and complaining to the plan. The measures of blame used as dependent variables in the models of blame attribution therefore become explanatory variables in the voicing models.
Hypothesis 12: Competence and Voice
The relationship between the perceived competence of the plan and voice again depends on the motive but should be consistent with the results for blame. Consequently, if voicing is found to be positively related to plan blame (suggesting that the explanatory motive dominates), then we should observe a negative relationship between plan competence and voice. Competence is measured by the plan's perceived capacity to cover the client's costs related to the treatment of mental illness, as described earlier (see Table 2).
Controlling for Other Factors Plausibly Related to Consumer Voice
Because there has been so little empirical research on consumer voicing, we could identify only a few variables that need to be controlled in order to accurately assess the relationship between blame and voice. In some other cases, we could identify factors deemed relevant in our conceptual discussions.
A study of appeals involving the court-ordered detention of people with mental illness in the United Kingdom found that the appeals were filed more often on behalf of or by clients who had a higher social status or were less severely ill (Bradley, Marshall, and Gath 1995). Given the obvious parallels to consumer grievances, it seems sensible to control for both social status (measured by educational attainment, as described earlier) and functional status (as measured by symptom severity; see Table 3). Similarly, clients may have a different propensity to voice dissatisfaction than do family members.
Our conceptual treatment of voice also points to several other factors as control variables. The first is the extent to which the plan is perceived to be responsible for the problem in question. As we stated, we assigned all the reported problems to one of three categories, and we would expect voicing to the plan to be the most common response for problems related to payment/coverage and the least common for problems related to the client's medical condition. The frequency of voicing for problems related to treatment should fall in between the other two categories of problems.
Because voicing is related to responsibility, managed care plans should receive more grievances than other health plans do. Managed care plans are perceived by the public as having increasing influence over health care and health outcomes. This influence provides the rationale for a grievance, because the plan is seen to be better able to affect the situation in question. We might therefore expect to find that when respondents are believed to be enrolled in a managed care plan (whether or not they are in fact), they would be more likely to complain to the plan.
Finally, the Hirschmann model suggests that the propensity to voice complaints depends on the availability of exit as a response to dissatisfaction. (Although these might generally be seen as substitutes for each other, Hirschmann notes that the potential for exit may actually increase voice, since an individual who can leave a situation will be less fearful that expressing a grievance will result in any sort of retaliation). We measured the availability of options for exit by the responses to a question about whether the client had been able to switch to another form of health insurance at some time in the previous year. As anticipated, the nature of serious mental illness makes this relatively unlikely. For only 11.6 percent of our cases did the client have an opportunity to switch insurance plans.
We might expect that complaints to health plans and complaints to health care providers would also be related to each other, though again it is unclear whether they would be substitutes or complements for each other. We measured voicing concerns to the client's primary mental health care provider from the list of parties who had been contacted after the problem occurred. Thirty-two percent of the respondents spoke to the provider about the problem. The tendency to contact the provider, of course, may itself be affected by whether the client or a family member felt comfortable contacting the health plan. In statistical terms, this variable is not exogenous to the regression model. Here again, the appropriate statistical solution is to estimate a two-stage regression model in which the predicted value for blame is included as an explanatory variable. Once again, we initially report the simple one-stage model of voice, with complaints to providers as an explanatory variable, and then discuss the results from the more complex two-stage model.
Empirical Findings
The Frequency of Blame and Voice for Problems Related to Mental Health Care
In almost half the cases of adverse events, the respondents assigned blame to either the primary therapist or the health plan. They were more likely to blame the provider (28 percent) than the plan (19 percent). Voicing dissatisfaction in response to problems was quite common. Fifty-five percent of our sample had talked with someone, whether family and friends or professionals, about the problem. However, they were much more likely to speak to the provider (32 percent) than to the plan (7 percent).
Factors Predicting the Attribution of Blame
The results from the single-stage regression models for blame attribution are presented in Table 4. Because logistic regression models produce nonlinear estimators, it can be difficult to interpret the magnitude of a coefficient from the regression models. We therefore have presented, for all coefficients for which the relationship to blame was statistically significant, an odds-ratio capturing the magnitude of the influence of the independent variable on the propensity to blame.4 As these results demonstrate, the propensity to blame did not differ for respondents who were themselves clients, compared with those who were family members of a person with a serious mental illness.
TABLE 4.
Factors Associated with Blame Allocation to Plan and Provider
| Blame to Provider | Blame to Health Plan | |||||
|---|---|---|---|---|---|---|
| Explanatory Variables | Coef. | St. Error | Odds-Ratio | Coef. | St. Error | Odds-Ratio |
| Variables Testing Specific Hypotheses | ||||||
| Hypothesis 1: Problem Involves Treatment | 1.082 | 0.269 | 2.95** | 0.578 | 0.351 | |
| Hypothesis 1: Problem Involves Payment | 0.592 | 0.351 | 1.80# | 1.843 | 0.374 | 6.31** |
| Hypothesis 2: Competence of Plan/Provider | −0.398 | 0.102 | 0.67** | −0.410 | 0.114 | 0.66** |
| Hypothesis 3: Years Client Has Been in Treatment | 0.035 | 0.016 | 1.04* | 0.016 | 0.019 | |
| Hypothesis 4: Severity of Illness (Behavior Problems) | −0.147 | 0.167 | −0.033 | 0.190 | ||
| Hypothesis 5: Plan/Provider Seen as Good Agent | −0.125 | 0.114 | 0.121 | 0.141 | ||
| Hypothesis 6: Social Status (College Educated) | 0.415 | 0.246 | 1.51# | −0.210 | 0.298 | |
| Hypothesis 8: Accurately Knows in Managed Care | 0.244 | 0.360 | 1.23 | 0.411 | 3.40** | |
| Hypothesis 8: Mistakenly Thinks in Managed Care | 1.32 | 0.637 | 3.76* | −12.77 | 444.4 | |
| Hypothesis 8: Not Aware in Managed Care but Is | 0.144 | 0.272 | 0.825 | 0.347 | 2.28* | |
| Variables Used to Control for Other Influences | ||||||
| Knowledge of Grievance Process | −0.960 | 0.454 | 0.38* | 0.307 | 0.479 | |
| Confusion about Paperwork | −0.018 | 0.084 | 0.055 | 0.100 | ||
| Needed Immediate Care in Past Year | 0.015 | 0.015 | −0.059 | 0.047 | ||
| Report from Family (versus Client) | 0.128 | 0.287 | 0.427 | 0.367 | ||
| Time Enrolled in Plan | NA | NA | NA | 0.005 | 0.016 | |
| Aggregate Regression Statistics | ||||||
| Number of observations | 372 | 372 | ||||
| Likelihood ratio (Pr > ChiSq) | 0.001 | 0.001 | ||||
| Pseudo R-squared | 0.140 | 0.157 | ||||
Statistical significance: # Pr < 0.10;
Pr < 0.05
Pr < 0.01.
The findings are consistent with the hypotheses that link blaming to perceptions of responsibility, plausible justifications, and experience with the illness in question. Health care providers are more likely to be blamed for problems in their primary domain of responsibility (treatment); plans, for problems related to their primary responsibility (paying for services). Plans and providers that are seen as incompetent in their core responsibilities are more likely to be blamed. Respondents who have more experience with chronic mental illness (as measured by the time since the client's first diagnosis) are more likely to blame plans and providers, although this relationship is statistically significant only for blaming health care providers.
The other three hypotheses related to blame attribution are less consistent with the regression results. There is no evidence that blame is inhibited by more severe illness or mitigated by the perception that either the health care professional or the health plan is acting in the best interests of the client. Blaming professionals may be weakly related to social status, but this is not true for blaming health plans.
Our tests of hypotheses related to the allocation of blame revealed little evidence supporting either the “blame magnet” or the “hydraulic” hypothesis. Recall that our test of the first of these hypotheses was comparing the blame allocation for clients who were accurately identified as enrolled in managed care plans, clients who were in managed care plans but for whom the respondent was unaware of this fact, and clients who purportedly were in managed care plans but in reality were not. If managed care is in fact a magnet for blame, the first and third of these groups should more frequently blame the health plan for problems than do respondents who accurately identify the client as not being covered by managed care. In fact, however, health plans bear more of the blame in both the first and the second of these categories. In other words, managed care plans are more likely to be blamed for problems even when the respondents are not aware that the plan is one of managed care. This suggests that the greater propensity to blame managed care plans is a result more of their practices than their image.
Curiously, the one case in which misperceptions of managed care appear to affect blame involves health care professionals. Controlling for the other factors measured in the regression models, respondents who mistakenly think that the client is enrolled in a managed care plan are more likely to blame providers for adverse events. We cannot determine whether this reflects a sort of guilt by association for providers or is capturing a propensity to blame providers by those respondents who are the least informed about the health care system. This latter interpretation is consistent with the finding that those who know less about a health plan's grievance process are also more likely to blame providers for adverse outcomes.
We tested the hydraulic hypothesis in two different ways, neither of which revealed a trade-off between blaming the provider and blaming the plan. Including our measures of provider competence and agency in the plan blame regression and vice versa revealed no crossover effects. Estimating a full two-stage model suggested that blaming the provider was not associated with a lower propensity to blame the plan. Nor was blame for the plan predictive of any reduction in blame for the provider. In short, there is no evidence to support a hydraulic relationship in blaming among multiple parties.
The failure to find significant relationships between provider blame and plan blame suggests that attributing blame requires an absolute rather than a relative assessment, much as did the now largely outdated notion of contributory liability in tort cases. Blaming appears to be a serial process in which the role of each actor is considered independently, with little attention to interactions among actors.
Factors Predicting the Expression of Dissatisfaction to the Health Plan
The results from the logistic regression for voice to the plan are presented in Table 5. Again, we present the odds-ratios for those results that are statistically significant to help readers interpret the relative magnitude of the effects.
TABLE 5.
Factors Associated with Expressing Dissatisfaction with Health Plan
| Voicing Complaint to Health Plan | |||
|---|---|---|---|
| Explanatory Variables | Regression Coefficient | Standard Error | Odds-Ratio |
| Hypothesis 10: Benefits and Costs | |||
| Seriousness of problem (impact on client) | 0.916 | 0.445 | 2.50* |
| Plan seen to respond positively to members’ concerns | 0.341 | 0.341 | |
| Knowledge of grievance process | 2.964 | 1.296 | 19.37* |
| Social support in considering grievance | 5.439 | 1.479 | 230.25** |
| Hypothesis 11: Blame and Voice | |||
| Blames health plan | 1.334 | 0.354 | 3.80** |
| Blames primary therapist | −0.464 | 0.478 | |
| Hypothesis 12: Competence | |||
| Plan not seen as competent | 0.632 | 0.266 | 1.88* |
| Variables Used to Control for Other Influences | |||
| Social status (college educated) | 1.001 | 0.715 | |
| Severity of illness (behavior problem index) | −1.334 | 0.670 | 0.26* |
| Problem involves treatment | 2.631 | 1.121 | 13.88* |
| Problem involves payment | 3.636 | 1.180 | 37.95** |
| Accurately knows is in managed care | 1.952 | 1.054 | 7.04# |
| Mistakenly thinks is in managed care | −10.665 | 563.700 | |
| Not aware of being in managed care but is | 0.207 | 1.008 | |
| Report from family (versus client) | −1.578 | 1.007 | |
| Had choice of health plan in past year | 0.621 | 1.069 | |
| Complaint made to primary therapist | 0.333 | 0.769 | |
| Aggregate Regression Statistics | |||
| Number of observations | 341 | ||
| Likelihood ratio (Pr > ChiSq) | 0.001 | ||
| Pseudo R-squared | 0.262 | ||
Statistical significance: # Pr < 0.10;
Pr < 0.05
Pr < 0.01.
These findings substantially support all three of the hypotheses developed for predicting consumer voice. Of most immediate interest are the findings related to blame. Blaming the health plan is positively and significantly related to voicing dissatisfaction to the health plan, while blaming the primary therapist is negatively related to expressing grievances to the plan (though this last relationship is not statistically significant). These results are consistent with the notion that grievances are motivated primarily by a search for an explanation (or recompense or apology), rather than an effort to remedy the problem. The findings related to the plan's perceived competence reinforce this interpretation. Plans that are seen as incompetent in their core responsibilities are more likely to be a target for grievances. Were remedy the primary motive, one would hardly complain to an actor that was incapable of achieving its basic mission.
Other results are consistent with the basic formulation of the voicing model as a multistage reasoning process. Three of the four measures associated with the balancing process for costs and benefits are statistically significant, with particularly large effects for our measures of the cost side of the equation. The more serious the consequences of the adverse event, the more knowledgeable the respondent, and the more available the sources of social support were, the more frequently the respondents complained to the health plan. Also as predicted, plans most likely face grievances for problems associated with core responsibilities and least likely for problems tied to worsening symptoms.
Several other findings merit attention. The more severe a client's symptoms are, the less likely dissatisfaction will be expressed to the health plan. This raises serious concerns about the efficacy of grievance mechanisms for those patients who are the most debilitated and vulnerable. When a client is accurately identified as being enrolled in a managed care plan, the propensity to voice complaints is significantly increased. The origins of this relationship are unclear. They cannot be related to public perceptions of managed care, or else they would also be found among respondents who mistakenly think that the client is enrolled in a managed care plan. They cannot be a simple product of managed care practices, or else the elevated rate of grievances would also apply to clients who are unknowingly in managed care settings. Perhaps only those who are both exposed to managed care practices and aware of this exposure are able to understand the ways in which managed care might positively improve their health care experiences (Schlesinger, Gray, and Perreira 1997).
We also should note some of the relationships that were not found to be statistically significant, although it is important to remember in this regard that our sample was relatively small, reducing the power of our statistical tests. Most strikingly, exit from the plan and voice to the provider appear to be neither substitutes nor complements for expressing grievances to the health plan. (Our measure of plan switching used the potential to switch, not the actual switching from one plan to the next. We will explore this point further in the next section). Lower social status did not appear to deter grievances to the health plan.
Discussion and Conclusion
Our findings suggest that attributional processes have an important role in medical consumerism. Although this was only an exploratory study using relatively crude empirical measures, we were able to identify some of the perceptions and attitudes that are consistently linked to blame attribution. And blaming itself has an independent influence on the willingness of consumers to express their dissatisfaction to their health plan. Blaming is a fairly common response to problems associated with the accessibility of services or the treatment received. Although some aspects of the blame process fit sensibly with our understanding of responsibility and competence, other aspects are more puzzling. Perceived competence plays an important role in blaming, but perceptions of agency do not, even for health care professionals whose fiduciary role is their most salient characteristic. Most curiously, the process of blame attribution does not appear to account for the interaction of the multiple parties—health care providers and health plans—who are contesting for control over the allocation of medical care. Instead, blame appears to be distributed in a serial fashion, with each actor held to an absolute standard in assessing blameworthiness.
How blame is attributed in turn affects the propensity to voice dissatisfaction to the health plan, as do various other factors associated with how individuals understand their health, medical care, and health care system. Because grievance arrangements are becoming an increasingly important mechanism through which policymakers attempt to protect the quality of care, it is essential that we better understand these processes. For example, our finding that social isolation reduces the expression of grievance to the plan is noteworthy, particularly if more elders are enrolled in managed care plans under Medicare's auspices. Since virtually all existing legal requirements for third-party review of health plan decisions require that members first exhaust their appeal options within the plan, factors that inhibit voice to the plan can seriously undermine the effectiveness of these sorts of oversight arrangements.
The various ways in which managed care affects blaming and voice also should be noted. Despite concerns that the managed care “backlash” has made these plans magnets for blame, we found no evidence of this in our analyses. To the contrary—managed care plans were more commonly blamed for adverse events even when the respondents did not identify them as managed care. But mistaken impressions about managed care did appear to affect blame attribution to health care professionals, although the way in which this occurs remains unclear. Finally, we found that managed care plans were more frequently targets for expressed dissatisfaction, at least among those who were aware that they were enrolled in a managed care plan. Here again, the cause of this relationship cannot be easily understood. Managed care plans may be more often the target of complaints because they must have clear and well-publicized grievance mechanisms (Pollitz et al. 1998), although our results controlled for knowledge of the grievance process. And if the results were the consequence of external regulation, they should apply to all those in managed care, whether or not they were aware that they were.
It is important to interpret these findings in light of the limitations of a study of this sort. Because our sample size was relatively small, our analyses may have lacked the statistical power to detect factors that were in fact influencing either the allocation of blame or the determinants of voice. Clearly, it will be important to replicate our study using a larger sample and one with a wider variety of medical conditions. Readers should also be aware of the possibility of reverse causality for some explanatory variables in the regression models. For example, those respondents who experienced a problem may have learned about the grievance process in the course of complaining. When we compared our respondents who reported problems with those who did not, the former were about 30 percent more likely to understand different aspects of the grievance process. Once the respondents had this initial experience, they should be more skilled at expressing grievances related to subsequent problems. But we lacked the information to assess this sort of experiential learning.
Readers may also question the generalizability of results from this study population, on the grounds that cases involving serious mental illness are not an appropriate natural experiment for examining health care consumerism. It is useful to bear in mind that about two-thirds of the cases in the analysis were reported by family members rather than clients. (Statistically controlling for the source of the information in the regression models indicated no distinctive patterns of blaming or voicing for the two types of respondents.) Also, many people with serious mental illness remain quite capable of informed decision making. Indeed, their great experience with illnesses of this sort often allows clients to become extremely sophisticated in their understanding of mental health treatments and the mental health care system.
Other readers may worry that respondents who are affiliated with an advocacy organization like NAMI may be predisposed to more readily blame or more willingly voice complaints than would the average patient. We can neither control for nor estimate the magnitude of these sorts of self-selection effects. But several observations may help assuage these concerns. First, we know that NAMI involvement did not directly affect attitudes or behaviors in this sample, because very few respondents (6 percent of the sample) reported that they had discussed the problem with their local AMI affiliate. Second, although predisposing attitudes might affect the prevalence of blame or voice, there is little reason to expect them to alter the relationship between blame and voice, or any of the other factors that predict blaming or voicing. In other words, we would not expect any qualities of NAMI affiliation to have biased the coefficients in the regression models reported in Tables 4 and 5.
Another consequence of our focus on mental illness may be even more relevant to how we interpret these findings. Coverage of mental health care is often “carved out” from the primary health care plans that cover other forms of illness. As a result, it may be more difficult for clients to understand managed care as it is applied to the treatment of mental illness. This may account for the relatively limited understanding of the grievance processes for the insurance paying for the client's mental health care. Consumers using managed care for other types of illnesses may have an easier time understanding the insurance plan, more accurately allocate blame, and more readily complain about problems when they develop.
Of somewhat greater concern is the crudeness of several of the measures we used as explanatory variables in the regression models. In particular, our measures of agency and competence captured only some dimensions of motives or performance of clinicians and health plans. Certainly it would be useful to replicate this study with a more robust set of measures, such as those that have emerged from recent empirical studies of trust in the health care system (Kao et al. 1998). And our claim to having identified a distinctive impact of blame on consumer behavior depends crucially on our assertion that responsibility can be partitioned into a treatment domain for clinicians and a payment domain for health plans. Because this is clearly a simplification, it would be useful to have more direct measures of the attributions of responsibility for adverse events. It would also be useful to have more direct measures of the motives for voicing grievances to the health plan.
Despite these limitations, we believe that our conceptual framework and empirical explorations shed some light on the process of blame attribution, the expression of dissatisfaction in health care settings, and the ways in which public policy might help consumers become more effective in each of these tasks. We begin by exploring some insights that follow from better understanding the process of blame attribution and the circumstances under which blame is translated into voice.
We started our conceptual analysis by suggesting that blame is part of a process through which people try to make sense of complex events. They may seek to do so for several different reasons. When problems occur, those affected may want to remedy the situation (or to reduce the odds that the problem will recur in the future). Alternatively, they may seek primarily to understand the chain of events, to make cognitive and emotional sense of the circumstances so that they are better able to come to terms with any unfortunate outcomes (Heider 1958). Our findings relating blame to voice suggest that at least in our sample, the latter motive was dominant.
State regulators typically assume the opposite, that the grievance process is being used primarily to remedy problems (e.g., overturning denials of treatment under utilization review). Little attention has been paid to this second function of voice, to make sense of bad outcomes. (The availability of social support may be important because friends and/or family contribute to people's efforts to make sense of the situation, by giving them a chance to talk about it). It is clear that administrative arrangements that work well for one function may work less well for the other. For example, if grievances are intended to prompt remediation, then they must be handled expediently. Indeed, five states have time limits for the plan's internal appeals process. To encourage faster deliberation, decision-making forums are usually kept small and closed.
Speed is not necessarily the object if one is trying to make sense of a problem rather than overturn a decision. For the sense-making function of blaming and voice, it may be more appropriate and efficacious to allow issues to be resolved more deliberately and in a more open forum. Because the injured parties must process the events emotionally as well as cognitively, additional time can be an asset rather than a liability. Part of this closure is having the parties at fault acknowledge their culpability in a public setting, so this sort of grievance deliberation should be made as open as possible, with the results widely disseminated to the public. Indeed, if this were the second avenue for processing complaints available, we believe that it would diffuse much of the current pressure to hold plans liable for their actions under proposals for a federal patients’ bill of rights.
A second set of implications follows from our finding that respondents rarely contacted their health plan when they were unhappy with their care. Only 7 percent of our respondents had contacted the health plan in the previous year. Such infrequent expression of dissatisfaction is not unique to our sample. States that monitor the number of grievances filed with health plans have found that relatively few members express their dissatisfaction in this manner. More optimistic observers have suggested that this may reflect a low level of dissatisfaction with managed care (Pollitz et al. 1998). Our findings imply otherwise. Only 22 percent of the events for which the plan was considered blameworthy resulted in any sort of comment to the plan itself. Problems with treatment were even less likely to trigger a grievance. In only 5 percent of the events in which the provider was deemed blameworthy was there any contact with the health plan.
Respondents who had not contacted the plan were asked why they had not done so. The vast majority indicated that they did not think that the plan could remedy the situation. A smaller portion (about one-third of those who had not complained) felt that complaining might lead to worse treatment by the plan in the future. Juxtaposed against the findings discussed earlier, these results point out an interesting bifurcation in the response to blameworthy situations. Those who complain under these circumstances often do so for reasons other than remedy. But the apparent lack of an effective remedy discourages many others from expressing their dissatisfaction.
What policy initiatives would create a more effective voice for those who have experienced problems with their treatment? According to our findings, better knowledge of the health plan in general and of the availability of grievance processes in particular appear to be important prerequisites to voice. Policymakers can and should adopt far more aggressive programs to provide individuals with this information. Several states, including Massachusetts, New Jersey, New York, and Connecticut, have instituted toll-free phone lines and/or Web sites to give citizens guidance on filing grievances and appealing managed care decisions.
Information alone is unlikely to be adequate. Many complaints appear to be discouraged by the feeling that complaining will do no good. To overcome this perception, state and/or federal regulators need to establish third-party arbitration systems to which people can turn when they receive problematic care. Roughly a dozen states have established programs of this sort. But these programs generally require that members first exhaust their opportunities for a review of grievance within the plan. Although this policy was adopted on sensible grounds—to discourage frivolous complaints—it has a chilling effect on the use of external review, because few people view it as sensible to complain to their health plan, especially for adverse events involving treatment. (Recall that this same pattern of limited complaints to the plan about problems of medical care was replicated in the Kaiser Foundation survey, although that survey did not directly identify which problems were judged to be blameworthy). Under these circumstances, allowing direct appeals to third-party arbiters may be the only mechanism for effectively enhancing voice. Although this may waste some time and resources on trivial complaints, this seems a small price to pay for a system that would provide better safeguards for those who need treatment.
Nor can we rely entirely on review processes that are prompted solely by patients or advocates in their families. As we have seen, patients who are more severely ill and those who are socially isolated are much less likely to express their dissatisfaction, even with events that they consider blameworthy. In short, the most vulnerable are the ones least effectively served by our existing mechanisms for voice. How can we do better? One way is suggested by an additional review of our data on voice. Although only 27 percent of the events in which the plan is considered blameworthy led to a complaint to the plan, more than 40 percent produced some kind of communication with the patient's primary therapist.5 This suggests that the efficacy of voice would be significantly enhanced if policies could encourage health care professionals to relay their patients’ concerns, that is, to be more aggressive advocates on their patients’ behalf (Mechanic 2000).
A final set of implications pertain to the need for “accurate” blaming. As we observed earlier, consumers can appropriately respond to problematic experiences with their health care only if they can identify which parties were the source of the problem. If consumers wrongly attribute problems to plans that are actually the fault of providers (or vice versa), the aggregate satisfaction measures included in the report cards will be systematically biased. To the extent that quality assurance mechanisms rely on members reporting problems with their medical care, inaccurate blaming may undermine the ability of collective purchasers (employers or public programs like Medicare or Medicaid) to protect their beneficiaries from plans that are systematically mistreating health problems.
Because we have no independent source of information about the events reported in our survey, we cannot determine directly whether our respondents appropriately or inappropriately assigned blame. However, several of our findings related to blame attribution offer some clues. Three factors suggest that awareness of managed care is related to blame attribution. The attribution of blame to providers appears to be most strongly affected by our measures of knowledge, experience, and understanding. Respondents who are less informed about their health plan's administration (such as grievance processes), who are less educated, who have less personal experience with mental illness, or who mistakenly think that they are in managed care when they are not, attribute blame very differently than do respondents who are more knowledgeable. (These various factors influence the propensity to blame providers in opposite directions, making it impossible to determine the direction of the bias in blame attribution by less sophisticated individuals). We cannot say conclusively that more knowledgeable respondents attribute blame more accurately, but the potential for erroneous attributions is clearly significant.
Blaming the health plan appears to be less attributable to the knowledge or education of the individuals in the case. Instead, the presence of managed care, rather than the perception of managed care, appears to drive blame attribution. Whether managed care plans are in fact more blameworthy is a matter for additional research.
This article is an initial effort to explore the meaning and ramifications of blame attribution for consumerism in health care. Although we examined some of the specific pathways through which blame is understood and translated into consumer behavior, we have only begun to explore this complex issue. It is our hope that by demonstrating some of the importance of blame attribution, we will encourage other researchers to examine this topic as well. More generally, we believe that it is important for social scientists and health services researchers to embrace a more conceptually nuanced understanding of the process through which people make sense of their health care experiences. Attributional processes appear to play a vital role in the public's understanding of medical care. But these processes have been little studied in this context and are even less well understood. The more that public policy uses consumerism for quality assurance, the more important it is for us to understand its strengths, weaknesses, and potential for enhancement. Clearly, we still have much to learn.
Acknowledgments
This research was supported by grant no. MH43450 from the National Institute of Mental Health. This paper was substantially improved by comments from reviewers for the Milbank Quarterly, as well as by the suggestions of participants in the Health Ploicy Seminar at Yale University. We would also like to thank Allan Horwitz, Stephen Hansell, Patricia Roos, Ira Cohen, Benjamin Zablocki, and the attendees of the Rutgers Sociology Department's Culture and Cognition seminar for their comments on Ms. Rosenthal's related work on blame. Our thinking on this project has also benefited from comments made by David Mechanic, Nancy Wolff, Allan Horwitz, and Jeffery Rubin, as well from the efforts of Anita Franzione, Firoozeh Vali, and Jeffery Mullis in their works on the Managed Care Evaluation Project. We thank Sandra Hoffman and the interviewing team for their assistance in collecting the data used in the empirical section of the article. We especially want to thank the National Alliance for the Mentally Ill and the respondents for their participation in the survey described in this article. Blame for all remaining errors, of course, should be attributed solely to the authors.
Endnotes
Researchers studying the malpractice system recognize the importance of blame in determining the effectiveness of this system in protecting against medical negligence (Brennan, Sox, and Brennan, Sox, and Burstin 1996; May and May and Stengel 1990). Somewhat related concepts were discussed by Brickman and Brickman and colleagues (1982) in their analysis of the ways in which patients made attributions about who was responsible for dealing with psychological disorders.
We recognize that plans can in principle be held responsible for the quality of care provided by their affiliated providers, as most models of managed competition are predicated on exactly this attribution (Enthoven 1993). But studies of consumer decision making are more consistent with the model described in the text, in which responsibility is partitioned, assigned to providers for medical care and to plans for issues of payment. Most consumers do not understand the ways in which a health plan might affect the content of medical care (Jewett and Jewett and Hibbard 1996; Miller and Horowitz 2000), A recent survey by the Kaiser Family Foundation found that members hold plans responsible for problems related to ‘billing and paperwork’ about half again as often as for problems related to medical care (Kaiser Family Foundation 2000).
Hirschmann also emphasized a third concept, the role of ‘loyalty.’ By raising the psychological value of maintaining established relationships, loyalty unambiguously discourages exit. Its impact on voice is much less clear. One can imagine consumers being loyal to a supplier by remaining silent in the face of problems. Alternatively, the most loyal customer might be one who takes the time and effort to try to improve the quality of the services being supplied. Because we are focusing on voice in this article, we do not fully develop the relationship between loyalty and blame. But we do statistically control for behavioral correlates (e.g., length of time enrolled in the health plan) in our empirical analyses of blame.
Because a single respondent could report more than one critical event, the data were ‘clustered,’ in the sense that the error term in the regression models tends to be correlated for the two events reported by a single source. We also estimated models using GEE specifications to adjust for this clustering affect, which did not alter the findings presented in the text.
One might wonder about the overlap between the two forms of voice. Further analysis suggests that for half the complaints to the provider, there was also a complaint to the plan. Put differently, if individuals who complained only to their providers were added to those who complained to their plan, the total rate for voice would be 47 percent of those who had experienced what they considered a blameworthy event involving their health plan. In the Kaiser Foundation survey, among those respondents who had experienced a problem with their health plan, 39 percent had contacted their health plan; 15 percent had contacted both their physician and their health plan; and 18 percent had contacted only their physician (2000, p. 10). These statistics suggest that using physicians as an indirect source of complaint resolution could make the general population's voice almost 50 percent more effective.
References
- Arnould R, Rich R, White W. Competitive Approaches to Health Care Reform. Washington, D.C.: Urban Institute Press; 1993. [Google Scholar]
- Blendon RJ, Brodie M, Benson JM. Understanding the Managed Care Backlash. Health Affairs. 1998;17(4):80–94. doi: 10.1377/hlthaff.17.4.80. [DOI] [PubMed] [Google Scholar]
- Bloche MG. U.S. Health Care after Pegram: Betrayal at the bedside. Health Affairs. 2000;19(5):224–27. doi: 10.1377/hlthaff.19.5.224. [DOI] [PubMed] [Google Scholar]
- Bradley C, Marshall M, Gath D. Why Do So Few Patients Appeal against Detention under Section 2 of the Mental Health Act? British Medical Journal. 1995;310:364–67. doi: 10.1136/bmj.310.6976.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan TA, Leape LL, Laird NM. Incidence of Adverse Events and Negligence in Hospitalized Patients: Results of the Harvard Medical Practice Study I. New England Journal of Medicine. 1991;324(6):370–76. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- Brennan T, Sox C, Burstin H. Relation between Negligent Adverse Events and the Outcomes of Medical Malpractice Litigation. New England Journal of Medicine. 1996;335(26):1963–67. doi: 10.1056/NEJM199612263352606. [DOI] [PubMed] [Google Scholar]
- Brickman P, Rabinowitz VC, Karuza J, Coates D, Cohn E, Kidder L. Models of Helping and Coping. American Psychologist. 1982;37:368–84. [Google Scholar]
- Brown G, Sukys P, Anderson LS. Business and Personal Law. New York: McGraw-Hill; 1988. [Google Scholar]
- Calabresi G. The Costs of Accidents: A Legal and Economic Analysis. New Haven, Conn.: Yale University Press; 1970. [Google Scholar]
- Coates D, Penrod S. Social Psychology and the Emergence of Disputes. Law and Society Review. 15(3–4):655–80. [Google Scholar]
- Cohen P. Response to Attack Splits Arabs in the West. New York Times. 2001:A9–A11. September 29. [Google Scholar]
- Coleman J. The Asymmetric Society. Syracuse, NY: Syracuse University Press; 1982. [Google Scholar]
- Collins MA. University of California at Los Angeles; 1990. Distinctions among the Attributions of Causality, Responsibility, and Blame Including the Effects of Each on Adjustment in a Victimizing Event. Ph.D. diss. [Google Scholar]
- Cunningham PJ, Denk C, Sinclair M. Do Consumers Know How Their Health Plan Works? Health Affairs. 2001;20(2):159–66. doi: 10.1377/hlthaff.20.2.159. [DOI] [PubMed] [Google Scholar]
- Davis K, Collins KS, Schoen C, Morris C. Choice Matters: Enrollees’ Views of Their Health Plans. Health Affairs. 1995;14(2):99–112. doi: 10.1377/hlthaff.14.2.99. [DOI] [PubMed] [Google Scholar]
- Emanuel E, Brett A. Managed Competition and the Patient-Physician Relationship. New England Journal of Medicine. 1993;329(12):879–82. doi: 10.1056/NEJM199309163291213. 10.1056/NEJM199309163291213. [DOI] [PubMed] [Google Scholar]
- Enthoven AC. The History and Principles of Managed Competition. Health Affairs. 1993;12(suppl.):24–48. doi: 10.1377/hlthaff.12.suppl_1.24. [DOI] [PubMed] [Google Scholar]
- Enthoven AC, Singer S. The Managed Care Backlash and the Task Force in California. Health Affairs. 1998;17(4):95–110. doi: 10.1377/hlthaff.17.4.95. [DOI] [PubMed] [Google Scholar]
- Felstiner WL, Abel R, Sarat A. The Emergence and Transformation of Disputes: Naming, Blaming and Claiming. Law and Society Review. 9(3)(4):631–95. 1980–81. [Google Scholar]
- General Accounting Office (GAO) Washington, D.C.: 1994. Health Care Reform: “Report Cards” Are Useful but Significant Issues Need to Be Addressed. GAO/HEHS-94-219. [Google Scholar]
- Giddens A. Modernity and Self-Identity. Stanford, Calif.: Stanford University Press; 1991. [Google Scholar]
- Hart HLA. Punishment and Responsibility. Oxford: Oxford University Press; 1968. [Google Scholar]
- Haug MR, Lavin B. Practitioner or Patient—Who's in Charge? Journal of Health and Social Behavior. 1981;22(3):212–29. [PubMed] [Google Scholar]
- Haug MR, Lavin B. Consumerism in Medicine: Challenging Physician Authority. Beverly Hills, Calif.: Sage; 1983. [Google Scholar]
- Heider F. The Psychology of Interpersonal Relations. New York: Wiley; 1958. [Google Scholar]
- Herzlinger RE. Market Driven Health Care: Who Wins, Who Loses in the Transformation of America's Largest Service Industry. Reading, Mass.: Addison-Wesley; 1997. [Google Scholar]
- Hewstone M, editor. Attribution Theory: Social and Functional Extensions. Oxford: Blackwell; 1983. [Google Scholar]
- Hibbard JH, Harris-Kojetin L, Mullin P, Lubalin J, Garfinkel S. Increasing the Impact of Health Plan Report Cards by Addressing Consumers’ Concerns. Health Affairs. 2000;19(5):138–43. doi: 10.1377/hlthaff.19.5.138. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Weeks EC. Consumer Use of the Physician Fee Information. Journal of Health and Human Resources Administration. 1985;7:321–35. [PubMed] [Google Scholar]
- Hibbard JH, Weeks EC. Consumerism in Health Care: Prevalence and Predictors. Medical Care. 1987;25(11):1019–32. doi: 10.1097/00005650-198711000-00001. [DOI] [PubMed] [Google Scholar]
- Hickson GB, Clayton EW, Githens PB, Sloan FA. Factors That Prompted Families to File Medical Malpractice Claims Following Perinatal Injuries. Journal of the American Medical Association. 1992;267(10):1359–63. [PubMed] [Google Scholar]
- Hirschmann A. Exit, Voice and Loyalty: Responses to Decline in Firms, Organizations and States. Cambridge, Mass.: Harvard University Press; 1970. [Google Scholar]
- Hoy EW, Curtis RE, Rice T. Change and Growth in Managed Care. Health Affairs. 1991;10(4):18–36. doi: 10.1377/hlthaff.10.4.18. [DOI] [PubMed] [Google Scholar]
- Immerwahr J, Johnson J, Kernan-Schloss A. Faulty Diagnosis: Public Misconceptions about Health Care Reform. New York: Public Agenda Foundation; 1992. [Google Scholar]
- Isaacs SL. Consumers’ Information Needs: Results of a National Survey. Health Affairs. 1996;15(4):31–41. doi: 10.1377/hlthaff.15.4.31. [DOI] [PubMed] [Google Scholar]
- Iyengar S. Framing Responsibility for Political Issues: The Case of Poverty. Political Behavior. 1990;12(1):19–40. [Google Scholar]
- Jacobs LR, Shapiro RY. The American Public's Pragmatic Liberalism Meets Its Philosophical Conservatism. Journal of Health Politics, Policy and Law. 1999;24(5):1021–31. doi: 10.1215/03616878-24-5-1021. [DOI] [PubMed] [Google Scholar]
- Jewett JJ, Hibbard JH. Comprehension of Quality of Care Indicators: Differences among Privately Insured, Publicly Insured and Uninsured. Health Care Financing Review. 1996;18(1):75–94. [PMC free article] [PubMed] [Google Scholar]
- Jones EE, Davis KE. From Acts to Dispositions: The Attribution Process in Person Perception. Advanced Experiments in Social Psychology. 1965;2:219–66. [Google Scholar]
- Kaiser Family Foundation. Survey of Americans about Health Care and the Stock Market. Menlo Park, Calif.: Kaiser Family Foundation; 1998. [Google Scholar]
- Kaiser Family Foundation. National Survey on Consumer Experiences with Health Plans. Menlo Park, Calif.: Kaiser Family Foundation; 2000. [Google Scholar]
- Kao A, Green D, Zaslavsky A. The Relationship between Method of Physician Payment and Patient Trust. Journal of the American Medical Association. 1998;280(19):1708–14. doi: 10.1001/jama.280.19.1708. [DOI] [PubMed] [Google Scholar]
- Kelley HH. Attribution Theory in Social Psychology. Nebraska Symposium on Motivation. 1967;15:192–238. [Google Scholar]
- Kultgen J. Ethics and Professionalism. Philadelphia: University of Pennsylvania Press; 1988. [Google Scholar]
- Lane RE. Moral Blame and Causal Explanation. Journal of Applied Psychology. 2000;17(1):45–58. [Google Scholar]
- Lau RR, Bernard TM, Hartman K. Further Explorations of Common-Sense Representations of Common Illnesses. Health Psychology. 1989;8(2):195–219. doi: 10.1037//0278-6133.8.2.195. [DOI] [PubMed] [Google Scholar]
- Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-Patient Communication: The Relationship with Malpractice Claims among Primary Care Physicians and Surgeons. Journal of the American Medical Association. 1997;277(7):553–59. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- Long SH, Marquis MS. Results from the Community Tracking Survey. Health System Change Data Bulletin. 1998;12:1. summer. [Google Scholar]
- Maxwell J, Briscoe F, Davidson S. Managed Competition in Practice: “Value Purchasing” by Fourteen Employers. Health Affairs. 1998;17(3):216–26. doi: 10.1377/hlthaff.17.3.216. [DOI] [PubMed] [Google Scholar]
- May ML, Stengel DB. Who Sues Doctors? How Patients Handle Medical Grievances. Law and Society Review. 1990;24(1):105–20. [Google Scholar]
- McGraw KM. Avoiding Blame: An Experimental Investigation of Political Excuses and Justifications. British Journal of Political Science. 1990;20:119. [Google Scholar]
- Mechanic D. Consumer Choice among Health Insurance Options. Health Affairs. 1989;8(1):138–48. doi: 10.1377/hlthaff.8.1.138. [DOI] [PubMed] [Google Scholar]
- Mechanic D. Changing Medical Organization and the Erosion of Trust. Milbank Quarterly. 1996;74(2):171–89. [PubMed] [Google Scholar]
- Mechanic D. Managed Care as a Target of Distrust. Journal of the American Medical Association. 1997;277(22):1810–12. [PubMed] [Google Scholar]
- Mechanic D. Managed Care and the Imperative for a New Professional Ethic. Health Affairs. 2000;19(5):100–11. doi: 10.1377/hlthaff.19.5.100. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Schlesinger M. The Impact of Managed Care on Patients’ Trust in Medical Care and Their Physicians. Journal of the American Medical Association. 1996;275(21):1693–97. [PubMed] [Google Scholar]
- Mechanic D, Schlesinger M, McAlpine D. Management of Mental Health and Substance Abuse Services: State of the Art and Early Results. Milbank Quarterly. 1995;72(4):19–56. [PubMed] [Google Scholar]
- Miller TE. Managed Care Regulation: In the Laboratory of the States. Journal of the American Medical Association. 1997;278(13):1102–9. doi: 10.1001/jama.278.13.1102. [DOI] [PubMed] [Google Scholar]
- Miller TE, Horowitz CR. Disclosing Doctor's Incentives: Will Consumers Understand and Value the Information. Health Affairs. 2000;19(4):149–55. doi: 10.1377/hlthaff.19.4.149. [DOI] [PubMed] [Google Scholar]
- Noble A, Brennan T. The Stages of Managed Care Regulation: Developing Better Rules. Journal of Health Politics, Policy and Law. 1999;24(6):1275–305. doi: 10.1215/03616878-24-6-1275. [DOI] [PubMed] [Google Scholar]
- Oberlander J. Is Premium Support the Right Medicine for Medicare. Health Affairs. 2000;19(5):84–99. doi: 10.1377/hlthaff.19.5.84. [DOI] [PubMed] [Google Scholar]
- Parsons T. The Social System. New York: Free Press; 1951. [Google Scholar]
- Perkins J, Olson K, Rivera L. Los Angeles: National Health Law Program; 1998. Ombudsprograms and Member Advocates: Consumer-Oriented Approaches to Problem-Solving in Medicaid Managed Care. [Google Scholar]
- Phares V, Ehrbar LA, Lum JJ. Parental Perceptions of the Development and Treatment of Children's and Adolescents’ Emotional/Behavioral Problems. Child and Family Behavior Therapy. 1996;18:19–36. [Google Scholar]
- Pollitz K, Dallek G, Tapay N. External Review of Health Plan Decisions: An Overview of Key Program Features in the States and Medicare. Menlo Park, Calif.: Kaiser Family Foundation; 1998. [Google Scholar]
- Pottick KJ, Davis DM. Attributions of Responsibility: Parents and Professionals at Odds. American Journal of Orthopsychiatry. 2001;71(3):66–84. doi: 10.1037/0002-9432.71.4.426. [DOI] [PubMed] [Google Scholar]
- Reschovsky J, Hargraves JL. Health Care Perceptions and Experiences: It's Not Whether You Are in an HMO, It's Whether You Think You Are. Washington, D.C.: Center for Studying Health System Change; 2000. Issue brief no. 30. [PubMed] [Google Scholar]
- Rodwin MA. Patient Accountability and Quality of Care: Lessons from Medical Consumerism and the Patients’ Rights, Women's Health and Disability Rights Movement. American Journal of Law & Medicine. 1994;20:147–74. [PubMed] [Google Scholar]
- Rodwin MA. The Neglected Remedy: Strengthening Consumer Voice in Managed Care. The American Prospect. 1997;34:45–50. [Google Scholar]
- Rodwin MA. Exit and Voice in American Health Care. University of Michigan Journal of Law Reform. 1999;32(4):1041–67. [Google Scholar]
- Ross C, Wheaton B, Duff R. Client Satisfaction and the Organization of Medical Practice: Why Time Counts. Journal of Health and Social Behavior. 1981;22(9):243–55. [PubMed] [Google Scholar]
- Roter DL, Hall JA. Doctors Talking with Patients/Patients Talking with Doctors. Westport, Conn.: Auburn House; 1992. [Google Scholar]
- Sapinwall A, Seitz MZ. Target: Terror. Newark Star Ledger. 2001:87. October 4, p. [Google Scholar]
- Schlesinger M. Countervailing Agency: A Strategy of Principled Regulation under Managed Competition. Milbank Quarterly. 1997;75(1):35–87. doi: 10.1111/1468-0009.00044. 10.1111/1468-0009.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesinger M, Druss B, Thomas T, Allen H. No Exit: The Impact of Health Status on Choice and Disenrollment from Managed Care Plans. Health Services Research. 1999;34(2):547–76. [PMC free article] [PubMed] [Google Scholar]
- Schlesinger M, Gray B, Perreira K. Medical Professionalism under Managed Care: The Pros and Cons of Utilization Review. Health Affairs. 1997;16(1):106–24. doi: 10.1377/hlthaff.16.1.106. [DOI] [PubMed] [Google Scholar]
- Shaver K. The Attribution of Blame: Causality, Responsibility and Blameworthiness. New York: Springer-Verlag; 1985. [Google Scholar]
- Simmel G. The Isolated Individual and Dyad: The Triad. In: Wolff Kurt., editor. The Sociology of Georg Simmel. New York: Free Press; 1950. [Google Scholar]
- Skitka LJ, Tetlock PE. Of Ants and Grasshoppers: The Political Psychology of Allocating Public Assistance. In: Mellers BA, Baron J, editors. Psychological Perspectives on Justice. Cambridge: Cambridge University Press; 1993. pp. 205–33. [Google Scholar]
- Sofaer S. Informing and Protecting Consumers under Managed Competition. Health Affairs. 1993;12(supp.):76–86. doi: 10.1377/hlthaff.12.suppl_1.76. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJ, Balding J. British Parents’ Beliefs about the Causes of Three Forms of Childhood Psychological Disturbance. Journal of Abnormal Child Psychology. 1993;21:367–76. doi: 10.1007/BF01261599. [DOI] [PubMed] [Google Scholar]
- Stone D. Causal Stories and the Formation of Policy Agendas. Political Science Quarterly. 1989;104(2):281–300. [Google Scholar]
- Tapay N, Feder J, Dallek G. Protection for Consumers in Managed Care Plans: A Comparison of Medicare, Medicaid and the Private Insurance Market. Menlo Park, Calif.: Kaiser Family Foundation; 1998. [Google Scholar]
- Thorne SE. Negotiating Health Care: The Social Context of Chronic Illness. Newbury Park, Calif.: Sage; 1993. [Google Scholar]
- Weiner B. Judgments of Responsibility. New York: Guilford Press; 1995. [Google Scholar]
- Werth B. Damages: One Family's Legal Struggles in the World of Medicine. New York: Simon & Schuster; 1998. [Google Scholar]
- Woodward R, Warren-Boulton F. Considering the Effects of Financial Incentives and Professional Ethics on Appropriate Medical Care. Journal of Health Economics. 1984;3(3):223–37. doi: 10.1016/0167-6296(84)90012-2. 10.1016/0167-6296(84)90012-2. [DOI] [PubMed] [Google Scholar]


