In the last decade, the health status of individuals with disabilities has emerged as an explicit focus of public health attention, with consumers, policymakers, and researchers joining in defining and implementing an agenda in this area. With small federal grants from a few agencies, the field has begun to produce research findings, academic curricula, and model policies and interventions to promote health and prevent adverse outcomes among people with disabilities (Andresen, Lollar, and Meyers 2000;Lollar 1994;Pope 1992;Seekins, White, Ravesloot, et al. 1999;Simeonsson and McDevitt 1999;Tanenhaus, Meyers, and Harbison 2000). The development of the term secondary conditions and the inclusion of the chapter “Disability and Secondary Conditions” in Healthy People 2010 (U.S. Dept. of Health and Human Services 2000) reflect this progress toward recognizing disability as a national public health issue.
At the state level, however, the notion that disability is a public health issue is still considered novel. State governments generally recognize disability as a focus of agencies that address rehabilitation, medical assistance, veterans” services, architectural access, employment, and transportation access. Specific conditions may be viewed as falling solely within the purview of targeted agencies like the departments of mental retardation and mental health. The chapter in Healthy People 2010 thus may encourage a concentration on disability in state and local public health activities.
The concept of secondary conditions is also still making its way into public health and some parts of the medical community. In 1988, Michael Marge first defined what he called secondary disabilities. Countering the notion of disability as the immutable and static outcome of physiological impairment, he noted that the health status of an individual with an impairment could, in fact, either worsen or improve. He also pointed out that an individual's health status reflected not only his or her primary condition but also any additional condition(s) at higher risk because of the primary disability (Marge 1988).
An Institute of Medicine (IOM) report in 1991 cited Marge's work but centered on what it termed secondary conditions (Institute of Medicine 1991). Drawing on the work of Nagi (1965, 1969), the report noted that the conditions for which a prior disability placed one at risk might or might not actually become disabling, partly depending on preventive interventions. Theoretically, the report suggested, both secondary conditions and any resulting additional disabilities could be prevented. Simeonsson and Leskinen (1999) compared models of disability and secondary conditions from the literature and agreed that secondary conditions were, by definition, preventable.
Although interested parties agree that secondary conditions are a common problem among people with disabilities, the term secondary conditions itself does not yet have an agreed-upon operational definition. Krause and Bell (1999) defined secondary conditions as physical and mental health conditions indirectly resulting from a primary disabling condition. Other studies (Lollar 1994, 1999; McMillen, Simeonsson, and McDevitt 1999; Seekins, Clay, and Ravesloot 1994; Simeonsson and Leskinen 1999) and the chapter on disabilities in Healthy People 2010 (U.S. Dept. of Health and Human Services 2000) use broader definitions, including self-concept, work and social participation, health-related economic consequences for the individual or family, and other family members. Healthy People 2010 defines secondary conditions as “medical, social, emotional, family, or community problems that a person with a primary disabling condition likely experiences.” At the National Conference on Disability and Women in 1999, Margaret Turk suggested that the “promotion of the health of people with disabilities” was a better way to conceptualize the range of issues raised in the discussion of preventing secondary conditions (Turk 1999). While the exact definition is still evolving, the emerging consensus is that secondary conditions (1) presuppose the existence of a disability (2) but are not necessarily consequences of it. Since the IOM report was published, researchers have identified various factors as predictive of secondary conditions.
A primary disabling condition is typically assumed to be predictive of the type of secondary conditions that follow it (for a recent example, see Marge 1999). As an alternative or an addition to a specific diagnosis, activity limitation and functional status have been investigated as potential predictors of secondary conditions (Verbrugge and Jette 1994). Beyond the primary disabling condition, physical and social environmental factors are widely acknowledged to mediate the development of secondary conditions. For example, Seekins and colleagues (1999) cited the importance of health promotion programs in reducing the number of secondary conditions among a sample of people with mobility impairments. Research on these factors has been limited, however, by the lack of research tools to characterize the environment affecting the lives of individuals with disabilities (Marge 1988;Rimmer 1999;Seekins, Clay, and Ravesloot 1994). Individual lifestyle and behavior choices are a fourth set of factors discussed in the literature as predictive of the health of individuals with disabilities (Seekins, Clay, and Ravesloot 1994;Turk, Geremski, and Rosenbaum 1997). In addition, sociodemographics, personal attributes such as self-concept, and aging (for children, developmental level) must be taken into account.
The Massachusetts Department of Public Health (MDPH) and the Boston University School of Public Health (BUSPH) developed the Massachusetts Survey of Secondary Conditions (MSSC) in 1995 to explore the epidemiology of secondary conditions. The MDPH was particularly interested in the possible impact of environmental factors amenable to public health intervention—such as access to personal and technology assistance, transportation, and health care—on the development of secondary conditions. As the sponsor of numerous programs aimed at promoting healthy behaviors (e.g., smoking cessation and exercise), the MDPH also investigated relationships between behavior and secondary conditions. The authors designed a conceptual framework to predict secondary conditions among adults with a broad range of disabilities living independently in Massachusetts. This framework guided the development of the MSSC and the analyses that we discuss in this article.
The key hypothesis of our study was that by controlling for type and severity of disabling condition or functional limitation and also for confounding sociodemographic factors, we would find fewer and less severe secondary conditions among respondents who
Received paid or unpaid personal assistance services appropriate to their activities of daily living (ADLs) and instrumental activities of daily living (IADLs) dependencies.
Reported no problems with accessing health promotion or disease prevention programs or activities.
Had consistent and continuous primary care.
Reported adequate access to other health care services.
Had better access to transportation.
Followed prescribed self-care regimens and reported no tobacco use or other high-risk behaviors.
We also hypothesized that people who reported fewer and less compromising secondary conditions would also report higher general levels of health and life satisfaction.
In this article we present (1) an analysis of baseline interviews with 656 MSSC respondents about whether they had experienced any of 17 secondary conditions; (2) an examination of the relationship among the primary disabling condition, the mediating factors, and the number of secondary conditions; (3) a multivariate analysis of the association among a number of secondary conditions, the primary disabling condition, the mediating factors, and other health outcomes; and (4) the association among the primary disabling condition, mediating factors, and two types of secondary conditions.
Conceptual Framework
Our MSSC conceptual framework (see figure 1) shows the relationship between health outcomes and those environmental factors amenable to public health intervention. The framework presupposes the existence of a disability, defined in terms of both “primary disabling condition” and activity limitations. We intended “primary disabling condition” to be self-reported (see Questionnaire Design, below), and it was variously reported as a diagnosis, injury, or impairment (e.g., spinal cord injury, spinal bifida, psychiatric conditions, multiple sclerosis). Activity limitations were defined according to measures of ADLs and IADLs. We explain these measures in the next section.
fig 1.
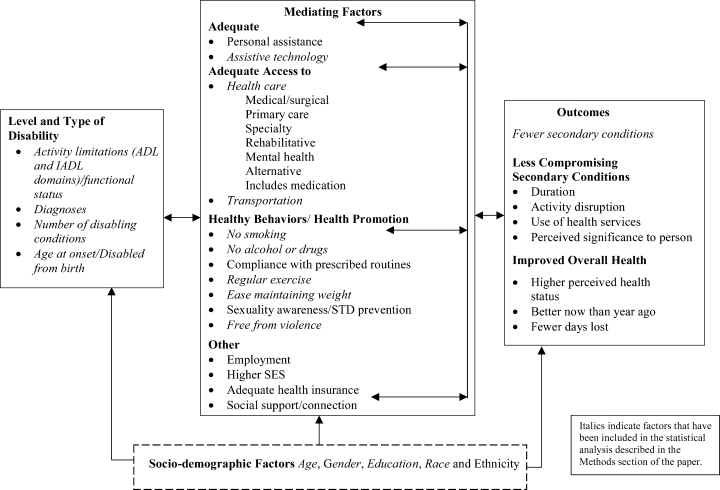
Massachusetts Survey of Secondary Conditions (MSSC) conceptual framework.
Although a variety of factors may “mediate” the relationship of an existing disability to the health outcomes in our framework, we focused on those identified as amenable to public health intervention defined by core public health functions (Institute of Medicine 1988, 1997) and thus most relevant to the MDPH. These “mediators” include adequacy of personal assistance and assistive technology, access to health care, access to transportation, healthy behaviors, access to health promotion programs or strategies, and insurance coverage. The framework also reports sociodemographic factors (gender, race/ethnicity, age, and education) in order to account for their possible confounding effects.
Health outcomes in the framework and the MSSC were self-reported health status, change in health status, number of days unable to do routine activities, and number and severity of secondary conditions. We defined secondary conditions as preventable physical and mental health conditions directly or indirectly resulting from a primary disabling condition. Examples of secondary conditions are anxiety, depression, burns, falls, chronic pain, respiratory infections, and contractures. Note that this definition of secondary conditions is narrower than some in the literature. Other authors cite unemployment, problems with weight regulation, and difficulty with access to services and medical care (McMillen, Simeonsson, and McDevitt 1999;Seekins et al. 1999;Simeonsson and Leskinen 1999;U.S. Dept. of Health and Human Services 2000). By contrast, we view such variables as either indicators of “participation” and “quality of life,” which may be affected by disability and secondary conditions, or factors mediating the development of secondary conditions.
Health outcomes, including secondary conditions, reflect the dynamic interplay of these factors. The MSSC framework draws heavily on insights from the IOM disability model, which uses interrelated circles to depict the interplay of multiple feedback loops affecting the development of secondary conditions (Institute of Medicine 1991). Although our MSSC model is not as dynamic as the IOM model, we tried to represent feedback within the system with double-sided arrows (figure 1). Together, a disability and/or functional limitation, individual sociodemographic characteristics, and mediating environmental factors put a person at increased risk for a secondary condition, which in turn can directly or indirectly influence the mediating factors, primary disabling condition, and functional limitation. For example, although the need for technological assistance may be driven by an individual's activity limitation (such as a limited ability to reach and pick up objects); with the appropriate technology (a grabber), the functional consequences of that limitation may be mitigated. Conversely, the lack of accessible transportation or the inability to pay for prescribed medication may increase dependency in activities of daily living.
Methods
Our survey consisted of three phases of data collection, and this article is based on baseline data collected from 656 respondents in 1996–98.
Sample Selection
The survey included respondents recruited from six independent living centers (ILCs) and two health maintenance organizations (HMOs) in Massachusetts. We decided to use a convenience sample because of the cost and the logistical complexity of locating adults with major disabling conditions in the general population. Although our sample was not random or based on population, the eight participating organizations were asked to select respondents systematically, for example, every third name from their alphabetical membership lists.
ILCs generally provide information and referrals, independent living skills training, peer counseling, individual advocacy, and other services to people with disabilities. The ILCs from which the MSSC respondents were drawn are located in Boston, Salem, Lawrence, Worcester, Amherst, and Pittsfield. We chose these six centers because their members represent a wide range of geographic locales, demographic characteristics, living circumstances, and disabling conditions.
The two HMOs were Community Medical Alliance (CMA) and Neighborhood Health Plan (NHP). CMA is a risk-based, capitated system exclusively for Massachusetts Medicaid (MassHealth) enrollees with major disabilities (Glover, Master, and Meyers 1996;Master, Dreyfus, Connors, et al. 1996). NHP is a capitated system that serves largely Medicaid, health center, and other low-income clients. While all CMA enrollees would have been appropriate respondents for the MSSC, we selected only those NHP members who were eligible for both MassHealth and federal Supplemental Security Income, which is restricted to individuals with disabilities. Eligible respondents had to be at least 18 years old at the time of recruitment and able to provide independent informed consent. No provision was made for proxy interviews. Potential respondents first received letters from an ILC or HMO explaining the project and inviting them to participate. They were offered a $20 honorarium for a completed interview. ILC or HMO staff later contacted the respondents to review information about the project and to obtain their consent to participate. Consenting respondents were asked to provide their names, addresses, telephone numbers, and Social Security numbers, which the ILC or HMO representatives gave to the research staff. Research assistants from the BUSPH then contacted the respondents to offer more information about the study and either schedule or conduct interviews.
Of the 656 interviews, 91 percent were by telephone using Ci3 software (Sawtooth Software in Sequim, Washington). Due to special circumstances (e.g., speech or hearing impairment, lack of telephone privacy, or respondent's request), the rest were in-person interviews conducted at either the respondent's home or another site (medical office, work site, or shelter). The median time for the interviews was 65 minutes, with a range of 45 minutes to more than two hours. After it began, fewer than 1 percent of respondents terminated the interview.
The ILCs and HMOs initially identified 1,487 individuals for interviews. Of those identified, 296 (20%) could not be contacted, and another 128 (9%) were ineligible because of age, death, institutionalization, or inability to give informed consent. Another 15 percent (227) refused to allow their names to be given to the BUSPH for the study. Of the 836 remaining persons whose names were provided to interviewers at the BUSPH, 111 (13%) were ineligible; 20 (2%) could not be contacted; and an additional 49 (6%) refused to participate. Excluding those known to be ineligible, the remaining 932 made up the total sample of respondents for the survey. The participation rate of the total sample was 70 percent (656/932).
Questionnaire Design
In order to elicit information about all components of the MSSC framework, we chose our baseline survey questions from three sources: (1) an earlier study of the health and health care experiences of the Independent Living–Primary Care (IL–PC) Program (Meyers, Cupples, Lederman, et al. 1988); (2) widely used and validated measures such as the Medical Outcomes Study (MOS) SF-36 (McHorney, Ware, Rogers, et al. 1992;Stewart 1992;Ware 1992) and the Craig Handicap Assessment and Reporting Technique (CHART) (Whiteneck, Charlifue, Gerhart, et al. 1992); and (3) new questions developed specifically for this survey by the research team.
The baseline survey contained approximately 350 questions covering demographics; major disabling condition; ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs); use of assistive devices and personal assistance; preventive and routine care; access to health care and other services; access to transportation; history of alcohol, tobacco, and drug use; and severity, duration, and consequences of secondary conditions. The participants themselves defined their disability in response to the question “What is your primary disabling condition?” Activity limitations were elicited through questions about ADLs and IADLs and the use of assistive technology and paid and unpaid personal care assistance. In order to ascertain secondary conditions, researchers asked about any “health problems” the respondents had experienced in the past 12 months, using a list of 17 secondary conditions selected from “Secondary Disability Prevention” by Seekins and colleagues (1990), supplemented by input from focus groups (persons with disabilities and providers of their care) and MDPH staff and advisory committee members. Those conditions listed in the survey administered at the baseline phase were urinary tract infection, skin problem (pressure sore, ulcer), depression, bowel problem, spasm, respiratory infection (e.g., flu and pneumonia but not colds), asthma, chronic pain, migraine, anxiety, reaction to medication, contracture, burns, falls or other types of injury, fatigue, autonomic dysreflexia, and seizure. For each condition, the respondents were asked about its frequency, duration, and need for medical or emergency care; bed days; and days lost from work or school. The respondents also were asked if they had experienced any conditions that were not on the list.
Analysis
We calculated the means and standard deviations for the continuous variables and the percentage of positive responses for categorical variables for the 656 persons in the sample, and we used T-tests to explore bivariate associations between the number of secondary conditions and other health outcomes. Hierarchical multiple regression (Tabachnick and Fidell 1983) was used to characterize the relationship between the number of secondary conditions an individual experienced and six sets of factors derived from the conceptual framework. Although the framework allows for multidirectional relationships, the regression model is unidirectional. In order of entry into the regression, the factors were (1) sociodemographics, (2) type of disability, (3) activity limitation, (4) access, (5) substance use, and (6) other health risks. The hierarchical entry of the sets of these factors into the model clarified the effect that each had on the number of secondary conditions while controlling for previously entered variables. After we entered the sociodemographic variables to control for known associations between them and health, we were able to isolate the unique predictive influence of such mediating factors as access, substance use, and other health risks. The significance level was set at p≤.05.
The sociodemographic factors entered in step 1 of the regression were age, gender, race/ethnicity, and years of formal education. Race/ethnicity was categorized as two groups, white and nonwhite. Because of their small numbers, black non-Hispanics, Hispanics, Asians, Native Americans, and others were treated as one group.
Two variables, primary disabling condition and number of disabling conditions, were added in step 2 to indicate the type of disability. The primary disabling condition was defined according to four dummy variables: spinal cord injury (SCI), cardiovascular/pulmonary conditions (CV), cerebral palsy and spina bifida (CP/SB), and other conditions. SCI, CV, and CP/SB comprised the three categories of disabling conditions most prevalent in our sample. The fourth dummy variable, other disabling conditions, included heterogeneous conditions. Spinal cord injury was used as the reference category in the model. The number of disabling conditions was captured as a two-level categorical variable: 1 = more than one disabling condition versus 0 = one primary disabling condition.
Activity limitation was entered in step 3 and was represented in the regression by the number of domains of ADL dependency and IADL difficulty. The ADL and IADL scales are two well-known measures of functional assessment (Katz 1983). ADLs reflect an individual's ability to perform routine personal care functions independently. In the MSSC, respondents were asked whether they needed help with bathing, getting from bed to chair, dressing, eating, bladder and bowel functions, personal grooming, wheelchair transfer, or indoor mobility. IADLs indicate that an individual is able to perform activities at a higher level of behavioral complexity than ADLs, such as those associated with home management and independent living. Respondents in the MSSC were asked whether they had difficulty with food preparation, shopping, or personal finance. The range of ADL dependency was 0 to 9, and the range of difficulty with IADL was 0 to 3.
The remaining three factors in the model—access, substance use, and other health risks—are defined in the conceptual framework as mediating factors. Access refers to difficulty obtaining transportation to all places, the number of ADLs with which an individual needed more help than he or she received, difficulty getting medical or surgical care, self-reported quality health care, unmet need for mobility aids, and unmet need for communication aids. The use of personal assistance services was not included in the model because of collinearity with ADL dependency, and the number of IADLs with which a person needed more help was not included because of collinearity with IADL difficulty. Substance use refers to whether an individual reported using tobacco during the four weeks before the interview, consuming three or more alcoholic drinks on any occasion four weeks before the interview, or using marijuana during the 12 months before the interview. Other health risks measured whether the respondent reported difficulty maintaining weight or engaging in physical exercise and whether he or she had been assaulted (hit, pushed, or physically hurt) in the past 12 months. Assault was used as a negative proxy for “violence-free environment,” a variable in the conceptual framework for which more direct measures were lacking.
The third step of the analysis examined the association between three other health outcomes and number of secondary conditions, controlling for type and level of disability, sociodemographics, and the mediating factors from our theoretical framework. The three health outcomes were (1) fair/poor versus good/very good/excellent health status, (2) somewhat/much worse versus same/somewhat better/much better health now than a year ago, and (3) number of days unable to do routine activities. The first two outcomes were analyzed using logistic regression models and the third using a multiple regression model.
We used factor analysis with a varimax rotation to determine whether and how secondary conditions could be grouped together. Two secondary conditions, migraines and seizures, were excluded from the factor analyses, since they were eliminated from later (post-baseline) phases of the survey. A correlation coefficient of .40 was selected as the cutoff for factor loadings. This produced two factors of four items each. Factor 1 was spasms (factor loading = .56), urinary tract infections (.54), autonomic dysreflexia (.51), and skin problems (.49). Factor 2 was depression (.65), anxiety (.62), fatigue (.53), and chronic pain (.42). The seven secondary conditions that did not meet the cutoff criterion were falls/injuries, bowel problems, asthma, respiratory infections, reactions to medicine, burns, and contractures.
Based on the factor analysis, we created two variables to describe specific types of secondary conditions. Variable 1 indicated anyone who reported secondary conditions that loaded on factor 1, which we characterized as “paralysis/mobility-related secondary conditions” (82% of respondents), and variable 2 indicated anyone who reported conditions that loaded on factor 2, which we characterized as “mental health/chronic pain conditions” (67.5% of respondents). The fourth step of the analysis examined the association between the two types of secondary conditions and level of disability, activity limitations, sociodemographics, and mediating factors, based on two separate logistic regression models. Given our theoretical framework, all these variables are of interest and were included in the multivariable analysis.
Results
Sample Description
The sample's characteristics are reported in table 1. The 656 respondents who participated in the baseline survey were, on average, 44 years old, with 13 years of formal education. Fifty-eight percent were women. Almost 73 percent were white non-Hispanic; 18 percent were black non-Hispanic; 5 percent were Hispanic; and fewer than 5 percent were Native American, Asian, or other racial groups. Half the respondents lived alone. All but three reported at least one source of health insurance; 40 percent were enrolled in both Medicaid and Medicare, 38 percent in Medicaid only, 11 percent in Medicare only, and the remaining 11 percent covered by other public or private insurance. Forty-six percent of the respondents were enrolled in an HMO.
TABLE 1.
Massachusetts Survey of Secondary Conditions (MSSC) Sample Profile
| Characteristics | Percentage/Mean | No. of Respondents/ Standard Deviation |
|---|---|---|
| Gender [% (n)] | ||
| Women | 58.2 | (382) |
| Race/ethnicity [% (n)] | ||
| White non-Hispanic | 72.7 | (463) |
| Black non-Hispanic | 17.9 | (114) |
| Hispanic | 4.6 | (29) |
| Other | 4.8 | (31) |
| Age [% (n)] | ||
| 18–35 | 29.1 | (187) |
| 36–55 | 51.6 | (332) |
| 56–65 | 13.7 | (88) |
| >65 | 5.6 | (36) |
| Years of formal education [mean (SD)] | 12.8 | (4.11) |
| Live alone [% (n)] | 49.2 | (323) |
| Health insurancea [% (n)] | ||
| Medicare | 51.3 | (320) |
| Medicaid | 78.2 | (485) |
| Enrolled in HMO | 45.8 | (301) |
| Private health insurance | 19.5 | (126) |
| No coverage | <1.0 | (3) |
| Primary disabling condition [% (n)] | ||
| Spinal cord injury | 17.9 | (117) |
| Cardiovascular/pulmonary | 15.6 | (102) |
| Cerebral palsy/spina bifida | 14.2 | (93) |
| Arthritis/orthopedic | 13.3 | (87) |
| Psychological, cognitive, behavioral | 13.0 | (85) |
| Multiple sclerosis | 7.5 | (49) |
| Muscular dystrophy/degenerative | 5.7 | (37) |
| Neurological | ||
| Traumatic brain injury | 2.9 | (19) |
| Other | 9.9 | (65) |
| Disabled from birth [% (n)] | 21.0 | (135) |
| Domains of ADL dependency [mean (SD)] (range 0–9) | 3.2 | (3.1) |
| Domains of IADL difficulty [mean (SD)] (range 0–3) | 1.3 | (1.1) |
| Personal care assistance | ||
| % needing (n) | 68.1 | (453) |
| % authorized (n) | 55.8 | (380) |
| Hours per day authorized [mean (SD)] (range 0–24) | 3.7 | (4.5) |
Individuals can have more than one type of coverage.
Source: MSSC baseline data (1996–98).
The respondents” primary disabling conditions were sorted into nine groups for analysis (see table 1). The most prevalent condition was spinal cord injury (18%), followed by cardiovascular/pulmonary conditions (16%) and cerebral palsy and spina bifida (14%). Psychological, cognitive, and behavioral conditions and arthritis each accounted for 13 percent of the sample.
Almost 21 percent of the respondents had been disabled all their lives, with most (65% of those with lifelong disabilities) having cerebral palsy or spina bifida as their primary disabling condition. More than half (52%) had more than one disabling condition. On average, the respondents required assistance in 3.2 (±3.1) ADLs and reported problems with 1.3 (±1.1) IADLs. While 68 percent reported needing personal assistance services (PAS), only 56 percent received them. Those respondents who received PAS obtained a mean of 3.7 (±4.5) hours per day. More than half the respondents also received some unpaid personal assistance.
Correlates of the Number of Secondary Conditions
On average, the respondents reported 5.3 (±3.1, range 0–15) secondary conditions, with almost 95 percent reporting at least one. The five most common secondary conditions were fatigue, depression, spasms, chronic pain, and anxiety (see table 2). Overall, our analysis of bivariate relationships between secondary conditions and other health-related outcomes indicated that fair/poor health outcomes were associated with a greater number of reported secondary conditions. Fair/poor general health status (p<.01) and somewhat/much worse health now than a year ago (p<.01) were associated with a greater number of secondary conditions. This greater number of secondary conditions was also associated with the number of days a respondent was temporarily unable to carry out routine activities (p<.01) (data not shown).
TABLE 2.
Secondary Conditions and Other Health Outcomes of MSSC Respondents
| Health Outcomes | Percentage/Mean | No. of Respondents/Standard Deviation |
|---|---|---|
| Number of secondary conditions [mean (SD)] | 5.33 | 3.11 |
| Type of secondary condition [% (n)] | ||
| Fatigue | 62.6 | 409 |
| Depression | 50.2 | 328 |
| Spasms | 50.0 | 327 |
| Chronic pain | 48.0 | 314 |
| Anxiety | 45.0 | 295 |
| Bowel problems | 39.2 | 256 |
| UTI | 36.2 | 237 |
| Skin problems | 33.5 | 219 |
| Fall/injury | 32.5 | 212 |
| Migraines | 26.0 | 170 |
| Reactions to medicine | 26.0 | 170 |
| Respiratory infections | 23.0 | 150 |
| Asthma | 20.5 | 134 |
| Contractures | 12.8 | 84 |
| Burns | 12.8 | 84 |
| Autonomic dysreflexia | 9.5 | 62 |
| Seizures | 5.4 | 35 |
| Number of days unable to do routine activities [mean (SD)] | 6.69 | 9.45 |
| Fair/poor health [% (n)] | 45.9 | 300 |
| Somewhat/much worse health now than a year ago [% (n)] | 31.3 | 205 |
Source: MSSC baseline data (1996–98).
The results of hierarchical multiple regression modeling are presented in table 3. The regression indicated that individuals with cerebral palsy or spina bifida and cardiovascular or pulmonary conditions and those whose primary disabling conditions were categorized as “other” experienced fewer secondary conditions than did persons with spinal cord injury (p<.01). Other significant correlates of a greater number of secondary conditions were (1) female gender, (2) more than one major disabling condition, (3) more ADL dependencies, (4) more difficulties with IADLs, (5) unmet need for mobility aids, (6) tobacco use, (7) marijuana use, (8) difficulty maintaining weight, (9) difficulty engaging in physical exercise, and (10) experience of assault (p<.05). Our initial model found no association between enrollment in an HMO and number of secondary conditions. The variable “enrolled in an HMO” was not included in the final model.
TABLE 3.
Hierarchical Multiple Regression Analysis of Number of Secondary Conditions (standardized regression coefficients and incremental r-square)
| Independent Variables | Standardized Regression Coefficients | r2a(%) |
|---|---|---|
| Sociodemographics | 2.6 | |
| Age at interview | −0.01 | |
| Gender (male = 1) | −0.10** | |
| Number of full years of education | 0.01 | |
| Race/ethnicity (nonwhite = 1) | −0.04 | |
| Type of Disability | 9.0 | |
| Primary disabling condition | ||
| Cerebral palsy/spina bifida | −0.17** | |
| Cardiovascular/pulmonary conditions | −0.14** | |
| Other disabling conditions | −0.19** | |
| Spinal cord injury (referent group) | ||
| More than one disabling condition (yes = 1) | 0.16** | |
| Activity Limitation | 13.4 | |
| Number of ADLs for which respondent is dependent | 0.14** | |
| Number of IADLs with which respondent has difficulty | 0.19** | |
| Access | 4.4 | |
| Difficulty transportation to all places (yes = 1) | 0.03 | |
| Number of ADLs with which respondent needs more help | 0.07 | |
| Difficulty getting medical/surgical care (yes = 1) | 0.07 | |
| Fair/poor quality of health care (yes = 1) | −0.03 | |
| Unmet need for mobility aids (yes = 1) | 0.11** | |
| Unmet need for communication aids (yes = 1) | 0.04 | |
| Substance Use | 3.5 | |
| Used tobacco in 4 weeks before interview (yes = 1) | 0.13** | |
| 3 or more drinks on any occasion in 4 weeks before interview (yes = 1) | −0.05 | |
| Used marijuana in 12 months before interview (yes = 1) | 0.08* | |
| Other Health Risks | 4.5 | |
| Difficulty maintaining weight (yes = 1) | 0.14** | |
| Difficulty with physical exercise (yes = 1) | 0.13** | |
| Being assaulted in past year (yes = 1) | 0.07* | |
| Total explained variance (full model r-square) | 37.3 |
Indicates incremental increase in r-square above the r-square for the previous blocks of variables.
p< .05.
p< .01.
Source: Massachusetts Survey of Secondary Conditions among Independently Living Adults with Disabilities.
Serial, adjusted r-square values are presented in table 3 and indicate that sociodemographic factors accounted for <3 percent of the variance in number of secondary conditions. The proportion of explained variance increased 9 percent with the inclusion of type of disability, 13.4 percent with activity limitation, 4.4 percent with access variables, 3.5 percent with substance use, and 4.5 percent with variables in the “other health risks” factor. The total variance explained by the model was 37.3 percent.
We examined the association between number of secondary conditions and other health outcomes to emphasize the impact of secondary conditions on self-reported health. A greater number of secondary conditions was associated with a higher risk of fair/poor health (OR (odds ratio) = 1.21, 95% CI (confidence interval) = 1.14–1.28) and somewhat/much worse health now versus a year ago (OR = 1.19, 95% CI = .13=1.26) and a greater number of days unable to do routine activities (slope = 0.98, 95% CI = 0.76=1.21). Controlling for sociodemographics, type and level of disability, and mediating factors, fair/poor health (adjusted OR = 1.19, 95% CI = 1.09/1.29) and number of days unable to do routine activities (adjusted slope = 0.41, 95% CI = 0.13–0.69) remained significantly associated with a greater number of secondary conditions. A respondent in the upper quartile (7) for number of secondary conditions was twice as likely to report fair/poor health compared with a respondent in the lower quartile (3). However, the association between number of secondary conditions and self-reported change in health was no longer significant (adjusted OR = 1.06, 95% CI = 0.98–1.15). (Data from regressions are available on request.)
The results of logistic regression modeling of the paralysis/mobility-related and the mental health/chronic pain groups of secondary conditions are presented in table 4. The Hosmer-Lemenshow statistic given in the table supports the appropriateness of each of the models. In the model for paralysis/mobility-related secondary conditions, those reporting cerebral palsy/spina bifida (OR = 0.15), cardiovascular/pulmonary (OR = 0.09), and other conditions (OR = 0.08) as their primary disabling condition (compared with those with a spinal cord injury) were less likely to report paralysis/mobility-related secondary conditions. In addition, age (OR = 0.97) and ADL dependency (OR = 1.24) were associated with paralysis/mobility-related secondary conditions.
TABLE 4.
Multiple Logistic Regression Model for Mental Health/Chronic Pain and Paralysis/Mobility-Related Secondary Conditions ( n= 656)a
| Mental Health/Chronic Painb | Paralysis/Mobilityc | |||
|---|---|---|---|---|
| Independent Variables | OR | 95% CI | OR | 95% CI |
| Sociodemographics | ||||
| Age at interviewd | 1.04 | (1.01–1.06) | 0.97 | (0.96–0.99) |
| Gender (male = 1) | 0.60 | (0.34–1.06) | 0.73 | (0.47–1.14) |
| Number of full years of educationd | 1.08 | (1.00–1.16) | 1.00 | (0.94–1.05) |
| Race/ethnicity (nonwhite = 1) | 0.81 | (0.42–1.56) | 0.85 | (0.53–1.36) |
| Type of Disability | ||||
| Primary disabling condition | ||||
| Cerebral palsy/spina bifida | 0.96 | (0.40–2.33) | 0.15 | (0.05–0.47) |
| Cardiovascular/Pulmonary conditions | 0.54 | (0.20–1.49) | 0.09 | (0.03–0.28) |
| Other disabling conditions | 1.13 | (0.49–2.56) | 0.08 | (0.03–0.24) |
| Spinal cord injury (referent group) | 1.00 | 1.00 | ||
| More than one disabling condition (yes = 1) | 1.81 | (1.01–3.22) | 1.34 | (0.88–2.04) |
| Activity Limitation | ||||
| Number of ADLs for which respondent is dependentd | 1.01 | (0.90–1.13) | 1.24 | (1.13–1.36) |
| Number of IADLs with which respondent has difficultyd | 1.64 | (1.24–2.18) | 1.17 | (0.95–1.42) |
| Access | ||||
| Difficulty transportation of all places (yes = 1) | 1.13 | (0.57–2.21) | 1.06 | (0.68–1.66) |
| Number of ADLs with which respondent needs more help d | 1.07 | (0.84–1.36) | 0.98 | (0.82–1.16) |
| Difficulty getting medical/ surgical care (yes = 1) | 1.67 | (0.78–3.63) | 1.39 | (0.88–2.34) |
| Fair/poor quality of health care (yes = 1) | 0.65 | (0.27–1.57) | 0.91 | (0.50–1.64) |
| Unmet need for mobility aids (yes = 1) | 4.32 | (1.56–12.05) | 1.48 | (0.83–2.64) |
| Unmet need for communication aids (yes = 1) | 1.65 | (0.51–5.30) | 1.25 | (0.58–2.71) |
| Substance Use | ||||
| Used tobacco in 4 weeks before interview (yes = 1) | 5.42 | (2.46–11.96) | 1.52 | (0.96–2.40) |
| >3 drinks on any one occasion in 4 weeks before interview (yes = 1) | 1.04 | (0.47–2.31) | 0.79 | (0.44–1.44) |
| Used marijuana in 12 months before interview (yes = 1) | 2.14 | (0.77–5.96) | 1.46 | (0.74–2.88) |
| Other Health Risks | ||||
| Difficulty maintaining proper weight: (yes = 1) | 2.07 | (1.14–3.77) | 1.40 | (0.89–2.18) |
| Difficulty physical exercise (yes = 1) | 4.03 | (2.02–8.06) | 1.37 | (0.88–2.14) |
| Being assaulted in past year (yes = 1) | 2.22 | (0.52–9.48) | 0.67 | (0.31–1.45) |
n= 538 with for people with mental health/chronic pain secondary conditions andn= 443 for people with paralysis/mobility secondary conditions.
The Hosmer and Lemenshow statistic = 3.95 with 8 degrees of freedom;p = .86.
The Hosmer and Lemenshow statistic = 9.36 with 8 degrees of freedom;p = .31.
Odds ratio described increased odds of particular type of secondary condition for one unit increase in predictor.
In the model for mental health/chronic pain secondary conditions, age (OR = 1.04), years of formal education (OR = 1.08), difficulties with IADLs (OR = 1.64), more than one primary disabling condition (OR = 1.81), need for mobility aids (OR = 4.32), tobacco use (OR = 5.42), difficulty maintaining weight (OR = 2.07), and difficulty engaging in physical exercise (OR = 4.03) were positively associated with reporting mental health/chronic pain secondary conditions.
Discussion
Our study found a high prevalence of secondary conditions—particularly fatigue, depression, spasms, and chronic pain—in a group of independently living Massachusetts adults with major disabilities. Access, substance use, and other health risks factors explained one-third of the 37 percent of variance in number of secondary conditions explained by our hierarchical regression model. The specific variables related to a greater number of secondary conditions were more than one disabling condition, number of ADL dependencies, number of IADL difficulties, difficulty maintaining weight and exercising, tobacco and marijuana use, and an experience with assault. Being male and having a primary disabling condition other than a spinal cord injury were associated with having fewer secondary conditions. The importance of the number of secondary conditions was demonstrated by its association with fair/poor self-reported health status and number of days unable to do routine activities. Correlates were also identified for two subsets of secondary conditions, paralysis/mobility-related secondary conditions and mental health/chronic pain secondary conditions.
Before discussing these findings, we should point out the study's limitations. Our sample was of adults identified by independent living centers and selected health maintenance organizations whose experiences may not be representative of Massachusetts residents with disabilities. Although the sample was diverse, persons with severe physical limitations were overrepresented, and persons with sensory or cognitive limitations were underrepresented, in part owing to the survey's methodology, including its lack of provision for proxy interviews. Although the diversity of the sample was helpful for understanding cross-disability issues, it made it difficult to analyze specific pathways for the development of secondary conditions within a heterogeneous sample of this size. Research with a more representative group of people with disabilities is needed.
The investigators chose to cover a range of topics in the survey and to use self-report as the primary source of data. Even though these are strengths of the study, permitting a broad understanding of the experience of persons with disabilities, they also are limitations. The range of topics meant that some could not be fully explored. In fact, some topics, such as individuals” coping styles, were excluded in order to limit the length of the survey. Several studies have found the reliability of self-reported health and disability data to be tenuous because of inaccuracies resulting from memory loss and overreporting and underreporting biases (Degnan, Harris, Ranney, et al. 1992;Kelly-Hayes, Jette, Wolf, et al. 1992;Zapka, Bigelow, and Hurley 1996).
Our framework implied some associations that could not be tested because of the small numbers in relevant cells, collinearity, unstable estimates, insufficient variation in responses, and other methodological issues. Even though mental health/chronic pain and paralysis/mobility-related secondary conditions were prevalent in our sample, the estimated odds ratios for these outcomes should not be interpreted as relative risks. In addition, since the data were cross-sectional, causality could not be inferred. Longitudinal analysis may permit some causal inferences.
Similar multivariate analyses between predictor variables and individual secondary conditions should be conducted. Future analyses will examine relationships between specific sets of risk factors and the most prevalent individual secondary conditions, as well as the severity of these conditions.
Another limitation of the baseline results, given that they were cross-sectional, is that we cannot truly know whether some of the health problems we called secondary conditions actually occurred after the disabling conditions. Rather, we used the term secondary conditions because of its currency in the field and the need to refine its research usage. Nevertheless, in the baseline results these conditions might technically be better termed other health problems. The term associated conditions is another option, but Lollar (1999) used this to refer to comorbid or disabling conditions other than the primary condition.
Despite its limitations, this baseline study of the correlates of number of secondary conditions is important both as a guide to future research and for the development of policies and interventions for adults with disabilities. We used an explicit conceptual framework as the basis for including particular variables, and we tested the associations among elements of the framework for which sufficient data were available.
Disability researchers are currently debating the extent to which secondary conditions are predicted by specific diagnoses or impairments versus attributes that cut across disabilities, such as activity limitations. In this sample of persons with diverse diagnoses and impairments, ADLs and IADLs explained the largest percentage of the variance in number of secondary conditions. The more activities (ADLs or IADLs) in which a person was dependent or had difficulty, the greater the number of secondary conditions that he or she reported.
The association between ADLs and IADLs and secondary conditions supports the need for attention to and further evaluation of interventions that reduce difficulties with ADLs and IADLs even while we await longitudinal analysis to better tease out causal directions. Intervention to increase independence in activities of ordinary living (such as personal assistance, assistive technology, and other environmental modifications) may also help prevent secondary conditions. At the very least, such interventions seem likely to reduce the stress and fatigue that can undermine an individual's ability to function, regardless of disability.
Our factor analysis suggested one set of secondary conditions that we called paralysis/mobility-related. In our sample, these conditions were most common in persons with SCI. The negative association found between age and paralysis/mobility-related secondary conditions may mean that this cluster of secondary conditions is most likely to arise secondary to earlier-onset primary disabling conditions such as SCI and CP, compared with arthritis and cardiovascular disease.
The MSSC did not collect information about the type and degree of impairment of body structure and function. In our sample, those respondents with cerebral palsy, spina bifida, and other congenital conditions may have more diverse impairments of body structure and function than do respondents with a spinal cord injury, because our SCI sample had predominantly cervical-level injuries. Regardless, it may be important to target interventions for persons with spinal cord injury. Of course, the greater number of secondary conditions related to spinal cord injury could be an artifact of the particular conditions we studied or the way we categorized disabilities. This is an important issue for researchers in this field, as we show next.
In contrast to the paralysis/mobility-related conditions, we named the mental health/chronic pain factor for the type of secondary conditions to which it referred, rather than for the underlying impairments or disabilities. Unlike paralysis/mobility-related conditions, the distribution of the second set of conditions was not skewed toward any particular primary disabling conditions but was common across all disabilities. Ravesloot, Seekins, and Walsh (1997) also found substantial commonality in secondary conditions across disabling conditions. Mental health/chronic pain conditions were, however, more likely to be found in older respondents. These secondary conditions were also associated with several factors often targeted for public health interventions, such as having an unmet need for mobility aids, difficulty engaging in physical exercise and maintaining weight, and using tobacco. Since causality cannot be determined, it is possible that those respondents with mental health/chronic pain secondary conditions are more likely to engage in unhealthy behaviors such as physical inactivity, smoking, and inadequate weight maintenance. It also is possible that an unmet need for mobility aids or the presence of unhealthy behaviors increases the occurrence of these secondary conditions.
Research, Policy, and Program Considerations
Disability research and public health interventions to prevent secondary conditions are now active areas of public health endeavor (Hough 1999;Simeonsson et al. 1999). For this reason, we believe that improving our conceptual framework merits as much attention as does assessing the results of individual studies. A consistent conceptual framework serves as a guide for hypotheses connecting biological, social, and environmental factors to health outcomes among adults with disabilities. Conceptual models may influence program planning both directly and through research. For research purposes, more elements should be added to the framework to explore correlates and causes of secondary conditions, and the elements should be defined more consistently. The International Classification of Functioning, Disability, and Health (ICF), adopted unanimously by the World Health Assembly, is a health or health-related classification that incorporates the social and environmental aspects of disability and health (World Health Organization 2001). The ICF provides a list of environmental factors that influence individual activity and participation levels, some of which should be included in an enhanced conceptual framework. In regard to national policy, the first objective in the chapter “Disability and Secondary Conditions” of Healthy People 2010 is to create “a standardized set of questions that identify `people with disabilities”” (U.S. Dept. of Health and Human Services 2000). The MSSC recommends including measures of activity limitations in the standard set of questions or adding them when feasible.
For state public health departments, the finding that many secondary conditions cut across diagnoses often regarded as indicating a disability suggests that health promotion programs can be targeted to individuals across diagnostic or impairment groups. Along with disability-focused programs, reducing environmental barriers to participation and accommodating persons with disabilities in the broader range of public health programs are crucial. People with disabilities need access to all public health services. Screening for STDs; breast, cervical, and colorectal cancer; and osteoporosis are examples. Particularly in relation to this study, the significance of a number of variables—such as smoking, difficulty maintaining weight, and experiencing an assault—as correlates of secondary conditions supports a policy of “including” persons with disabilities in existing health promotion efforts and/or campaigns targeted to persons with disabilities. Programs targeted to persons with disabilities should be both general and specialized. Funding policies that limit services to certain diagnostic groups may unnecessarily restrict the cost effectiveness of those resources. At the same time, however, to prevent certain types of secondary conditions, such as those we grouped as paralysis/mobility-related conditions, targeting may be effective. Further discussion and research are needed to determine when programs should be targeted. The inclusion of persons with disabilities in both research and planning interventions as not only participants but also researchers, planners, and leaders is essential to developing the “consumer”-focused systems valued in public health (Anderson and Bryant 1999).
Finally, this article brings a discrepancy to the attention of policymakers and program developers in public health, the medical community, and other human service systems. Fewer than 15 percent of our survey's respondents reported their health care to be of fair or poor quality, and fewer than 1 percent of the MSSC respondents did not have health insurance. Even so, 26 percent reported difficulty with access to care, and many respondents cited poor health outcomes, including a high prevalence of theoretically preventable secondary conditions and fair/poor general health and number of days unable to do routine activities. This suggests a gap in health care or other delivery systems. To some extent, this gap might be addressed by introducing people with disabilities to health promotion activities. But the discrepancy between perceived quality and access to care and poor outcomes indicates a need for something more. In some instances, broadening the definition of what is considered to be “medically necessary,” and therefore reimbursable by insurance, may be appropriate. Or the discrepancy between expressed satisfaction and outcomes may reflect consumer expectations that are unnecessarily low, ambivalent, or confused about the health care system and what can or should be expected of it. Low expectations may be an accommodation to past experience. Ambivalence and confusion may reflect the fact that self-advocacy for health care can be difficult, given the energy and information required and the fact that some persons with disabilities may be disenchanted with the medical community (DeJong 1979, 1993). A comprehensive, flexible case management system that goes beyond a medical or employment-related model may be one way of bridging the gap between expectations and outcome. Such systems have long been a feature of state public health programs for children with special health care needs (American Academy of Pediatrics 1999). Case managers linked to or based in the health care system could help clients obtain health and related services and resources as well as learn to advocate within the system for themselves.
Historically, the relationship of public health and disability has been ambiguous. Too often, disability has been seen as a static condition reflecting a failure of public health intervention. Increasingly, however, disability is recognized as a dynamic attribute, amenable to public health intervention. That is one of our study's central findings, that disability is a public health issue and requires public health action. First, existing primary and secondary population-based public health prevention efforts must include people with disabilities. Second, specialized programs must address the unique needs of people with disabilities. Given the prevalence of secondary conditions that we found, the stakes for human well-being and health care costs are likely to be substantial.
Acknowledgments
This article was supported in part by a Cooperative Agreement (#U59/CCU103370) with the Disability and Health Branch, U.S. Centers for Disease Control and Prevention, and grants from the National Institute on Disability and Rehabilitation Research (NIDRR), Office of Special Education and Rehabilitative Services, U.S. Department of Education, Washington, D.C. (grants number H133660037, for Field-Initiated Research, and H133N50014, for Boston Medical Center's New England Regional Spinal Cord Injury Center, a National Model Spinal Cord Injury Center). The opinions expressed in this article are the authors” only and do not necessarily reflect the official positions of the funding agencies, Massachusetts Department of Public Health, Boston University, or Boston Medical Center. The authors wish to thank Laura Rauscher, the first director of the Office on Health and Disability of the Massachusetts Department of Public Health (MDPH), for her invaluable contribution in the development of the theoretical framework and study design. We also want to thank Professor Tim Heeren of Boston University School of Public Health and anonymous readers at MDPH for their careful reviews of the manuscript.
References
- American Academy of Pediatrics, Committee on Children with Disabilities. Care Coordination: Integrating Health and Related Systems of Care for Children with Special Health Care Needs. Pediatrics. 1999;104(4):978–81. [PubMed] [Google Scholar]
- Anderson RJ, Bryant KB. Disability and Quality of Life: A Personal Perspective. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 1–14. [Google Scholar]
- Andresen EM, Lollar DJ, Meyers AR. Disability Outcomes Research: Why This Supplement on This Topic, at This Time? Archives of Physical Medicine and Rehabilitation. 2000;81(12):S1–S4. doi: 10.1053/apmr.2000.20614. [DOI] [PubMed] [Google Scholar]
- Degnan D, Harris R, Ranney J, Quade D, Earp JA, Gonzalez J. Measuring the Use of Mammography: Two Methods Compared. American Journal of Public Health. 1992;82:1386–8. doi: 10.2105/ajph.82.10.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeJong G. Independent Living: From Social Movement to Analytic Paradigm. Archives of Physical Medicine and Rehabilitation. 1979;60:435–46. [PubMed] [Google Scholar]
- DeJong G. Health Care Reform and Disability: Affirming Our Commitment to Community. Archives of Physical Medicine and Rehabilitation. 1993;74:1017–23. doi: 10.1016/0003-9993(93)90055-f. [DOI] [PubMed] [Google Scholar]
- Glover M, Master RJ, Meyers AM. Boston's Community Medical Group (BCMG): A National Model of Prepaid, Managed Care for Independently-Living Persons with Spinal Cord Injuries. American Rehabilitation. 1996;22:2–9. [Google Scholar]
- Hough J. Disability and Health: A National Public Health Agenda. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 161–203. [Google Scholar]
- Institute of Medicine. The Future of Public Health. Washington, D.C.: National Academy Press; 1988. [Google Scholar]
- Institute of Medicine. Disability in America: Toward a National Agenda for Prevention. Washington, D.C.: National Academy Press; 1991. [Google Scholar]
- Institute of Medicine. Improving Health in the Community: A Role for Performance Monitoring. Washington, D.C.: National Academy Press; 1997. [PubMed] [Google Scholar]
- Katz S. Assessing Self-Maintenance: Activities of Daily Living, Mobility, and Instrumental Activities of Daily Living. Journal of the American Geriatrics Society. 1983;31:721–7. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- Kelly-Hayes M, Jette AM, Wolf PA, D'Agostino RB, Odell PM. Functional Limitations and Disability among Elders in the Framingham Study. American Journal of Public Health. 1992;86:1016–21. doi: 10.2105/ajph.82.6.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause JS, Bell RB. Measuring Quality of Life and Secondary Conditions: Experiences with Spinal Cord Injury. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 129–43. [Google Scholar]
- Lollar DJ. Encouraging Personal and Interpersonal Independence. In: Lollar DJ, editor. Preventing Secondary Conditions Associated with Spina Bifida or Cerebral Palsy: Proceedings and Recommendations of a Symposium. Atlanta: Centers for Disease Control and Prevention; 1994. pp. 17–25. [Google Scholar]
- Lollar DJ. Clinical Dimensions of Secondary Conditions. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 41–50. [Google Scholar]
- Marge M. Health Promotion for Persons with Disabilities: Moving beyond Rehabilitation. American Journal of Health Promotion. 1988;2(4):29–44. doi: 10.4278/0890-1171-2.4.29. [DOI] [PubMed] [Google Scholar]
- Marge M. Defining a Prevention Agenda for Secondary Conditions. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 15–40. [Google Scholar]
- Master RJ, Dreyfus T, Connors S, Tobias C, Zhou Z, Kronick R. The Community Medical Alliance: An Integrated System of Care in Greater Boston for People with Severe Disability and AIDS. Managed Care Quarterly. 1996;4:26–37. [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Jr, Rogers W, Raczek AE, Lu JF. The Validity and Relative Precision of MOS Short- and Long-Form Health Status Scales and Dartmouth COOP Charts. Results from the Medical Outcomes Study. Medical Care. 1992;30(5; suppl.):MS253–65. doi: 10.1097/00005650-199205001-00025. [DOI] [PubMed] [Google Scholar]
- McMillen JS, Simeonsson RJ, McDevitt L. Preventing Secondary Conditions and Promoting Health, Well Being and Quality of Life. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 205–20. [Google Scholar]
- Meyers AR, Cupples A, Lederman RI, et al. The Epidemiology of Medical Care Utilization by Severely-Disabled Independently-Living Adults. Journal of Clinical Epidemiology. 1988;41(2):163–72. doi: 10.1016/0895-4356(88)90090-x. [DOI] [PubMed] [Google Scholar]
- Nagi SZ. Some Conceptual Issues in Disability and Rehabilitation. In: Sussman MB, editor. Sociology and Rehabilitation. Washington, D.C.: American Sociological Association; 1965. pp. 100–13. [Google Scholar]
- Nagi SZ. Disability and Rehabilitation: Legal, Clinical, and Self-Concepts and Measurements. Columbus: Ohio State University Press; 1969. [Google Scholar]
- Pope AM. Preventing Secondary Conditions. Mental Retardation. 1992;30(6):347–54. [PubMed] [Google Scholar]
- Ravesloot C, Seekins T, Walsh J. A Structural Analysis of Secondary Conditions Experienced by People with Physical Disabilities. Rehabilitation Psychology. 1997;42(1):3–16. [Google Scholar]
- Rimmer JH. Health Promotion for People with Disabilities: The Emerging Paradigm Shift from Disability Prevention to Prevention of Secondary Conditions. Physical Therapy. 1999;79(5):495–502. [PubMed] [Google Scholar]
- Seekins T, Clay J, Ravesloot CH. A Descriptive Study of Secondary Conditions Reported by a Population of Adults with Physical Disabilities Served by 3 Independent Living Centers in a Rural State. Journal of Rehabilitation. 1994:47–51. April, [Google Scholar]
- Seekins T, Smith N, McLeary T, Clay J, Walsh J. Secondary Disability Prevention: Involving Consumers in the Development of a Public Health Surveillance Instrument. Journal of Disability Policy Studies. 1990;1(3):21–36. [Google Scholar]
- Seekins T, White GW, Ravesloot C, et al. Developing and Evaluating Community-Based Health Promotion Programs for People with Disabilities. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 221–38. [Google Scholar]
- Simeonsson RJ, Bailey DB, Scandlin D, Huntington GS, Roth M. Disability, Health, Secondary Conditions and Quality of Life: Emerging Issues in Public Health. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 239–55. [Google Scholar]
- Simeonsson RJ, Leskinen M. Disability, Secondary Conditions and Quality of Life: Conceptual Issues. In: Simeonsson RJ, McDevitt LN, editors. Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. pp. 51–72. [Google Scholar]
- Issues in Disability and Health: The Role of Secondary Conditions and Quality of Life. Chapel Hill: University of North Carolina Press; 1999. [Google Scholar]
- Stewart A. The Medical Outcomes Study Framework of Health Indicators. In: Stewart A, Ware J, editors. Measuring Functioning and Well-Being. Durham, N.C.: Duke University Press; 1992. pp. 12–24. [Google Scholar]
- Tabachnick B, Fidell LS. Using Multivariate Statistics. New York: Harper & Row; 1983. [Google Scholar]
- Tanenhaus RH, Meyers AR, Harbison LA. Disability and the Graduate Curriculum in the United States” Graduate Schools of Public Health (Research Letter) American Journal of Public Health. 2000;90(8):1315–6. doi: 10.2105/ajph.90.8.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk MA. Secondary Conditions—Issues in Definition and Measurement. Paper presented at the conference Promoting the Health and Wellness of Women with Disabilities; San Antonio, Tex.. Centers for Disease Control and Prevention; [Google Scholar]
- Turk MA, Geremski CA, Rosenbaum P F. The Health Status of Women with Cerebral Palsy. Archives of Physical Medicine and Rehabilitation. 1997;78(suppl.):S10–S17. doi: 10.1016/s0003-9993(97)90216-1. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010. Washington, D.C: 2000. Disability and Secondary Conditions. Chap. 6, [Google Scholar]
- Verbrugge LM, Jette AM. The Disablement Process. Social Science Medicine. 1994;38(1):1–13. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Ware J. Measures for a New Era of Health Assessment. In: Stewart A, Ware J, editors. Measuring Functioning and Well-Being. Durham, N.C.: Duke University Press; 1992. pp. 3–11. [Google Scholar]
- Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. Quantifying Handicap: A New Measure of Long-Term Rehabilitation Outcomes. Archives in Physical and Medical Rehabilitation. 1992;73:519–26. [PubMed] [Google Scholar]
- World Health Organization. ICF International Classification of Functioning Disability and Health. Geneva: 2001. [PubMed] [Google Scholar]
- Zapka JG, Bigelow C, Hurley T. Mammography Use among Sociodemographically Diverse Women: The Accuracy of Self-Report. American Journal of Public Health. 1996;85:566–70. doi: 10.2105/ajph.86.7.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]


