As a social construct, race has been and remains a powerful organizing feature of American social life. Racial categories both reflect and reinforce group differences in access to economic, political, and social resources. In the United States, racial ideologies operate politically, legally, and socially to limit African Americans’ and other labeled racial groups’ access to economic resources (Darden 1986; Farley et al. 1994; Hummer 1996; Krieger 1999; LaVeist 1992; Massey and Denton 1993; Williams 1996, 1999). For example, institutional or structural forms of systematic discrimination can limit educational, employment, and housing opportunities.
In this article, we suggest that efforts to reduce or eliminate well-established racial disparities in health must consider the complex relationships between race and socioeconomic status, including the political, social, and economic processes that create and maintain racial differences in access to social and economic resources. We present evidence that race-based residential segregation is a fundamental cause of racial disparities in health, one that (1) influences access, at both the individual and residential-area levels, to social and material resources that promote health and avoid disease; and (2) influences many health outcomes (Cassel 1976; House et al. 1990; Link and Phelan 1995; Williams and Collins 2001). Our conceptual framework draws on previously published literature from the Detroit metropolitan area to examine relationships among race-based residential segregation, socioeconomic status, and health. Race-based residential segregation as a fundamental determinant of health has been found to disproportionately expose African Americans to the effects of concentrated poverty. We discuss the intermediate (e.g., social and physical environments) and proximate (e.g., social networks, social support, health-related behaviors) pathways through which race-based residential segregation and concentrations of poverty influence health outcomes. Our intent is to bring together research on race-based residential segregation and economic systems in urban neighborhoods with epidemiological research on health disparities to create a conceptual framework to generate research hypotheses that can be tested empirically.
Racial Disparities in Health
African Americans in the United States have significantly higher risks of morbidity and mortality than the national average (Hummer 1996; Kington and Nickens 2001; Krieger et al. 1993; McLeod and Lozoff 2001; NCHS 2000; Williams 2001; Williams and Collins 1995). Racial disparities in morbidity and mortality are found across age groups, in both urban and rural areas, and for various causes of disease (Geronimus, Bound, and Waidmann 1999; House and Williams 2000; Lillie-Blanton et al. 1996; Williams 1999). In both 1950 and 1998, the age-adjusted, all-cause mortality rate for African Americans nationally was 1.5 times higher than that for whites (NCHS 2000), with the mortality rate for blacks increasing for coronary heart disease, cancer, diabetes, and infant mortality (NCHS 2000; Williams 1999). Although all urban residents have a significantly higher risk of mortality compared with that of the population as a whole, African Americans have higher mortality rates than do whites living in the same city (Freudenberg 1998; Geronimus, Bound, and Waidmann 1999; Geronimus et al. 1996; House et al. 2000). These differences have persisted and, in some cases, widened despite the declining mortality rates for many causes of death for the population as a whole (House and Williams 2000). Reducing racial disparities in health thus offers an opportunity to improve the health of the U.S. population as a whole.
A large body of research suggests that to lower morbidity and mortality rates, we must first identify the fundamental causes of disease, that is, those that involve access to the resources necessary to maintain health and avoid disease (House et al. 1990; Link and Phelan 1995; Navarro 2002). Socioeconomic status is one such fundamental cause of disease (Antonovsky 1967; House et al. 1994; Kaplan and Lynch 1999; Link and Phelan 1995), and differences in socioeconomic status clearly contribute to the persistent racial disparities in health (Navarro 1989; Sorlie, Rogot, and Anderson 1992; Williams 1999). This research indicates that addressing socioeconomic inequalities among racial groups in the United States would go a long way toward addressing racial disparities in health.
Relationships between race and socioeconomic status are complex and occur within the context of political, economic, and social systems whose influence extends beyond their effects on individual socioeconomic status (Cooper and David 1986; House et al. 1994; House and Williams 2000; Krieger et al. 1993; Lillie-Blanton et al. 1996; Williams 1996). For African Americans, these relationships include more day-to-day encounters with interpersonal discrimination than whites have, regardless of social class (Feagin 2000). Such encounters are significantly associated with health outcomes (Noh et al. 1999; Ren, Amick, and Williams 1999). Furthermore, African Americans at all socioeconomic levels live in neighborhoods that are inferior to those of whites (Sampson and Wilson 1995; Wilson 1987), residential environments that may well be injurious to good health (Cohen and Northridge 2000; Collins and Williams 1999; Cooper and David 1986; Geronimus 2000; Krieger et al. 1993; LaVeist 1989; Polednak 1991, 1993; Williams and Collins 2001; Williams et al. 1997).
Between 1950 and the present, the political, social, and economic conditions of many metropolitan areas helped cluster African Americans into older urban areas with high concentrations of poverty (Jargowsky 1997; Massey and Denton 1993). These areas are often surrounded by newer suburban areas whose residents have more privileged racial and class statuses (Garreau 1991; Harris 1999; Jargowsky 1997). Residence in areas characterized by high concentrations of poverty and economic underdevelopment has been connected with higher rates of all-cause mortality (Anderson et al. 1997; Collins and Williams 1999; Geronimus, Bound, and Waidmann 1999; Geronimus et al. 1996), cardiovascular disease (Diez-Roux et al. 2001; Haan, Kaplan, and Camacho 1987; James 1999; Pickett and Pearl 2001), infant mortality and low birth weight (LaVeist 1989; O’Campo et al. 1997; Roberts 1997), and poorer mental health (Aneshensal and Sucoff 1996; Fitzpatrick, LaGory, and Ritchey 1999). Other research indicates that the effects of place of residence on health operate independently of indicators of individual socioeconomic status such as household income and education (Pickett and Pearl 2001; Williams and Collins 2001).
Together, these two bodies of research have established that both low individual socioeconomic status and residence in areas of concentrated poverty are related to poorer health. These findings prompt a series of questions about the relationships among race, individual and neighborhood socioeconomic status, and health. For example, how are the relationships between race and socioeconomic status sustained over time? How does residence in areas of concentrated poverty contribute to racial disparities in health? Perhaps most important, what are potential points of intervention to reduce racial disparities in health? Researchers are now moving beyond descriptive relationships among race, socioeconomic status, and health and toward an understanding of the underlying causes and how they operate. Conceptual frameworks describing potential relationships can provide a foundation for generating specific research hypotheses and effective intervention strategies. Accordingly, we propose a conceptual framework for examining race-based residential segregation as a spatial manifestation of macrolevel social processes and racial ideologies, that keeps many African Americans from resources necessary to maintain health.
As one of the country's most racially segregated metropolitan areas, Detroit offers an opportunity to examine the relationship between race-based residential segregation and socioeconomic status and their combined effects on the city's social and physical environments. African American residents in the Detroit metropolitan area have a disproportionately higher risk of mortality compared with that of either white residents of the metropolitan area or whites nationally (Geronimus, Bound, and Waidmann 1999; Geronimus et al. 1996). Table 1 illustrates the racial disparities in infant mortality and age-adjusted all-causes mortality for African American and white residents of the city of Detroit, Wayne County, and Oakland County. Research conducted in the Detroit metropolitan area indicates that racial disparities in self-reported health status remain after controlling for household income (Schulz, Israel, et al. 2000). The results from the Detroit area are consistent with national data indicating that racial disparities in health are reduced but not eliminated even when accounting for household income and individual education and that African Americans report poorer general health status than do whites at all levels of income (NCHS 2000).
TABLE 1.
Infant Mortality Rates and Age-Adjusted Mortality Rates for African American and White Residents of Detroit, Wayne County, and Oakland County, 1998–2000
| Detroit | Wayne County | Oakland County | |
|---|---|---|---|
| Infant Mortality, Three-Year | |||
| Moving Average: | |||
| 1998–2000 | |||
| Black | 16.7 ± 1.3 | 16.7 ± 5.3 | 23.3 ± 4.1 |
| White | 6.3 ± 1.7 | 5.6 ± 0.7 | 4.2 ± 0.6 |
| Age-Adjusted Mortality | |||
| Rates, 2000 | |||
| Black | 1,184.0 | 1,180.4 | 1,122.9 |
| White | 904.4 | 866.6 | 801.7 |
Note: The city of Detroit is located in Wayne County. Oakland County is part of the Detroit metropolitan area and lies immediately north of the city of Detroit.
Source: Michigan Department of Community Health, July 8, 2002. http://www.mdch.state.mi/us/PHA/OSR/chi/Deaths/frame.html
Fundamental Causes of Racial Disparities in Health: Racial Segregation and Poverty in Detroit
Macrosocial processes (e.g., legal, political, and economic systems) work with racial ideologies to shape the spatial distribution of racial groups and the distribution of resources among them (shown on the far-left side of figure 1). A disproportionate number of African Americans in the Detroit metropolitan area—as do many African Americans nationally—live in communities in which they are isolated from economic resources, institutions that support community life, and opportunity structures (Massey and Denton 1993; Massey and Fischer 2000; Sugrue 1996; Thomas 1997; Wacquant and Wilson 1989).
fig. 1.
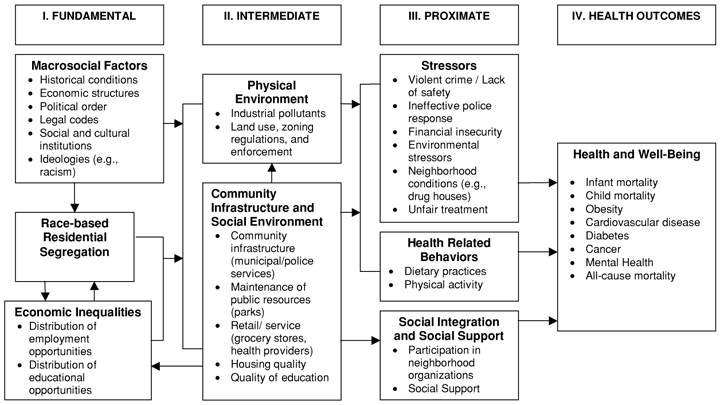
Racial segregation as a fundamental determinant of racial disparities in health.
Over the past 50 years, the Detroit metropolitan area has followed a pattern of change in which the city and its suburbs have become increasingly stratified by race and income. In the 1950s, the city's population reached its peak of 1.8 million, 16.2 percent of whom were African Americans. Since that time, expanding highway systems and the availability of cheap land outside the city led many employers to relocate to outlying suburban areas, with racially selective migrations to these newly developing areas (Garreau 1991; Sugrue 1996). By 2000, Detroit had fewer than a million residents, 82 percent of whom were identified as African American (U.S. Bureau of the Census 2000). As shown in Table 2, the dissimilarity indexes (an indicator of segregation) for the Detroit metropolitan area and for the city of Detroit have remained consistently above 84 and 72 percent, respectively. An index of dissimilarity of 0.87 means that 87 percent of African American residents would have to move in order to achieve an equal distribution of African Americans in the area. An index of dissimilarity above 0.60 is generally thought to represent very high segregation (Williams and Collins 2001).
TABLE 2.
Dissimilarity Index for the Detroit Metropolitan Area and Detroit City, 1980, 1990, and 2000
| Detroit Metropolitan Area | Detroit City | |
|---|---|---|
| 1980 | 87.5 | 72.0 |
| 1990 | 87.5 | 72.7 |
| 2000 | 84.7 | 72.8 |
Note: An index of dissimilarity is an indicator of segregation. An index of dissimilarity of 0.87 means that 87 percent of African American residents would have to move to achieve equal distribution of African Americans in the area.
Source: Lewis Mumford Center 2002.
A number of factors contributed to increasing inequalities in the economic resources available to those who remained in the city and those available to suburban residents, and to the concentration of African Americans in those areas of the city with the fewest economic resources. Immediately following World War II, the number of jobs in the city far exceeded that in the outlying suburban areas (Farley, Danziger, and Holzer 2000). However, between 1960 and 1990, the number of jobs in outlying suburban areas grew while the number of jobs in the city of Detroit fell by an estimated 350,000, from 700,000 in 1960 to roughly 350,000 in 1990 (Darden et al. 1987; Farley, Danziger, and Holzer 2000). In 1995, Detroit had 55 jobs for every 100 persons, compared with Bloomfield Hills, a wealthy outlying suburb, with 272.7 jobs per 100 residents (up from 186.6 jobs per 100 residents in 1985) (Maines and McMillan 2001). Furthermore, as the high-paying blue-collar jobs that had provided a middle-class income for many moved out of the city, the employment opportunities that remained behind became more and more divided between low-paying positions and white-collar jobs (Darden 1986; Farley, Danziger, and Holzer 2000). Industrial workers were increasingly unable to find positions in the city that offered secure middle-class wages, and so many left to find employment in the edge cities or suburban areas. Those who remained in the city had fewer employment opportunities and lower-paying jobs (Zax and Cain 1996).
Thomas (1997) documented the racially selective manner of these shifts in employment opportunities. As Detroit's employers moved to the suburbs, a greater proportion of white than African American employees kept their jobs. The older factories that stayed behind in Detroit's increasingly African American neighborhoods were less technologically sophisticated than the newer plants in suburban areas. Consequently, workers were exposed to more physical hazards and poorer working conditions in general (Hill 1980) as well as a greater risk of unemployment as the older plants were phased out. Cole and Deskins (1988) demonstrated that some employers explicitly factored in the racial composition of various areas when deciding where to locate new facilities, avoiding areas with high concentrations of African American residents and thus further reducing access to jobs for African Americans living in racially segregated communities. Each of these actions raised the risk of poverty for residents of Detroit's racially segregated neighborhoods.
Although the housing covenants in real estate titles that blocked the sale of homes to African Americans in many segregated white Detroit neighborhoods were ruled unconstitutional in 1948, the ruling did not end discriminatory real estate practices (McWhirter 2001). In the 1950s, the racial integration of Detroit's neighborhoods was undermined by stereotypes that fueled white residents’ fears, contributing to their attempts to prevent African Americans from moving into their neighborhoods or to drive them out (Frey 1980a, 1980b; Sugrue 1996; Turrini 1999). In addition, the houses that were razed in the 1950s and 1960s for several interstate highways through the city were in predominantly African American neighborhoods, forcing the residents to relocate. As African Americans moved into previously white, segregated neighborhoods, the white residents fled, influenced by fears of declining property values and by racial stereotypes encouraged by the real estate agents who stood to profit from the rapid turnover of housing (Frey 1980a; McWhirter 2001; Sugrue 1996).
The results of such changes are visible in the current spatial organization of poverty and race in the Detroit metropolitan area. Between 1970 and 1980, when 51 percent of the city's white residents moved out, the number of census tracts in Detroit in which more than 40 percent of the residents were below the poverty line nearly doubled, from 24 to 51. Then the number of high-poverty census tracts tripled again—from 51 in 1980 to 149 in 1990—as 48 percent of the remaining whites left the city (Jargowsky 1997). Simultaneously, the number of Detroit residents who lived in high-poverty census tracts rose from 55,913 in 1970 to 418,947 in 1990 (Jargowsky 1997). Figure 2 shows the growth and spatial distribution of high-poverty census tracts in the Detroit metropolitan area between 1970 and 1990. This exponential growth in high-poverty census tracts in the city is juxtaposed against the near absence in outlying areas of census tracts with high concentrations of poverty. For example, in 1990, in the neighboring counties of Oakland and Macomb, just 0.4 and 0 percent of the census tracts, respectively, contained 40 percent or more households that were below the poverty line (U.S. Bureau of the Census 2000).
fig. 2.
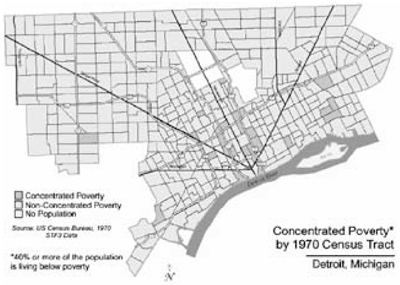
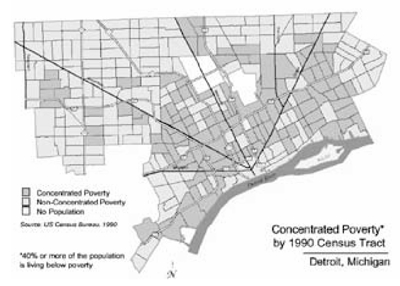
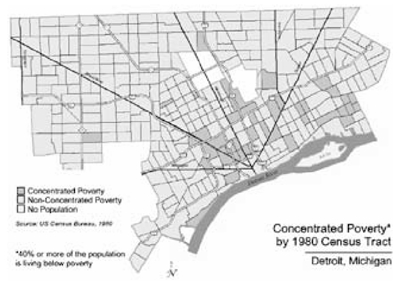
Census tracts with more than 40 percent of residents below the poverty line in Detroit, Michigan, 1970, 1980, and 1990. “Nonconcentrated poverty” refers to census tracts in which less than 40 percent of households reported incomes that fell below federal poverty standards in that year. The cities of Highland Park and Hamtramck, at one time “edge cities” on the outskirts of Detroit, are now completely surrounded by the city. In this figure, they appear as white areas in the center of the city. The racial composition of these areas, once predominantly white ethnic, is now similar to that of the surrounding Detroit neighborhoods. Source: Maps created by Jason C. Booza, Center for Urban Studies, Wayne State University.
In 1990 the median value for owner-occupied homes in Bloomfield Hills, an outer-ring suburb in Oakland County, was $500,000; in Royal Oak, an inner-ring suburb, $75,900; and in Detroit, $25,300 (U.S. Bureau of the Census 1990). Many other major urban areas have similar spatial arrangements of poverty and wealth (see Jargowsky 1997), a configuration that has led some to describe urban landscapes as social hierarchies laid on their sides—that is, as geographical reflections of social statuses or rankings, with those with the lowest social status in the center and those with higher social statuses on the periphery.
Figure 3 shows the spatial organization of African American and white residents in Detroit in 1990. African Americans are concentrated in census tracts inside the city, with the majority of whites living on the periphery, or (not shown) outside the city boundaries. Table 3 shows that the proportion of both white and African American residents of Detroit who live in high-poverty census tracts increased dramatically between 1970 and 1990. In 1970, just 2 percent of whites and 6 percent of African Americans lived in census tracts in which 40 percent or more of households were below the poverty line. By 1990, 35 percent of the city's white and 43 percent of its African American residents lived in such census tracts. Because the city's population is predominantly African American, 79 percent of all residents of high-poverty census tracts are African American.
fig. 3.
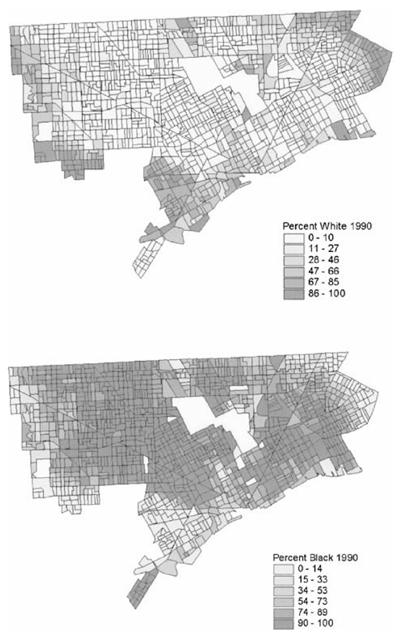
Census tracts by percentage of Detroit residents who identify as white or as African American, 1990. Source: Maps created by Jason C. Booza, Center for Urban Studies, Wayne State University.
TABLE 3.
Number and Percentage of Non-Hispanic White, African American, and Hispanic Detroit Residents Living in Census Tracts in Which More Than 40 Percent of Households Have Incomes below the Poverty Line, 1970–1990
| 1970 | 1980 | 1990 | |
|---|---|---|---|
| Non-Hispanic White | |||
| Number in City | 838,877 | 408,627 | 212,804 |
| Number in High-Poverty Census Tracts | 16,286 | 22,515 | 73,731 |
| Percentage Living in High-Poverty | 2 | 6 | 35a |
| Census Tracts | |||
| African American | |||
| Number in City | 660,428 | 753,863 | 775,833 |
| Number in High-Poverty Census Tracts | 39,127 | 96,225 | 333,014 |
| Percentage Living in High-Poverty | 6 | 13 | 43b |
| Census Tracts | |||
| Hispanic | |||
| Number in City | 27,038 | 28,466 | 27,157 |
| Number in High-Poverty Census Tracts | 500 | 1,699 | 12,202 |
| Percentage Living in High-Poverty | 2 | 6 | 45c |
| Census Tracts | |||
Notes:
In 1990, 2% of white residents of standard metropolitan areas (SMAs) nationally lived in census tracts in which >40% of households were below the poverty line (Jargowsky 1997, table A.1).
In 1990, 17% of African American residents of SMAs nationally lived in census tracts in which>40% of households were below the poverty line (Jargowsky 1997, table A.1).
In 1990, nationally 10% of Hispanic residents of SMAs lived in census tracts in which40% of households were below the poverty line (Jargowsky 1997, table A.1).
Source: Data from Jargowsky 1997; and from U.S. Bureau of the Census 1970, 1980, and 1990.
Table 3 also shows the combination of demographic trends that have helped cluster African Americans in high-poverty neighborhoods. Specifically, three-quarters of whites residing in the city in 1970 had moved out of the city by 1990, while the total number of African American residents rose slightly. As a result of these trends, the ratio of African American to white residents shifted from 1 to 1.3 in 1970 to 3 to 1 in 1990. Those African Americans who remained in the city were thus far more likely to feel the effects of the city's declining tax base, property values, and employment opportunities than were the white residents who relocated to the suburbs. While the 2000 census shows a slight decline in segregation, it was only because some African Americans had moved into previously all-white census tracts. This decline has not reduced the residential segregation of African Americans or the concentration of urban poverty (Glaeser and Vigdor 2001). (These trends are visible in Table 2, which shows a slight decline in the index of dissimilarity for the Detroit metropolitan area [from 87.5 in 1990 to 84.7 in 2000], while the index of dissimilarity for the city itself has continued to trend upward.) African Americans in the Detroit metropolitan area continue to be more likely than white residents to live in high-poverty census tracts.
The increasing segregation of African Americans in high-poverty Detroit neighborhoods reflects the cumulative effects of multiple forms of discrimination. Both direct and indirect discrimination in housing persists (Fix and Struyk 1993), and the exclusion of African Americans from white residential areas is visible in Detroit as well as in national census data (Glaeser and Vigdor 2001). Continuing racial stereotypes contribute to whites’ movement out of areas where the African American population is growing (Clark 1991; Farley, Bianchi, and Colasanto 1979; Farley, Danziger, and Holzer 2000; Farley et al. 1994; Krysan and Farley 2002). Racial stereotypes may also be linked to other forms of discrimination, including everyday interactions that are insulting, derogatory, or unfair. According to research conducted in the Detroit metropolitan area, African Americans report more incidences of unfair treatment than do whites, and these encounters are associated with negative health outcomes (Schulz, Israel, et al. 2000; Schulz, Williams, et al. 2000; Williams et al. 1997).
The movement of employers and employment opportunities out of the city, which has intensified the segregation of African American residents in the older areas and concentrated the poverty in those aging urban census tracts, has shaped the present landscape of race and wealth in the Detroit metropolitan area. As described in some detail by Wilson (1996) and others, the movement of jobs to outlying suburban areas, combined with race-based housing discrimination, physically separated those African Americans living in older urban areas from employment opportunities and thus contributed to lower household incomes. Often termed the spatial mismatch hypothesis, the movement of relatively high-wage manufacturing jobs from older urban areas to newer suburban areas in the Northeast and Midwest, combined with discriminatory housing practices, has been used to explain unemployment and the higher poverty rates among African Americans in urban communities (Kain 1992).
Farley, Danziger, and Holzer (2000) explained how three out of four production jobs were lost from Detroit's manufacturing industries between 1972 and 1992. As manufacturing jobs that offered workers a stable middle-class income left the city, many African Americans were left behind in communities with few employment opportunities. Furthermore, the jobs that remained disproportionately required either less than a high school education or a postgraduate degree. Orfield (1993, 2001) described the impact of residential segregation on the quality of urban public schools, which, because of the rising poverty, have lost both their tax base and their resources. As a result, the graduates of poor urban schools tend to have learned less and be less apt to continue on to college, when compared with graduates of suburban schools with better resources. Thus, the educational opportunities available to African Americans residing in segregated, high-poverty urban communities do not prepare them for the better-paid employment opportunities available.
Some residents commute to jobs in the suburbs. Farley, Danziger, and Holzer note that
just 8 percent of metropolitan whites lived in the city in 1990, but 14 percent worked there. There is a counterbalancing flow of central-city blacks to the suburbs: only 17 percent of blacks lived in the [suburban] rung, but 50 percent of those with jobs worked there … in 1990, 150,000 suburban whites commuted to jobs in the city, while 91,000 blacks left the city for jobs in the ring. (2000, 69)
For others, the mismatch between educational qualifications and the jobs available in the city actually reduced their household income. For example, there is evidence that employers in the poorest areas of Detroit lowered wages in response to the surplus of Detroit residents seeking employment in the city (Zax and Kain 1996).
Race-based residential segregation, economic divestment, and increased segregation are linked to legal, political, and economic systems that interact with racial ideologies. The spatial distribution of racial groups as a physical expression of these factors isolates many African Americans in urban communities with few employment opportunities, institutions that support community life, and opportunity structures (Jargowsky 1997; Massey and Denton 1993; Wacquant and Wilson 1989; Wilson 1987). More than simply reflecting the aggregate implications of the individual characteristics of households clustered in areas of concentrated poverty—which have been termed composition effects (Macintyre, Maciver, and Sooman 1993)—there are also substantial contextual or areal effects above and beyond the effects of the residents’ individual characteristics. If living in a poor area adversely affects health—and the evidence suggests that this is the case—then the disproportionate clustering of African Americans into very poor census tracts most likely contributes to racial disparities in health.
The Spatial Distribution of Poverty and Intermediate Factors: Physical and Social Environments
In keeping with the definition of a fundamental cause, the withdrawal of economic resources from older, racially segregated urban areas reduces access to those resources essential to prevent disease and promote health. According to figure 1, racial segregation and the concurrent withdrawal of economic resources affect the physical environment (e.g., air quality, exposure to excessive noise), the community infrastructure, and the social environment (e.g., municipal services such as street maintenance, police, and firefighting; public institutions like public schools; medical services such as hospitals and pharmacies; retail establishments like grocery stores). These, in turn, influence more proximate factors (e.g., physical activity, dietary patterns, social integration, social support) that affect health outcomes, which we examine next.
Race-Based Residential Segregation, Concentrated Poverty, and the Physical Environment
There is substantial evidence that residents of urban communities with high concentrations of poverty are disproportionately exposed to physical environments that place them at higher risk for a variety of diseases (Bryant and Mohai 1992; Bullard 1994; Freudenberg 1998; Maantay 2001). Residents are exposed on a number of fronts, including airborne pollutants, heavy traffic, and industrial contaminants from industrial areas.
For example, we described the spatial mismatch between employment opportunities and educational preparation in the Detroit metropolitan area, which results in thousands of metropolitan area residents commuting to work. Many of Detroit's most impoverished neighborhoods are next to the highways that run through the city (see figure 2). In addition, southwest Detroit is the home of the Ambassador Bridge, the main transportation route between Detroit and Canada, over which thousands of diesel-powered trucks travel daily. The truck traffic for the Ambassador Bridge is routed through surface streets in southwest Detroit neighborhoods, exposing residents to noise, traffic hazards, and diesel exhaust. Data from the Community Action Against Asthma (CAAA) study in Detroit show that the exposure to airborne particulate matter (PM10) is approximately 22 percent higher in Detroit's southwest neighborhoods than on the city's east side (Keeler et al. 2002). Studies conducted in other urban areas have found increased exposure to airborne particulate matter is associated with asthma (Mortimer et al. 2000) and cardiovascular disease (Samet et al. 2001).
Decisions about land use, such as the siting of hazardous waste facilities, the routing of truck traffic through areas of the city, and industrial land use, are made by elected officials and so are partly determined by the residents’ ability to influence political processes (Maantay 2001). In a study of land use decisions in New York City, Maantay quotes a zoning expert as saying,
No question that zoning protects some people better than others. Zoning is responsive to wealth, property, political power, and those areas or communities that are more politically empowered or connected clearly will be able to get done the zoning changes that they desire and to prevent the zoning changes that they don't desire. Less politically or economically empowered communities, even though you have a formal structure (for public participation), will be less able to impact on changes that are taking place to them or around them.
(Maantay 2001, 1038)
Cohen and Dawson (1993) documented the effects of residence in very poor census tracts on political influence in Detroit neighborhoods. The poorer an area is, the fewer people it will contain who have the requisite economic resources and political influence to shape decisions regarding land use or the enforcement of existing regulations. Concentrating those residents with few political and economic resources into specific areas of the city may thus increase their exposure to hazards in the physical environment.
Race-Based Residential Segregation, Concentrated Poverty, and Community Infrastructure
Figure 1 also shows the relationships between race-based residential segregation and poverty to a community's infrastructure and social environment. This figure reflects the evidence that such communities have experienced a series of setbacks contributing to the loss of infrastructure that supports community residents (Wacquant and Wilson 1989; Wilson 1996). For example, urban renewal projects like the new highway systems of the 1960s destroyed thriving African American businesses and residential neighborhoods like Detroit's Black Bottom area (Sugrue 1996). Banks, restaurants, grocery stores, and other white-owned retail establishments fled predominantly African American neighborhoods as they became poorer and as racial tensions in Detroit heightened in the 1960s (Hartigan 1999). The exodus of major grocery stores and other retail outlets from high-poverty areas in Detroit has forced residents to shop in small convenience or liquor stores in their communities, which have limited selections, often of poor quality and at high prices (Schulz et al. 2001; Sugrue 1996).
As businesses and employment opportunities moved out of Detroit, residents lost important sources of household income, and communities lost the tax base that had helped sustain their infrastructure (Farley, Danziger, and Holzer 2000; Sugrue 1996). Nationally, between 1986 and 1996, the average property tax base per household rose by 30.8 percent, but in Detroit it dropped by 8.4 percent (Maines and McMillan 2001). The declining tax base has particularly affected residents of high-poverty neighborhoods in Detroit. The deterioration of those systems designed to protect public safety—for example, police and firefighting services, as well as municipal supports such as the enforcement of regulations against illegal dumping—is a pervasive concern voiced by Detroit residents (Schulz and Lempert 2000; Schulz et al. 2001).
The city's failure or inability to maintain public safety or to uphold city regulations leads to more crimes (Sampson 1987) and to fears and concerns about safety, termed subjective stressors (Harburg et al. 1970; Schulz et al. 2001). These findings suggest that the loss of capital from urban communities affects not only the residents’ material conditions but also the responsiveness of institutional supports and services.
These changes in institutional supports and the increasing concentration of poverty among residents also affect health service providers located in the city. Health care facilities in very poor neighborhoods have a higher burden of indigent care and are more likely to close than are health care facilities located in more affluent neighborhoods (McLafferty 1982; Whiteis 1992). Furthermore, Detroit residents note the cost of medications is higher in poor Detroit neighborhoods than it is in outlying suburban areas (Schulz and Lempert 2000). A recent study found also that pharmacies in minority neighborhoods have less access to some medications than do those in other areas (Morrison et al. 2000).
Concentrations of Poverty and Proximate Factors: Stress, Social Networks, and Behaviors
We now turn to the most immediate factors related to health, as indicated in figure 1, specifically the implications of the factors described in the preceding section for psychosocial stressors, health-related behaviors, and social networks and the support that those networks may provide. We also present the results of etiologic research linking each to health outcomes.
Neighborhood Characteristics, Stress, and Health
The combination of reduced household income and the structural dissolution of city services and supports contributes to a variety of neighborhood characteristics that may be expressed at the individual level as stressors (see figure 1). Very poor neighborhoods have greater numbers of deteriorated or vacant houses and fewer houses occupied by their owners (Jargowsky 1997; U.S. Bureau of the Census 1990). Similarly, illegally dumped materials in vacant lots or vacant buildings can create hazards for residents, particularly for children in poor neighborhoods (Farquhar et al. 2002; Fitzpatrick and LaGory 2000). In sum, the physical and social environments in poor neighborhoods in Detroit have multiple implications for the residents of those communities.
Harburg and colleagues (1970) found that residents of high-poverty Detroit neighborhoods were more likely than residents of low-poverty neighborhoods to report slower police response time, worries about fires in their neighborhoods, and higher crime rates and other concerns about safety. Residents of such neighborhoods were also much more likely to have high blood pressure than were residents of less poor Detroit neighborhoods (Harburg et al. 1970). More recent studies conducted in Detroit similarly indicate that residents of census tracts with high concentrations of poverty report more stressors related to neighborhood conditions (e.g., concerns about safety, lack of confidence in police response, stressors related to the physical environment) than do residents of census blocks with lower concentrations of poverty (Schulz, Israel, et al. 2000) and that self-reports of neighborhood stressors are significantly and negatively associated with indicators of mental and physical well-being (Schulz et al. 1998; Schulz, Israel, et al. 2000: Schulz et al. 2001). The expansion of very poor areas in the city between 1970 and 1990, described earlier, indicates that the number of residents whose health might be affected by these processes also has increased and that those residents who are usually affected are African American.
Neighborhood Characteristics, Social Support, and Health
Research conducted in Detroit and other poor urban communities (Buffalo, Newark) revealed the effects of deteriorating structural supports of community life on interpersonal relationships (Fine and Weiss 1998; Schulz and Lempert 2000). Residents described the impact of the deterioration of their neighborhood's infrastructures on relationships and trust among neighbors (Fine and Weiss 1998). The structural conditions of the neighborhoods—described as significant sources of stress or worry—also appear to erode the social relationships that might help protect health under stressful life conditions (Fine and Weiss 1998; Schulz and Lempert 2000). The protective effects of social relationships on health have been well established (Heaney and Israel 1997; House, Landis, and Umberson 1988), and the deterioration of those networks resulting from a perceived lack of safety or trust in neighbors is consistent with research indicating that lower socioeconomic status groups report less access to social support than do those with more economic resources (Lantz et al. 1998).
Health-Related Behaviors
Neighborhood conditions, including the physical environment, can influence a number of health-related behaviors. For example, the absence of grocery stores in poor neighborhoods reduces access to a variety of food products that have been linked to health (Cheadle et al. 1991; Nestle and Jacobson 2000; Swinburn, Egger, and Raza 1999; Travers 1996). Similarly, the safety of neighborhood streets and the extent to which they are kept free of dumped materials are likely to influence physical activity, as residents may choose to remain indoors rather than walk or engage in other forms of physical activity (Sherwood and Jeffery 2000; Stahl et al. 2001). These results suggest that socioeconomic status influences social support and health-related behaviors beyond individual characteristics to include the effects of living in areas with high concentrations of poverty.
Discussion
Understanding and addressing racial disparities in health in the United States must account for—not simply document—the relationship between race and socioeconomic status. In this article, we argued that race-based residential segregation is a fundamental cause of racial disparities in health, isolating many African Americans in spatially distinct neighborhoods where their access to the resources necessary to maintain health is limited. Communities in which large numbers of residents are impoverished have less political power and therefore have less control over their environments (e.g., the siting of industrial plants, the enforcement of environmental regulations) and greater exposure to hazards in the physical environment. Similarly, this framework suggests that residents of very poor communities also have less access to resources that help sustain daily life, including grocery stores and other retail outlets, as well as police, fire, and other municipal protection. Finally, we reviewed evidence showing that these intermediate factors influence more proximate factors related to health, including physical activities, dietary patterns, and social relationships. A substantial body of research evidence links various aspects of our model, and we believe that evidence is relevant. Identifying the relationships among fundamental, intermediate, and social factors can help us understand the multiple and dynamic mechanisms by which these factors cause racial disparities in health.
Our model also outlines the challenges as well as opportunities faced by public health professionals and residents of racially segregated urban communities in determining where efforts to improve health should be focused. Opportunities for intervention include efforts to increase access to health care or to enhance social connections. Such efforts can provide essential and immediate resources to help minimize the substantial negative impacts of poverty on health and—because African Americans are disproportionately represented in poor communities—may help reduce pervasive racial disparities in health.
Similarly, interventions might focus on intermediate social factors, such as limiting the number or size of industrial or waste facilities and ensuring that regulations limiting noxious emissions are enforced in or near neighborhoods with high concentrations of poverty and high proportions of labeled ethnic groups. Because political and regulatory systems may be less responsive to residents of urban areas with fewer political and economic resources (Cohen and Dawson 1993; Maantay 2001; Sclar and Northridge 2001), the success of such efforts may rely on the ability to enhance civic engagement and political influence (e.g., coalitions that bring together residents of very poor neighborhoods with residents of other neighborhoods and public health and housing officials). Strategies like these may lower the risk of disease linked to toxic exposures, again helping reduce racial disparities in health because African American and Hispanic Americans are disproportionately likely to live near such noxious land uses.
The definition of a fundamental social determinant of health is one that operates through several mechanisms to affect many health outcomes. While interventions that address proximate or intermediate social factors may lead to short-term improvements in health, they are unlikely, in the long run, to eliminate health disparities based on social inequalities. In social systems in which diseases, risks, treatment options, and knowledge are constantly changing, those with greater access to resources that can be used to avoid the risk of disease or minimize its consequences—resources such as money, prestige, knowledge, and social connectedness—are better positioned to protect and promote their health (Link and Phelan 1995). Following this rationale, eradicating racial disparities in health may require intervening in the processes that sustain racial segregation and the concentration of poverty that disproportionately affect access to resources in predominantly African American communities. These include addressing fundamental economic and political processes, as well as racial ideologies whose consequences are the spatial separation of African Americans from white Americans and the uneven distribution of resources across racial groups. This spatial separation of races is an important mechanism through which African Americans’ access to educational, economic, political, and other resources necessary to maintain health is limited.
Efforts to counter the large-scale changes in the organization of metropolitan areas that have resulted in the isolation of many African American households in areas without economic opportunities could help reduce concentrations of poverty—and health risks—in those neighborhoods. Analyses conducted by Hart and colleagues (1998) suggest that metropolitan areas with separate, decentralized governments (e.g., distinct government structures for large urban areas, edge cities, and suburban areas) also tend to have higher levels of race-based residential segregation and poorer health outcomes for African Americans. In contrast, those areas with centralized governments usually have lower levels of racial segregation and better health outcomes among African Americans (Hart et al. 1998). Hart and colleagues suggest that the fragmentation of government structures facilitates the adoption of policies that increase racial and economic residential segregation through, for example, zoning regulations (e.g., minimum lot or house sizes that preclude the development of low- and moderate-income housing). Furthermore, such government structures may not recognize the shared interests of residents in a larger metropolitan area.
Where local governments are decentralized, political alliances or coalitions that cross current governmental boundaries may facilitate the development of, for example, integrated public transportation systems that allow travel between core cities and surrounding cities and suburban areas. Similarly, encouraging those decentralized governments to work together to develop regional plans for disposal of wastes—whether residential or industrial—in a manner that does not endanger the health of any residents, as an alternative system to endangering those residents who are least able to resist, will require cooperation across class, racial, and local political boundaries. Building the political will for such cooperation remains a challenge for metropolitan areas like Detroit, which over the past several decades have leaned toward the fragmentation of municipalities and decision-making bodies, along with consistently high levels of racial segregation and growing economic inequalities. Finding mechanisms through which those with greater racial and class privileges can recognize shared interests across race and class may provide opportunities for change.
There is increasing evidence that the problems created by racism and segregation are not confined to very poor African American communities. Research in Chicago and New York City indicates that areas are affected not only by the conditions inside them but also by those close to them (Morenoff and Sampson 1997; Morenoff and Tienda 1997; Wallace 1990). As conditions in a municipal area deteriorate, they also influence adjacent areas. These patterns are visible in the expansion of high-poverty areas over time to proximate census tracts in figure 2 and also are apparent in the growth of high-poverty census tracts in other major urban areas (Jargowsky 1997; Morenoff and Sampson 1997; Morenoff and Tienda 1997). Over the past several decades, whites—who have had greater residential mobility than African Americans—have disproportionately responded by moving out of the city. This trend toward flight and fragmentation has contributed to the current spatial configurations of race and wealth typical of Detroit and other similar urban areas, contributing to racial disparities in health. Reversing these trends will require sustained efforts to recognize shared interests and the potential for change.
Race-based residential segregation is a fundamental determinant of health, one that disproportionately affects African Americans who reside in those communities by sharply constraining their access to the resources necessary to maintain health. While this article focuses on the Detroit metropolitan area, similar processes are apparent in many older urban areas, particularly those in the Midwest and Northeast. The conceptual framework presented here describes how racial discrimination and economic divestment contribute to racial disparities in health. While strategies to address intermediate and proximate social factors may reduce racial disparities in specific health outcomes, eliminating those disparities requires both recognizing the social processes that sustain racial and socioeconomic inequalities and implementing strategies to address those social factors.
Acknowledgments
The authors wish to thank Shannon Zenk for research assistance, Jim Roll for assistance with census data, and Jason Booza at the Center for Urban Studies, Wayne State University, for mapping the census data. In addition, we thank Sue Andersen for her contributions to the preparation of this manuscript. The research reported here was supported in part by a cooperative agreement with the Centers for Disease Control and Prevention, grant no. U48/CCU515775.
References
- Anderson RP, Sorlie PD, Backlund E, Johnson N, Kaplan GA. Mortality Effects of Community Socioeconomic Status. Epidemiology. 1997;8:42–7. doi: 10.1097/00001648-199701000-00007. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Sucoff CA. The Neighborhood Context of Adolescent Mental Health. Journal of Health and Social Behavior. 1996;37:293–310. [PubMed] [Google Scholar]
- Antonovsky A. Social Class, Life Expectancy, and Overall Mortality. Milbank Quarterly. 1967;45:31–73. [PubMed] [Google Scholar]
- Bryant B, Mohai P. Race and the Incidence of Environmental Hazards: A Time for Discourse. Boulder, Colo.: Westview Press; 1992. [Google Scholar]
- Bullard RD. Solid Waste Sites and the Black Houston Community. Sociological Inquiry. 1994;53:273–88. doi: 10.1111/j.1475-682x.1983.tb00037.x. [DOI] [PubMed] [Google Scholar]
- Cassel J. The Contribution of the Social Environment to Host Resistance. American Journal of Epidemiology. 1976;104:107–23. doi: 10.1093/oxfordjournals.aje.a112281. [DOI] [PubMed] [Google Scholar]
- Cheadle A, Psaty BM, Curry S, Wagner E, Diehr P, Koepsell T, Kristal A. Community-Level Comparisons between the Grocery Store Environment and Individual Dietary Practices. Preventive Medicine. 1991;20:250–61. doi: 10.1016/0091-7435(91)90024-x. [DOI] [PubMed] [Google Scholar]
- Clark WA. Residential Preferences and Neighborhood Racial Segregation: A Test of the Schelling Segregation Model. Demography. 1991;28(1):9–19. [PubMed] [Google Scholar]
- Cohen CJ, Dawson M. Neighborhood Poverty and African American Politics. American Political Science Review. 1993;87(2):286–302. [Google Scholar]
- Cohen H, Northridge M. Getting Political: Racism and Urban Health. American Journal of Public Health. 2000;90(6):841–2. doi: 10.2105/ajph.90.6.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole RE, Deskins DR. Racial Factors in Site Location and Employment Patterns of Japanese Auto Firms in America. California Management Review. 1988;31(9):9–22. [Google Scholar]
- Collins C, Williams DR. Segregation and Mortality: The Deadly Effects of Racism? Sociological Forum. 1999;14(3):495–523. [Google Scholar]
- Cooper R, David R. The Biological Concept of Race and Its Application to Public Health and Epidemiology. Journal of Health Politics, Policy and Law. 1986;11:97–116. doi: 10.1215/03616878-11-1-97. [DOI] [PubMed] [Google Scholar]
- Darden JT. The Residential Segregation of Blacks in Detroit, 1960–1970. International Journal of Comparative Sociology. 1986;17(1–2):84–91. [Google Scholar]
- Darden JT, Hill RC, Thomas J, Thomas R. Race and Uneven Development. Philadelphia: Temple University Press; 1987. [Google Scholar]
- Diez-Roux A, Merkin SS, Arnett D, Chambless L, Massing M, Nieto F, Sorlie P, Szklo M, Tyroler H, Watson R. Neighborhood of Residence and Incidence of Coronary Heart Disease. New England Journal of Medicine. 2001;345(2):94–105. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Farley R, Bianchi S, Colasanto D. Barriers to the Racial Integration of Neighborhoods: The Detroit Case. Annals of the American Academy of Political and Social Science. 1979;441:97–113. [Google Scholar]
- Farley R, Danziger S, Holzer HJ. Detroit Divided. New York: Russell Sage; 2000. [Google Scholar]
- Farley R, Steeh C, Krysan M, Jackson T, Reeve K. Stereotypes and Segregation: Neighborhoods in the Detroit Area. American Journal of Sociology. 1994;100(3):750–80. [Google Scholar]
- Farquhar SA, Parker EA, Schulz AJ, Israel BA. A Qualitative Analysis of the Effects of Environmental Stressors on the Well-Being of Residents in Detroit, Michigan. 2002. Unpublished manuscript.
- Feagin JR. Racist America: Roots, Current Realities, and Future Reparations. New York: Routledge; 2000. [Google Scholar]
- Fine M, Weiss L. The Unknown City: The Lives of Poor and Working Class Young Adults. Boston: Beacon Press; 1998. [Google Scholar]
- Fitzpatrick KM, LaGory ME. Unhealthy Places: The Ecology of Risk in the Urban Landscape. New York: Routledge; 2000. [Google Scholar]
- Fitzpatrick KM, LaGory ME, Ritchey FJ. Dangerous Places: Exposure to Violence and Its Mental Health Consequences for the Homeless. American Journal of Orthopsychiatry. 1999;69(4):438–47. doi: 10.1037/h0080392. [DOI] [PubMed] [Google Scholar]
- Fix M, Struyk RJ. Clear and Convincing Evidence: Measurement of Discrimination in America. Washington, D.C.: Urban Institute Press; 1993. [Google Scholar]
- Freudenberg N. Community-Based Health Education for Urban Populations: An Overview. Health Education and Behavior. 1998;25(1):11–23. doi: 10.1177/109019819802500103. [DOI] [PubMed] [Google Scholar]
- Frey WH. Black In-Migration, White Flight and the Changing Economic Base of the Central City. American Journal of Sociology. 1980a;85(6):1396–417. [Google Scholar]
- Frey WH. Status Selective White Flight and Central City Population Change: A Comparative Analysis. Journal of Regional Science. 1980b;20(1):71–89. doi: 10.1111/j.1467-9787.1980.tb00627.x. [DOI] [PubMed] [Google Scholar]
- Garreau J. Edge City: Life on the New Frontier. New York: Doubleday; 1991. [Google Scholar]
- Geronimus AT. To Mitigate, Resist or Undo: Addressing Structural Influences on the Health of Urban Populations. American Journal of Public Health. 2000;90(6):867–72. doi: 10.2105/ajph.90.6.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Bound J, Waidmann T. Poverty, Time, and Place: Variation in Excess Mortality across Selected US Populations, 1980–1990. Journal of Epidemiology and Community Health. 1999;53:325–34. doi: 10.1136/jech.53.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Bound J, Waidmann T, Hillemeier M, Burns P. Excess Mortality among Blacks and Whites in the United States. New England Journal of Medicine. 1996;335:1552–8. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- Glaeser EL, Vigdor JL. Racial Segregation in the 2000 Census: Promising News. Washington, D.C.: Brookings Institution; 2001. Survey Series. [Google Scholar]
- Haan MN, Kaplan GA, Camacho C. Poverty and Health: Prospective Evidence from the Alameda County Study. American Journal of Epidemiology. 1987;125:989–98. doi: 10.1093/oxfordjournals.aje.a114637. [DOI] [PubMed] [Google Scholar]
- Harburg E, Schull WJ, Erfurt JC, Schork MA. A Family Set Method for Estimating Heredity and Stress. Journal of Chronic Disease. 1970;23:69–81. doi: 10.1016/0021-9681(70)90066-4. [DOI] [PubMed] [Google Scholar]
- Harris DR. Ann Arbor: Population Studies Center at the Institute for Social Research, University of Michigan; 1997. All Suburbs Are Not Created Equal: A New Look at Racial Differences in Suburban Location. Research Report. [Google Scholar]
- Hart KD, Kunitz SJ, Sell RR, Mukamel DB. Metropolitan Governance, Residential Segregation, and Mortality among African Americans. American Journal of Public Health. 1998;88(3):434–8. doi: 10.2105/ajph.88.3.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartigan J. Racial Situations: Class Predicaments of Whiteness in Detroit. Princeton N.J.: Princeton University Press; 1999. [Google Scholar]
- Heaney CA, Israel BA. Social Networks and Social Support in Health Education. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education. San Francisco: Jossey-Bass; 1997. pp. 179–205. [Google Scholar]
- Hill RC. Race, Class and the State: The Metropolitan Enclave System in the United States. The Insurgent Sociologist. 1980;10(2):45–59. [Google Scholar]
- House JS, Kessler RC, Herzog R, Mero RP, Kinney AM, Breslow B. Age, Socioeconomic Status and Health. Milbank Quarterly. 1990;68(3):383–411. [PubMed] [Google Scholar]
- House JS, Landis K, Umberson D. Social Relationships and Health. Science. 1988;241:540–5. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- House JS, Lepkowski JM, Kinney AM, Mero RP, Kessler RC, Herzog AR. The Social Stratification of Aging and Health. Journal of Health and Social Behavior. 1994;35:213–34. [PubMed] [Google Scholar]
- House JS, Lepkowski JM, Williams DR, Mero R, Lantz P, Robert S, Chen J. Excess Mortality among Urban Residents: How Much, for Whom, and Why. American Journal of Public Health. 2000;90(12):1898–1904. doi: 10.2105/ajph.90.12.1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Williams DR. Promoting Health: Intervention Strategies from Social and Behavioral Research. Washington D.C.: National Academy Press; 2000. Understanding and Reducing Socioeconomic and Racial/Ethnic Disparities in Health; pp. 81–124. [Google Scholar]
- Hummer RA. Black-White Differences in Health and Mortality: A Review and Conceptual Model. Sociological Quarterly. 1996;37(1):105–25. [Google Scholar]
- James SA. Primordial Prevention of Cardiovascular Disease among African Americans: A Social Epidemiological Perspective. Preventive Medicine. 1999;29:S84–9. doi: 10.1006/pmed.1998.0453. [DOI] [PubMed] [Google Scholar]
- Jargowsky PA. Poverty and Place: Ghettos, Barrios, and the American City. New York: Russell Sage; 1997. [Google Scholar]
- Kain JF. The Spatial Mismatch Hypothesis: Three Decades Later. Housing Policy Debate. 1992;3(2):371–460. [Google Scholar]
- Kaplan GA, Lynch JW. Socioeconomic Considerations in the Primordial Prevention of Cardiovascular Disease. Preventive Medicine. 1999;26(2) 6:S30–5. doi: 10.1006/pmed.1999.0540. [DOI] [PubMed] [Google Scholar]
- Keeler GJ, Dvonch JT, Yip FY, Parker E, Israel B, Marsik F, Morishita M, Barreo J, Robins T, Brakefield-Caldwell W, Sam M. Assessment of Personal and Community-Level Exposures to Particulate Matter among Children with Asthma in Detroit, Michigan, as part of Community Action Against Asthma (CAAA) Environmental Health Perspectives. 2002;2:173–81. doi: 10.1289/ehp.02110s2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kington RS, Nickens HW. Racial and Ethnic Differences in Health: Recent Trends, Current Patterns, Future Directions. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America Becoming: Racial Trends and Their Consequences. Vol. 2. Washington D.C.: National Academy Press; 2001. pp. 253–310. [Google Scholar]
- Krieger N. Embodying Inequality: A Review of Concepts, Measures, and Methods for Studying Health Consequences of Discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, Sexism, and Social Class: Implications for Studies of Health, Disease, and Well-Being. American Journal of Preventive Medicine. 1993;9(6):82–122. [PubMed] [Google Scholar]
- Krysan M, Farley R. The Residential Preferences of Blacks: Do They Explain Persistent Segregation. Social Forces. 2002;80:937–80. [Google Scholar]
- Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic Factors, Health Behaviors and Mortality. Journal of the American Medical Association. 1998;279(21):1703–8. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- LaVeist TA. Linking Residential Segregation to the Infant-Mortality Disparity in U.S. Cities. Sociology and Social Research. 1989;73(2):90–4. [Google Scholar]
- LaVeist TA. The Political Empowerment and Health Status of African-Americans: Mapping a New Territory. American Journal of Sociology. 1992;97(4):1080–95. [Google Scholar]
- Lewis Mumford Center for Comparative Urban and Regional Research. Metropolitan Racial and Ethnic Change—Census 2000. 2002. [accessed June 8, 2002]. Available at http://www.albany.edu/mumford/census.
- Lillie-Blanton M, Parsons PE, Gayle H, Dievler A. Racial Differences in Health: Not Just Black and White, but Shades of Gray. Annual Review of Public Health. 1996;17:411–48. doi: 10.1146/annurev.pu.17.050196.002211. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social Conditions as Fundamental Causes of Disease. Journal of Health and Social Behavior. 1995;42(extra issue):80–94. [PubMed] [Google Scholar]
- Maantay J. Zoning, Equity and Public Health. American Journal of Public Health. 2001;91(7):1033–41. doi: 10.2105/ajph.91.7.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S, Maciver S, Sooman A. Area, Class and Health: Should We Be Focusing on Places or People? Journal of Social Policy. 1993;22:213–33. [Google Scholar]
- Maines M, McMillan M. Urban Inequality and Detroit Archdiocesan Reorganization. In: Maines DR, editor. The Faultline of Consciousness: A View of Interactionism in Sociology. Hawthorne N.Y.: Aldine; 2001. pp. 115–34. [Google Scholar]
- Massey DS, Denton NA. The Creation of Underclass Communities. In: Massey DS, Denton NA, editors. American Apartheid. Cambridge Mass.: Harvard University Press; 1993. pp. 115–47. [Google Scholar]
- Massey DS, Fischer M. How Segregation Concentrates Poverty. Ethnic and Racial Studies. 2000;23(4):670–91. [Google Scholar]
- McLafferty S. Neighborhood Characteristics and Hospital Closures: A Comparison of the Public, Private, and Voluntary Hospital Systems. Social Science & Medicine. 1982;16(19):1667–74. doi: 10.1016/0277-9536(82)90091-0. [DOI] [PubMed] [Google Scholar]
- McLeod V, Lozoff B. Racial and Ethnic Trends in Children's and Adolescents’ Behavior and Development. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America Becoming: Racial Trends and Their Consequences. Vol. 2. Washington D.C.: National Academy Press; 2001. pp. 311–50. [Google Scholar]
- McWhirter C. Broken Detroit: Death of a City Block. 2001. [accessed January 18, 2002]. Detroit News, Special Reports, June 17–21. Available at http://www.detnews.com/specialreports/2001/elmhurst/thulead/thulead.htm.
- Morenoff J D, Sampson R J. Violent Crime and the Spatial Dynamics of Neighborhood Transition: Chicago 1970–1990. Social Forces. 1997;76(1):31–64. [Google Scholar]
- Morenoff J D, Tienda M. Underclass Neighborhoods in Temporal and Ecological Perspective. Annals of the American Academy of Political and Social Science. 1997;551:59–72. [Google Scholar]
- Morrison R S, Wallenstein S, Natale D K, Senzel R S, Huang L-L. We Don't Carry That”—Failure of Pharmacies in Predominantly Nonwhite Neighborhoods to Stock Opioid Analgesics. New England Journal of Medicine. 2000;342(14):1023–6. doi: 10.1056/NEJM200004063421406. [DOI] [PubMed] [Google Scholar]
- Mortimer K M, Tager IB, Dockery D W, Neas L M, Redline S. The Effect of Ozone on Inner-City Children with Asthma. American Journal Respiratory and Critical Care Medicine. 2000;162:1838–45. doi: 10.1164/ajrccm.162.5.9908113. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) Health, United States, 2000, with Adolescent Health Chartbook. Hyattsville Md.: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- Navarro V. Race or Class, or Race and Class. International Journal of Health Services. 1989;19(2):311–4. doi: 10.2190/CNUH-67T0-RLBT-FMCA. [DOI] [PubMed] [Google Scholar]
- Navarro V. The Political Economy of Social Inequalities: Consequences for Health and Quality of Life. New York: Baywood; 2002. [Google Scholar]
- Nestle M, Jacobson M F. Halting the Obesity Epidemic: A Public Health Policy Approach. Public Health Reports. 2000;115(1):12–24. doi: 10.1093/phr/115.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived Racial Discrimination, Depression and Coping: A Study of Southeast Asian Refugees in Canada. Journal of Health and Social Behavior. 1999;40(3):193–207. [PubMed] [Google Scholar]
- O’Campo P, Xue S, Wang M-C, O’Brien Caughy M. Neighborhood Risk Factors for Low Birth Weight in Baltimore: A Multi-Level Analysis. American Journal of Public Health. 1997;87(7):1113–8. doi: 10.2105/ajph.87.7.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orfield G. Cambridge Mass: Report of the Harvard Project on School Desegregation to the National School Boards Association; 1993. The Growth of Segregation in American Schools: Changing Patterns of Separation and Poverty since 1968. [Google Scholar]
- Orfield G. Cambridge Mass: The Civil Rights Project, Harvard University; 2001. Schools More Separate: Consequences of a Decade of Resegregation. [Google Scholar]
- Pickett K E, Pearl M. Multilevel Analyses of Neighborhood Economic Context and Health Outcomes: A Critical Review. Journal of Epidemiology and Community Health. 2001;55(2):111–22. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polednak A P. Black-White Differences in Infant Mortality in 38 Standard Metropolitan Areas. American Journal of Public Health. 1991;81(11):1480–2. doi: 10.2105/ajph.81.11.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polednak A P. Poverty, Residential Segregation, and Black/White Mortality Ratios in Urban Areas. Journal of Health Care for the Poor and Underserved. 1993;4(4):363–73. doi: 10.1353/hpu.2010.0094. [DOI] [PubMed] [Google Scholar]
- Ren X S, Amick BC, Williams DR. Racial/Ethnic Disparities in Health: The Interplay between Discrimination and Socioeconomic Status. Ethnicity and Disease. 1999;9(2):151–65. [PubMed] [Google Scholar]
- Roberts E. Neighborhood Social Environments and the Distribution of Low Birthweight in Chicago. American Journal of Public Health. 1997;87:597–603. doi: 10.2105/ajph.87.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet J M, Dominici F, Curriero C, Ciyrsac I, Zeger SL. Fine Particulate Air Pollution and Mortality in 20 US Cities, 1987–1994. New England Journal of Medicine. 2001;343(24):1742–9. doi: 10.1056/NEJM200012143432401. [DOI] [PubMed] [Google Scholar]
- Sampson R J. Urban Black Violence: The Effect of Male Joblessness and Family Disruption. American Journal of Sociology. 1987;93:348–82. [Google Scholar]
- Sampson RJ, Wilson WJ. Toward a Theory of Race, Crime and Urban Inequality. In: Hagan J, Peterson RD, editors. Crime and Inequality. Stanford Calif: Stanford University Press; 1995. pp. 37–54. [Google Scholar]
- Schulz A J, Israel BA, Williams D R, Parker E A, James SA. Social Inequalities, Stressors and Self-Reported Health Status among African American and White Women in the Detroit Metropolitan Area. Social Science and Medicine. 2000;51:1639–53. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- Schulz A J, Lempert LB. “Being Part of the World”: Detroit Women's Perceptions of Health and the Social Environment. 2000. Paper presented to the annual meeting of the American Sociological Association, Anaheim, Calif., August.
- Schulz A J, Parker EA, Israel B A, Becker A B, Maciak B J, Hollis R. Conducting a Participatory Community-Based Survey: Collecting and Interpreting Data for a Community Intervention on Detroit's East Side. Journal of Public Health Management and Practice. 1998;4(2):10–24. doi: 10.1097/00124784-199803000-00004. [DOI] [PubMed] [Google Scholar]
- Schulz A J, Parker EA, Israel B A, Fisher T. Social Context, Stressors and Disparities in Women's Health. Journal of the American Medical Women's Association. 2001;56:143–9. [PubMed] [Google Scholar]
- Schulz A J, Williams DR, Israel B A, Becker A B, James S A, Jackson J. Unfair Treatment, Neighborhood Effects, and Mental Health in the Detroit Metropolitan Area. Journal of Health and Social Behavior. 2000;41:314–32. [PubMed] [Google Scholar]
- Sclar E, Northridge M. Property, Politics and Public Health. American Journal of Public Health. 2001;91(7):1013–4. doi: 10.2105/ajph.91.7.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood N E, Jeffery RW. The Behavioral Determinants of Exercise: Implications for Physical Activity Interventions. Annual Review of Nutrition. 2000;20:21–44. doi: 10.1146/annurev.nutr.20.1.21. [DOI] [PubMed] [Google Scholar]
- Sorlie P D, Rogot E, Anderson R. Black-White Mortality Differences by Family Income. Lancet. 1992;340:346–50. doi: 10.1016/0140-6736(92)91413-3. [DOI] [PubMed] [Google Scholar]
- Stahl T, Rutten A, Nutbeam D, Bauman A, Kannas L, Abel T, Luschen G, Diaz-Rodriguez J A, Vinck J, Vanderzee J. The Importance of the Social Environment for Physically Active Lifestyle—Results from an International Study. Social Science and Medicine. 2001;52(1):1–10. doi: 10.1016/s0277-9536(00)00116-7. [DOI] [PubMed] [Google Scholar]
- Sugrue T J. The Origins of the Urban Crisis: Race and Inequality in Postwar Detroit. Princeton, N.J.: Princeton University Press; 1996. [Google Scholar]
- Swinburn B, Egger G, Raza F. Dissecting Obesogenic Environments: The Development and Application of a Framework for Identifying and Prioritizing Environmental Interventions for Obesity. Preventive Medicine. 1999;29:563–70. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- Thomas J M. Redevelopment and Race: Planning a Finer City in Postwar Detroit. Baltimore: Johns Hopkins University Press; 1997. [Google Scholar]
- Travers K D. The Social Organization of Nutritional Inequities. Social Science and Medicine. 1996;43(4):543–53. doi: 10.1016/0277-9536(95)00436-x. [DOI] [PubMed] [Google Scholar]
- Turrini J. Sweet Justice. Michigan History. 1999:22–7. July/August. [Google Scholar]
- U.S. Bureau of the Census. Statistical Abstract of the United States. Washington D.C: 1970. 1980, 1990, 2000. [Google Scholar]
- Wacquant L J D, Wilson W J. The Cost of Racial and Class Exclusion in the Inner City. Annals of the American Academy of Political and Social Science. 1989;501:8–25. [Google Scholar]
- Wallace R. Urban Desertification, Public Health and Public Order: “Planned Shrinkage,” Violent Death, Substance Abuse and AIDS in the Bronx. Social Science and Medicine. 1990;31:801–13. doi: 10.1016/0277-9536(90)90175-r. [DOI] [PubMed] [Google Scholar]
- Whiteis D G. Hospital and Community Characteristics in Closures of Urban Hospitals, 1980–87. Public Health Reports. 1992;107(4):409–16. [PMC free article] [PubMed] [Google Scholar]
- Williams D R. Race/Ethnicity and Socioeconomic Status: Measurement and Methodological Issues. International Journal of Health Services. 1996;26:483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14. [DOI] [PubMed] [Google Scholar]
- Williams D R. Race, Socioeconomic Status and Health: The Added Effects of Racism and Discrimination. Annals of the New York Academy of Sciences. 1999;896:173–88. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams D R. Racial Variations in Adult Health Status: Patterns, Paradoxes, Prospects. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America Becoming: Racial Trends and Their Consequences. Vol. 2. Washington, D.C.: National Academy Press; 2001. pp. 371–410. [Google Scholar]
- Williams D R, Collins C. US Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995;21:349–86. [Google Scholar]
- Williams D R, Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D R, Yu Y, Jackson J, Anderson N B. Racial Differences in Physical and Mental Health: Socioeconomic Status, Stress and Discrimination. Journal of Health Psychology. 1997;2:335–51. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass and Public Policy. Chicago: University of Chicago Press; 1987. [Google Scholar]
- Wilson W J. When Work Disappears: The World of the New Urban Poor. New York: Knopf; 1996. [Google Scholar]
- Zax J S, Kain J F. Moving to the Suburbs: Do Relocating Companies Leave the Black Employees Behind? Journal of Labor Economics. 1996;14(3):472–504. [Google Scholar]


