Abstract
Many studies have explored the extent to which physicians' characteristics and Medicaid program factors influence physicians' decisions to accept Medicaid patients. In this article, we turn to patient race/ethnicity and residential segregation as potential influences. Using the 2000/2001 Community Tracking Study and other sources we show that physicians are significantly less likely to participate in Medicaid in areas where the poor are nonwhite and in areas that are racially segregated. Surprisingly—and contrary to the prevailing Medicaid participation theory—we find no link between poverty segregation and Medicaid participation when controlling for these racial factors. Accordingly, this study contributes to an accumulating body of circumstantial evidence that patient race influences physicians' choices, which in turn may contribute to racial disparities in access to health care.
Keywords: Medicaid, race, physician participation, segregation
The literature documenting racial and ethnic disparities in access to health care in the United States is growing. African Americans and Latinos, for example, are less likely to have a consistent source of care and are more apt to consider the emergency department their medical care home than whites are, even after controlling for sociodemographic differences (Walls, Rhodes, and Kennedy 2002; Weinick, Zuvekas, and Cohen 2000; Zuvekas and Weinick 1999). Minorities also are less likely to use any medical services or to receive preventive care, and their rates of preventable hospitalizations and unmet health needs are substantially higher than those of whites (Gaskin and Hoffman 2000; Hargraves and Hadley 2003; Schneider, Zaslavsky, and Epstein 2002).
The dynamics underlying these disparities are undoubtedly complex. One contributing factor may be physicians' failure to participate in the Medicaid program (Eichner and Vladeck 2005; Rosenbaum 2003). Historically, physicians' participation in Medicaid has been suboptimal. National studies document that between 15 and 30 percent of private physicians do not accept any Medicaid patients and many more limit their participation (Mitchell 1991; Perloff et al. 1997; Sloan, Mitchell, and Cromwell 1978). The potential for limited access is clear: in a recent audit study, callers posing as Medicaid recipients were almost half as likely to be offered an appointment within one week compared with those claiming to have private insurance (Asplin et al. 2005). Minority Americans are disproportionately affected by physicians' limited participation in Medicaid, since African Americans, Latinos, and Native Americans are two and half times more likely to have Medicaid coverage than whites are (Hoffman and Wang 2003).
Another body of research suggests a connection between patient race and physicians' participation in Medicaid.1 This literature explores the influence of residential segregation on physicians' participation in Medicaid. However, as we shall detail here, that empirical work leaves open the question as to whether physicians' participation is linked to residential segregation based on poverty or race and whether the racial composition of the Medicaid population itself matters. For this article, we empirically tested three competing, but not mutually exclusive, hypotheses about physicians' participation in Medicaid as it relates to race, poverty, and segregation. The three hypotheses are as follows:
Physicians are more likely to accept Medicaid patients in areas where the poor are white.
Physicians are less likely to accept Medicaid patients in areas that are more racially segregated.
Physicians are less likely to accept Medicaid patients in areas that are more economically segregated.
Review of the Literature
The Medicaid Segregation Hypothesis
Scholarly research on physicians' Medicaid participation has been heavily influenced by Sloan and colleagues' “two-market demand model” (1978). In this model, physicians prefer to treat private-paying patients until the point at which the marginal revenue in the private market falls below the Medicaid fee. The empirical evidence has generally supported this model. Physicians, for example, are generally more likely to accept Medicaid patients when reimbursements are higher (Adams 1995; Mitchell 1983, 1991; Perloff, Kletke, and Neckerman 1986), with some exceptions (Perloff et al. 1997). Physicians' participation is lower in wealthier communities (Greene, Blustein, and Remler 2005; Perloff, Kletke, and Neckerman 1986; Perloff et al. 1997) and among physicians with stronger credentials (Backus et al. 2001; Margolis et al. 1992; Sloan, Mitchell, and Cromwell 1978).
Contrary to the classic economic expectation, however, in urban areas with greater physician supply, primary care physicians were found to be less likely to participate in Medicaid (Perloff, Kletke, and Neckerman 1986; Sloan, Mitchell, and Cromwell 1978). In a landmark and widely cited paper, Fossett and Peterson (1989) hypothesized that the segregation of Medicaid patients is one dynamic underlying this surprising finding regarding physician supply. Since most physicians' offices in urban areas are located in affluent areas, the residential segregation of Medicaid and private-paying patients would result in many physicians facing low demand from Medicaid patients. Fossett and Peterson argue that physicians in prosperous areas therefore have little ability to increase the demand for Medicaid, short of moving their practice, which in turn would threaten their private-patient base. As a result, the authors hypothesize that whereas physicians in high-income urban areas have few or no Medicaid patients, those in low-income areas have mainly Medicaid patients.
It is noteworthy that Fossett and Peterson's theory invokes income segregation—specifically poverty residential segregation—as the underlying dynamic. That is, poor Medicaid beneficiaries and their wealthier, privately insured counterparts live in different neighborhoods. Their theory does not consider physicians' preference for higher-income patients or concern about “mixing” patients from different socioeconomic classes. Nor does the theory refer to race or ethnicity. This is crucial, for, as we shall note in our review of the empirical literature examining the Medicaid segregation hypothesis, researchers have sometimes measured the impact of poverty segregation on participation. At other times they have tested the impact of racial segregation, and in still other cases they have investigated the impact of racial composition. Therefore, before turning to the empirical evidence that ostensibly supports the theory, we shall examine these distinctions further. In so doing, we draw on some of the broader literature on the relationships among race, residential segregation, and poverty. We believe that this literature—particularly on residential segregation concerning race—may be helpful in understanding physicians' behavior and choices.
Three Important and Sometimes Conflated Distinctions
Race versus Poverty
The first distinction is between race and poverty. Minority groups in the United States are disproportionately poor compared with whites. According to the 2000 census, the proportion of African Americans, Hispanics, Asians, and Native Americans living below the poverty level was 25 percent, 23 percent, 13 percent, and 26 percent, respectively, compared with 9 percent of whites (U.S. Bureau of the Census 2005). This relationship has led some researchers in the Medicaid participation literature to operationalize poverty in terms of race. But race is only a rough a proxy for poverty (Kawachi, Daniels, and Robinson 2005). Together, all minorities constitute less than half the poor population (44 percent), with African Americans making up less than a quarter (24 percent).
Racial versus Economic Residential Segregation
The segregation of both minorities and the poor has been implicated in the development of economically depressed neighborhoods, which in turn limits residents' access to quality jobs, education, safety, social networks, and health care (Charles 2003; Laveist 2003; O'Regan and Quigley 1996; Waitzman and Smith 1998). Although they are related, segregation by poverty and segregation by race differ, are driven by different dynamics, and in fact have only a moderate correlation (Abramson, Tubin, and VanderGood 1995).
Economic segregation is a common feature of American residential life, but because housing is generally viewed as a free-market commodity, segregation based on individuals' willingness and ability to pay is often seen as inevitable and unproblematic. Racial segregation, in contrast, has been driven largely by racism at both the institutional and individual levels (Charles 2003; Massey and Denton 1993; Yinger 1986). This has been repeatedly documented through the use of fair-housing audits (Feins and Bratt 1983; Turner et al. 2002; Yinger 1995), in which two people of different races pose as equally qualified and visit the same real estate agent or landlord in succession. Approximately 15 to 30 percent of the time, African Americans and Hispanics receive less information about available housing units and are invited to inspect fewer apartments and homes than are whites.
The prejudice of real estate agents and landlords may be one explanation for this discrimination. Another is that agents discriminate against minorities because they fear upsetting—that is, violating the norms and expectations of—their white clients. Some evidence supports this explanation. Yinger (1986), for example, found that discrimination was more common in white areas and less evident in areas undergoing racial transition. Another study found that agents were less likely to discriminate against black customers when housing units were far from the agent's office and presumably less visible to white customers (Ondrich, Ross, and Yinger 2001).
Composition versus Segregation
The final distinction is that between composition and segregation, since these, too, have been conflated in the Medicaid physician participation literature. Composition is a population's proportion of individuals with particular characteristics (e.g., 30 percent white or 20 percent low income). Composition is related to segregation in that many measures of segregation compare composition across subunits in a larger geographic unit. For a given geographic unit, however, composition is independent of segregation. An area that is 30 percent African American could be perfectly segregated residentially if all the African Americans in the larger geographic area under study lived in this one geographic subunit—or it could be perfectly integrated if all other subunits in the geographic area also had the same percentage of African Americans.
The literature on composition is less developed than that on segregation. It has shown, however, that whites express higher levels of racial prejudice when minorities make up a greater proportion of the population (Branton and Jones 2005; Oliver and Mendelberg 2000). Furthermore, racial composition appears to influence social policy. Studies over the last twenty-five years have found that those states with a greater percentage of African Americans have stricter welfare sanctions as well as lower income-support levels (Howard 1999; Soss et al. 2003; Wright 1976).
Empirical Studies Addressing the Medicaid Residential Segregation Hypothesis
With these distinctions in mind, we now turn to the body of work supporting the Medicaid segregation hypothesis. We begin with two studies that examined the rates of physicians' participation in Medicaid in one highly segregated metropolitan area: Chicago (Fossett et al. 1990, 1992). Both studies found that physicians were much more likely to participate in Medicaid if they practiced in zip codes with a greater percentage of poor people (i.e., poverty composition) than in areas with lower levels, a finding consistent with the hypothesis. A study by Adams (1995) is the only empirical examination that we found that explicitly investigated whether county physicians' participation rates differed across counties with higher and lower levels of Medicaid patient segregation. Adams found in Tennessee a negative relationship between the even distribution of Medicaid recipients across zip codes in a county and the percentage of that county's physicians participating in Medicaid. While all three studies showed an association between local poverty and physicians' participation in Medicaid, they notably did not control for local racial segregation or for the racial makeup of the Medicaid population itself. Given the substantial correlation between poverty and racial segregation noted earlier, and in view of the current knowledge of the role of patient race in the provision of medical care (discussed later), these are important limitations.
Other studies examining the Medicaid residential segregation hypothesis used composition rather than segregation measures, and/or they used race measures rather than income-based measures.
Studies Using Racial Composition Measures
Several studies examining the Fossett and Peterson explanation measured the racial composition of the physicians' practice community rather than economic segregation (Bronstein, Adams, and Florence 2004; Mitchell 1991; Perloff et al. 1997). Mitchell (1991, 649), for example, used the percentage of the county population that was nonwhite as her measure of residential segregation, noting that “areas with relatively larger nonwhite populations are hypothesized to be more segregated.” Her findings, that the larger the nonwhite proportion was, the less likely physicians were to participate in Medicaid, were interpreted as confirmation of the residential Medicaid segregation hypothesis, yet they seem to implicate patient race in the participation decision.2
The evidence regarding racial composition and physicians' participation in Medicaid is inconsistent, however, likely due to the use of different composition measures (percentage of nonwhites or African Americans) and different ecological units (zip codes, zip code clusters, or counties). In their national study of physicians practicing in metropolitan areas, Perloff and colleagues (1997) employed a narrower racial composition measure: percentage of African Americans living in the practice zip code area. But at the time of the study, blacks made up less than 30 percent of all Medicaid recipients, and only 28 percent of blacks received Medicaid (U.S. Bureau of the Census 1995). Finally, Bronstein and colleagues (2004) also used the percentage of African Americans as their measure, although their geographic region was slightly larger (zip code clusters in Alabama and Georgia). They found that in areas where African Americans made up more than 30 percent of the population, physicians were actually more likely to participate in Medicaid. In sum, the impact of local racial composition on physicians' participation is unclear.
Studies Using Racial Segregation Measures
Perloff and colleagues (1997) described the segregation hypothesis as encompassing both income and racial segregation, since “physicians practicing in more segregated cities will choose to practice in the predominantly white and more prosperous communities and will therefore be significantly less likely to participate in Medicaid than will their counterparts in less racially segregated cities” (Perloff et al. 1997, 147). They tested this proposition by measuring the segregation of blacks (as well as the percentage of blacks in each zip code described earlier). They found that physicians were less likely to participate in Medicaid in urban metropolitan areas where the segregation of African Americans was greatest. They concluded that this finding supported the Fossett and Peterson economic hypothesis, rather than interpreting it as being driven by an inherently racial dynamic.
Studies Using Combined Income and Race-Based Scales
Yet another approach has been used to examine the Medicaid segregation hypothesis. In their 1989 article, Fossett and Peterson examined the influence of a five-item scale measuring physicians' participation in Medicaid. The scale items were residential poverty segregation (dissimilarity), percentage of nonwhite Medicaid recipients, and three other items (including the percentage of the low-income population without access to a car). This and another article (Fossett et al. 1991) found the scale to be negatively associated with physicians' participation in Medicaid. Notably, however, the scale in both studies had a higher loading for the racial composition than for poverty segregation. This again raises the question as to whether it is local patient income or race that influences physicians' decision to participate in Medicaid.
A Notable Void: Studies Examining Patient Race in the Medicaid Participation Decision
Although this reviewed literature examines physicians' participation in Medicaid and the racial segregation and composition of the geographic areas where they practice, it does not directly address the extent to which the racial composition of the Medicaid population might influence their decision to participate. Several of the key researchers in this field, however, have suggested a possible link (Fossett, Chang, and Peterson 1991; Mitchell and Schurman 1984).
Exploring these matters empirically is important given the correlation between race and Medicaid eligibility and in light of the growing recognition of the influence of patient race in medical treatment more generally. Patient race historically has been a key factor determining a person's access to health care in the United States. For example, until the mid-1960s, hospitals were segregated by race, by either law or custom (Smith 1999). The passage of the Civil Rights Act made it illegal for hospitals to segregate explicitly on the basis of race, although they have not yet completely desegregated (Smith 1998). Continued segregation is based partly on the continued residential segregation of racial minorities (Smith 1998). In areas with more geographic racial segregation, like the Northeast and Midwest, minorities and whites often rely on different local hospitals for their care. Finally, in some hospitals, there may be policies that have racial implications. For instance, in the 1990s two hospitals in New York City were cited for segregating their largely minority, Medicaid-covered maternity patients in lesser-quality facilities than those used by predominantly white, privately insured patients (Jones 1993; Sullivan 1994).
Unlike hospitals, doctors' offices are not subject to the Civil Rights Act regulations (Smith 1999). Physicians, therefore, can refuse to treat minority patients or can treat them differently from their white patients (Rosenbaum, Markus, and Darnell 2000), and the degree of segregation in physicians' offices has never been systematically monitored (Smith 2005). A recent study by Bach and colleagues found that blacks and whites usually receive care from different primary care physicians, a finding that the authors attribute primarily to residential racial segregation (Bach et al. 2004; Bach, Schrag, and Pham 2004). But a recent anecdotal report suggests that physicians, too, may segregate their waiting rooms on economic and possibly racial bases (Sachdev 2004).
The Institute of Medicine's Unequal Treatment cites factors attributed to the provider, such as bias, stereotyping, prejudice, and clinical uncertainty, as possibly contributing to the racial disparities in health care (Smedley, Stith, and Nelson 2003). This conclusion, though somewhat controversial (Satel and Klick 2005), is based on research indicating that physicians' decisions seem to be partly influenced by patient race. The strongest such evidence comes from audit studies finding that physicians' treatment recommendations and health assessments are different for black (or black women) patient-actors than they are for white patient-actors presenting with identical symptoms (Rathore et al. 2000; Schulman et al. 1999; Weisse et al. 2001). These research findings agree with popular perceptions: national survey results show that approximately one-third of physicians and almost half of adults in the United States believe that the health care system often treats people unfairly “based on what their race or ethnic background is” (Kaiser Family Foundation 2002, chart 2).
In sum, the literature on physicians' participation in Medicaid often touches on race and segregation but does not consistently differentiate between residential racial and economic segregation. Nor has it systematically addressed the possible influence of Medicaid patient race. This article contributes to the literature by testing the three different physician participation hypotheses cited at the outset. All the hypotheses are plausible in view of the empirical and theoretical notions just reviewed and are not mutually exclusive. By testing all three simultaneously within the same source of data, we weighed the evidence supporting these various alternative (and likely correlated) explanations for physicians' behavior.
Methods
Data Sources
We used two primary sources of data in this cross-sectional study, the Community Tracking Study Physician Survey (CTS), which provides physician-level data on Medicaid participation, and U.S. Census 2000 data for county-level race and poverty composition and segregation measures.
The CTS is a large, nationally representative telephone survey of physicians. The sample was drawn from the master files of the American Medical Association and the American Osteopathic Association and excludes federally employed physicians, those outside the continental United States, and those in training. More than 10,000 physicians in twenty-five states (and 422 counties) were surveyed. We used the 2000/2001 survey, which had a response rate of 59 percent. More extensive details on the design of the CTS have been published previously (Kemper et al. 1996). The restricted version of the CTS includes the county where each physician practices, which enabled us to merge it with census and other data sources, described next.
The 2000 census data were our other major source for this study. Summary file 1, which is a 100 percent file, provided race data at the census track and county levels for calculating racial residential segregation. Summary file 3, which is based on a sample of 16 percent of the population, provided poverty data at the census track and county levels for calculating poverty segregation and county data based on the percentage of the poor nonwhite population.
We used additional sources of data for several covariates, all of which we describe in more detail. These included the Medicare/Medicaid reimbursement ratio (Menges et al. 2001), the percentage of the county's population receiving Medicaid and the county-level Medicaid managed care penetration rate (Greene, Blustein, and Remler 2005), the ratio of physicians to population (U.S. Department of Health and Human Services 2002), and a measure of Medicaid program hassle (Berman et al. 2002). The Medicaid program hassle measure is the percentage of pediatricians surveyed in each state citing Medicaid paperwork concerns as a “very important” factor for limiting or not participating in Medicaid.
Sample
All physicians in the CTS, with the exception of psychiatrists, were included in the study sample if they practiced in metropolitan statistical areas (MSAs) and accepted new patients. We included only providers practicing in MSAs because Fossett and Peterson's Medicaid segregation theory (1989) was developed to address the phenomenon of physicians' having low participation rates in urban areas. We excluded physicians with closed practices (accounting for 3 percent of the sample) because of their unwillingness to accept Medicaid patients, regardless of the local population's characteristics. Unlike some earlier studies of physicians' participation in Medicaid, we did include institutional providers—those working in hospitals, clinics, and medical schools—as well as office-based providers in order to examine the availability of all physicians to the Medicaid population. The findings of models that excluded institutional providers were similar to those presented here. As expected, institutional providers were much more likely overall to accept Medicaid patients than were office-based providers (92 percent versus 78 percent). The final study sample was 9,178 physicians, 65 percent of whom were primary care providers. Because we were missing data for some Medicaid variables, our multivariate analyses used a smaller sample of 8,582 (reduction of 6.5 percent).
Measures
Acceptance of New Medicaid Patients
The dependent variable used in this study was whether or not a physician accepted new Medicaid patients. The CTS asked the physicians: “Is the practice accepting all, most, some, or no new patients who are insured through Medicaid, including Medicaid managed care patients?” We then created a dichotomous version of this variable for our analysis, contrasting those physicians accepting any Medicaid patients with those accepting none. This measure was used in a recent study of physicians' participation in Medicaid (Greene, Blustein, and Remler 2005). We repeated our analyses using two alternative measures of physicians' participation. These measures, which differed in the extent of participation, were (1) having at least 1 percent revenue from Medicaid and (2) accepting all new Medicaid patients versus those accepting none, some, or most. According to these definitions, 85 percent and 51 percent of physicians participated in Medicaid, respectively, compared with 81 percent from our primary measure. The patterns reported here for our chosen measure were substantially replicated when repeated with these alternative measures.
Level of Aggregation of Ecologic Variables
The study's unit of analysis was the individual physician who participated in the CTS. However, in accordance with the theory developed earlier, we wanted to measure the independent variables of interest at the level of geographical aggregation that would be expected to influence a physician's decision to participate in Medicaid. Our choice of the county as the ecological unit reflects a practical constraint: the CTS does not include information about practice location at a geographically lower level of aggregation. Beyond practical considerations, however, the county seemed to be a plausible choice for at least two reasons. First, most of the earlier studies in the field used the county as the ecological unit, including the original Fossett and Peterson paper. Second, the appropriate unit is probably much larger than the zip code or census tract. For instance, with respect to the second hypothesis, recent analyses suggest that primary care physicians typically attract patients, including lower-income and Medicaid patients, from areas that span substantial distances, generally multiple zip codes or three miles, on average (Goodman et al. 2003; Guagliardo et al. 2004; Shannon, Bashur, and Spurlock 1978). The expectation used by primary care health planners in the Medicaid program is thirty minutes of travel to primary care (Rosenbaum, Stewart, and Sonosky 2002). In short, when physicians consider who might appear in their waiting rooms if offered financial access, they are likely to be thinking about people living well beyond their immediate practice neighborhood.
Racial Composition of the Medicaid Population
Since the racial breakdown of the Medicaid population is not available at the county level, we used as a proxy measure the racial makeup of those with incomes below the federal poverty level. We believe that this is a reasonable proxy: whereas the income requirements for Medicaid eligibility extend above the poverty line, the racial makeup of the near-poor is similar to that of the poor (Lillie-Blanton, Martinez, and Salganicoff 2001). Our measure was the percentage of the poor population in a county that was white, and our definition of white was those who identified their race as “white” and were not Hispanic. Conversely, nonwhites in this study include all “people of color,” including African Americans, Latinos, Asians, and Native Americans.
Measures of Residential Segregation
We used the dissimilarity index to measure both poverty and racial residential segregation. The dissimilarity measure is the most commonly used measure of segregation (Acevedo-Garcia et al. 2003) and the one that was used in most of the earlier studies of Medicaid participation and segregation. It measures “evenness,” or how consistently a subgroup (e.g., those below the federal poverty level or the nonwhite population) is spread across the separate areal units in a larger geographic area (for the formula, see the appendix 1). The dissimilarity index can range from 0 to 1. A value of 0 indicates total integration, in which subgroup members are evenly spread across all the areal units in the larger geographic area, and a value of 1 indicates complete segregation, in which all subgroup members are clustered in one areal unit. The dissimilarity value is commonly interpreted as the proportion of subgroup members that would have to move in order to achieve even distribution across the larger geographic area. For instance, a value of .6, which is considered the threshold for a ghetto (Cutler, Glaeser, and Vigdor 1999), means that 60 percent of the subgroup of interest (in this case, the black population) would need to move in order to be evenly distributed throughout the larger geographic area.
Control Variables
The control variables in our multivariate analyses fall into three categories: physician and practice characteristics, Medicaid program characteristics, and county characteristics. The first group, physician and practice characteristics, includes the physician's age, gender, race, type of physician (internist, pediatrician, family practice/general, medical specialist, surgical specialist, obstetrician/gynecologist), board certification (certified or eligible versus neither), place of medical school graduation (U.S. versus foreign medical school), and type of practice (office-based versus institutional). The Medicaid program characteristics include the Medicaid/Medicare reimbursement ratio, which is the average ratio for thirty-one common CPT codes for the Medicaid population; a Medicaid program hassle factor; the county Medicaid managed care penetration rate; and the percentage of the county's population receiving Medicaid. The two county characteristics included in the study are the county's per capita income and physician density (primary care physician to patient ratio and specialty care physician to patient ratio, respectively, in the primary care and specialty multivariate models).
Analytical Approach
We began our analysis by profiling the urban physicians in the 2000/2001 CTS sample. We then explored in bivariate analysis the extent to which each of the three independent variables (percentage of poor that are white, racial segregation, and poverty segregation) were associated with physicians' participation in Medicaid. We categorized the independent variables into rounded quartiles to allow for nonlinear relationships in both the bivariate and the multivariate models. We stratified these analyses to examine the relationships separately for primary care and specialty physicians because of their historically different patterns of Medicaid participation (Mitchell 1983, 1991; Sloan, Mitchell, and Cromwell 1978) and because the original Fossett and Peterson (1989) theory pertained to primary care physicians. We also stratified the bivariate analyses by the physicians' race. We did this because earlier research indicated that physicians of color were more likely to participate in Medicaid and to care for minority and poor populations in general (Backus et al. 2001; Komaromy et al. 1996; Moy and Bartman 1995; Perloff et al. 1997); thus physicians of color may exhibit different patterns of Medicaid participation as related to our independent variables. Unfortunately, because of our relatively small samples of African American and Hispanic physicians, we were not able to conduct multivariate analyses by physicians' race.
In order to test further the three hypotheses in this study, we built a series of multivariate logistic regression models. We first tested each key independent variable separately in a reduced form model that included the control variables. Then we estimated full models that simultaneously included the three key independent variables as well as the controls. That model took the following form:
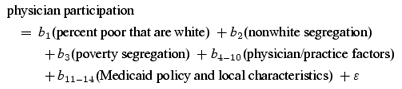
The first hypothesis, that physicians are more likely to treat Medicaid patients when the poor are white, would be supported if the odds ratio for b1 were greater than 1. An odds ratio of less than 1 for b2 would be consistent with the second hypothesis, that physicians are more likely to treat Medicaid patients in areas with little racial segregation. Finally, an odds ratio of less than 1 for b3 would be consistent with the third hypothesis, that physicians are more likely to treat Medicaid patients in areas of little poverty segregation. To facilitate the interpretation of the odds ratios for our key findings, we calculated predicted probabilities of participating in Medicaid at specific values for the independent variables, holding control variables at their means.
Since the CTS used a complex sampling scheme, all analyses were conducted using SUDAAN software. This enabled us to adjust the estimates to be representative of physicians nationally and also to correct the standard errors to account for the without-replacement, stratified, and clustered sampling design.
Findings
Urban physicians in 2000/2001 were overwhelmingly male, white, and between the ages of thirty-five and fifty-four (table 1). The majority were specialists (61 percent), and almost all (86 percent) were board certified or eligible. The Medicaid program characteristics varied substantially for physicians across the country. For most, Medicaid reimbursement rates were generally low relative to Medicare rates. Twenty percent of the physicians practiced in areas where reimbursement was less than 65 percent of Medicare rates, and a quarter of the physicians practiced in areas with ratios of 80 percent or higher. One-quarter of the physicians practiced in counties that offered no Medicaid managed care, while 41 percent practiced in counties where at least half the Medicaid recipients were enrolled in managed care. There also were large ranges in level of Medicaid hassle as well as the percentage of county population receiving Medicaid.
TABLE 1.
Description of Urban Physicians from the Community Tracking Study, 2000/2001
| Percentage of Physicians (n= 9,178) | |
|---|---|
| Physician and Practice Characteristics | |
| Age | |
| <35 | 8.4 |
| 35–44 | 36.5 |
| 45–54 | 35.2 |
| 55–64 | 15.0 |
| 65+ | 4.9 |
| Gender | |
| Female | 23.7 |
| Male | 76.3 |
| Race | |
| White (non-Hispanic) | 76.1 |
| Asian | 12.4 |
| African American | 3.4 |
| Hispanic | 5.5 |
| Other | 2.7 |
| Type of physician | |
| Internist | 14.9 |
| Pediatrician | 8.7 |
| Family practice/general practice | 15.0 |
| Medical specialist | 33.6 |
| Surgical specialist | 20.8 |
| Obstetrician/gynecologist | 7.0 |
| Board certification | |
| Certified or eligible | 85.8 |
| Neither | 14.2 |
| Medical school | |
| United States | 78.4 |
| Foreign | 21.6 |
| Type of practice | |
| Office-based | 75.0 |
| Institutional | 25.0 |
| Medicaid Characteristics | |
| Medicaid/Medicare reimbursement ratio | |
| <65% | 19.9 |
| 65%–<80% | 54.4 |
| 80%+ | 25.8 |
| Medicaid hassle factora | |
| Low (<35%) | 40.7 |
| Medium (35%–<45%) | 22.8 |
| High (45%+) | 36.5 |
| Percentage of county population receiving Medicaid | |
| <10% | 41.4 |
| 10%–<15% | 30.1 |
| 15%+ | 28.5 |
| Medicaid managed care penetration rate | |
| 0% | 24.5 |
| >0%–<25% | 12.0 |
| 25%–<50% | 22.4 |
| 50%+ | 41.2 |
Percentages of pediatricians surveyed in a given state reporting that Medicaid paperwork was “very important” in their decision to limit or not participate in Medicaid (Berman et al. 2002).
Most urban physicians (81 percent) participated in Medicaid (table 2), although specialists were much more likely to participate than primary care physicians were (84 percent versus 75 percent). The differences in participation level by physicians' race were considerable. Black and Asian physicians were, respectively, 10 and 7 percentage points more likely to participate in Medicaid than whites were, whereas Latinos were slightly less likely to participate.
TABLE 2.
Bivariate Relationships between the Ecological Measures and Urban Physician Participation in Medicaid, by Physician's Practice Type and Race
| Percentage of Physicians Participating in Medicaid | |||||||
|---|---|---|---|---|---|---|---|
| Physician Type | Physician Race | ||||||
| All Physicians (n= 9,178) | Primary Care (n= 5,937) | Specialist (n= 3,241) | White (n= 6,863) | Asian (n= 1,163) | Black (n= 374) | Latino (n= 551) | |
| All Physicians | 80.7 | 75.1 | 84.3 | 79.6 | 87.0 | 89.6 | 78.4 |
| Percentage of the Poor That Are White | |||||||
| <25% (group 1) | 72.2c | 69.6a | 73.9c | 67.8c | 80.7b | 81.6 | 81.5 |
| 25%–<45% | 81.2 | 75.4 | 84.7 | 80.0 | 88.7 | 95.4 | 70.9 |
| 45%–<65% | 82.1 | 75.7 | 85.9 | 81.6 | 88.2 | 91.0 | 82.5 |
| 65%+ (group 4) | 88.1 | 79.9 | 94.4 | 86.8 | 91.7 | d | d |
| Difference in participation rates (group 4 − group 1) | 15.9 | 10.3 | 20.5 | 19.0 | 11.0 | n/a | n/a |
| Racial Segregatione | |||||||
| <.35 (group 1) | 82.1 | 76.5 | 87.7a | 81.0 | 83.9a | d | 83.9b,f |
| .35–<.45 | 83.3 | 75.8 | 87.9 | 81.4 | 91.6 | 93.1f | 91.3f |
| .45–<.55 | 79.2 | 72.9 | 82.4 | 79.3 | 85.1 | 83.4 | 70.8 |
| .55+ (group 4) | 79.6 | 76.0 | 81.8 | 77.2 | 87.5 | 93.1 | 85.1f |
| Difference in participation rates (group 4 − group 1) | −2.5 | −0.5 | −5.9 | −3.8 | 3.6 | n/a | 1.2 |
| Poverty Segregatione | |||||||
| <.25 (group 1) | 84.1a | 77.0 | 89.9b | 82.6 | 91.8a | d | d |
| .25–<.33 | 80.9 | 78.2 | 82.6 | 80.0 | 84.7 | 92.2 | 80.8 |
| .33–<.37 | 76.8 | 67.6 | 81.7 | 76.1 | 83.1 | 79.0f | 70.3 |
| .37+ (group 4) | 83.1 | 77.1 | 86.8 | 81.2 | 91.6 | 93.4 | 85.9f |
| Difference in participation rates (group 4 − group 1) | −1.0 | 0.1 | −3.1 | −1.4 | −0.2 | n/a | n/a |
p < .05.
p < .01.
p < .001.
Category combined with adjacent category because fewer than 50 physicians.
Segregation is measured using the dissimilarity index, which can be interpreted as the percentage of the subgroup (nonwhites or poor population in racial and poverty segregation, respectively) that would need to move in order to be evenly spread across the zip codes in the county.
Fewer than 100 physicians in race/income category.
We observed a strong bivariate relationship between the racial composition of the county's poor population and physicians' participation in Medicaid (table 2). In counties whose poor were mainly white, physicians were much more likely to participate in Medicaid, providing preliminary support for the first hypothesis. Specifically, 72 percent of physicians practicing in counties whose poor population was in the quartile with the fewest whites (<25 percent white) participated in Medicaid, compared with 88 percent of physicians practicing in counties whose vast majority of poor were white (65 percent or more), a difference of 16 percentage points. The percentage point difference in participation across the range in “percentage of poor that are white” was twice as great for specialists as for primary care physicians (21 versus 10 percentage points). We also observed differences in the relationship as a function of the physicians' race. White physicians' participation was most sensitive to the racial composition of the poor, followed by that of Asian physicians. Notably, no such sensitivity was found for black or Latino physicians.
In contrast to the strong relationship observed for the first hypothesis, we found less evidence supporting the second hypothesis in table 2. Segregation of nonwhites did not exhibit a consistent pattern with physicians' participation in Medicaid. Specialist physicians had a negative relationship between segregation and Medicaid participation, but primary care physicians did not. Asian physicians exhibited the opposite pattern; they were more likely to participate in Medicaid in highly segregated counties.
Nor did we observe strong support for the third hypothesis. The relationship between poverty segregation levels and physician participation is “U” shaped rather than monotonic. Consequently, physicians' participation levels were the highest for physicians practicing in counties of very low and very high poverty segregation, and those practicing in moderately segregated counties participated less.
Table 3 emphasizes the substantial correlations among the independent variables of interest. In contrast, the three variables show relatively little linear correlation with the physician acceptance variable, consistent with table 2.
TABLE 3.
Correlations between Ecological Measures and Urban Physicians' Participation in Medicaid (n= 9,178)
| Medicaid Participation | Percentage of the Poor That Are White | Racial Segregation | Poverty Segregation | |
|---|---|---|---|---|
| Medicaid participation | 1.00 | |||
| Percentage of the poor that are white | 0.12a | 1.00 | ||
| Racial segregation | −0.06 | −0.63a | 1.00 | |
| Poverty segregation | −0.06 | −0.45a | 0.71a | 1.00 |
p < .001.
Table 4 presents multivariate models corresponding to each of the three hypotheses individually and then in combination. Controlling for potential confounders, we continued to observe support for the first hypothesis (columns 1 and 2). We found more support for the second hypothesis in the multivariate model for primary care providers (column 3) than in the bivariate analyses, with those practicing in the most racially integrated counties being more willing to take Medicaid patients than those practicing in more segregated counties. And our findings for poverty segregation (the third hypothesis) again showed the nonmonotonicity seen in the bivariate findings, with those physicians practicing in moderately economically segregated counties being the least likely to participate in Medicaid (columns 5 and 6).
TABLE 4.
Key Odds Ratios from Multivariate Models Predicting Urban Physicians' Participation in Medicaid
| Percentage of the Poor That Are White | Racial Segregation | Poverty Segregation | Full Model | |||||
|---|---|---|---|---|---|---|---|---|
| (1) Primary Care Physicians (n= 5,551) | (2) Specialist Physicians (n= 3,031) | (3) Primary Care Physicians (n= 5,551) | (4) Specialist Physicians (n= 3,031) | (5) Primary Care Physicians (n= 5,551) | (6) Specialist Physicians (n= 3,031) | (7) Primary Care Physicians (n= 5,551) | (8) Specialist Physicians (n= 3,031) | |
| Percentage of the Poor That Are White | ||||||||
| <25% | (1.00) | (1.00) | (1.00) | (1.00) | ||||
| 25%–<45% | 1.42a | 1.26 | 1.21 | 1.01 | ||||
| 45%–<65% | 1.46a | 1.35 | 1.32b | 1.20 | ||||
| 65%+ | 2.06c | 4.87c | 1.83a | 4.36c | ||||
| Racial Segregationd | ||||||||
| <.35 | (1.00) | (1.00) | (1.00) | (1.00) | ||||
| .35–<.50 | 0.66a | 0.99 | 0.65a | 0.86 | ||||
| .50–<.60 | 0.63a | 0.63e | 0.87 | 0.83 | ||||
| .60+ | 0.64a | 0.80 | 0.79 | 0.51e | ||||
| Poverty Segregationd | ||||||||
| <.25 | (1.00) | (1.00) | (1.00) | (1.00) | ||||
| .25–<.33 | 0.90 | 0.61e | 1.13 | 0.83 | ||||
| .33–<.37 | 0.52c | 0.52a | 0.73e | 0.96 | ||||
| .37+ | 0.78 | 0.96 | 1.12 | 2.13e | ||||
All models control for physician and practice characteristics (age, gender, race, type of physician, board certification, place of medical school graduation, type of practice), Medicaid characteristics (Medicaid/Medicare reimbursement ratio, Medicaid hassle factor, percentage of county population receiving Medicaid, Medicaid managed care penetration), and county characteristics (per capita income, primary care or specialty physician/population ratio).
p < .01.
p < .10.
p < .001.
Segregation is measured using the dissimilarity index, which can be interpreted as the percentage of the subgroup (nonwhites or poor population in racial and poverty segregation, respectively) that would need to move in order to be evenly spread across the zip codes in the county.
p < .05.
The final two models presented in table 4 isolate the independent effect of each of the three ecological independent variables, holding the others constant. While the odds ratios for “percentage of poor that are white” were slightly attenuated, they remained significant in both primary care and specialty models (columns 7 and 8), thereby implicating the racial composition of the poor as a factor in physicians' decisions to participate in Medicaid. Translating the final set of odds ratios into predicted probabilities of participation, we estimated that primary care physicians in counties whose poor population was mostly white (the highest quartile) were 11 percentage points more likely to participate in Medicaid than were those in the counties in the lowest quartile (83 percent versus 72 percent). The difference was of the same magnitude for specialist physicians (97 percent versus 86 percent).
In the final model we also found some evidence for the second hypothesis. In highly racially segregated counties, physicians, particularly specialists, were less likely to participate in Medicaid. Specifically, the predicted probability of participation in the least segregated quartile of counties was 91 percent, compared with 84 percent in the most segregated quartile of counties. Finally—and notably—we found little consistent support for the third hypothesis. In the areas of greatest poverty segregation, physicians were either equally likely (primary care physicians) to participate in Medicaid or more likely (specialists) than in integrated counties.
The relationships between the model's covariates and physician participation were generally as expected. In both the primary care and specialist models, African American and Asian physicians were more likely to participate in Medicaid than white physicians were. Those practicing in institutional settings, in lower-income counties, and in states with higher Medicaid/Medicare reimbursement rates were also more likely to participate in Medicaid.
In sum, when we controlled for the highly correlated independent variables, we found that physicians' reluctance to participate in Medicaid was concentrated in areas where the poor were nonwhite and where the nonwhite were segregated. This was true for both primary care and specialist physicians. However, we did not find decreased participation to be concentrated in areas of high poverty segregation. In fact, for specialist physicians, we observed the opposite pattern, that they were more likely to participate in Medicaid if they practiced in highly economically segregated counties.
Discussion
To date, studies of physicians' participation in Medicaid have generally been interpreted as supporting the Medicaid (poverty) segregation hypothesis. This hypothesis says that in economically segregated urban areas, physicians are less likely to accept Medicaid patients because of the combination of low Medicaid demand and practice economics. At the same time, this literature has suggested that racial segregation and/or composition also influence the participation decision. But as reviewed here, none of the studies ostensibly supporting the Medicaid (poverty) segregation hypothesis controlled for these race-related factors. In this article, we explored what happened to the poverty segregation factor when we controlled for local racial factors. Under these circumstances, we found that poverty segregation had a substantially attenuated effect on participation. This is one contribution of our work.
We also documented that local race-related factors exhibited robust relationships with physicians' participation in Medicaid, even when controlling for poverty segregation. Physicians' inclination to participate in Medicaid is influenced by the race of the local Medicaid population and also by the local racial segregation patterns. When the poor population was composed of a greater proportion of non-Hispanic whites, primary care and specialty physicians were more likely to participate in Medicaid. The effect of the racial makeup of the local poor was quite large: physicians were 11 percentage points more likely to participate in Medicaid if they practiced in a county with the highest quartile of “percentage of the poor that are white,” compared with those practicing in the lowest quartile. In addition, our findings point to a role for local racial segregation. Physicians were several percentage points less likely to participate in Medicaid in counties with the highest level of white/nonwhite residential segregation.
Thus, this study has contributed to the accumulating body of circumstantial evidence that patient race influences physicians' choices and behaviors. Most of the earlier research in this field concentrated on differences in communication, diagnosis, and treatment (Cooper-Patrick et al. 1999; Johnson et al. 2004; Schulman et al. 1999). In this study we found that patient race also appears to influence access to physicians. This raises the question as to why patient race and/or local segregation patterns should influence physicians' decisions to participate in Medicaid. Certainly race, racism, and segregation are pervasive features of American social life, influencing employment, housing, education, and medical care. We believe it therefore would be surprising if physicians' decisions to participate in Medicaid were free of racial considerations.
How the reported patterns of physicians' participation influence disparities in access to care for Medicaid recipients needs to be investigated further. It is notable that almost half of all people of color living below the poverty threshold reside in counties where less than 25 percent of the poor are white. At a minimum we would expect that Medicaid recipients in these counties, as well as those residing in highly segregated counties, would have more difficulty finding a physician willing to accept Medicaid coverage. It is also quite plausible that Medicaid recipients in these counties experience more restricted overall access to physicians.
Although our study does not address the dynamics underlying the observed patterns, we can offer two possible scenarios. First, we would expect fewer physicians to participate in Medicaid in areas where the poor are nonwhite if the physician's racial bias or stereotyping influenced his or her decision to participate in Medicaid. This does not necessarily imply intentional or conscious discrimination against minority Medicaid patients. Rather, physicians, like all people, are likely to feel most comfortable interacting with people who are like them (Burgess, Fu, and van Ryn 2004; van Ryn and Burke 2000). To the extent that most physicians are white, they may be more motivated to care for the poor when the poor also are white.
Second, the findings related to lower participation levels in highly racially segregated areas are consistent with physicians' concern about “mixing” white, privately insured patients with minority Medicaid patients. Like real estate agents working in prejudiced communities who discriminate against minorities in order to avoid alienating white clients, physicians may be less inclined to participate in Medicaid in highly segregated areas because of the perception (real or otherwise) that their established patients would be uncomfortable sharing the waiting room with low-income minority patients. Clearly, more work is needed to ascertain the dynamics underlying the patterns described here.
Our findings do point to one approach to improving physicians' participation for minority Medicaid recipients: increasing the pool of minority physicians. As we showed, African American and Asian physicians were more likely than white physicians to participate in Medicaid. Furthermore, minority physicians were more likely than whites to participate in Medicaid in counties where most of the poor were nonwhite and in areas that had high levels of racial segregation. This finding is consistent with earlier studies showing that minority physicians are generally more likely to treat low-income and minority patients (Komaromy et al. 1996; Moy and Bartman 1995). Over the last five years, however, even though the number of Asian physicians has risen, the number of African American and Hispanic medical school graduates has dropped (Association of American Medical Colleges 2005). In order to increase the percentage of minority physicians, policymakers will need to raise, rather than cut, funding for training minority physicians (Pear 2004).
Our findings should be interpreted in light of several limitations. The first is that the described associations draw on county-level measures and thus are prone to the ecological fallacy. Those physicians who do not participate in Medicaid in highly nonwhite poor counties may not actually be located in areas where the nonwhite poor population lives and seeks medical care. Likewise, the nonparticipating physicians in counties with high levels of racial segregation may practice in more integrated areas. As we have discussed, it is not clear what ecological unit of measurement would be most appropriate to resolve this issue. It is even possible that the appropriate ecological unit should be larger than the county. More precise physician location information would enable testing areal factors at various levels of aggregation.
Second, our study may also have understated the influence of race-related factors on physicians' participation in Medicaid. It is possible that physicians who accept some, but not all, Medicaid patients may limit participation based on patients' race, but it was beyond the scope of this study to test this possibility. In addition, some physicians only accept Medicaid coverage for already established patients who have fallen on hard times, and this could differentially influence white and nonwhite Medicaid recipients. Audit studies similar to those conducted in the housing field could address these possibilities.
Our study was also limited by its cross-sectional design and consequently the potential for omitted variables bias. Given that the areal variables of interest change slowly over time, a more sophisticated design (e.g., a panel approach) was not feasible. The study used several controls for Medicaid program characteristics, including reimbursement rates, perceived Medicaid program hassle factor, and Medicaid managed care penetration. But it did not include information about the factors motivating physicians' practice location choices, which may be correlated with their inclination to accept Medicaid patients. It bears noting that some of those factors may include racial attitudes and practices.
Finally, our measure of participation in Medicaid was based on self-report. Even though self-reported measures of participation in Medicaid have been shown to overstate physician participation, the correlation between participation measured by self-reported and aggregated patient records has been found to be very high (Kletke et al. 1985).
While these limitations are important, this study is the only one testing the Medicaid segregation hypothesis against rival race-based explanations for lower physician participation in urban areas. Our work does not support the widely accepted Medicaid segregation hypothesis. Rather, we found that urban physicians are more likely to participate in Medicaid in counties whose poor are white and in areas that are racially integrated. Although our study perhaps raises more questions than it answers, it underscores the importance of examining the influence of race and residential segregation on future studies of physicians' participation in Medicaid and, more broadly, in studies of Medicaid recipients' access to care.
Appendix: Formula for Dissimilarity
For poverty (racial) dissimilarity, ti is the total population of census tract i; pi is the proportion of the census tract population with incomes below the poverty threshold (nonwhite); T is the population size of the county; and P is the proportion of the county population with incomes below the poverty threshold (nonwhite).
Endnotes
In the United States, minority populations differ from the majority white population in terms of race (e.g., African American or Asian) and ethnicity (e.g., Hispanic). In this article, for the sake of parsimony, we use the term race to refer to both race and ethnicity.
For completeness, we should mention a study conducted before the Fossett and Peterson work. Mitchell and Schurman (1984) found that Medicaid participation was lower among obstetricians and gynecologists practicing in counties with a greater minority population, although this was not the case for pediatricians or general surgeons. At that time, Mitchell and Schurman interpreted those results as suggesting racial discrimination against minority Medicaid patients.
References
- Abramson A, Tubin M, VanderGood M. The Changing Geography of Metropolitan Opportunity: The Segregation of the Poor in U.S. Metropolitan Areas, 1970 to 1990. Housing Policy Debate. 1995;6(1):45–72. [Google Scholar]
- Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future Directions in Residential Segregation and Health Research: A Multilevel Approach. American Journal of Public Health. 2003;93(2):215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams EK. Effect of Increased Medicaid Fees on Physician Participation and Enrollee Service Utilization in Tennessee, 1985–1988. Inquiry. 1995;31(2):173–87. [PubMed] [Google Scholar]
- Asplin BR, Rhodes KV, Levy H, Lurie N, Crain AL, Carlin BP, Kellermann AL. Insurance Status and Access to Urgent Ambulatory Care Follow-up Appointments. Journal of the American Medical Association. 2005;294(10):1248–54. doi: 10.1001/jama.294.10.1248. [DOI] [PubMed] [Google Scholar]
- Association of American Medical Colleges. Minorities in Medical Education: Facts & Figures 2005. [accessed September 6, 2005]. https://services.aamc.org/Publications Available at.
- Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary Care Physicians Who Treat Blacks and Whites. New England Journal of Medicine. 2004;351(6):575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- Bach P, Schrag D, Pham H. Authors Reply: Primary Care Physicians Who Treat Blacks and Whites. New England Journal of Medicine. 2004;351(20):2127. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- Backus L, Osmond D, Grumbach K, Vranizan K, Phuong L, Bindman AB. Specialists' and Primary Care Physicians' Participation in Medicaid Managed Care. Journal of General Internal Medicine. 2001;16(12):815–21. doi: 10.1111/j.1525-1497.2001.01239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman S, Dolins J, Tang SF, Yudkowsky B. Factors That Influence the Willingness of Private Primary Care Pediatricians to Accept More Medicaid Patients. Pediatrics. 2002;110(2):239–48. doi: 10.1542/peds.110.2.239. part 1. [DOI] [PubMed] [Google Scholar]
- Branton R, Jones B. Reexamining Racial Attitudes: The Conditional Relationship between Diversity and Socioeconomic Environment. American Journal of Political Science. 2005;49(2):359–72. [Google Scholar]
- Bronstein JM, Adams EK, Florence CS. The Impact of S-CHIP Enrollment on Physician Participation in Medicaid in Alabama and Georgia. Health Services Research. 2004;39(2):301–17. doi: 10.1111/j.1475-6773.2004.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess D, Fu S, van Ryn M. Why Do Providers Contribute to Disparities and What Can Be Done about It? Journal of General Internal Medicine. 2004;19(11):1154–59. doi: 10.1111/j.1525-1497.2004.30227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles C. The Dynamics of Racial Residential Segregation. Annual Review of Sociology. 2003;29:167–207. [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, Gender, and Partnership in the Patient-Physician Relationship. Journal of the American Medical Association. 1999;282(6):583–89. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Cutler D, Glaeser E, Vigdor J. The Rise and Decline of the American Ghetto. Journal of Political Economy. 1999;107(3):455–506. [Google Scholar]
- Eichner J, Vladeck BC. Medicare as a Catalyst for Reducing Health Disparities. Health Affairs. 2005;24(2):365–75. doi: 10.1377/hlthaff.24.2.365. [DOI] [PubMed] [Google Scholar]
- Feins J, Bratt R. Barred in Boston: Racial Discrimination in Housing. Journal of the American Planning Association. 1983;43(3):344–55. [Google Scholar]
- Fossett J, Chang H, Peterson J. Hospital Outpatient Services and Medicaid Patients' Access to Care. Medical Care. 1991;29(10):964–76. doi: 10.1097/00005650-199110000-00003. [DOI] [PubMed] [Google Scholar]
- Fossett JW, Perloff JD, Kletke PR, Peterson JA. Medicaid Patients' Access to Office-Based Obstetricians. Journal of Health Care for the Poor and Underserved. 1991;1(4):405–21. doi: 10.1353/hpu.2010.0044. [DOI] [PubMed] [Google Scholar]
- Fossett JW, Perloff JD, Kletke PR, Peterson JA. Medicaid and Access to Child Health Care in Chicago. Journal of Health Politics, Policy and Law. 1992;17(2):273–98. doi: 10.1215/03616878-17-2-273. [DOI] [PubMed] [Google Scholar]
- Fossett JW, Perloff JD, Peterson JA, Kletke PR. Medicaid in the Inner City: The Case of Maternity Care in Chicago. The Milbank Quarterly. 1990;68(1):111–41. [PubMed] [Google Scholar]
- Fossett J, Peterson J. Physician Supply and Medicaid Participation: The Causes of Market Failure. Medical Care. 1989;27(4):386–96. doi: 10.1097/00005650-198904000-00006. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Hoffman C. Racial and Ethnic Differences in Preventable Hospitalizations across 10 States. Medical Care Research and Review. 2000;57(suppl. 1):85–107. doi: 10.1177/1077558700057001S05. [DOI] [PubMed] [Google Scholar]
- Goodman DC, Mick SS, Bott D, Stukel T, Chang CH, Marth N, Poage J, Carretta HJ. Primary Care Service Areas: A New Tool for the Evaluation of Primary Care Services. Health Services Research. 2003;38(1, part 1):287–309. doi: 10.1111/1475-6773.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J, Blustein J, Remler D. The Impact of Medicaid Managed Care on Primary Care Physician Participation in Medicaid. Medical Care. 2005;43(9):911–20. doi: 10.1097/01.mlr.0000173598.85217.7f. [DOI] [PubMed] [Google Scholar]
- Guagliardo M, Ronzio C, Cheung I, Chacko E, Joseph J. Physician Accessibility: An Urban Case Study of Pediatric Providers. Health and Place. 2004;10(3):273–83. doi: 10.1016/j.healthplace.2003.01.001. [DOI] [PubMed] [Google Scholar]
- Hargraves JL, Hadley J. The Contribution of Insurance Coverage and Community Resources to Reducing Race Disparities in Access to Care. Health Services Research. 2003;38(3):809–29. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman C, Wang M. Health Insurance Coverage in America. [accessed September 5, 2005]. http://www.kff.org/uninsured/4154.cfm Available at.
- Howard C. The American Welfare State, or States? Political Research Quarterly. 1999;52(2):421–42. [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient Race/Ethnicity and Quality of Patient-Physician Communication during Medical Visits. American Journal of Public Health. 2004;94(12):2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C. Mt. Sinai Changing Allocation of Rooms as Bias Inquiry Starts. New York Times. 1993. October 19, Section B, page 1.
- Kaiser Family Foundation. National Survey of Physicians: Highlights and Chartpack. [accessed August 25, 2005]. http://www.kff.org/minorityhealth/20020321a-index.cfm Available at.
- Kawachi I, Daniels N, Robinson DE. Health Disparities by Race and Class: Why Both Matter. Health Affairs. 2005;24(2):343–52. doi: 10.1377/hlthaff.24.2.343. [DOI] [PubMed] [Google Scholar]
- Kemper P, Blumenthal D, Corrigan JM, Cunningham PJ, Felt SM, Grossman JM, Kohn LT, Metcalf CE, St Peter RF, Strouse RC, Ginsburg PB. The Design of the Community Tracking Study: A Longitudinal Study of Health System Change and Its Effects on People. Inquiry. 1996;33(2):195–206. [PubMed] [Google Scholar]
- Kletke PR, Davidson SM, Perloff JD, Schiff DW, Connelly JP. The Extent of Physician Participation in Medicaid: A Comparison of Physician Estimates and Aggregated Patient Records. Health Services Research. 1985;20(5):503–23. [PMC free article] [PubMed] [Google Scholar]
- Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, Bindman AB. The Role of Black and Hispanic Physicians in Providing Health Care for Underserved Populations. New England Journal of Medicine. 1996;334(20):1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- Laveist TA. Racial Segregation and Longevity among African Americans: An Individual-Level Analysis. Health Services Research. 2003;38(6, part 2):1719–34. doi: 10.1111/j.1475-6773.2003.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillie-Blanton M, Martinez RM, Salganicoff A. Site of Medical Care: Do Racial and Ethnic Differences Persist? Yale Journal of Health Policy, Law, and Ethics. 2001;1:15–32. [PubMed] [Google Scholar]
- Margolis PA, Cook RL, Earp JA, Lannon CM, Keyes LL, Klein JD. Factors Associated with Pediatricians' Participation in Medicaid in North Carolina. Journal of the American Medical Association. 1992;267(14):1942–46. [PubMed] [Google Scholar]
- Massey D, Denton N. American Apartheid: Segregation and the Making of the Underclass. Cambridge, Mass: Harvard University Press; 1993. [Google Scholar]
- Menges J, Park C, Babcock J, Chimento L, Haught R, Ho S. Comparing Physician and Dentist Fees among Medicaid Programs. 2001. [accessed on August 24, 2005]. http://www.chcf.org/topics/medi-cal/index.cfm?itemID=20412 Available at.
- Mitchell JB. Medicaid Participation by Medical and Surgical Specialists. Medical Care. 1983;21(9):929–38. doi: 10.1097/00005650-198309000-00008. [DOI] [PubMed] [Google Scholar]
- Mitchell JB. Physician Participation in Medicaid Revisited. Medical Care. 1991;29(7):645–53. doi: 10.1097/00005650-199107000-00004. [DOI] [PubMed] [Google Scholar]
- Mitchell JB, Schurman R. Access to Private Obstetrics/Gynecology Services under Medicaid. Medical Care. 1984;22(11):1026–37. doi: 10.1097/00005650-198411000-00005. [DOI] [PubMed] [Google Scholar]
- Moy E, Bartman BA. Physician Race and Care of Minority and Medically Indigent Patients. Journal of the American Medical Association. 1995;273(19):1515–20. [PubMed] [Google Scholar]
- Oliver J, Mendelberg T. Reconsidering the Environmental Determinants of White Racial Attitudes. American Journal of Political Science. 2000;44(3):574–89. [Google Scholar]
- Ondrich J, Ross S, Yinger J. Geography of Housing Discrimination. Journal of Housing Research. 2001;12(2):217–38. [Google Scholar]
- O'Regan K, Quigley J. Spatial Effects on Employment Outcomes: The Case of New Jersey Teenagers. New England Economic Review. 1996 (May/June) [Google Scholar]
- Pear R. Taking Spin out of Report That Made Bad into Good. New York Times. 2004 February 22, Section 1, page 16. [Google Scholar]
- Perloff JD, Kletke PR, Fossett JW, Banks S. Medicaid Participation among Urban Primary Care Physicians. Medical Care. 1997;35(2):142–57. doi: 10.1097/00005650-199702000-00005. [DOI] [PubMed] [Google Scholar]
- Perloff JD, Kletke PR, Neckerman KM. Recent Trends in Pediatrician Participation in Medicaid. Medical Care. 1986;24(8):749–60. doi: 10.1097/00005650-198608000-00010. [DOI] [PubMed] [Google Scholar]
- Rathore S, Lenert L, Weinfurt K, Tinoco A, Taleghani C, Harless W, Schulman K. The Effects of Patient Sex and Race on Medical Students' Ratings of Quality of Life. American Journal of Medicine. 2000;108(7):561–66. doi: 10.1016/s0002-9343(00)00352-1. [DOI] [PubMed] [Google Scholar]
- Rosenbaum S. Racial and Ethnic Disparities in Healthcare: Issues in the Design, Structure, and Administration of Federal Healthcare Financing Programs Supported through Direct Public Funding. In: Smedley B, Stith A, Nelson A, editors. Unequal Treatment. Washington, D.C.: National Academies Press; 2003. pp. 664–98. edited by. [Google Scholar]
- Rosenbaum S, Markus A, Darnell J. U.S. Civil Rights Policy and Access to Health Care by Minority Americans: Implications for a Changing Health Care System. Medical Care Research and Review. 2000;57(suppl. 1):236–59. doi: 10.1177/1077558700057001S11. [DOI] [PubMed] [Google Scholar]
- Rosenbaum S, Stewart A, Sonosky C. Negotiating the New Health System Fourth Edition—Medicaid Managed Care General Service Agreements. 2002. [accessed on August 24, 2005]. http://www.gwumc.edu/sphhs/healthpolicy/nnhs4/GSA/ Available at.
- Sachdev A. State Violating Medicaid Laws. Chicago Tribune. 2004 August 25, Section A, page 1. [Google Scholar]
- Satel S, Klick J. The Institute of Medicine Report: Too Quick to Diagnose Bias. Perspectives in Biology and Medicine. 2005;48(1S):S15–S25. [PubMed] [Google Scholar]
- Schneider EC, Zaslavsky AM, Epstein AM. Racial Disparities in the Quality of Care for Enrollees in Medicare Managed Care. Journal of the American Medical Association. 2002;287(10):1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dube R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ, Ayers W. The Effect of Race and Sex on Physicians' Recommendations for Cardiac Catheterization. New England Journal of Medicine. 1999;340(8):618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- Shannon G, Bashur R, Spurlock C. The Search for Medical Care: An Exploration of Urban Black Behavior. International Journal of Health Service. 1978;8(3):519–30. doi: 10.2190/0F28-23GM-42K0-PQDN. [DOI] [PubMed] [Google Scholar]
- Sloan F, Mitchell J, Cromwell J. Physician Participation in State Medicaid Programs. Journal of Human Resources. 1978;13(suppl):211–45. [PubMed] [Google Scholar]
- Smedley B, Stith A, Nelson A. Unequal Treatment. Washington, D.C.: National Academies Press; 2003. [PubMed] [Google Scholar]
- Smith DB. The Racial Segregation of Hospital Care Revisited: Medicare Discharge Patterns and Their Implications. American Journal of Public Health. 1998;88(3):461–63. doi: 10.2105/ajph.88.3.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DB. Health Care Divided: Race and Healing a Nation. Ann Arbor: University of Michigan Press; 1999. [Google Scholar]
- Smith DB. Racial and Ethnic Health Disparities and the Unfinished Civil Rights Agenda. Health Affairs. 2005;24(2):317–24. doi: 10.1377/hlthaff.24.2.317. [DOI] [PubMed] [Google Scholar]
- Soss J, Schram S, Vartanian T, O'Brien E. The Hard Line and the Color Line. In: Schram S, Soss J, Fording R, editors. Race and the Politics of Welfare Reform. Ann Arbor: University of Michigan Press; 2003. pp. 225–53. edited by. [Google Scholar]
- Sullivan R. Two Hospitals Are Accused of Segregating by Race. New York Times. 1994 May 20, Section B, page 3. [Google Scholar]
- Turner M, Ross S, Galster G, Yinger J, Godfrey E, Bednarz B, Herbig C, Lee S, Hossain A, Zhao B. Discrimination in Metropolitan Housing Markets: National Results from Phase I HDS 2000 Final Report. 2002. [accessed September 5, 2005]. http://www.urban.org/UploadedPDF/410821_Phase1_Report.pdf Available at.
- U.S. Bureau of the Census. Statistical Abstract of the United States 2001. Washington, D.C.: U.S. Bureau of the Census; 1995. [Google Scholar]
- U.S. Bureau of the Census. Statistical Abstract of the United States 2005: sec. 1, Population. 2005. [accessed on August 16, 2005]. http://www.census.gov/prod/www/statistical-abstract-us.html Available at.
- U.S. Department of Health and Human Services. Area Resource File (ARF) Rockville, Md.: 2002. Health Resources and Services Administration, Bureau of Health Professions. [Google Scholar]
- van Ryn M, Burke J. The Effect of Patient Race and Socio-Economic Status on Physicians' Perceptions of Patients. Social Science & Medicine. 2000;50(6):813–28. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- Waitzman NJ, Smith KR. Separate but Lethal: The Effects of Economic Segregation on Mortality in Metropolitan America. The Milbank Quarterly. 1998;76(3):341–73. doi: 10.1111/1468-0009.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls CA, Rhodes KV, Kennedy JJ. The Emergency Department as Usual Source of Medical Care: Estimates from the 1998 National Health Interview Survey. Academic Emergency Medicine. 2002;9(11):1140–45. doi: 10.1111/j.1553-2712.2002.tb01568.x. [DOI] [PubMed] [Google Scholar]
- Weinick RM, Zuvekas SH, Cohen JW. Racial and Ethnic Differences in Access to and Use of Health Care Services, 1977 to 1996. Medical Care Research and Review. 2000;57(suppl. 1):36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- Weisse CS, Sorum PC, Sanders KN, Syat BL. Do Gender and Race Affect Decisions about Pain Management? Journal of General Internal Medicine. 2001;16(4):211–17. doi: 10.1046/j.1525-1497.2001.016004211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright GC. Racism and Welfare Policy in America. Social Science Quarterly. 1976;57(1):718–30. [Google Scholar]
- Yinger J. Measuring Racial Discrimination with Fair Housing Audits: Caught in the Act. American Economic Review. 1986;76(5):881–93. [Google Scholar]
- Yinger J. Closed Doors, Opportunities Lost: The Continuing Costs of Housing Discrimination. New York: Sage; 1995. [Google Scholar]
- Zuvekas SH, Weinick RM. Changes in Access to Care, 1977–1996: The Role of Health Insurance. Health Services Research. 1999;34(1):271–80. [PMC free article] [PubMed] [Google Scholar]


