Abstract
Nursing home care is currently a two-tiered system. The lower tier consists of facilities housing mainly Medicaid residents and, as a result, has very limited resources. The nearly 15 percent of U.S. nonhospital-based nursing homes that serve predominantly Medicaid residents have fewer nurses, lower occupancy rates, and more health-related deficiencies. They are more likely to be terminated from the Medicaid/Medicare program, are disproportionately located in the poorest counties, and are more likely to serve African-American residents than are other facilities. The public reporting of quality indicators, intended to improve quality through market mechanisms, may result in driving poor homes out of business and will disproportionately affect nonwhite residents living in poor communities. This article recommends a proactive policy stance to mitigate these consequences of quality competition.
Those writing on the quality of nursing home care have, for the most part, framed the discussion in terms of its uniformly poor quality and have largely ignored the prospects and implications of a two-tiered system differentiated by quality. In contrast, our article provides evidence of a two-tiered system of nursing home care. The lower tier consists of facilities with high proportions of Medicaid residents and, as a result, very limited resources. Thus, stratification affects the number, type, and quality of services provided to residents of lower-tier facilities, who are disproportionately poor and from minority groups. Our focus in this article is on the effects of stratification for the traditional long-stay nursing home population. We discuss the implications for the care provided to minority and disadvantaged residents in poor communities with the knowledge that increased competition on the basis of quality may accelerate the closure of these facilities (Harrington et al. 2003; Mukamel and Spector 2003). We consider policy initiatives that promote the positive aspects of turning many “upper-tier” nursing homes into postacute care facilities while protecting those operating in the “lower tier.”
The quality of nursing home care is a long-standing public policy concern (Angelelli et al. 2003; Institute of Medicine 1996, 2001), and the causes and consequences of racial disparities in health care have emerged as a priority concern as well (Institute of Medicine 2002, National Healthcare Disparities Report 2002). Numerous studies reveal racial disparities and segregation across a wide spectrum of health care providers (Epstein and Ayanian 2001; Lee et al. 1998; Smith 1990, 1993, 1999; Wallace 1990; Weinick, Zuvekas, and Cohen 2000), including nursing homes (Brooks 1996; Fennell, Miller, and Mor 2000; Hanley et al. 1990; Reed and Tobias 2001; Wallace et al. 1998). Other studies indicate that the care given to African-American residents may be of lesser quality (Bernabei et al. 1998; Castle and Mor 1998; Christian, Lapane, and Toppa 2003; Intrator, Mor, and Zinn 2004; Lapane et al. 1999). The resources available to nursing homes, particularly staffing, have a significant impact on their ability to provide good-quality care (Cherry 1991; Cohen and Spector 1996; Institute of Medicine 1996, 2001; Munroe 1990; Spector and Takada 1991; Zinn 1993). Moreover, their source of revenue (payer mix) is a prime determinant of their ability to secure resources. The Medicaid program is the United States’ largest purchaser of nursing home services (Strahan 1997). Despite the considerable variation in Medicaid's per diem payment rates from state to state, these rates are usually lower than others and may even be below the actual cost of providing care (Seidman 2002). Although earlier studies failed to establish a relationship between Medicaid payment rates and the quality of nursing home care (Nyman 1985, 1988a, 1988b, 1989), more recent studies have found a positive relationship between reimbursement and quality (Cohen and Spector 1996; Grabowski and Angelelli 2003; Grabowski, Angelelli, and Mor 2004). That is, those homes that are highly dependent on Medicaid as a source of revenue have the greatest difficulty securing the resources needed to provide good-quality care. Because they have no other sources of revenue (other payers or philanthropy), they are unable to cross-subsidize the care of Medicaid residents, that is, to use surpluses from other sources to cover any Medicaid shortfall.
This suggests that the residents of homes highly dependent on Medicaid may be more likely to receive poorer care. Accordingly, we studied homes dependent on Medicaid (our lower-tier facilities) to determine the characteristics of these facilities and their clientele, the quality of care they provide, and whether the two-tiered system of nursing home care is a source of racial disparity. Our findings document the stratification of the nursing home industry and uncover highly suggestive evidence that the poor, frail, and minority residents served by “lower-tier” providers are particularly likely to receive substandard care.
Methods
Data
This study uses data from three sources. The On-line Survey, Certification and Reporting (OSCAR) is a data network maintained by the Centers for Medicare & Medicaid Services (CMS) in cooperation with the states’ long-term care surveying agencies. OSCAR provides information on nursing homes’ structure (proprietary status, number of beds, hospital affiliation, etc.), staffing, case mix, and service availability obtained from annual survey inspections. By law, nursing homes certified to receive Medicare and/or Medicaid funding must be surveyed by state agencies every nine to 15 months. Surveyors evaluate the homes’ structural features, such as staffing and policies, care processes, and resident functional status, to establish whether minimum standards have been met. Even though the actual survey practices and the resulting findings of violations vary from state to state, the data elements collected during these surveys are uniform (Harrington 2001). The number and types of health deficiency citations given to each nursing home are the key features of the OSCAR data (Harrington et al. 2000).
The second source, the Minimum Data Set (MDS), is a resident-level record combining demographic, clinical, and functional data relevant to treatment planning. Data are gathered for all admissions (including private-pay residents) to Medicare- and Medicaid-certified nursing homes in the United States at the time of admission and periodically thereafter, depending on the patients’ payer source. Studies of the reliability and validity of these data suggest that they are useful for clinical applications and epidemiological and policy research studies (Gambassi et al. 1998; Gambassi et al. 2000; Miller, Gozalo, and Mor 2001; Mor 2004; Mor et al. 2003b; Morris et al. 1997). Since June 22, 1998, CMS has maintained a centralized repository of all MDS data. These data are used to aid in the quality inspection process, to set Medicare's case mix–adjusted per diem payments under the Prospective Payment System for skilled nursing facilities, and to create and report to the public any quality performance measures taken to help consumers and their advocates select a nursing facility (Mor 2004; Mor et al. 2003a). We used 2000 MDS data to characterize the population of all residents of all the facilities covered in our study. Finally, the OSCAR and MDS data were supplemented by the 2000 Area Resource File, a county-level collection of data drawn from 2000 census information as well as from national surveys of health service resource availability.
Sample
The United States has more than 17,000 Medicare- and Medicaid-certified nursing facilities, approximately 2,500 of which are owned or operated by hospitals. These hospital-based facilities are postacute recuperative settings serving mainly Medicare-eligible residents. Therefore, since our focus is on the traditional long-stay nursing home population, we excluded hospital-based facilities and their residents from our study.
Variables
Before making our case for what may be driving and sustaining stratification in the nursing home industry, we should define membership in the upper (“have”) and lower (“have-not”) tiers. Historically, those facilities with high concentrations of Medicaid residents are in the lower tier of financial performance and quality (Weech-Maldonado, Neff, and Mor 2003). We constructed a composite measure based on the payer configuration of Medicaid, private pay, and Medicare in each facility. To qualify as a lower-tier facility required that 85 percent or more of the residents be supported by Medicaid, less than 10 percent be supported by private payers, and less than 8 percent be supported by Medicare. These figures represent facilities at the 10th percentile of the private pay, 88th percentile of the Medicaid, and 65th percentile of the Medicare distribution. While it is true that the limits on resources due to the mix of residents is conceptually a continuum, we felt that a relatively “extreme” payer-mix configuration provided the fewest opportunities for cross-subsidizing the residents’ care. Although Medicaid payment rates vary dramatically from state to state, they generally are substantially lower than the private-pay rate or the level at which Medicare reimburses facilities for the least impaired Medicare-eligible patient and often fall below costs (Nyman and Connor 1994; Swan et al. 2000). Over the past decade, although the increase in Medicaid payment rates has outstripped that of inflation, it has lagged behind the increase in medical care costs (Harrington et al. 2000). Ninety-three percent of the residents of the average lower-tier facility (representing between 13 percent and 15 percent of all nonhospital-based facilities during the 1990s) were Medicaid recipients; 2 percent were Medicare recipients; and 5 percent were private-pay residents. Only 200 nonhospital-based SNFs serve exclusively Medicaid patients.
Using the OSCAR data, we calculated the number of administrators, registered nurses, licensed practical nurses, and certified nursing assistants per resident. We also determined whether the facility had a physician extender or a nurse practitioner on staff, the provision of which is associated with fewer avoidable hospitalizations (Intrator, Castle, and Mor 1999). The number of cited deficiencies of quality standards was also taken from OSCAR. Since much of the considerable interstate variation in this measure is not related to other facility characteristics, we standardized the intrastate variation in order to compare the facilities’ performance across states (Angelelli et al. 2003). The longitudinal OSCAR data allowed us to determine whether the facility changed ownership during selected periods of time as well as whether the facility terminated its participation in the Medicare/Medicaid program. Finally, we calculated the occupancy rate as the percentage of occupied certified beds.
Using the MDS data, we calculated the distribution of facility residents by race (African American v. white non-Hispanic) and calculated the facility case-mix severity index used to create the Resource Utilization Groupings III (RUGs III) resident classification system (Fries et al. 1994). RUGs III is the case-mix classification system that Medicare uses to determine the level of payment for each resident eligible for Medicare. The higher the case-mix severity index is, the greater the medical and functional care needs of the residents in the facility will be. The MDS data also enabled us to characterize facilities according to their performance on the quality measures that the CMS is currently reporting on the Internet (http://www.medicare.gov/nhcompare/home.asp) to help prospective residents and their advocates choose a nursing facility (Berg et al. 2002). Finally, for each county in which a sample facility is located, we used the Area Resource File to calculate quintiles of the county's median family income.
Analytic Approach
We examined the relationship between lower-tier status and particular facility or aggregate resident characteristics. Because a number of studies have documented the staffing and quality differences between for-profit and nonprofit nursing homes and because nonprofit facilities may have access to philanthropic resources to supplement their reimbursements, we stratified all analyses by for-profit versus nonprofit status (Harrington et al. 2002). We used the Kruskal-Wallis two-sample nonparametric test of the chi-square distribution to examine the effect of lower-tier and proprietary status on selected outcomes.
Results
In 2000 there were a total of 14,130 nonhospital-based Medicare- and Medicaid-certified nursing facilities in the United States, 13 percent of which were classified as lower tier. Proprietary facilities, accounting for nearly three-quarters of the total, were significantly more likely to be lower tier (15.4 percent v. 10.2 percent; p < .001). Among proprietary facilities, 66.6 percent were affiliated with a chain. Chain-affiliated proprietary facilities were significantly less likely to be in the lower tier (19.7 percent v. 13.3 percent; p < .01). Nonprofit facilities operating within a chain also were less likely to be in the lower tier than were the nonchain, nonprofit facilities (7.8 percent v. 10.8 percent).
Lower-Tier Facilities
Location
Not surprisingly, facilities in the lower tier and serving predominantly Medicaid patients tended to be located in poor communities. Table 1 indicates the relationship between a county's relative wealth and the likelihood that the facilities located in that county were in the lower tier. In light of the relationship between the rural status of a county and the poverty rate, we stratified this analysis by rural versus urban location.
TABLE 1.
Distribution of “Lower-Tier” Facilities by Quintile of County per Capita Income, Stratified by Urban/Rural Settings, 2000
| Quintiles of County per Capita Income | Urban (n= 9,290) | Rural (n= 4,840) |
|---|---|---|
| Wealthiest quintile | 15.4% | 5.6% |
| Second wealthiest | 12.6% | 7.2% |
| Middle quintile | 18.7% | 11.0% |
| Next to poorest quintile | 21.9% | 16.9% |
| Poorest quintile | 20.0% | 27.6% |
As the table shows, in both rural and urban counties there is a gradient between the median per capita income and the proportion of facilities classified as lower tier. The poorest urban counties are more likely to contain lower-tier facilities than are the wealthiest urban counties. This gradient is even steeper in rural counties, with more than one-quarter of the nursing facilities in the poorest rural counties categorized as lower tier.
Figure 1 presents a map of the United States indicating the proportion of facilities classified as lower tier. With the exception of Florida, many of the higher percentages of lower-tier facilities are in the Deep South (e.g., Louisiana, Mississippi, and Georgia). However, some states on the relatively more affluent east and west coasts also have high percentages of lower-tier facilities, suggesting a concentration of Medicaid patients in poor urban communities. In contrast, the facilities in the Northwest are much less likely to have a high concentration of Medicaid patients.
figure 1.
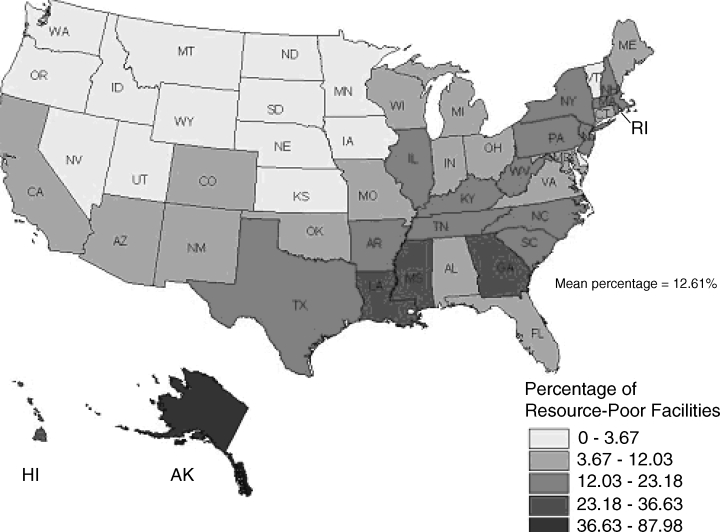
Percentage of Nonhospital-Based, Lower-Tier Facilities, by State, 2000
Characteristics
Table 2 presents the relationship between selected facility characteristics and lower-tier status, stratified by ownership, to test the effect of lower-tier status within ownership type. As can be seen, compared with upper-tier facilities, lower-tier facilities have significantly fewer registered nurses (RNs) per resident in both for-profit and nonprofit facilities. No such differences were observed for licensed practical nurses (LPNs), caregivers who are far more prevalent than RNs in nursing homes, suggesting that in lower-tier facilities, less qualified staff may be substituted for more qualified professional staff. Only among the for-profit facilities do lower-tier facilities have fewer certified nursing assistants (CNAs) per resident, but the difference is not very large in regard to the median number of aides. Other staff, such as administrators or physician extenders (nurse practitioners and physician assistants), are also less common in proprietary lower-tier facilities, although not in nonprofit facilities. Finally, for-profit, lower-tier facilities have lower occupancy rates than do other for-profit facilities, but this relationship was not observed in nonprofit facilities.
TABLE 2.
Characteristics of Lower-Tier and Upper-Tier Facilities by Ownership, 2000
| For-Profit | Nonprofit | |||
|---|---|---|---|---|
| Staffing and Case-Mix Characteristics | Lower Tier (n= 1,578) | Upper Tier (n= 8,624) | Lower Tier (n= 382) | Upper Tier (n= 3,546) |
| Registered nurses and full-time equivalents (FTEs)/residents | 3.4a | 5.5 | 5.4a | 7.2 |
| Licensed practical nurses and FTEs/residents | 12.9 | 12.8 | 13.3 | 12.6 |
| Certified nurse assistants and FTEs/residents | 36.7b | 37.6 | 43.6 | 42.5 |
| Administrators and FTEs/residents | 4.3a | 4.9 | 5.8 | 6.2 |
| Any physician extenders | 16.8%a | 20.7% | 24.3% | 21.4% |
| Occupancy rates | 87.5c | 88.3 | 91.9 | 92.9 |
| % of residents with psychiatric diagnosis | 22.3a | 11.5 | 15.9a | 9.3 |
| % of residents with mental retardation | 3.6a | 1.7 | 3.1a | .9 |
| Case-mix intensity index | .77c | .81 | .82a | .80 |
Kruskal-Wallis two-sample nonparametric test chi-square probability below .001.
Kruskal-Wallis two-sample nonparametric test chi-square probability below .01.
Kruskal-Wallis two-sample nonparametric test chi-square probability below .05.
We examined the relationship between lower-tier status and the likelihood of ownership change and program termination during two periods, 1993 through 1995 and 1996 through 1998. Table 3 shows the proportion of facilities in each time period that changed ownership or terminated from the program (either voluntarily or involuntarily), according to whether they were lower tier at the beginning of each of the two observation periods. In both periods, the likelihood of Medicare or Medicaid program termination was nearly twice as high among lower-tier as among upper-tier facilities. A change in ownership also was higher among lower-tier facilities. These both may be signals of financial or managerial difficulties.
TABLE 3.
Percentage of Lower-Tier Facilities Experiencing Ownership Change or Program Termination by Medicaid Concentration in Two Periods in the 1990s
| 1993 to 1995 | 1996 to 1998 | |||
|---|---|---|---|---|
| Structural Change | Lower Tier (n= 2,416) | Upper Tier (n= 12,106) | Lower Tier (n= 2,197) | Upper Tier (n= 12,523) |
| New owner | 8.9% | 6.6% | 9.1% | 7.5% |
| Program termination | 13.0% | 6.6% | 13.3% | 6.5% |
Quality of Care
Having identified the characteristics of “lower-tier” facilities, we next tried to determine whether their quality placed their residents at risk. Because health-related deficiencies identified in the annual certification survey varied considerably from state to state (1.5 to 13.7; average 5.8), we controlled for state to test the effect of lower-tier status and ownership on the number of health-related deficiencies. Lower-tier facilities had significantly more deficiencies (12.3 v. 7.9), and specifically health-related deficiencies (5.8 v. 3.7; p < .001), than did upper-tier facilities. Adjusting for interstate variation, lower-tier facilities had .75 (95 percent confidence interval [CI] .51–.99; p < .001) more health-related deficiencies than did upper-tier facilities. For-profit facilities had 1.6 (95 percent CI 1.41–1.81; p <.001) more deficiencies than did their nonprofit counterparts. Since the average number of deficiencies is only 5.8, when controlling for state and ownership, a high concentration of Medicaid patients means a 13 percent increase in the number of health-related deficiencies. These differences are even more striking when viewed state by state. For example, in Virginia the average number of health-related deficiencies in for-profit, lower-tier facilities is 7.5, compared with 3.8 for upper-tier, nonprofit facilities.
We next compared the distribution of four MDS-based quality measures across lower-tier and upper-tier facilities distinguished by proprietary status (Table 4). Quality measures summarizing the incidence of pressure ulcers, the use of physical restraints, the inadequacy of pain control, and the use of antipsychotic medications were examined. Based on these measures, lower-tier facilities offered worse care than did their less Medicaid-concentrated counterparts on three of the four quality measures reported by the Centers for Medicare & Medicaid Services. The results of comparisons for inadequate pain control went in the opposite direction, however. One explanation for this reversal of findings comes from a recent study finding that when a facility had no pain specialists, such as hospice staff, pain was underassessed, suggesting that the documentation of low levels of pain might actually indicate incomplete assessment (Wu et al. 2003).
TABLE 4.
MDS-Based Aggregated Quality Measures by Lower-Tier Status, Stratified by Ownership, 2000
| For-Profit Facilities | Nonprofit Facilities | |||
|---|---|---|---|---|
| Quality Measures | Lower Tier (n= 1,578) | Upper Tier (n= 8,624) | Lower Tier (n= 382) | Upper Tier (n= 3,546) |
| Restraint use | .11a | .10 | .10a | .09 |
| High-risk pressure ulcers | .18a | .17 | .16 | .15 |
| Low-risk antipsychotic use | .18b | .14 | .16b | .12 |
| Pain control | .11a | .12 | .11b | .12 |
Kruskal-Wallis two-sample nonparametric test chi-square probability below .001.
Kruskal-Wallis two-sample nonparametric test chi-square probability below .01.
Clientele
Regardless of ownership, lower-tier facilities are significantly more likely to serve residents with psychiatric conditions or those with a history of mental retardation (Table 2). Indeed, lower-tier facility residents are almost twice as likely to have a psychiatric diagnosis, and the proportion of mentally disabled residents is three times greater. Relative to that of upper-tier facilities, the case mix is more severe in the nonprofit lower-tier facilities and is significantly less severe among for-profit, lower-tier facilities. Since nonprofit lower-tier facilities may receive funds from philanthropic organizations, they may be apt to serve the more needy residents in any case. In contrast, proprietary facilities may prefer residents whose needs can be served with fewer staff and resources.
We looked at the relative distribution of African-American nursing home residents in both lower-tier and upper-tier facilities. We chose not to include other minority groups, since they are concentrated in relatively few states and do not account for a great part of the general nursing home population. Using the MDS data for all individuals residing in nonhospital-based facilities in 2000, we calculated separately the number of black and white residents in lower- and upper-tier facilities. Figure 2 depicts the ratio of the percentage of black to white nursing home residents (rate ratio) in lower-tier facilities by state. In the entire country, approximately 9 percent of all white nursing home residents are in lower-tier facilities, whereas 40 percent of African-American residents are in lower-tier facilities. The resulting rate ratio shows that African-American nursing home residents are approximately four times more likely to be in a lower-tier facility than whites are. Although there is some variation among the states, African-American nursing home residents are much more likely to live in a lower-tier nursing facility in nearly every state. For example, in Missouri, 33 percent of African-American nursing home residents are in lower-tier facilities, while this is true for only 5 percent of all white nursing home residents. Kentucky, with 16 percent of both white and black residents in lower-tier facilities, is the only state where blacks and whites are equally likely to live in a lower-tier facility. Since these maps and rate ratios are calculated on a state level, they miss the intrastate variation that would more clearly differentiate the general effect of rural poverty among African Americans in states like Mississippi and the effect of segregation in urban areas in states like Minnesota and Illinois (Smith 1990). Indeed, when contrasting Figures 1 and 2, it is apparent that there are more facilities with few resources in the Deep South than in the other states, indicating a smaller race differential in the likelihood of living in a poor facility in the Deep South than in the northern states.
figure 2.
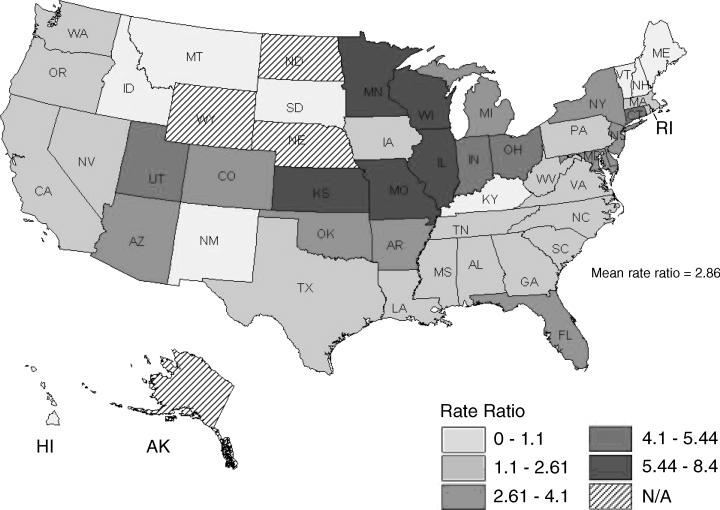
Rate Ratio of Percentage of Blacks in Lower-Tier versus Upper-Tier Facilities, by State, 2000
Discussion
In many respects, our description of stratification in the system of nursing home care is not new, as numerous components of the government-supported service system in the United States (e.g., education, transportation, landfill location) indicate an ongoing disadvantage for poor and racial and ethnic minorities (Bullard 2000; Bullard and Torres-Angel 2004). Allusions to this finding in the nursing home context have appeared in the past, but to our knowledge, ours is the first comprehensive treatment of this issue. The following sections summarize the implications of the primary findings of our study, identify the market and regulatory forces that may be sustaining this stratification, and explain why lower-tier facilities should not be forced to close. We end with a series of policy alternatives for ameliorating the negative consequences of the two-tiered system without undermining the industry's overall responsiveness to competitive incentives to provide quality care.
Implications of Lower-Tier Status
Staffing
Lower-tier facilities not only have fewer nurses, they also have fewer administrative resources and are less likely to have nurse practitioners or physician assistants available. Furthermore, these facilities presumably do not have enough resources to attract professional staff even if they could afford them. The communities in which lower-tier facilities tend to be located may offer little to attract qualified executives, contributing to a maldistribution of managerial talent and leadership, with the more capable managers gravitating toward resource-rich facilities in wealthier communities. As a result, these facilities are less able to design and implement innovative programs that may attract more profitable payers and motivate their staff. The net result is limited leadership in facilities with unimaginative policies serving the most vulnerable residents. A recent study examining the influence of administrators’ membership in professional organizations revealed that after controlling for available resources, leadership and innovation were independently associated with quality (Castle and Fogel 2002). A study of turnover among administrators in New York State nursing homes also showed that facilities with more deficiencies and relatively fewer resources were more apt to lose administrators (Angelelli, Petrisek, and Mor 2001). The stability, training, and professional membership of the top managers were important to predicting the introduction of innovation, particularly among nonchain facilities in which guidance could not be supplied by corporate offices (Castle 2001; Castle and Banaszak-Holl 1997).
Quality
Although other studies have noted that proprietary nursing facilities have more deficiencies than nonprofit facilities do, ours is the first to demonstrate this relationship with aggregated MDS-based performance measures (Angelelli et al. 2003; Harrington et al. 2001; Intrator, Castle, and Mor 1999). By separately examining the performance of lower-tier facilities, it is clear that the payer mix for both proprietary and nonprofit facilities is independently associated with poorer performance. Even our analyses of the effect of health-related deficiencies revealed that high concentrations of Medicaid residents were associated with more health-related deficiencies in both proprietary and nonprofit facilities, suggesting that not only “mission” and the profit motive affect performance (Harrington et al. 2001). The level of resources available also has a substantial influence.
Racial Composition
The fact that African-American nursing home residents are grossly overrepresented in these low-revenue, understaffed, and poor-quality facilities is consistent with the patterns of segregation observed in hospitals, schools, and other social institutions (Lee et al. 1998; Reed and Tobias 2001; Smith 1990, 1993). The evidence for racial disparities with respect to access to and receipt of high-quality acute hospital care, ambulatory care, and lifesaving procedures has been accumulating over the past decade, and these results are consistent with findings from nearly every other sector of health care (Epstein and Ayanian 2001; Wallace 1990; Weinick, Zuvekas, and Cohen 2000).
Location
We found that lower-tier facilities tend to be located in the poorest counties, both urban and rural. That facilities in poor communities are more likely to be lower tier reflects a maldistribution of social investment in nursing home care. These facilities have few if any financial, staff, and management resources and little in the way of interorganizational linkages with other providers in the community that could help them fulfill their mission (Smith 1990). The connection between locale and the availability of good-quality nursing home care may also contribute to the racial composition of lower-tier nursing facilities. Since African Americans are much more likely to reside in lower-tier facilities, which tend to be located in the poorer areas of the country, our findings essentially reflect the fact that just as poverty is not randomly distributed, poor-quality facilities are not randomly distributed either.
This finding was confirmed by a detailed study of nursing home bed supply in Chicago, which found that “nursing homes in the poorest communities have high percentages of Medicaid residents, are larger, and employ fewer staff per resident” (Reed and Tobias 2001, 88). From a policy perspective, the fact that lower-tier facilities are not randomly distributed across the country complicates strategies to improve the quality of care in nursing homes. Our definition of lower tier reflects the facilities’ disproportionate share of Medicaid residents but “standardizes” for the substantial state-to-state variation in Medicaid reimbursement rates (Grabowski 2001; Harrington 1999). In this sense it indicates the state's degree of payer source segregation. In states like Mississippi and Georgia, more than one-quarter of all the Medicaid- and Medicare-certified facilities are classified as lower tier, whereas less than 5 percent of facilities in the Northern Plains and Northwest are in the lower tier. When contrasting Figures 1 and 2, in these latter states this small number of African-American nursing home residents is usually concentrated in just a few lower-tier facilities.
Forces Sustaining the Two-Tiered System
Our findings have shown that a dependence on Medicaid affects the nursing home's staffing, case mix, occupancy, and risk of termination from public reimbursement programs. This, in turn, affects the quality of the facility as reflected in the cited health-related deficiencies as well as quality measures aggregated from resident-level data. In this section we go beyond our findings, drawing on the literature to consider what market and regulatory forces may be driving and sustaining the two-tier structure.
Fewer Opportunities to Cross-Subsidize
Cross-subsidization has historically been as closely tied to nursing facility finances as to hospital finances. Cross-subsidy can be explicit through cost shifting, that is, having enough profitable private-pay or Medicare residents to compensate for the Medicaid residents whose payments are quite low. For example, using data from Florida between 1994 and 1996, Troyer (2002) found that Medicaid covered the marginal cost of care in only two-thirds to three-fourths of all facilities. In essence, Medicaid payments are analogous to state or municipally issued school vouchers applied to private school tuition. If the voucher payment is less than the fees for a particular school, unless the difference can be made up through scholarships or a sliding fee scale by which the wealthier students subsidize the tuition of the less wealthy, access to that school is denied. Similarly, in the past the Medicaid per diem shortfall was covered by the higher rates paid by Medicare and by privately paying residents.
The recent changes in Medicare s reimbursement policies have made cross-subsidization less likely. In the past, nursing home facilities were reimbursed by Medicare under a retrospective, reasonable, cost-based system. The Medicare Prospective Payment System (PPS) for skilled nursing facilities (SNFs), which was implemented nationwide in 1999, changed reimbursements to facilities to a case mix–adjusted payment determined by resource utilization groups (RUGs) for care covered under Part A benefits. Among its provisions, PPS bundles all of Part A and B services for a Part A stay into a single RUG payment, thereby placing nursing homes at financial risk for those services previously billed independently by outside vendors (Angelelli et al. 2002). Shifting these costs to Medicare is less possible now that a fixed-price system has replaced the cost-based system.
In recent testimony before the Senate Finance Committee, the administrator of CMS acknowledged Medicare's historical cross-subsidization of the Medicaid program and noted that the end of some of the Medicare payment provisions of the Balanced Budget Refinement Act of 1999 have made it more difficult for nursing facilities to compensate for the lower Medicaid payments resulting from the states’ efforts to balance their budgets (Scully 2003).
Cross-subsidy is also found in the mix of patients requiring varying levels of care. If enough residents need little care, it is possible to care for a small number of residents needing a lot of care as long as no case-mix reimbursement system is in place. Over the past decade, as these systems have been instituted under Medicaid payment, the opportunities for case mix–based cross-subsidy have evaporated. As in the acute care sector, over the past few years the various payers of nursing home costs, including managed care organizations using nursing facilities in lieu of or to speed up hospital discharge, have been less willing to subsidize the care of other patients (Intrator et al. 1996; Zinn, Mor, and Gozalo 2000).
If the Boren amendment had not been repealed by the Balanced Budget Amendment of 1997, the need for cross-subsidization might have diminished considerably. When it was passed in 1980, the Boren amendment required state agencies to pay hospitals and nursing facilities according to a reasonable rate that was adequate to meet the costs of efficiently and economically operated facilities in order to provide care and services conforming to the applicable state and federal laws, regulations, and quality and safety standards (section 1902[a][13]). After this statute was repealed, nursing homes were left with no federal statutory protection for adequate reimbursement now or in the foreseeable future. Furthermore, the repeal of this amendment severed the link between Medicaid's nursing home rates and minimum state and federal quality and safety standards (Wiener and Stevenson 1998).
The financial impact of this policy change has not yet been analyzed. Using data from 1997 to 1999, Swan and colleagues (2000) found that in most states, the average rates of nursing facilities increased after the amendment was repealed. But in the late 1990s the economy was booming, and the states did not have huge budget deficits. Reflecting the adverse economic circumstances of more recent years, a study by the Kaiser Family Foundation found that 37 states planned to reduce or freeze the amount of Medicaid funding for nursing home care (Kaiser Family Foundation 2002).
The Deinstitutionalization of the Long-Term Psychiatric Population
Lower-tier facilities, particularly for-profit facilities, are much more likely to serve the least desirable long-term care residents, those with a history of psychiatric diagnoses (Mosher-Ashley and O'Neill 1991). Many of these facilities may be serving the legacy of national policy directed at the deinstitutionalization of public mental hospitals over the last several decades (Mishara, Budd, and Dixon 1973). Once a facility is marked as attracting a preponderance of these residents in the community, potential referral sources may stereotype them in that capacity. Privately paying individuals will resist moving to a residence with a predominance of psychiatric patients, thus contributing to the facility's becoming increasingly dependent on Medicaid. Once established, it may be difficult to alter this reputation without a major investment of capital and the skills necessary to alter the community's perceptions. But as the number of residents funded by neither Medicare nor Medicaid increases, the number with a psychiatric hospital history will decline to the point that only 11 percent of residents in facilities with more than 50 percent “other” pay residents have a psychiatric history. (An analysis of 2000 OSCAR data is available from the authors.)
Assisted-Living Facilities
At the same time that nursing facilities are required to take increasingly complex patients and provide adequate resources to care for them, assisted-living facilities are attracting patients who need less care and could have helped cross-subsidize their care. While the extent of substitution appears to depend on the local market's supply and demand, estimates range from 10 to 25 percent of nursing home admissions (Newcomer et al. 2001; Spector, Reschovsky, and Cohen 1996). In the past, nursing home residents have needed relatively little care, mainly some help in the activities of daily living because they were unable to function well independently. By drawing away the custodial private-pay patients from nursing homes, assisted-living facilities contribute to increasing the acuity of nursing home residents. The only remaining sources of lower-acuity residents for nursing facilities are Medicaid recipients. Thus, the emergence of assisted living has contributed to the development of a two-tiered system of care because some facilities, unable to attract Medicare or private-pay patients, can offer only custodial care to Medicaid recipients.
Furthermore, in the long run, assisted living may not necessarily substitute for nursing home care but, rather, only delay the time of admission (Zimmerman et al. 2003). More and more elders are putting off going into nursing facilities until they are both more impaired and more likely to have begun the “spend-down” process to Medicaid eligibility (Mollica 2003; Phillips et al. 2003). This further reduces the number of private-pay patients in the pool of nursing home admissions and increases the homes’ dependence on Medicaid program revenues.
Managed Care (Health Maintenance Organizations and Preferred-Provider Organizations)
Given the financial uncertainty associated with PPS reimbursement, managed care contracting could be viewed as an attractive alternative to relying on prospective payment under Medicare. The emergence of Managed Care Organization (MCO) benefits for SNF care in the early 1990s opened opportunities for SNFs, many of which tried to secure contracts (Zinn, Mor, and Gozalo 2000). Our results suggest that lower-tier facilities would be the least likely to attract MCOs, since they have none of the characteristics and capabilities that MCOs want. This also makes them more dependent on Medicaid, regardless of the state and the market, further stratifying the market for nursing home care.
In sum, the combined effects of the market and regulatory forces just described may completely transform long-term care, with custodial services for privately paying residents provided only in assisted-living facilities and nursing facilities increasingly used to meet the relatively short-term needs of patients recovering from a hospital stay or beginning a terminal episode. The residual pool of nursing facilities unable to respond to this challenge are likely to be relegated to serving higher concentrations of poorly reimbursed Medicaid patients. The net result will be a bifurcation of the nursing home industry into those facilities that have the resources and sophistication needed to compete in the new environment and those that do not. Such transformations are common in many other industries and always create temporary dislocations of workers and consumers. However, for long-term care, such dislocations may translate into inadequate care and clinical resources for frail, old, and poor patients living in facilities that are predominantly supported by public reimbursement.
The Case for Maintaining the Lower Tier
Our findings demonstrate that lower-tier facilities are much more likely to leave the Medicaid and Medicare programs. Although only a few terminations are involuntary (i.e., terminated by CMS for serious health violations), even voluntary terminations, in which the facility has chosen to leave the federal programs, are associated with more deficiencies and other performance problems, suggesting that these facilities leave the Medicare and Medicaid programs for financial reasons before being forced out by regulators (Angelelli et al. 2003). In 2002 CMS began its nationwide public reporting of nursing home performance measures to enable consumers and their advocates to make more informed choices when selecting a nursing home (Berg et al. 2002; Mor et al. 1998; Zimmerman et al. 1995). The response to the public reporting of nursing home quality measures will only exacerbate the financial vulnerability of homes with a disproportionate share of Medicaid residents and may hasten their departure from the Medicaid and Medicare programs (Mor et al. 2003c; Mukamel and Spector 2003).
All things considered, why shouldn't we let these facilities fail? Why not let the market forces act as they are intended? Since regulators have been unable or unwilling to shut down chronically poor performing facilities, why not have them progressively lose money until they close voluntarily or conditions become so bad that they will be forced to close? In addition to the danger of such a laissez-faire approach to current residents, there are larger policy considerations. The rural and poor urban counties in which these facilities are located are areas where opportunities are limited and employment as a certified nursing assistant is a stable source of income. The viability of these facilities should be a major public policy concern because their closure would be a hardship for not only the residents who must be moved but also the community faced with losing an important source of employment. The resulting disruption would be felt most strongly by African-American and other minority residents of the nation's nursing homes. As we have shown, fully 40 percent of all minority nursing home residents live in these “at-risk” facilities, and even this figure underestimates the impact on the local area due to residential segregation (Reed and Tobias 2001). If these mainly Medicaid-dependent homes fail or are closed because of poor performance, then in many markets institutional long-term care for the historically underserved, including minority elders and those with a history of mental illness, will be much harder to find.
Thus, although we no longer have the condition of bed shortages that in the past had prevented underperforming nursing facilities from closing, the current oversupply does not mean that the appropriate policy response is to merely let the market act (Wiener, Stevenson, and Goldenson 1999). A more proactive stance is needed. Rather than merely reacting to market forces, the government regulatory and reimbursement apparatus should plan for the eventuality of facilities’ failing performance associated with dropping admissions and revenues that may worsen as public quality reporting steers prospective residents away from poor homes. As we have pointed out, current state and federal policies may inadvertently accelerate the lower-tier facilities’ incapability to meet their patients’ needs. The challenge is to design policies that promote the natural evolution of nursing home care without penalizing the residents of those homes that may be unable to compete in the survival of the fittest.
Policy Alternatives
Selectively Increase the Amount of the Medicaid Voucher
Ultimately, elevating the quality of lower-tier facilities depends on society's willingness to provide more resources. Any strategy to improve the quality of these facilities will be seriously hampered by the continuation of the same level and distribution of financial resources to nursing home care. There must be a minimal level of reimbursement below which it is impossible to provide quality care, an assumption that was the premise of the Boren amendment. The problem is that there is no conclusive agreement on what that minimum is (Wiener and Stevenson 1998). Furthermore, increasing the Medicaid payments across the board would be inflationary, would likely meet with political resistance, and would undermine the competing goal of more funding for community-based care (Kane 2001). Conversely, adding money only to those states where the amount of the Medicaid voucher is insufficient to ensure access to acceptable facilities would be a more sustainable approach. The American Health Care Association, a trade association representing the nursing home industry, recently commissioned a study of the shortfall between the states’ Medicaid reimbursement and Medicaid's reimbursable costs. While the adequacy of the methodology has been questioned, this study found that on average, facilities in every state but Alabama experienced a loss because of inadequate Medicaid per diem payments (Seidman 2002). Lower-tier facilities in those states with the greatest negative variances clearly are at the greatest disadvantage with respect to their ability to provide adequate care. However, increasing payments for improvements in quality, such as more staff, is challenging, requiring complex risk adjustments, and does not address the problem of local area nursing shortages or the poor “reputation” of problem facilities. A recent report examining state policies regarding minimum staffing ratios found that few states explicitly tied the mandated increases to payment rates (Tilly et al. 2003).
The political viability of higher Medicaid payments, even relatively minor ones differentially applied, is obviously problematic in light of the recent freezes and reductions in payments due to the states’ fiscal deficits (Kaiser Family Foundation 2002). But an interventionist approach to increase the funding for those facilities willing to commit to improvement and to state-provided guidance will certainly be less expensive and possibly more effective than generalized increases in payment rates. If the program were to require facilities to acknowledge their performance problems, the demand for this differential payment might be lower than it otherwise might be.
Offer Training Programs for Managers of Nursing Homes
There is increasing evidence that achieving resident outcome quality targets may be associated with better financial performance (Weech-Maldonado, Neff, and Mor 2003). For those facilities serving predominantly Medicaid residents, one approach could be to have the state identify the top managers charged with “turning around” a floundering facility in order to improve quality and efficiency. This may require giving the existing managers the training needed to develop the relevant skills.
As the managers of lower-tier facilities use this training to become more marketable, they may seek higher-paying jobs in better-endowed facilities. Thus, rather than expanding the pool of managerial talent available to lower-tier facilities, training programs could make the current maldistribution even worse. If this happens, a program like the Public Health Service's “underserved areas” approach to sending physicians to underserved communities might be necessary to ensure that well-trained managerial staff are available in lower-tier facilities.
Have State or Municipal Government Rescue Permanently Failed Facilities
A third alternative borrows from remedies designed to rescue another failure-prone social institution responsible for a vulnerable population, the public school system. In several cases across the country, the states or local municipalities have taken over the operation of poorly performing school districts (Chute 2002). Municipalities across the country have also contracted with proprietary education companies to operate troubled schools under the eye of the city or the state (Caruso 2002). In some instances, short-term turnarounds have resulted in measurable improvement in student achievement, safety, or administrative efficiency. Indeed, in some localities, the courts have been particularly aggressive in this regard, appointing court “masters” to adjudicate the school's daily operation. Similarly, states or counties have, although rarely, chosen to place some nursing facilities in receivership, appointing a third party to manage the facility (Walker 2003). This step is taken only as a last resort, however, when the deficiencies are chronic and long-standing, even life threatening, or when the facility becomes bankrupt.
We propose that responsible government entities consider expanding their authority to assume control over lower-tier facilities with serious quality problems. Modeled on VISTA, the domestic Peace Corps, a “SWAT” team composed of retired health executive volunteers could be dispatched to make short-term improvements in quality and efficiency. To supplement these efforts, the community must help support the care of residents in a variety of ways. There is a precedent in that the conditions of Medicare and Medicaid for participating in the hospice program include involvement with volunteers. This model could be applied to nursing homes either generally or more specifically when management experts are brought in to forestall closure. Indeed, the legal basis for mandating the introduction of external managers would be to ensure the residents’ safety and might be complemented by creating a community board empowered to stabilize the facility's long-term viability.
Provide Risk Pools for Displaced Residents
In the long run, governments do not want to be in the business of running nursing homes. For facilities that cannot improve, closure may be the only option. Closing these failed facilities requires a plan to relocate the displaced residents. If new ownership and permanent management cannot be found, a transitional management team should provide an organized and controlled way to close the home and move the residents. Borrowing from the insurance industry, which applies the concept to high-risk, uninsurable drivers and patients, these residents could be relocated through the creation of a risk pool. Roughly two-thirds (66 percent) of lower-tier facilities are in urban areas, so the transfer of lower-tier residents to a facility relatively close by is logistically feasible. But in order to avoid transferring the residents to other poorly performing facilities eager to admit anyone, policymakers could temporarily raise the payment for such transfers to make sure that high-quality facilities are willing to accept Medicaid residents. In some states the difference between Medicaid payment rates and either Medicare or private pay makes it economically reasonable for providers to keep some beds empty in hopes of admitting a Medicare or private-pay resident rather than filling the bed with a Medicaid patient. Thus, the level of the “transfer premium” must be sufficient to overcome this incentive. Non-lower-tier facilities could be required to admit some number of displaced residents as a condition for participating in the Medicare program. Given the declining occupancy rates (from 86.5 percent in 1991 to 83.0 percent in 2001), there appears to be sufficient excess capacity to accommodate transfers.
Conclusions
We have described and examined the implications of the “two-tiered” system of nursing homes in the United States and have offered policy alternatives that may help protect the interests of residents in the lower tier. All the proposed alternatives will require an increase in the level of resources devoted to nursing home care. We acknowledge that there is a policy dilemma associated with investing more money in nursing homes at a time when the public prefers home care and/or assisted living (Teno et al. 2004). Most Americans know little about nursing homes, have little interest in knowing more, and desperately want to avoid them. Although the number of alternatives to nursing home care is growing throughout the country, the proportion of the population living in a nursing home, if only for short-term recuperation, is growing and is likely to continue to grow. Thus, this is a policy dilemma that cannot be avoided. Nursing homes will not disappear from the array of available long-term care options. It is better to face the dilemma proactively rather than ignore it, since exposure to “poor” care is not a risk faced only by someone else's mother or widow.
Acknowledgments
This research was supported in part by grant no. HS10322 from the Agency for Healthcare Research and Quality, grant no. AG11624 from the National Institute on Aging, and grants no. 97385 and 03188 from the Robert Wood Johnson Foundation.
References
- Angelelli J, Gifford D, Intrator O, Gozalo P, Laliberte L, Mor V. Access to Postacute Nursing Home Care before and after the BBA (Balanced Budget Act) Health Affairs. 2002;21:254. doi: 10.1377/hlthaff.21.5.254. [DOI] [PubMed] [Google Scholar]
- Angelelli J, Mor V, Intrator O, Feng Z, Zinn J. Oversight of Nursing Homes: Pruning the Tree or Just Spotting Bad Apples? Gerontologist. 2003;43:67. doi: 10.1093/geront/43.suppl_2.67. spec. no. 2. [DOI] [PubMed] [Google Scholar]
- Angelelli J, Petrisek GD, Mor V. External Threats and Nursing Home Administrator Turnover. Health Care Management Review. 2001;26:52. doi: 10.1097/00004010-200107000-00006. [DOI] [PubMed] [Google Scholar]
- Berg K, Murphy K, Mor V, Moore T, Morris JN, Harris Y. Identification and Evaluation of Existing Nursing Home Quality Indicators. Health Care Financing Review. 2002;23:19. [PMC free article] [PubMed] [Google Scholar]
- Bernabei R, Gambassi G, Lapane K, Landi F, Gatsonis C, Dunlop R, Lipsitz L, Steel K, Mor V. Management of Pain in Elderly Patients with Cancer. SAGE Study Group, Systematic Assessment of Geriatric Drug Use via Epidemiology. Journal of the American Medical Association. 1998;279:1877. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- Brooks S. Separate and Unequal. Contemporary Long Term Care. 1996;19:40. [PubMed] [Google Scholar]
- Bullard R. Dumping in Dixie: Race, Class and Environmental Quality. Boulder, Colo.: Westview Press; 2000. [Google Scholar]
- Bullard R, Torres-Angel JG. Highway Robbery: Transportation, Racism and New Routes to Equity. Atlanta: South End Press; 2004. [Google Scholar]
- Caruso DB. Associated Press State & Local Wire; After Delay, Philadelphia Starts Paying Edison Schools; p. 1. Oct. 29. [Google Scholar]
- Castle NG. Innovation in Nursing Homes: Which Facilities Are the Early Adopters? Gerontologist. 2001;41:161. doi: 10.1093/geront/41.2.161. [DOI] [PubMed] [Google Scholar]
- Castle NG, Banaszak-Holl J. Top Management Team Characteristics and Innovation in Nursing Homes. Gerontologist. 1997;37:572. doi: 10.1093/geront/37.5.572. [DOI] [PubMed] [Google Scholar]
- Castle NG, Fogel BS. Professional Association Membership by Nursing Facility Administrators and Quality of Care. Health Care Management Review. 2002;27:7. doi: 10.1097/00004010-200204000-00002. [DOI] [PubMed] [Google Scholar]
- Castle NG, Mor V. Physical Restraints in Nursing Homes: A Review of the Literature since the Nursing Home Reform Act of 1987. Medical Care Research and Review. 1998;55:139–70. doi: 10.1177/107755879805500201. [DOI] [PubMed] [Google Scholar]
- Cherry RL. Agents of Nursing Home Quality of Care: Ombudsmen and Staff Ratios Revisited. Gerontologist. 1991;31:302. doi: 10.1093/geront/31.3.302. [DOI] [PubMed] [Google Scholar]
- Christian JB, Lapane KL, Toppa RS. Racial Disparities in Receipt of Secondary Stroke Prevention Agents among U.S. Nursing Home Residents. Stroke. 2003;34:2693. doi: 10.1161/01.STR.0000096993.90248.27. [DOI] [PubMed] [Google Scholar]
- Chute E. We've Made Some Progress”: Future Uncertain as Duquesne Schools Mark 2 Years as “Distressed. Pittsburgh Post-Gazette. 2002 Oct. 11. [Google Scholar]
- Cohen J, Spector W. The Effect of Medicaid Reimbursement on Quality of Care in Nursing Homes. Journal of Health Economics. 1996;15:23. doi: 10.1016/0167-6296(95)00030-5. [DOI] [PubMed] [Google Scholar]
- Epstein A, Ayanian JZ. Racial Disparities in Medical Care. New England Journal of Medicine. 2001;344:1471. doi: 10.1056/NEJM200105103441911. [DOI] [PubMed] [Google Scholar]
- Fennell M, Miller S, Mor V. Facility Effects on Racial Differences in Nursing Home Quality of Care. American Journal of Medical Quality. 2000;15:174. doi: 10.1177/106286060001500408. [DOI] [PubMed] [Google Scholar]
- Fries B, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III) Medical Care. 1994;32:668. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Gambassi G, Landi F, Peng L, Brostrup-Jensen C, Calore K, Hiris J, Lipsitz L, Mor V, Bernabei R. Validity of Diagnostic and Drug Data in Standardized Nursing Home Resident Assessments: Potential for Geriatric Pharmacoepidemiology. Medical Care. 1998;36:167. doi: 10.1097/00005650-199802000-00006. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. [DOI] [PubMed] [Google Scholar]
- Gambassi G, Lapane K, Sgadari A, Carbonin P, Gatsonis C, Landi F, Peng L, Lipsitz L, Mor V, Bernabei R. Archives of Internal Medicine. Vol. 160. SAGE Study Group; 2000. Effects of Angiotensin-Converting Enzyme Inhibitors and Digoxin on Health Outcomes of Very Old Patients with Heart Failure; p. 53. Systematic Assessment of Geriatric Drug Use via Epidemiology. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. Medicaid Reimbursement and the Quality of Nursing Home Care. Journal of Health Economics. 2001;20:549. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Angelelli JJ, Mor V. Health Affairs. 2004. Medicaid Payment and Risk-Adjusted Nursing Home Quality. In press. [DOI] [PubMed] [Google Scholar]
- Hanley RJ, Alecxih LM, Wiener JM, Kennell DL. Predicting Elderly Nursing Home Admissions. Results from the 1982–1984 National Long-Term Care Survey. Research on Aging. 1990;12:199. doi: 10.1177/0164027590122004. [DOI] [PubMed] [Google Scholar]
- Harrington C. 1998 State Data Book on Long Term Care Program and Market Characteristics. Baltimore, Md: Centers for Medicare & Medicaid Services; 1999. [Google Scholar]
- Harrington C. Residential Nursing Facilities in the United States. BMJ. 2001;323:507. doi: 10.1136/bmj.323.7311.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C, Collier E, O'Meara J, Kitchener M, Simon LP, Schnelle JF. Federal and State Nursing Facility Websites: Just What the Consumer Needs? American Journal of Medical Quality. 2003;18:21. doi: 10.1177/106286060301800105. [DOI] [PubMed] [Google Scholar]
- Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. Does Investor Ownership of Nursing Homes Compromise the Quality of Care? American Journal of Public Health. 2001;91:1452. doi: 10.2105/ajph.91.9.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. Does Investor-Ownership of Nursing Homes Compromise the Quality of Care? International Journal of Health Services. 2002;32:315. doi: 10.2190/EBCN-WECV-C0NT-676R. [DOI] [PubMed] [Google Scholar]
- Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing Home Staffing and Its Relationship to Deficiencies. Journal of Gerontology: Social Sciences. 2000;55:S278. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Nursing Staffing in Hospitals and Nursing Homes: Is It Adequate? Washington, D.C.: National Academy Press; 1996. [Google Scholar]
- Institute of Medicine. Improving the Quality of Long-Term Care. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- Institute of Medicine. Guidance for the National Healthcare Disparities Report. Washington, D.C.: National Academy Press; 2002. [PubMed] [Google Scholar]
- Intrator O, Castle NG, Mor V. Facility Characteristics Associated with Hospitalization of Nursing Home Residents: Results of a National Study. Medical Care. 1999;37:228. doi: 10.1097/00005650-199903000-00003. [DOI] [PubMed] [Google Scholar]
- Intrator O, Mor V, Hines MA, Lancaster T, Laliberte LL, Freiberger W. Effect of the Medicare Catastrophic Coverage Act on Payer Source Changes among Nursing Home Residents. Inquiry. 1996;33:42. [PubMed] [Google Scholar]
- Intrator O, Mor V, Zinn J. The Impact of Nursing Homes on Potentially Preventable Hospitalization of Long-Stay Residents. Journal of the American Geriatrics Society. 2004 doi: 10.1111/j.1532-5415.2004.52469.x. In press. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Nursing Home Quality: State Agency Survey Funding and Performance. Washington, D.C.: Kaiser Commission on Medicaid and the Uninsured; 2002. [Google Scholar]
- Kane RL. What Older People Want from Long-Term Care, and How They Can Get It. Health Affairs. 2001;20:114. doi: 10.1377/hlthaff.20.6.114. [DOI] [PubMed] [Google Scholar]
- Lapane KL, Barbour MM, Van Haaren A, Gambassi G. Pharmacotherapy. Vol. 19. (SAGE) Group; 1999. Antiischemic Therapy in Patients with Coronary Heart Disease Living in Long-Term Care; p. 627. Systematic Assessment of Geriatric Drug Use by Epidemiology. [DOI] [PubMed] [Google Scholar]
- Lee A, Baker C, Gehlbach S, Hosmer D, Reti M. Do Black Elderly Medicare Patients Receive Fewer Services? An Analysis of Procedure Use for Selected Patient Conditions. Medical Care Research and Review. 1998;55:314. doi: 10.1177/107755879805500305. [DOI] [PubMed] [Google Scholar]
- Miller S, Gozalo P, Mor V. Hospice Enrollment and Hospitalization of Dying Nursing Home Patients. American Journal of Medicine. 2001;111:38. doi: 10.1016/s0002-9343(01)00747-1. [DOI] [PubMed] [Google Scholar]
- Mishara B, Budd RE, Dixon T. Transferring Elderly Patients from Mental Hospital to Nursing Home. Hospital Community Psychiatry. 1973;24:837. doi: 10.1176/ps.24.12.837. [DOI] [PubMed] [Google Scholar]
- Mollica R. Coordinating Services across the Continuum of Health, Housing, and Supportive Services. Journal of Aging Health. 2003;15:165. doi: 10.1177/0898264302239022. [DOI] [PubMed] [Google Scholar]
- Mor V. A Comprehensive Clinical Assessment Tool to Inform Policy and Practice: Applications of the Minimum Data Set. Medical Care. 2004;42(suppl. III):50. doi: 10.1097/01.mlr.0000120104.01232.5e. [DOI] [PubMed] [Google Scholar]
- Mor V, Angelelli J, Gifford D, Morris J, Moore T. Benchmarking and Quality in Residential and Nursing Homes: Lessons from the U.S. International Journal of Geriatric Psychiatry. 2003a;18:258. doi: 10.1002/gps.821. [DOI] [PubMed] [Google Scholar]
- Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-Rater Reliability of Nursing Home Quality Indicators in the U.S. BMC Health Services Research. 2003b;3:20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Berg K, Angelelli J, Gifford D, Morris J, Moore T. The Quality of Quality Measurement in U.S. Nursing Homes. Gerontologist. 2003c;43:37. doi: 10.1093/geront/43.suppl_2.37. spec. no. 2. [DOI] [PubMed] [Google Scholar]
- Mor V, Morris J, Lipsitz L, Fogel B. Benchmarking Quality in Nursing Homes: The Q-Metrics System. Canadian Journal of Quality in Health Care. 1998;14:12. [Google Scholar]
- Morris J, Nonemaker S, Murphy K, Hawes C, Fries BE, Mor V, Phillips C. A Commitment to Change: Revision of HCFA's RAI. Journal of the American Geriatric Society. 1997;45:1011. doi: 10.1111/j.1532-5415.1997.tb02974.x. [DOI] [PubMed] [Google Scholar]
- Mosher-Ashley PM, O'Neill TB. Attitudes of Nursing and Rest Home Administrators toward Deinstitutionalized Elders with Psychiatric Disorders. Community Mental Health Journal. 1991;27:241. doi: 10.1007/BF00757259. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD. Quality Report Cards and Nursing Home Quality. Gerontologist. 2003;43:58. doi: 10.1093/geront/43.suppl_2.58. spec. no. 2. [DOI] [PubMed] [Google Scholar]
- Munroe DJ. The Influence of Registered Nurse Staffing on the Quality of Nursing Home Care. Research in Nursing Health. 1990;13:263. doi: 10.1002/nur.4770130409. [DOI] [PubMed] [Google Scholar]
- National Healthcare Disparities Report. Rockville Md.: Agency for Healthcare Research and Quality; 2002. Fact Sheet. AHRQ Publication no. 03-P007, October http://www.ahrq.gov/news/nhdrfact.htm. [Google Scholar]
- Newcomer R, Swan J, Karon S, Bigelow W, Harrington C, Zimmerman D. Residential Care Supply and Cognitive and Physical Problem Case Mix in Nursing Homes. Journal of Aging Health. 2001;13:217. doi: 10.1177/089826430101300204. [DOI] [PubMed] [Google Scholar]
- Nyman JA. Prospective and “Cost-Plus” Medicaid Reimbursement, Excess Medicaid Demand, and the Quality of Nursing Home Care. Journal of Health Economics. 1985;4:237. doi: 10.1016/0167-6296(85)90031-1. [DOI] [PubMed] [Google Scholar]
- Nyman JA. The Effect of Competition on Nursing Home Expenditures under Prospective Reimbursement. Health Services Research. 1988a;23:555. [PMC free article] [PubMed] [Google Scholar]
- Nyman JA. Excess Demand, the Percentage of Medicaid Patients, and the Quality of Nursing Home Care. Journal of Human Resources. 1988b;23:76. [Google Scholar]
- Nyman JA. Excess Demand, Consumer Rationality, and the Quality of Care in Regulated Nursing Homes. Health Services Research. 1989;24:105. [PMC free article] [PubMed] [Google Scholar]
- Nyman JA, Connor RA. Do Case-Mix Adjusted Nursing Home Reimbursements Actually Reflect Costs? Minnesota's Experience. Journal of Health Economics. 1994;13:145. doi: 10.1016/0167-6296(94)90021-3. [DOI] [PubMed] [Google Scholar]
- Phillips CD, Sherman MY, Rose M, Spector W, Hawes C. Effects of Facility Characteristics on Departures from Assisted Living: Results from a National Study. Gerontologist. 2003;43:690. doi: 10.1093/geront/43.5.690. [DOI] [PubMed] [Google Scholar]
- Reed SC, Tobias AS. Concentrated Poverty and Nursing Home Bed Supply in Chicago. Journal of Health Care for the Poor and Underserved. 2001;12:88. doi: 10.1353/hpu.2010.0667. [DOI] [PubMed] [Google Scholar]
- Scully T. Medicare Reform Opinions. Modern Healthcare. 2003;33:22. [PubMed] [Google Scholar]
- Seidman B. A Briefing Chartbook on Shortfalls in Medicaid Funding for Nursing Home Care. 2002. Report prepared for the American Health Care Association.
- Smith DB. Population Ecology and the Racial Integration of Hospitals and Nursing Homes in the United States. Milbank Quarterly. 1990;68:561. [PubMed] [Google Scholar]
- Smith DB. The Racial Integration of Health Facilities. Journal of Health Politics Policy Law. 1993;18:851. doi: 10.1215/03616878-18-4-851. [DOI] [PubMed] [Google Scholar]
- Smith DB. Health Care Divided: Race and Healing a Nation. Ann Arbor: University of Michigan Press; 1999. [Google Scholar]
- Spector WD, Reschovsky JD, Cohen JW. Appropriate Placement of Nursing-Home Residents in Lower Levels of Care. Milbank Quarterly. 1996;74:139. [PubMed] [Google Scholar]
- Spector WD, Takada HA. Characteristics of Nursing Homes That Affect Resident Outcomes. Journal of Aging Health. 1991;3:427. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- Strahan GW. Advance Data. Washington, D.C.: U.S. Department of Health and Human Services, National Center for Health Statistics, Centers for Disease Control and Prevention; 1997. An Overview of Nursing Homes and Their Current Residents: Data from the 1995 National Nursing Home Survey. no. 280. [PubMed] [Google Scholar]
- Swan J, Harrington C, Clemena W, Pickard RB, Studer L, Dewit SK. Medicaid Nursing Facility Reimbursement Methods: 1979–1997. Medical Care. 2000;57:361. doi: 10.1177/107755870005700306. [DOI] [PubMed] [Google Scholar]
- Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family Perspectives on End-of-Life Care at the Last Place of Care. Journal of the American Medical Association. 2004;291:88. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- Tilly J, Black K, Ormond B, Harvell J. State Experiences with Minimum Nursing Staff Ratios for Nursing Facilities: Findings from Case Studies of Eight States. Washington, D.C.: U.S. Department of Health and Human Services, Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy; 2003. [Google Scholar]
- Troyer JL. Cross-Subsidization in Nursing Homes: Explaining Rate Differentials among Payer Types. Southern Economic Journal. 2002;68:750. [Google Scholar]
- Walker J. Missouri Nursing Home Operator to Take over Livingston County, Ky., Facility. Paducah (Ky.) Sun. 2003:1. Sept. 7. [Google Scholar]
- Wallace S. Race versus Class in the Health Care of African-American Elderly. Social Problems. 1990;37:517. [Google Scholar]
- Wallace S, Levy-Storms S, Kington R, Andersen R. The Persistence of Race and Ethnicity in the Use of Long-Term Care. Journal of Gerontology. 1998;53B:S104. doi: 10.1093/geronb/53b.2.s104. [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R, Neff G, Mor V. The Relationship between Quality of Care and Financial Performance in Nursing Homes. Journal of Health Care Finance. 2003;29:48. [PubMed] [Google Scholar]
- Weinick RM, Zuvekas SH, Cohen JW. Racial and Ethnic Differences in Access to and Use of Health Care Services, 1977 to 1996. Medical Care Research Review. 2000;57(suppl. 1):36. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- Wiener JM, Stevenson DG. State Policy on Long-Term Care for the Elderly. Health Affairs. 1998;17:81. doi: 10.1377/hlthaff.17.3.81. [DOI] [PubMed] [Google Scholar]
- Wiener JM, Stevenson DG, Goldenson SM. Controlling the Supply of Long-Term Care Providers in Thirteen States. Journal of Aging Social Policy. 1999;10:51. doi: 10.1300/J031v10n04_04. [DOI] [PubMed] [Google Scholar]
- Wu N, Miller SC, Lapane K, Gozalo P. The Problem of Assessment Bias When Measuring the Hospice Effect on Nursing Home Residents’ Pain. Journal of Pain Symptom Management. 2003;26:998. doi: 10.1016/s0885-3924(03)00328-2. [DOI] [PubMed] [Google Scholar]
- Zimmerman D, Karon SL, Arling G, Clark BR, Collins T, Ross R, Sainfort F. Development and Testing of Nursing Home Quality Indicators. Health Care Financing Review. 1995;16:107. [PMC free article] [PubMed] [Google Scholar]
- Zimmerman SG, Sloane PD, Eckert JK, Hebel JR, Morgan LA, Stearns SC, Wildfire J, Magaziner J, Chen C, Konrad TR. Assisted Living and Nursing Homes: Apples and Oranges? Gerontologist. 2003;43:107. doi: 10.1093/geront/43.suppl_2.107. [DOI] [PubMed] [Google Scholar]
- Zinn J. The Influence of Nurse Wage Differentials on Nursing Home Staffing and Resident Care Decisions. Gerontologist. 1993;33:721. doi: 10.1093/geront/33.6.721. [DOI] [PubMed] [Google Scholar]
- Zinn J, Mor V, Gozalo P. Market and Regulatory Forces and the Transformation of the Nursing Facility Industry. Advances in Health Care Management. 2000;1:369. [Google Scholar]


