Abstract
One pressing challenge facing the U.S. health care system is the development of effective policies and clinical management strategies to address deficiencies in health care quality. In collaboration with researchers at the University of Washington, the Washington State Department of Labor and Industries has created a communitywide delivery system intervention to improve health outcomes and reduce disability among injured workers. This intervention is currently being tested in two sites in western and eastern Washington. So far, it appears to be possible to engage physicians and health care institutions in quality improvement initiatives and to form effective public-private partnerships for this purpose. Furthermore, collaborating with university researchers may help enhance the scientific rigor of the quality improvement initiative and create more opportunities for a successful evaluation.
The search for new approaches to improve the quality of health care has become even more important in recent years with the mounting evidence of serious errors and deficiencies in the delivery of health services (Chassin and Galvin 1998; Committee on the Quality of Health Care in America 2001; Kohn et al. 1999; Schuster, McGlynn, and Brook 1998). Within the field of workers’ compensation, the quality of occupational health care has been a long-standing concern. Studies indicate that the outcomes of care for workers’ compensation patients are worse than the outcomes for similar procedures for patients with non-work-related conditions (Greenough and Fraser 1989; Javid 1992; Katz et al. 1998). Not only are the treatment outcomes worse for workers’ compensation than for general medical care, but the medical cost of the treatment of similar conditions is higher (Baker and Krueger 1995; Johnson, Baldwin, and Furton 1996). Furthermore, workers’ compensation faces the difficult task of preventing and managing serious and costly disabilities (Cheadle et al. 1994). Nonetheless, the workers’ compensation system has paid relatively little attention to the important issue of disability prevention.
The Institute of Medicine (IOM) report Crossing the Quality Chasm (Committee on the Quality of Health Care in America 2001) called attention to the critical need for system redesign to address health care quality problems. Many of the problems and recommended strategies that the IOM report listed apply directly to workers’ compensation health care delivery. Even though practitioners both inside and outside the workers’ compensation system face many difficulties in developing effective quality improvement interventions, they have little systematic evidence to guide them.
This article describes an innovative quality improvement project in Washington State that is designed to improve the outcomes for and reduce the disabilities of injured workers receiving care through the workers’ compensation system. This project started in April 2002 and will continue through July 2006.
Prior Workers’ Compensation Delivery System Interventions
Washington State uses a state fund system to provide workers’ compensation insurance. Such a system requires employers who do not self-insure to buy workers’ compensation insurance through the state fund, which is administered by the Department of Labor and Industries (DLI). The DLI provides workers’ compensation insurance for approximately two-thirds of the nonfederal workforce in the state, or 1.4 million workers. In fiscal year 2000, the DLI expended $472.4 million for medical care and an additional $683.3 million for temporary and permanent disability payments.
The quality improvement initiative we describe in this article builds on an earlier managed care intervention begun in 1993 by the DLI in collaboration with researchers at the University of Washington. This intervention was intended to assess the effects of providing medical treatment to injured workers through designated occupational health care networks under managed care arrangements (Wickizer et al. 1999, 2001). It changed the method of payment from fee-for-service to capitation and made important changes in the organization of care through an occupational medicine model emphasizing the coordination of care and ongoing follow-up to get the injured worker back to work in a timely manner. The model also extensively used treatment guidelines, both concurrently and retrospectively for utilization management.
A research team at the University of Washington conducted a comprehensive evaluation of the intervention. The evaluation found that the managed care intervention was associated with lower costs per claim (Cheadle et al. 1999) and greater employer satisfaction with the timing and quality of information provided by physicians (Kyes, Wickizer, and Franklin 2003), but less patient satisfaction (Kyes et al. 1999). No statistically significant differences were observed in health outcomes (Kyes et al. 1999;Kyes, Wickizer, and Franklin 2001) between the managed care group and the fee-for-service group.
In addition, the evaluation found that managed care was associated with a 45 percent reduction in disability compensation paid for lost work time (Cheadle et al. 1999). (Workers in Washington State are eligible for disability payments if they miss four or more days of work because of an injury.) Since the managed care plans were not capitated for disability payments (the DLI continued to pay workers for disabilities in the usual way), it is likely that this favorable outcome resulted from the change in how care was organized and delivered through the occupational medicine model. In turn, this conclusion suggested that the quality of health care and the prevention of disabilities could be improved by using an occupational medicine model to deliver care. However, Washington industrial insurance laws guarantee workers the freedom to choose their own attending physician, thereby precluding the use of managed care arrangements that might limit their choice in some way (the DLI obtained a temporary waiver to form the physician networks for the pilot project). The researchers at the University of Washington conducted a policy study to examine options for developing a quality improvement initiative that would preserve the fundamental right of workers to choose their provider yet offer the important benefits of organizing care around an occupational medicine model (Wickizer et al. 1998). The recommendations of this policy study provided the foundation for the quality improvement initiative that we describe here, which is known as the Occupational Health Services (OHS) project.
This article (1) describes the quality indicators used to establish the benchmarks and quality improvement goals for the OHS project; (2) discusses the organizational entity—the center for occupational health and education (COHE)—that oversees and coordinates care and provides many of the quality improvement activities; (3) examines the major impediments to quality addressed by the OHS project and the main problems the project has encountered; (4) reports the data for one pilot site; and (5) offers some observations regarding our early experience in implementing the project.
Quality Indicators
The primary goal of the OHS project was to improve the outcomes for and reduce the disabilities of injured workers. Accordingly, it was necessary to create quality indicators that would (1) establish expectations for the delivery of care by physicians participating in the project and (2) provide information to support the development of quality improvement activities. A panel of experts met in Seattle over a six-month period beginning in May 1999. They reviewed the existing scientific and clinical literature and treatment guidelines and, based on this review, established quality indicators, including both generic occupational health performance indicators and condition-specific indicators related to three common conditions: low back sprain, carpal tunnel syndrome, and fractures.
Table 1 lists the final set of performance quality indicators that we decided on for the OHS project (more detailed information about the quality indicators can be obtained from the authors). These quality indicators were intended to enhance the timeliness of treatment (indicators 1, 5, and 6), encourage the return to work (indicators 2, 3, and 4), and promote “best practices” in occupational health care (indicators 2, 3, 4, 5, and 7). In order to promote occupational health care practice patterns consistent with the OHS's quality improvement goals, the DLI offered financial incentives for certain quality indicators, including reimbursement for some previously unreimbursed activities, as well as higher fees for procedures and activities that previously were reimbursed. For example, the physician's fee for sending in the Report of Accident was increased by 50 percent, from $24 to $36, if the report was received within two business days.
TABLE 1.
Performance Quality Indicators Developed for Occupational Health Services (OHS) Project
| 1. Timeliness of submitting the Report of Accident: percentage of claims for which Report of Accident was received within two business days of the first office visit. |
| 2. Two-way communication with employer: percentage of claims for which two-way communication between the provider and employer about the worker's return to work or work modification was completed at the first visit when the worker was off or expected to be off work. |
| 3. Activity prescription at each evaluation: percentage of workers for whom an activity prescription was discussed and documented in the chart at each evaluation (no more than once per week) when the worker was off or expected to be off work. |
| 4. Assessment for impediments to returning to work: percentage of workers on time loss who received an assessment or referral for an assessment of impediments to return to work after four weeks of work loss. |
| 5. Timeliness of access to care: percentage of workers seen within three business days of the worker's first contact with the provider. |
| 6. Probability of work relatedness adequately specified on the Report of Accident: percentage of claims for which the probability of work relatedness was adequately specified on the accident report. |
| 7. Continuity of care: percentage of workers who had not returned to work who were visited by a health care provider every two weeks for the first two months and at least once every two to four weeks following the worker's return to work. |
| 8. Condition-specific quality indicators: Twelve indicators were adopted for the three OHS target conditions, two for carpal tunnel syndrome (CTS), four for low back injury, and six for fractures. The following indicators are presented as examples: (1) nerve conduction studies to corroborate the presence or absence of CTS if a time loss of more than two weeks or surgery was being considered; (2) exam screens for the presence or absence of radiculopathy for patients with low back injuries (using recognized, reliable criteria) at the first visit; (3) the need for advanced imaging (low back injuries) to be adequately justified; and (4) a fracture's severity graded by documenting key elements at initial visit. The specific measure is the percentage of claims with specific conditions (CTS, low back injury, or extremity fracture) for which each indicator is documented in the medical record. |
OHS Pilot Sites and Centers for Occupational Health and Education
The OHS project was designed as a communitywide delivery system intervention and was tried on a pilot basis through the development of two centers for occupational health and education. One center was at a large hospital, located in the south Seattle metropolitan area, which already had an active occupational health program. This region is a competitive urban health care market with an established manufacturing and industrial business environment. The other center for occupational health and education (COHE) was located at a rehabilitation hospital in Spokane, Washington, that serves a large geographic area in eastern Washington. This region offers a more rural industrial base with a different industrial mix, oriented toward agriculture and a more geographically dispersed but less competitive health care environment. The Seattle COHE has been fully operational since July 2002. It has recruited approximately 130 providers (physicians and chiropractors) who have treated more than 12,000 injured workers. The Spokane COHE began operation in April 2003. To date, it has recruited 155 providers and treated more than 2,500 workers. In this article, we describe primarily the experience of the Seattle COHE.
Figure 1 is a schematic of the OHS-COHE organization. The COHEs are expected to recruit physicians for the pilot from the community, including primary care providers, specialists, and chiropractors. The centers conducted limited marketing activities within their target areas to recruit providers and offered free continuing medical education to providers in order to explain the program. Providers participating in the OHS project had to sign a formal letter of agreement with the DLI that stipulated the mutual roles and responsibilities of the parties (the provider, the DLI, and the COHE). Other activities performed by the COHEs were tracking the care delivered by the participating providers, sponsoring provider training in the form of continuing medical education, arranging for provider mentoring by local senior clinicians, and initiating care coordination activities to avoid delays in treatment that could lead to costly and unnecessary disabilities. This coordination took different forms and involved the participation of the worker's attending physician, a specialist, the worker's employer, or the DLI claims manager.
Figure 1.
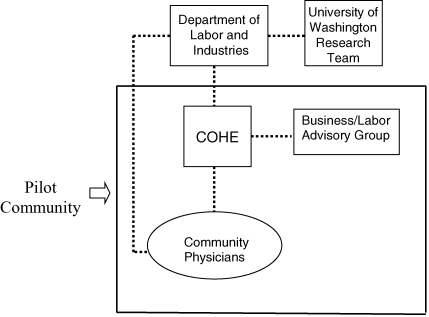
Organization of Occupational Health Services (OHS) and the Center for Occupational Health and Education (COHE)
In short, as its name implies, the COHE has a central role in providing the community of workers, employers, and providers with occupational health education, expertise, care coordination, and clinical services. The center's role is essentially that of a catalyst to improve quality within the community and as the identified entity working to resolve problems and issues that may result in (avoidable) long-term disabilities.
Other components of the OHS-COHE organization shown in Figure 1 are a local COHE advisory group consisting of business and labor representatives and the University of Washington's research team. This team is conducting a two-phase evaluation of the OHS pilot. Phase I is a process evaluation documenting the COHE's implementation and early operational experience and determining the consistency of the care provided by OHS participant physicians with the quality indicators. Phase I covers the COHE's initial 12-month operating period. In phase II, we will assess the outcomes of the intervention. Using a matched comparison group design, we will determine the effect of the intervention on medical costs, utilization, lost work time, and disability payments. The data for these measures will be gathered on OHS patients for a period of up to 18 months after treatment. We then will compare the OHS patients with the non-OHS (comparison group) patients, controlling for selected differences in provider characteristics. In addition, the evaluation will examine the effect of the OHS pilot on the patients’ satisfaction, recovery status, changes in wages, job status, and employment measures six months after treatment. For this purpose, we will survey approximately 500 OHS patients and 500 non-OHS patients, using an adaptation of a survey protocol used earlier to evaluate patients’ satisfaction across the state (Wickizer et al. 2004).
The OHS project represents a community-level quality improvement intervention. Its goal is to improve the quality of occupational health care across the community rather than in a single organization or treatment setting. As we point out later, this community focus poses certain challenges because it requires cross-institutional collaborations (relationships among hospital emergency departments, urgent care facilities, specialty medical groups, etc.) and the recruitment of a broad base of physicians in the community.
Impediments to Quality Improvement in Washington's Workers’ Compensation System and Strategies to Overcome Them
Improving the quality of workers’ compensation health care (and general medical care) at a community level requires systematic interventions that address the major impediments to quality. Based on the analysis performed as part of the OHS research and development work, we identified those factors that we believed (1) were important impediments to quality and (2) could be modified through a communitywide delivery system intervention. Table 2 lists these impediments and the targeted activities incorporated into the OHS project to address them.
TABLE 2.
Quality Impediments and Target Activities Undertaken by OHS Project to Address Impediments
| Quality Impediment | Target Activities Performed to Address Impediment |
|---|---|
| • Infrequent use of best practices resulting in poor quality | • Tracking care through performance quality indicators relative to established quality benchmarks; providing mentoring, continuing medical education, and academic detailing* |
| • Ineffective disability prevention | • Initiating time-linked clinical management action to promote return to work; providing systematic patient reviews to assess barriers to return to work; following occupational health best practices |
| • Administrative delays | • Promoting timely submission of report of accident and improving provider documentation of work-relatedness to facilitate quicker claim authorization |
| • Poor communication among providers, employers, and administrative parties | • Initiating case coordination within local health care system; encouraging two-way communication between provider and employer; promoting more effective use of electronic communication |
| • Inadequate reimbursement and misaligned financial incentives | • Using financial incentives linked to quality indicators |
| • Heavy provider administrative burden | • Using case coordination to reduce provider's administrative burden |
| • Lack of patient care tracking data | • Developing information technology to track patients, coordinate data, and provide feedback to providers |
| • Lack of evidence-based care | • Using quality indicators; distributing treatment guidelines |
*Academic detailing is a form of continuing medical education involving one-on-one training of the physician in his or her own office.
By their nature, workers’ compensation systems are somewhat regulatory and burdensome because they have evolved in part as publicly and politically negotiated liability systems, with a significant emphasis on workplace factors. The resulting clinical and administrative problems are frequently not part of the general provider training, and a failure to address them quickly when industrial injuries occur increases the risk of chronic disability (Cheadle et al. 1994). Although specifically developed within the Washington State workers’ compensation regulatory and health care environment, the impediments and strategies we identified can be applied to general health care settings as well as other workers’ compensation systems.
Infrequent Use of Best Practices Resulting in Poor Quality
Poor quality includes the provision of too little care, too much care, or the wrong care (Schuster, McGlynn, and Brook 1998), essentially because the best clinical, administrative, or procedural practices for given conditions or patient populations were lacking. Problems regarding quality have been widely documented for general medical care (Chassin and Galvin 1998; Committee on the Quality of Health Care in America 2001; Kohn et al. 1999; McGlynn et al. 2003; Schuster, McGlynn, and Brook 1998), but these problems in regard to workers’ compensation health care are not understood as well. What evidence is available (Greenough and Fraser 1989; Javid 1992; Katz et al. 1998; Mahmud et al. 2000) suggests that quality is a common problem in the workers’ compensation system. Examples of quality occupational health best practices include providers communicating with employers about workers’ return to work, early detection of impediments to recovery, timely access to care and diagnostic procedures, timely decisions about the value of surgical intervention, and an adequate occupational history of work relatedness to avoid delaying adjudicative decisions that may postpone necessary treatment. Because workers’ compensation, unlike general medical care, provides disability payments for lost work time, any financial consequences of poor quality that lead to delays in treatment or prolong recovery and thus a timely return to work, are significant. In workers’ compensation systems, disability payments for lost work time generally account for at least 50 percent of the total payments.
The OHS project has tried to improve the quality of care by means of several methods. The quality indicators described earlier are intended to address problems and deficiencies in the provision of occupational health care. For these indicators, quality is considered to be acceptable if an OHS participant provider meets the performance measure 80 percent of the time within a given period. The COHEs are tracking how often the OHS providers achieve the quality benchmarks and are periodically feeding back this information. The other target activities listed in Table 2 that address the problem of poor quality are providing continuing medical education, offering the mentoring of OHS participant providers by senior clinicians, and conducting academic detailing. (Academic detailing is a form of continuing medical education involving one-on-one training of the physician in his or her own office.)
Ineffective Prevention of Disabilities
Improving the prevention of disabilities is a key goal of the OHS project. Chronic disabilities from work-related conditions are devastating to workers’ health and quality of life. Therefore, the early identification of care for clinical and biopsychosocial issues that can lead to long-term disability are critical to providers to ensure a successful outcome for the patient.
In an earlier study, we showed that injured workers with musculoskeletal injuries who had not returned to work within three to four months were unlikely ever to return to meaningful employment (Cheadle et al. 1994). A more recent analysis of workers receiving disability compensation for carpal tunnel syndrome shows a similar pattern (Daniell et al. 2000). To address the problem of long-term disability, workers’ compensation insurers and self-insured employers often rely on external case managers to perform “disability management” after a worker has missed several months of work. This form of delayed, reactive case management offers little real chance of preventing long-term disability and returning the worker to meaningful employment.
The OHS project tries to prevent disabilities through several related activities. Certain quality indicators require time-linked action, for example, ordering nerve conduction tests to determine the presence of carpal tunnel syndrome if the patient is expected to be away from work for two or more weeks. One indicator (indicator 4 in Table 1) states that workers who are away from work for four weeks should have a detailed assessment to identify barriers to the return to work. Other quality indicators promote the use of occupational best practices aimed at getting the patient back to work as soon as possible. Indicators 2 and 3 of Table 1 pertain to the need for the provider to communicate with the employer and to prescribe activities if the patient is away from or is expected to be away from work. Each of these activities is intended to prevent disabilities.
Administrative Delays
The authorization of a claim is often delayed because the Report of Accident has not been filed promptly by the physician or because the report lacks the necessary information for the claims manager to determine the accident's relation to work. Such delays can also delay treatment and ultimately increase the patient's risk of developing an extended disability. The problem of administrative delays is addressed by two quality indicators pertaining to submitting the Report of Accident and supplying the appropriate documentation regarding work relatedness (indicators 1 and 6 on Table 1).
Poor Communication among Providers, Employers, and Administrative Parties
Poor communication is a significant problem in workers’ compensation. Rarely do providers communicate with employers about workers’ return to work or job modification. Moreover, communication between providers and claims managers is often sporadic and ineffective. The OHS project addresses this problem in two ways. First, it coordinates cases through the COHE to facilitate communication among clinical and administrative parties. Each COHE has at least one full-time equivalent (FTE) case coordinator who is familiar with the local health care system and workers’ compensation administrative procedures to provide this function. Second, it establishes, through a quality indicator, specific performance goals for the provider and employer (indicator 2 in Table 1).
Inadequate Reimbursement and Misaligned Financial Incentives
The need to align financial incentives to promote quality is a central theme of the IOM report Crossing the Quality Chasm (Committee on the Quality of Health Care in America 2001), as it also is for workers’ compensation. Inadequate reimbursement and misaligned financial incentives are obstacles to the improvement of quality. The OHS project therefore links financial incentives with quality improvement objectives and increases the reimbursement to providers for specific occupational health services. For example, OHS participant physicians can receive from $14 to $42 for time spent telephoning employers or other parties to coordinate care or discuss workers’ return to work.
Heavy Provider Administrative Burden
Those providers treating workers’ compensation patients have many complaints about the onerous administrative burdens imposed by the system. These burdens can delay medical care as well as decrease the willingness of providers to treat workers’ compensation patients. The OHS project is responding to this problem by enabling the COHE to coordinate the cases for the OHS participant providers, relieving them of the administrative burdens associated with claims or clinical management.
Lack of Patient Care Tracking Data
The improvement of quality care requires the systematic collection of reliable performance data for individual providers on patient care activities. While such data are sometimes collected in integrated delivery systems, they are almost never collected in the general fee-for-service system because it lacks the necessary organizational infrastructure. The development of information technology to track patient care and to feed back patient care data to OHS participant providers routinely is an important part of the OHS project. Data-tracking systems that allow providers and their staff to determine how they are performing on quality indicators and real-time reminders for key clinical and administrative tasks are central functions of the COHE.
Lack of Evidence-Based Care
The need for better clinical and scientific evidence to help clinicians care for their patients is widely recognized (Connis et al. 2000; Lohr, Eleazer, and Mauskopf 1998). Although significant progress has been made in recent years using evidence-based care to treat certain chronic illnesses such as diabetes and asthma (Franz et al. 2003; Frijling et al. 2002; Jadad 2002), occupational medicine has lagged far behind these developments. The OHS project has tried to correct this by creating evidence-based quality indicators. In addition, as new evidence-based treatment guidelines become available, the COHE will distribute them to OHS participant providers.
Challenges to Implementing Communitywide Quality Improvement Interventions
When carrying out our communitywide quality improvement initiative, we encountered several problems, such as developing information technology to track patient care, recruiting a broad base of community physicians and other health care providers, and fashioning cross-institutional collaborative relationships in very competitive markets. Each of these problems may differ in the various practice systems, community settings, and regulatory environments.
Information technology is critical to the improvement of quality because it allows patient care activities to be tracked and measured against explicit indicators or benchmarks. It is important that this information be fed back in real time to providers so that patients’ care can be adjusted when possible. Despite its acknowledged importance, the many practical obstacles to developing information technology for communitywide quality improvement interventions are often not recognized. Off-the-shelf patient tracking software programs are now available but may not have the flexibility to accommodate all the information needs of a particular quality improvement initiative.
The Seattle pilot site encountered significant problems and delays when creating its patient tracking system. Although the system is operating now, the time, cost, and effort required were far greater than what was anticipated at the beginning of the project. The Spokane pilot site had more success devising its patient tracking system, as it was able to draw on the technical expertise of the COHE staff and the sponsoring organization to design the system and the software. The Spokane system enables the COHE to track patients’ progress against the quality benchmarks, communicate with employers via electronic mail regarding patients’ status, and extract and aggregate data for the provider for analysis.
It is beyond the scope of this article to offer guidance regarding the many technical issues related to the development of patient-tracking systems. We therefore simply underscore the complexity of this task and the difficulty of creating such a system. Effective communication and close collaboration between the parties responsible for clinical management and the system's design and program staff are essential.
The OHS quality improvement model assumed that a broad base of physicians within each pilot site could be recruited. Even though the project offered greater reimbursement, the coordination of cases to reduce the burden on providers, and clinical consultation, recruiting providers proved to be difficult. One obstacle was the fact that a large proportion of community physicians treat relatively few workers’ compensation patients. The DLI's data show that in 2001, 84 percent of the attending doctors in the Seattle pilot site served 24 percent of the patients, and 6 percent of the attending doctors served 60 percent of the patients.
The practical implication of this treatment pattern to improve the quality of workers’ compensation is the need to identify the high-volume physicians who are more experienced in and perhaps more committed to caring for workers’ compensation patients. As of this writing, the Seattle pilot site has recruited approximately 130 providers (physicians and chiropractors), and the Spokane site has recruited 155 providers. Both sites have recruited a mix of high- and low-volume providers, as well as hospital emergency department physicians. As indicated by the data presented later, improving the quality and outcomes for low-volume providers may be especially difficult.
Another challenge arises when community-level quality improvement initiatives are established in very competitive health care markets. In such markets, the tasks of coordinating care, tracking patients across provider groups and organizations, and forging institutional relationships become more difficult. Providers and health care administrators are accustomed to short-run financial considerations and are thus more skeptical of initiatives whose benefits may not directly contribute to the organization's profit margin, at least in the short run. There is no easy way of relieving the tension between the short-term financial considerations that arise from competitive market forces and the longer-term quality improvement goals. Health care organizations participating in quality improvement initiatives may be better able to differentiate themselves from their competitors on the basis of quality and therefore become stronger financially in the long run.
Preliminary Data from the OHS Evaluation
The following are data gathered from the process evaluation for the Seattle OHS pilot site, which began treating patients in July 2002. The Spokane site, which began operation in July 2003, lacks sufficient data for a meaningful analysis. Figure 2 presents data on selected quality indicators over time for “high-volume” providers (physicians and chiropractors who treated more than 250 workers’ compensation patients in the initial pilot year). The data shown in Figure 2 represent approximately 2,700 treated cases, and the quality indicators show different patterns. For approximately 70 percent of the cases, the physicians submitted the accident report within two business days, making little change in the submission rate over time. In contrast, the rate of completing the activity prescription reports changed substantially, increasing from 11 percent in the first quarter of tracking to 79 percent by the second quarter of 2003. The third quality indicator, the physicians’ contact with employers, changed little over time, remaining at a modest level of 40 to 50 percent. Note that the data in Figure 2 do not represent a defined, single group of providers. Some of the variation in the quality indicators may reflect differences in the providers, who entered the high-volume group at different times.
Figure 2.
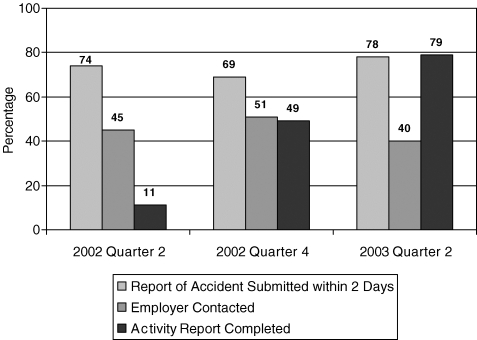
Percentage of Cases Achieving Quality Indicator Benchmark among Physicians Who Treated 250 or More Workers’ Compensation Patients during the Initial Pilot Year
The quality indicators for emergency room physicians as well as other community physicians (and chiropractors) who treated fewer cases during the initial pilot period also were tracked. The emergency room physicians achieved significant progress for two of the quality indicators: submission of the accident report and completion of the activity prescription report. For these two indicators, the percentage of cases reaching the goal for the indicator rose from 17 to 53 percent and 8 to 79 percent, respectively. Those community physicians and chiropractors who saw fewer patients made less progress in meeting the quality benchmarks. For example, among the moderate-volume providers, that is, the providers who treated between 50 and 250 cases during the tracking period, the rate of submission of the accident report within two business days rose only slightly, from 35 to 41 percent over the tracking period. A similar pattern was observed for this provider group for completing the activity prescription forms. The low-volume providers, those who treated fewer than 50 cases, reached fewer quality indicator benchmarks, from 20 to 30 percent, with little change over time.
It is not surprising that physicians with different numbers of workers’ compensation patients would differ in their performance with regard to the quality indicators. Those physicians who treated fewer workers’ compensation patients tended to have less interest in changing their practice behavior to conform to the quality indicators, and the financial incentives of doing so also were less important to them.
Conclusions
This article summarizes our early experience in implementing a communitywide quality improvement intervention in Washington State for workers’ compensation patients. Guided by a set of quality (performance) indicators, the OHS initiative addresses the principal problems of delivering workers’ compensation health care with the aim of improving outcomes and reducing disabilities. An important underlying assumption of the OHS project is that the occupational health care provided in the first month or two of a claim is critical to preventing disabilities. This assumption is consistent with the findings of a randomized clinical trial of back pain management, which showed that early occupational intervention with back pain patients who had been absent from work for four weeks was significantly more effective than the usual clinical care in returning patients to regular work (Loisel et al. 1994, 1997).
Workers’ compensation quality improvement interventions aimed at reducing workers’ disabilities must address three issues: the targeting of the intervention, its timing, and the appropriate expertise to use. It clearly is not efficient to target all patients for disability prevention. Rather, the strategy should be to identify those most at risk for a long-term disability (Turner, Franklin, and Turk 2000). In addition, we know little about population-level risk factors (e.g., older age). Early intervention to prevent disabilities is important as well. Our earlier managed care pilot (Wickizer et al. 2001) and other studies (Loisel et al. 1994, 1997) suggest the importance of having providers with formal training in occupational medicine deliver the care. The cases should be coordinated by persons familiar with workers’ compensation and the local health care delivery system. An effective way of identifying and intervening in cases at risk for a prolonged disability is essential.
Is quality improvement in workers’ compensation justified economically? Although recent data have cast doubt on whether there is a “business case for quality” in general medical care (Leatherman et al. 2003), workers’ compensation may be an exception. There may be a business case for quality in workers’ compensation if costly, unnecessary disabilities can be prevented (Cheadle et al. 1999; Wickizer et al. 2001). A recent study we conducted showed that injured workers reporting less favorable treatment were 3.5 times as likely (p= .02) to be out of work and receiving compensation for lost work time as were workers reporting more favorable treatment (Wickizer et al. 2004). Furthermore, the study's findings cited several areas critical to improving quality, including care coordination, provider expertise (both technical and interpersonal), and patient access (Wickizer et al. 2004).
Beyond these considerations, we would offer several other observations concerning our early experience in implementing the OHS quality improvement project. First, it is possible to construct a network of community providers outside the framework of a preferred provider organization or health maintenance organization to voluntarily improve health care quality. We see no reason why our basic model could not apply to other conditions or diseases beside occupational injuries. The OHS project attempts to manage care processes in order to improve outcomes, without restricting patients’ choices or limiting utilization to control costs. Second, recruiting providers does not require strong financial incentives. Both OHS pilot sites were able to recruit more than 130 community providers (physicians and chiropractors) while offering only modest financial incentives. The Spokane pilot plans to recruit additional physicians and expand the pilot to neighboring rural counties. Thus our experience suggests that it is possible to engage physicians voluntarily to improve the quality of care if they see the practical value of such efforts in providing better-quality patient care and if these efforts do not impose additional administrative burdens. Third, it is possible to engage the leadership of major health care institutions in communitywide quality improvement initiatives without the promise of immediate rewards or payback for the institution. The executive management leaders at our two sponsoring pilot institutions recognized the value and potential importance of the project for improving workers’ compensation health care beyond the boundaries of their respective institutions. Fourth, the OHS project demonstrates that public-private partnerships can be successful. Of importance here is the willingness and ability of the DLI administrative staff to attract stakeholder groups and private organizations (physician groups and business and labor organizations) to support demonstrations and pilot studies (Wickizer et al. 2001). Finally, we would emphasize the important benefits that result from collaborating with a university. The close collaboration between the DLI and the University of Washington has benefited the OHS project by enhancing the scientific rigor of the intervention and maximizing the opportunity to conduct an evaluation that will better explain how to improve the quality of care in the workers’ compensation system.
Acknowledgments
The research and intervention described in this article were supported by funding provided by the Washington State Department of Labor and Industries. The authors thank Jerry Gluck for his assistance with data analysis. The opinions and conclusions expressed are those of the authors and do not necessarily represent the views of the Department of Labor and Industries.
References
- Baker LC, Krueger AB. Medical Costs in Workers’ Compensation Insurance. Journal of Health Economics. 1995;14:531–49. doi: 10.1016/0167-6296(95)00020-8. [DOI] [PubMed] [Google Scholar]
- Chassin MR, Galvin RW. The Urgent Need to Improve Health Care Quality. Institute of Medicine National Roundtable on Health Care Quality. Journal of the American Medical Association. 1998;280:2533–7. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- Cheadle A, Franklin G, Wolfhagen C, Savarino J, Liu PY, Salley C, Weaver M. Factors Influencing the Duration of Work-Related Disability: A Population-Based Study of Washington State Workers’ Compensation. American Journal of Public Health. 1994;84:190–6. doi: 10.2105/ajph.84.2.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheadle A, Wickizer TM, Franklin G, Cain K, Joesch J, Kyes K, Madden KC, Murphy L, Plaeger-Brockway R, Weaver M. Evaluation of the Washington State Workers’ Compensation Managed Care Pilot Project II: Medical and Disability Costs. Medical Care. 1999;37:982–93. doi: 10.1097/00005650-199910000-00003. [DOI] [PubMed] [Google Scholar]
- Committee on the Quality of Health Care in America. Crossing the Quality Chasm. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- Connis RT, Nickinovich DG, Caplan RA, Arens JF. The Development of Evidence-Based Clinical Practice Guidelines. Integrating Medical Science and Practice. International Journal of Technology Assessment of Health Care. 2000;16:1003–12. doi: 10.1017/s0266462300103071. [DOI] [PubMed] [Google Scholar]
- Daniell W, Wickizer TM, Fulton-Kehoe D, Franklin G. University of Washington, Department of Environmental and Occupational Health Sciences, Occupational Epidemiology and Health Outcomes Program; 2000. Work-Related Carpal Tunnel Syndrome: Clinical Practices and Outcomes for Workers’ Compensation Patients in Washington State. Unpublished report, March. [Google Scholar]
- Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD, Purnell JQ, Wheeler M. Evidence-Based Nutrition Principles and Recommendations for the Treatment and Prevention of Diabetes and Related Complications. Diabetes Care. 2003;26(suppl. 1):S51–S61. doi: 10.2337/diacare.26.2007.s51. [DOI] [PubMed] [Google Scholar]
- Frijling BD, Lobo CM, Hulscher ME, Drenth BB van, Braspenning JC, Prins A, Wouden JC van der, Grol RP. Multifaceted Support to Improve Clinical Decision Making in Diabetes Care: A Randomized Controlled Trial in General Practice. Diabetes Medicine. 2002;19(10):836–42. doi: 10.1046/j.1464-5491.2002.00810.x. 10.1046/j.1464-5491.2002.00810.x. [DOI] [PubMed] [Google Scholar]
- Greenough CG, Fraser RD. The Effects of Compensation on Recovery from Low-Back Injury. Spine. 1989;14:947–55. doi: 10.1097/00007632-198909000-00006. [DOI] [PubMed] [Google Scholar]
- Jadad AR. Evidence-Based Decision Making and Asthma in the Internet Age: The Tools of the Trade. Allergy. 2002;57(74):15–22. doi: 10.1034/j.1398-9995.57.s74.4.x. suppl. 10.1034/j.1398-9995.57.s74.4.x. [DOI] [PubMed] [Google Scholar]
- Javid MJ. A 1- to 4-Year Follow-Up Review of Treatment of Sciatica Using Chemonucleolysis or Laminectomy. Journal of Neurosurgery. 1992;76:184–90. doi: 10.3171/jns.1992.76.2.0184. [DOI] [PubMed] [Google Scholar]
- Johnson WG, Baldwin MI, Furton JF. Why Is the Treatment of Work-Related Injuries So Costly? New Evidence from California. Inquiry. 1996;33:53–65. [PubMed] [Google Scholar]
- Katz JN, Lew RA, Bessette L, Punnett L, Fossel AH, Mooney N, Keller RB. Prevalence and Predictors of Long-Term Work Disability Due to Carpal Tunnel Syndrome. American Journal of Industrial Medicine. 1998;33:543–50. doi: 10.1002/(sici)1097-0274(199806)33:6<543::aid-ajim4>3.0.co;2-r. 10.1002/(SICI)1097-0274(199806)33:6<543::AID-AJIM4>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson M, Donaldson S. To Err Is Human: Building a Safer Health System. Washington, D.C.: National Academy Press; 1999. [PubMed] [Google Scholar]
- Kyes KB, Wickizer TM, Franklin G. Two-Year Health and Employment Outcomes among Injured Workers Enrolled in the Washington State Managed Care Pilot Project. American Journal of Industrial Medicine. 2001;40:619–26. doi: 10.1002/ajim.10001. 10.1002/ajim.10001. [DOI] [PubMed] [Google Scholar]
- Kyes KB, Wickizer TM, Franklin G. Employer Satisfaction with Workers’ Compensation Health Care: Results of the Washington State Workers’ Compensation Managed Care Pilot. Journal of Occupational and Environmental Medicine. 2003;45(3):234–40. doi: 10.1097/01.jom.0000058337.05741.a1. 10.1097/01.jom.0000058337.05741.a1. [DOI] [PubMed] [Google Scholar]
- Kyes KB, Wickizer TM, Franklin G, Cain K, Cheadle A, Madden C, Murphy L, Plaeger-Brockway R, Weaver M. Evaluation of the Washington State Workers’ Compensation Managed Care Pilot Project I: Medical Outcomes and Patient Satisfaction. Medical Care. 1999;37:972–81. doi: 10.1097/00005650-199910000-00002. 10.1097/00005650-199910000-00002. [DOI] [PubMed] [Google Scholar]
- Leatherman S, Berwick D, Iles D, Lewin LS, Davidoff F, Nolan T, Bisognano M. The Business Case for Quality: Case Studies and an Analysis. Health Affairs. 2003;22(2):17–30. doi: 10.1377/hlthaff.22.2.17. 10.1377/hlthaff.22.2.17. [DOI] [PubMed] [Google Scholar]
- Lohr KN, Eleazer K, Mauskopf J. Health Policy Issues and Applications for Evidence-Based Medicine and Clinical Practice Guidelines. Health Policy. 1998;46(1):1–19. doi: 10.1016/s0168-8510(98)00044-x. 10.1016/S0168-8510(98)00044-X. [DOI] [PubMed] [Google Scholar]
- Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, Simard R, Turcotte J, Lemaire J. A Population-Based, Randomized Clinical Trial on Back Pain Management. Spine. 1997;22:2911–8. doi: 10.1097/00007632-199712150-00014. 10.1097/00007632-199712150-00014. [DOI] [PubMed] [Google Scholar]
- Loisel P, Durand P, Abenhaim L, Gosselin L, Simard R, Turcotte J, Esdaile JM. Management of Occupational Back Pain: The Sherbrooke Model. Results of a Pilot and Feasibility Study. Occupational and Environmental Medicine. 1994;51:597–602. doi: 10.1136/oem.51.9.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmud M, Webster B, Courtney T, Matz S, Tacci J, Christiani D. Clinical Management and the Duration of Disability for Work-Related Low Back Pain. Journal of Occupational and Environmental Medicine. 2000;42(12):1178–87. doi: 10.1097/00043764-200012000-00012. 10.1097/00043764-200012000-00012. [DOI] [PubMed] [Google Scholar]
- McGlynn E, Asch S, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr E. The Quality of Care Delivered to Adults in the United States. New England Journal of Medicine. 2003;348(26):2635–45. doi: 10.1056/NEJMsa022615. 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Schuster MA, McGlynn EA, Brook RH. How Good Is the Quality of Health Care in the United States? Milbank Quarterly. 1998;76:517–63. doi: 10.1111/1468-0009.00105. 10.1111/1468-0009.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner JA, Franklin G, Turk DC. Predictors of Chronic Disability in Injured Workers: A Systematic Literature Synthesis. American Journal of Industrial Medicine. 2000;38:707–22. doi: 10.1002/1097-0274(200012)38:6<707::aid-ajim10>3.0.co;2-9. 10.1002/1097-0274(200012)38:6<707::AID-AJIM10>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- Wickizer TM, Franklin G, Fulton-Kehoe D, Mootz R, Turner JA, Smith-Weller T. Patient Satisfaction, Treatment Experience and Disability Outcomes in a Population-Based Cohort of Injured Workers in Washington State: Implications for Quality Improvement. Health Services Research. 2004;39(4):727–48. doi: 10.1111/j.1475-6773.2004.00255.x. Part I. 10.1111/j.1475-6773.2004.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickizer TM, Franklin G, Plaeger-Brockway R, Cheadle A, Kyes K. Workers’ Compensation Managed Care Pilot Project: Final Report to the Legislature. Olympia: Washington State Department of Labor and Industries; 1999. [Google Scholar]
- Wickizer TM, Franklin G, Plaeger-Brockway R, Mootz RD. Improving the Quality of Workers’ Compensation Health Care Delivery: The Washington State Occupational Health Services Project. Milbank Quarterly. 2001;79:5–33. doi: 10.1111/1468-0009.00194. 10.1111/1468-0009.00194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickizer TM, Schulman B, Schwartz S, Drylie D. Occupational Health Services Project: Final Report. Olympia: Washington State Department of Labor and Industries; 1998. [Google Scholar]


