Initiatives designed to improve the quality of health services and to make these services more responsive to patients have a long history. In the British National Health Service (NHS), these initiatives have recently included total quality management, business process reengineering, and quality collaboratives. Drawing on experience outside the health sector, where quality improvement methods of this kind typically originate, NHS policymakers have focused particularly on changing work processes in their quest to improve performance. In so doing they have had to confront not only the inevitable challenges of managing organizational change (Kotter 1996) but also some specific features of health care organizations that make change particularly problematic.
This article analyzes and uses the NHS's experience to identify the lessons for future quality improvement initiatives. At the heart of this article is an account of one recent initiative, the national booked admissions program, which illustrates both the opportunities and the challenges in introducing and sustaining change. By comparing the different impacts of the national booked admissions program on a number of pilots and interviewing the program's participants to discover the reasons why some pilots were more successful than others, we identify those conditions that must be met in order to achieve quality improvements in health care organizations. We also examine the sustainability of the program and the factors that influence sustainability.
In the United Kingdom, the national booked admissions program is important as the first of a series of quality improvement programs that were central to the Blair government's reform of the NHS. The government developed a ten-year plan for investment and reform (Secretary of State for Health 2000), whose rationale was that just doing more of the same was unlikely to resolve the problems confronting the NHS. Doing things differently was also essential to enable resources to be used more appropriately and to deliver services that were responsive to patients. The national booked admissions program thus was the forerunner of an ambitious policy to redesign health services around the patient, and the experience reported here is important in shedding light on the likely impact of the Blair government's reforms.
This program is important internationally as an example of an initiative to use redesign methods to improve health care in order to overcome the quality shortcomings identified in the Institute of Medicine's report Crossing the Quality Chasm (Institute of Medicine 2001). As this report noted, safe, effective, and patient-centered health services require health care organizations based on sound design principles. Consistent with the NHS plan's approach, these principles mean working smarter and not just harder and applying methods developed outside health care to improve performance. The Institute for Healthcare Improvement (IHI) has been at the forefront of efforts in the United States and other countries to use these methods, and it has been prominently involved in much of the NHS's work since 1998. The IHI is a not-for-profit organization based in Boston that seeks to improve health by advancing the quality and value of health care.1 The evidence reported here therefore has implications for the future of the current quality improvement initiatives as well as for the impact of health care reform in the United Kingdom. At the end of this article we will discuss these implications.
A Brief History of the NHS's Quality Improvement Initiatives
Total quality management (TQM) was applied to the NHS in a pilot program initiated by the British Department of Health in the early 1990s. The program was independently evaluated by a research team that also examined the application of TQM to two private-sector organizations (Joss and Kogan 1995). They found that the impact of TQM varied across the NHS pilots, with only a few able to demonstrate substantial change. The reasons for this included a context in which major organizational reform created an unstable environment for work on quality improvement. In addition, the NHS pilots did not invest in training and support for change on the same scale as the private-sector organizations had done. Relying, as they did, mainly on data drawn from interviews with participants in TQM, the evaluators were not able to quantify the extent of the changes that did occur. But they did note that TQM had to be applied to the NHS in a way that made sense to the staff, and they attributed its limited impact in part to the failure to involve doctors fully in its implementation.
Hard on the heels of TQM was an initiative to use business process reengineering at the Leicester Royal Infirmary (LRI) in the mid-1990s. This site was chosen because it was felt to be a relatively well-performing organization that would be receptive to reengineering techniques. As with TQM, the initiative was evaluated independently, using a mixture of quantitative and qualitative methods (McNulty and Ferlie 2002). The evaluation found some evidence of quantitative change resulting from the reengineering, although it fell short of the ambitious claims made at the outset. Part of the reason for this was that the LRI was a high-performing organization and therefore the scope for achieving further change was limited.
Equally important, qualitative data from this study underscored the challenges of applying to health care organizations those quality improvement methods developed in sectors such as manufacturing. This was illustrated by the need to adapt the uniform and top-down approach to reengineering to the LRI's particular circumstances. Indeed, those participating in the initiative found that some of the hospital's units needed to be handled differently depending on the work processes they were trying to change and the attitudes of their staff. Even allowing for this reengineering had a variable effect in the LRI and confirmed the difficulty of introducing change from the top down and without the engagement of the physicians.
These evaluations echo reports on the impact of quality improvement programs in other settings. For example, Shortell and colleagues systematically reviewed the literature in this field based on 55 studies, drawn mainly from the United States (Shortell, Bennett, and Byck 1998). Whereas most of the studies reported progress in improving quality, the authors noted weaknesses in the studies’ designs and cautioned against drawing firm conclusions from the published literature. Having issued this warning, they went on to identify the strengths and limitations of the continuous quality improvement approach, emphasizing the importance of there being a receptive context, sustained leadership, training and support, measurement and data systems, and protection from overburdensome regulation.
Research on reengineering in U.S. hospitals has found a number of barriers and facilitators of organizational change (Walston and Kimberly 1997). The main facilitators were establishing and maintaining a consistent vision, preparing and training for change, planning smooth transitions in reengineering efforts, establishing multiple communication efforts, ensuring strong support and involvement, creating mechanisms to measure progress, establishing authority relationships, and involving physicians. Walston and Kimberly concluded that “in an overall strategy for change these factors have to be linked and to be managed simultaneously” (Walston and Kimberly 1997, 161). This conclusion is supported by research outside health care that points to the importance of making complementary sets of changes in order to improve performance (Pettigrew and Fenton 2000). The difficulty of making complementary changes may help explain the tendency for change in health care organizations to deliver less than expected.
One of the reasons why change is hard to bring about in health care organizations is that these organizations are “professional bureaucracies” (Mintzberg 1983) in which control resides among the professionals delivering services. The ability of managers and others in positions of formal authority to change the behavior of professionals is highly constrained. As Mintzberg noted in his analysis of different organizational types, coordination in professional bureaucracies relies heavily on peer and collegial processes, and change is often slow and disjointed. There are also limits to the degree to which change can be made through management action or what Mintzberg referred to as “government technostructures intent on bringing the professionals under their control” (Mintzberg 1983, 213). Empirical studies of health care organizations, such as those examining the impact of reengineering, have demonstrated the veracity of Mintzberg's insights and the tendency for change to proceed in fits and starts (Denis, Lamothe, and Langley 2001). The implication is that quality improvement initiatives, including those developed outside health care, have to be applied in a way that recognizes the distinctive features of hospitals and other health care organizations, particularly the autonomy of physicians.
The National Booked Admissions Program
Against this background of the NHS's partial but ultimately limited success of total quality management and reengineering, the national patients’ access team (NPAT) was formed in 1998 by the Department of Health to tackle the problems of waiting for treatment that have been endemic to the NHS since its inception. When it was established, the NPAT was a small multidisciplinary team that combined clinical and managerial expertise to redesign hospital services. Members of the team were recruited from their jobs in the NHS to help improve patients’ access and convenience. One of the NPAT's first programs was the national booked admissions program.
The idea behind the program was simple. Instead of being placed on a waiting list and being notified of a hospital admission when there was an opening, patients would agree on an admission date at the time the decision was made to undertake treatment, thereby giving them greater choice and more certainty. This apparently small change in practice had widespread ramifications for work processes in the NHS. Among other things, the introduction of booking required medical specialists to relinquish some control over their work by agreeing to treat patients on a specified future date and by sharing with nurses and administrative staff the responsibility for scheduling the appointment and constructing a list of patients to be treated. Because the autonomy of medical specialists is long established and highly valued by them, those implementing the booked admissions program had to find ways of persuading physicians to participate and of resolving their concerns.
The NPAT's first members had been part of the reengineering initiative at the Leicester Royal Infirmary, which meant that they brought to the booked admissions program a knowledge of the advantages and disadvantages of the reengineering methods. The program ran 24 pilots in different parts of the NHS in England chosen to work with the NPAT to test the feasibility of offering patients booked hospital appointments. Many of the pilots were confined to a single hospital on one site, but others included hospitals on split sites. The most ambitious pilots included a number of hospitals in the area covered by the host health authority. This approach enabled each pilot to decide how to offer patients booked appointments within the national framework provided by the NPAT.
When the NPAT was set up, it was thought that it would be discontinued after two years when its original work had been completed. As things turned out, the team advanced the idea of booking into subsequent waves of development, and it extended its work on redesign in areas such as cancer and coronary heart disease services. The latter programs entailed collaboration with the Institute for Healthcare Improvement in applying the quality collaborative approach to the NHS. Therefore, the national booked admissions program is best seen as a stepping-stone between reengineering and quality collaboratives, developed in a pragmatic way by a group of reflective practitioners (Schon 1983).
In the case of the national booked admissions program, redesigning the services meant looking at the services from the patient's point of view. According to Locock,
An exact definition of redesign is difficult to encapsulate, largely because advocates, both in the USA and in the UK, are continuously developing the concept. However, in essence it entails: describing and understanding the complexity of existing patient processes; examining them critically and challenging taken-for-granted ways of doing things; and redesigning processes to eliminate steps that do not add value to the patient (for example, steps that create delays, duplication or potential for error). Redesign questions not just how things could be done better but whether they need doing at all and by whom. (Locock 2003, 121)
Redesign in some of the booked admissions pilots had primary care physicians schedule a hospital appointment for their patients when they decided to make a hospital referral. More commonly, redesign meant that patients undergoing day surgery made a single visit, rather than several, to the hospital to be seen by a medical specialist and undergo preoperative assessment and tests. When the booked admissions program was extended to inpatient treatment, the redesign affected the use of other hospital services, such as when nurse supervisors were used to improve the flow of patients through hospitals and to avoid delayed discharges. These changes meant that an initiative originally meant to improve access at the front end of service provision, for example, at the time the appointment was made, came to encompass all stages of the patient's pathway, from referral to discharge.
The NPAT supported the first wave of pilots in a number of ways. Consistent with the program's philosophy, learning and development were emphasized as a means of improving quality. Much of the learning and development took place at the monthly meetings that brought together clinicians and managers from the 24 pilots and the NPAT staff to share their experiences and to update and review their progress. These meetings also offered training in specific skills such as redesign and matching capacity and demand. The NPAT supported the pilots in the development of project management, and each member of the team participated in one or more of the steering groups established by the pilots to oversee the implementation of booking. Knowledge of what was happening across the program as a whole enabled the team to use their experience and learning for all the pilots and the subsequent developments.
The criteria for selecting the 24 pilots included having waiting times of or close to six months. This requirement was based on previous research indicating that when patients waited longer than six months, it was difficult for hospitals to make and keep appointments (Bensley et al. 1997). The pilots also were expected to show that medical specialists were interested in and committed to booking. These favorable circumstances were intended to enable the pilots to demonstrate what it was possible to achieve with booking with the provision of both support from the NPAT and additional resources. Between £165,000 and £756,000 was made available to the pilots, the exact amount reflecting the pilots’ different objectives and ambitions. These funds were used for a variety of purposes, the most common being project management, administrative staff, and information and communications technology. Almost £10 million was allocated for the 18 months covered by the first program (October 1998–March 2000), and thereafter the pilots were expected to fund recurrent costs from their mainstream budgets.
Offering patients an opportunity to book a date that is convenient for them rather than placing them on a waiting list symbolizes the challenge of reforming the NHS to make it more accessible and responsive to patients. It also resonates with the simple rules for improving performance set out in Crossing the Quality Chasm (Institute of Medicine 2001). The Blair government made the national booked admissions program one of the centerpieces of its reform of the NHS and assigned the NPAT to extend booking to all hospitals in subsequent waves of development. The decision announced in 2000 to establish the NHS Modernisation Agency to lead an ambitious, systemwide program of reform, incorporating the NPAT's work, signified the way in which the redesign of work processes had come to occupy a central place on the NHS agenda.
Methods and Results
To evaluate the impact of booking, we collected quantitative data from the pilots for three time periods. Data from the first quarter of 1999 enabled us to establish a baseline period; data from the first quarter of 2000 provided a snapshot of what had been achieved at the end of the pilot period; and data from the first quarter of 2001 allowed us to determine whether booking was sustained after the end of the pilot period. The main outcome measure at the end of these periods was the proportion of patients waiting with a date for their surgery.
Along with collecting and analyzing quantitative data, we conducted 257 interviews, either in person or by telephone, which included 152 managers, 44 medical specialists, 21 nurses, 12 administrative and clerical staff, 12 general practitioners, and 16 others. Data from these interviews were supplemented by a questionnaire survey of project managers to explore the reasons for our outcomes. We selected four pilots as case studies for more detailed analysis. In these pilots, we conducted questionnaire surveys of medical specialists and general practitioners, analyzed relevant papers and documents, and sat in on meetings. Our final research report presents the full results of the evaluation and contains additional information on the methods we used (Ham et al. 2002).
The main focus of the program's first wave was offering patients an opportunity to book appointments for day surgery. Twenty-three of the 24 pilots offered booked appointments for day surgery, and 20 of them supplied data for analysis. We tested program-level changes in performance for statistical significance, using a weighted paired t-test based on the logistic transform of clustered (pilot-level) data (Donner and Donald 1987). For the program as a whole, the proportion of patients waiting with a date increased from 51.1 to 72.7 percent between the end of March 1999 and the end of March 2000 (p < .001) and then fell back from 72.7 to 66.2 percent by the end of March 2001 (p= .651).
The pilots’ achievements varied. Most obvious were the wide differences in the proportion of patients waiting with a date during and after the first wave. The pilots also differed in their scope, defined here as the proportion of all day surgery included in the pilot. Figure 1 combines the results for these two measures and shows that among pilots with more than half of all day-surgery admissions in the first quarter of 2001 (those exceeding 50 percent, represented in the graph by the darker columns) only three—pilots 16, 4, and 12—achieved a high level of booking, defined as more than 80 percent of patients with a date (represented in the graph by the lighter columns). Seven other pilots—pilots 14, 19, 18, 20, 17, 6, and 2—also achieved a high level of booking, but as the figure illustrates, their scope was much more limited (that is, under 50 percent of all day-surgery admissions).
FIG. 1.
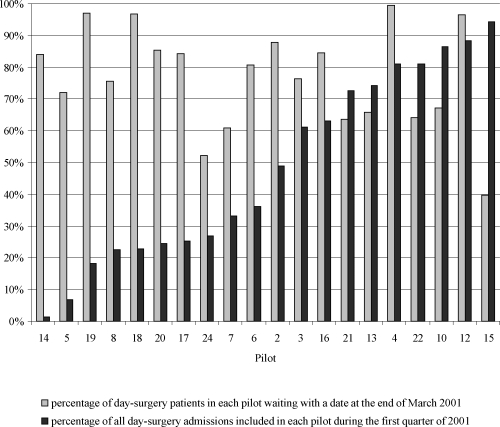
Percentage of patients in 20 of the day-surgery pilots waiting with a date at the end of March 2001. Each number refers to a different pilot.
The results for inpatients followed a pattern similar to that for day surgery. Sixteen of the 24 pilots offered booked appointments for inpatient surgery, and 14 of them supplied data for analysis. For the program as a whole, the proportion of patients waiting with a date increased from 39 to 50.6 percent between the end of March 1999 and the end of March 2000 (p= .099) and then fell back from 50.6 to 40.7 percent by the end of March 2001 (p= .599).
The pilots varied widely in both the proportion of patients waiting with a date and their scope. Figure 2 shows that among pilots with more than half of all inpatient admissions in the first quarter of 2001 (those exceeding 50 percent, represented in the graph by the darker columns) only one—pilot 4—achieved a high level of booking, defined as more than 80 percent of patients with a date (represented in the graph by the lighter columns). Three other pilots—pilots 14, 7, and 11—also achieved a high level of booking, but their scope was much more limited. The results show that booking patients for inpatient surgery was less well developed than booking patients for day surgery, and we discuss the reasons for this later.
FIG. 2.
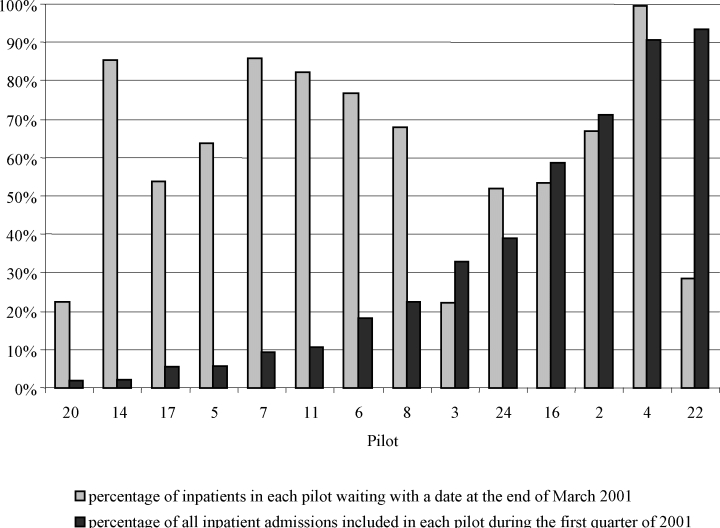
Percentage of patients in 14 of the inpatient pilots waiting with a date at the end of March 2001. Each number refers to a different pilot.
The story that emerges from these data has two major themes. The first is that although the pilots made substantial progress in increasing booking for day surgery during the pilot period, some of this progress was eroded in the subsequent year. Also, almost all the gains for inpatient surgery made during the pilot period were lost, thus raising the issue of the sustainability of quality improvement initiatives of this kind. Although previous research on quality improvement in health care has rarely explored sustainability, the data we gathered enable us to start closing this gap in knowledge.
The second major theme was the wide variations in what was achieved, suggesting that some pilots were more receptive to change than others. In the remainder of our analysis, we will explore both the variations among pilots and the difficulty of sustaining progress beyond the end of the pilot period.
Variation and Sustainability
To explore variation and sustainability, we switched from analyzing the quantitative findings to looking at the service redesign from the perspective of the participants in the booked admission program. To do this, we used the results of our interviews with the program's participants, the findings of the case studies, and the surveys of project managers and medical specialists carried out during the evaluation.
In making sense of the evidence gathered from these different sources, we kept in mind the argument of Pettigrew, Ferlie, and McKee (1992) that research on change in health care organizations should be processual, comparative, pluralistic, and historical. Adopting a processual focus means looking at actions and behaviors and not just the organizational structures involved. A comparative perspective assesses the experience of a range of organizations. Drawing on the views of different actors like physicians and managers meets the pluralistic criterion, and a historical focus requires attending to previous experience in booking and related areas. In a more recent paper, Pettigrew, Woodman, and Cameron (2001) reaffirmed and extended this framework for studying change, arguing that change should be analyzed along with continuity and also examined over time. The importance of these points is reflected in the experience of the booked admissions program.
Besides this framework, we also used Pawson and Tilley's approach (Pawson and Tilley 1997) to realistic evaluation. They contended that the results of policy interventions can be explained in terms of the interplay between the context of change and the mechanisms of change. We therefore began our search for explanations by examining the context in which the booked admissions program was implemented and then turned to the mechanisms used in the program. Along the way, we looked at the results of research on quality improvements in health care in other settings (e.g., Shortell, Bennett, and Byck 1998) to help identify the similarities and the differences between our work and what is already known about the challenges of improving health care organizations.
Although allowing patients to schedule their day surgery rather than being placed on a waiting list had been tested in a number of local initiatives before the national booked admissions program, the launch of the program in 1998 had the effect of creating a national context that supported booking. This was important in that it signaled to NHS managers and physicians that booking was a high political priority, and so time and energy that might have been spent elsewhere should be used to support booking. The other relevant feature of the national context was the establishment of the NPAT to lead the program. The interviews with the program's participants indicated strong support for the team's role and the advice and expertise they could offer the pilots. Of particular value was the training and development offered by the team for service redesign.
Despite the importance of the political priority associated with booking and the NPAT's work, the variations in the pilots’ outcomes indicate that the local context had more influence on what was achieved than the national context did. These variations cannot be explained by factors in their external environment, given that the pilots received similar advice and support from the NPAT and implemented booking in the same national policy context. Rather, the variations derived from factors within the organizations themselves and the extent to which there was a receptive context for quality improvement initiatives of this kind. The importance of having a receptive context has been noted in previous studies (Pettigrew, Ferlie, and McKee 1992; Shortell, Bennett, and Byck 1998), and our study confirmed its significance. Data from the interviews with participants and the survey of project managers suggest that the main ingredients of a receptive context were previous experience with booking; the existence of the preconditions needed to support booking, such as relatively short waiting times for treatment; and organizational leadership. When these conditions were present, booking developed further and faster than where they were absent.
The role of the local context can be illustrated by contrasting two of the pilots chosen for more detailed analysis as case studies. The first pilot was a 400-bed general hospital in inner London that already was booking many patients for day surgery before the program was launched. Waiting times were under six months, and booking had become routine, owing to the leadership of the chief executive and the support of most medical specialists. This pilot achieved and sustained booking to the point that it had become the accepted way of serving patients throughout the hospital. Accordingly, the main challenge for this hospital was building on and sustaining what it had already achieved rather than undertaking a major innovation. This challenge was made easier by the existence of a relatively young group of medical specialists who believed that offering patients an opportunity to schedule their surgery was the right thing to do.
The second pilot was a 580-bed general hospital in a spa town in southwest England that had little experience with booking. Although the hospital made progress in introducing and sustaining booking in three specialties during the program, the planned extension to the rest of day surgery did not succeed. The extension was stymied by long waiting times in other specialties and by funding and capacity constraints. The leadership provided by the chief executive and physicians in the three specialties being booked was not strong enough to overcome these constraints. In addition, there were problems in maintaining the project management and introducing information and communications technology to support the booking. Unlike the first pilot, this hospital had little previous experience with booking, and the persistence of waiting times beyond the six-month maximum deemed necessary to schedule day surgery proved to be an insurmountable obstacle.
The experience of the second pilot illustrates a further point, namely, that the impact of booking varied within as well as among pilots, indicating that receptiveness to change affects both hospitals as organizations and specialties within hospitals. Across the program as a whole, it was unusual for booking to take hold in all specialties included in a pilot, even in those pilots that made the most progress. This is because NHS hospitals, as organizations, are made up of clinical teams with much flexibility in organizing their work. It is within these so-called microsystems (Nelson et al. 2002) that changes in work process must become firmly established. Our research indicates that microsystems varied in their receptiveness to change and that the most successful pilots were able to work with these variations in order to make progress.
A number of mechanisms determined how booking was implemented in the first wave. Each pilot was expected to arrange for the project's management, using a project team and a steering group. Interviews with participants testified to the importance of these arrangements, particularly full-time project managers dedicated to introducing booking and sustaining it beyond the end of the pilot period. Those pilots whose project managers had responsibilities in areas other than booking or who moved on to new roles during the program reported greater difficulties than those who did not.
Our survey of project managers indicated that the implementation processes also were important. Some of the pilots began by working with medical specialists who were familiar with booking and enthusiastic about it. Booking was then extended to other specialists as waiting times were shortened, thus demonstrating what was possible. In practice, implementation was rarely linear or unproblematic, and as the outcome measures show, there were wide variations in what was achieved and in sustaining progress after the end of the pilot period. Nevertheless, the opportunity to make the change incrementally and to learn while doing it was seen by those we interviewed to be important to making progress.
Another helpful mechanism was the provision of training and development opportunities. As we noted, some of these opportunities were provided by the NPAT, and some were arranged by the pilots themselves. The training and development included skills in service redesign and the provision of time away from the job for the staff to discuss and agree on new ways of working. Training sessions were reported to be valuable in enabling staff to understand what was involved in booking appointments and allowing them to air and deal with their concerns. These concerns often focused on changes in the role of different staff groups, as when the medical specialists’ secretaries had to relinquish to nurses or dedicated booking staff their control over making appointments for patients. Skills in service redesign gave staff the tools they needed to look at the services from the patient's point of view and to streamline them in the interest of both efficiency and responsiveness.
Flexibility in the methods used to schedule surgery was important as well, in both the members of staff making the appointment and the use of paper or electronic systems. Consistent with its philosophy, the NPAT did not insist on a particular booking method, except to caution against using complex information and communications technology “solutions.” This advice proved wise in that those pilots that did invest in new forms of electronic booking had difficulties or experienced delays. An example was the pilot described earlier that was able to implement booking in only three specialties. This pilot placed greater emphasis on electronic booking than did any of the others, and its difficulties in implementing the new information technology system was one of the factors contributing to its limited progress. By comparison, pilots that built on established methods or followed the preferences of medical specialists had fewer problems, even if the result was the coexistence of different approaches. The same applied to the staff member making the appointment, with pilots using physicians, nurses, and administrative staff in different combinations, depending on local traditions and preferences.
The availability of extra funds helped establish booking by investing in additional staff and equipment and paying for training and development. This included offering incentives to physicians to participate in booking, for example, by buying computers to enable doctors to schedule patients directly and equipment to help them assess patients. Extrinsic incentives of this kind worked alongside the intrinsic desire of physicians to offer a high-quality service to their patients. Booking appealed to this intrinsic desire when it reduced the number of canceled appointments and of patients failing to appear, thereby allowing medical specialists to use their time more productively.
The mechanisms of change used in the booked admission program were similar to the rules for disseminating innovations in health care proposed by Berwick (2003). These rules are finding and supporting innovators, investing in early adopters, enabling early adopter activity to be observed, encouraging and supporting reinvention of change, creating room for change, and leading by example. Despite following these rules, however, the program encountered difficulties in implementation and sustainability. One of the main causes was the attitude of medical specialists, which we now examine in more detail.
Medical Power
While most specialists in the pilots supported booking, some clinical teams and specialties were not receptive to change. In a resource-limited NHS, these teams’ objections were that the NHS lacked the capacity to enable appointments to be booked. This was perceived to be a particular problem in relation to booking for inpatient surgery for which—unlike the case of day surgery—hospitals did not have beds and operating theaters used solely for the treatment of patients with scheduled appointments. As a consequence, the demands of patients admitted as emergencies made it difficult to honor the inpatients’ booked appointments. This helps explain why scheduling inpatient surgery developed much more slowly than did scheduling day surgery.
To understand the medical specialists’ views, we conducted a questionnaire survey of 133 specialists involved in booking in three of the pilots chosen as case studies. The response rate was 77 percent. About one-quarter of respondents were skeptical of booking or were not convinced of its value. Given that the pilots were selected in part because the medical specialists showed an interest in and a commitment to booking, the sizable minority of specialists who doubted its benefits indicates the challenges of implementing this change. Capacity constraints and long waiting times were the main factors the specialists cited as holding back the development of booking, but our interviewees also offered other reasons.
For example, some physicians believed that treating those patients with the greatest clinical needs should be given priority over offering increased convenience to patients with less severe medical conditions: “I think it is an appalling use of taxpayers’ money. Instead, the money should be directed toward serious diseases and not toward a gimmick…. This is wallpapering by the government.” To some specialists, this meant that the political priority attached to booking made its introduction harder rather than easier. As one surgeon told us: “You tell Tony Blair that he can give me his diary and he can see how he likes to have someone else fill it for him.” In addressing the challenge of medical autonomy, the booked admissions program tried to shift from a service traditionally based on the main group of professionals delivering care to one centered on the patients receiving that care. Making this shift required a number of changes in work processes that affected different staff groups. Medical specialists in hospitals were the most affected, in that many had to change their established ways of working in order to offer patients increased convenience. The secretaries of these medical specialists were affected as well, and their antipathy to new ways of working might have influenced the specialists’ willingness to participate.
As a concrete example, specialists had to plan their leave sufficiently far ahead in order to keep their scheduled appointments. Some specialists were reluctant to do so for fear that this would reduce their ability to alter their schedules on short notice, for example, to attend an academic meeting or take a vacation. And by requiring specialists to plan their work ahead, booking also reduced the autonomy traditionally enjoyed by NHS physicians. The importance that specialists attached to their autonomy was exemplified by their rejection of a new employment contract in 2002 that offered increases in remuneration in return for managers having greater influence over the specialists’ work. The majority of specialists were willing to forgo the proposed pay increases in order to keep control of their work (Wright 2002).
The certainty that booking offers to patients also restricted specialists’ ability to undertake private work on short notice. This is because booking requires specialists to be present at certain times to carry out their NHS responsibilities. Because many of the specialists in the booked admissions program combine NHS and private work, their opportunities to earn money from treating patients privately are thus curtailed. In addition, some specialists see the drive to cut waiting times to facilitate the introduction of booking as a threat to their private practice, by reducing the demand for treatment in the private sector as the NHS queues grow shorter.
Booking was introduced into a service in which in the past some doctors tended to maintain long waiting lists and waiting times as an indication of their popularity, as well as an opportunity to increase their income through private work. The values implied by this behavior are the reverse of those needed to make booking work. Changing these values thus is much more difficult than simply overcoming a reluctance to adopt new ways of working or to question a different interpretation of NHS priorities. Among other things, it depends on the willingness of managers and physicians who support innovations like booking to challenge medical specialists when appropriate.
Our evaluation shows that this is precisely what happened in those pilots that achieved high levels of booking. A combination of chief executives, who made it clear that booking was a high priority for the organization, and medical champions willing to lead by example and exert peer pressure on reluctant colleagues were often effective in overcoming objections to booking by physicians not receptive to change. A good example was one of the pilots chosen as a case study (pilot 16) whose leadership by the chief executive of a health authority over a number of years in making services accessible and responsive was instrumental in enabling booking to be introduced across a wide scope of activities. In this pilot, the development of booking was facilitated by an organizational culture that valued convenience for the patients. The chief executive used several measures to improve access and convenience and was willing to personally challenge practices that got in the way (Locock 2002). Also important to this pilot was a history of short waiting times, together with some previous experience of booking, which contributed to this being a receptive context for improvement.
Yet even in this pilot, booking by medical specialists was not universal, demonstrating that receptive contexts with effective leadership may not be enough to make new practices the norm. As we have noted, this is because hospitals as organizations are made up of specialties and service areas that provide a powerful focus for professional work and are themselves relatively autonomous. If specialties and service areas are not receptive to change, or contain subcultures opposing the values and priorities of organizational leaders, quality improvements like booking may struggle to become established across the organization. This is, of course, consistent with the conclusion from reengineering at the Leicester Royal Infirmary (McNulty and Ferlie 2002) and by Shortell and colleagues that many quality improvement programs result in only pockets of innovation rather than organization-wide change (Shortell, Bennett, and Byck 1998).
Therefore, managing a change like the introduction of booking depends on understanding and working with the culture of the organizations and professions concerned and focusing on those mechanisms that affect implementation. By culture, we mean the values, beliefs, and norms that shape actions and behaviors in hospitals and health care organizations. In practice, the challenge is knowing how to do this given the elusive nature of culture and the difficulty of changing deeply held beliefs, long established practices, and “the way things are done around here” (Davies, Nutley, and Mannion 2000). It also is important to recognize the many cultures in hospitals based on occupation, specialty, and other affiliations.
Cultural change presents a particular challenge insofar as it requires persuading staff to give priority to the organization's values over those of their profession or specialty, when their loyalty to the organization may matter less than that to other affiliations. The fact that some of the pilots in our study made more progress than others, even though all had to overcome the conservatism built into professional practices, suggests that organizational cultures do have an impact on the implementation of quality improvement initiatives like the booked admissions program. These cultures depend on the nature and style of the organization's leaders—both managerial and clinical—and their ability to secure the acceptance of values and behaviors that support new work processes.
Recognizing that changing cultural obstacles is not easy, our evidence indicates that many factors are relevant. In the three pilots that achieved a high level of booking, the factors that made a difference were
The recruitment of a young group of physicians in the first pilot who were willing to change their current work processes (pilot 4).
The sustained commitment from a chief executive in the second pilot to the implementation of booking as part of a wider and longer-term strategy to improve access (pilot 16).
An effective change management program in the third pilot, led by a chief executive and a project manager, that concentrated on working with enthusiasts and overcoming the anxiety of physicians (pilot 12).
These observations support the argument that cultural and organizational change are inseparable. In most circumstances, organizational and cultural change must be negotiated and accomplished over time, except when a real or perceived crisis threatens the organization's survival and requires more immediate intervention. The need to make organizational and cultural change over time through the actions of many individuals is consistent with the evaluation of reengineering at the Leicester Royal Infirmary:
Significant change in clinical domains cannot be achieved without the co-operation and support of clinicians…. Clinical support is associated with process redesign that resonates with clinical agendas related to patient care, services development and professional development…. To a large degree interesting doctors in re-engineering involves persuasion that is often informal, one consultant at a time, and interactive over time … clinical commitment to change, ownership of change and support for change constantly need to be checked, reinforced and worked upon. (Bowns and McNulty 1999, 66–7)
We would add that the experience of the booked admissions program demonstrates that work processes can be changed through quality improvement initiatives when the context for change and implementation processes create conducive conditions. Reflecting the complexity of health care organizations, improvement tends to result from the interplay of different factors. Figure 3 illustrates the specific factors relevant to the booked admissions program. To achieve substantial change that can be sustained over time requires as many of the conditions favorable to quality improvement as possible. In the case of the program reviewed here, particularly important were a previous history of booking, sufficient capacity to enable waiting times to be reduced to the point that widespread booking was possible, effective leadership, and an organizational culture conducive to bringing about change.
FIG. 3.
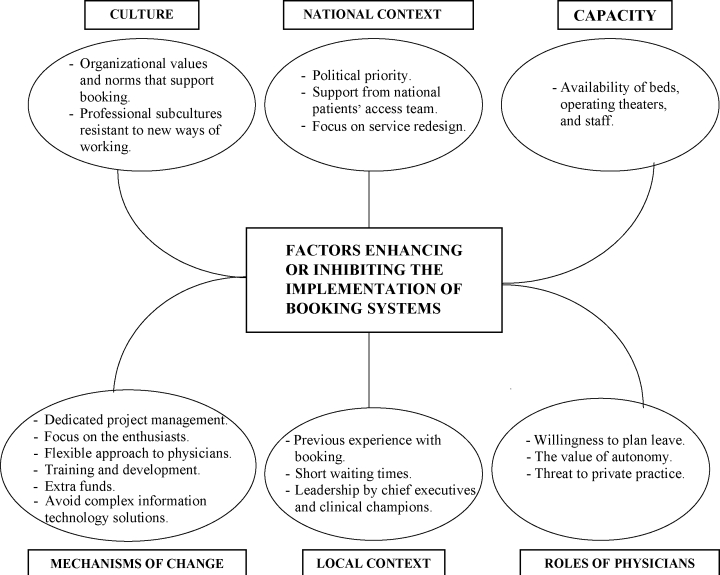
Factors enhancing or inhibiting the implementation of booking systems.
Conclusions and Implications
The research reported here underscores the difficulty of making changes in health care organizations. As previous work in the United Kingdom and elsewhere has shown, the power of physicians, the inertia built into established ways of working, and the effort needed to implement new work processes help explain why the impact of quality improvement initiatives is varied and often limited. And even when changes are made, there is no guarantee that they will be sustained and extended, because in health care organizations, the risk of taking two steps forward and one back is always present (Plsek and Wilson 2001). The difficulties in sustaining quality improvements are among this study's most significant contributions to the literature in this area and stresses the importance of analyzing change over time and examining continuity along with change (Pettigrew, Woodman, and Cameron 2001).
What, then, does our study contribute to promoting quality improvement programs? First, achieving and sustaining change require managing a series of dualities (Pettigrew and Fenton 2000; Pettigrew, Ferlie, and McKee 1992). For the booked admissions program, the key dualities were a national political commitment and local management and clinical leadership; external support from the NPAT, linked to training and change management within the organizations making the change; attention to the technical aspects of change such as information technology, as well as the implications for staff and their roles; and a focus on increasing capacity together with working on service redesign.
The balance between a top-down and a bottom-up approach is precarious. Whereas quality improvement in health care cannot be imposed from the top down without taking into account the realities of professional work, change will continue to be made only in pockets of innovation unless a bottom-up commitment from the staff making the changes is combined with organizational and systemwide leadership. Leadership from the top depends on chief executives and medical champions, and commitment from the bottom means working with clinical teams and microsystems.
The second point, which is closely linked to the first, is the need for action at different levels to achieve changes in performance. Ferlie and Shortell (2001) argued, on the basis of their analysis of experience in the United Kingdom and the United States and with the Institute of Medicine (2001), that there are at least four levels of change for improving quality: individual, team, organization, and the larger system. The main focus of our research was on individuals and teams, with some attention also to organizations. This focus helps explain why the progress in introducing booking tended to be concentrated in specialties that were receptive to this way of working and was rarely implemented effectively across a whole hospital or local health system. Designing quality improvement programs that stimulate change at all four levels is much more demanding than change that is directed at clinical teams willing to embrace new practices.
Third, it is important to be realistic about the time needed to bring about and sustain change. The evidence we gathered suggests that quality improvement often takes longer than expected to take hold and longer still to become widely and firmly established within an organization. Those in the booked admissions program often did not realize this fact, which meant that the time allowed to test new ways of working was insufficient. Also, the challenges of sustaining improvement were not always understood. The regression in booking in the year after the pilot program ended provided evidence of the need for the momentum that accompanies quality improvement initiatives to be maintained over time and for the pilot period to be long enough to overcome challenges and obstacles. Establishing long-term responsibility for quality programs at the outset is therefore essential.
Fourth, the staff affected by quality improvement programs must be able to see that they, as well as the patients, will benefit from the changes. Extrinsic incentives have a part to play in this, but equally important to the program evaluated here was the need to demonstrate that fewer patients failed to keep their appointments, fewer canceled their appointments, and they used their clinical sessions more efficiently. The specific benefits for staff will vary depending on the change but will always be needed to compensate for the effort to make the change. As other work has shown (Denis et al. 1999), without benefits, professionals such as physicians are likely to block improvements and frustrate the ambitions of reformers.
Finally, and to return to our starting point, our work contains lessons for the future of health care reform in the United Kingdom. Specifically, it suggests that redesigning work processes can improve the performance of health services but that the impact of redesign depends on the local context of the change and the way in which the mechanisms of change are used. In a health care system as large and complex as Britain's National Health Service, it remains an open question as to whether these challenges can be overcome.
There are also implications from our analysis for the current generation of quality improvement initiatives as a whole. According to the Institute of Medicine's report, Crossing the Quality Chasm,
The challenge before us is to move away from today's highly decentralized, cottage industry to one that is capable of providing primary and preventive care, caring for the chronically ill, and coping with acute and catastrophic events. To meet this challenge, there must be a commitment to organising services around common patient needs and applying information technology and engineering concepts to the design of care processes. (Institute of Medicine 2001, 30)
The evidence presented here suggests that this is much easier said than done. The Institute for Healthcare Improvement's emphasis on quality collaboratives and the application of improvement methods drawn from other sectors appear to hold promise, notwithstanding the dearth, until recently, of independent assessments of their impact (Ovretveit et al. 2002). In one early National Health Service example, during its lifetime a quality collaborative made a number of improvements in orthopedic services, although these improvements did not result in systematic changes (Bate, Robert, and McLeod 2001). Together with the results reported here, this example suggests the need to be cautious about the more ambitious claims made for quality improvement methods.
Berwick's analysis of the barriers to making innovations in health care acknowledges the difficulties that confront those promoting improvement and recognizes that there are “no shortcuts” (Berwick 2003, 1974). Again, this emphasizes the importance of allowing time for change to occur and of building up the capacity for change and reform within hospitals and other health care organizations. It is especially important to engage physicians in quality improvement and, as in the booked admissions program, to support the innovators in demonstrating that change is possible. The Quality Chasm is most likely to be crossed through a long slow journey rather than a single massive leap.
Endnote
Further information about the IHI can be found at http://www.ihi.org.
References
- Bate SP, Robert G, McLeod H. Birmingham: Health Services Management Centre, University of Birmingham; 2001. Report on the “Breakthrough” Collaborative Approach to Quality and Service Improvement within Four Regions of the NHS. [Google Scholar]
- Bensley D, Halsall J, McIlwain C, Scott L. Total Booking systems for Elective Admission: Feedback from Site Visits. 1997. Unpublished manuscript, Department of Health, Leeds.
- Berwick D. Disseminating Innovations in Health Care. Journal of the American Medical Association. 2003;289(15):1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- Bowns I, McNulty T. Re-engineering Leicester Royal Infirmary: An Independent Evaluation of Implementation and Impact. Sheffield: School of Health and Related Research, University of Sheffield; 1999. [Google Scholar]
- Davies H, Nutley S, Mannion R. Organisational Culture and Quality of Health Care. Quality in Health Care. 2000;9:111–9. doi: 10.1136/qhc.9.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denis J-L, Lamothe L, Langley A. The Dynamics of Collective Leadership and Strategic Change in Pluralistic Organizations. Academy of Management Journal. 2001;44(4):809–37. [Google Scholar]
- Denis J-L, Lamothe L, Langley A, Valette A. The Struggle to Redefine Boundaries in Health Care Systems. In: Brock D, Powell M, Hinings CR, editors. Restructuring the Professional Organization. London: Routledge; 1999. pp. 105–30. [Google Scholar]
- Donner A, Donald A. Analysis of Data Arising from a Stratified Design with the Cluster as Unit of Randomisation. Statistics in Medicine. 1987;6:43–52. doi: 10.1002/sim.4780060106. [DOI] [PubMed] [Google Scholar]
- Ferlie E, Shortell S. Improving the Quality of Health Care in the United Kingdom and the United States: A Framework for Change. Milbank Quarterly. 2001;79(2):281–315. doi: 10.1111/1468-0009.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham C, Kipping R, McLeod H, Meredith P. Capacity, Culture and Leadership: Lessons from Experience of Improving Access to Hospital Services. Birmingham: Health Services Management Centre, University of Birmingham; 2002. [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- Joss R, Kogan M. Advancing Quality: Total Quality Management in the National Health Service. Buckingham: Open University Press; 1995. [Google Scholar]
- Kotter J. Leading Change. Boston: Harvard Business School Press; 1996. [Google Scholar]
- Locock L. Birmingham: Health Services Management Centre, University of Birmingham; Factors contributing to the achievement of low waiting times in Dorset. [Google Scholar]
- Locock L. Redesigning Health Care: New Wine from Old Bottles? Journal of Health Services Research and Policy. 2003;8(2):120–122. doi: 10.1258/135581903321466102. [DOI] [PubMed] [Google Scholar]
- McNulty T, Ferlie E. Reengineering Health Care: The Complexities of Organizational Transformation. Oxford: Oxford University Press; 2002. [Google Scholar]
- Mintzberg H. Structure in Fives: Designing Effective Organizations. Englewood Cliffs, N.J.: Prentice-Hall; 1983. [Google Scholar]
- Nelson E, Batalden P, Huber T, Mohr J, Godfrey M, Headrick L, Wasson J. Microsystems in Health Care, Part 1: Learning from High-Performing Front-line Clinical Units. Journal on Quality Improvement. 2002;28(9):472–93. doi: 10.1016/s1070-3241(02)28051-7. [DOI] [PubMed] [Google Scholar]
- Ovretveit J, Bate P, Cleary P, Cretin S, Gustafson D, McInnes K, McLeod H, Molfenter T, Plsek P, Robert G, Shortell S, Wilson T. Quality Collaboratives: Lessons from Research. Quality and Safety in Health Care. 2002;11:345–51. doi: 10.1136/qhc.11.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997. [Google Scholar]
- Pettigrew A, Fenton E. The Innovating Organization. London: Sage; 2000. [Google Scholar]
- Pettigrew A, Ferlie E, McKee L. Shaping Strategic Change. Making Change in Large Organizations: The Case of the National Health Service. London: Sage; 1992. [Google Scholar]
- Pettigrew A, Woodman RW, Cameron KS. Studying Organisational Change and Development: Challenges for Future Research. Academy of Management Journal. 2001;44(4):697–713. [Google Scholar]
- Plsek P, Wilson T. Complexity Science: Complexity, Leadership, and Management in Healthcare Organisations. BMJ. 2001;323:746–9. doi: 10.1136/bmj.323.7315.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schon DA. The Reflective Practitioner: How Professionals Think in Action. New York: Basic Books; 1983. [Google Scholar]
- Secretary of State for Health. The NHS Plan. London: HMSO; 2000. [Google Scholar]
- Shortell S, Bennett C, Byck G. Assessing the Impact of Continuous Quality Improvement on Clinical Practice: What It Will Take to Accelerate Progress. Milbank Quarterly. 1998;76(4):593–624. doi: 10.1111/1468-0009.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walston S, Kimberley J. Reengineering Hospitals: Experience and Analysis from the Field. Hospital and Health Services Administration. 1997;42(2):143–63. [PubMed] [Google Scholar]
- Wright O. Freedom More Important Than a Rise in Pay, Says Surgeon. The Times. 2002 October 29. [Google Scholar]


