I would like to begin by taking you back to the years preceding the Second World War, because the problem I wish to discuss must be seen as a historical process if it is to be understood. I am going to talk about a particular chapter in the history of disease, a chapter characterized by the surprising fact that the net effect of successful technical innovations used in disease control has been to raise the prevalence of certain diseases and disabilities by prolonging their average duration. The beginning of this historical period coincided with the introduction of the systematic clinical trial and of the sulfonamides in 1937 and 1938.
The health situation regarding modern man's chronic diseases and disabilities immediately before that period was well described by Osler in 1904 in his famous textbook, The Principles and Practice of Medicine, and the same description was still present in the 1935 edition revised by McCrae (Osler, 1935):
There is truth in the paradoxical statement that persons rarely die of the disease with which they suffer. Secondary terminal infections carry off many patients with incurable disease.
Osler could not have anticipated the coming successes in curing the terminal infections associated with these incurable, or chronic, diseases that were to be introduced by a new era of medical research—the era of the clinical trial. What happened was that at the beginning of the era, in 1936, on a very small grant from the Rockefeller Foundation, a group of investigators searching for a cure for puerperal fever revealed to the world the antibacterial powers of sulfanilamide. The impact that sulfa drugs were to have on pneumonia, the most frequent of the terminal infectious diseases at that time, was as dramatic as it was serendipitous. Figure 1 shows the steep decline in death from pneumonia after 1936, following the introduction of sulfa drugs.
Figure 1.
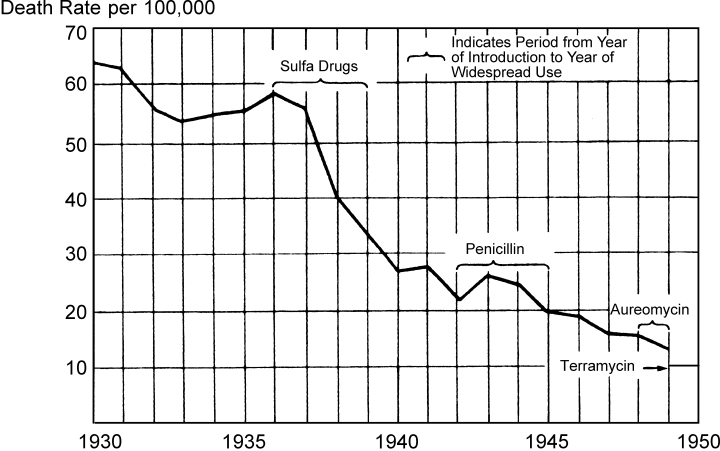
Curve of the Mortality Rate per 100,000 from Pneumonia between 1930 and 1950 as Prepared by the Metropolitan Life Insurance Company
From Reimann, Hobart A., Pneumonia, 1954. Courtesy of Charles C. Thomas, Publisher, Springfield, Illinois.
Coincidental to the discovery of the sulfonamides was the invention of the clinical trial, the seeds of which had been developing for many years. In 1937 Professor A. Bradford Hill gave researchers a means for comparing a new treatment with an old one on a carefully selected population, and getting a definitive answer, usually within a few months. Quite by accident, the first new treatment that was tested adequately by the clinical trial was sulfanilamide. The clinical trial was then used to examine the efficacy of treatments whose effects, while not so apparent as those of the sulfa drugs, represented major clinical successes.
The rate at which new, effective remedies were discovered accelerated suddenly. The most important of these turned away impending death by simple techniques. The once fatal disease or injury might be in an otherwise healthy or vigorous person. As it turned out, these successful life-saving measures were disproportionately needed in people suffering from an incurable disease or disability. But these new techniques did not cure the chronic diseases, nor did they prevent them in the next patient.
If we assume no change in the age-specific annual incidence of the diseases formerly terminated early by now curable infections, and that, in fact, the anti-infectious drugs have been postponing death, then the average duration of these conditions has presumably been increasing. Therefore at the same time that persons suffering from chronic diseases are getting an extension of life, they are also getting an extension of disease and disability.
It is obvious that, with increasing duration, we would expect the proportion of the population in any given age group suffering from these conditions to rise. And, in fact, as the result of advances in medical care, we are seeing a rising prevalence of certain chronic conditions which previously led to early terminal infections, but whose victims now suffer from them for a longer period. The goal of medical research work is to “diminish disease and enrich life” (Gregg, 1941), but it produced tools which prolong diseased, diminished lives and so increase the proportion of people who have a disabling or chronic disease.
That is a major but unintended effect of many technical improvements stemming from health research. These increasingly common chronic conditions represent the failures of success. Their growing prevalence and longer duration are a product of progress in health technology.
Mongolism
How much does the elimination of fatal complications increase the proportion of the population with a specific chronic condition? That depends on how much the duration is increasing.1 The increased duration has been measured best for mongolism (Down's syndrome).
Mongolism has long been known to be associated with a high susceptibility to respiratory infections (Record and Smith, 1955; Penrose, 1932). Children born with Down's syndrome rarely reached maturity until the 1940 birth cohort started to age. Persons in that cohort are now passing their thirty-sixth birthdays. However, their predecessors who managed to survive the first few years of life have also experienced an increased life expectancy—a much larger increase than that of the general population. For the first time in human history we are seeing 70-year-old mongoloids. Spain's excellent pathology text (1963) on diseases resulting from medical advances does not describe the consequences of this new type of extended disease process in adults which the pathologist sees at the autopsy table. According to the director of the new Institute on Aging, Robert Butler, the geriatrics program will have to include plans for mongoloids, a situation that would have been unimaginable 40 years ago!
Several sets of life tables for mongolism have been prepared, but none allows us to measure with precision how the life expectancy has changed and how much the prevalence rates have been rising since 1939. However, Carter (1958) makes what I think is a reasonable set of estimates of the prevalence rate of mongolism at age ten years. The rate doubled between 1929 and 1949, and doubled again in the following decade, reaching a level of more than one per thousand by 1958.
If we look at prevalence data from Victoria, Australia, in 1961 (Collmann and Stoller, 1963) and Salford, England, in 1974 (Fryers, 1975), we see that this trend is continuing. The overall prevalence rate increased by about 150 percent between 1961 and 1974. For children aged five to fourteen years, the prevalence rate per 1,000 was 1.3 in 1974, or almost twice the 1961 rate of .70.
Prevalence rates for mongolism would have risen dramatically even if nothing had been added to medical technology beyond antimicrobial drugs. Cardiac complications, which today are the most common cause of mortality among mongoloids (Deaton, 1973), usually do not occur until the teens or twenties, whereas previously most mongoloid children died of pneumonia before the age of six years. The most dangerous period of life for mongoloids is still the first year, but gains in survivorship have also been the most dramatic in this early period.
Of the mongoloid children who survive to age five years today, 50 percent live on into their fifties (Øster et al., 1975). Even this situation is changing. As more and more cardiac and gastrointestinal lesions are being surgically corrected, and patients with leukemia and other cancers are receiving life-prolonging treatments, we can expect to see an even greater rise in the prevalence of Down's syndrome.
Yet, no large scale searches for preventable causes of mongolism are under way. Such inquiry seems to represent no one's priority. Even the door to new studies, which opened dramatically in 1959 when mongolism was shown to be due to trisomy, has given us no new insight into how to keep this condition from beginning. Fetal diagnosis of the trisomic condition followed by elective abortion does indeed represent an attempt to reduce the incidence of live-born mongoloid infants. At best it is a method for recognition of the condition early enough in fetal development so that women willing to do so can arrange for an early termination of the pregnancy. But this is merely a method of precipitating death, not an attempt to find preventable causes of the condition itself.
If this phenomenon of rising prevalence had occurred only in mongolism, the situation would be disturbing, for mongoloids now represent one-fourth of the severely retarded population (Kushlick, 1966). But because the prevalence rate of the severely retarded has been growing in general, it becomes alarming. The lives of youngsters with other causes of severe mental retardation are also being extended more rapidly than those of the general population due to the falling neonatal, infant, and childhood mortality rates associated with these conditions. The best data on the subject of rising prevalence rates come from Salford, the industrial suburb of Manchester, England (Fryers, 1975). There the school-age prevalence rates of the severely mentally retarded more than doubled between 1961 and 1974. We do not have much information on the diagnostic groups represented, but if I interpret correctly the criteria for severe retardation, many young people are going to live handicapped lives of unpredictable duration.
Senile Brain Disease (SBD)
Another example of the failures of our successes occurs at the other end of life. We have long known that the age-specific prevalence of serious mental disorders rises rapidly in the last decades of life (Fig. 2). We also know that the general population is aging.
Figure 2.
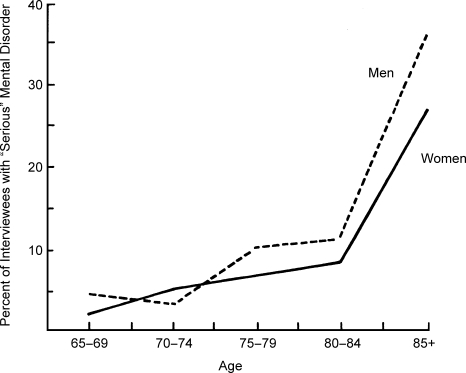
“Serious” Mental Disorder. “Serious” in this study meant with enough evidence of danger to self or others, or, more commonly, inability to care for self so that an involuntary mental hospital certificate could have been properly signed by a physician if those in the individual's home situation stopped being able and willing to provide care.
Source: Staff of the Mental Research Unit, New York State Department of Mental Hygiene. 1960. A mental health survey of older people. Psychiatric Quarterly (supplement) 34(1):34–75. (Constructed from data in Table 3.21, p. 56.)
With the exponentially rising age-specific prevalence rates of mental illness with age, and with an increasing number of aged in the population, it is clear that we are headed for a great increase in serious mental disorder associated with aging. I can see no reason to think that the incidence of senile brain disease might be falling, nor do I think there is evidence that it is rising. I suspect that psychosis with cerebral arteriosclerosis may be getting more common, because coronary artery disease is getting more common, but I know of no assembled facts on this issue.
However, since senile brain disease was probably the condition which led Osler to think of pneumonia as the old man's friend, we may properly ask whether the large-scale conquest of pneumonia has reduced the usefulness of this friend, stretching out the course of senile brain disease, which produces the mental manifestations of “senile dementia.”
We have some facts from a small (approximately 2,500), south Swedish population which was carefully screened for psychiatric illness in 1947 by Essen-Möller (1956), and rescreened in 1957 by Hagnell. Hagnell and I selected two diagnoses believed to be dominated by cases of senile brain disease, although the classification might be slightly contaminated by cerebral arteriosclerosis and depressive states. (The silent cases of senile brain disease which occur will, of course, be missed by the type of clinical screen used.) (Gruenberg and Hagnell, 1976.)
There were twenty-four people over the age of sixty with senile dementia in 1947, and there were forty-eight over the age of sixty in 1957. All twenty-four of the people found to have senile dementia in 1947 died by 1953, but of the forty-eight cases prevailing in 1957, five were still alive in 1967. The average duration of the episodes had at least doubled in a decade. The data suggest no concentration of this doubling in either sex or in any age group, but the number of cases is too small to examine this issue with confidence.
From 1947 to 1957, the prevalence rate of senile dementia in women over sixty years old rose from 3.2 percent to 5.7 percent, and in men from 2.3 percent to 4.9 percent.
Survivorship of the cases prevailing in 1957 closely resembled that of the general population, whereas cases prevailing in 1947 died off faster than the general population. The evidence suggests that this process did not end in 1957, but probably still continues today.
Who Else Was Killed by Pneumonia?
The chronic disabilities I have discussed so far—Down's syndrome and senile brain disease—are only two examples of the failures of success. What other conditions have been extended because of the elimination of fatal complications? First let us ask what other conditions have risen in prevalence due to the advent of antimicrobial drugs. Collins and Lehmann (1953) examined the excess death rates caused by conditions other than pneumonia during local influenza and pneumonia epidemics in the 1920s and ‘30s. From this material, they were able to provide us with evidence regarding those diseases which were frequently terminated by these respiratory infections in the days when the treatment resources against them were limited. From their data, we can infer what those conditions were (Table 1).
TABLE 1.
Conditions Showing Excess Death Rates during Epidemics of Influenza and Pneumonia a
| Heart disease |
| Tuberculosis (especially before 1921) |
| Intracranial vascular lesions |
| Nephritis (especially before 1929) |
| Diabetes |
| Puerperal diseases |
| Cancer |
| Chronic bronchitis |
If no other causes of death had been conquered by modern medicine except those which respond to the sulfa drugs and antibiotics, we would be justified in suspecting that the durations of these conditions were being prolonged. They are conditions which do not recover spontaneously. They are also diseases for which no cures have been developed, and for which no preventions have been found.
But there have been other major advances against the killing complications of chronic diseases, some of which I will mention to illustrate the fact that the rising prevalence of chronic diseases and disability is not merely the result of a decreased case fatality rate in pneumonia.
Some Other Conditions
In Table 2 are listed some of the conditions which should be looked at from the same point of view—diseases made more prevalent by medical progress. I have listed them approximately in their rank order in terms of prevalence rates, regardless of which age group experiences the highest prevalence rate. In doing this I have taken the unusual step of eliminating discrimination by age.
TABLE 2.
Conditions Showing Increased Prevalence in the Last 30 Years
| Condition | Highest Prevalencea | Next Steps in Research |
|---|---|---|
| Senile brain diseaseb | 300/1,000 (80 years) | Case-control; autopsies; laboratory diagnosis |
| Arterioscleroticc | ||
| Heart disease | 140/1,000 (65–74 years) | Case-control |
| Brain disease | 100/1,000 (65–74 years) | Case-control |
| Hypertensionc | 150/1,000 (over 65 years) | Case-control |
| Schizophreniac | 12/1,000 (35–44 years) | Penetrance factors |
| Diabetesb | 9/1,000 (65–74 years) | Case-control on individuals with similar indices for metabolism of glucose |
| Severe mental retardationb | 4.7/1,000 (5–15 years) | Nutritional preventive trials |
| Spina bifidab | 2.5/1,000 (birth) | ? |
| Down's syndromeb | 1.3/1,000 (birth) | Is increased incidence in older women due to more trisomic mutations or decreased lethal effects of trisomy? |
Author's best estimate, based on available data
Pretty certain
Inferred
Arteriosclerosis
Most cases of arteriosclerosis cannot be recognized by clinical examination. We have no good estimate of the prevalence of subclinical cases, but we do know that arteriosclerosis represents the most important single cause of chronic brain disease interfering with mental functioning, as well as the largest cause of chronic heart disease in this country. Chronic kidney disease and hypertension are also closely related to this condition. Previously, cases of arteriosclerosis were terminated by a number of complications: pneumonia, coronary occlusion, and ruptured arteries in the brain (stroke) and aorta. In the last forty years, medical research workers have developed a variety of means for outmaneuvering each of these fatal complications.
Hypertension
The prevention of fatal complications by moderating the level of hypertension with diuretics seems to be working. Most hypertensive patients lead almost normal lives and experience only a low level of disability. We have discovered an ideal way to control this disease, but we have yet to learn how to prevent it from occurring.
Schizophrenia
This is a common enough condition to worry about and a damaging one. While the highest point prevalence rates run only a little over 1 percent (Kramer, 1976), the proportion of the population who will at some time in life get clinical treatment for a schizophrenic episode is close to 5 percent. Its prevalence may be rising because in the recent past schizophrenic patients in mental hospitals had much higher mortality rates from many conditions than the general population (Malzberg, 1934). Yolles and Kramer (1969) have shown that since then this high mortality rate has declined. The pattern of community care has reduced the implications of these institutional death rates radically. But the frequency of schizophrenic diagnoses has also risen with the expansion of outpatient treatment and the broadening of diagnostic criteria. Balancing these two forces which affect the available data, I estimate that the life expectancy of schizophrenics has been increasing faster than that of the general population.
Diabetes
The discovery of insulin in 1922 dramatically changed the life expectancy of diabetics. While formerly the majority died of fatal complications (in conformity with Osler's paradox) over 40 percent died in diabetic coma. This figure rapidly dropped to a tiny fraction. Pneumonia continued to account for over 10 percent of the deaths until approximately 1944. By the 1960s over three-fourths of the diabetic deaths were due to vascular complications (Marble, 1972) which must be occurring at older ages.
Spina Bifida
In 1963, a British surgeon developed a marvelous operation to save newborn babies with extreme spina bifida, a congenital anomaly of the spine. Over half those who survived this surgery were severely or very severely disabled (Laurence, 1974; Hunt, 1973). They were doubly incontinent, immobile, and often retarded and incoherent. Ford (1970) estimated that this surgery would add 358 children with severe mental and physical handicaps to the British population each year. Routine use of this surgery in the United States would result in about 1,700 families each year being “blessed” with totally crippled children (Eisenberg, 1975). No one yet knows how many years these children will survive because this is a new “advance.” Previously they would have died in the newborn nursery; now they will be saved to live crippled lives.
Other advances have had similar effects. The fatal complications of pernicious anemia have been thwarted, since this condition can now be suppressed with medication. Cases of Huntington's chorea have been prolonged by successfully treating terminal pneumonia. Hemophiliacs can now be treated so that they less often die of hemorrhages. The thoughtful reader will undoubtedly be able to list numerous other examples.
Discussion
Why are we preventing death in the presence of illness and disability? Why these successes which produce these failures? Is it because the scientific period of modern medicine and public health continues to gain its drama from the idea of a life and death struggle against the causes of death? Public health departments once routinely put falling death rate curves on the outside cover of their annual reports. This was their index of success. They only gave up using crude death rates as a selling point when their successes in lowering childhood deaths increased the proportion of old people in the population, which resulted in a rise in the crude death rate. In fact, many health officers no longer know what the death rates in their jurisdictions are or how they compare with those of the country as a whole.
I, among others, predicted that morbidity would become the priority of public health once the giant killers had been conquered and the average age of the population rose. Events have refuted my hopeful expectation. Yet our research programs continue to put primary emphasis on causes of death rather than on causes of non-killing chronic diseases. More and more of the health dollar is being used to provide services to the chronically ill and disabled. A recent estimate (R. Morris, 1976) of the health and medical care and transfer expenditures for the chronically disabled was around $83 billion—almost as much as the hotly debated defense budget.
The major advances in medical science have in fact been against killing diseases. It is noteworthy that the sulfonamides emerged out of the fight against maternal mortality in a search for a treatment of puerperal sepsis. The other effects of the sulfa drugs were all serendipitous to that goal.
Next Steps in Research
It seems obvious that the rising prevalence rates of serious conditions should lead to new priorities for research. We should focus on furthering our understanding of the forces which determine the patterns of occurrence of these conditions, and thus try to identify some modifiable causal factors. Intensive searches for preventive measures are at least as important for bettering the people's health today as were the searches to gain control over plague, smallpox, cholera, diphtheria, tuberculosis, pellagra, and lung cancer a generation or so ago. In principle there is no reason to think that different types of epidemiological forces are at work in the causation of these diseases. Infections, poisons, genes, physical agents, and nutritional deficiencies are the classes of agents we have come to worry about, and we should continue to worry about them. The epidemiologists of the future must seek out such modifiable agents in the causal chains which lead to these newly stretched out diseases of medical progress.
In order to indicate that this precept is not just empty rhetoric, I have undertaken to suggest a next step in epidemiological research for each of these conditions (Table 2). In selecting a next step I have tried to keep in mind Sir Peter Medawar's excellent dictum: “If politics is the art of the possible, science is the art of the soluble” (Medawar, 1967). Selecting the next issue to investigate is not a science but an art—it is a matter of judging what problem is soluble today with today's understanding and research techniques. “Any fool can ask a question, the trick is to ask a question which can be answered” (Lemkau and Pasamanick, 1957).
Trisomy 21
We have known for some time that mongolism (Down's syndrome) is the most common of the human trisomic disorders. I will confine my suggestions to those cases caused by nondisjunction, the failure of the chromosomal material to divide properly when the ovum is being formed in the mother's ovary.2 The obvious approach to this problem is to look for the causes of nondisjunction and to look at its epidemiology. The nondisjunctions which occur in the various trisomic conditions (for example, mongolism, Turner's syndrome) may be caused by different agents or they may have a single underlying cause. If all nondisjunctions have similar causes and result only in different patterns of trisomy because they affect different chromosomes, we should then turn our attention to all the nondisjunctions including those which do not cause human disease. Most trisomic patterns are likely to be lethal to the embryo, so the obvious research step is to compare fetuses which spontaneously abort with those that do not. We would then be able to tell whether trisomy of chromosome 21 (which produces mongolism) is the most common human trisomy, or only the most common one which survives the fetal period and produces disease.
I suspect that trisomies are fairly common and that quality control occurs by weeding out the “misfits” during fetal development. One way to pursue that hypothesis is to determine whether the much higher rate of mongoloids born to older women is associated with a higher rate of trisomic conceptions or with a decreased ability for discriminating weeding through resorption, abortion, and miscarriage. There is abundant evidence that the mortality rate in mongoloid fetuses is enormous. How does it compare in women of different ages? That, I think is a soluble problem.
Senile Brain Disease
Clinical diagnosis of senile dementia is not terribly difficult but this does not identify the frequent asymptomatic silent cases of it. So we need autopsy surveys on clinically surveyed populations. Case control studies cannot yet be done because we know too little about the age of risk. There is some evidence in Hagnell's data that incidence rates, which soar between age 70 and age 80, begin to fall off after age 80. Perhaps everyone who is going to develop this condition does so by age 85 or 90. If so, we know that our case control studies should be done on people who have passed their ninetieth birthday. All of the important questions about the epidemiology of senile brain disease would become rapidly answerable if we had a reliable, valid means of knowing whether senile plaques were present during life. The new evidence about aluminum deposits in the senile plaques suggests the possibility that some clever biophysicist might develop a noninvasive device for ascertaining the presence of such deposits.
Arteriosclerosis
We need a means of identifying people in the early presymptomatic stages of this group of diseases. These early stages can be detected at autopsy, and autopsy surveys for this purpose can be done on young people who die of other conditions, particularly accidents. This would provide an opportunity to compare the characteristics of cases and non-cases—a simple case control study.
Schizophrenia
The next fruitful step in elucidating the pathogenesis of schizophrenic conditions may be reached by identifying populations with high levels of familial aggregation of the condition and comparing these families with the families of schizophrenics in which the concentration of secondary cases among first degree relatives is low. This is based on the general notion that there are two types of factors which must interact to produce clinical schizophrenic syndromes: factors associated with the family of origin (polygenic mechanisms, dominant gene with low penetrance?) and external environmental factors. Comparing the environments and living habits of these two sets of families would be an attempt, through a type of case control study, to identify risk factors other than the familial tendency to develop schizophrenia. That is a long shot, but it attracts me. I have used the single word “penetrance” in Table 2 to signify this line of reasoning.
Diabetes
The individual's inability to metabolize glucose, which was earlier thought to be the hallmark of the diabetic condition, is no longer an adequate criterion for case identification. Survey findings have revealed that the indices which measure the ability to metabolize glucose fall with age in the general population, whether diabetes is present or not. This has made the task of the epidemiologist more difficult, as has the fact that these falling indices are accompanied by greater variations in value for older age groups. A next worthwhile step for research would be to compare diabetic and nondiabetic individuals who have low index values with respect to factors associated with clinical diabetes (overweight, familial aggregation, and so on).
Severe Mental Retardation
Epidemiology cannot help us to find causes for this group of conditions when approached collectively. Some forms of retardation are associated with genes. Some are caused by the trisomic conditions discussed above. But there is a large group which are not familial and are probably associated with brain damage early in fetal development. The “continuum of fetal damage” concept introduced by Lilienfeld and Parkhurst (1951) and elaborated by Pasamanick and Knobloch (1961) has not been picked up and elaborated sufficiently in more concrete investigations. Causative agents often interact with suboptimal nutrition to produce disease, and many women who become pregnant are in a suboptimal nutritional state. Preventive trials in which nutritious food is supplied to pregnant women would seem to be the logical next step in research.
There have been so many examples in the last forty years of how our health technology too often advances by postponing death and thus increases the duration of chronic conditions, that one might conclude that this trend is inevitable. But there is one great victory during the same period which went just the other way. It may not be as impressive as the conquest of smallpox, but as a consequence of the discovery that a very large proportion of tooth decay was due to a correctable deficiency of the trace element fluorine, millions of persons who would have lost their teeth in early adulthood have been able to keep them. The final link in the chain of evidence came from the great preventive trial which compared the incidence of caries in Newburgh and Kingston (New York) after one of the towns had fluoridated its water supply. Our techniques for treating dental decay have improved only slightly, but we have made great strides in reducing the incidence of decay. The fact that more dentists are making more money than ever should relieve any anxiety that the medical fraternity might have about successful disease control programs.
Envoi
In assessing the effect of our technical advances in the past four decades, I have attempted to demonstrate that the net contribution of our successes has actually been to worsen the people's health. The prevalence of chronic diseases and disabilities depends on both the frequency with which they occur and their average duration. It is true that we have lowered the occurrence of certain chronic conditions through preventive measures; the prevalence of dental decay and lost teeth has diminished, and the prevalence rate of paralytic poliomyelitis has fallen. However, these few reductions in the occurrence of chronic conditions have been more than offset by the increased average duration of a wide range of conditions whose fatal complications we have learned how to postpone.
You will recall that Semmelweis was led to connect puerperal sepsis with contamination from the autopsy room after a close friend of his, a pathologist, had died with tissue changes similar to those seen in puerperal sepsis after he had been pricked with a knife during an autopsy on an infected person. I can give you no such dramatic episode which forced me to the conclusions outlined in this paper, but I do have enough recollection of transient ideas and insights to know that I was extremely resistant to the generalizations laid out here. I now recognize that we should have predicted by 1940 that some chronic diseases and disabilities would become more common because we had better techniques for thwarting killers which had been weeding out the chronically ill.
I tell you about this resistance within myself to let you know that if you find alien the whole idea that the techniques we have to improve life expectation perpetuate sick lives more than they do healthy lives, I was recently of your company. I know that part of my resistance and caution stemmed from a feeling that colleagues would also be resistant and that I would have to be able to defend myself against much methodological quarreling. But after looking at the issue from many angles, and examining multiple sources of information, I am convinced that this unpleasant proposition is true.
The paradoxical fact about death is that it is at once the great leveler and the great discriminator. It is the greatest of all equalizers because it is everyone's ultimate end, and the lowliest beggar can be no more dead than the most eminent monarch. But it is also a great discriminator because it comes later for those more privileged than for those less privileged. As Sir Thomas Browne (1642) said so elegantly in Religio Medici, “There is little difference between one man's death and another's except in the time and the manner of dying.”
While the universal fear of the great plagues might leave us with the impression that they were no respecters of persons, in fact, all the great killers have discriminated, more readily taking those who were half dead or half grown than those who were healthy and in their prime. There are a few examples of killers which discriminate in the opposite direction. The generals have always wanted the flower of our youth for cannon fodder. Paralytic poliomyelitis selected people of strong athletic build who were more vigorous than the average person (Draper, 1917). In this instance, it was later discovered that higher social status was associated with a lower chance of having a subclinical immunizing attack of poliomyelitis in early childhood. But the few real exceptions only underline the general rule that the large-scale killers are cowardly and select those least able to defend themselves. That greatest of all iatrogenic killers, puerperal sepsis, was concentrated in women of childbearing age, but from all the records I can find, showed special favoritism for the weakest of them.
But now our technological successes defy death's claim on the sick and the weak. We are proud of these successes, and perhaps it is partly our pride which prevents us from seeing that the successes result in the prolongation of sick lives.
Surely another reason why it has been so difficult to see the effects of our medical successes is that we have been suffering from that terrible ailment of modern technological man, his fragmented specializations. I did not see, for example, the way that chronic brain syndromes are made more common in the population by the systematic application of new health technologies until I stopped thinking of mental disorder epidemiology as somehow isolated from general epidemiology. It seems obvious to me now that general epidemiology also needs to be capable of dealing with the mental conditions which are manifestations of brain disease or of cerebrovascular disease. But our thought processes have been suffering from excessive hardening of the categories.
It is easy to see, in such cases as Karen Ann Quinlan's, that maintaining the vital systems artificially is not maintaining an intact person. And it is easy to see that there are profound ethical, professional, and legal questions involved. But my concern is not these small gains in extending life at the last moment before death. Such cases, which Jerry Morris (1975) has aptly called “snatch victories,” make up only a minute part of the paradoxical effect of medical progress which I am trying to make more visible to you. The vast bulk of the increases in prevalence rates consists of only slightly impaired lives: memory loss in elderly people who are continuing to get and give pleasure in their lives, generally well-controlled cases of diabetes, or early hypertension. I am myself a handicapped person who survives by courtesy of modern medical care at its best. The extensive antishock and reconstructive surgery procedures I had following an automobile accident saved my life. The same injury would have been fatal a few years earlier.
So the successes I have been referring to are real successes representing real advances. But the increase in disease and disability which ensues is also real and must be faced. What then are the proper lessons to learn from these failures? Not the silly notion that we should give up our efforts to overcome the killers. Not that we should go backward to a pre-enlightenment stage of society in which we throw away the umbrellas and say, “If God meant you to stay dry, he wouldn't have made it rain.” Nor should we conclude that the cheapest solution to chronic disease is the best solution. Hitler knew that the cheapest “solution” to cases of chronic illness was death. If our technology has blunted the edge of the grim reaper's scythe, that's exactly what it was meant to do and we should rejoice. We cannot avoid the successes. We must learn to overcome the ensuing failures.
As a first step, we must come to recognize that the socially organized application of health technology is one of the greatest epidemiological forces in the world. We have seen how the provision of medical care, while it has served as an important means of postponing death, has done so, to a great extent, by defeating the fatal complications that used to terminate the diseases people were suffering from, thus making those diseases more common in the population.
Today's socially organized campaigns to prevent killing diseases can have a similar effect; that was the object of the swine flu vaccination program. The eradication of smallpox from the earth—perhaps public health's greatest single victory—may have a similar effect. Smallpox must have been weeding out some individuals with chronic conditions. Who had it been killing? I admit to feeling foolish in raising this question only after the campaign has been completed. If we had posed the question before the campaign got started, we would now be in a position to state what conditions will become more common as a result of the eradication of smallpox. If we are to be more sensible in our efforts to improve the people's health we must have the foresight to look for these failures as soon as we recognize the possibility for advance.
The increase in chronic illness and disability which results from our advances makes finding ways to prevent these chronic conditions a matter of top priority for research programs. We are now over thirty years late in recognizing the failures that are bound to follow such successes. We should not waste time crying because we are so tardy, but rather hasten to see how quickly we can catch up.
I have indicated in the last column of Table 2 a few ideas which I think are worth pursuing. To my eye, what is dramatic about these conditions is the paucity of existing epidemiological data. We don't even have good case control data for many of them. We haven't failed in our efforts to find preventable causes of these conditions—we have hardly made any effort at all! There are whole sequences of investigations which are obvious even when we have no clues. But even in cases where we do get a clue, I think that we are unduly passive in our approaches to preventing chronic diseases.
Preventive trials are interventions based upon an accumulated body of experience. Their great value lies in their ability to prove or disprove seemingly credible hypotheses. If preventive trials were done often enough, most would yield negative results, and we could rid ourselves of a number of erroneous “common sense” ideas. But preventive trials are not used to the extent that they should be. Most often, they are thought to be too expensive. Frequently they are viewed as “manipulations” which raise social and ethical problems, even though in most applications (like improved maternal nutrition) they are innocuous and involve interventions known to be desirable. Frequently, preventive trials are not done because they call for stable research teams which cannot be organized under the present project grant system.
Our weakness today in finding preventive measures for chronic illnesses in contrast to our strength in finding curative measures for fetal complications is due largely to the way health research money is organized. I think the time has come to examine afresh the administrative mechanisms by which research is supported. Can't we find new ways to encourage research which will emphasize chronic disease prevention? If we don't, research which produces means for thwarting fatal complications—research which, when applied, increases the frequency of postmature deaths—will continue to advance more rapidly.
I have always been mortified by public health's preoccupation with death. We have always known that there are fates worse than death. But epidemiology and biostatistics have never sufficiently weaned themselves from John Graunt's great bills of mortality studies and William Farr's brilliant use of birth and death records. I have long been sick and tired of this morbid preoccupation with the first and last months of life. But it doesn't matter that this backwardness in public health made me sick. Now that we know that instead of enhancing the people's health this kind of deathly thinking has been increasing the people's sickness and disability, it is time to call for a change.
Now that we recognize that our life-saving technology of the past four decades has outstripped our health-preserving technology and that the net effect has been to worsen the people's health, we must begin the search for preventable causes of the chronic illnesses which we have been extending. Epidemiologists must play a key role in finding these causes, but without the application of social pressures in that direction, few will take up the opportunity. For a period, at least, health saving must take precedence over life saving. And we will not move forward in enhancing health until we make the prevention of nonfatal chronic illness our top research priority.
Acknowledgments
The preparation of this manuscript depended upon the excellent help of Linda LeResche, Sc.D., in assembling and organizing the relevant facts, and upon the writing skills of Janet Archer. Abraham Lilienfeld, M.D., gave very useful advice. David Willis kept us going with persistent encouragement and suggestions through numerous versions.
Endnotes
The duration of each person's illness extends from the time he becomes ill until he no longer is ill. A person with an incurable chronic illness will remain ill until he dies.
The normal human cell has twenty-three pairs of chromosomes, one of each pair coming from the father's sperm and one from the mother's ovum. The ovum and sperm each have only twenty-three chromosomes. Nondisjunction in oogenesis results in an egg having twenty-four chromosomes because one pair failed to split. When fertilized such an egg has three chromosomes where a pair normally exists, hence the name “trisomy.”
References
- Browne T. A Letter to a Friend. Boston: Roberts Brothers; 1642. Religio Medici. Reprinted in Religio Medici. Christian Morals, Urn-Burial and Other Papers. 1889. [Google Scholar]
- Carter CO. A Life-Table for Mongols with the Causes of Death. Journal of Mental Deficiency Research. 1958;2:64–74. [Google Scholar]
- Collins SD, Lehmann J. Public Health Monograph. Washington, D.C.: Government Printing Office; 1953. Excess Deaths from Influenza and Pneumonia and from Important Chronic Diseases during Epidemic Periods, 1918–51. No. 10. [PubMed] [Google Scholar]
- Collmann RD, Stoller A. Data on Mongolism in Victoria, Australia: Prevalence and Life Expectation. Journal of Mental Deficiency Research. 1963;7:60–68. doi: 10.1111/j.1365-2788.1963.tb00784.x. [DOI] [PubMed] [Google Scholar]
- Deaton JG. The Mortality Rate and Causes of Death among Institutionalized Mongols in Texas. Journal of Mental Deficiency Research. 1973;17:117–122. doi: 10.1111/j.1365-2788.1973.tb01192.x. [DOI] [PubMed] [Google Scholar]
- Draper G. Acute Poliomyelitis. Philadelphia: P. Blakiston's Son & Co; 1917. [Google Scholar]
- Eisenberg L. The Ethics of Intervention: Acting amidst Ambiguity. Journal of Child Psychology and Psychiatry. 1975;16:93–104. doi: 10.1111/j.1469-7610.1975.tb01260.x. [DOI] [PubMed] [Google Scholar]
- Essen-Möller E, Larsson H, Uddenberg CE, White G. Individual Traits and Morbidity in a Swedish Population. Acta Psychiatrica et Neurologica Scandinavica. 1956 Supplementum 100. [PubMed] [Google Scholar]
- Ford AB. Casualties of Our Time. Science. 1970;167:256–263. [PubMed] [Google Scholar]
- Fryers T. Life Expectancy and Causes of Death in the Mentally Retarded. British Journal of Preventive and Social Medicine. 1975;29:61. [Google Scholar]
- Gregg A. The Furtherance of Medical Research. New Haven: Yale University Press; 1941. [Google Scholar]
- Gruenberg EM, Hagnell O, Ojesso L, Mittleman M. The Rising Prevalence of Chronic Brain Syndrome in the Elderly. Symposium: Society, Stress and Disease: Aging and Old Age. Stockholm, June 14–19.1976. [Google Scholar]
- Hunt GM. Implications of the Treatment of Myelomeningocele for the Child and his Family. Lancet. 1973;1:1308–1310. doi: 10.1016/s0140-6736(73)92881-x. [DOI] [PubMed] [Google Scholar]
- Kramer M. Population Changes and Schizophrenia, 1970–1985. Paper presented at the Second Rochester International Conference on Schizophrenia. Rochester, N.Y., May.1976. [Google Scholar]
- Kushlick A. A Community Service for the Mentally Subnormal. Social Psychiatry. 1966;1(2):73–82. [Google Scholar]
- Laurence KM. Effect of Early Surgery for Spina Bifida on Survival and Quality of Life. Lancet. 1974;1(7852):301–304. doi: 10.1016/s0140-6736(74)92606-3. [DOI] [PubMed] [Google Scholar]
- Lemkau PV, Pasamanick B. Problems in Evaluation of Mental Health Programs. American Journal of Orthopsychiatry. 1957;27(1):55–58. doi: 10.1111/j.1939-0025.1957.tb05199.x. [DOI] [PubMed] [Google Scholar]
- Lilienfeld AM, Parkhurst E. A Study of the Association of Factors of Pregnancy and Parturition with the Development of Cerebral Palsy: Preliminary Report. American Journal of Hygiene. 1951;53:262–282. doi: 10.1093/oxfordjournals.aje.a119453. [DOI] [PubMed] [Google Scholar]
- Malzberg B. Mortality among Patients with Mental Disease. Utica, New York: State Hospitals Press; 1934. [Google Scholar]
- Marble A. Insulin—Clinical Aspects: The First Fifty Years. Diabetes. 1972;21(2):632–636. doi: 10.2337/diab.21.2.s632. [DOI] [PubMed] [Google Scholar]
- Medawar P. The Art of the Soluble. London: Methuen; 1967. [Google Scholar]
- Morris JN. Uses of Epidemiology. 3rd ed. London: Churchill Livingstone; 1975. [Google Scholar]
- Morris R. Alternative Forms of Care for the Disabled: Developing Community Services. In: Bergsma D, Pulver AE, editors. Developmental Disabilities: Psychologic and Social Implications. New York: Alan Liss, Inc; 1976. [Google Scholar]
- Osler WO. In: The Principles and Practice of Medicine. 12th ed. McCrae T, editor. New York: D. Appleton-Century Company, Inc; 1935. revised by. [Google Scholar]
- Øster J, Mikkelsen M, Nielsen A. Mortality and Life-Table in Down's Syndrome. Acta Paediatrica Scandinavica. 1975;64:322–326. doi: 10.1111/j.1651-2227.1975.tb03842.x. [DOI] [PubMed] [Google Scholar]
- Pasamanick B, Knobloch H. Epidemiologic Studies on the Complications of Pregnancy and the Birth Process. In: Caplan G, editor. Prevention of Mental Disorders in Children. New York: Basic Books; 1961. pp. 74–94. [Google Scholar]
- Penrose LS. On the Interaction of Heredity and Environment in the Study of Human Genetics (with Special Reference to Mongolian Imbecility) Journal of Genetics. 1932;25:407–422. [Google Scholar]
- Record RG, Smith A. Incidence, Mortality and Sex Distribution of Mongoloid Defectives. British Journal of Preventive and Social Medicine. 1955;9:10–15. doi: 10.1136/jech.9.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spain DM. The Complications of Modern Medical Practice: A Treatise on Iatrogenic Diseases. New York: Grune and Stratton; 1963. [Google Scholar]
- Yolles SF, Kramer M. Vital Statistics. In: Bellak L, Loeb L, editors. The Schizophrenic Syndrome. New York: Grune and Stratton; 1969. pp. 66–113. [Google Scholar]


