Abstract
Context
Late-life disability has been declining in the United States since the 1980s. This study provides the first comprehensive investigation into the reasons for this trend.
Methods
The study draws on evidence from two sources: original data analyses and reviews of existing studies. The original analyses include trend models of data on the need for help with daily activities and self-reported causes of such limitations for the population aged seventy and older, based on the National Health Interview Surveys from 1982 to 2005.
Findings
Increases in the use of assistive and mainstream technologies likely have been important, as have declines in heart and circulatory conditions, vision, and musculoskeletal conditions as reported causes of disability. The timing of the improvements in these conditions corresponds to the expansion in medical procedures and pharmacologic treatment for cardiovascular disease, increases in cataract surgery, increases in knee and joint replacements, and expansion of medications for arthritic and rheumatic conditions. Greater educational attainment, declines in poverty, and declines in widowhood also appear to have contributed. Changes in smoking behavior, the population's racial/ethnic composition, the proportion of foreign born, and several specific conditions were eliminated as probable causes.
Conclusions
The substantial reductions in old-age disability between the early 1980s and early 2000s are likely due to advances in medical care as well as changes in socioeconomic factors. More research is needed on the influence of health behaviors, the environment, and early- and midlife factors on trends in late-life disability.
Keywords: Disability, aging, population health
Disability prevalence rates have declined dramatically among older Americans during the past quarter century (Freedman, Martin, and Schoeni 2002; Freedman et al. 2004; Manton, Gu, and Lamb 2006; Waidmann and Liu 2000). If these rates continue to fall, a greater number of older Americans could remain economically and socially active, and fewer would need medical and long-term care (Cutler 2001; Lubitz et al. 2001; Singer and Manton 1998). Despite these implications for policy and society, however, there currently is very little evidence indicating why these declines have occurred (Freedman 2006). The reason may be that disability in late life is affected by a complex set of biological, medical, behavioral, economic, social, and environmental determinants throughout the life course.
Determining the reasons for the declines in late-life disability is more than an academic exercise. Because the first baby boomers will turn sixty-five in 2011, it is imperative that we understand the prospects for additional reductions in disability rates. An understanding of past trends can help improve predictions of future changes in disability and can also give policymakers and clinicians an idea of the costs of achieving these reductions and where in the disablement process any interventions might be most effective. Understanding this decline also would enable us to determine the likely effects of competing factors influencing health and disability. For example, although millions of people with specific diseases and conditions have clearly benefited from medical advances, health care tends to account for only a relatively small variation in a population's health (McGinnis, Williams-Russo, and Knickman 2002). Accordingly, economic, social, and environmental factors have long been recognized as major determinants of a population's health (McKeown 1979; McKinlay and McKinlay 1977; Preston 1977). In this article, therefore, we take a broad perspective that integrates medical, behavioral, economic, social, and environmental factors throughout the life course, assessing the extent to which each accounts for the drop in disability rates.
Unfortunately, no single available data source covers the breadth of possible explanations. Largely because of this limitation, the decline in disability rates cannot be explained with a single monolithic study design that produces precise results based on a handful of coefficient estimates. Moreover, even when data are available and individual-level factors are identified as likely influences, changes in these factors may themselves be driven by other, more basic causes, such as changes in social and economic policies. Furthermore, our confidence that the estimates represent true causal effects, as opposed to a simple accounting for the trends, varies with the factors considered. We thus address these challenges by piecing together evidence from a variety of sources, some more convincing and some less, some based on original analyses and some drawn from other scientists' work.
Before assessing the evidence, we begin by briefly describing the trends in disability that we are trying to explain. We focus on changes at the level of the U.S. population during the last two to three decades, which have been the focus of most of, but not all (Costa 2002), the recent work on old-age disability trends. The facts of these trends are more broadly accepted for this period, and the data available for assessing the causes are richer. We then describe a framework for understanding the diverse factors that may influence disability and hence account for these trends. With this framework as our guide, we consider the empirical evidence that supports or refutes the particular factors. Finally, we synthesize the evidence, dismissing some factors and pointing to others as explaining the remarkable declines in late-life disability.
Trends in Old-Age Disability
Countries and surveys define and measure disability in different ways. One recent conceptualization suggests that disability is a process by which a person's health, environment, and personal factors influence his or her body structures, activities, and participation (World Health Organization 2002). Much of the literature on late-life disability trends, however, defines the term more narrowly to refer to limitations in personal care and other daily activities. Accordingly, the bulk of the evidence on trends in old-age disability is based on indicators of limitations in activities of daily living (ADLs) and instrumental activities of daily living (IADLs). ADLs are personal care activities, such as bathing, eating, toileting, and dressing. IADLs are activities related to independent living, such as preparing meals, shopping, managing money, and doing housework. Some surveys measure difficulties carrying out these activities without help or special equipment; others focus on the need for help; and still others measure whether help is received with these activities. Although seemingly insignificant, these differences in measurement approaches have important implications for estimating both levels and trends (Freedman et al. 2004) and hence making policies.
In regard to the empirical evidence for these trends, Manton, Corder, and Stallard's influential research showed a decrease in the 1980s in the prevalence of chronic late-life disability (Manton, Corder, and Stallard 1993). Other studies (e.g., Schoeni, Freedman, and Wallace 2001; Spillman 2004; Wolf, Hunt, and Knickman 2005) showed a remarkable agreement in their estimates of a decline in the prevalence of disability during the 1980s and 1990s, according to five national surveys. The strongest evidence supports declines in the IADL disability rate, typically falling 1.5 to 2.5 percent per year (Freedman, Martin, and Schoeni 2002). Reductions in the prevalence of more severe ADL disabilities appear to have been smaller (Freedman et al. 2004).
We summarized these trends for the population aged seventy and older using recent data from the National Health Interview Survey (NHIS), which provides annual observations and the longest consistently measured time trend for disabilities in the national population. Although these data omit the institutionalized population, sensitivity analyses suggest that this omission does not appreciably bias trends (Schoeni, Freedman, and Martin 2005; Schoeni, Freedman, and Wallace 2001). The NHIS measures the need for help with personal (ADL) and routine (IADL) care activities (for details, see the Methods section).
Figure 1 shows that in 1983, 21.8 percent of the noninstitutionalized population aged seventy and older had an ADL or IADL disability. The age-adjusted disability prevalence rate (i.e., holding steady the age distribution within the population aged seventy and older at the 1983 distribution) fell substantially during the next two and a half decades. As Schoeni, Freedman, and Wallace (2001) pointed out, this decline was neither monotonic nor persistent over the period. By 2005, however, the rate had fallen to 14.0 percent, an average decline of 0.36 percentage points per year.
Figure 1.
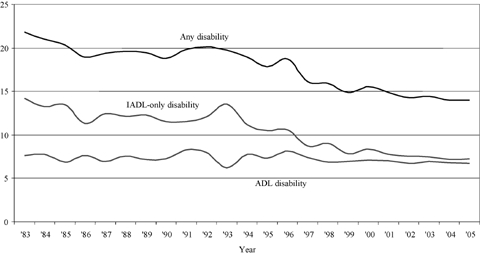
Age-Adjusted Prevalence of Disability among the Noninstitutionalized Population 70 and Older, 1983 to 2005.
Source: Authors' tabulations using the National Health Interview Survey.
These improvements in overall disability were driven more by the changes in IADL disabilities than by those in ADL disabilities (figure 1). The rate of having only IADL disabilities fell, from 14.2 percent in 1983 to 7.3 percent in 2005 (adjusted for age), whereas the rate of ADL disabilities dropped from 7.6 percent to 6.8 percent; thus the average annual rates of decline were 2.7 percent and 0.06 percent, respectively. Although the NHIS does not permit disaggregation into specific activities over this time period, Spillman (2004) found that from 1984 to 1999 the largest decreases were in three IADL activities: managing money, shopping for groceries, and doing laundry.
Conceptual Framework
Before attempting to determine empirically what might be driving the gains described in figure 1, we show in figure 2 the conceptual framework that guides our discussion of potential causes.
Figure 2.
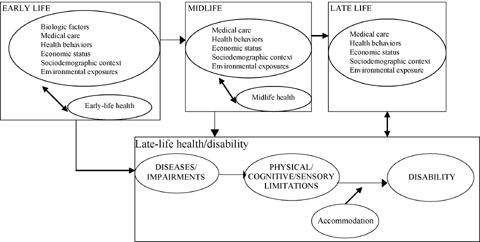
The Late-Life Disablement Process: Influences over the Life Course.
The Disablement Process
The bottom right-hand portion of figure 2 illustrates the three major stages (Pope and Tarlov 1991; Verbrugge and Jette 1994) of the disablement process, with disease, impairment, and physical, cognitive, or sensory limitation representing deficits or damage at the cellular, organ, and organism levels, respectively. In practice, the notion of “ disease” is sometimes difficult to distinguish from “impairment” and often is limited to measures of whether a doctor has diagnosed a particular condition. Hence this stage of the disablement process also is influenced by the advancement of diagnostic capabilities and access to care. “Limitation” is the notion that a person cannot carry out a physical, cognitive, or sensory task, at least not without difficulty. “Disability” is socially defined, being the product of a person's functional limitations, the demands of the environment, and that person's expectations about daily life. “Accommodations” refer to those actions that people take in response to their limitations, such as changing their behavior, using assistive or mainstream technology, or relying on personal care. For example, arthritis (a disease) may cause stiffness in the knee (an impairment), which may prevent individuals from being able to walk long distances (a limitation). Whether they can carry out daily activities without help (ADL or IADL disability) depends partly on the environment that they must navigate and whether they use assistive technology (accommodations).
Influences over the Life Course
To guide our discussion of the major influences on disability, we placed the disablement framework within a life course perspective (Kuh and Ben-Shlomo 1997). Although the distinctions are not always precise, we grouped the influences on late-life health into early-life, midlife, and late-life factors. In all three stages of life, medical, behavioral, economic, social, and environmental factors have a reciprocal relationship with health and may contribute to the formation of biological and social “chains of risk” (Kuh and Ben-Shlomo 1997). For example, medical intervention at the early stages of life may improve midlife health, which then improves labor market outcomes and income, which in turn may translate into better health in late life. At the same time, early-life factors may directly affect late-life health through biologically “programmed” mechanisms (Power and Hertzman 1997).
Midlife factors also affect late-life health, in two ways. First, midlife factors may affect the disablement process in late life. For example, a person's occupation in midlife is related to his or her income streams and asset accumulation in late life. In addition, midlife factors also directly affect health in late life. Occupational exposures, behaviors such as smoking, poor nutrition, obesity, and a lack of medical care in midlife increase the risk for a number of chronic conditions in late life. Finally, late-life factors clearly affect—and are affected by—late-life health. For example, income not only affects an individual's ability to purchase medical care and medications but also may depend on that person's ability to work.
Our framework identifies multiple factors that may account for changes in the prevalence of disability. We did not, however, empirically assess several of the factors noted here (e.g., environmental exposures, many early and midlife factors). Rather, we include them here because theory or earlier cross-sectional studies indicate that they may be important determinants of disability trends. In this way, we highlight their potential importance and recommend that future studies investigate them. For the other factors, we reviewed the empirical studies linking them to the prevalence of disabilities (for accommodations; physical, sensory, and cognitive functioning; medical care; physical activity) or presented new empirical analyses using the NHIS (for diseases and conditions; smoking; economic and sociodemographic factors).
Methods
We assembled evidence from whatever sources were available to determine whether the factors in our conceptual framework contributed to each possible explanation, focusing on changes in the prevalence of disability, not onset and recovery, simply because the data on them are sparse. When the data permitted, we examined whether the prevalence of a factor changed along with the change in disability prevalence, whether the association of that factor with disability changed, and, most important, whether such changes were large enough to produce meaningful changes in the disability prevalence. Definitive statements of causality are not always possible because of limitations in the literature, the available data, and the nature of the changes in the factor being examined, and we discuss these issues when relevant.
Most of the original analyses that we present draw on the NHIS. The cross-sectional NHIS is nationally representative of the noninstitutional population, and it is conducted annually. Disabilities among people aged seventy and older (seventy-one and older in 1982) are measured by two questions. The first asks about ADL limitations: “Because of any impairment or health problem, does —— need help of other persons with personal care needs, such as eating, bathing, dressing, or getting around this home?” Those who answered no to this question were then asked about IADL limitations: “Because of any impairment or health problem, does —— need help of other persons in handling routine needs, such as everyday household chores, doing necessary business, shopping, or getting around for other purposes?” Before 1982, the questions were substantially different. In 1997, the introductory phrase was changed to “Because of a physical, mental, or emotional problem, does …?”
If the respondents report a disability, they are asked what condition(s) or health problem(s) caused it. In 1997, the NHIS changed the way it captured and classified causes of disability, but for most cases, the causal conditions for the two periods, 1982 to 1996 and 1997 to 2005, can be consistently classified (table 1 lists the specific diseases included in each group for the two periods).
TABLE 1.
Classification of Causal Conditions in the NHIS, 1982–2005
| Diagnostic Code Category | ||
|---|---|---|
| Assigned Condition Group | 1982–1996 | 1997–2005 |
| Heart and circulatory disease | Rheumatic fever/heart disease; hypertension; ischemic heart disease; pulmonary circulatory disease; cerebrovascular disease; atherosclerosis; heart symptoms; other disease of the circulatory system | Heart problem; stroke; hypertension |
| Vision | Glaucoma; cataract; all other eye disorders | Vision problem |
| Musculoskeletal conditions | Disease of the musculoskeletal system and connective tissue | Arthritis/rheumatism; back/neck problem; fracture/bone/joint injury |
| Diseases of esophagus, ulcers, appendicitis, etc. | Disease of the digestive system (not including oral cavity, salivary glands, or jaws) | Not available |
| Senility | Senility without mention of psychosis | Senility |
| Ear disease | Disease of the ear and mastoid process | Hearing problem |
| Diabetes | Diabetes | Diabetes |
| Lung disease | Respiratory tract diseases | Lung/breathing problem |
| Cancer | Cancer | Cancer |
| Mental conditions | Mental disorders | Depression/anxiety/emotional problems |
| Nervous system | Diseases of the nervous system | Not available |
The NHIS also contains other items for the same study population we used in our analyses: smoking behavior (for selected years), education, marital status, age, sex, race, Hispanic ethnicity, birth in a foreign country (data available from 1989 to 2005), and total family income. In the surveys for 1982 to 1996 and 1997 to 2005, family income is reported by the respondent as being in one of twenty-six or eleven categories, respectively. To create consistent income codings across all years, we calculated a continuous income amount within the categories. First, we estimated family income as a function of sociodemographic variables and the family income categories appearing in the NHIS for each year from 1982 to 2005 using the seventy and older sample from the March Current Population Survey (CPS). Second, we used parameter estimates from these models along with demographic and income bracket information from the NHIS to calculate an estimate of family income within the category for each NHIS respondent. All dollar values are in 2005 dollars, indexed for inflation. When we compared them, we found that the income distributions and trends using the calculated NHIS income and the March CPS income were substantially similar.
Our estimates, from logistic models of disability status, use as the dependent variable “any disability,” that is, the report of a need for help with any ADL or IADL. We also estimated a series of multinomial logit models that further distinguished between ADL and IADL-only disabilities. All available years of data, 1982 to 2005, are pooled, except for those models that examine the effects of smoking, which are restricted to the years 1983, 1985, 1987, 1990 through 1994, and 1997 through 2005, and those models that examine the effects of being foreign born, which are limited to 1989 to 2005. We specified the trend as a linear term, with 0 representing the first year and increments of 1 for each subsequent calendar year. All models control for sex, whether a proxy responded to the survey, whether the observation was after 1996 (to adjust for the change in NHIS in 1997), and an interaction of these last two factors. We adjusted all tests for the complex design of the NHIS using SUDAAN.
As we controlled for various factors, we looked at how the coefficient of the trend variable changed and then attributed the change to the factor being added. According to Mare (2006), this approach can lead to incorrect conclusions within logistic models because the variance of the latent value of the dependent variable is different across the models. Therefore, we also standardized the logistic estimates on the latent value of the dependent variable (Williams 2006), and we also estimated linear probability models, which do not suffer from this problem. Compared with the initial logistic models, both approaches led to identical substantive conclusions concerning the impact of controlling for various factors on the estimated trend in disability. We report in the tables the unstandardized logistic estimates because they provide an estimate of the parameter of interest, that is, the change in disability prevalence over time.
The NHIS data, 1982 to 2005 for the seventy and older population, also are used to estimate models in which the dependent variable is an indicator for whether the person reports needing help and reports a specific disease as the cause of his or her disability. One model is estimated for each of the diseases reported in table 1, with separate models for 1982 to 1996 and 1997 to 2005 because of the change in measurement of this outcome in the NHIS. Using individual-level data, all models control for age, sex, and the proxy respondent dummy just described. The key explanatory variable is the trend variable, which takes the value 0 in the base year (1982 or 1997) and increases by 1 in each subsequent calendar year. We then compared the estimates of trends in cause-specific disability with the trend in overall disability, in order to identify the disease-specific causes that could account for the overall trend. Therefore, these models are estimated with ordinary least squares because they gauge the change in the level of disability prevalence, that is, the percentage-point change (as opposed to odds ratios from logistic models, which estimate trends relative to the prevalence of disease-specific causes of disability, or the percentage change). Logistic models also were estimated (though not reported here), and the qualitative results were identical. We used SUDAAN to adjust for the complex sample design of the NHIS.
Analysis
In our review and analysis of the causes of this decline in disability, we begin with those factors most proximate to disability: changes in accommodations, in underlying physical, sensory, and cognitive functioning, and in diseases and conditions among older adults. We then consider late-life factors that might influence the disablement process: changes in medical care, in health behaviors, in economic and social contexts, and in environmental exposures. Finally, we touch on a few factors related to mid- and early life that may directly or indirectly influence late-life disability and, hence, trends.
Changes in Accommodations
Accommodations take various forms, most commonly changes in behavior (e.g., performing a task less often) or in how a task is carried out (e.g., by using assistive or mainstream technology or the addition of personal assistance). In the case of shopping, for example, older people may shop less often, use an electric cart at the store, order groceries online to be delivered, or have other family members shop for them.
Determining the role of accommodations in decreasing the need for help with daily activities is challenging because the direction of the relationship is not always clear (see also Wolf, Hunt, and Knickman 2005). That is, reports of need for help may depend on the particular accommodations that have been put into place, or the lack of nearby family or resources to obtain paid help may result in particular choices about behavior change and technological assistance. Nevertheless, several studies have tracked changes in one form of accommodation—the use of assistive technologies—and its relationship to personal care. First reported more than a decade ago (Manton, Corder, and Stallard 1993; Russell et al. 1997) is the trend toward using equipment as the sole form of assistance with daily activities, which has continued through the 1990s (Freedman et al. 2004, 2005; Russell et al. 1997; Spillman 2004). The percentage of adults with a chronic disability who report using modifications such as grab bars in the bathroom and raised toilet seats also increased (American Association of Retired Persons 2003).
To date, studies have not been able to explore the role of technologies in the decline in IADL disabilities. The reason is that the growth of common household and convenience technologies not specifically intended to address disabilities (e.g., so-called mainstream technologies such as microwaves, cordless phones, and direct deposit) may be compensating for some of the functional decline. With respect to ADL trends, however, Freedman, Agree, and colleagues (2006) decomposed the declines between 1992 and 2001 in the number of older people getting help with ADLs into the contributions of demographic shifts, declines in underlying difficulty, and shifts toward assistive technology. For this time period, declines in underlying difficulty were the most important, but shifts toward assistive technology explained a substantial portion of the decline, helping offset the increases resulting from growth of the older population and the aging within that group.
Changes in Physical, Sensory, and Cognitive Functioning
Several surveys offer strong evidence that limitations in physical functioning fell during the 1980s and early 1990s (Freedman, Martin, and Schoeni 2002). For example, an analysis of data from the Survey of Income and Program Participation (SIPP) (Freedman and Martin 1998) between 1984 and 1993 suggested substantial decreases in the prevalence for older Americans of difficulty with climbing stairs, lifting and carrying, and walking three blocks. Similar findings were evident in additional analysis of the SIPP through 1999 (Cutler 2001) and from the NHIS's 1984 and 1994–1995 supplements on aging (Freedman and Martin 2000). These improvements were similar in magnitude to the declines in disability (around 1 to 2 percent per year).
The evidence regarding trends in cognitive function among the elderly population is not as well developed, in part because of the challenges of assessing cognition in surveys (Freedman and Martin 2003). An analysis of the Health and Retirement Study shows that from 1993 to 1998, the proportion of the population aged seventy years and older who were severely cognitively impaired dropped from 5.8 to 3.8 percent (Freedman, Aykan, and Martin 2002). Analyses of later data from 2000 suggest that some of this improvement may be an artifact of repeat testing (Rodgers, Ofstedal, and Herzog 2003). Analyses based on the National Long Term Care Survey between 1982 and 1999 (Manton, Gu, and Ukraintseva 2005), however, show declines in the prevalence of dementia among older Americans. In sum, these changes are not yet well enough defined and understood to draw conclusions about their contributions to declines in disability.
With respect to sensory functioning, the percentage of older Americans with vision limitations has fallen over the last few decades (Cutler 2001; Freedman and Martin 1998; Freedman et al. 2007), although rates of hearing impairment have been constant (Crimmins and Saito 2000; Desai et al. 2001; Freedman et al. 2007).
Changes in Diseases and Conditions
Thus far, the evidence regarding trends in chronic disease prevalence among older adults has been mixed. The prevalence of some chronic diseases is increasing, but that of others is falling (see, e.g., Allaire et al. 1999; Crimmins and Saito 2000; Freedman and Martin 2000; Manton, Stallard, and Corder 1995). Overall, though, many conditions appear to have become less debilitating (Crimmins and Saito 2000; Freedman and Martin 2000; Freedman et al. 2007). Moreover, the trends of disease prevalence have been influenced by both changes in disease incidence and mortality trends among those with particular conditions.
The most recent evidence points to some specific conditions that may be linked to the improvements in disability over time. Drawing on multiple waves of the National Long Term Care Survey from 1984 to 1999, Cutler, Landrum, and Stewart (2006) concluded that 14 to 22 percent of the total disability decline could be attributed to reductions in the disabilities associated with cardiovascular disease. After examining annual reports of conditions causing disabilities in the 1997 to 2004 NHIS, Freedman and colleagues (2007) concluded that reductions in heart and circulatory conditions, vision difficulty, and possibly musculoskeletal conditions as reported causes of disability accounted for a substantial share of the disability decline for that period.
Figure 3 displays the prevalence of the major causes of disability reported by persons seventy and older, regardless of whether or not they reported a disability, for causes cited in the NHIS during the full period of 1982 to 2005. This figure traces the declines in heart and circulatory conditions, vision limitations, and musculoskeletal system conditions. Table 2 presents specific estimates of the declines based on ordinary least squares models (as described earlier). Note that the reported influence of each disease is modeled separately from all the others and that the total proportion of disability decline explained by all the diseases in sum may be more than 100 percent because each person may have cited multiple causes.
Figure 3.
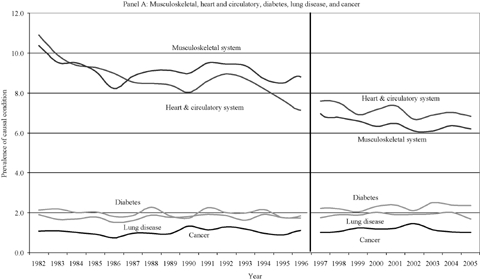
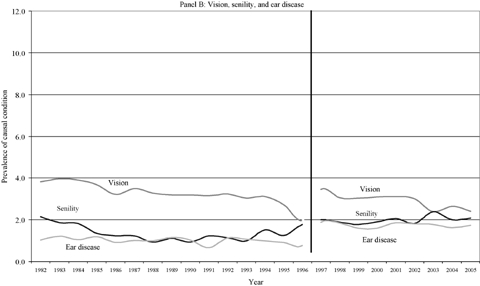
Trends in the Prevalence of Reported Causes of Disability for the Population 70 and Older, 1982 to 2005.
Source: Authors' tabulations using the National Health Interview Survey.
TABLE 2.
Trends in Prevalence of Disability and Self-Reported Cause of Disability: OLS Models
| 1982–1996 (N = 124,949) | 1997–2005 (N = 70,024) | |||||
|---|---|---|---|---|---|---|
| Outcome | Annual Percentage Point Change | Implied Percentage Point Change over the Entire Period ([1]*14) | Percentage of Disability Change Accounted for by the Condition ([2]/-2.663) | Annual Percentage Point Change | Implied Percentage Point Change over the Entire Period ([1]*8) | Percentage of Disability Change Accounted for by the Condition ([2]/-2.475) |
| [1] | [2] | [3] | [1] | [2] | [3] | |
| Disability | −0.1902** | −2.663 | Not applicable | −0.3094** | −2.475 | Not applicable |
| Disability and cause is reported as | ||||||
| Heart and circulatory system | −0.1815** | −2.541 | 95% | −0.1381** | −1.105 | 45% |
| Other diseases of circulatory system | −0.0804** | −1.126 | 42% | |||
| Atherosclerosis | −0.0667** | −0.934 | 35% | |||
| Hypertension | −0.0666** | −0.932 | 35% | |||
| Pulmonary circulation disease | −0.0550** | −0.770 | 29% | |||
| Ischemic heart disease | −0.0369** | −0.517 | 19% | |||
| Cerebrovascular disease | −0.0081 | −0.113 | 4% | |||
| Rheumatic fever, heart disease | −0.0051* | −0.071 | 3% | |||
| Heart symptoms | −0.0018 | −0.025 | 1% | |||
| Vision | −0.1092** | −1.529 | 57% | −0.1432** | −1.146 | 46% |
| Glaucoma | −0.0077 | −0.108 | 4% | |||
| Cataracts | −0.0653** | −0.914 | 34% | |||
| Musculoskeletal system | −0.0591* | −0.827 | 31% | −0.1400** | −1.120 | 45% |
| Diseases of esophagus, ulcers, appendicitis, etc. | −0.0526** | −0.736 | 28% | |||
| Senility | −0.0368** | −0.515 | 19% | −0.0003 | −0.002 | 0% |
| Ear disease | −0.0209** | −0.293 | 11% | −0.0337 | −0.270 | 11% |
| Diabetes | −0.0121 | −0.169 | 6% | 0.0249 | 0.199 | −8% |
| Lung disease | 0.0039 | 0.055 | −2% | −0.0072 | −0.058 | 2% |
| Bronchitis, emphysema, asthma | −0.0043 | −0.060 | 2% | |||
| Any cancer | 0.0059 | 0.083 | −3% | −0.0081 | −0.065 | 3% |
| Mental conditions | 0.0122* | 0.171 | −6% | 0.0188 | 0.150 | −6% |
| Nervous system disease | 0.0358** | 0.501 | −19% | |||
Notes: Each row for each time period (1982–1996; 1997–2005) is based on a different model, and the annual percentage point change is the coefficient estimate on the trend variable in that model, multiplied by 100. All models include controls for age, sex, and proxy, and SUDAAN is used to adjust for complex survey design.
Percentage of total change accounted for by conditions can sum to more than 100% because conditions are examined independently.
**and *indicates statistical significance at the 0.01 and 0.05 levels, respectively.
For the period 1982 to 1996, the coefficient estimate on trend implies that the average annual decline in disability prevalence was 0.19 percentage points. For the entire fifteen-year period, this estimate implies a decline of 2.7 percentage points. The subsequent rows of table 2 report the estimated trends for each causal condition. The regression-adjusted proportion of the population who reported a disability, with a heart and circulatory condition as the cause, declined by a total of 2.5 percentage points. This finding implies that changes in this disease—either the share of the population with the disease or the disabling influences of the disease—could account for 95 percent of the drop in disability. Among the heart and circulatory conditions, or the so-called other diseases of the circulatory system, atherosclerosis, hypertension, pulmonary circulation disease, and ischemic heart disease were important contributors to these improvements. Also important were musculoskeletal conditions, accounting for about one-third of the decline in disability, and vision, especially the improved treatment of cataracts, which showed particularly large decreases. Less important were changes in diseases of the digestive system, senility, diseases of the ear, and diabetes. The other conditions listed in table 2—cancer, lung disease, mental conditions, and nervous system disease—contributed to increases, not decreases, in disabilities over this period.
Between 1997 and 2005, the annual decline in disability prevalence was 0.31 percentage points, somewhat higher than during the earlier period. This estimate implies a drop over this period of 2.5 percentage points. Despite the less detailed information on causal conditions for 1997 to 2005, the patterns are quite similar in the two periods. That is, a substantial share of the decline in disability was accounted for by changes in heart and circulatory disease, vision, and musculoskeletal conditions. The contributions of each of these conditions was documented further by Freedman and colleagues (2007), using models for 1997 to 2004 that included multiple conditions and sociodemographic factors.
Changes in Medical Care
The finding that particular classes of conditions were less likely to be reported as causes of late-life disability suggests that advances in medical care may play a prominent role in the disability trend. For example, as described by Cutler and colleagues (2006) and Freedman and colleagues (2007), the treatments for heart and circulatory disease and for vision problems have changed significantly. The pharmacologic treatment of cardiovascular disease using, for example, beta blockers, ace inhibitors, anticholesterol agents, and antihypertensive combinations, has expanded (Moeller, Miller, and Banthin 2004), and declines in high-risk total cholesterol and homocysteine have been documented (Crimmins et al. 2005). Such surgical procedures as stent insertion to hold open narrowed arteries, first introduced in the early 1990s, and balloon angioplasty also have increased substantially. Among the population sixty-five and older, the rate of coronary artery stent insertion per 100,000 population nearly tripled within just four years, from 251 in 1996 to 672 in 2000 (National Center for Health Statistics 2003).
The treatment of vision impairment also has undergone significant advances. The major causes of vision impairment in late life are age-related macular degeneration, glaucoma, cataracts, and diabetic retinopathy (U.S. Department of Health and Human Services 2000). The major source of vision improvements reported in table 2 are cataracts, which now can be corrected by surgery that replaces the clouded lens with an artificial one. The number of cataract surgeries more than doubled between 1984 and 1995 (Desai et al. 2001), and it is now the most frequently performed surgery in the United States, with more than 1.5 million each year. Nine out of ten people who have cataract surgery regain very good vision, somewhere between 20/20 and 20/40, and there is evidence that cataract surgery also can improve functioning and reduce disability (Applegate et al. 1987; Owsley et al. 2002; Wood and Carberry 2006).
Although varying by the specific condition, musculoskeletal treatments also have changed in both surgical techniques and materials, for example, with major advances in hip and knee replacement. These procedures are much less risky than in the past, and the number of knee replacement surgeries increased from 390 per 100,000 in 1991 to 650 per 100,000 in 2000 for people aged sixty-five to seventy-four (National Center for Health Statistics 2003). The trend during this period has been toward the increased use of nonsteroidal anti-inflammatory drugs, the expansion and then the contraction in the use of COX 2 inhibitors for osteoarthritis, and the increased use of antirheumatic drugs for rheumatoid arthritis (Fries et al. 1996; Ward and Fries 1998).
Changes in Health Behaviors
Besides medical care, many other factors may influence the trends in older people's disablement process. Changes in health behaviors over time may be important, particularly in reducing chronic disease incidence, but they have not been a focus of much attention in the literature on old-age disability trends. Here we review the evidence for smoking and physical activity.
Smoking
Smoking is strongly associated with lung disease, heart disease, and mortality (see, e.g., U.S. Department of Health and Human Services 1990), and therefore it is a natural candidate to consider. Figure 4 shows smoking status (i.e., has a person ever smoked?) by age for 1983, 1994, and 2005, years for which detailed smoking data are available from the NHIS and that span the time we are examining. At almost all ages, the rate of smoking fell substantially during this period. Only those people about seventy and older did not show reductions in ever having smoked. Similarly, the share who currently smoke (not shown in the figures) dropped between 1983 and 2005 for all ages except people eighty and older. The lack of decline for the oldest old may be due to true differences in smoking behavior across birth cohorts or because smokers are now more likely to live until older ages than earlier cohorts did. If it is the former, and if the association between smoking and disability remains the same, then the large drop in the smoking rate during the past twenty years among people under about seventy bodes well for improvements in old-age disability for these birth cohorts when they grow older.
Figure 4.
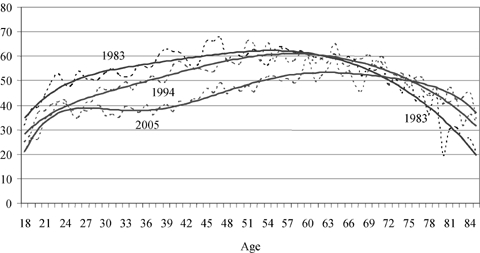
Percentage Who Ever Smoked, by Age: 1983, 1994, and 2005.
Source: Authors' tabulations using the National Health Interview Survey.
Table 3 reports estimates from logistic models looking at whether or not trends in smoking can account for trends in old-age disability. Given the lack of decline in smoking for people seventy and older, as shown in figure 4, we do not expect smoking to account for disability trends for this population. The models use the NHIS data for the population seventy and older for each year that smoking behavior was assessed (1983, 1985, 1987, 1990–1994, 1997–2005). Model 1 reports the sex- and age-adjusted annual percentage decline in disability for these years. The odds ratio of 0.9897 is an annual percentage decline of 1.03 percent (=(1 – 0.9897) × 100.) Model 2 controls for smoking with three groups identified in the NHIS data: never a smoker, current smoker, former smoker. As expected, current smokers were more likely to report a disability than were quitters, who in turn were more likely to report a disability than were people who had never smoked. Nonetheless, smoking behavior accounted for none of the drop in disability prevalence, for the estimated annual rate of decline was 1.02 percent after adjusting for smoking. In addition, controlling for race/ethnicity, education, and income led to the same substantive conclusion. This result is consistent with the findings in table 2 that lung disease and cancer accounted for very little of the decline in disability. It also suggests that the decline in reports of heart disease causing disability did not stem from changes in smoking behavior.
TABLE 3.
Odds Ratio from Logistics Models of Any Disability: Effects of Smoking (Reports in Italics Are the Implied Average Annual Percentage Change in Disability)
| Explanatory Variables | Model 1 | Model 2 |
|---|---|---|
| Trend∼ | 0.9897* | 0.9898** |
| −1.03 | −1.02 | |
| Age | ||
| 70–74 (reference group) | ||
| 75–79 | 1.4939** | 1.5211** |
| 80–84 | 2.5717** | 2.6674** |
| 85+ | 5.3353** | 5.6330** |
| Smoking | ||
| Never (reference group) | ||
| Current | 1.4393** | |
| Former | 1.1363** | |
Notes: Other controls included in all models: sex, proxy, post-1996, proxy*post-1996, don't know if proxy, don't know if proxy*post-1996.
∼“Trend” is a linear term that takes the value 0 in the base year and increments by 1 for each subsequent calendar year.
**and *indicate statistical significance of the effect within a model of a given variable on the odds of having disability at the .01 and .05 levels, respectively.
N = 69,063; Years of data: 1983, 1985, 1987, 1990–1994, 1997–2005.
Physical Activity
In recent decades, greater physical activity has frequently been recommended as a pathway to better health and the prevention of many conditions (see, e.g., U.S. Department of Health and Human Services 1996). For a number of reasons, though, it is difficult to determine whether these exhortations have contributed to the declines in disability. Data on trends in aspects of physical activity (e.g., the physical strenuousness of work versus leisure activities) at the population level are quite limited and show different trajectories (Johnson 2004; National Center for Health Statistics 2006). Furthermore, measuring physical activity, whether at work or play, is challenging (Manini et al. 2006). Assessing the causal relations between physical activity and various health outcomes also is difficult because health may influence the amount of activity reported. One strategy is to use longitudinal data, as was done in studies of cognitive function (Abbott et al. 2004; Weuve et al. 2004) and disability (Clark 1996) that showed protective effects of walking. The substantial literature on late-life exercise interventions shows improvements in physical function but not necessarily in disability (Keysor and Jette 2001). In sum, the evidence for physical activity as a factor in the decline in disability is suggestive but thin and difficult to interpret.
Obesity
Disability in late life has also been linked to obesity, which is a function of diet, physical activity, and metabolism. Recent analyses, based on the disability/obesity relation in the cross section for those aged fifty to sixty-nine, together with trends in obesity, have highlighted the possibility that increasing obesity prevalence may reverse the improvements in old-age disability that we are discussing here (Sturm, Ringel, and Andreyeva 2004). Indeed, Freedman and Martin (2000) found in their analysis of trends from 1984 to 1995 in chronic conditions and functional limitations among the population seventy and over that their functioning would have improved even more were it not for the increase in obesity. Moreover, between 1997 and 2004, Freedman and colleagues (2007) showed that obesity tripled as a reported cause of disability, although its prevalence still remained low (in 2004, just 0.37 percent of people sixty-five and older reported having an ADL or IADL disability and that a weight problem had caused it). These results are notable because past evidence has suggested that health problems related to obesity might be attenuated with age because of mortality selection (Crimmins 2001). But because the proportion of older people who are overweight or obese is growing (Flegal et al. 2005), this factor is unlikely to account for declines in late-life disability.
Changes in Economic and Sociodemographic Factors
Age, Race/Ethnicity, Marital Status, and Place of Birth
Throughout life, disparities in health across demographic factors are substantial, and the demographic composition of the older population also has changed substantially in recent decades. Previous studies (Schoeni, Freedman, and Martin 2005) considered the role of these factors in the decline in disability from 1982 to 2002. Here we update that analysis using data from the 1982 to 2005 NHIS and the series of logistic models of any disability in table 4.
TABLE 4.
Odds Ratios from Logistic Models of Any Disability: Effects of SES and Demographic Factors (Reports in Italics Are the Implied Average Annual Percentage Change in Disability)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Trend∼ | 0.990** | 0.985** | 0.985** | 0.987** | 0.982** | 0.982** | 0.993** | 0.988** | 0.994* |
| −1.05 | −1.48 | −1.50 | −1.35 | −1.76 | −1.77 | −0.68 | −1.16 | −0.58 | |
| Age | |||||||||
| 70–74 (reference group) | |||||||||
| 75–79 | 1.592** | 1.607** | 1.541** | 1.564** | 1.564** | 1.509** | 1.527** | 1.504** | |
| 80–84 | 2.768** | 2.813** | 2.564** | 2.622** | 2.623** | 2.463** | 2.523** | 2.447** | |
| 85+ | 5.821** | 5.948** | 5.061** | 5.250** | 5.257** | 4.758** | 4.986** | 4.743** | |
| Race/ethnicity | |||||||||
| Hispanic (reference group) | |||||||||
| Non-Hispanic white | 0.711** | 0.755** | 0.757** | 0.744** | 0.881** | 0.805** | 0.909** | ||
| Non-Hispanic black | 1.317** | 1.290** | 1.274** | 1.250** | 1.341** | 1.270** | 1.321** | ||
| Non-Hispanic other | 0.707** | 0.714** | 0.698** | 0.697** | 0.775** | 0.746** | 0.789** | ||
| Married | 0.583** | 0.542** | 0.542** | 0.606** | 0.619** | 0.633** | |||
| Foreign born | 0.968 | ||||||||
| Education | |||||||||
| 0–8 (reference group) | |||||||||
| 9–11 | 0.820** | 0.838** | |||||||
| 12 | 0.662** | 0.695** | |||||||
| 13–15 | 0.617** | 0.657** | |||||||
| 16+ | 0.591** | 0.640** | |||||||
| Income | |||||||||
| <$10,000 (reference) | |||||||||
| $10,000–19,999 | 0.738** | 0.774** | |||||||
| $20,000–29,999 | 0.632** | 0.691** | |||||||
| $30,000–39,999 | 0.585** | 0.641** | |||||||
| $40,000–49,999 | 0.589** | 0.655** | |||||||
| >=$50,000 | 0.596** | 0.688** | |||||||
| N | 194,973 | 194,973 | 194,973 | 194,973 | 141,583 | 141,583 | 194,973 | 194,973 | 194,973 |
| Time period | 1982–2005 | 1982–2005 | 1982–2005 | 1982–2005 | 1989–2005 | 1989–2005 | 1982–2005 | 1982–2005 | 1982–2005 |
Notes: Other controls included in all models: sex, proxy, post-1996, proxy*post-1996, don't know if proxy, don't know if proxy*post-1996.
A dummy variable that takes the value one if education is missing is also included in the models when education is examined.
∼“Trend” is a linear term that takes the value 0 in the base year and increments by 1 for each subsequent calendar year.
**and *indicate statistical significance of the effect within a model of a given variable on the odds of having disability at the .01 and .05 levels, respectively.
Model 1 in table 4, which controls only for sex and proxy status, estimates that the decline in disability was 1.05 percent per year. Because the population seventy and older itself aged during this period, controlling for age increased the estimated annual decline to 1.48 percent (model 2). Adjusting for race/ethnicity slightly increased the estimated trend to 1.50 percent (model 3). The share of the population seventy and older that was married rose from 47 to 53 percent (not reported in the table), and married people were much less likely to report a disability. As a result, the estimated trend fell to 1.35 percent once marital status was included in the model (model 4).
Over the past twenty years or so, the number of immigrants to the United States has risen substantially, so we investigated the implications of this shift by including in the model controls for whether the person was born in another country. These data are available from 1989 onward, so we first report in model 5 the same specification as in model 4, but for 1989 to 2005. (Data on the specific country of birth are not available in the NHIS.) Model 5 shows an average percentage decline of 1.76 percent, somewhat larger than the decline over the full period from 1982 to 2005. Adding a control for being born outside the United States (model 6) did not change the estimated decline, so shifts in the percentage of foreign born accounted for none of the decline in disability.
In a series of comparable multinomial logit models that further distinguished between ADL and IADL-only disabilities (not shown), we found substantially similar results. That is, the prevalence of IADL-only disabilities fell about 1.7 percent per year, whereas that of ADL disabilities was flat. We further found that controlling for age increased the IADL-only trend to 2.1 percent per year and that adding race/ethnicity made no difference. Adjusting for marital status reduced the trend only slightly, to 1.9 percent, and controlling for the percentage of foreign born accounted for none of the decline in IADL disability.
Education
As with sex and race/ethnicity, the influence of education continues throughout a person's life, and the mechanisms by which it influences health are many (Cutler and Lleras-Muney 2006; Ross and Wu 1995). Education can improve health behaviors, social support, income, access to care, quality of care, and quality of self-management of disease (Goldman and Smith 2002). A greater amount of education also may be associated with the greater use of assistive technologies or modifications to home and work environments (Freedman et al. 2005).
Education is perhaps the most widely cited factor related to recent trends in late-life functioning. Persons having less than a high school education, for example, have double the risk of developing late-life functional limitations compared with those having graduated from high school (Freedman and Martin 1999). Moreover, the educational attainment of older cohorts has risen dramatically over the past few decades. For those people seventy and older, 46 percent had zero to eight years of education as of 1982, but by 2005 this proportion had dropped to 17 percent.
We added education to our model of disability in table 4 and found that it lowered the estimated rate of decline in disability from 1.35 (model 4) to 0.68 percent (model 7). Thus, one-half the decline in disability can be accounted for by the rise in educational attainment. All the (very small and not significant) decline in ADL disabilities and more than one-third of the decline in IADL-only disabilities are accounted for by educational shifts in the population (not shown).
What is unclear is whether or not this relationship represents a causal effect of education and whether or not the predicted increases in educational attainment in the coming decades can be expected to cause subsequent declines in disability. Some studies that explicitly address this issue did indeed conclude that education has a causal influence on health (Adams et al. 2003). But Freedman and Martin (1999) cautioned that although the educational attainment of the older population will continue to rise, it will do so more slowly and that the advantage for functioning associated with greater education may change over time.
Income and Poverty
At an individual level, people with low incomes, and especially those in poverty, have a higher mortality rate and a worse health status (for reviews, see Preston and Taubman 1994; Smith 1999). At a national level, trends in old-age poverty and disability also show a very close correspondence (figure 5). When the old-age poverty rate fell rapidly in the early 1980s, so too did the prevalence of disability. Then, when the poverty rate increased in the early 1990s, disability prevalence increased as well. The simple correlation between these two outcomes is very high, at 0.93.
Figure 5.
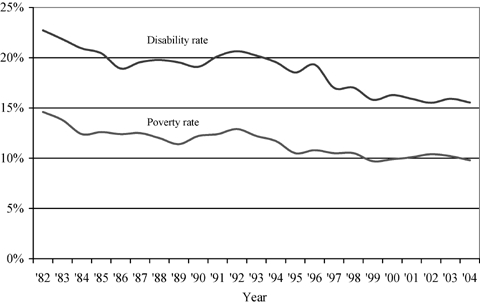
Poverty and Disability Rates for Noninstitional Population 70 and Older, 1982 to 2004.
Source: Disability rates are based on authors' tabulations using the National Health Interview Survey, and poverty rates are from the U.S. Bureau of the Census.
Higher income may reduce disability by enabling older people with functional limitations to buy assistive technology and personal care, thereby allowing them to avoid disability. Higher income also may reduce disease and functional limitations by supporting the purchase of health-improving goods and services such as medical care, healthful foods, exercise equipment and classes, and safe homes and neighborhoods.
There is an ongoing debate over whether the empirical relationship between income and health represents the causal effects of these factors, and if it does, whether the cause runs from income to health or from health to income. Herd, House, and Schoeni (2006) reviewed the evidence for the older population and concluded that it was mixed. But a recent study found that increases in government cash assistance to the elderly did reduce the prevalence of disability among the poor (Herd, Schoeni, and House 2007). Some of the relationship represented by this simple correlation in figure 5 is clearly due to confounding factors and reverse causation. At the same time, higher incomes probably do have some beneficial effects on some health outcomes, at least for the very poor, for whom the income-health gradient is the steepest (Smith 1999).
We investigated this relationship further using the NHIS data and building on the models in table 4. Model 8 adds family income to the model, specified in categories of $10,000 increments up to $50,000. This model should be interpreted as only an accounting exercise and not as providing estimates of the causal effects of income on disability, but income clearly is a strong predictor of disability. Compared with the 10 percent of the population with incomes below $10,000, the group with incomes from $10,000 to $19,999 (18 percent of the sample) were 26 percent less likely to report a disability. Income was negatively associated with disability for those with incomes through $30,000 to $39,999 (incomes of 72 percent of the sample were below $40,000), but additional income was not associated with further declines in reported disabilities. Most important, the aggregate trend in disability fell to 1.16 percent once income was accounted for, representing a 14 percent decline compared with model 4 when income is not included. Results differentiating between ADL and IADL-only disabilities suggest that income accounts for a similar share of the IADL decline (not shown).
Finally, if all demographic, social, and economic factors are accounted for simultaneously, the estimated trend falls to −0.58 percent. While still statistically significant, this estimate is substantially smaller, and all these factors account for 61 percent of the simple trend in model 2, which was adjusted for only sex, age, and proxy status. Similarly, about 50 percent of the simple trend in IADL-only disability is accounted for by demographic, social, and economic factors (not shown).
Environmental Exposures
The surrounding environment can influence health and disability throughout life, but because poor health and disability are more likely in late life, environment may be especially important then. The built environment also may influence the disablement process, in several ways (Balfour and Kaplan 2002; Clarke and George 2005). For example, safe sidewalks and well-lit streets may lead to fewer injuries; better street connectivity, sidewalks, and curbs can facilitate physical activities; and access to health care facilities can mean better chronic care (World Health Organization 2002). Other outgrowths of the built environment, such as traffic, air pollution, and poor housing quality, may produce chronic stress over the life course, which in turn may lead to poor health outcomes (McEwen and Stellar 1993, Seeman and Chen 2002). In addition, older adults' social and economic environment is linked to health and disability (Rogowski, Freedman, and Schoeni 2006). Although the mechanisms are not well understood, many studies have demonstrated that the socioeconomic status of neighborhoods (e.g., poverty, poor educational attainment, high unemployment) are associated with worse health outcomes when controlling for individual socioeconomic status (for reviews, see Morenoff and Lynch 2002; Roberts 1999; Yen and Syme 1999; and, for an exception, Winkleby, Cubbin, and Ahn 2006). The neighborhood environment also can facilitate or impede social relationships, which in turn are linked to older adults' maintenance of health (House, Landis, and Umberson 1988; Seeman et al. 1995). To our knowledge, no analyses evaluating changes in older adults' neighborhoods or their contribution to recent disability trends have been published.
Early- and Midlife Factors
Evidence of the link among occupation, work-related injuries, and late-life disabilities and between earlier life events and late-life health is growing. But the goal of such research has not been to explain trends in old-age disability, and therefore the direct evidence as an explanation of these trends has not been thoroughly developed. Although we do not present any new analyses in this section, we do highlight two areas needing further investigation.
Occupation and Workplace Conditions
One of the earliest studies of disparities in health status, the Black Report, documented mortality disparities in Great Britain by social class (defined by occupation) (Townsend, Davidson, and Whitehead 1988). Subsequent work, including the famous Whitehall studies of British civil servants, showed that cause-specific mortality and morbidity were much lower among people in higher-class occupations (Buring et al. 1987; Marmot et al. 1991, 1997; Marmot, Shipley, and Rose 1984; Pocock et al. 1987; Van Rossum et al. 2000). Furthermore, U.S. evidence demonstrates that the effect of occupation on mortality is not simply an artifact of income and education differentials (Moore and Hayward 1990).
Recent evidence suggests that workplace injuries, accidents, and illnesses are a major determinant of disability for the older population. Reville and Schoeni (2003) found that nearly 50 percent of men aged fifty-one to sixty-one who were work disabled (i.e., their health limited their ability to work) claimed that they became disabled because of an accident or injury at work. Costa (2002) attributed long-run (from 1910 to 1990) declines in chronic conditions among white male veterans partly to shifts in occupation. More recent trends also show that the incidence of workplace injuries/illnesses in the United States has fallen since the 1970s (the earliest available national data). In the early 1970s, a large share of the workforce (more than ten per one hundred full-time workers per year) had injuries or accidents in the workplace. By 2004, however, that rate had been cut in half.
Steuerle, Spiro, and Johnson (1999) found that the percentage of workers in physically demanding jobs (requiring frequent lifting or carrying of heavy objects) dropped from about 20 percent in 1950 to 11 percent in 1970, with a further decline to 8 percent in 1996. Even these estimates are likely to understate the true decline because they do not consider that some jobs classified as physically demanding today have become less strenuous over time.
Other explanations for the decline in workplace-related disability are the expansion of safety requirements and changes in the industrial mix. For example, employment in the manufacturing industry, which historically has had a relatively high injury rate (e.g., 9.2 per 100 workers in 2000), has shrunk from 41 percent of employment in 1940 to 16 percent in 2000. At the same time, employment in the service industries, whose injury rate in 2000 was just 4.9 per 100 workers, has increased from 13 to 36 percent.
Early Childhood Conditions
In recent decades there has been a growing interest in the effects of earlier life factors on health outcomes in adult life (Kuh and Ben-Shlomo 1997; Lynch and Kaplan 2000; Power and Hertzman 1997). Perhaps best known is the work by Barker (1998), who observed that a mother's nutrition in pregnancy and pelvic size influenced fetal growth and birth weight, and who hypothesized that these in turn may cause lasting changes in metabolism and organ structure. Fogel (1994) compared Union Army veterans in 1910 with more recent veterans of the same ages in 1985 to 1988 and found that increasing body mass index and height were important factors in the declining prevalence of chronic disease. There also is a substantial literature associating greater height with reduced cardiovascular disease and related death (for a recent review, see Silventoinen et al. 2006). However, there is a continuing debate about the extent to which measures such as height reflect childhood nutrition versus childhood disease. Indeed, Blackwell, Hayward, and Crimmins (2001), using data from a 1996 experimental module of the Health and Retirement Study, found that in the cross section, childhood disease—but not height—was a significant predictor of disease at ages fifty-five to sixty-five. Studies have shown that low socioeconomic status in childhood—as measured by the father's occupation and/or the mother's education—predicts chronic diseases such as heart disease, arthritis, and diabetes (Blackwell, Hayward, and Crimmins 2001; Wannamethee et al. 1996) and cognitive function in late life (Freedman, Aykan, and Martin 2001; Turrell et al. 2002). In general, early-life conditions would be expected to have improved across the birth cohorts examined here, with higher standards of living and better nutrition, although shocks such as wars and depression may result in effects specific to particular birth cohorts.
Discussion
Many factors influence the process by which older adults develop a need for help with daily activities, including biology, medical care, and health behaviors, as well as economic, social, and environmental forces. Some of these factors have immediate effects, whereas others may result in the accumulation of advantages or disadvantages throughout life. All these influences may help explain the decline in disability. Given the available data, the sensitivity of the results to the years analyzed, and the complex structure of the relationship among various factors, identifying the causal influences of the declines in old-age disability is a tall order. No one study is likely to identify definitively all the causes and determine their contributing share, but we believe that our study has moved this exploration ahead significantly.
First, we have been able to eliminate some potential factors. Perhaps most important, the nation's smoking rates have fallen over the past several decades, but these declines do not account for the lower rate of disability for those aged seventy and older. The surviving members of cohorts with fewer disabilities did not change their smoking behavior to the same degree as other cohorts did. But those cohorts with greater declines in smoking will be entering old age soon, a factor that may help lower the prevalence of disability even more in the future.
Demographic factors such as racial/ethnic composition do not account for any of the improvements, and marital status accounts for only about 10 percent. The shift in the percentage of foreign born also explains none of the decline in disability, although additional analyses are needed to determine the association with changes in the mix of the foreign-born population by country of origin (information not available in the NHIS) as well as duration of residence. Based on self-reports of conditions causing disability, several common diseases, including cancer, diabetes, conditions of the ear, lung disease, mental conditions, and conditions of the nervous system, do not explain much or any of the declines in disability.
At the same time, the evidence points to several important factors. The nature of the disablement process itself seems to be changing. Assistive and mainstream technologies have become more widespread. In addition, the prevalence of physical and vision limitations has dropped, and heart and circulatory diseases, vision problems, and musculoskeletal conditions have fallen as reported causes of disability.
The timing of the improvements in these conditions corresponds to the expansion in medical procedures (stent insertion and balloon angioplasty) and pharmacologic treatment (beta blockers, ace inhibitors, anticholesterol agents, and antihypertensive combinations) of cardiovascular disease, the increased number of cataract surgeries, the greater number of knee and joint replacements, and the use of more medications for arthritic and rheumatic conditions. Of course, these advances in treatment have come with both individual and societal costs (Cutler 2004). The role of health behaviors is less clear, although it is possible that the growing trend toward obesity has been a countervailing force. That is, if fewer older adults had become obese, the decline in disability might have been slightly greater.
Socioeconomic factors appear to have played a substantial role. Most important, the large increase in educational attainment across cohorts accounts for one-half of the decline in disability prevalence between 1982 and 2005. Gains in income, especially for those people at the bottom of the income distribution, have contributed further to these changes. However, the mechanism through which socioeconomic factors may have helped achieve these gains has not yet been determined. Moreover, a recent analysis of longitudinal data highlighted the different associations of income and education with the onset versus the recovery of functional limitations (Zimmer and House 2003). A variety of other factors, such as the environment in which older adults live, occupational exposures, workplace safety, and early-life events, may be associated with disability, and additional research is needed to determine whether these factors can explain the trends in the prevalence of disability in the population. Further insights may be gained from greater attention to the potential role of societal level trends, including those in intrafamily relationships and gender roles, the market for caregiving, and attitudes toward independence, which may be the root cause of some of the observed changes in the explanatory factors we examined (Wolf, Hunt, and Knickman 2005).
We were not able to quantify the relative influence of all the factors explored here, but the literature has made some partial attempts to do so. For example, Freedman and colleagues (2007) modeled trends in disability from 1997 to 2004 as a function of causal conditions jointly with shifts in demographic and socioeconomic status. Their findings suggest that of the total 1.45 percentage point decline in disability during that period, chronic conditions accounted for twice as much as demographic factors did (69 percent versus 30 percent). Their analysis also suggests that the advantage associated with additional years of education may be waning and that the disadvantage associated with eight or fewer years of education is growing.
Explanations for the declines in the past few decades can be contrasted with the explanations for the long-run declines. Costa (2002), for example, attributes the twentieth-century declines in white males' chronic conditions to fewer infections (18 percent to 19 percent), shifts in occupation from manual to white collar (13 percent to 39 percent, depending on the conditions), and “unexplained” factors (40 percent to 65 percent). Similarly, Costa (2002) apportioned declines in functional limitations to falling chronic disease rates (37 percent), less-debilitating conditions (24 percent), and “unexplained” factors (39 percent). Unexplained factors include improvements in nutrition, food preparation, and storage; improvements in the public health infrastructure; and the widespread use of effective medical treatments such as antibiotics, but Costa did not offer explicit tests of such hypotheses.
Of course, we cannot assume that the gains achieved in the past will continue or that the causes of earlier improvements will lead to further declines. But the evidence indicates that for the cohorts currently approaching old age, the rate of smoking is lower and their educational attainment is higher relative to those of older birth cohorts. Both these developments may work to reduce disability prevalence further. At the same time, rising obesity levels may, to some degree, offset these trends. In addition, the influences of cognitive limitations and dementia on disability trends and the differential trends of ADL and IADL disabilities need to be more fully understood.
Declining late-life disability prevalence represents one of the most significant advances in the health and well-being of Americans in the past quarter century. Explaining what caused these improvements and predicting future changes are important to policy and research, but another goal should be to find ways to reduce the number of these disabilities further. These reductions might come from new and cheaper accommodations, medical advances, behavioral interventions, or perhaps social and economic changes. Some of the innovations associated with the recent declines in disability, including pharmacologic treatments and assistive devices, were developed to improve health status and functioning, but others, such as the expansion of educational attainment, were motivated by different goals. A broad effort should be mounted to identify potential interventions and then systematically evaluate their effectiveness.
Acknowledgments
This research was funded by a grant from the National Institute on Aging (R01-AG021516). We thank Tim Waidmann and Jim Lubitz for their helpful comments.
References
- Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, Petrovitch H. Walking and Dementia in Physically Capable Elderly Men. Journal of the American Medical Association. 2004;292(12):1447–53. doi: 10.1001/jama.292.12.1447. [DOI] [PubMed] [Google Scholar]
- Adams P, Hurd M, McFadden D, Merrill A, Ribeiro T. Healthy, Wealthy, and Wise? Tests for Direct Causal Paths between Health and Socioeconomic Status. Journal of Econometrics. 2003;112(1):3–56. [Google Scholar]
- Allaire SH, LaValley MP, Evans SR, O'Connor GT, Kelly-Hayes M, Meenan RF, Levy D, Felson DT. Evidence for Decline in Disability and Improved Health among Persons Aged 55 to 70 Years: The Framingham Heart Study. American Journal of Public Health. 1999;89(11):1678–83. doi: 10.2105/ajph.89.11.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Association of Retired Persons. Beyond 50.03: A Report to the Nation on Independent Living and Disability. Washington D.C.: AARP Public Policy Institute; 2003. [accessed December 4, 2007]. Available at http://research.aarp.org/il/beyond_50_il.html. [Google Scholar]
- Applegate WB, Miller ST, Elam JT, Freeman JM, Wood TO, Gettlefinger TC. Impact of Cataract Surgery with Lens Implantation on Vision and Physical Function in Elderly Patients. Journal of the American Medical Association. 1987;257(8):1064–66. [PubMed] [Google Scholar]
- Balfour JL, Kaplan GA. Neighborhood Environment and Loss of Physical Function in Older Adults: Evidence from the Alameda County Study. American Journal of Epidemiology. 2002;155(6):507–15. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- Barker DJP. Mothers, Babies and Health in Later Life. Edinburgh: Churchill Livingstone; 1998. [Google Scholar]
- Blackwell DL, Hayward MD, Crimmins E. Does Childhood Health Affect Chronic Morbidity in Later Life? Social Science and Medicine. 2001;52(8):1269–84. doi: 10.1016/s0277-9536(00)00230-6. [DOI] [PubMed] [Google Scholar]
- Buring JE, Evans DA, Fiore M, Rosner B, Hennekens CH. Occupation and Risk of Death from Coronary Heart Disease. Journal of the American Medical Association. 1987;258(6):791–92. [PubMed] [Google Scholar]
- Clark DO. The Effect of Walking on Lower Body Disability among Older Blacks and Whites. American Journal of Public Health. 1996;86(1):57–61. doi: 10.2105/ajph.86.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, George LK. The Role of the Built Environment in the Disablement Process. American Journal of Public Health. 2005;95(11):1933–39. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa DL. Changing Chronic Disease Rates and Long-Term Declines in Functional Limitation among Older Men. Demography. 2002;39(1):119–37. doi: 10.1353/dem.2002.0003. [DOI] [PubMed] [Google Scholar]
- Crimmins EM. Mortality and Health in Human Life Spans. Experimental Gerontology. 2001;36(4–6):885–97. doi: 10.1016/s0531-5565(00)00248-5. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Alley D, Reynolds SL, Johnston M, Karlamangla A, Seeman T. Changes in Biological Markers of Health: Older Americans in the 1990s. Journals of Gerontology: Medical Sciences. 2005;60A:1409–13. doi: 10.1093/gerona/60.11.1409. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y. Change in the Prevalence of Diseases among Older Americans: 1984–1994. Demographic Research. 2000;3(9) [Google Scholar]
- Cutler DM. Declining Disability among the Elderly. Health Affairs. 2001;20(6):11–27. doi: 10.1377/hlthaff.20.6.11. [DOI] [PubMed] [Google Scholar]
- Cutler DM. Your Money or Your Life? Strong Medicine for America's Health Care System. New York: Oxford University Press; 2004. [Google Scholar]
- Cutler DM, Landrum MB, Stewart K. Intensive Medical Care and Cardiovascular Disease Disability Reductions. Cambridge Mass.: Harvard University; 2006. NBER Working Paper 12184. [Google Scholar]
- Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence. Ann Arbor: University of Michigan; 2006. National Poverty Center Working Paper 2006-19. [Google Scholar]
- Desai M, Pratt LA, Lentzner H, Robinson KN. Trends in Vision and Hearing among Older Americans. Aging Trends. 2001;(2):1–8. doi: 10.1037/e620682007-001. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess Deaths Associated with Underweight, Overweight, and Obesity. Journal of the American Medical Association. 2005;293(15):1861–67. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Fogel RW. Economic Growth, Population Theory, and Physiology: The Bearing of Long-Term Processes on the Making of Economic Policy. American Economic Review. 1994;84(3):369–95. [Google Scholar]
- Freedman VA. Late-Life Disability Trends: An Overview of Current Evidence. In: Field M, Jette A, Martin L, editors. Workshop on Disability in America: A New Look. Washington D.C.: National Academies Press; 2006. pp. 101–12. [Google Scholar]
- Freedman VA, Agree E, Martin LG, Cornman JC. Trends in the Use of Assistive Technology and Personal Care for Late-Life Disability, 1992–2001. The Gerontologist. 2006;46(1):124–27. doi: 10.1093/geront/46.1.124. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Aykan H, Martin LG. Aggregate Changes in Severe Cognitive Impairment among Older Americans: 1993 and 1998. Journal of Gerontology: Social Sciences. 2001;56B(2):100–11. doi: 10.1093/geronb/56.2.s100. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Aykan H, Martin LG. Another Look at Aggregate Changes in Severe Cognitive Impairment: Cumulative Effects of Three Survey Design Issues. Journals of Gerontology: Social Sciences. 2002;57:S126–31. doi: 10.1093/geronb/57.2.s126. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Crimmins EM, Schoeni RF, Spillman BC, Aykan H, Kramarow E, Land K, Lubitz J, Manton K, Martin LG, Shinberg D, Waidmann T. Resolving Inconsistencies in Trends in Old-Age Disability: Report from a Technical Working Group. Demography. 2004;41(3):417–41. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Hodgson N, Lynn J, Spillman B, Waidmann T, Wilkinson A, Wolf DA. Promoting Declines in the Prevalence of Late-Life Disability: Comparisons of Three Potentially High-Impact Interventions. The Milbank Quarterly. 2006;84(3):493–520. doi: 10.1111/j.1468-0009.2006.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Martin LG. Understanding Trends in Functional Limitations among Older Americans. American Journal of Public Health. 1998;88(10):1457–62. doi: 10.2105/ajph.88.10.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Martin LG. The Role of Education in Explaining and Forecasting Trends in Functional Limitations among Older Americans. Demography. 1999;36(4):461–73. [PubMed] [Google Scholar]
- Freedman VA, Martin LG. Contribution of Chronic Conditions to Aggregate Changes in Old-Age Functioning. American Journal of Public Health. 2000;90(11):1755–60. doi: 10.2105/ajph.90.11.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Martin LG. Beyond Inconsistent Results: Finding the Truth about Trends in Late-Life Cognitive Functioning. Journals of Gerontology: Social Sciences. 2003;58B:S347–48. doi: 10.1093/geronb/58.6.s347. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Cornman JC, Agree EM, Schoeni RF. Trends in Assistance with Daily Activities: Racial/Ethnic and Socioeconomic Disparities Persist in the U.S. Older Population. Ann Arbor: University of Michigan; 2005. TRENDS Working Paper 05-2. [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent Trends in Disability and Functioning among Older Adults in the United States: A Systematic Review. Journal of the American Medical Association. 2002;288(24):3137–46. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Schoeni RF, Martin LG, Cornman JC. Chronic Conditions and the Decline in Late-Life Disability. Demography. 2007;44(3):459–77. doi: 10.1353/dem.2007.0026. [DOI] [PubMed] [Google Scholar]
- Fries JF, Williams CA, Morfeld D, Singh G, Sibley J. Reduction in Long-Term Disability in Patients with Rheumatoid Arthritis by Disease-Modifying Antirheumatic Drug-Based Treatment Strategies. Arthritis and Rheumatism. 1996;39(4):616–22. doi: 10.1002/art.1780390412. [DOI] [PubMed] [Google Scholar]
- Goldman D, Smith JP. Can Patient Self-Management Help Explain the SES Health Gradient? Proceedings of the National Academy of Sciences. 2002;99(16):10929–34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herd P, House J, Schoeni RF. Income Support Policies and Health among the Elderly. Ann Arbor: University of Michigan; 2006. National Poverty Center Working Paper 06-27. [Google Scholar]
- Herd P, Schoeni RF, House J. Does the Supplemental Security Income Program Reduce Disability among the Elderly? University of Michigan; 2007. Working Paper. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social Relationships and Health. Science. 1988;241:540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Johnson RW. Trends in Job Demands among Older Workers, 1992–2002. Monthly Labor Review. 2004;127(7):48–56. [Google Scholar]
- Keysor JJ, Jette AM. Have We Oversold the Benefit of Late-Life Exercise? Journal of Gerontology: Medical Sciences. 2001;56A(7):M412–23. doi: 10.1093/gerona/56.7.m412. [DOI] [PubMed] [Google Scholar]
- Kuh D, Ben-Shlomo Y. A Life Course Approach to Chronic Disease Epidemiology. Oxford: Oxford University Press; 1997. [PubMed] [Google Scholar]
- Lubitz J, Greenberg L, Gorinaa Y, Wartzman L, Gibson D. Three Decades of Health Care Use by the Elderly: 1965–1998. Health Affairs. 2001;20:19–32. doi: 10.1377/hlthaff.20.2.19. [DOI] [PubMed] [Google Scholar]
- Lynch J, Kaplan G. Socioeconomic Position. In: Berkman L, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- Manini TM, Everhart JE, Patel KV, Schoeller DA, Colbert LH, Visser M, Tylavsky F, Bauer DC, Goodpaster BH, Harris TB. Daily Activity Energy Expenditure and Mortality among Older Adults. Journal of the American Medical Association. 2006;296(2):171–79. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- Manton KG, Corder L, Stallard E. Changes in the Use of Personal Assistance and Special Equipment from 1982 to 1989: Results from the 1982 and 1989 NLTCS. The Gerontologist. 1993;33(2):168–76. doi: 10.1093/geront/33.2.168. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. Change in Chronic Disability from 1982 to 2004/2005 as Measured by Long-Term Changes in Function and Health in the U.S. Elderly Population. Proceedings of the National Academy of Sciences. 2006;103(48):18374–79. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Gu X, Ukraintseva S. Declining Prevalence of Dementia in the U.S. Elderly Population. Advances in Gerontology. 2005;16:30–37. [PubMed] [Google Scholar]
- Manton KG, Stallard E, Corder LS. Changes in Morbidity and Chronic Disability in the U.S. Elderly Population: Evidence from the 1982, 1984, and 1989 National Long Term Care Surveys. Journals of Gerontology. 1995;50(B):S194–204. doi: 10.1093/geronb/50b.4.s194. [DOI] [PubMed] [Google Scholar]
- Mare DR. Response: Statistical Models of Educational Stratification—Hauser and Andrew's Models for School Transitions. Sociological Methodology. 2006;36:27–37. [Google Scholar]
- Marmot MG, Bosma H, Hemingway H, Brunner EJ, Stansfeld SA. Contribution of Job Control and Other Risk Factors to Social Variations in Coronary Heart Disease Incidence. Lancet. 1997;350:235–39. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Stansfeld S, Patel C, North F, Head J, White I, Brunner E, Feeney A, Smith G Davey. Health Inequalities among British Civil Servants: The Whitehall II Study. Lancet. 1991;337:1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Shipley MJ, Rose G. Inequalities in Death—Specific Explanations of a General Pattern. Lancet. 1984;1(8384):1003–6. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Stellar E. Stress and the Individual: Mechanisms Leading to Disease. Archives of Internal Medicine. 1993;153(19):2093–2101. [PubMed] [Google Scholar]
- McGinnis MJ, Williams-Russo P, Knickman J. The Case for More Active Policy Attention to Health Promotion. Health Affairs. 2002;21(2):78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- McKeown T. The Role of Medicine: Dream, Mirage or Nemesis? Oxford: Blackwell; 1979. [Google Scholar]
- McKinlay JB, McKinlay SM. The Questionable Contribution of Medical Measures to the Decline of Mortality in the United States in the Twentieth Century. The Milbank Memorial Fund Quarterly: Health and Society. 1977;55(3):405–28. [PubMed] [Google Scholar]
- Moeller JF, Miller GE, Banthin JS. Looking inside the Nation's Medicine Cabinet: Trends in Outpatient Drug Spending by Medicare Beneficiaries, 1997 and 2001. Health Affairs. 2004;23(5):217–25. doi: 10.1377/hlthaff.23.5.217. Millwood. [DOI] [PubMed] [Google Scholar]
- Moore DE, Hayward MD. Occupational Careers and Mortality of Elderly Men. Demography. 1990;27(1):31–53. [PubMed] [Google Scholar]
- Morenoff J, Lynch J. Washington D.C.: 2002. What Makes a Place Healthy? Neighborhood Influences on Racial/Ethnic Disparities in Health over the Life Course Paper prepared for Workshop on Ethnic Disparities in Aging Health. [Google Scholar]
- National Center for Health Statistics. Health Care in America: Trends in Utilization. Hyattsville Md: 2003. [Google Scholar]
- National Center for Health Statistics. Trends in Health and Aging website. 2006. [accessed July 27, 2006]. Available at http://209.217.72.34/aging/TableViewer/tableView.aspx.
- Owsley C, McGwin G, Sloane M, Wells J, Stalvey BT, Gauthreaux S. Impact of Cataract Surgery on Motor Vehicle Crash Involvement by Older Adults. Journal of the American Medical Association. 2002;288(7):841–49. doi: 10.1001/jama.288.7.841. [DOI] [PubMed] [Google Scholar]
- Pocock SJ, Cook DJ, Shaper AG, Phillips AN, Walker M. Social Class Differences in Ischemic Heart Disease in British Men. Lancet. 1987;330(8552):197–201. doi: 10.1016/s0140-6736(87)90774-4. [DOI] [PubMed] [Google Scholar]
- Pope AM, Tarlov AR. Disability in America: Toward a National Agenda for Prevention. Washington D.C.: National Academy Press; 1991. [Google Scholar]
- Power C, Hertzman C. Social and Biological Pathways Linking Early Life and Adult Disease. British Medical Bulletin. 1997;53(1):210–22. doi: 10.1093/oxfordjournals.bmb.a011601. [DOI] [PubMed] [Google Scholar]
- Preston SH. Mortality Trends. Annual Review of Sociology. 1977;3:163–78. [Google Scholar]
- Preston SH, Taubman P. Socioeconomic Differences in Adult Mortality and Health Status. In: Martin LG, Preston SH, editors. Demography of Aging. Washington D.C.: National Academy Press; 1994. pp. 279–318. [Google Scholar]
- Reville R, Schoeni RF. The Fraction of Disability Caused at Work. Social Security Bulletin. 2003;65(4):31–37. [PubMed] [Google Scholar]
- Roberts SM. Socioeconomic Position and Health: The Independent Contribution of Community Socioeconomic Context. Annual Review of Sociology. 1999;25:489–516. [Google Scholar]
- Rodgers WL, Ofstedal MB, Herzog AR. Trends in Scores on Tests of Cognitive Ability in the Elderly U.S. Population, 1993–2000. Journals of Gerontology. 2003;58:S338–46. doi: 10.1093/geronb/58.6.s338. [DOI] [PubMed] [Google Scholar]
- Rogowski J, Freedman VA, Schoeni RF. Neighborhoods and the Health of the Elderly: Challenges in Using National Survey Data. 2006. Michigan Population Studies Center Research Report 06-600, Ann Arbor.
- Ross CE, Wu C. The Links between Education and Health. American Sociological Review. 1995;60:719–45. [Google Scholar]
- Russell JN, Hendershot GE, LeClere F, Howie LJ, Adler M. Trends and Differential Use of Assistive Technology Devices: United States, 1994. Advance Data. 1997;(292):1–9. [PubMed] [Google Scholar]
- Schoeni RF, Freedman VA, Martin LG. Socioeconomic and Demographic Disparities in Trends in Old-Age Disability. Ann Arbor: University of Michigan; 2005. TRENDS Working Paper 05-1. [Google Scholar]
- Schoeni RF, Freedman VA, Wallace RB. Persistent, Consistent, Widespread, and Robust? Another Look at Recent Trends in Old-Age Disability. Journals of Gerontology: Social Science. 2001;56:S206–18. doi: 10.1093/geronb/56.4.s206. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Berkman LF, Charpentier PA, Blazer DG, Albert MS, Tinetti ME. Behavioral and Psychosocial Predictors of Physical Performance: MacArthur Studies of Successful Aging. Journals of Gerontology: Biological and Medical Science. 1995;50(4):M177–83. doi: 10.1093/gerona/50a.4.m177. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Chen X. Risk and Protective Factors for Physical Functioning in Older Adults with and without Chronic Conditions: MacArthur Studies of Successful Aging. Journals of Gerontology: Psychological and Social Science. 2002;57:S135–44. doi: 10.1093/geronb/57.3.s135. [DOI] [PubMed] [Google Scholar]
- Silventoinen K, Zdravkovic S, Skytthe A, McCarron P, Herskind AM, Koskenvuo M, de Faire U, Pedersen N, Christensen K, Kaprio J for the GenomEUtwin Project. Association between Height and Coronary Heart Disease Mortality: A Prospective Study of 35,000 Twin Pairs. American Journal of Epidemiology. 2006;163(7):615–21. doi: 10.1093/aje/kwj081. [DOI] [PubMed] [Google Scholar]
- Singer BH, Manton KG. The Effects of Health Changes on Projections of Health Service Needs for the Elderly Population of the United States. Proceedings of the National Academy of Sciences USA. 1998;95(26):15618–22. doi: 10.1073/pnas.95.26.15618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JP. Healthy Bodies and Thick Wallets: The Dual Relation between Health and Economic Status. Journal of Economic Perspectives. 1999;13(2):145–66. [PMC free article] [PubMed] [Google Scholar]
- Spillman BC. Changes in Elderly Disability Rates and the Implications for Health Care Utilization and Cost. The Milbank Quarterly. 2004;82(1):157–94. doi: 10.1111/j.0887-378X.2004.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steuerle CE, Spiro C, Johnson RW. Can Americans Work Longer? Straight Talk on Social Security and Retirement Policy, Number. 1999;5 Urban Institute. [Google Scholar]
- Sturm R, Ringel JS, Andreyeva T. Increasing Obesity Rates and Disability Trends. Health Affairs. 2004;23(2):199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- Townsend P, Davidson N, Whitehead M. Inequalities in Health. London: Penguin; 1988. [Google Scholar]
- Turrell G, Lynch JW, Kaplan GA, Everson SA, Helkala E, Kauhanen J, Salonen JT. Socioeconomic Position across the Lifecourse and Cognitive Function in Late Middle Age. Journal of Gerontology: Social Science. 2002;57B:S43–51. doi: 10.1093/geronb/57.1.s43. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The Health Benefits of Smoking Cessation. Washington D.C.: U.S. Government Printing Office; 1990. A Report of the Surgeon General. [Google Scholar]
- U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta: 1996. National Center for Chronic Disease Prevention and Health Promotion, Center for Disease Control and Prevention, U.S. Department of Health and Human Services. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010, Understanding and Improving Health. 2nd ed. Vol. 2. Washington D.C.: U.S. Government Printing Office; 2000. [Google Scholar]
- Van Rossum C, Shipley M, Van de Mheen H, Grobbee D, Marmot MG. Employment Grade Differences in Cause Specific Mortality: A 25 Year Follow Up of Civil Servants from the First Whitehall Study. Journal of Epidemiology and Community Health. 2000;54(3):178–84. doi: 10.1136/jech.54.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The Disablement Process. Social Science and Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Waidmann T, Liu K. Disability Trends among the Elderly and Implications for the Future. Journals of Gerontology: Social Sciences. 2000;55B:S298–307. doi: 10.1093/geronb/55.5.s298. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Whincup PH, Shaper G, Walker M. Influence of Fathers' Social Class on Cardiovascular Disease in Middle-Aged Men. Lancet. 1996;348:1259–63. doi: 10.1016/S0140-6736(96)02465-8. [DOI] [PubMed] [Google Scholar]
- Ward MM, Fries JF. Trends in Antirheumatic Medication Use among Patients with Rheumatoid Arthritis, 1981–1996. Journal of Rheumatology. 1998;25(3):408–16. [PubMed] [Google Scholar]
- Weuve J, Kang JH, Manson JE, Breteler MMB, Ware JH, Grodstein F. Physical Activity, Including Walking, and Cognitive Function in Older Women. Journal of the American Medical Association. 2004;292(12):1454–61. doi: 10.1001/jama.292.12.1454. [DOI] [PubMed] [Google Scholar]
- Williams R. Standardized Coefficients in Logistic Regression. 2006. [accessed December 7, 2006]. Available at http://www.nd.edu/~rwilliam/xsoc73994/l06.pdf.
- Winkleby M, Cubbin C, Ahn D. Effect of Cross-Level Interaction between Individual and Neighborhood Socioeconomic Status on Adult Mortality Rates. American Journal of Public Health. 2006;96(12):2145–53. doi: 10.2105/AJPH.2004.060970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf D, Hunt K, Knickman J. Perspectives on the Recent Decline in Disability at Older Ages. The Milbank Quarterly. 2005;83(3):365–95. doi: 10.1111/j.1468-0009.2005.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JM, Carberry T. Bilateral Cataract Surgery and Driving Performance. British Journal of Ophthalmology. 2006;90:1277–80. doi: 10.1136/bjo.2006.096057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Toward a Common Language for Functioning, Disability, and Health, ICF. Geneva: 2002. [Google Scholar]
- Yen IH, Syme SL. The Social Environment and Health: A Discussion of the Epidemiologic Literature. Annual Review of Public Health. 1999;20:287–308. doi: 10.1146/annurev.publhealth.20.1.287. [DOI] [PubMed] [Google Scholar]
- Zimmer Z, House JS. Education, Income, and Functional Limitation Transitions among American Adults: Contrasting Onset and Progression. International Journal of Epidemiology. 2003;32(6):1089–97. doi: 10.1093/ije/dyg254. [DOI] [PubMed] [Google Scholar]


