Abstract
As people continue to age and receive complex health care services at home, concern has arisen about the availability of family caregivers and their ability to combine employment with caregiving. This article evaluates the international research on unpaid caregivers and their labor market choices, highlighting three conclusions: first, caregivers in general are equally as likely to be in the labor force as noncaregivers; second, caregivers are more likely to work fewer hours in the labor market than noncaregivers, particularly if their caring commitments are heavy; and finally, only those heavily involved in caregiving are significantly more likely to withdraw from the labor market than noncaregivers. Policy recommendations are targeting greater access to formal care for “intensive” caregivers and developing workplace policies for employed caregivers.
Keywords: Unpaid caregivers, home care, employment, labor supply
As individuals in societies around the globe age, many policymakers are becoming concerned about future demands on health care systems. Although the extent to which these concerns are warranted is debated (McKnight 2006; Payne et al. 2007; Spillman and Pezzin 2000), demographics show that many countries' populations as a whole are indeed aging (Heitmueller and Inglis 2007; Toosi 2006; Van Houtven and Norton 2004). In the United States, the percentage of the population above the age of sixty-five is projected to rise from the current 12.4 percent to 20 percent by 2030 (U.S. Department of Health and Human Services 2006). In the European Union, this share will rise from 16 percent today to 30 percent by 2050 (Bolin, Lindgren, and Lundborg 2007a). The impact of this aging population on their future use of health services is only one issue facing policymakers. On a different track, policymakers are concerned about securing enough workers to sustain their economies and provide the tax base needed to support large cohorts of retired citizens (Bolin, Lindgren, and Lundborg 2007b; Ettner 1995; Hedge, Borman, and Lammlein 2006; Heitmueller and Inglis 2007; Karoly and Panis 2004; Spillman and Pezzin 2000; Toosi 2006; Wolf 1999).
In health care, perceptions of an impending financial crisis have led to a desire to control public spending. Many countries' method of limiting state spending has been to encourage individuals to age in their own homes, for which the share of publicly financed services is generally lower than in institutional settings, even though the economic burden placed on individuals and their families is much higher (Arno, Levine, and Memmott 1999; Coyte and McKeever 2001; Doty 2000; Lundsgaard 2005; Shireman and Rigler 2004; Stabile, Laporte, and Coyte 2006; Tranmer et al. 2005; Wolf 1999).
Although the home has been the primary health care setting for most of human history, societal shifts during the current demographic changes have complicated the use of the home as a setting for providing cost-effective health care services. First, the number of women, the traditional caregivers for ill family members, in the labor force has increased substantially, raising questions about their willingness and availability to continue caregiving in the future. Second, people are living longer and are remaining in their homes with higher levels of illness and disability than ever before. Consequently, the duration of caregiving has become longer and the role of family caregivers has become more complex, with tasks ranging from changing gastronomy tubes and colostomy bags to providing home chemotherapy (Levine 1999; Yantzi, Rosenberg, and McKeever 2007). Third, the composition of families and households is changing, with fewer coresiding adult children and elderly parents, more single-parent households, and smaller families (Bolin, Lindgren, and Lundborg 2007b; Doty, Jackson, and Crown 1998; Ettner 1995; Heitmueller and Inglis 2007; Jenkins 1997; Johnson and Lo Sasso 2000; McLanahan and Monson 1990; Spillman and Pezzin 2000; Van Houtven and Norton 2004; Wolf, Hunt, and Knickman 2005). Given that many countries' governmental programs are based on the assumption that family members will provide the majority of home care services (Arno, Levine, and Memmott 1999; Bittman et al. 2004; Bolin, Lindgren, and Lundborg 2007b; Carmichael and Charles 1998, 2003a, 2003b; Heitmueller and Inglis 2007; Levine et al. 2006; MacDonald, Phipps, and Lethbridge 2005), securing an adequate supply of family caregivers for the future has been a major priority. Henceforth we shall refer to them as unpaid caregivers, the family members and friends who, on the basis of their close personal relationships, provide home care services to recipients in their private residences without financial compensation (Fast, Eales, and Keating 2001).
Determining the appropriate amount of public investment in formal home care services in order to optimize these unpaid caregivers' service outputs has been the focus of intense research interest. There has been some debate over whether formal (paid) and informal (unpaid) care are substitutes or complements (Muramatsu and Campbell 2002; Muramatsu et al. 2007; Wolf 1999). If they are substitutes, an increase in the generosity of paid home care programs would result in a decrease in the provision of unpaid care. However, if this care is complementary, both types of service provision would act together to improve the overall provision of care, without reducing service levels of the other type. As Charles and Sevak (2005) outlined, the early research evidence was mixed (Muramatsu and Campbell 2002; Tennstedt, Crawford, and McKinlay 1993), but more recent evidence consistently suggests that the two may be partial substitutes, so an increase in formal service provision is associated with fewer hours of care contributed by family members. Similarly, a decrease in formal service provision is associated with an increase in hours of care by family members (Bolin, Lindgren, and Lundborg 2007a; Charles and Sevak 2005; Levine et al. 2006; Spillman and Pezzin 2000; Stabile, Laporte, and Coyte 2006; Van Houtven and Norton 2004; Viitanen 2007).
Assuming that paid and unpaid care are substitutes, some policymakers have suggested that increasing public expenditures on formal home and community care services may erode long-standing informal networks of support (Tennstedt, Crawford, and McKinlay 1993). But such policy positions may be shortsighted in failing to recognize the growing demographic pressures facing our societies. Inducing family members to take up caregiving roles may curtail health care spending in the short term, but what would such policies mean for future labor markets? Specifically, if family members are allocating their time to provide care, what other uses of their time are they giving up? Given that a significant proportion of caregivers in many countries are labor force participants under the age of sixty-five (Arber and Ginn 1995; Doty, Jackson, and Crown 1998; Hawranik and Strain 2000; Heitmueller and Inglis 2007; Henz 2004; Keating et al. 1999; Spillman and Pezzin 2000), the effects of unpaid caregiving could be significant for labor forces and economies in general and could extend beyond the period of direct caregiving.
In this article, we examine the impact of unpaid caregiving on caregivers' labor force participation and on their hours of labor market work. We describe the results of a systematic review of the international literature pertaining to caregivers and their labor market choices, by describing the relationships between unpaid caregiving and three distinct, but related, labor supply questions. First, we consider the impact of caregiving on labor force participation, a binary measure reflecting a person's status as being either “in” or “out” of the labor market. Second, we consider the sociodemographic, health, and labor market factors that influence caregivers' participation in the labor force and the number of hours they work in the labor market. Third, we examine the relationship between the intensity of unpaid caregiving and the intensity of labor market work as measured by the number of weekly hours committed to each. This article synthesizes and compares the results of various studies, identifies trends, and makes both policy recommendations and suggestions for future research.
Theoretical Framework
The labor force participation decision making process undertaken by potential caregivers has already been well described (Heitmueller 2007). Put simply, individuals have a series of choices when faced with caregiving decisions, the first one being whether to accept the caregiving role.1 Their current labor force status and the availability of other family members who may be able to take on caregiving duties may influence this decision. For instance, spouses of care recipients who are employed full-time and are earning relatively high wages may opt not to care but instead to maintain or even increase their labor force commitments in order to buy care services. Similarly, the adult children of the care recipient who are earning high wages may remain in the labor market and opt to forgo their future inheritance in order to allow their parents to buy care services. Conversely, caregivers may self-select from a pool of underemployed or labor force nonparticipants, whose labor market opportunity costs are relatively low and where the risk of losing access to the care recipient's assets, such as their home, may be great. If working individuals decide to take on caregiving responsibilities, they then must decide whether to remain in the labor force and how many hours per week they will devote to unpaid caregiving versus paid employment, as well as other uses of their time (Arber and Ginn 1995; Bolin, Lindgren, and Lundborg 2007b; Carmichael and Charles 1998, 2003a; Ettner 1995, 1996; Johnson and Lo Sasso 2000; Pavalko and Artis 1997; Spiess and Schneider 2003; Stabile, Laporte, and Coyte 2006; Wolf and Soldo 1994).
Methods
The methods we used in this review comply with Long's (2006) recommendations for conducting systematic reviews in the social care arena and also with those of the Evidence for Policy and Practice Information and Coordinating (EPPI) Centre (2007) for conducting systematic reviews in the social sciences. We conducted a literature search in March 2006 to identify articles published in English between 1986 and 2006. Owing to the scarcity of evidence, we chose a publication range of twenty years. To capture all relevant literature from the various disciplines of economics, health services research, social work, gerontology, nursing, and gender studies, we searched thirteen databases, including AgeLine, PsycINFO, EconLit, CINAHL, MEDLINE, and the Gender Studies Database.2 We used the following search terms (and their affiliated truncations): at least one of “family caregiving,” or “informal caregiving,” or “unpaid caregiving,” combined with at least one of “employment,” or “labor supply,” or “labor force.”3 We reviewed eighty-nine abstracts of the 328 citations we retrieved after eliminating all duplicates. We excluded articles from the complete literature review if (1) their titles/abstracts indicated that unpaid caregivers were not the primary focus of the article or (2) they presented no quantitative empirical work on the probability of labor force participation, hours of work, or wages. Forty-two articles were retained for a complete review.
To increase sensitivity and reduce the potential for publication bias (Stanley 2001; Sterne, Egger, and Smith 2001), we performed author and hand searches of the forty-two articles and their bibliographies to identify another ten articles, two working papers (Carmichael et al. 2005; McLanahan and Monson 1990), and two published reports for review (Johnson and Lo Sasso 2000; Keating et al. 1999). Then, following the suggestion of an anonymous reviewer, we identified two more articles. Following a detailed review of all fifty-eight articles, we excluded twenty-three from further analysis for failing to meet our eligibility criteria. Of these, we excluded a small number (n= 4) because the care recipients resided in institutions or because caregiving was defined as “time assistance” to elderly individuals who were not necessarily ill (Dautzenberg et al. 2000; Johnson and Lo Sasso 2000; Kolodinsky and Shirey 2000; Pezzin and Schone 1999).4 We also excluded four articles because of their exclusive focus on subpopulations of caregivers to children with special needs (Brennan and Brannan 2005; Leiter et al. 2004) or patients with mental illness (Cannuscio et al. 2004; Roberts 1999). While these are important and related areas of inquiry, results from these studies cannot be generalized to the majority of people caring for adults with a physical illness and/or disability. In the end, thirty-five articles met our inclusion criteria and are analyzed in this literature review.
General Study Characteristics
With the exception of one multinational European study and one Canadian study, the remaining thirty-three studies analyzed data from either the United States (n= 27) or the United Kingdom (n= 6). Approximately two-thirds of studies (n= 22) focused exclusively on caregiving to the elderly, and a significant minority focused solely on female caregivers (n= 12), caregiving only for family members (n= 8) or labor force participants (n= 11), and 40 percent (n= 14) compared caregivers with noncaregivers or the general population.
Again, unpaid caregivers are defined as family members and friends who provide home care services to recipients without financial compensation. Even though those activities considered as “home care services” vary within and between countries (Muramatsu and Campbell 2002), typical services include those necessary to allow care recipients to remain living in their home and avoid nursing home or long-term care facility admission (Weissert, Cready, and Pawelak 2005). In the studies reviewed here, those services included helping with activities of daily living (ADLs) and instrumental activities of daily living (IADLs) and may have included any of the following: personal care activities such as bathing, dressing, and feeding the care recipient; assisting with toileting, taking medication, and using medical devices; preparing meals and cleaning up; cleaning the house; doing the laundry; maintaining the house; shopping for groceries; taking the care recipient to medical appointments; and helping with paying household bills and banking (Boaz 1996; Levine et al. 2006; Muramatsu and Campbell 2002; Stabile, Laporte, and Coyte 2006; Wolf 1999).
Methodologically, 86 percent (n= 30) of the studies involved secondary data analysis. Thirty-two studies used cross-sectional (n= 25) or longitudinal (n= 7) survey instruments, and the remaining three used experimental or quasi-experimental study designs (Chang and White-Means 1995; Muurinen 1986; White-Means 1993). Despite the common use of surveys in economics (Atkinson and Brandolini 2001), such instruments are difficult to assess for validity and reliability. However, surveys can also offer the advantage of strong statistical power achieved through a large sample size. Most of the surveys discussed here were developed and administered by such government bodies as the U.S. Census Bureau and the United Kingdom's Office of National Statistics, with sample populations greater than one thousand. Two such longitudinal surveys from the United States are of particular importance: the National Long-Term Care Survey (NLTCS) and its accompanying Informal Caregiver Survey (ICS), a national dataset of two thousand caregivers to seniors aged sixty-five and older enrolled in Medicare; and the National Survey of Families and Households (NSFH), a nationally representative survey of 13,000 adults living in private residences (Duke University Center for Demography 2006; University of Wisconsin at Madison 2006). Data from various years of these two surveys were used in 40 percent (n= 14) of the studies we reviewed. Similarly, the United Kingdom's (UK) General Household Survey, a nationally representative cross-sectional survey of more than 13,000 adults, was analyzed in another four articles.
Seven other articles from the United States and all eight from other countries used various other secondary datasets to explore these issues. These studies offer important comparisons with the NLTCS and NSFH studies. The six remaining studies from the United States used primary data collected by study authors and have smaller sample sizes (n= 118 – 293). Finally, almost one-third of the studies were authored by two groups of researchers, one from the United States (White-Means and colleagues, n= 6) and the other from the United Kingdom (Carmichael and Charles, and Carmichael and colleagues, n= 4). For all studies, only those findings with p < 0.05 are referenced as being statistically significant.
Table 1 summarizes the data, methods, and major findings of each study, divided into five sections according to country and data source: (1) U.S. studies analyzing the National Long-Term Care Survey, (2) U.S. studies analyzing the National Survey of Families and Households, (3) U.S. studies using other data, (4) UK studies, and (5) Canadian and European studies.
Table 1.
Study Characteristics
|
Sample Limited to |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Author | Data Source | Study Design | N | Sample Population | Women | Caregivers | Labor Force Participants | Caring for Elderly | Caring for Family |
| 1. U.S. Studies Using the National Long Term Care Survey (NLTCS) and Informal Care Survey (ICS) (n = 10) | |||||||||
| Boaz and Muller 1992 | 1982 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 1,917 | Adults of all ages providing unpaid care for a period of 3+ months to a nationally representative sample of functionally limited (at least 1 ADL/IADL limitation) Medicare-enrolled seniors living at home | ✓ | ✓ | |||
| Boaz 1996 | 1982 and 1989 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 1,489 (1989); 597 (1989) | ICS sample; bivariate analysis considered adults of all ages; regression analysis considered those aged 64 and under | ✓ | ✓ | |||
| Doty, Jackson, and Crown 1998 | 1989 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 818 | ICS sample; bivariate analysis considered both adults of all ages and those aged 18–64; regression analysis considered only women | ✓ | ✓ | |||
| Mutschler 1993 | 1982 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 494 | ICS sample; analysis limited to current or former labor force participants | ✓ | ✓ | ✓ | ||
| Mutschler 1994 | 1982 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 1,059 | ICS sample; analysis limited to current labor force participants | ✓ | ✓ | ✓ | ||
| Stone and Short 1990 | 1982 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 1,003 | ICS sample; analysis limited to children and nonspousal caregivers aged 65 and under | ✓ | ✓ | |||
| White-Means and Thornton 1990 | 1982 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 231 | ICS sample; analysis limited to 4 self-identified ethnic groups (German, Irish, English, and African Americans) | ✓ | ✓ | ✓ | ||
| White-Means 1992 | 1982 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 615 | ICS sample; analysis limited to labor force participants | ✓ | ✓ | ✓ | ||
| White-Means and Chollet 1996 | 1982 and 1989 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 741 | ICS sample; analysis limited to current or former labor force participants | ✓ | ✓ | ✓ | ||
| White-Means 1997 | 1989 NLTCS and ICS | Cross-sectional survey; secondary data analysis | 326 | ICS sample; analysis limited to current or former labor force participants aged 21–65 | ✓ | ✓ | ✓ | ||
| 2. U.S. Studies Using the National Survey of Families and Households (NSFH) (n = 4) | |||||||||
| Ettner 1996 | 1987 NSFH | Cross-sectional survey; secondary data analysis | 6,451 | Nationally representative sample of adults aged 19 and over living in private residences in the U.S.; analysis limited to those with a living parent; caregivers included those who lived with someone who was disabled or chronically ill, or who provided care to someone outside of their home who was seriously ill or disabled | ✓ OAa | ✓ | |||
| McLanahan and Monson 1990 | 1987 NSFH | Cross-sectional survey; secondary data analysis | 10,785 | NSFH sample; analysis limited to those aged 64 and under | |||||
| Wakabayashi and Donato 2005 | 1987 and 1992 NSFH | Longitudinal surveyb; secondary data analysis | 2,638 | NSFH sample; analysis limited to women aged 19–70 who were labor force participants, and who had at least 1 living nonresidential parent, step-parent, or parent-in-law in both survey years | ✓ | ✓ | ✓ OA | ✓ | |
| Wolf and Soldo 1994 | 1987–1988 NSFH | Cross-sectional survey; secondary data analysis | 1,717 | NSFH sample; analysis limited to married women with at least 1 living parent, step-parent, or parent-in-law aged 65 and over | ✓ | ✓ | ✓ | ||
| 3. U.S. Studies Using Other Data (n = 13) | |||||||||
| Barnes, Given, and Given 1995 | Original interviews and self-administered questionnaires | Cross-sectional survey | 118 | Convenience sample of 118 adult daughters/daughters-in-law acting as primary caregivers to 1 dependent community-dwelling elderly parent or parent-in-law | ✓ | ✓ | ✓ | ✓ | |
| Bullock, Crawford, and Tennstedt 2003 | Springfield Elder Project | Cross-sectional survey | 119 | 1,975 noninstitutionalized elderly living in Springfield, Massachusetts; analysis limited to adults of any age acting as caregivers to functionally disabled elderly African Americans living in private households | ✓ | ✓ 60+ | |||
| Chang and White-Means 1995 | 1982–1984 National Long Term Care Channeling Evaluation | Randomized trial; secondary data analysis | 1,926 | Adults of all ages acting as primary caregivers to the frail elderly at risk of hospitalization at 10 sites across the U.S. | ✓ | ✓ | |||
| Covinsky et al. 2001 | 1992–1998 Caregivers of patients enrolled in the Program of All-Inclusive Care for the Elderly (PACE) | Cross-sectional survey; secondary data analysis | 4,592 | Caregivers to frail elderly at risk of institutionalization; 11 of 12 cities across the U.S.; sample limited to labor force participants or those who left their jobs to provide care | ✓ | ✓ | ✓ | ||
| Dentinger and Clarkberg 2002 | 1994–1995 Cornell Retirement and Well-Being Study (CRWB) | Cross-sectional survey; secondary data analysis | 763 | Employees aged 50–72 of 6 large randomly selected employers in upstate New York; caregivers helped relatives or friends who were elderly or disabled; additional caregiving elements considered by this study included checking up by telephone and making care arrangements | ✓ | ||||
| Ettner 1995 | Pooled data from 1986, 1987, and 1988 Survey of Income and Program Participation (SIPP) | Cross-sectional survey; secondary data analysis | 11,486 | Analysis limited to women aged 35–64; among caregiving subsample, analysis limited to those providing personal assistance to parents for a health condition lasting 3+ months | ✓ | ✓ | |||
| Franklin, Ames, and King 1994 | Postacute home care patients in Michigan | Longitudinal survey | 236 | 630 family members of patients discharged from Michigan acute care hospitals; analysis limited to female employed family members acting as primary caregivers to individuals with at least 1 ADL or 2 IADL limitations and living at home | ✓ | ✓ | ✓ | ✓ 55+ | ✓ |
| Moen, Robison, and Fields 1994 | 1956 and 1986 Women's Roles Survey | Longitudinal survey | 293 | Random sample of wives and mothers from a mid-sized community in upstate New York, interviewed in 1956 and again in 1986; caregivers provided assistance to the ill, disabled, and elderly | ✓ | ||||
| Muurinen 1986 | 1980–1983 National Hospice Study (NHS) | Quasi-experimental; secondary data analysis | 1,445 | Adults of all ages acting as primary caregivers to terminally ill cancer patients enrolled in the NHS at multiple sites across the U.S. | ✓ | ||||
| Pavalko and Artis 1997 | 1984 and 1987 National Longitudinal Survey of Mature Women | Longitudinal survey; secondary data analysis | 3,083 | Nationally representative sample of women in the U.S.; analysis limited to those aged 47–64 in 1987; caregivers provided assistance to an ill or disabled family member | ✓ | ||||
| Pohl et al. 1994 | Combined 2 data sets from the midwest U.S. | Cross-sectional survey | 159 | Family caregivers to elderly individuals with at least 1 ADL limitation (n = 536) and to older adults with Alzheimer's disease (n = 229); analysis limited to adult caregiving daughters and daughters-in-law | ✓ | ✓ | ✓ 55+ | ✓ | |
| Pohl, Collins, and Given 1998 | Postacute home care patients in Michigan | Longitudinal survey | 157 | 628 family members of patients discharged from Michigan acute-care hospitals; analysis limited to adult caregiving daughters and daughters-in-law to individuals with at least 1 ADL or 2 IADL limitations and living at home | ✓ | ✓ | ✓ 55+ | ✓ | |
| White-Means 1993 | 1982–1984 National Long Term Care Channeling Evaluation | Randomized trial; secondary data analysis | 454 | Adults of all ages acting as primary caregivers to the frail elderly at risk of institutionalization at 10 sites across the U.S.; analysis limited to 454 African Americans | ✓ | ✓ | |||
| 4. UK Studies (n = 6) | |||||||||
| Arber and Ginn 1995 | 1985 and 1990 General Household Survey (GHS) | Cross-sectional survey; secondary data analysis | 11,879 | Nationally representative sample of adults aged 16 and older living in private households; analysis limited to those aged 20–60; caregivers were regularly caring for someone in a private residence who was sick, handicapped, or elderly | |||||
| Carmichael and Charles 1998 | 1985 GHS | Cross-sectional survey; secondary data analysis | 7,269 | GHS sample; limited to women aged 21–59 | ✓ | ||||
| Carmichael and Charles 2003a | 1990 GHS | Cross-sectional survey; secondary data analysis | 5,463 | GHS sample; limited to women aged 18–59 | ✓ | ||||
| Carmichael and Charles 2003b | 1990 GHS | Cross-sectional survey; secondary data analysis | 10,098 | GHS sample; limited to women aged 18–59 and men aged 18–64 | |||||
| Carmichael et al. 2005 | 1992 and 1999 British Household Panel Survey (BHPS) | Longitudinal survey; secondary data analysis | 7,836 | Nationally representative survey of 10,000 adults living in private households in the UK; analysis limited to working-aged adults; caregivers provided regular service to someone who was sick, disabled, or elderly | |||||
| Henz 2004 | 1994–1995 Family and Working Lives Survey | Cross-sectional survey; secondary data analysis | 1,259 | Nationally representative 2-stage sample of adults aged 16–69 living in private households in the UK; analysis limited to individuals who cared for someone for at least 3 months who was sick, disabled, or elderly | ✓ | ||||
| 5. Canadian and European Studies (n = 2) | |||||||||
| Keating et al. 1999 | 1996 General Social Survey | Cross-sectional survey | 1,366 | Nationally representative sample of 12,000 individuals aged 15 and over living in private households in Canada; labor supply subanalysis limited to adults aged 18–64 providing unpaid care to seniors with a long-term health condition lasting at least 6 months | ✓ | ✓ | |||
| Spiess and Schneider 2003 | 1994 and 1996 waves of the European Community Household Panel | Longitudinal survey; secondary data analysis | 6,390 | Sample of 127,000 adults aged 16 and over living in private residences in 12 European countries; bivariate analysis limited to women aged 45–59; regression analysis further limited to labor force participants; caregivers provided regular assistance to adults who needed special help as a result of old age, illness, or disability | ✓ | ✓ | |||
OA = caregiving to older adults who may not be over 65 years of age; 60+ or 55+ denotes caregiving to adults aged 60+ or 55+.
Longitudinal surveys are considered to be cross-sectional in the study design column if only one wave of data was considered or if multiple years of data were pooled.
Results
Labor Force Participation: Most Caregivers' Labor Force Status Remains Stable
Labor force participants are individuals who are employed or actively seeking employment; otherwise, they are “not in the labor force.” In most countries, labor force participation (LFP) is measured among noninstitutionalized individuals aged sixteen to sixty-four, although the upper age limit is increasing in some jurisdictions in accordance with the repeal of mandatory retirement legislation (U.S. General Accounting Office 2003). The LFP rate represents the percentage of those in the labor force relative to the total working-age population. Examining LFP rates among societal subgroups is a method to gauge social inclusion (Pavis, Hubbard, and Platt 2001). For unpaid caregivers, the LFP rate provides only one indication of their overall economic well-being. The studies' primary measure for labor force participation varied, with some including the unemployed who were seeking work; however, the majority considered only those who were employed or self-employed. Because the unemployed represent a small proportion of the total labor force, the use of one measure versus the other is unlikely to affect our general conclusions.5
Before summarizing findings on caregivers' LFP, we first outline a landmark article that introduces a critical methodological issue. Muurinen (1986) compared the labor market effects of unpaid caregiving by those providing primary care to terminally ill cancer patients in the United States in three care settings (home hospice, institutional hospice, or conventional care). The results showed that caregivers who selected the home hospice option were significantly less likely to be engaged in the labor market at the onset of caregiving (42.8 percent) compared with those who opted for institutional hospices (48.3 percent) or conventional care (51 percent) settings.
As described in the theoretical framework, Muurinen's finding that home-based caregivers were less likely to be employed a priori leads to the question of whether they self-selected into the unpaid caregiving role because they already were outside, or had looser attachment to, the labor force when faced with the initial caregiving decision. Such a possibility suggests that the lower LFP of caregivers versus noncaregivers stems not from caregiving activities but from other unidentified factors systematically influencing caregivers' employment decisions. The possibility that such individuals were less likely to have been employed before becoming caregivers presents a statistical dilemma when testing in cross-sectional data: the endogeneity bias. Endogenous variables are those that are jointly determined and where the distinction between dependent and independent variables may be uncertain (Gujarati 2003). In the case of LFP and caregiving, an individual's LFP may be partially determined by her or his caregiving status, and at the same time, the decision to care may be partially determined by the person's preexisting participation in the labor force. At the heart of the endogeneity problem is whether individuals who undertake caregiving duties differ in some systematic way from noncaregivers with respect to labor supply. In short, could some factors unrelated to caregiving explain their divergent labor market behavior? As several authors (Bolin, Lindgren, and Lundborg 2007b; Doty, Jackson, and Crown 1998; Ettner 1995; Heitmueller 2007; Johnson and Lo Sasso 2000) noted, the failure to test and account for endogeneity can lead to biased and inaccurate results. Because this methodological problem is often overlooked, we will highlight throughout this article the extent to which authors addressed endogeneity.
We now are ready to review the twenty-three studies that presented caregiver LFP rates: fifteen were from the United States (including Muurinen's), six were from the United Kingdom, and one article each was from Canada and elsewhere in Europe. In eight U.S. studies limited to working-age caregivers, LFP rates for females ranged from 34 percent6 among preretirement-age women (Pavalko and Artis 1997) to 68 percent among the daughters and daughters-in-law of elderly care recipients (Pohl, Collins, and Given 1998).7 Most studies, however, presented rates clustered around 50 percent (Barnes, Given, and Given 1995; Doty, Jackson, and Crown 1998; Pohl et al. 1994; Stone and Short 1990; Wolf and Soldo 1994). As expected, the three U.S. studies that included LFP rates for working-age caregiving men reported higher rates, between 57 percent and 77 percent (Doty, Jackson, and Crown 1998; Ettner 1996; Stone and Short 1990).
The wide variation of LFP rates for U.S. caregivers may be partly attributable to age differences between the study samples. On the whole, rates were inversely related to the mean age of caregivers (Barnes, Given, and Given 1995; Bullock, Crawford, and Tennstedt 2003; Doty, Jackson, and Crown 1998; Ettner 1996; Pavalko and Artis 1997; Pohl, Collins, and Given 1998; Pohl et al. 1994). Similarly, the seven remaining U.S. studies that did not exclude retirement-age caregivers found much lower rates, from 25 percent to 34 percent (Boaz 1996; Boaz and Muller 1992; Chang and White-Means 1995; Muurinen 1986; White-Means 1993; White-Means and Chollet 1996), with one upper-limit outlier of 52 percent (Bullock, Crawford, and Tennstedt 2003).
Figure 1 underscores the importance of controlling for age and gender in LFP analysis. Figure 1a shows box plots of the LFP rates of fifteen studies of unpaid caregivers in the United States, before and after excluding studies (n= 7) that did not control for reaching retirement age. Figure 1b is further refined, presenting the LFP rates of caregiving women (n= 8 studies) versus men (n= 3 studies) under sixty-five years of age. It is evident that both age and gender are central factors influencing caregivers' LFP in the United States, and if they are not controlled for in statistical analysis, these variables are likely to confound results.
Figure 1.
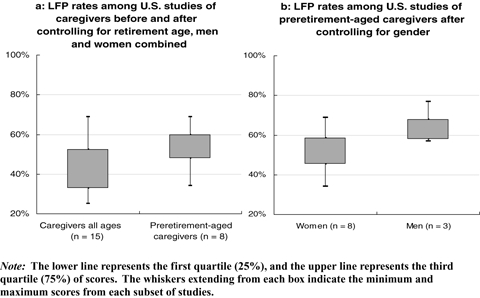
The Interquartile Range for Each Subset of Studies
Study results from the United Kingdom (n= 6) diverged dramatically from those of the United States. LFP rates from UK-based studies were higher across all groups, independent of caregiving status, and the LFP rates for caregiving women were consistently clustered around 64 percent (Arber and Ginn 1995; Carmichael and Charles 2003a, 2003b; Carmichael et al. 2005; Henz 2004). Only one study presented a lower rate, 51 percent (Carmichael and Charles 1998), and it also reported a higher LFP rate for caregivers than for noncaregivers. Rates were also higher for caregiving men in the United Kingdom (n= 4), ranging from 70 percent to 82 percent (Arber and Ginn 1995; Carmichael and Charles 2003b; Carmichael et al. 2005; Henz 2004).
A single multinational study of women in twelve European countries found that only 6 percent of preretirement-age (45 to 59) caregivers were in the labor force, compared with 50 percent of all women in this age cohort (Spiess and Schneider 2003). In contrast, the one Canadian study reported that 62 percent of female caregivers and 78 percent of male caregivers were employed in 1996,8 and the authors found no evidence that caregiver LFP rates were lower than those for the general population (Keating et al. 1999).
The degree to which the differences noted in these twenty-three studies can be attributed to actual variation in caregivers' LFP is unknown. Heterogeneity between studies' inclusion criteria related to age, marital status, care recipient relationship, coresidence, and even the definition of a caregiver all may have contributed to the variation. In addition, macroeconomic factors such as regional and national unemployment rates during the survey years may have been important. In order to provide further context, we performed chi-square analyses of LFP rates for caregivers versus noncaregivers. For four studies that did not provide rates for noncaregivers (Doty, Jackson, and Crown 1998; Henz 2004; Keating et al. 1999; Stone and Short 1990),9 we imputed sex-specific rates from national census and labor market data, matched for the year and original caregiver sample size (Office for National Statistics 2006; Statistics Canada 2001; U.S. Bureau of Labor Statistics 2005). Eleven studies remained after eliminating all articles that (1) included individuals aged sixty-five and older (n= 7), (2) did not state a sample size (Wolf and Soldo 1994), (3) provided neither an LFP rate for noncaregivers nor a data collection year in order to impute a rate (Barnes, Given, and Given 1995; Bullock, Crawford, and Tennstedt 2003; Pohl, Collins, and Given 1998; Pohl et al. 1994), or (4) would have resulted in multiple representations of participants from the same study. Following the Cochrane Collaboration's recommendation (Higgins and Green 2006) to ensure that study participants be counted in a meta-analysis only once, we removed one study (Carmichael and Charles 2003a), as it presented the same subset of data as a broader study by the same authors (Carmichael and Charles 2003b). For a second study (Pavalko and Artis 1997), we included both substudies of a single population and reweighted the frequencies to ensure that the participants received a final weight equivalent to one. While recognizing the debate in the literature surrounding the exclusion and reweighting of such studies (Stanley 2001), the direction and statistical significance of our results remained unchanged when we analyzed the data both with and without these modifications. We weighted the studies by sample size to avoid giving undue influence to very small studies,10 and Table 2 summarizes the results.
Table 2.
Labor Force Participation Rates for Working-Aged Caregivers versus Noncaregivers
| Women |
Men |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Country | Caregivers |
Noncaregivers |
Caregivers |
Noncaregivers |
||||||
| N | % LFP | N | % LFP | N | % LFP | N | % LFP | ||||
| Doty, Jackson, and Crown 1998 | USA | 333 | 52.4 | 333 | 57.4a | ns | 81 | 56.8 | 81 | 76.4a | ** |
| Ettner 1996 | USA | 261 | 64.0 | 3,427 | 65.0 | ns | 134 | 77.0 | 2,629 | 87.0 | *** |
| Pavalko and Artis 1997 | USA | 185b | 29.3 | 1,357 | 43.0 | *** | — | — | — | — | |
| Pavalko and Artis 1997 | USA | 278c | 37.2 | 1,264 | 43.0 | ns | — | — | — | — | |
| Stone and Short 1990 | USA | 752 | 45.7 | 752 | 52.6a | ** | 251 | 58.7 | 251 | 76.7a | *** |
| Arber and Ginn 1995 | UK | 1,204 | 63.0 | 5,037 | 67.8 | ** | 749 | 82.0 | 4,889 | 84.7 | ns |
| Carmichael and Charles 1998 | UK | 977 | 51.3 | 6,292 | 45.0 | *** | — | — | — | — | |
| Carmichael and Charles 2003b | UK | 1,002 | 63.7 | 4,461 | 68.0 | ** | 612 | 81.2 | 4,023 | 85.6 | ** |
| Carmichael et al. 2005 | UK | 1,428 | 63.9 | 2,727 | 71.7 | *** | 1,025 | 72.3 | 2,656 | 86.0 | *** |
| Henz 2004 | UK | 841 | 64.2 | 841 | 53.6a | *** | 332 | 69.6 | 332 | 67.0a | ns |
| Keating et al. 1999 | Canada | 833 | 62.1 | 833 | 58.6a | ns | 533 | 77.9 | 533 | 72.7a | * |
| Spiess and Schneider 2003 | Europe | 1,150 | 6.0 | 5,240 | 50.0 | *** | — | — | — | — | |
| Weighted total | 9,244 | 51.7 | 32,563 | 57.5 | *** | 3,717 | 75.2 | 15,394 | 84.6 | *** | |
| Weighted subtotal USA | 1,809 | 46.6 | 7,133 | 55.3 | *** | 466 | 63.7 | 2,961 | 85.8 | *** | |
| Weighted subtotal UK | 5,452 | 61.4 | 19,358 | 60.4 | ns | 2,718 | 76.6 | 11,900 | 84.8 | *** | |
Sex-specific rates for noncaregivers imputed from national census/labor market data, matched for the year and caregiver's sample size.
Subsample of coresident caregivers.
Subsample of extraresident caregivers.
p < 0.05.
p < 0.01.
p < 0.001.
ns = not significant.
When we considered all eleven studies together, we found that caregivers were significantly less likely to participate in the labor force compared with noncaregivers (p < 0.001). The mean weighted female caregiver LFP rate was 52 percent, compared with 58 percent for noncaregivers, and the male rate was 75 percent, versus 85 percent for noncaregivers. However, countries' overall labor market trends differ systematically, and our results also suggest systematic differences between the United States and United Kingdom.
In the United States, both male and female caregivers overall had significantly lower LFP rates compared with noncaregivers (p < 0.001). However, when we considered the studies separately, three demonstrated no significant difference between the LFP rates of female caregivers versus those of noncaregivers (Doty, Jackson, and Crown 1998; Ettner 1996; Pavalko and Artis 1997).11
In the United Kingdom, only male caregivers were significantly less likely to be employed compared with male noncaregivers (p < 0.001). Among UK women there was no statistical difference between the weighted LFP rates for caregivers versus those for noncaregivers. Furthermore, when we considered the studies separately, half revealed that caregiving men were not significantly less likely to be employed compared with noncaregivers (Arber and Ginn 1995; Henz 2004), and two studies demonstrated that caregiving women were significantly more likely to be employed than noncaregivers (Carmichael and Charles 1998) or the general population (Henz 2004).
Although the overall chi-square results suggest that caregiving may have a large and negative effect on labor force participation, other factors influencing LFP have not been considered. Thus a simple bivariate analysis may be methodologically inadequate. In addition to age and gender, a number of other variables are likely to influence LFP as well. Indeed, based on the ten studies (five U.S. and five UK) that controlled for a variety of such factors in multivariate analysis, few conclusions can be drawn. Only one reported that caregiving had an overall negative effect on women's LFP (Pavalko and Artis 1997); two reported that caregiving had no significant effect on LFP (McLanahan and Monson 1990; Wolf and Soldo 1994); and five found that subpopulations of caregivers were negatively impacted (Arber and Ginn 1995; Carmichael and Charles 2003a, 2003b; Carmichael et al. 2005; Ettner 1995). Finally, two articles reported that some groups of caregivers were significantly more likely to be in the labor force compared with noncaregivers (Carmichael and Charles 1998; Dentinger and Clarkberg 2002). Next we briefly describe these findings.
First, Pavalko and Artis (1997) were the only authors to conclude that caregiving generally had a negative effect on women's LFP and was likely to accelerate the early retirement of U.S. women aged forty-seven to sixty-four. In contrast, two other U.S. studies (McLanahan and Monson 1990; Wolf and Soldo 1994) that used 1987 NSFH data and controlled for possible confounders did not find that caregivers on the whole were less likely to be employed than noncaregivers (note that Wolf and Soldo's study was limited to women).
Five articles (one U.S. and four UK) reported that subpopulations of caregivers experienced declining LFP. Three studies reported that coresidence with the care recipient was associated with lower caregiver LFP (Arber and Ginn 1995; Carmichael and Charles 2003b; Ettner 1995).12 Similarly, three articles found that the provision of more than ten hours of care per week resulted in lower LFP, regardless of living arrangements (Carmichael and Charles 2003a, 2003b; Ettner 1995), although Arber and Ginn (1995) found the labor force exit threshold to be ten hours for men but twenty hours for women. Interestingly, Carmichael and Charles (2003a, 2003b) found that women providing fewer than ten hours of care per week were significantly more likely to be employed than noncaregivers. Since 60 percent of the caregivers in their sample provided fewer than ten hours of care per week, the net effect on LFP would have been positive. Longitudinal analyses by Carmichael and colleagues (2005) found that only new female caregivers in the United Kingdom were less likely to be employed than noncaregivers. However, women who had already been caregiving for some time were no less likely to be employed than noncaregivers, unless they were providing more than twenty hours of care each week. The opposite effect was revealed for men: those who had been giving care for some time were less likely to be working than noncaregivers, although new caregivers were not less likely to be employed than noncaregivers.
Finally, two studies found that caregiving had a positive effect on LFP. In exploring retirement timing among caregivers in the United States, Dentinger and Clarkberg (2002) found that caregiving men were significantly less likely to retire than noncaregiving men (caregiving was not a significant predictor of women's retirement timing unless they were caring for spouses or for more than one person, in which case caregiving women were much more likely to retire than noncaregivers).13 Similarly, Carmichael and Charles (1998) found that caregiving women in the United Kingdom were 10 percent more likely to be in the labor force than noncaregivers.
We began our analysis of caregiver LFP by analyzing the rates from twenty-three studies. Together with the chi-square analysis, the results seem to suggest that caregivers have a much lower LFP compared with that of the general population, with the possible exception of women in the United Kingdom. However, a number of these studies did not control for factors that may have influenced the caregivers' LFP, particularly age. Of the ten studies that controlled for such variables, only one concluded that caregivers generally had lower LFP rates than noncaregivers. Thus, on the whole, caregivers do not seem less likely to be employed than noncaregivers. Instead, those who coreside with care recipients or who report heavy caregiving commitments appear to be much less likely to be in the labor force. It would seem then that policy supports related to caregiver labor force participation should not target caregivers in general but perhaps instead should be targeted at this “intensive” caregiving subset. We discuss this later.
In no way are we suggesting that there is no relationship between caregiving and employment. Instead, the absolute (binary) measure of LFP may be too crude: labor force participants include everyone from occasional workers providing only a few hours to the labor market each week to those providing more than seventy hours. Caregivers may be making more subtle changes in their working lives that cannot be captured by the LFP measure, such as keeping their jobs but reducing their hours. Thus, further analysis is necessary to reveal the true labor market costs borne by this group.
Sociodemographic and Health Factors Influencing Caregivers' LFP and Labor Market Hours
The preceding analysis demonstrates that age and gender are central factors influencing caregivers' LFP, and we now examine what other characteristics may affect their employment and work adjustments. Work adjustments include such changes as taking unpaid leave, reducing hours or changing work schedules, or leaving the labor force because of caregiving (White-Means 1997; White-Means and Thornton 1990). In total, eighteen studies (fifteen U.S., two UK, and one Canadian) examined such variables. Together, they suggest that caregivers with the following characteristics were more likely to be out of the labor force, to work fewer hours in the labor market, or to adjust their work schedules to accommodate their caregiving responsibilities:
Women (Arber and Ginn 1995; Boaz 1996; Boaz and Muller 1992; Chang and White-Means 1995; Covinsky et al. 2001; Henz 2004; Mutschler 1993; Stone and Short 1990; White-Means 1992; White-Means and Thornton 1990).
Those in poor health (Bullock, Crawford, and Tennstedt 2003; Chang and White-Means 1995; Stone and Short 1990; White-Means 1992; White-Means and Chollet 1996; White-Means and Thornton 1990).
Older caregivers and those nearing retirement age (Bullock, Crawford, and Tennstedt 2003; Covinsky et al. 2001; Dentinger and Clarkberg 2002; Henz 2004; Pohl et al. 1994; Spiess and Schneider 2003; Stone and Short 1990; White-Means and Chollet 1996), although one study found that older caregivers who were still in the labor force were less likely to make accommodations (White-Means 1997).
Those more involved in caregiving duties (Barnes, Given, and Given 1995; Dentinger and Clarkberg 2002; Pohl et al. 1994), primary caregivers (Stone and Short 1990), and those without caregiver substitutes (Bullock, Crawford, and Tennstedt 2003; Chang and White-Means 1995; Covinsky et al. 2001; White-Means 1992; White-Means and Chollet 1996).
Immediate family members of care recipients (Arber and Ginn 1995; Keating et al. 1999; White-Means 1992, 1997; White-Means and Chollet 1996), although one study found that daughters and daughters-in-law were more likely to accommodate than were sons and sons-in-law (Covinsky et al. 2001), and another study found that close relatives were less likely to make work accommodations (Chang and White-Means 1995).
Caregivers to persons with greater ADLs or health limitations (Covinsky et al. 2001; Doty, Jackson, and Crown 1998; Keating et al. 1999; White-Means 1992; White-Means and Chollet 1996; White-Means and Thornton 1990), although one study found no significant association (White-Means 1997).
Those with young children at home (Keating et al. 1999; Mutschler 1993; White-Means and Thornton 1990). Boaz and Muller (1992) and Chang and White-Means (1995) found that these caregivers were less likely to make accommodations than were those without young children. Both studies, however, kept persons over the age of sixty-five in their samples, possibly creating a bias resulting in insufficient power to detect an effect.
Those with lower incomes (Mutschler 1993; Pohl et al. 1994; White-Means 1992; White-Means and Chollet 1996), although one study found that caregivers earning higher incomes were likely to work fewer hours (Chang and White-Means 1995) compared with caregivers earning lower incomes.
Those with less education (Boaz 1996; Boaz and Muller 1992; Chang and White-Means 1995; Pohl et al. 1994; Stone and Short 1990), although two studies suggested the opposite, possibly indicating the greater job flexibility experienced by better-educated people (Keating et al. 1999; White-Means and Chollet 1996).
Two additional points with contradictory findings are noteworthy as well. First, more than half the articles addressing living arrangements found that caregivers coresiding with care recipients were more likely than other caregivers to be out of the labor force, to work fewer hours in the labor market, or to make work accommodations (Arber and Ginn 1995; Carmichael and Charles 2003b; Chang and White-Means 1995; Covinsky et al. 2001; Ettner 1995). Dentinger and Clarkberg (2002), however, found no statistically significant effect related to coresidence, and White-Means (1997) and White-Means and Thornton (1990) found that coresident caregivers were less likely to make work accommodations than extraresident caregivers. Because coresidence could have a number of conflicting effects on caregivers' time and income (Carmichael and Charles 2003b), further research is recommended.
Second, White-Means and colleagues in the United States and Carmichael and Charles in the United Kingdom consistently found that caregivers to those receiving state-provided subsidies were less attached to the labor force than were caregivers to those who received no subsidies. In the United States, caregivers to those receiving Medicaid were more likely to be out of the labor force or to work fewer hours in the labor market than were caregivers of nonrecipients (White-Means 1992; White-Means and Chollet 1996; White-Means and Thornton 1990[significant at p < 0.1]). In the United Kingdom, female caregivers to those receiving Attendance Allowance (provided to care recipients who meet strict eligibility criteria related to dependence) were significantly less likely to be employed compared with the caregivers of nonrecipients, but there was no significant effect for male caregivers (Carmichael and Charles 2003a, 2003b). It is uncertain whether these findings can be attributed to caregivers' rising nonwage income, which reduced their need to be employed, whether the original variables were merely proxy indicators for the care recipient's greater need for care that required caregivers to leave the labor force in order to provide adequate care, or whether such caregivers were less likely to be employed a priori.
Overall, the findings of these eighteen studies suggest that caregivers facing the highest opportunity costs are the least likely to leave the labor force; in other words, those with the most to lose by leaving the labor force are the most likely to remain employed. This point highlights the major shortcoming of this group of studies, which is that all but two (Arber and Ginn 1995; Dentinger and Clarkberg 2002) focused exclusively on caregivers. A comparison with the general population would have revealed similar results. Men, persons with higher wage rates, and those with more education tend to have the strongest attachments to the labor force. Meanwhile, women, persons with young children at home, those in poor health, and those approaching retirement age tend to have weaker attachments to the labor force.
As expected, our analysis of eleven studies (six U.S., four UK, and one European) that included both caregivers and noncaregivers demonstrates that regardless of their caregiving status, individuals were less likely to be in the labor force and more likely to make work accommodations if they were older (Carmichael and Charles 1998, 2003a, 2003b; Carmichael et al. 2005; Dentinger and Clarkberg 2002; Ettner 1996; McLanahan and Monson 1990; Pavalko and Artis 1997; Wakabayashi and Donato 2005), if they had less education or work experience (Carmichael and Charles 2003b; Ettner 1996; McLanahan and Monson 1990; Pavalko and Artis 1997; Spiess and Schneider 2003; Wakabayashi and Donato 2005), or if they were in poor health themselves (Dentinger and Clarkberg 2002; Pavalko and Artis 1997; Spiess and Schneider 2003). Women were more likely to make work accommodations if they had young children at home (Carmichael and Charles 1998, 2003a, 2003b; Carmichael et al. 2005; Ettner 1996; McLanahan and Monson 1990; Wakabayashi and Donato 2005; Wolf and Soldo 1994). Carmichael and Charles (1998, 2003a, 2003b) were the only researchers to find the expected result that higher wages increased LFP but that greater sources of nonwage income (including public subsidies to care recipients with female caregivers) lowered LFP (2003a, 2003b).
Our finding that the factors most likely to influence caregivers' employment are not specific to caregivers but instead are consistent with a general model of labor supply underscores the importance of controlling for such factors to avoid overstating the importance of caregiving. The extent to which these variables may interact with caregiving to compound negative labor market effects has not been well measured, with two notable exceptions (Dentinger and Clarkberg 2002; Pavalko and Artis 1997), related to the interaction between caregiving and age on retirement timing. We also found that some characteristics specific to caregivers exaggerate the negative labor market effects within the cohort of caregivers. These include being the primary caregiver and/or having heavier caregiver commitments, being closely related to or coresiding with the care recipient, and the care recipient's increasing health limitations.
Labor Market Factors Influencing Caregiver Employment
Until this point, we have described individual characteristics that influence caregivers' employment decisions. In order to address the possible endogeneity bias related to the caregiving-LFP decisions, we also must identify labor market characteristics that might predict who is most likely to be a caregiver. Five studies addressed such factors (three U.S. and two UK).
Mutschler's 1994 occupational analysis of work adaptations by employed caregivers in the NLTCS database found that caregivers in the United States were less likely to be in managerial or professional occupations and more likely to be in service occupations, compared with the general population of employed Americans. Combined with the findings from her previous research (Mutschler 1993), which demonstrated that service employees work fewer hours per week than do those in other occupational categories (for both caregivers and those in the labor force generally), Mutschler's results may indicate that caregiving and LFP are endogenous.
In contrast, Moen, Robison, and Fields (1994) used longitudinal data from the Women's Roles Survey spanning thirty years to explore caregiving women's LFP in the United States and found that women were just as likely to combine work with caregiving as they were to be engaged in only one activity. They also found that employed women were as likely as women who were out of the labor force to assume caregiving roles, suggesting that previous employment status was a poor indicator of the likelihood of becoming a caregiver.
Similarly, Pavalko and Artis's (1997) longitudinal study of three thousand U.S. women approaching their retirement years also refutes the notion that women with weaker labor force attachment self-select into the caregiving role. Multivariate regression models predicting which women might become caregivers indicated that prior employment status (not employed, employed part-time, and employed full-time) had no effect on the likelihood of undertaking caregiving roles. That is, employed women were as likely to become caregivers as were women who were not employed, and full-time employees were as likely to become caregivers as part-timers.
Finally, results from two UK studies again provide support for the endogeneity hypothesis. Henz (2004) performed logit regression on data from 502 employed women, which demonstrated that only women already working part-time before having to make the caregiving decision were likely to further reduce their work hours after becoming caregivers. Carmichael and colleagues (2005) analyzed the 1992 and 1999 British Household Panel Survey and performed logit regression to predict which persons were most likely to become caregivers between survey years. They found that being older, female, not working or working fewer weekly hours in the labor force, and earning a lower wage all were predictors of becoming a caregiver. Conversely, persons who were employed full-time and earning higher wages were less likely to become caregivers.
Given the level of disagreement between studies regarding the influence of preexisting employment status on the likelihood of becoming a caregiver, we concluded that the extent of the potential for endogeneity bias remains uncertain. Two recent papers from the United Kingdom and Europe (Bolin, Lindgren, and Lundborg 2007b; Heitmueller 2007),14 which fall outside the eligibility criteria for this review, address the endogeneity issue specifically and are worthy of mention. In models in which the use of instrumental variables was found to be valid, neither study found evidence that caregiving was endogenous to LFP, suggesting that perhaps it is exogenous.15 Nevertheless, further longitudinal analysis that allows researchers to examine the timing of caregiving and employment decisions in relation to each other (Johnson and Lo Sasso 2000) is recommended.
Caregiving's Impact on Hours of Labor Market Work
The previous two sections suggest that on the whole, caregivers are no less likely to be employed than are otherwise similar noncaregivers and that many of the characteristics identified as negatively influencing caregivers' employment have similar effects on noncaregivers. However, because those people who have more caregiving commitments (measured by weekly hours of caregiving, primary caregiver status, lack of caregiver substitutes, care recipient's increasing need, and number of care recipients) are less likely to be in the labor market than other caregivers, it is worthwhile to examine the relationship between the intensity of caregiving and the number of hours spent in labor force work among labor force participants. Fifteen articles addressed this issue (twelve U.S., two UK, and one European).
Three of six studies found a relationship between caregiving generally and the number of hours of labor market work. In the United States, Mutschler (1993) found that each additional hour of weekly caregiving work was associated with six fewer hours of weekly labor market work. McLanahan and Monson (1990) also found that U.S. women caregivers worked two to four fewer hours per week than noncaregivers. Among men, only those caring for a spouse were likely to work fewer hours in the labor market (by 3.2 hours per week). In the United Kingdom, Carmichael and Charles (1998) found that female caregivers supplied two fewer hours to the labor market per week than noncaregivers.
In contrast, Boaz (1996) and Boaz and Muller (1992) found that an increase in caregiving commitment was associated with a drop in the likelihood of full-time employment by only 0.3 percent and had no significant relationship to the probability of part-time employment among U.S. caregivers aged sixty-four and younger. Wolf and Soldo (1994) also found that caregiving had no significant relationship to U.S. women's hours of labor force work.
Other studies found that the number of labor market hours changed only for subsets of caregivers. Similar to findings that heavily committed caregivers were less likely than noncaregivers to be in the labor force, Ettner (1995) found that for U.S. women, providing more than ten hours of care per week resulted in reductions of approximately four labor market hours per week. In addition, employed women who coresided with their elderly parents also lost between 2.3 and 7 hours of labor market work weekly.16 But in 1996, Ettner reported that only the labor market hours of caregiving women not residing with the care recipient were significantly lower than those of noncaregiving women. Given the similarly conflicting results related to coresidence described in previous sections, the overall importance of caregiver-care recipient living arrangements on caregivers' labor supply remains uncertain.
Two longitudinal studies also found that caregivers adjusted their labor market hours shortly after becoming caregivers, rather than over a period of many years. Wakabayashi and Donato (2005) found that only those women who had been caregivers for less than five years were likely to reduce their hours significantly (by two per week) compared with noncaregiving women. Women who stopped caregiving or who had been caregiving for more than five years were no more likely to reduce their work hours than noncaregivers. Similarly, Spiess and Schneider's (2003) multinational European study of older women found that caregivers who had been caregiving for less than two years or who had increased their caregiving commitments reduced their weekly employment hours by 2.4 and 5 compared with those of noncaregivers. Reducing, stopping, or maintaining the same levels of caregiving, however, were unlikely to result in significant changes in employment hours compared with those of noncaregivers.
To summarize, the studies we reviewed indicate that caregiving is associated with a moderate reduction in the number of labor market hours, but the magnitude of this effect varies from almost negligible (Boaz 1996; Boaz and Muller 1992) to six fewer hours of labor market work per week for each additional hour of caregiving (Mutschler 1993). Combined with the findings from the previous sections, we concluded that there is an inverse relationship between intensity of caregiving and hours of labor market work. A small literature on the existence of a threshold effect suggests that individuals can balance their employment, caregiving, and other life responsibilities when their caregiving commitments are not heavy but that caregiving for more than ten hours per week has serious negative consequences for both LFP and hours of labor force work, particularly for women (Arber and Ginn 1995; Carmichael and Charles 2003a, 2003b; Ettner 1995).
Other Findings and Future Research
In pursuit of our three primary research questions, we now look at additional subfindings and areas in need of further research.
Labor Force Adjustments within the Caregiving Trajectory
Studies of caregiving women suggest that labor force adjustments are made during the first three months of caregiving and then remain fairly stable thereafter (Carmichael et al. 2005; Franklin, Ames, and King 1994; Pohl, Collins, and Given 1998; Wakabayashi and Donato 2005). However, these results may be specific to women, as the only study to address these issues among men reported the opposite result. Carmichael and colleagues (2005) found that new caregiving men in the United Kingdom were not likely to leave the labor force or reduce their hours; however, men who had been caregiving for a number of years were much less likely to be employed compared with noncaregivers.
The long-term impact of these early labor market interruptions is less certain for female caregivers and has not yet been addressed for male caregivers. The evidence regarding women suggests that once caregivers reduce their labor force commitments, they are unlikely to return to previous levels even after their caregiving responsibilities end (Henz 2004; Pavalko and Artis 1997; Pohl, Collins, and Given 1998; Spiess and Schneider 2003; Wakabayashi and Donato 2005). Further research into the long-term effects of caregiving for both women and men may offer important new insights into the lifelong employment costs of caregiving.
Whether Employment Offers Respite from Caregiving
Carmichael and Charles (1998, 2003a) suggest that some caregivers remain in the labor force to gain respite from caregiving responsibilities. There is some limited evidence supporting this hypothesis. Stone and Short (1990) found that caregivers of those with behavioral problems and dementia were 17 percent more likely to be employed than other caregivers. Henz (2004), Pavalko and Artis (1997), and Pohl, Collins, and Given (1998) also found that a significant minority of caregivers (from 8 percent to 33 percent) increased their labor market hours during the caregiving period. It also is possible that labor force participation offers respite only when caregiving responsibilities are manageable but then becomes a double burden when caregiving duties grow heavier (Carmichael and Charles 2003a). The study by Pohl, Collins, and Given (1998) and other qualitative studies in the broader literature found as well that employment provides respite from caregiving duties, offering positive mental, social, and emotional benefits (Hawranik and Strain 2000; Yantzi, Rosenberg, and McKeever 2007).
The Importance of Gender Analysis
One-third of the studies in this review focused exclusively on women (Spitze and Logan 1991). While we support the conclusion that caregiving women are more negatively affected in the labor force than men, research that excludes men from analyses overlooks the extent to which caregivers' involvement in the labor force is a complex gender issue. Although women comprise the majority of caregivers, overall, fewer women than men are employed and women spend fewer hours in the labor force and earn lower wages than men. Failure to control for these issues by studying both women and men may lead to the inappropriate attribution of labor market effects to unpaid caregiving and neglects the long history of gender inequality in the labor market more generally (Carmichael et al. 2005). In addition, more and more men are becoming caregivers, and the limited evidence presented here indicates that caregiving may affect their labor force participation and hours of labor market work as well.
More Research Needed on Caregivers' Wages and Earnings
There is insufficient research on the impact of caregiving on wages and earnings. In the United States, Wakabayashi and Donato (2005) found that caregiving had no significant effect on women's annual earnings, except among caregivers, who lost an average of $750 annually relative to noncaregivers. Subgroups of these caregivers had more pronounced earnings losses as a result of working fewer hours. In the United Kingdom, Carmichael and Charles (1998, 2003a, 2003b) found that on the whole, caregiving women's wages were 4 to 10 percent lower than noncaregivers' wages, holding other variables constant. They further found (2003a, 2003b) that caregivers who provided more than ten hours of care per week received wages that were between 10 percent (for women) and 18 percent (for men) lower than those of similar noncaregivers. These researchers concluded that caregiving responsibilities depressed individuals' earning power by limiting their job opportunities, particularly for men (2003b). Results from Carmichael and colleagues (2005) were less conclusive, suggesting that caregiving had no impact on women's earnings and lowered caregiving men's earnings in only one of two survey years. Regarding the endogeneity problem, results from this same 2005 study suggest that those receiving lower wages were more likely to become caregivers a priori. Finally, in a recent study beyond the scope of this review, Heitmueller and Inglis (2007) found that after controlling for confounders, caregivers earned approximately 3 percent less than noncaregivers. Further research is needed in this area.
The Unknown Impacts of Ethnicity and Immigration
The experience of caregivers who are recent immigrants or from ethnic minorities is not well understood in the home and community care literature generally, and in the caregiver employment subliterature specifically. In addition, immigrants and individuals from ethnic minorities face unique labor market barriers that make research in this area important. We next briefly summarize the results of the studies from the United States that compared ethnic groups (none considered immigration). Note that many of these findings are based on large surveys of individuals who spoke English (Pohl, Collins, and Given 1998) and who self-identified as belonging to a predefined list of ethnic groups. A large literature exists on the questionable validity and reliability of the findings based on such surveys (Bhopal and Donaldson 1998; Pfeffer 1998; Winker 2004).
Two studies found that black (White-Means and Chollet 1996), African American, and Hispanic caregivers (Covinsky et al. 2001) were less likely to be in the labor force and more likely to work fewer hours in the labor force than white caregivers. Conversely, another two studies found that white caregivers were more likely than nonwhites to make work accommodations, to leave the labor force, or to reduce their hours of work (Mutschler 1993; Stone and Short 1990). Three studies found no statistically significant relationship between ethnicity and LFP (Chang and White-Means 1995; White-Means and Thornton 1990). Of the two studies that included noncaregivers as well, one researcher (Ettner 1996) found that black and Asian men were more likely to work fewer hours in the labor market, regardless of their caregiving status, but neither study reported significant findings for women (Ettner 1996; McLanahan and Monson 1990). Together, these findings offer little insight into the roles that ethnicity and immigration may play in the labor market decisions of caregivers, so further research is required.
Interaction between Unpaid Caregiver Employment and Use of Paid Caregiving Services
An area in need of analysis is the relationship between the use of paid (formal) home care services and unpaid caregiver employment. Four articles from the United States addressed these issues. Doty, Jackson, and Crown (1998) found evidence that unpaid caregivers in the labor force substituted their own caregiving labor with that of others, both paid and unpaid. Although female primary caregivers in the labor force provided 6.7 fewer hours of care per week than did caregivers who were out of the labor force, these missing hours were substituted with 5.3 hours of labor by other unpaid or paid caregivers, resulting in an overall deficit of only 1.4 hours per week for these care recipients. Covinsky and colleagues (2001) found, however, that caregivers of patients who used formal home care services were more likely to reduce their labor market hours than were those who did not receive formal services, suggesting instead that unpaid caregiving may complement formal service provision and that higher levels of both types of care may simply reflect the care recipient's increasing care needs. Finally, two other studies found no relationship between the use of formal services by care recipients and caregivers' LFP (Bullock, Crawford, and Tennstedt 2003; White-Means 1997).
The receipt of public subsidies by care recipients also has been demonstrated to influence caregivers' employment. As previously described, five articles from the United States and United Kingdom found that state-funded subsidies (such as Medicaid and Attendance Allowance) to care recipients were associated with caregivers' lower labor force commitments (White-Means 1992; White-Means and Chollet 1996; White-Means and Thornton 1990), particularly among women (Carmichael and Charles 2003a, 2003b). These findings also warrant further investigation.
Finally, in order to adequately address potential endogeneity bias, it is important to capture formal service use by persons who, when faced with the decision to become unpaid caregivers, opt not to become caregivers and instead maintain or even increase their labor market commitments in order to purchase formal home care services. We are aware of no literature that has successfully identified such individuals. Thus, the research methods used to date to address caregiver labor market choices may have inadvertently given preference to persons induced to leave the labor market, by failing to capture those more strongly induced to increase their labor market attachments. This oversight on the research agenda indirectly sends the value-laden message that only individuals who leave their jobs to care are worthy of public support, and may also underestimate the overall societal burden of home care. In this context, it would be particularly important to understand the relationship between caregivers' labor force participation, labor force hours, and nursing home admission for care recipients with severe ADL/IADL restrictions. Care responsibilities for these people may be so heavy that the majority of potential caregivers opt to admit the care recipient to a nursing home rather than providing the care themselves.
Study Limitations
The relevance of this literature review on these issues must be placed within the context of the original studies. The studies we reviewed came predominantly from the United States and United Kingdom, both of which have unique labor markets and community care environments that may have affected our results. In addition, few studies have been published in the last five years, despite the continuing proliferation of home care and the ongoing reliance on unpaid caregivers as the backbone of community care policies internationally. Thus, future research should be based on new data and data from other international jurisdictions.
Policy Implications
This review found that after controlling for sociodemographic variables and accounting for potential endogeneity, unpaid caregivers are equally as likely to be employed as noncaregivers. It would seem that both caregiving and labor force participation can be maintained when caregiving responsibilities are relatively small, as they are for the majority of unpaid caregivers. But when caregiving duties become heavy, caregivers are significantly less likely than noncaregivers to be employed. We also found substantial evidence that unpaid caregivers commit fewer hours to the labor market than do noncaregivers even when their caregiving responsibilities are small, but particularly if their caring commitments exceed ten hours per week. In addition, we found conflicting evidence regarding whether precaregiving employment status predicts who will become a caregiver, making the importance of the endogeneity bias uncertain. Without more longitudinal research to better understand the timing of caregiving and employment decisions in relation to each other, it remains uncertain whether there are systematic differences between caregivers and noncaregivers that might explain their divergent employment patterns.
Placing these findings in the greater context of demographic change and international labor markets raises a number of policy issues. There are clear trade-offs between the desire to limit health spending by continuing to rely on unpaid caregivers, and the need to achieve an adequate labor force for the future (Bolin, Lindgren, and Lundborg 2007b; Heitmueller and Inglis 2007). This review demonstrated that unpaid caregiving activities have an impact on labor force participation. Despite the relatively high unemployment in some member countries such as France and Spain, the European Union has made greater labor force participation a strong policy mandate and has been trying to improve historically underemployed groups' access to the labor force. Canada and the United States have not been as active, even though North America has lower unemployment but is facing demographic pressures similar to those in Europe.
In countries where encouraging maximum labor force participation is a priority, increasing access to formal care services may be warranted (Bolin, Lindgren, and Lundborg 2007b; Heitmueller and Inglis 2007). In particular, programs could be targeted to caregivers with very heavy caring commitments, who comprise the majority of those who withdraw from the labor force or greatly reduce their weekly hours of labor market work. Furthermore, state policies to provide access to formal care cannot be premised on the lack of availability of family caregivers, as this unfairly locks available family members into caregiving roles (Muramatsu et al. 2007) and gives disproportionate access to formal care to individuals without families. In addition, formal services should be flexible and meet the needs of care recipients and their caregivers. Several recent studies document the extent to which state-supported services in the United States and Canada fail to meet the needs of unpaid caregivers, offering inflexible hours for home care visits and respite and often sending paid caregivers who are not qualified to carry out the necessary health care tasks (Levine 1999; Wiles 2003; Yantzi, Rosenberg, and McKeever 2007). These programs contrast greatly with the flexible and user-friendly services offered in countries such as the United Kingdom and Australia, where the caregiver agenda has gained significant public attention.
Increasing access to formal care services depends on the availability of a large supply of personal assistance workers in the coming decades. In the United States, the job categories of personal assistance worker and home care aide are among the fifteen fastest growing occupations through 2010 (Karoly and Panis 2004), and the country already is experiencing a major shortage of these workers owing to the poor working conditions, low wages, and poor benefits typically associated with these jobs (Kaye et al. 2006; Stone 2004). Large-scale increases in the recruitment and training of new workers will be necessary to meet future demand.
Some countries may be less interested in expanding their labor market supply than in limiting health expenditures. Making state-supported payments to care recipients and their caregivers is one much discussed strategy to balance health spending with the increased demand for services and has been tested to varying degrees in different countries (Lundsgaard 2005). Essentially, care recipients who meet predefined criteria related to disability level and income are given cash payments to spend as they wish on care provision. They can hire agency workers and relieve their unpaid caregivers of caring duties, enabling caregivers instead to engage fully in the labor market. Alternatively, care recipients can use the payments to compensate their unpaid caregivers, who can then leave the labor market. Some schemes even allow caregivers to do both, to remain employed and to keep the payment to provide care themselves (Lundsgaard 2005). Programs in the United States have been favorably evaluated by caregivers and care recipients alike (Dale et al. 2005).
From a labor economics perspective, these self-directed care programs can also be efficient. Theory suggests that individuals with high labor market wages will opt to remain in the labor force and use the funds to purchase less expensive formal care (Ettner 1996), whereas those with lower wages may be more likely to leave the labor market and keep the funds to provide care themselves (McKnight 2006). The largest problem associated with self-directed care programs arising directly from this review is the finding that caregivers who leave the labor force or reduce their labor market hours during the caregiving period are unlikely to return to their previous levels of labor force commitment after caregiving ends (Lundsgaard 2005). Given that these payment programs create economic incentives for caregivers receiving low wages to leave the labor market in favor of receiving cash payments, this approach may place the most economically vulnerable caregivers at risk of long-term financial losses and even poverty when the caregiving period and its associated income stop.
Even if more formal services are made available to care recipients, which could enable many caregivers to withdraw from caring in order to work full-time, some caregivers will instead opt to maintain both their jobs and caregiving responsibilities. Thus, the development of labor market legislation and workplace policies to support caregivers may also be warranted. For example, the UK government is currently considering the expansion of flexible work arrangements to unpaid caregivers, as already exists for people with young children who wish to combine work and child care (Heitmueller 2007; Heitmueller and Inglis 2007). The emphasis of this legislation is on retaining workers and contrasts the policy direction being pursued in North America. Through the United States' Family and Medical Leave Act and Canada's Compassionate Care Benefit program, both these countries offer guaranteed job protection (and in the case of Canada, partial income replacement) to caregivers who leave the labor market temporarily to care for sick and dying relatives (Johnson and Lo Sasso 2000; Williams et al. 2006). Both countries are also now considering expanding these programs to improve access. Given the evidence suggesting that caregivers who leave the labor market are unlikely to return after the caregiving period ends (resulting in both short- and long-term economic losses), it may be more beneficial to focus on initiatives that create incentives for caregivers to remain in the labor force.
Employers also have an interest in these issues. A 1997 MetLife study of employers' costs related to employees' caregiving found that the most expensive category ($4.9 billion in 1997 U.S.$) was replacing employees who quit due to their caring responsibilities. Since most work adjustments seem to occur in the early months of caregiving, employers can take a number of steps to help, from offering flexible work hours and working from home to offering short-term leaves and paid benefits (Karoly and Panis 2004; Spillman and Pezzin 2000). For example, another MetLife study (2001) found that caregivers to people with long-term care insurance were twice as likely to remain in the labor force as were caregivers to people without this type of insurance. Such initiatives can help ensure that the job adjustments of unpaid caregivers represent short-term career interruptions rather than a permanent withdrawal from the labor force.
Workplace assistance programs may also help unpaid caregivers address other workplace problems described in the literature, such as arriving late, being absent, taking extended breaks and leaving early, experiencing reduced productivity, and not accepting overtime or career-advancing opportunities such as promotions (Barr, Johnson, and Warshaw 1992; Dautzenberg et al. 2000; Fast, Williamson, and Keating 1999; Fredriksen 1996; Fredriksen-Goldsen and Farwell 2004; Gottlieb, Kelloway, and Fraboni 1994; Jenson and Jacobzone 2000, 14; Keating et al. 1999; Keefe and Medjuck 1997; MetLife 2001; Scharlach 1994; Scharlach and Boyd 1989).
While caregivers and employers may be able to negotiate mutually satisfactory workplace accommodations, unpaid caregivers' reduction of labor market hours should be carefully considered from a policymaking perspective. Even small reductions in work hours to provide unpaid care can have long-term consequences for caregivers' future pensions and retirement savings (Johnson and Lo Sasso 2000, 2001). Since all indications suggest that current and future cohorts of working-aged individuals will be held increasingly responsible for their own economic well-being in retirement (Ettner 1995; Wolf 1999), today's working-age caregivers may risk greater economic insecurity in their retirement years. Thus there may be a place for tax benefits and pension concessions that can offset these losses.
In the final analysis, individual countries must weigh the benefits of creating policy supports for unpaid caregivers to the sick and disabled against a number of issues. National demographic trends, unemployment rates, social values toward the family generally (such as parental leave policies for those caring for young children), health worker shortages, and rising health care costs all must inform decisions to ensure that labor market policies for unpaid caregivers offer desirable long-term outcomes for caregivers, care recipients, and societies more broadly.
Acknowledgments
Meredith Lilly acknowledges funding support as follows: Canadian Institutes of Health Research (CIHR), Doctoral Research Award (Institute of Health Services and Policy Research, Institute of Gender, Institute of Aging); the CIHR Strategic Training Program in Health Care, Technology and Place; and a CHSRF/CIHR Genesis Fellowship Award. Peter Coyte is supported by funds from the Canadian Health Services Research Foundation, the Canadian Institutes of Health Research, and the Ontario Ministry of Health and Long-Term Care for his Chair in Health Care Settings and Canadians. The authors would like to thank the editor and three reviewers for their thoughtful comments and suggestions.
Endnotes
A small literature exists to suggest that caregivers feel they have little choice in taking on the caring role (Heitmueller 2007; Spiess and Schneider 2003). However, this literature has been focused entirely on those who did become caregivers, failing to capture those who did not take on caring roles, and may have perceived a greater choice.
We also searched ASSIA: Applied Social Sciences Index and Abstracts; E-Journals @ Scholars Portal; IBSS: International Bibliography of the Social Sciences; PAIS International; Social Sciences Abstracts @ Scholars Portal; Social Sciences E-Journals @ Scholars Portal; Sociology: A SAGE Full-Text Collection.
We tested and dropped the term labor owing to the large number of inappropriate citations related to childbirth.
We recognize that a significant proportion of individuals provide unpaid care to persons residing in institutions and that this use of their time could affect their labor supply.
National unemployment rates for 2005 were 5.1 percent in the United States (U.S. Bureau of Labor Statistics 2006), 4.8 percent in the United Kingdom (Office for National Statistics 2006), and 6.8 percent in Canada (Statistics Canada 2006). Unemployment rates were higher in the 1980s and 1990s when most of the data for this review were collected, peaking in the United States at 9.7 percent in 1982, in Canada at 11.9 percent in 1983, and in the United Kingdom at 11.9 percent in 1984.
The LFP rates reported in this study for coresident versus extraresident caregivers were averaged to derive a single LFP score.
While caregivers' age was not specified in any of the studies by Pohl, Collins, and Given (1998), Pohl and colleagues (1994), and Barnes, Given, and Given (1995), all caregivers were daughters or daughters-in-law, which acts as a proxy indicator of preretirement age.
These LFP rates were derived from original data that divided part-time and full-time workers.
Doty, Jackson, and Crown (1998) included LFP rates for noncaregivers from the broader literature, but these rates were not derived from their study sample. To maintain consistency with the other three studies that did not include rates, we also applied national census data to this study rather than to the referenced literature provided by the authors.
For example, the first study by Doty, Jackson, and Crown (1998) had a caregiver sample size of 333 caregivers out of a total of 9,244 caregivers across all eleven studies. Its caregiver LFP rate contributed 3.6 percent (333/9,244) to the overall weighted LFP rate. Carmichael and colleagues' 2005 caregiver sample was 1,428, meaning that the caregiver LFP rate in this study contributed 15.4 percent (1,428/9,244) to the weighted total LFP rate. Unweighted results were very similar and are not reported here.
The finding for Doty, Jackson, and Crown (1998) is based on our imputed LFP rate for noncaregivers.
The dataset used in Ettner's 1995 study did not report the number of care hours for coresident caregivers, and the results may be limited by the underlying assumption that coresident caregivers provided more hours of care than did extraresident caregivers. For a discussion of measurement issues related to joint production and caregiver time valuation, see van den Berg and Spauwen (2006).
In addition to the caregiving activities outlined in our Methods section, this study also considered caregiving to include checking up by telephone and making care arrangements.
Bolin, Lindgren, and Lundborg's (2007b) analysis pertains to extraresidential caregivers aged fifty and older in ten European countries. The care recipients in this sample may not have been ill and may have lived in institutions, warranting caution in applying these results broadly.
Based on Heitmueller's (2007) findings for coresidential caregivers. The instrumental variables used for extraresidential caregiving did not survive tests for validity (suggesting possibly weak instruments).
Ettner accounted for endogeneity, and thus her findings are reported as causal rather than as associations.
References
- Arber S, Ginn J. Gender Differences in the Relationship between Paid Employment and Informal Care. Work, Employment and Society. 1995;9(3):445–71. [Google Scholar]
- Arno PS, Levine C, Memmott MM. The Economic Value of Informal Caregiving. Health Affairs. 1999;18(2):182–88. doi: 10.1377/hlthaff.18.2.182. [DOI] [PubMed] [Google Scholar]
- Atkinson AB, Brandolini A. Promise and Pitfalls in the Use of “Secondary” Data-Sets: Income Inequality in OECD Countries as a Case Study. Journal of Economic Literature. 2001;39(3):771–99. [Google Scholar]
- Barnes C, Given B, Given C. Parent Caregivers: A Comparison of Employed and Not Employed Daughters. Social Work. 1995;40(3):375–81. [PubMed] [Google Scholar]
- Barr JK, Johnson KW, Warshaw LJ. Supporting the Elderly: Workplace Programs for Employed Caregivers. The Milbank Quarterly. 1992;70(3):509–33. [PubMed] [Google Scholar]
- Bhopal R, Donaldson L. White, European, Western, Caucasian or What? Inappropriate Labeling in Research on Race, Ethnicity and Health. American Journal of Public Health. 1998;88(9):1303–7. doi: 10.2105/ajph.88.9.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bittman M, Fast JE, Fisher K, Thomson C. Making the Invisible Visible: The Life and Time(s) of Informal Caregivers. In: Folbre N, Bittman M, editors. Family Time: The Social Organization of Care. London: Routledge, Taylor & Francis Group; 2004. pp. 69–84. [Google Scholar]
- Boaz RF. Full-Time Employment and Informal Caregiving in the 1980s. Medical Care. 1996;34(6):524–36. doi: 10.1097/00005650-199606000-00003. [DOI] [PubMed] [Google Scholar]
- Boaz RF, Muller CF. Paid Work and Unpaid Help by Caregivers of the Disabled and Frail Elders. Medical Care. 1992;30(2):149–58. doi: 10.1097/00005650-199202000-00006. [DOI] [PubMed] [Google Scholar]
- Bolin K, Lindgren B, Lundborg P. Informal and Formal Care among Single-Living Elderly in Europe. 2007a. [accessed July 1, 2007]. Tinbergen Institute Discussion Paper TI 2007-031/3. Available at, http://www.tinbergen.nl/discussionpapers/07031.pdf. [DOI] [PubMed]
- Bolin K, Lindgren B, Lundborg P. 2007b. [accessed July 1, 2007]. Your Next of Kin or Your Own Career? Caring and Working among the 50+ of Europe Tinbergen Institute Discussion Paper TI 2007-032/3. Available at, http://www.tinbergen.nl/discussionpapers/07032.pdf.
- Brennan E, Brannan AM. Participation in the Paid Labor Force by Caregivers of Children with Emotional and Behavioral Disorders. Journal of Emotional and Behavioral Disorders. 2005;13(4):237–46. [Google Scholar]
- Bullock K, Crawford SL, Tennstedt SL. Employment and Caregiving: Exploration of African American Caregivers. Social Work. 2003;48(2):150–62. doi: 10.1093/sw/48.2.150. [DOI] [PubMed] [Google Scholar]
- Cannuscio CC, Colditz GA, Rimm EB, Berkman LF, Jones CP, Kawachi I. Employment Status, Social Ties, and Caregivers' Mental Health. Social Science and Medicine. 2004;58:1247–56. doi: 10.1016/S0277-9536(03)00317-4. [DOI] [PubMed] [Google Scholar]
- Carmichael F, Charles S. The Labour Market Costs of Community Care. Journal of Health Economics. 1998;17(6):747–65. doi: 10.1016/s0167-6296(97)00036-2. [DOI] [PubMed] [Google Scholar]
- Carmichael F, Charles S. Benefit Payments, Informal Care and Female Labour Supply. Applied Economic Letters. 2003a;10:411–15. [Google Scholar]
- Carmichael F, Charles S. The Opportunity Costs of Informal Care: Does Gender Matter? Journal of Health Economics. 2003b;22:781–803. doi: 10.1016/S0167-6296(03)00044-4. [DOI] [PubMed] [Google Scholar]
- Carmichael F, Connell G, Hulme C, Sheppard S. Who Cares and at What Cost? The Incidence and the Opportunity Costs of Informal Care. Salford: University of Salford; 2005. [Google Scholar]
- Chang CF, White-Means S. Labour Supply of Informal Caregivers. International Review of Applied Economics. 1995;9(2):192–205. [Google Scholar]
- Charles KK, Sevak P. Can Family Caregiving Substitute for Nursing Home Care? Journal of Health Economics. 2005;24:1174–90. doi: 10.1016/j.jhealeco.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Covinsky K, Eng C, Lui L, Sands L, Sehgal A, Walter L, Wieland D, Eleazer G, Yaffe K. Reduced Employment in Caregivers of Frail Elders: Impact of Ethnicity, Patient Clinical Characteristics, and Caregiver Characteristics. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2001;56(11):707–13. doi: 10.1093/gerona/56.11.m707. [DOI] [PubMed] [Google Scholar]
- Coyte P, McKeever P. Home Care in Canada: Passing the Buck. Canadian Journal of Nursing Research. 2001;33:11–25. [PubMed] [Google Scholar]
- Dale S, Brown R, Phillips B, Carlson B. 2005. [accessed July 1, 2007]. Experiences of Workers Hired under Cash and Counseling: Findings from Arkansas, Florida and New Jersey. U.S. Department of Health and Human Services and ASPE Office of Disability, Aging and Long-Term Care Policy. Available at, http://aspe.hhs.gov/daltcp/reports/workerexp.htm.
- Dautzenberg MGH, Diederiks JPM, Philipsen H, Stevens FCJ, Tan FES, Vernooij-Dassen MJFJ. The Competing Demands of Paid Work and Parent Care. Research on Aging. 2000;22(2):165–87. [Google Scholar]
- Dentinger E, Clarkberg M. Informal Caregiving and Retirement Timing among Men and Women. Journal of Family Issues. 2002;23(7):857–79. [Google Scholar]
- Doty P. 1998. [accessed August 27, 2007]. Cost-Effectiveness of Home and Community-Based Long-Term Care Services. U.S. Department of Health And Human Services and ASPE Office of Disability, Aging and Long-Term Care Policy. Available at, http://aspe.hhs.gov/daltcp/reports/costeff.htm.
- Doty P, Jackson M, Crown W. The Impact of Female Caregivers' Employment Status on Patterns of Formal and Informal Eldercare. The Gerontologist. 1998;38(3):331–41. doi: 10.1093/geront/38.3.331. [DOI] [PubMed] [Google Scholar]
- Duke University Center for Demography. National Long Term Care Survey. 2006. [accessed October 1, 2006]. Available at, http://nltcs.cds.duke.edu/index.htm.
- EPPI-Centre. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2007. [accessed June 15, 2007]. EPPI-Centre Methods for Conducting Systematic Reviews. Available at, http://eppi.ioe.ac.uk/cms/Default.aspx?tabid=89. [Google Scholar]
- Ettner S. The Impact of “Parent Care” on Female Labour Supply Decisions. Demography. 1995;32(1):63–80. [PubMed] [Google Scholar]
- Ettner S. The Opportunity Costs of Elder Care. Journal of Human Resources. 1996;31(1):189–205. [Google Scholar]
- Fast J, Eales J, Keating N. Economic Impact of Health, Income Security & Labour Policies on Informal Caregivers of Frail Seniors. Ottawa: Status of Women Canada; 2001. [Google Scholar]
- Fast JE, Williamson DL, Keating NC. The Hidden Costs of Informal Elder Care. Journal of Family and Economic Issues. 1999;20(3):301–26. [Google Scholar]
- Franklin ST, Ames BD, King S. Acquiring the Family Eldercare Role: Influence on Female Employment Adaptation. Research on Aging. 1994;16(1):27–42. [Google Scholar]
- Fredriksen KI. Gender Differences in Employment and the Informal Care of Adults. Journal of Women and Aging. 1996;8(2):35–53. [Google Scholar]
- Fredriksen-Goldsen KI, Farwell N. Dual Responsibilities among Black, Hispanic, Asian, and White Employed Caregivers. Journal of Gerontological Social Work. 2004;43(4):25–44. [Google Scholar]
- Gottlieb BH, Kelloway EK, Fraboni M. Aspects of Eldercare That Place Employees at Risk. The Gerontologist. 1994;34(6):815–21. doi: 10.1093/geront/34.6.815. [DOI] [PubMed] [Google Scholar]
- Gujarati DN. Basic Econometrics. 4th ed. Boston: McGraw-Hill; 2003. [Google Scholar]
- Hawranik PG, Strain LA. Health of Informal Caregivers: Effects of Gender, Employment, and Use of Home Care Services. 2000. [accessed October 21, 2006]. Available at, http://www.pwhce.ca/pdf/informal-care/informal_report.pdf.
- Hedge JW, Borman WC, Lammlein SE. The Aging Workforce: Realities, Myths, and Implications for Organizations. Washington, D.C: American Psychological Association; 2006. [Google Scholar]
- Heitmueller A. The Chicken or the Egg? Endogeneity in Labour Market Participation of Informal Carers in England. Journal of Health Economics. 2007;26(3):536–59. doi: 10.1016/j.jhealeco.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Heitmueller A, Inglis K. The Earnings of Informal Carers: Wage Differentials and Opportunity Costs. Journal of Health Economics. 2007;26(3):821–41. doi: 10.1016/j.jhealeco.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Henz U. The Effects of Informal Care on Paid-Work Participation in Great Britain: A Lifecourse Perspective. Ageing and Society. 2004;24:851–80. [Google Scholar]
- Higgins JPT, Green S. The Cochrane Library. issue 4. Chichester: Wiley; 2006. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6. [updated, September 2006] [Google Scholar]
- Jenkins CL. Women, Work and Caregiving: How Do These Roles Affect Women's Well-Being? Journal of Women and Aging. 1997;9(3):27–45. [Google Scholar]
- Jenson J, Jacobzone S. Care Allowances for the Frail Elderly and Their Impact on Women Care-Givers. Paris: Organisation for Economic Co-Operation and Development; 2000. [Google Scholar]
- Johnson R.W, Lo Sasso AT. The Trade-Off between Hours of Paid Employment and Time Assistance to Elderly Parents at Midlife. 2000. [accessed October 20, 2006]. Available at, http://www.urban.org/UploadedPDF/elderly_parents.pdf.
- Johnson RW, Lo Sasso AT. Balancing Retirement Security with the Needs of Frail Parents: Caregiving, Financial Transfers and Work by Women at Midlife. North American Actuarial Journal. 2001;5(1):104–8. [Google Scholar]
- Karoly LA, Panis CWA. The 21st Century at Work: Forces Shaping the Future Workforce and Workplace in the United States. Santa Monica, Calif: Rand Corporation; 2004. [Google Scholar]
- Kaye HS, Chapman S, Newcome RJ, Harrington C. The Personal Assistance Workforce: Trends in Supply and Demand. Health Affairs. 2006;25(4):1113–20. doi: 10.1377/hlthaff.25.4.1113. [DOI] [PubMed] [Google Scholar]
- Keating N, Fast J, Frederick J, Cranswick K, Perrier C. Ottawa: 1999. Eldercare in Canada: Context, Content and Consequences. Report no. 89-570-XPE. [Google Scholar]
- Keefe J, Medjuck S. The Contribution of Long Term Economic Costs to Predicting Strain among Employed Women Caregivers. Journal of Women and Aging. 1997;9(3):3–25. [Google Scholar]
- Kolodinsky J, Shirey L. The Impact of Living with an Elder Parent on Adult Daughter's Labor Supply and Hours of Work. Journal of Family and Economic Issues. 2000;21(2):149–75. [Google Scholar]
- Leiter V, Wyngaarden Krauss M, Anderson B, Wells N. The Consequences of Caring: Effects of Mothering a Child with Special Needs. Journal of Family Issues. 2004;25(3):379–403. [Google Scholar]
- Levine C. Home Sweet Hospital: The Nature and Limits of Private Responsibilities for Home Health Care. Journal of Aging and Health. 1999;11(3):341–59. doi: 10.1177/089826439901100305. [DOI] [PubMed] [Google Scholar]
- Levine C, Albert SM, Hokenstad A, Halper DE, Hart AY, Gould DA. “This Case Is Closed”: Family Caregivers and the Termination of Home Health Care Services for Stroke Patients. The Milbank Quarterly. 2006;84(2):305–31. doi: 10.1111/j.1468-0009.2006.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long A. Some Methodological Challenges in Undertaking Reviews in Social Care. In: Popay J, editor. Moving beyond Effectiveness in Evidence Synthesis: Methodological Issues in the Synthesis of Diverse Sources of Evidence. London: National Institute for Health and Clinical Excellence; 2006. pp. 41–49. [Google Scholar]
- Lundsgaard J. Consumer Direction and Choice in Long-Term Care for Older Persons, Including Payments for Informal Care: How Can It Help Improve Care Outcomes, Employment and Fiscal Sustainability. 2005. [accessed June 25, 2007]. OECD Health Working Papers no. 20, Available at http://www.oecd.org/dataoecd/53/62/34897775.pdf,
- MacDonald M, Phipps S, Lethbridge L. Taking Its Toll: The Influence of Paid and Unpaid Work on Women's Well-Being. Feminist Economics. 2005;11(1):63–94. [Google Scholar]
- McKnight R. Home Care Reimbursement, Long-Term Care Utilization, and Health Outcomes. Journal of Public Economics. 2006;2006:293–323. [Google Scholar]
- McLanahan SS, Monson RA. Madison: Center for Demography and Ecology, University of Wisconsin; 1990. Caring for the Elderly: Prevalence and Consequences. NSFH Working Paper no. 18. [Google Scholar]
- MetLife Mature Market Institute. The MetLife Study of Employer Costs for Working Caregivers. 1997. [accessed June 24, 2007]. Available at, http://www.metlife.com/WPSAssets/88881768001015600333V1F5.1.066.pdf.
- MetLife Mature Market Institute. The MetLife Study of Employed Caregivers: Does Long Term Care Insurance Make a Difference. 2001. [accessed June 24, 2007]. Available at, http://www.metlife.com/WPSAssets/20031939151018862160V1Femployed.pdf.
- Moen P, Robison J, Fields V. Women's Work and Caregiving Roles: A Life Course Approach. Journals of Gerontology: Series B. Psychological Sciences and Social Sciences. 1994;49(4):S176–86. doi: 10.1093/geronj/49.4.s176. [DOI] [PubMed] [Google Scholar]
- Muramatsu N, Campbell RT. State Expenditures on Home and Community Based Services and Use of Formal and Informal Personal Assistance: A Multilevel Analysis. Journal of Health and Social Behavior. 2002;43(1):107–24. [PubMed] [Google Scholar]
- Muramatsu N, Hongjun Y, Campbell RT, Hoyem RL, Jacob MA, Ross CO. Risk of Nursing Home Admission among Older Americans: Does States' Spending on Home- and Community-Based Services Matter? Journal of Gerontology: Social Sciences. 2007;62B(3):S169–78. doi: 10.1093/geronb/62.3.s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutschler PH. Bearing the Costs of Our Eldercare Policies: Work Constraints among Employed Caregivers. Journal of Aging and Social Policy. 1993;5(4):23–49. doi: 10.1300/j031v05n04_03. [DOI] [PubMed] [Google Scholar]
- Mutschler PH. From Executive Suite to Production Line: How Employees in Different Occupations Manage Elder Care Responsibilities. Research on Aging. 1994;16(1):7–26. [Google Scholar]
- Muurinen J-M. The Economics of Informal Care. Medical Care. 1986;24(11):1007–17. doi: 10.1097/00005650-198611000-00005. [DOI] [PubMed] [Google Scholar]
- Office for National Statistics. Labour Market Review 2006. Hampshire: Palgrave Macmillan; 2006. [Google Scholar]
- Pavalko EK, Artis JE. Women's Caregiving and Paid Work: Causal Relationships in Midlife. Journals of Gerontology. Series B: Psychological Sciences and Social Sciences. 1997;52(4):S170–79. doi: 10.1093/geronb/52b.4.s170. [DOI] [PubMed] [Google Scholar]
- Pavis S, Hubbard G, Platt S. Young People in Rural Areas: Socially Excluded or Not? Work, Employment and Society. 2001;15(2):291–309. [Google Scholar]
- Payne G, Laporte A, Deber R, Coyte PC. Counting Backward to Health Care's Future: Using Time-to-Death Modeling to Identify Changes in End-of-Life Moribidity and the Impact of Aging on Health Care Expenditures. The Milbank Quarterly. 2007;85(2):213–57. doi: 10.1111/j.1468-0009.2007.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezzin L, Schone BS. Intergenerational Household Formation, Female Labor Supply and Informal Caregiving: A Bargaining Approach. Journal of Human Resources. 1999;34(3):475–503. [Google Scholar]
- Pfeffer N. Theories of Race, Ethnicity and Culture. British Medical Journal. 1998;317:1381–84. doi: 10.1136/bmj.317.7169.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohl J, Collins C, Given C. Longitudinal Employment Decisions of Daughters and Daughters-in-Law after Assuming Parent Care. Journal of Women and Aging. 1998;10(1):59–74. doi: 10.1300/j074v10n01_05. [DOI] [PubMed] [Google Scholar]
- Pohl J, Given C, Collins C, Given B. Social Vulnerability and Reactions to Caregiving in Daughters and Daughters-in-Law Caring for Disabled Aging Parents. Health Care for Women International. 1994;15:385–95. doi: 10.1080/07399339409516131. [DOI] [PubMed] [Google Scholar]
- Roberts AA. The Labor Market Consequences of Family Illness. Journal of Mental Health Policy and Economics. 1999;2:183–95. doi: 10.1002/(sici)1099-176x(199912)2:4<183::aid-mhp62>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Scharlach AE. Caregiving and Employment: Competing or Complementary Roles? The Gerontologist. 1994;34(3):378–85. doi: 10.1093/geront/34.3.378. [DOI] [PubMed] [Google Scholar]
- Scharlach AE, Boyd S. Caregiving and Employment: Results of an Employee Survey. The Gerontologist. 1989;29(3):382–87. doi: 10.1093/geront/29.3.382. [DOI] [PubMed] [Google Scholar]
- Shireman TI, Rigler SK. Penny Wise, Pound Wise: A Comparison of Medicaid Expenditures for Home and Community-Based Services versus Nursing Facility Care for Older Adults. Home Health Care Services Quarterly. 2004;23(4):15–28. doi: 10.1300/J027v23n04_02. [DOI] [PubMed] [Google Scholar]
- Spiess K, Schneider AU. Interactions between Care-Giving and Paid Work Hours among European Midlife Women, 1994 to 1996. Ageing and Society. 2003;23:41–68. [Google Scholar]
- Spillman BC, Pezzin LE. Potential and Active Family Caregivers: Changing Networks and the “Sandwich Generation.”. The Milbank Quarterly. 2000;78(3):347–74. doi: 10.1111/1468-0009.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitze G, Logan JR. Employment and Filial Relations: Is There a Conflict? Sociological Forum. 1991;6(4):681–97. [Google Scholar]
- Stabile M, Laporte A, Coyte PC. Household Responses to Public Home Care programs. Journal of Health Economics. 2006;25(4):674–701. doi: 10.1016/j.jhealeco.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Stanley TD. Wheat from Chaff: Meta-Analysis as Quantitative Literature Review. Journal of Economic Perspectives. 2001;15(3):131–50. [Google Scholar]
- Statistics Canada. 2001. [accessed December 8, 2006]. Population 15 Years and over by Sex, Age Groups and Labour Force Activity, for Canada, Provinces and Territories, 1981–1996. Available at, http://www.statcan.ca/english/census96/mar17/labour/table6/t6p00a.htm.
- Statistics Canada. Labour Force Survey. 2006. [accessed November 1, 2006]. Available at, http://www.statcan.ca/english/Subjects/Labour/LFS/lfs-en.htm.
- Sterne JAC, Egger M, Smith GD. Systematic Reviews in Health Care: Investigating and Dealing with Publication and Other Biases in Meta-analysis. British Medical Journal. 2001;323(7304):101–5. doi: 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone R. The Direct Care Worker: The Third Rail of Home Care Policy. Annual Review of Public Health. 2004;25:521–37. doi: 10.1146/annurev.publhealth.25.102802.124343. [DOI] [PubMed] [Google Scholar]
- Stone R, Short P. The Competing Demands of Employment and Informal Caregiving to Disabled Elders. Medical Care. 1990;28(6):513–26. doi: 10.1097/00005650-199006000-00004. [DOI] [PubMed] [Google Scholar]
- Tennstedt SL, Crawford SL, McKinlay JB. Is Family Care on the Decline? A Longitudinal Investigation of the Substitution of Formal Long-Term Care Services for Informal Care. The Milbank Quarterly. 1993;71(4):601–24. [PubMed] [Google Scholar]
- Toosi M. A New Look at Long-Term Labor Force Projections to 2050. Monthly Labor Review. 2006:19–39. November. [Google Scholar]
- Tranmer JE, Guerriere DN, Ungar WJ, Coyte PC. Valuing Patient and Caregiver Time: A Review of the Literature. Pharmacoeconomics. 2005;23(5):449–59. doi: 10.2165/00019053-200523050-00005. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey. 2005. [accessed November 1, 2006]. Available at, http://www.bls.gov/cps/home.htm.
- U.S. Bureau of Labor Statistics. Labor Force Participation Rate: Labor Force Statistics from the Current Population Survey. 2006. [accessed December 12, 2006]. Available at, http://www.bls.gov/cps/home.htm.
- U.S. Department of Health and Human Services Administration on Aging. A Profile of Older Americans: 2006. 2006. [accessed July 18, 2007]. Available at, http://www.aoa.gov/PROF/Statistics/profile/2006/profiles2006.asp.
- U.S. General Accounting Office. Older Workers: Policies of Other Nations to Increase Labor Force Participation: Report to the Ranking Minority Member, Special Committee on Aging, U.S. Senate. 2003. [accessed October 1, 2006]. Available at, http://eric.ed.gov/ERICDocs/data/ericdocs2/content_storage_01/0000000b/80/27/d0/e7.pdf.
- University of Wisconsin at Madison. National Survey of Families and Households. 2006. [accessed September 1, 2006]. Available at, http://www.ssc.wisc.edu/nsfh/
- Van Den Berg B, Spauwen P. Measurement of Informal Care: An Empirical Study into the Valid Measurement of Time Spent on Informal Caregiving. Health Economics. 2006;15(5):447–60. doi: 10.1002/hec.1075. [DOI] [PubMed] [Google Scholar]
- Van Houtven CH, Norton EC. Informal Care and Health Care Use of Older Adults. Journal of Health Economics. 2004;23:1159–80. doi: 10.1016/j.jhealeco.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Viitanen TK. Informal and Formal Care in Europe. 2007. [accessed June 1, 2007]. Tinbergen Institute Discussion Paper no. 2648, Available at http://ftp.iza.org/dp2648.pdf,
- Wakabayashi C, Donato KM. The Consequences of Caregiving: Effects on Women's Employment and Earnings. Population Research and Policy Review. 2005;24:467–88. [Google Scholar]
- Weissert WG, Cready CM, Pawelak JE. The Past and Future of Home- and Community-Based Long-Term Care. The Milbank Quarterly. 2005;83(4):1–71. [PubMed] [Google Scholar]
- White-Means SI. Allocation of Labor to Informal Home Health Production: Health Care for Frail Elderly, If Time Permits. Journal of Consumer Affairs. 1992;26(1):69–89. [Google Scholar]
- White-Means SI. Informal Home Care for Frail Black Elderly. Journal of Applied Gerontology. 1993;12(1):18–33. [Google Scholar]
- White-Means SI. The Demands of Persons with Disabilities for Home Health Care and the Economic Consequences for Informal Caregivers. Social Science Quarterly. 1997;78(4):955–72. [Google Scholar]
- White-Means SI, Chollet D. Opportunity Wages and Workforce Adjustments: Understanding the Cost of In-Home Elder Care. Journals of Gerontology. Series B: Psychological Sciences and Social Sciences. 1996;51B(2):S82–90. doi: 10.1093/geronb/51b.2.s82. [DOI] [PubMed] [Google Scholar]
- White-Means SI, Thornton M. Labor Market Choices and Home Health Care Provision among Employed Ethnic Caregivers. The Gerontologist. 1990;30(6):769–75. doi: 10.1093/geront/30.6.769. [DOI] [PubMed] [Google Scholar]
- Wiles J. Informal Caregivers' Experiences of Formal Support in a Changing Context. Health and Social Care in the Community. 2003;11(2):189–207. doi: 10.1046/j.1365-2524.2003.00419.x. [DOI] [PubMed] [Google Scholar]
- Williams A, Crooks VA, Stajduhar KI, Allan D, Cohen SR. Canada's Compassionate Care Benefit: Views of Family Caregivers in Chronic Illness. International Journal of Palliative Nursing. 2006;12(8):438–49. doi: 10.12968/ijpn.2006.12.9.21872. [DOI] [PubMed] [Google Scholar]
- Winker M. Measuring Race and Ethnicity: Why and How? Journal of the American Medical Association. 2004;292(13):1612–14. doi: 10.1001/jama.292.13.1612. [DOI] [PubMed] [Google Scholar]
- Wolf DA. The Family as Provider of Long-Term Care. Journal of Aging and Health. 1999;11(3):360–82. doi: 10.1177/089826439901100306. [DOI] [PubMed] [Google Scholar]
- Wolf DA, Hunt K, Knickman J. Perspectives on the Recent Decline in Disability at Older Ages. The Milbank Quarterly. 2005;83(3):365–95. doi: 10.1111/j.1468-0009.2005.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf DA, Soldo BJ. Married Women's Allocation of Time to Employment and Care of Elderly Parents. Journal of Human Resources. 1994;29(4):1259–76. [Google Scholar]
- Yantzi NM, Rosenberg MW, McKeever P. Getting out of the House: The Challenges Mothers Face When Their Children Have Long-Term Care Needs. Health and Social Care in the Community. 2007;15(1):45–55. doi: 10.1111/j.1365-2524.2006.00663.x. [DOI] [PubMed] [Google Scholar]


