Abstract
Context
The mortality numbers and rates of chronic disease are rising faster in developing than in developed countries. This article compares prevailing explanations of population chronic disease trends with theoretical and empirical models of population chronic disease epidemiology and assesses some economic consequences of the growth of chronic diseases in developing countries based on the experiences of developed countries.
Methods
Four decades of male mortality rates of cardiovascular and chronic noncommunicable diseases were regressed on changes in and levels of country income per capita, market integration, foreign direct investment, urbanization rates, and population aging in fifty-six countries for which comparative data were available. Neoclassical economic growth models were used to estimate the effect of the mortality rates of chronic noncommunicable diseases on economic growth in high-income OECD countries.
Findings
Processes of economic growth, market integration, foreign direct investment, and urbanization were significant determinants of long-term changes in mortality rates of heart disease and chronic noncommunicable disease, and the observed relationships with these social and economic factors were roughly three times stronger than the relationships with the population's aging. In low-income countries, higher levels of country income per capita, population urbanization, foreign direct investment, and market integration were associated with greater mortality rates of heart disease and chronic noncommunicable disease, less increased or sometimes reduced rates in middle-income countries, and decreased rates in high-income countries. Each 10 percent increase in the working-age mortality rates of chronic noncommunicable disease decreased economic growth rates by close to a half percent.
Conclusions
Macrosocial and macroeconomic forces are major determinants of population rises in chronic disease mortality, and some prevailing demographic explanations, such as population aging, are incomplete on methodological, empirical, and policy grounds. Rising chronic disease mortality rates will significantly reduce economic growth in developing countries and further widen the health and economic gap between the developed and developing world.
Keywords: Chronic disease, globalization, political economy, social epidemiology
In 2008, more than 31 million people will die from four leading chronic, noncommunicable diseases: heart disease, cancer, respiratory disease, and diabetes. For brevity, in this article the term chronic disease refers to these four chronic, noncommunicable diseases, based on the usage by the Oxford Health Alliance (http://www.oxha.org) and the recent identification of Grand Challenges in chronic disease control (Daar et al. 2007). Close to half of these deaths are estimated to be premature (WHO 2005). Nearly 80 percent will occur in low- and middle-income countries, where these chronic diseases claim around 80 percent more lives than do the total of all infectious causes. Over the past decade, rises in chronic diseases have been most greatly concentrated in developing countries and, in the case of diabetes, have outpaced some of the original Global Burden of Disease's “pessimistic scenario” forecasts (Murray and Lopez 1996).
The outlook for chronic diseases is no better. In 2002, chronic diseases were responsible for 46 percent of all deaths in developing countries, a figure that will grow to 59 percent by 2030, or to more than 37 million lives a year (a 64 percent increase). In all regions of the world, even in low-income countries, the leading chronic diseases are projected to be the major killers.
This means that globally, chronic diseases will rise as infectious diseases fall (see figure 1 and tables 1 and 2; also Omran 1971).1 Although clearly something must be the leading cause of death, the increased risk of chronic disease mortality is not simply a result of a reduction in infectious disease mortality. In East Asia and the Pacific countries, for example, the expected rise in chronic disease mortality rates will be more than five times the expected drop in infectious disease mortality rates. Even in sub-Saharan Africa, where the HIV/AIDS crisis is at its worst, infectious disease mortality rates are expected to drop by 40 percent over the next twenty years while chronic disease mortality rates rise by 12 percent. More generally, infectious diseases are falling and chronic diseases are growing at a much faster pace in low- and middle-income countries than in high-income countries.
Figure 1.
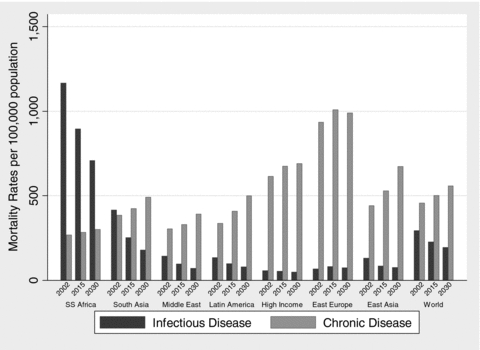
Evolution of the Global Burden of Disease, 2002 to 2030
Notes: Infectious disease classification is based on WHO's type 1 burden of disease cluster. Chronic disease classification is based on cardiovascular disease, cancers, respiratory disease, and diabetes mellitus subcategories of WHO's type 2 burden of disease cluster. Appendix 1 further describes the data sources, disease classifications, and calculations.
Source: Author's calculations based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections.
TABLE 1.
Expected Change in Mortality Rates of Infectious and Chronic Disease per 100,000 Population from 2002 to 2030
| Region | Infectious Diseases | Chronic Diseases |
|---|---|---|
| World | −99.54 | 100.44 |
| High income | −8.02 | 74.26 |
| Eastern Europe and Central Asia | 7.11 | 53.71 |
| East Asia and Pacific | −55.17 | 231.12 |
| South Asia | −236.42 | 107.36 |
| Latin America | −55.80 | 162.18 |
| Middle East and North Africa | −71.52 | 86.47 |
| Sub-Saharan Africa | −457.11 | 32.66 |
Sources: Author's calculations. Data and region categories are based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections. Infectious diseases classification is based on WHO's type 1 burden of disease cluster. Chronic diseases classification is based on cardiovascular disease, cancers, respiratory disease, and diabetes mellitus subcategories of WHO's type 2 burden of disease cluster. Appendix 1 further describes the data sources, disease classifications, and calculations.
TABLE 2.
Expected Growth of Infectious and Chronic Disease Mortality Rates (% per year), 2002 to 2030
| Region | Infectious Diseases | Chronic Diseases |
|---|---|---|
| World | −1.45 | 0.71 |
| High income | −0.53 | 0.41 |
| Eastern Europe and Central Asia | 0.35 | 0.20 |
| East Asia and Pacific | −1.91 | 1.51 |
| South Asia | −2.94 | 0.88 |
| Latin America | −1.87 | 1.41 |
| Middle East and North Africa | −2.42 | 0.89 |
| Sub-Saharan Africa | −1.76 | 0.41 |
Sources: Author's calculations. Data and region categories are based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections. Infectious diseases classification is based on WHO's type 1 burden of disease cluster. Chronic diseases classification is based on cardiovascular disease, cancers, respiratory disease, and diabetes mellitus subcategories of WHO's type 2 burden of disease cluster. Appendix 1 further describes the data sources, disease classifications, and calculations.
This simple taxonomic division between infectious and chronic diseases, originally institutionalized by the World Health Organization (WHO) as types 1 and 2 burden of disease categories (note the implicit policy ordering, type 1 as first-order and type 2 as second-order), has become increasingly problematic for epidemiologists and health policymakers. Diseases can be acute or chronic and infectious (communicable) or noninfectious (noncommunicable), with considerable overlap among these categories (for a comprehensive discussion on medical problems associated with developing a disease taxonomy, see Nolte and McKee 2008 and appendix 1). An epidemiologic justification for focusing on the four leading chronic diseases is that more than four-fifths of all deaths and two-fifths of all disabilities due to chronic noncommunicable diseases are derived from them. Although other important chronic noncommunicable diseases, such as neuropsychiatric disorders and sensory organ diseases, have high morbidity rates, they have comparably lower mortality rates. Another pragmatic policy motivation for concentrating on this subset of chronic noncommunicable diseases pertains to their similar set of determinants: of the many chronic noncommunicable diseases, these four in particular are related to three modifiable risks: (1) tobacco use, (2) alcohol consumption, and (3) unhealthy diet and physical inactivity. Although this does not mean that the other chronic noncommunicable diseases are not important, if the risks of contracting the leading chronic diseases were lowered, the outcome of many of the high-burden, low-probability chronic noncommunicable diseases would be improved as well.
With these foreseeable consequences of chronic diseases and given the potential for their prevention, we might expect that key health organizations, such as the World Health Organization and national health ministries, and also development institutions that focus on poverty, such as the World Bank and the United Nations Development Program, would be aggressively trying to combat the rising tide of chronic diseases in developing countries. But this is, unfortunately, not the case. For example, WHO's headquarters spends US $1 for every chronic noncommunicable disease death (excluding mental health) versus $15 for every infectious disease death (see WHO 2003; Yach et al. 2004). In 2002, official development assistance for chronic noncommunicable diseases represented just under 0.1 percent of the health-sector development assistance provided by OECD countries. Moreover, a 2001 survey of 167 national health ministries found that nearly two-thirds did not have a budget line for chronic noncommunicable diseases (WHO 2003; Yach et al. 2004).2Table 3 outlines some of the reasons for this chronic disease “neglect,” and the rest of this article examines what some of the long-term consequences will be if chronic diseases, and their drivers, remain unchecked, which is the current “no action” scenario.
TABLE 3.
Sources of Weak Global Responses to Chronic Diseases
| Dimension | Key Feature | Implications for Chronic Disease Control |
|---|---|---|
| Exposure, Prevention, and Treatment Aspects | ||
| Health systems | Historical orientation of health care systems toward acute care. | Favors care practices focusing on high-risk individuals rather than on population risks; bias toward tertiary and specialist care rather than prevention. |
| Determinants | Role of macrosocial and macroeconomic forces in propelling risks. | Health sector exhibits low competence and capacity for acting on upstream and globalized drivers of risks. |
| Behavioral and choice aspects of chronic disease risks. | Frames risks as problems of individual responsibility, emphasizing role of individual rather than socioenvironmental intervention. | |
| Heterogeneity | Diversity of chronic disease inputs and end points. | Complicates prevention and treatment intervention analysis, implementation, and evaluation. |
| Population Accumulation and Distribution of Risks and Disease | ||
| Risk accumulation | Long and variable lag times between risk exposure and clinical expression as disease or disability. | Greater population dispersion and lower recognizability make chronic diseases easier to ignore and less likely to stimulate fear or public outrage; longer-term benefits of interventions mismatch with shorter-term political cycles; more difficult to model empirically. |
| Age distribution | Chronic diseases tend to occur in middle to later stages of life. | Are less politically salient than conditions that afflict youth; promote the misconception that chronic diseases are inevitable consequences of aging. |
| Social distribution | Within countries: as countries develop, higher-SES groups tend to first absorb transformed risk habits and are thus the earliest to develop chronic diseases. | Promotes the notion that chronic diseases are “diseases of affluence” despite evidence that the within-population distribution of chronic disease risks undergoes a “social transition” to disproportionately afflict lower-SES groups. |
| Between countries: burden of chronic disease is higher in developed countries but is a higher absolute burden in developing countries. | Global actors lower prioritization of chronic diseases on distributive grounds, even though chronic disease growth will be concentrated in developing countries and further widen the gap between the health of the rich and poor. | |
| Political, Economic, and Managerial Aspects | ||
| Role of markets | Economic notion that markets will achieve optimal level of chronic disease control. | Individual responsibility paradigm associated with behavioral risk factors provides no legitimate role for state intervention; does not reflect evidence of market failures. |
| Health-sector reform | Expanding marketization of health systems. | Cost-shifting reforms have levied greater costs of chronic disease prevention and treatment onto patients. |
| Decentralization and devolution of health authority. | Policymaking capacity of national health ministries and systems is circumscribed. | |
| Governance trends | Diffusion of governance authority to private actors. | Tensions are apparent between profit incentives of some private actors and chronic disease prevention. |
I begin my analysis by introducing a basic transition model of chronic disease epidemiology, which I then test against a series of comparative epidemiologic facts about chronic diseases to ascertain some key drivers of population chronic disease growth. Next I evaluate these determinants in the context of globalization and provide some empirical tests of these hypotheses with respect to prevailing explanations. I then draw on this evidence base to forecast some of the global consequences of chronic disease growth for health and economic development in rich and poor countries. I conclude with some implications for global health policy and recommendations for controlling chronic diseases.
Drivers of Chronic Disease Risk
Chronic diseases have a common set of clinical risk factors—hypercholesterolemia, hypertension, and obesity—and their associated behavioral risk factors—tobacco, physical inactivity, and unhealthy diets. Figure 2 shows a standard model of chronic disease epidemiology, in which a member of the population transitions (1) from being healthy to acquiring a behavioral risk factor, at a probability modified by the effectiveness of primary prevention and a set of social determinants (P1), and then (2) from having a behavioral risk factor to having a clinical risk factor at a probability modified by the effectiveness of secondary prevention as well as other modifiers such as age, coexisting risks, and social determinants (P2), and so forth. Exposures to risk factors act synergistically and cumulatively over the life course, speeding up the progression from being healthy to future chronic disease morbidity and mortality. As chronic diseases move from one state to the next, the health and economic burdens increase. With low probability, a person's movement toward chronic disease morbidity and mortality can be reversed, but with successful intervention, the progression of chronic disease can be stopped.
Figure 2.
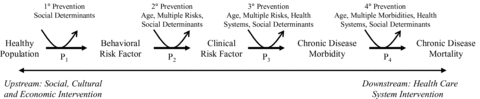
Transition-State Model of Chronic Disease Epidemiology
Notes: P is a population probability, and for each state (healthy, behavioral risk, clinical risk, morbidity, and mortality) refers to the probability that an individual transitions from one chronic disease state to the next. For example, P1 refers to an individual's transition from being healthy to acquiring a behavioral risk, such as initiating tobacco or being sedentary. Sitting above P1 in the model is the effectiveness of primary prevention and a set of social determinants, which are shown to modify this population transition probability both positively and negatively. The model is based upon a Markov process modeling framework, which is increasingly being used to model comparatively the effectiveness of population interventions at various stages of the transitions from health to chronic disease mortality.
What does this model tell us about chronic disease trends? I use three comparative epidemiologic facts about the population distributions of chronic diseases to identify the key drivers of chronic disease growth:
Persons in poor countries tend to die at younger ages from chronic diseases than do persons in rich countries.
Poor countries have higher morbidity rates of chronic disease than rich countries do.
The rate of chronic diseases is growing faster in poor countries than in rich countries.
Fact 1, depicted in table 4, implies that people in poorer countries either are moving through the transitions from being healthy to dying more rapidly than people in rich countries are or are accumulating behavioral risks at younger ages. There is evidence for both these possibilities: (1) health systems in resource-poor settings are less effective at stopping chronic disease progression, and (2) the use of alcohol and tobacco is begun at younger ages in poor countries, and coexisting risks, such as micronutrient deficiencies and stunting, lead to greater risks for childhood obesity and early-onset diabetes.3
TABLE 4.
Standardized Mortality Rate Ratios of Chronic Diseases, Low- versus High-Income Countries by Age Group
| Age Group | |||||||
|---|---|---|---|---|---|---|---|
| 0–14 | 15–29 | 30–44 | 45–59 | 60–69 | 70–79 | 80+ | |
| Mortality Rate Ratio | 3.24 | 2.77 | 1.80 | 2.06 | 2.16 | 1.97 | 1.35 |
Source: Author's calculations, based on World Health Organization Global Burden of Disease statistics, 2002 update.
In regard to fact 2, that poor countries have higher morbidity rates of chronic disease than rich countries do (about 31 percent more disability-adjusted life years per 100,000 population), together with fact 3, that the rate of chronic disease is growing faster in poor countries, suggests that health care is unlikely to be a crucial driver. Health care might possibly account for fact 2 (although a higher P4 would compress morbidity in poor countries; see appendix 1), but health systems alone cannot explain the rise in chronic disease incidence. Indeed, P3, the probability of a transition from clinical risk to chronic disease morbidity, has likely been decreasing across the world as health systems have become stronger.
What about population aging? Several studies cite it as the principal driver of the rise in population chronic disease rates (Marks and McQueen 2002; Mathers and Loncar 2006; Murray and Lopez 1997; Roglic and Unwin 2005; WB 2007). But this conclusion is often a (spurious) feature of a commonly used method to decompose population mortality forecasts into demographic and epidemiologic change components (for a methodological critique, see appendix 1). The aging of a population cannot independently account for the global differences in the growth of the mortality rate: the percentage of the population over age sixty-five is rising faster in developed than in developing countries, even though the absolute numbers of persons aging is much higher in developing countries (CDC 2003; Murray and Lopez 1997). In sub-Saharan Africa, the proportion of persons over sixty-five will increase from 3.1 percent in 2007 to 3.7 percent in 2030. At the same time, mortality numbers are projected to roughly double from 1.8 million to 3.7 million, and mortality rates are projected to grow at a rate of 0.4 percent a year during this period (for more details, see appendix 1).
Perhaps the set of behavioral risk factors is responsible. Together, they are estimated to account for 30 to 60 percent of chronic diseases, and their burden is growing. In 2015, tobacco is projected to be responsible for 50 percent more deaths than is HIV/AIDS, or more than 10 percent of all deaths, roughly 6.4 million. Some of the behavioral risks are global vices, such as tobacco, for which the risk always increases as exposure rises. Other behavioral factors, however, can be favorable to chronic disease, such as healthy dietary intake and greater physical activity.
What the behavioral risks have in common is that they operate at the individual level. These occupy the space in the model at P1, or the probability that a population member starts smoking, drinking, not exercising, or eating unhealthy foods. To explain cross-national patterns of chronic disease using these individual risk factors thus begs the question: Why are people all over the world today making worse personal choices than before, and at a rate much higher in developing countries than in developed countries? Clearly, this is only a partial explanation of chronic disease growth, and a large residual risk remains to be accounted for. Putting too much emphasis on the individual perspective suffers exactly the opposite bias of ecologic fallacy: whereas an ecological fallacy distorts individual causes through population associations, an individual fallacy distorts population causes through individual associations.
To fully understand what is driving such sweeping individual changes—that is, population changes—we must look to the social forces that are transforming risk factors acting at both the individual and societal levels.
The Role of Macrosocial and Macroeconomic Factors and Some Empirical Tests
Globalization provides the best theoretical framework for understanding today's rising risk of chronic disease and for thinking about what will happen in the future. Next I outline three structural aspects of globalization: economic flows, economic growth, and technological change, which are shifting the entire healthy population's risk distribution to the right (or increasing P1 much faster in poor than in rich countries).
Economic Flows
Recent years have seen a rapid increase in global interconnectivity, or “transnationality,” which facilitates the free flow of goods, resources, and services across countries. Many of these products flow from the global North to the global South and, in so doing, tap existing local markets and often create new ones. Most of these flows as they relate to behavioral risks favor items that can be easily transported, such as processed and prepackaged items like sodas and cigarettes. Since supply chains and technology are more advanced in the global North, many of these products outcompete more expensive products generated by local suppliers. As a result of transnational companies' significant market advantages, the large-scale entry of Western foods and beverages and tobacco companies into emerging markets will continue (Gilmore and McKee 2004).
Countries often wish to encourage such investment by foreign sources (foreign direct investment, or FDI) as a way to boost their economic growth. FDI offers expertise and resources that are typically unavailable at home. In order to enhance the potential for these flows, countries seek to integrate themselves more fully into the global marketplace by liberalizing trade restrictions and transferring the ownership of large state-owned monopolies to the private sector.
Much of this is to the good. When markets work well, people are better off. More competition brings lower prices and more efficiently delivers goods to populations. Conversely, in the presence of market failures4 relating to the increased risk of chronic disease (Suhrcke et al. 2006; WB 2007), boosting a market's competitiveness may spread a population's chronic diseases even further. From a chronic disease control perspective, strategies such as liberalizing trade restrictions break down for global vices like tobacco but can improve access to nutritious fruits and vegetables. Many critics, however, believe that the current market environment in poor countries, where regulatory regimes are often underdeveloped and where global companies may be able to undermine efforts to strengthen regulation (Gilmore, Collin, and McKee 2006), privileges risky rather than healthy products (on foreign direct investment's differential effects on diets in developed and developing countries, see Hawkes 2005 and 2006, and for evidence in relation to tobacco, see Gilmore and McKee 2005; also Beaglehole and Yach 2003; Pang and Guindon 2004; Popkin 2002; Rayner et al. 2006). How this might be the case can be better understood by examining the interaction between these prevailing economic growth strategies and co-occurring social transformations.
Economic Growth
As a population's income level increases, people's habits and consumption patterns change. Rapid growth creates many opportunities to modify a population's risk just as people's lifestyles catch up to their newfound wealth. This is particularly true for rapidly developing countries such as India and China, which have registered record economic growth rates of more than 5 percent on average over the past decade but have also experienced a rapid rise in the risk of chronic disease (Reddy et al. 2005; Wang et al. 2005).
Unlike in Western countries, where people buy more healthy foods and spend more time exercising as their income levels rise, in developing countries the opposite seems to happen (Cutler, Glaeser, and Shapiro 2003; Drewnowski and Darmon 2005; Popkin et al. 2001). Why might this be the case?
First, transnational companies have aggressively engaged in information campaigns in developing countries using advanced marketing strategies proven in Western countries. In less competitive information environments, such as those in developing countries, marketing is even more powerful than persons in the West can appreciate. One particularly effective strategy has been to confer social status or prestige on eating in restaurants, often by associating restaurant consumption with cosmopolitan Western habits (for a discussion, see Yum! brands marketing strategies in developing countries and Witkowski 2007).5 This and other effective marketing strategies raise the desirability of Western imports and outside-the-home food consumption as they become more affordable, that is, as incomes grow.
Technological Change and Social Flows
Growth is only part of the story. Technological changes driving growth also are relevant. As societies advance technologically, labor shifts from agrarian to intellectual production, and workplaces become increasingly sedentary. Work becomes more centralized as tech and service industries grow (think of the call centers in India), and these work opportunities in turn drive people en masse from rural to urban settings.
In urban settings, food production can be concentrated and take advantage of economies of scale, leading to lower prices and further encouraging people to eat outside the home. Urban settings in developing countries also commonly have few opportunities for physical activity. As more women begin to enter the workforce—a possibility encouraged by technological advance—they face greater time constraints for the household production of food, and this reduction of time also acts to move food consumption away from the home. Because of the market structure and incentives just described, the net effect on society is a greater consumption of unhealthy products, especially energy-dense foods, and increasingly sedentary behavior.
In sum, economic flows have improved the accessibility of behavioral risks; the social changes accompanying economic growth have encouraged their adoption; and technological change has created incentives for people to exercise less and eat out more. All these forces join to heighten the developing country's population's risk of chronic diseases. I have concluded that the following five factors are contributing to the rising risk of chronic disease and mortality in the developing world:
Globalization is leading to greater intercountry dietary dependence.
Foreign direct investment in foods and beverages in developing economies favors less healthy products.
Transnational companies' marketing strategies influence persons in poor countries to prefer Western products as their income rises.
Technological change speeds up all these processes.
Technological change also encourages more inactive lifestyles and shifts the locus of food consumption away from the home.
In the developed world today, however, higher country-income levels, more foreign direct investment, and greater urbanization relate favorably to chronic diseases, and thus can be expected to be associated with lower mortality rates of chronic diseases.
A Simple Model of the Effects of Globalization on Chronic Disease Mortality
To illustrate these effects on chronic diseases more formally and how they differ across rich and poor countries, I offer a simple comparative analysis using correlations and multivariate regression. Before proceeding, however, I must mention some significant methodological challenges in the empirical analysis. Some longitudinal chronic disease data in poor countries lacking vital registration data are not directly observed but are instead constructed by applying model life tables and demographic methods that correct for underregistration (Lopez 2005). This construction renders the data imperfectly comparable across different levels of country development but makes them suitable for analysis within countries and income regions. Because fine-grained historical chronic disease data were not available for several countries and regions, I also used the WHO type 2 chronic noncommunicable diseases cluster and one of the four leading chronic diseases, heart disease, as indicators of trends in the leading chronic diseases. The overlap between these two categories provides a stronger test of the relationships between the macrosocial and macroeconomic factors and chronic diseases than would be provided if they were made mutually exclusive as CVD and non-CVD chronic noncommunicable diseases. This categorization also reveals the extent to which the drivers of population heart disease intersect with the drivers of the WHO type 2 chronic noncommunicable diseases more generally. Nonetheless, the results were found to be similar when excluding heart disease from the chronic noncommunicable disease category, and the correlations between the non-CVD chronic noncommunicable disease category and the WHO type 2 chronic noncommunicable disease category were strong in all income regions. Appendix 2 describes the technical methods used to cope with further data limitations, such as changes in the International Classification of Disease codes.
First, using a set of poor, middle, and rich countries, determined by the tertiles of the average gross domestic product per capita from 1960 to 2000 and using World Health Organization Global Mortality data, I correlate logged country per capita income levels with logged male cardiovascular and chronic noncommunicable disease mortality rates. The patterns are clear: greater per capita income is associated with a higher rate of chronic noncommunicable diseases in poor countries, and the relationship appears to worsen linearly for poor countries compared with middle and rich countries. For rich countries, the direction reverses, so that greater income levels are associated with lower rates of male heart disease and chronic noncommunicable diseases (see figure 3).
Figure 3.
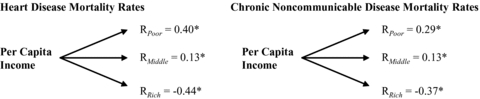
Associations between Country-Income Levels per Capita and Log Heart Disease and Chronic Noncommunicable Disease Mortality Rates
Notes: Poor countries < US$3,000 per capita income, middle countries > $3,000 and < $7,000, and rich countries > $7,000 on average from 1960 to 2002. Male mortality rate data are from the WHO Global Mortality Database and are in logs. Chronic noncommunicable disease is WHO's type 2 burden of disease category. Economic data are from the World Bank's World Development Indicators, 2005 ed., and the International Monetary Fund's International Financial Statistics, 2007 series. Per capita income is based on gross domestic product (GDP) per capita. Cross-country data are de-trended for effects of changing ICD classifications. Appendix 2 describes all data and presents descriptive statistics.
Significance at *p < 0.01.
The key aspects of economic globalization identified earlier (levels of market integration and foreign direct investment) and urbanization (the main social change discussed) reveal patterns similar to that for income levels. Urbanization is linked to higher mortality rates for heart disease and chronic noncommunicable disease in poor countries, but lower mortality rates in middle and rich countries. Market integration follows the same pattern, except that it has no significant association in middle-income countries. Foreign direct investment correlates with higher cardiovascular and chronic noncommunicable disease mortality rates in poor countries, lower chronic disease mortality rates in middle-income countries, and even lower cardiovascular and chronic disease mortality rates in rich countries. This accords with the analysis that the effects of foreign direct investment, market integration, and urbanization on chronic diseases qualitatively differ by levels of country development (see figure 4).
Figure 4.
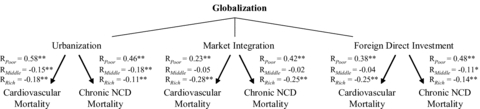
Associations between Globalization and Log Heart Disease and Chronic Noncommunicable Disease Mortality Rates
Notes: Poor countries < US$3,000 per capita income, middle countries >$3,000 and <$7,000, and rich countries >$7,000 on average from 1960 to 2002. Male mortality rate data are from the WHO Global Mortality Database and are in logs. Chronic NCD is chronic noncommunicable disease mortality based on WHO's type-2 burden of disease category. Economic data are from the World Bank's World Development Indicators, 2005 ed., and the International Monetary Fund International Financial Statistics 2007 series. Urbanization is the percentage of population living in urban settings. Market integration is total capital flows as a percentage of GDP. Foreign direct investment is the log level of foreign direct investment inflows. Cross-country data are de-trended for effects of changing ICD classifications. Appendix 2 describes all data and presents descriptive statistics.
*p < 0.05, **p < 0.01.
What does this mean for developing countries in the future? To find out, I offer some multivariate regression models of how these factors have historically related to chronic disease trends in high-income countries, where the burden of chronic disease has fully matured. More specifically, since some chronic diseases have a decadal lag time between the exposure to risk and the development of chronic disease, I focus on high-income countries to determine how exposures to populations twenty years ago have shaped their current chronic disease burden, in order to understand the consequences for developing countries today.
Table 5 shows that historically, greater growth, foreign direct investment, market integration, and urbanization all have fueled a significant part of the rises in the mortality rates of heart disease and chronic noncommunicable disease. For example, each 1 percent increase in the population living in urban settings has increased the long-term growth of chronic noncommunicable disease in the population by 3.2 percent. By comparison, from 1960 to 1980, mortality rates of chronic noncommunicable disease grew by an average of 9.8 percent in this sample of rich OECD countries, clearly a sizable effect.
TABLE 5.
Twenty-Year Long Difference Models of Chronic Noncommunicable Diseases from 1960 to 2000, High-Income Countries
| Covariate | Change in Heart Disease Mortality Rate over 20-Year Span | Change in Chronic NCD Mortality Rate over 20-Year Span |
|---|---|---|
| Change in log GDP per capita | 0.11%** | 0.05%** |
| (0.02) | (0.18) | |
| Change in log FDI | 0.03%** | 0.02%** |
| (0.01) | (0.01) | |
| Change in market integration | 0.45%** | 0.60%** |
| (0.13) | (0.11) | |
| Change in urbanization | 1.41% | 3.20%** |
| (0.74) | (0.53) | |
| Change in population age dependency | 2.09%** | 3.93%** |
| (0.54) | (0.33) | |
| Average CD growth, 1960–1980* | 3.58% | 9.79% |
| R2 | 0.26 | 0.59 |
Notes: Robust standard errors are in parentheses.
The average rate of growth for chronic noncommunicable diseases (CNCD) from 1960 to 1980 was 0.94%. By comparison, the average rate of growth projected for leading chronic disease mortality rates in high-income countries is 0.50%; for East Asia and Pacific, 1.58%; and for Latin America, 1.51% (see table 2). The coefficients are transformed such that each 1 percent increase in the explanatory variable to correspond to the specified percentage increase in the dependent variable (elasticity). Chronic noncommunicable disease is the WHO type 2 NCD category. Economic growth is the percentage change in real GDP per capita. Urbanization is the change in the percentage of the population living in urban settings. Market integration is the change in total capital flows as a percentage of GDP. FDI is the change in the log of foreign direct investment inflow levels. Population aging is the change in the percentage of the population over age sixty-five. Countries include fifteen high-income OECD countries for which twenty-year comparative data from the WHO Global Mortality Database are available. Data de-trended using period effects to adjust for changing ICD classifications and secular trends from 1960 to 2000. Appendix 2 further describes the empirical sample and modeling strategy and offers definitions and descriptive statistics for all variables.
Significance at p < 0.01.
The model supports the common explanation of this growth in chronic disease—that the population's aging is the primary driver—but not nearly to the extent that has been emphasized in the literature. The aging of a population, as measured by the change in the population's age dependency (or the percentage of the population over age sixty-five), was linked to increases in changes in the mortality rates of both heart disease and chronic noncommunicable disease. Compared with the changes in economic growth, however, these effects accounted for only a fraction of the total changes in the mortality rate of chronic noncommunicable disease and less than one-fifth the effect on those for heart disease as did the changes in GDP per capita (for a decomposition of these effects, see table 6). In fact, only the aging of the population was more powerful for heart disease than urbanization and market integration. Overall, the population's aging explained 10 percent of the changes in mortality rates for heart disease and 25 percent for chronic noncommunicable disease, and the rest was attributed to macrosocial and macroeconomic factors (for more details, see appendix 2). Although my analyses are somewhat simplified because they look only at the population younger and older than sixty-five, the results here indicate that the notion that the growth of chronic diseases in a population is simply the inevitable consequence of aging is overstated—and historically false.
TABLE 6.
Decomposition of Population Aging and Socioeconomic Effects on Chronic Noncommunicable Diseases, High-Income Countries
| Covariate | Average Change (%) | Estimated Effect on Heart Disease Mortality over 20-Year Span (%) | Estimated Effect on Chronic NCD Mortality over 20-Year Span (%) |
|---|---|---|---|
| Economic growth | 249.05 | 26.51 | 12.13 |
| Foreign direct investment | 253.39 | 8.19 | 4.20 |
| Market integration | 9.87 | 4.40 | 5.93 |
| Urbanization | 1.86 | 2.63 | 5.96 |
| Population aging | 2.38 | 4.97 | 9.38 |
Notes: Estimated effects are given by the formula  *β, where X is the determinant and β=ΔCD/ΔX. Model parameters are based on the regression coefficients presented in table 5.
*β, where X is the determinant and β=ΔCD/ΔX. Model parameters are based on the regression coefficients presented in table 5.
Chronic noncommunicable disease is WHO's type 2 NCD category. Economic growth is the percentage change in real GDP per capita. Urbanization is the change in the percentage of the population living in urban settings. Market integration is the change in total capital flows as a percentage of GDP. FDI is the percentage change in foreign direct investment levels. Population aging is the change in the percentage of the population over age sixty-five. Appendix 2 further describes the empirical sample and modeling strategy and presents definitions and descriptive statistics for all variables. Appendix 2 also presents alternative estimates based on partial correlations and standardized regression coefficients, with decomposition results similar in magnitude.
Now we finally can clarify what will happen in the coming years.
Long-Term Epidemiologic and Economic Consequences of Rising Chronic Diseases
Chronic Diseases Will Further Widen the Health Gap between Rich and Poor Countries
Since the incidence of chronic diseases is growing faster in low- and middle-income countries, their impact will widen the health gap between the global North and South. From 2002 to 2030, mortality rates for chronic disease will rise by 15 percent in high-income countries and by 22 percent in low- and middle-income countries. As shown earlier using standardized mortality rate ratios (table 4), the mortality will hit working-age populations much harder in poorer than in richer countries.
Chronic Diseases Are Killing and Disabling People at Their Peak Productivity
It is often argued that infectious diseases in Africa have caused a “poverty trap.” Because so many working-age people are dying, the workforce is unable to push Africa's economy forward. In turn, so many people are dying because there are not enough resources to combat the epidemics.
Why have diseases like AIDS hurt Africa's growth so much? First, once acquired, HIV/AIDS cannot easily be clinically reversed and leads to long-term suffering on the road to a painful death. Second, this disease costs the health system a lot of money. Third, left unchecked, it can spread at an alarming pace, as the population's exposure to risks grows.
All these burdens apply to other chronic diseases as well (see appendix 1). The global data show that the question is not whether infectious diseases will overtake chronic diseases but when. The concern is that in the coming years, just as AIDS is being conquered and given the costly similarities between AIDS and chronic diseases, the AIDS poverty trap will simply morph into a chronic disease poverty trap.
Chronic Diseases Will Slow Countries' Economic Growth Rates
Consider the economic impacts of heart disease in working-age men today in OECD countries. As before, understanding the historical impact of chronic diseases on the economies of developed countries provides insight into what the potential economic impact on developing countries will be once the chronic diseases risks prevalent today are manifested as rising chronic disease morbidity and mortality rates. Applying the experiences of rich countries to illuminate trends in poor countries can further be justified because poor countries are about a decade behind rich ones in the evolution of their chronic disease burden (WHO 2005; Yach et al. 2004).
Table 7 shows the results of a neoclassical growth model, augmented with the working-age population's mortality rates for chronic noncommunicable diseases. Each 1 percent increase in these rates is associated with a −0.05 percent decline in economic growth. These results are consistent with previous economic models (see Suhrcke and Urban 2006) and a large set of studies linking chronic noncommunicable diseases to high micro- and macroeconomic costs (Leeder et al. 2004; Suhrcke et al. 2006; WB 1993, 2007; WHO 2005; Yach, Stuckler, and Brownell 2006). Extending this model to low-income countries suggests that a 50 percent rise in chronic diseases—the amount expected in Latin America from 2002 to 2030—will result in more than a 2 percent slowdown in economic growth each year. This is indeed a large effect: by comparison, the United States' economy grows an average of about 2 percent every year.6 Again, since the rises in chronic diseases will be concentrated in poor countries, it follows that chronic diseases are contributing to an economic divergence between the global North and South.
TABLE 7.
Effect of Chronic Noncommunicable Disease Working-Age Mortality on Economic Growth, 1960–2002
| Dependent Variable: Percentage Annual Change in Real GDP per Capita | |
|---|---|
| Covariate | Fixed-Effects Model |
| Log chronic noncommunicable disease working-age mortality rates | −4.67 (1.63)* |
| Log inflation | −0.74 (0.49)* |
| Openness | 0.06 (0.02)* |
| Secondary education levels | 0.03 (0.04) |
| Savings rate | 0.07 (0.05) |
| Number of country years | 758 |
| Number of countries | 23 |
Notes: Robust standard errors are in parentheses, clustered by country to reflect nonindependence of sampling and for robustness to serial correlation. Models include country- and time-fixed effects. Appendix 2 presents definitions and descriptive statistics for all variables. High-income OECD countries included in the sample are Australia, Austria, Belgium, Canada, Denmark, Finland, France, Germany, Greece, Ireland, Iceland, Italy, Japan, Mexico, Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, Switzerland, United Kingdom, and United States.
Significance at p < 0.01.
Source: GDP growth data are from the Penn World Tables, vol. 6.2.
The Way Forward
Emerging from this analysis is a clear, long-term picture of the proliferation of chronic diseases and rising economic burdens concentrated in poor countries, and also of an inadequate response to the need for control by individuals, markets, and global players. The global challenge faced by WHO and other major international players is how to act in concert to tackle the rising rate of chronic diseases without discouraging equitable and sustainable economic development.
One obvious solution is a coordinated approach to combating infectious and chronic diseases, that is, to build the capacity of health systems while transforming the systems from acute to chronic care. As recent studies have shown, AIDS treatment in resource-poor settings is failing owing to poor adherence (see Rosen, Fox, and Gill 2007). What the studies do not mention is that AIDS is a chronic disease. That AIDS is one of the few infectious diseases that are on the rise reflects the same limitations fueling the unchecked growth of chronic diseases in poor countries today. Yet learning and sharing regarding the control of AIDS-CVD-diabetes is not taking place, and a tremendous opportunity for enabling health systems to address long-term population health care problems is lost as billions of dollars are spent controlling AIDS and TB.7
The priorities of populations, not just the priorities of donors, should be emphasized. In the past several decades, national health ministries have raised more than forty resolutions at the WHO World Health Assembly to develop stronger systems for combating chronic diseases. Heeding these national calls for global change would bring the world's health closer to what it aspires to be: an equitable practice, committed to the egalitarian principles espoused by WHO's Health for All population health approach, originally outlined in the Declaration of the Alma-Ata (WHO 1978; also see recent calls by the WHO Commission on the Social Determinants of Health to return to the Alma Ata principles 2008) and subsequently at the first international conference of health promotion in the Ottawa Charter (WHO 1986).
The reality is that despite the very clear economic and epidemiologic effects of chronic diseases and their inequitable global distribution, little or no action will be forthcoming in the next few years. The control of infectious disease will remain the priority and given the current forecasts of a drop in its rate around the world under the baseline scenario, this will probably be heralded as a great success of the global health triumvirate: WHO, the World Bank, and the Bill and Melinda Gates Foundation. The Millennium Development Goals (MDGs)—the United Nations' social development agenda for “reducing poverty and improving lives”—do not compare actual declines against baseline expected drops. Without any intervention, the global health MDG 6 will be met: “to halt and begin to reverse the spread of infectious diseases (HIV/AIDS, malaria, and other diseases)” (for early signs of achieving MDG 6 well before the target date, see WHO 2008). But the die has been cast, and the patterns have been set: the overwhelming focus on infectious diseases will have only a marginal impact, which will be exchanged for the greater number of losses due to chronic diseases. The scenarios described here under the “baseline case” correspond to where we are today and will be tomorrow: “the no-action case.”8
What is to be done?
First, it is understandably very difficult for public health practitioners to engage the global drivers of chronic diseases, particularly when transnational corporations play a leading role in the process. There is thus a critical need to engage with some parts of the private sector and to overcome the “anticorporate” culture that exists in public health today (owing much to a better understanding of the activities of tobacco companies) (Wiist 2006). Public health has an important role to play in convincing corporations to expand healthy product lines and can help as “health investment advisers” to show the economic benefits of doing so. Likewise, public health can learn from the private sector, and their collaboration could yield significant gains in the effectiveness of public health.
Second, interactions with ministers of finance are necessary in order to align economic growth policy with health policy. Economic development need not lead to chronic disease. While the way to bring about such interactions may seem unclear and foreign to many, the economic growth analysis provided here explains how to proceed on this front. Model parameters, such as the one provided here for a neoclassical growth model, can be replicated in each country to identify what the effects will be on national economies in the scenarios of low-, medium-, and high-chronic disease growth, which is the strategy recommended by the British Wanless report for shifting treasury funding (Wanless 2002, 2004). More generally, there is a need for public health to look at how chronic disease relates to a range of social and economic dependent variables as a strategy for engaging non-health sectors. This would be relatively easy to do and may in the long run result in greater population health gains than the plethora of studies within the field that further characterize the relationships between individual risk factors and chronic diseases.
Next, NGOs must fill the donor gap. Donors will not be interested until they are rewarded by the public for their positive involvement, mainly owing to the political economy failures outlined in table 3. Evidence redressing pervasive chronic disease myths, such as that they are “inevitable consequences of aging” or “diseases of affluence,” must be more widely disseminated (WHO 2005). Some groups, such as the Oxford Health Alliance, are pushing in positive directions and beginning to mobilize and integrate fragmented chronic noncommunicable disease interest groups. But clearly, much more needs to be done.
While numerous cost-effective interventions for chronic diseases have been tested and are available (Suhrcke et al. 2006; WB 2007), we still need a road map of appropriate interventions based on the population- and individual-causes of chronic diseases, from which a coherent prevention plan can be constructed. At the broadest level, the road map could begin with economic, political, and social factors, and at the narrowest level, it might begin with psychological and biological factors that affect eating and activity. In the case of eating, these would be taste, accessibility, convenience, cost, and the amount of promotion. The factors lying between the broad and narrow factors must be defined so that prevention can be based on estimates of the most powerful point at which to intervene in the causal chain at different stages of chronic disease progression (Yach, Stuckler, and Brownell 2006, see figure 2).
The academy can be of great help in all these processes, but currently it is not doing enough. The evidence that upstream forces are driving chronic diseases, as outlined here, is quite clear and robust. Genetics or biomedical factors alone cannot independently explain any of the rises in populations' chronic diseases. Yet almost all the scant academic resources today are being devoted to genetic research, mainly driven by the pharmaceutical sector, with the hope of creating ways to cure obesity and other afflictions. As a result, this individual biomedical paradigm is being reproduced in public health and medical classrooms worldwide.
What is desperately needed—and long overdue in the academic world—is cross-disciplinary collaboration with economists, sociologists, and political scientists to understand the social transformations at the population levels that are driving chronic diseases and to develop feasible and effective strategies to reverse them. Until then, the chronic disease prevention road map will implicitly remain fixated on the narrow set of biomedical factors.
Reversing chronic disease growth will therefore require “intersectoral action”—that hot WHO buzzword, whose meaning no one knows, nor how to bring it about. Simply put, intersectoral action is coherent action. The way to start is to change the way we think, the way we do research, and the way we are trained in public health and medicine. Only then will the urgently needed changes be put in motion, and public health, by transforming itself into a science of population health, will be able to lay claim to a significant cause-and-effect in its own relationship to chronic disease prevention and control.
Acknowledgments
I would like to thank Andrea Bertola and Marc Suhrcke at the World Health Organization Venice Office for providing the global chronic disease longitudinal mortality rate data. I am particularly grateful to Martin McKee for valuable comments on various drafts as well as helpful epidemiologic and editorial advice in the preparation of this article. Derek Yach, Corinna Hawkes, Sanjay Basu, and Karen Siegel offered important suggestions on different versions of this paper. Thanks are also to Christopher Meissner for insights on the economic growth models and regression decompositions. Lastly, I appreciate the constructive feedback from the editor and three anonymous reviewers.
Appendix 1 Data and Methods
Burden of Disease Projection Calculations
Chronic disease projection data are based on the forecasts generated by Mathers and Loncar in association with the WHO Global Burden of Disease project (PLoSMed November 2006, 3 (11):2011–30). Regression equations followed the original Global Burden of Disease cross-national specification:
| (1) |
Here a is age group, k is sex, and i is cause of death. γ is GDP per capita, M is the mortality level, HC is human capital, SI is an index of smoking impact, and t is a linear time trend. Model parameters were estimated using ordinary least squares regression separately for each age-sex-cause group for 106 countries for death data from 1950 to 2002. The population levels used to determine mortality rates were taken from the UN's fertility rate projections (UN 2005).
Despite the high levels of uncertainty associated with these models, their results have important public policy implications (Murray and Lopez 1997).
Chronic Noncommunicable Disease and Chronic Disease Categories
Figure 1 and tables 1 and 2 in the text present the total mortality rate for infectious and chronic diseases. Infectious disease is based on the WHO type 1 infectious disease (ID) category, which includes infectious and parasitic diseases, respiratory infections, maternal conditions, perinatal conditions, and nutritional deficiencies. Chronic disease is based on a subset of the WHO type 2 noncommunicable disease (NCD) category, which includes cardiovascular disease, malignant neoplasms, respiratory disease, and diabetes mellitus. As table A1 shows, these four categories account for more than 80 percent of all NCD mortality and 40 percent of NCD morbidity. They also have the highest percentage mortality/percentage morbidity ratio of the chronic noncommunicable subcategories apart from the other neoplasms category (all greater than 1.2).
TABLE A1.
Morbidity and Mortality Rates for Chronic Noncommunicable Diseases
| Chronic Noncommunicable Diseases | Percentage Mortality | Percentage DALYs |
|---|---|---|
| Cardiovascular disease | ||
| Rheumatic heart disease, hypertensive heart disease, ischemic heart disease, cerebrovascular disease, inflammatory heart disease | 49.90 | 21.23 |
| Malignant neoplasms | ||
| Mouth and oropharynx cancers; esophagus cancer; stomach cancer; colon and rectum cancers; liver cancer; pancreas cancer; trachea, bronchus, lung cancers; melanoma and other skin cancers; breast cancer, cervix uteri cancer; corpus uteri cancer; ovary cancer; prostate cancer; bladder cancer; lymphomas; multiple myeloma; leukemia | 21.23 | 10.83 |
| Respiratory diseases | ||
| Chronic obstructive pulmonary disease, asthma | 11.04 | 7.90 |
| Digestive diseases | ||
| Peptic ulcer disease, cirrhosis of the liver, appendicitis | 5.87 | 6.66 |
| Neuropsychiatric conditions | ||
| Unipolar depressive disorders, bipolar disorder, schizophrenia, epilepsy, alcohol use disorders, Alzheimer's and other dementias, Parkinson disease, multiple sclerosis, drug use disorders, posttraumatic stress disorder, obsessive-compulsive disorder, panic disorder, insomnia, migraine, lead-caused mental retardation | 3.32 | 27.70 |
| Diabetes mellitus | 2.95 | 2.32 |
| Genitourinary diseases | ||
| Nephritis and nephrosis, benign prostatic hypertrophy | 2.53 | 2.18 |
| Endocrine disorders | 0.72 | 1.14 |
| Other neoplasms | 0.44 | 0.25 |
| Musculoskeletal diseases | ||
| Rheumatoid arthritis, osteoarthritis, gout, low back pain | 0.32 | 4.32 |
| Skin diseases | 0.21 | 0.54 |
| Congenital anomalies | ||
| Abdominal wall defect, anencephaly, anorectal atresia, cleft lip, cleft palate, esophageal atresia, renal agenesis, Down syndrome, congenital heart anomalies, spina bifida | 0.15 | 3.92 |
| Sense organ diseases | ||
| Glaucoma, cataracts, age-related vision disorders, adult-onset hearing loss | 0.01 | 9.94 |
| Oral conditions | ||
| Dental caries, periodontal disease, edentulism | 0.01 | 1.06 |
| Total leading chronic disease: CVD, DM, COPD, cancer | 85.12 | 42.29 |
Source: Author's calculations, based on World Health Report 2004 and Global Burden of Disease Statistics, World Health Organization.
Notes: CVD is cardiovascular disease; DM is diabetes mellitus; COPD is chronic obstructive pulmonary disease; and cancer is malignant neoplasms.
Placing diseases into broad categories is complicated (for details, see Nolte and McKee 2008). For example, the terms infectious and chronic are very often juxtaposed, even though they are on different dimensions. Thus, diseases can be either infectious or noninfectious and chronic or acute (see table A2). Conforming with common usage and in the interests of brevity, I use chronic in this article as shorthand for chronic noninfectious diseases. Infectious encompasses acute and chronic diseases with an infectious etiology. Another cell, acute noninfectious disease, is dominated by injuries and violence but is not considered here. Furthermore, in practice the divisions are much more complex. To illustrate this, consider type 1 diabetes, a disease that we know originates when a virus infects a genetically predisposed individual. The diabetes disease process is clearly noncommunicable (the virus has done the damage and cleared the body), but some of the long-term complications, such as skin ulcers, are clearly infectious. Another example is AIDS. The disease is clearly infectious but gives rise to disease processes, such as Kaposi's sarcoma, that are noninfectious. Added to this, long-term antiretrovirals greatly increase the risk of cardiovascular disease. There is no satisfactory terminology, and whatever is used, it is possible to argue that there are exceptions. I thank an anonymous reviewer and Martin McKee for raising this important point.
TABLE A2.
Characteristics of Acute and Chronic Diseases
| Characteristic | Acute Diseases | Chronic Diseases |
|---|---|---|
| Onset | Rapid | Gradual |
| Duration | Short term | Long term |
| Causation | Isolable agent causation | Multivariate causation |
| Diagnostic and prognostic accuracy | High | Low |
| Treatment modality | Curative | Palliative |
| Therapeutic options | Specific; self-limited | Multiple; undulating course |
| Medical technology | Less invasive; highly effective | More invasive; high toxicity |
| Level of uncertainty | Low | High |
| Professional-patient relationship | Asymmetric: physician highly knowledgeable, patient inexperienced | More symmetric: physician and patient equally knowledgeable |
Source: Adapted from Stuckler, Hawkes, and Yach 2008.
I calculated the average annual percentage change (or the growth rate) by solving the formula for the growth rate r for each income region and for each disease type:
| (2) |
Income categories are based on the World Bank's 2003 World Development Indicators report, which Mathers and Loncar used for their forecasts (2006). Countries are stratified into groups according to 2001 GNI per capita, calculated using the World Bank Atlas method: low income, US $745 or less; middle income, $746 to $9,205; and high income, $9,206 or more. Using the WHO data, I replicated these calculations for disability-adjusted life years (DALYs) rates in figure A1 and table A3. Figure A1 and table A3 show that in all countries disability rates of infectious disease are projected to fall, whereas disability rates of chronic diseases are projected to rise except in high- and upper-middle-income countries.
TABLE A3.
Growth Rate in Infectious and Chronic Disease Disability-Adjusted Life Years (% per year), 2002 to 2030
| Region | Infectious Diseases | Chronic Diseases |
|---|---|---|
| World | −1.83 | 0.15 |
| High income | −2.57 | −0.45 |
| East Asia and Pacific | −2.85 | 0.65 |
| Eastern Europe and Central Asia | −0.49 | −0.57 |
| South Asia | −3.36 | 0.33 |
| Latin America | −2.92 | 0.59 |
| Middle East and North Africa | −3.04 | 0.29 |
| Sub-Saharan Africa | −1.94 | 0.25 |
Sources: Author's calculations. Data and region categories are based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections. Infectious diseases classification is based on WHO's type 1 burden of disease cluster. Chronic diseases classification is based on cardiovascular disease, cancers, respiratory disease, and diabetes mellitus subcategories of WHO's type 2 burden of disease cluster.
Figure A1.
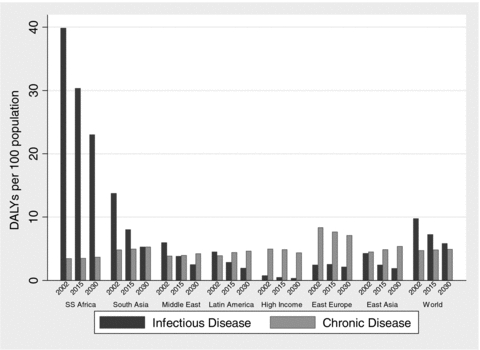
Evolution of the Global Burden of Disease, 2002 to 2030
Notes: DALYs are disability-adjusted life years. Infectious disease classification is based on WHO's type 1 burden of disease cluster. Chronic disease classification is based on cardiovascular disease, cancers, respiratory disease, and diabetes mellitus subcategories of WHO's type 2 burden of disease cluster.
Source: Author's calculations based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections.
Tables also have been replicated using mortality numbers, which follow a pattern similar to that of mortality rates, as seen in table A4.
TABLE A4.
Growth Rate in Infectious and Chronic Disease Mortality Levels (% per year), 2002 to 2030
| Region | Infectious Diseases | Chronic Diseases |
|---|---|---|
| World | −0.60 | 1.58 |
| High income | −0.27 | 0.67 |
| Eastern Europe and Central Asia | −0.01 | −0.16 |
| East Asia and Pacific | −1.43 | 2.01 |
| South Asia | −1.78 | 2.10 |
| Latin America | −1.01 | 2.30 |
| Middle East and North Africa | −0.90 | 2.47 |
| Sub-Saharan Africa | 0.27 | 2.48 |
Sources: Author's calculations. Data and region categories are based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections. Infectious diseases classification is based on WHO's type 1 burden of disease cluster. Chronic diseases classification is based on cardiovascular disease, cancers, respiratory disease, and diabetes mellitus subcategories of WHO's type 2 burden of disease cluster.
Standardized Mortality Rate Ratio
I used the WHO Global Burden of Disease 2002 update statistics (available on the Web at http://www.who.int/healthinfo/bod/en/index.html) to calculate mortality rate ratios in each age band for low- versus high-income countries. The formula is simply
where a is the age group and low and high refer to high- and low-income countries.
In all age groups, the mortality rate is higher in poor countries than in rich countries; overall the probability is higher that persons in poor countries will die at a younger age from chronic disease than persons in rich countries.
Chronic Disease Morbidity-to-Mortality Ratios
Table A5 indicates that the morbidity/mortality ratios for chronic diseases are higher in poor countries than in rich countries and that this gap is widening over time.
TABLE A5.
Morbidity-to-Mortality Ratio of Chronic Disease
| DALY/MR Ratio | |||
|---|---|---|---|
| Region | 2002 | 2015 | 2030 |
| World | 10.38 | 9.62 | 8.88 |
| High income | 8.09 | 7.26 | 6.37 |
| Eastern Europe and Central Asia | 8.91 | 7.63 | 7.19 |
| East Asia and Pacific | 10.20 | 9.26 | 8.04 |
| South Asia | 12.60 | 11.73 | 10.81 |
| Latin America | 11.69 | 10.81 | 9.33 |
| Middle East and North Africa | 12.76 | 12.03 | 10.80 |
| Sub-Saharan Africa | 12.87 | 12.38 | 12.32 |
Note: DALY/mortality ratio calculated as total DALYs/total mortality, which is equivalent to population DALY rates/mortality rates when population units are the same.
Chronic diseases are classified according to a restricted definition of WHO's type 2 NCD category. Appendix 1 details the inclusion criteria for the chronic disease category.
The DALY (disability-adjusted life year)/mortality ratio presented here can also be viewed as a measure of the compression of morbidity (Fries 1983). Thus, the data here suggest that morbidity is much more compressed in rich countries and that the compression of chronic disease morbidity is occurring faster in rich than in poor countries.
WHO Projection Decomposition and Population Aging
Mathers and Loncar (2006) decomposed the total change in deaths from 2002 to 2030 into two components: epidemiologic change and demographic change.
The total projected change in the number of deaths between 2002 and 2030 would be
where
Mathers and Loncar argue that demographic change and epidemiologic change can be calculated as follows:
We calculated the expected number of deaths in 2030 given the 2030 projected age-specific rates under the baseline scenario and the 2002 population. The difference between this and the 2002 mortality estimates is a measure of the change in mortality expected solely on the basis of changing age-specific mortality rates, and is labeled “epidemiological change.” (2006, p. 2019)
Second, we calculated the expected number of deaths in 2030 by taking the 2002 age-specific death rates and applying them to the 2030 projected population. The difference between this and the 2002 mortality estimates is the measure of the change in mortality expected solely on the basis of changing demography (including size and age composition of the population) (2006, p. 2019).
The authors then concluded that “the total projected change in the number of deaths between 2002 and 2030 is the sum of [demographic change] and epidemiological change components” (2006, p. 2020).
The logic is appealing: hold the mortality rates constant and change the population to determine mortality-attributable demographic change. Similarly, hold the population's composition and size constant and change the mortality rates to determine the mortality attributable epidemiologic change.
But the identity:
 |
or simplifying the right-hand side:
does not hold.A1
Another methodological issue is that demographic change is defined by these studies as the remainder from the total forecast change in deaths minus the mortality changes attributable to changes in age-specific mortality rates. But the explanatory variables in equation 1 that are used to capture changes in age-specific mortality rates do not include the chronic disease–promoting factors identified here (only a proxy for smoking) and, in so doing, falsely attribute these omitted variables to demographic change. This is a common regression misspecification issue, although the forecasts are not affected.
From a policy perspective, it is misleading to decompose epidemiologic and demographic change as though the former were tractable and the latter intractable. Mathers and Loncar point out that the two components appear to have orthogonal effects on the burden of disease, but this is virtually by construction of the forecasts. It would be expected a priori that demographic changes, particularly for chronic diseases, would give rise to a greater burden of disease, whereas epidemiologic changes would trend downward, since the trend of secular declines in mortality rates in association with country development has been recognized since the theory of epidemiologic transition (Omran 1971).
Such a determination can have important policy implications, for if chronic diseases are driven principally by population aging, as the WHO models imply, there will be little rationale for intervention (see WB 2007; WHO 2006). The World Bank notes that “an overemphasis on aging … could result in a mistaken belief that policy cannot make a difference” (WB 2007, p. xxiv). However, as a sampling, several scholars note that “age is the single most important determinant of mortality” with regard to diabetes (Roglic and Unwin 2005, p. 34); the WHO Burden of Disease Project notes that the “ageing of the population will result in significantly increasing total deaths due to [NCDs] over the next thirty years” (Mathers and Loncar 2006, p. 65). Strong, Mathers, and Bonita note that “these countries have experienced a rise in the burden of chronic diseases, to almost 50 percent of total disease burden over the past decade. This increase can be attributed to population ageing and [risk factors]” (2007, p. 182). Mathers and Loncar state,
In almost all cases, demographic and epidemiological factors are operating in opposing directions in determining mortality in 2030…. Although age-specific death rates for most Group II conditions are projected to decline, aging of the population will result in significantly increasing total deaths due to most Group II conditions over the next 30 years. (2006, p. 2020)
Finally Marks and McQueen observe that the “aging of the population in the first quarter of the twenty-first century will be the major force in the further tremendous increase in the burden of chronic diseases” (2002, p. 119, italics added).
Age-Specific, Age-Standardized, and Age-Unadjusted Mortality Rates and Public Policy
Should global health policy be dictated by within-age-group trends, age-standardized trends, or overall population trends? The total unadjusted mortality rates shown in tables 1 and 2 in the text reflect the actual burden of disease and, as a result, the actual consequences of chronic diseases on human lives and economies and their dynamics over time. While within-age-group trends can be important to identifying epidemics and sudden breaks, the theory of epidemiologic transition has long demonstrated that the within-age-group rates usually decline with development (Omran 1971). (According to the WHO projections, as within-age-group mortality rates are projected to fall, even tuberculosis and malaria appear to be inevitable consequences of aging and demographic changes in a population.) Within-age-group trends can be better applied to policy in the comparative perspective by answering such questions as why within-age-group morbidity and mortality rates are declining faster (or, conversely, remaining steady) in some countries, diseases, and age groups than in others.
Tables A6 and A7 give age-disaggregated versions of tables 1 and 2 in the text using the WHO projections for four age groups: 5 to 14, 15 to 59, 60 to 69, and 70 and older. As shown in table A6, age-standardized mortality rates are generally expected to decline worldwide, with the exception of sub-Saharan Africa, where chronic disease rates are projected to rise for ages fifteen and older. The results in table A7 differ comparatively from those of table A6 because the growth rate, r, needed to achieve the difference depends on the principal, or the initial mortality level. This table is based on table 2 in the text, that within age clusters, chronic diseases are declining at a slower rate than infectious diseases are.
TABLE A6.
Expected Change in Mortality Rates of Infectious and Chronic Diseases per 100,000 Population from 2002 to 2030, by Age Group
| Infectious Diseases | Chronic Diseases | |||||||
|---|---|---|---|---|---|---|---|---|
| Region | ||||||||
| 5–14 | 15–59 | 60–69 | 70+ | 5–14 | 15–59 | 60–69 | 70+ | |
| World | −35.99 | 15.33 | −145.91 | −347.26 | −3.18 | −8.64 | −409.75 | −608.28 |
| High income | −0.60 | −4.16 | −28.87 | −147.90 | −1.79 | −36.79 | −359.63 | −791.06 |
| Eastern Europe and Central Asia | −1.87 | 44.58 | −17.80 | −38.10 | −3.00 | −69.76 | −937.50 | −1008.99 |
| East Asia and Pacific | −14.05 | 11.01 | −153.20 | −401.59 | −3.07 | −3.36 | −491.94 | −792.69 |
| South Asia | −75.66 | −44.53 | −390.59 | −977.20 | −5.33 | −1.41 | −306.06 | −228.98 |
| Latin America | −7.81 | 1.00 | −107.40 | −475.73 | −3.19 | 3.71 | −315.80 | −498.89 |
| Middle East and North Africa | −12.14 | 14.02 | −101.36 | −333.86 | −5.09 | 0.13 | −505.91 | −580.88 |
| Sub-Saharan Africa | −116.24 | −177.60 | −172.39 | −559.60 | −1.54 | 4.20 | 89.52 | 574.43 |
Sources: Author's calculations. Data and region categories are based on Mathers and Loncar 2006 and WHO's projections.
TABLE A7.
Expected Growth (% per year) of Infectious and Chronic Disease Mortality Rates per 100,000 Population from 2002 to 2030, by Age Group
| Infectious Diseases | Chronic Diseases | |||||||
|---|---|---|---|---|---|---|---|---|
| Region | ||||||||
| 5–14 | 15–59 | 60–69 | 70+ | 5–14 | 15–59 | 60–69 | 70+ | |
| World | −2.60 | 0.37 | −2.70 | −2.46 | −1.87 | −0.31 | −0.97 | −0.40 |
| High income | −3.82 | −1.81 | −3.28 | −1.55 | −2.16 | −1.28 | −1.55 | −0.72 |
| Eastern Europe and Central Asia | −0.77 | 2.54 | −1.03 | −1.43 | −1.58 | −1.10 | −1.70 | −0.50 |
| East Asia and Pacific | −4.25 | 0.63 | −4.60 | −3.38 | −1.85 | −0.09 | −1.19 | −0.47 |
| South Asia | −5.14 | −1.08 | −3.70 | −3.18 | −1.61 | −0.03 | −0.50 | −0.14 |
| Latin America | −2.95 | 0.06 | −3.36 | −3.09 | −1.67 | 0.10 | −0.85 | −0.36 |
| Middle East and North Africa | −3.65 | 1.34 | −3.22 | −3.00 | −1.55 | 0.00 | −1.12 | −0.35 |
| Sub-Saharan Africa | −2.57 | −0.89 | −0.61 | −1.46 | −0.68 | 0.10 | 0.15 | 0.28 |
Sources: Author's calculations. Data and region categories are based on Mathers and Loncar 2006 and WHO's projections.
Population Aging as a Leading Explanation
Do the WHO forecasts suggest that chronic disease growth is being entirely fueled by the aging of a population? Several aspects of observed chronic disease epidemiology suggest otherwise.
First, a population's aging cannot account for why the incidence of chronic diseases is dropping within various groups faster in some countries than in others or at different speeds in different age groups.
Second, trends in population aging, as described earlier, do not directly track with country-specific changes in the rate of chronic disease. For example, the rate of age-unadjusted chronic diseases is growing faster in poor than in rich countries, yet the aging population is growing faster in rich than in poor countries. Only by means of an interaction with other factors, such as the health care system, behavioral risk factors, or socioecological determinants, can a population's aging be connected to the observed trends.
Third, it is difficult to use the aging of a population to explain the projected rises in chronic diseases such as diabetes and their reported incidence in youth populations.
Fourth, a population's aging is endogenous: many of the factors promoting economic growth, improving the health system, reducing fertility, and other factors that contribute to aging also affect chronic diseases (e.g., see the neoclassical models of fertility and population change in Schultz 1969).
To overcome some of the limitations of the analyses based on forecasts and contemporary data, I used historical mortality rate data to test the extent to which a population's aging has contributed to rising chronic diseases compared with, and controlling for, other widely cited socioeconomic factors.
Appendix 2 Data and Methods
Data Sources
The data used in the regression analyses are drawn primarily from four sources: male cardiovascular mortality rates per 100,000 population and chronic noncommunicable diseases (WHO type 2 category) are from the World Health Organization Global Mortality Database, and the social, demographic, and economic variables are from the World Bank World Development Indicators, 2005 edition; Penn World Tables; and International Monetary Fund International Financial Statistics, 2007 edition. Table A8 defines and presents descriptive statistics for all variables. Analyses were conducted using STATA vol. 9.2.
TABLE A8.
Summary Statistics and Variable Definitions, Full 56-Country Empirical Sample, 1960 to 2002
| Variable | Description | N | Mean | Std. Dev. | Min | Max | Source | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Log male total CVD rates | Total rates per 100,000; unadjusted for age | 1415 | 5.62 | 0.68 | 3.05 | 6.49 | WHO Global Mortality Database, 1960–2002 | |||
| Log male total NCD rates | Total rates per 100,000; unadjusted for age | 1415 | 6.36 | 0.51 | 4.23 | 7.70 | WHO Global Mortality Database, 1960–2002 | |||
| Log GDP per capita | GDP per capita in constant 2000 $US | 2267 | 8.12 | 1.24 | 4.36 | 10.47 | Penn World Tables, vol. 6.2 | |||
| Growth rate | Percentage change in real GDP per capita | 2264 | 2.61 | 5.10 | −53.12 | 107.53 | Penn World Tables, vol. 6.2 | |||
| Age dependency | Percentage of population over age 65 | 2255 | 7.62 | 4.48 | 2.23 | 18.45 | World Bank World Development Indicators, 2005 ed. | |||
| Urbanization rate | Percentage of population living in urban setting | 1271 | 68.83 | 19.75 | 12.58 | 100.00 | World Bank World Development Indicators, 2005 ed. | |||
| Market integration | Sum of the absolute values of FDI inflows, FDI outflows, portfolio assets, and portfolio liabilities/GDP | 1434 | 0.04 | 0.09 | 0.00 | 1.61 | IMF International Financial Statistics, 2007 ed. | |||
| Log foreign direct investment | Natural log of foreign direct investment inflows in rep. econ., US$ millions | 1400 | 6.15 | 2.21 | −2.64 | 12.27 | IMF International Financial Statistics, 2007 ed. | |||
| Savings rate | Gross domestic savings, % of GDP | 2067 | 21.25 | 8.69 | −73.99 | 53.35 | World Bank World Development Indicators, 2005 ed. | |||
| Secondary education | Total second level of education as highest attained, percentage of population age 25+, smoothed using 5-year moving average | 2186 | 11.72 | 9.68 | 0.00 | 47.50 | World Bank World Development Indicators, 2005 ed. | |||
| Openness | Sum of exports and imports as a percentage of GDP, smoothed using 5-year moving average | 2113 | 53.77 | 34.54 | 3.68 | 276.81 | World Bank World Development Indicators, 2005 ed. | |||
| Inflation rate | Log of inflation in consumer prices, annual %, smoothed using 5-year moving average | 2062 | 2.11 | 1.23 | −2.84 | 7.79 | World Bank World Development Indicators, 2005 ed. | |||
| Correlation Matrix | ||||||||||
| Log CVD | Log CNCD | Log GDP | Age Dep. | Urban | Mkt Intg | Log FDI | Savings Rate | Educ | Open | |
| Log CVD | 1 | |||||||||
| Log CNCD | 0.91 | 1 | ||||||||
| Log GDP | 0.47 | 0.50 | 1 | |||||||
| Age Dep. | 0.78 | 0.79 | 0.75 | 1 | ||||||
| Urban | 0.32 | 0.24 | 0.45 | 0.29 | 1 | |||||
| Market integration | 0.07 | 0.12 | 0.34 | 0.19 | 0.00 | 1 | ||||
| Log FDI | 0.04 | 0.14 | 0.20 | 0.08 | −0.05 | 0.40 | 1 | |||
| Savings rate | 0.12 | 0.24 | 0.10 | 0.14 | −0.13 | 0.20 | 0.15 | 1 | ||
| Education | 0.47 | 0.45 | 0.51 | 0.55 | 0.16 | 0.17 | 0.07 | 0.19 | 1 | |
| Openness | 0.14 | 0.13 | 0.26 | 0.22 | 0.00 | 0.43 | 0.22 | −0.12 | 0.19 | 1 |
| Inflation | −0.27 | −0.32 | −0.52 | −0.56 | −0.05 | −0.28 | −0.07 | −0.25 | −0.46 | −0.25 |
Correlation Analysis within Country-Income Strata
First, I used Pearson correlations to compare unadjusted associations of socioeconomic variables with chronic disease mortality rates across income strata. I define low-, middle-, and high-income countries following the cutoffs available in the data: low corresponds to average < US$3,000 per capita income; middle corresponds to > $3,000 and < $7,000 per capita income; and high corresponds to > $7,000 from 1960 to 2002. These cutoffs also were chosen to stratify the sample into roughly equal thirds. Table A9 lists those countries included in each of these categories.A2
TABLE A9.
Sample Description
| Empirical Model | Countries |
|---|---|
| Model 1. correlation analysis | Rich countries: Australia, Austria, Belgium, Canada, Denmark, Finland, France, Germany, Iceland, Italy, Japan, Netherlands, New Zealand, Norway, Sweden, Switzerland, United Kingdom, United States |
| Middle countries: Argentina, Chile, Costa Rica, Greece, Hong Kong, Ireland, Israel, Mexico, Portugal, Singapore, South Africa, Spain, Taiwan, Uruguay, Venezuela | |
| Poor countries: Bangladesh, Brazil, China, Colombia, Cote D'Ivoire, Ecuador, Egypt, Ghana, India, Indonesia, Jamaica, Korea, Malaysia, Nigeria, Pakistan, Paraguay, Peru, Philippines, Senegal, Sri Lanka, Thailand, Turkey, Zimbabwe | |
| Model 2. long difference model | OECD countries for which data are available: Australia, Austria, Canada, Denmark, Finland, France, Iceland, Italy, Japan, Netherlands, New Zealand, Norway, Sweden, United Kingdom, United States |
| Model 3. neoclassical growth model | OECD countries for which time-series data are available: Australia, Austria, Belgium, Canada, Denmark, Finland, France, Germany, Greece, Ireland, Iceland, Italy, Japan, Mexico, Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, Switzerland, United Kingdom, United States |
To cope with potential biases associated with changing International Classification of Disease variations (ICD) during the sample period, I purged nonlinear time trends from the data by regressing them on a set of time dummies using the following method:
First, consider the true chronic disease mortality rates as the sum of unadjusted mortality rates plus a term for detection bias associated with changing ICD classifications and/or secular time trends. Mathematically, this can be expressed as
or rearranging it as
Note that the sign estimated for the detection bias term does not matter for this framework. To capture adjusted chronic disease mortality rates, I regressed unadjusted chronic disease mortality rates on a set of dummy variables for each year, as follows:
Here i is country, t is year. Yeart is a vector of period dummies. With this regression, we can retain the error-term ɛit as the chronic disease mortality rates purged for any nonlinear period effects. In other words, the error term of this model provides time de-trended chronic disease mortality rates. However, none of the results presented qualitatively differed when modeled without using this adjustment.
The analysis was also replicated using “other chronic noncommunicable diseases,” which does not include CVD, as compared to the WHO type 2 chronic noncommunicable disease category, which does include CVD. As shown in figure A2, the patterns were similar to those presented in the main text. Correlations between the non-CVD chronic noncommunicable disease and overall chronic noncommunicable disease categories were strong: r = 0.97, 0.92 and 0.86 at p<0.001 in low-, middle-, and high-income countries, respectively.
Figure A2.
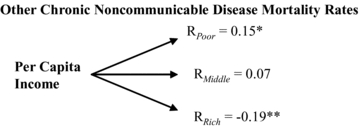
Replication Using Other Chronic Noncommunicable Disease Mortality Rates
Notes: Poor countries < US$3,000 per capita income, middle countries > $3,000 and < $7,000, and rich countries > $7,000 on average from 1960 to 2002. Male mortality rate data are from the WHO Global Mortality Database and are in logs. Other chronic noncommunicable disease is WHO's type 2 burden of disease category excluding cardiovascular disease. Economic data are from the World Bank's World Development Indicators, 2005 ed., and the International Monetary Fund's International Financial Statistics, 2007 series. Per capita income is based on gross domestic product (GDP) per capita. Cross-country data are de-trended for effects of changing ICD classifications. Appendix 2 describes all data and presents descriptive statistics.
Significance at *p < 0.05, **p < 0.01.
Cross-National Multivariate Regression Analysis of Chronic Noncommunicable Disease Mortality Rates
After establishing an empirical connection between the often-cited socioeconomic variables and chronic noncommunicable diseases using the Pearson correlations shown in figures 3 and 4 in the text, I applied multivariate regression models to further control for potential confounders and surveillance variations as well as to quantify and compare the relationships between the socioeconomic variables of interest and chronic disease changes. I estimated these models using rich OECD countries for three empirical and theoretical reasons: (1) the sample reduces the heterogeneity associated with countries at different levels of development (as suggested by my earlier correlation analysis and hypotheses); (2) there are greater levels of missing data for the longitudinal analysis for low- and middle-income countries; and (3) developing countries are just now undergoing many of the social and economic transformations that OECD countries underwent two decades ago. Thus the experience of OECD countries provides a model, albeit an imperfect one, with which to illuminate the probable future trajectories of the developing countries.
In table 5 in the text I used a long-differencing approach to wipe out potential unobserved changes within countries over time. This approach is necessary to take into account the decadal lag between exposure to chronic disease risk and mortality. I also controlled for period effects using a set of year dummies. Thus I specified the empirical model as
Here i is country and t is year. For each variable, ΔXit is calculated using a difference operator as Xi,t− Xi,t−20; GDP is log GDP per capita in constant 2000 US $; FDI is the logged level of foreign direct investment in constant 2000 US$; MKT is market integration calculated as total capital flows/GDP, following the calculations by IMF economists (Edison et al. 2002); URBAN is the percentage of the population living in urban settings; and AGE is the percentage of the population over age sixty-five. Changes in these variables correspond to the processes of interest: a change in the percentage of the population living in urban settings yields urbanization; a change in the percentage of the population over age sixty-five yields population aging; and so forth.
These models were robust to excluding outliers (based on standardized residuals greater than |2|), using alternative decadal lag measures (such as 10, 15, and 25 years), and to alternative measures of population aging, such as the ratio of the working-age population to the total population. It is unlikely that reverse causation exists such that heart disease would affect urbanization or market integration. The differencing operation also in part nets out unobserved factors that have remained fixed over time. Since the social and economic factors are ecological, it is hard to envision what third factor might be correlated with both these measures and heart disease that does not mediate the relationship between the social and economic measures and heart disease. Other globalization factors that have been indicated in the public health literature as significant drivers of chronic disease, such as trade liberalization, are captured by market integration.A3 The negative constant and time trend controls in this framework can in part be interpreted as a correction for downward pressures related to “epidemiologic transition” in mortality rates.
Figure A3 is a sample unadjusted dynamic figure showing that despite average declines in male CVD mortality rates over twenty-year periods in high-income countries, higher economic growth rates were connected with greater increases and smaller decreases in CVD mortality rates.
Figure A3.
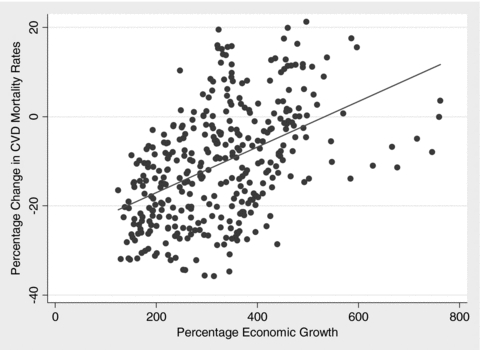
Sample Unadjusted Relationship between Economic Growth and Cardiovascular Disease Mortality Rates, High-Income Countries, Twenty-Year Differences, 1960 to 2002
After estimating these equations, I used regression decomposition methods to compare the magnitude of the effects attributed to each parameter, as shown in table 6 in the text (Bowerman and O'Connell 1993). This method provides an alternative, and arguably more substantive, way to evaluate the strength of relationships, compared with traditional goodness-of-fit measures (a statistically significant relationship and good fit does not necessarily imply a larger effect size). That is, I calculated the average change in each variable over a twenty-year period in the set of OECD countries and then multiplied by the estimated beta-coefficient. Repeating this process for each variable provided a comparison of the substantive, as opposed to the statistical, significance of each variable. Microsoft Excel was used to generate these calculations.
An alternative method using standardized beta-coefficients (so that one standard deviation change in the independent variable corresponded to a standardized beta amount of standard deviation changes in the dependent variable) is provided here. Partial correlations are multiplied by the standardized beta-coefficients to give a measure of variance explained. Comparing population aging with the set of macrosocial and economic factors yields fairly similar results: population aging accounts for close to 40 percent of WHO type 2 noncommunicable diseases but only 15 percent of the heart disease category. The stronger relationship observed between heart disease and the socioeconomic factors would be expected because it more closely approximates the subset of chronic diseases described throughout this article.
Economic Growth Models
Table 7 in the text uses an alternative estimation method to answer a different question: Is there a significant effect of chronic disease working-age mortality levels on economic growth? I offer the most standard macroeconomic set of controls, which are based on the Solow economic growth model, also referred to in the economic literature as the “neoclassical growth model” (see, e.g., Romer 2000). It is standard in the macroeconomics literature to control for fixed effects to hold constant unobserved confounding variables that are relatively fixed over time or national in scope but time variant (essentially by using country-specific slopes) (Jones 2000).
Here i is country and t is year. GDP is the percentage growth in real GDP per capita from the Penn World Tables v6.2; NCD is log total chronic disease death rates in working-age adults; INF is the log of inflation in the consumer price index; EDUC is secondary education rates; GDS is the gross domestic savings rate; and μ and η are sets of dummy variables controlling for country- and period-specific effects. Inflation rates, openness, education, and savings rates were smoothed using a five-year moving average calculation.
To identify the economics costs associated with chronic disease mortality, unadjusted chronic disease mortality levels may be preferable because they capture the full losses of human life and, as a result, better reflect the full costs of disease. Differences between age-adjusted and age-unadjusted rates are probably minimal in the fixed-effects framework. Similarly, differences between changes in mortality levels and mortality rates are minor when using within-country variation. (The results were replicated using both rates and levels in table A11.) Although data on DALYs would be a better measure than mortality rates, comparative longitudinal data are not available.
The fixed-effects estimation approach is sometimes referred to as the “within-estimator” because it isolates the variation within countries while netting out the variation between countries. Standard errors are clustered for robustness to serial correlation and contemporary heteroskedasticity across countries and to reflect nonindependence of sampling (Wooldridge 2002; STATA: xtreg module using “fe” and “cluster [id]” options). Since previous models established greater economic development as a determinant of increasing chronic diseases, any residual bidirectionality in these models arising from the growth's relationship to chronic disease would bias the results in a conservative direction.
Alternative Economic Growth Models
Table A10 shows that the results are robust to sample and different estimation methods. What is presented in the text is the most conservative model. Table A11 also shows the results of five regression models using alternative chronic disease measures with the same set of controls.
TABLE A10.
Effect of Chronic Noncommunicable Disease Working-Age Mortality Rates on Economic Growth
| Dependent Variable: Real GDP per Capita Change | |||
|---|---|---|---|
| Covariate | Fixed-Effects Model, 1972–2000 | Fixed-Effects Model, 1960–2002 | Fixed-Effects AR(1), 1960–2002 |
| Log male CNCD working-age mortality rate | −5.11** | −4.67*** | −5.10*** |
| (1.43) | (1.63) | (1.80) | |
| Log inflation | −1.73** | −0.74 | −1.12*** |
| (0.37) | (0.49) | (0.30) | |
| Openness | 0.01 | 0.06*** | 0.04* |
| (0.02) | (0.02) | (0.02) | |
| Secondary education levels | −0.02 | 0.03 | 0.01 |
| (0.03) | (0.04) | (0.02) | |
| Savings rate | 0.23** | 0.07 | 0.06 |
| (0.07) | (0.05) | (0.04) | |
| Number of country years | 532 | 758 | 758 |
| Number of countries | 20 | 23 | 23 |
Notes: Robust standard errors are in parentheses, clustered by country to reflect nonindependence of sampling and for robustness to serial correlation. AR(1) model uses panel-corrected standard errors (Beck and Katz 1995). Models include country- and time-fixed effects.
Significance at *p < 0.05, **p < 0.01, ***p < 0.001.
TABLE A11.
Effect of Male Chronic Disease Mortality Rates on Economic Growth, 1960–2002
| Covariate | Real GDP per Capita Change |
|---|---|
| Log CVD working-age mortality rates | −2.50** |
| (0.72) | |
| Log total CVD mortality rates | −4.54** |
| (1.26) | |
| Log chronic disease working-age mortality number | −4.12* |
| (1.58) | |
| Log chronic disease working-age mortality rates | −4.67** |
| (1.61) | |
| Log total chronic disease mortality rates | −5.68* |
| (2.24) |
Notes: Results presented from five separate regression models. Robust standard errors are in parentheses, clustered by country to reflect nonindependence of sampling and for robustness to serial correlation. Models also control for log inflation in the consumer price index, population level of secondary education, openness to trade (exports + imports/GDP), savings rates, and country- and time-fixed effects.
Significance at *p < 0.05, **p < 0.01.
As robustness checks, several additional controls were sequentially introduced to the model, including age dependency rates, market integration, and foreign direct investment. None of these results was affected. I also removed potential outliers, defined as growth rates greater than or less than 25 percent in a given year; again, the results were unaffected. Similar results also were produced after removing standardized regression residuals >|2|. Figure A4 presents an added-variable diagnostic plot for the regression in table 7 in the text. More sophisticated methods of coping with serial correlation, such as using xtabond2 (with finite sample bias correction) or xtpcse in STATA, produce statistically indistinguishable results from the models shown in table 7. Finally, tables A10, A11, and A12 present robustness checks and alternative estimates using both total chronic noncommunicable disease mortality rates and heart disease mortality rates as well as mortality numbers. Table A13 describes baseline and optimistic scenarios of economic change relating to chronic disease based on WHO projections of chronic disease trends and the WHO goals set out for chronic disease reductions in Preventing Chronic Diseases: A Vital Investment (2005).
TABLE A12.
Effect of Expected Changes in Chronic Disease Mortality Rates on Economic Growth, 2002 to 2030
| Region | Projected Chronic Disease Increase (% Change from 2002 to 2030) | Estimated Effect on Growth Rates in 2030 (% per Year) |
|---|---|---|
| World | 21.90 | −1.02 |
| High income | 12.06 | −0.56 |
| Eastern Europe and Central Asia | 5.73 | −0.27 |
| East Asia and Pacific | 52.23 | −2.43 |
| South Asia | 27.89 | −1.30 |
| Latin America | 48.01 | −2.24 |
| Middle East and North Africa | 28.28 | −1.32 |
| Sub-Saharan Africa | 12.13 | −0.57 |
Sources: Percentage changes are based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections. Estimated effects are based on results shown in table 7 in the text.
TABLE A13.
Scenarios for Changes in Chronic Disease Mortality Rates and Economic Growth, 2005 to 2015
| Chronic Disease Mortality Rates Overall Percentage Change from 2005 to 2015 | Effect on Economic Growth Rates Percentage per Year in 2015 | |||
|---|---|---|---|---|
| Region | WHO forecast change (baseline) | WHO 2% yearly reduction—baseline (optimistic) | Baseline | Optimistic |
| World | +7.3 | −14.6 | −0.34 | +0.66 |
| High income | +7.4 | −14.5 | −0.35 | +0.68 |
| Eastern Europe and Central Asia | +6.0 | −15.9 | −0.28 | +0.74 |
| East Asia and Pacific | +14.9 | −7.0 | −0.70 | +0.33 |
| South Asia | +7.8 | −14.1 | −0.36 | +0.66 |
| Latin America | +16.0 | −5.9 | −0.74 | +0.28 |
| Middle East and North Africa | +6.2 | −15.7 | −0.29 | +0.73 |
| Sub-Saharan Africa | +4.4 | −17.5 | −0.21 | +0.82 |
Sources: Percentage changes are based on Mathers and Loncar 2006 and WHO's Global Burden of Disease projections. Estimated effects are based on results shown in table 7 in the text. WHO's goal of 2% reduction per year is from WHO's Preventing Chronic Diseases: A Vital Investment (2005). Growth rates in 2015 do not reflect cumulative economic gains associated with higher growth rates. For example, each WHO reduction of 2% is estimated to correspond to a yearly 0.09% boost to economic growth (table 7). Thus, when cumulated, WHO's optimistic 2% yearly reduction without subtracting baseline increases from 2005 to 2015 would correspond to a 5.3% higher current GDP per capita level in 2015 than in 2005 and a cumulative 20.8% economic gain overall (not time discounted), which is incidentally similar in magnitude to the overall chronic disease reduction of 21.9% associated with a 2% reduction each year (not shown).
Figure A4.
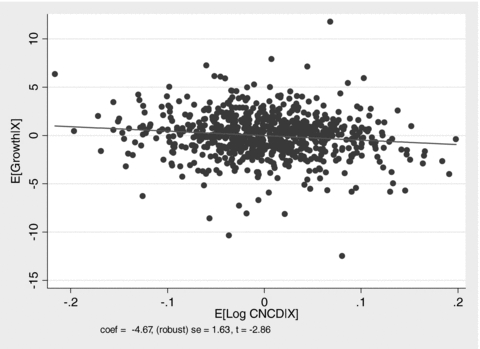
Added-Variable Plot
Appendices Endnotes
To make this more explicit, consider a simple example with hypothetical data: 30 mortality rate in 2002 and 20 mortality rate in 2030; 15 population in 2002 and 25 population in 2030. The total change in numbers of deaths is (20 × 25)2030− (30 × 15)2002= 500 − 450 = 50. Now, take the “epidemiologic change” as (20 × 15 − 30 × 15) =−150, and the demographic change as (25 × 30 − 15 × 30) = 300. Clearly, −150 + 300 does not equal 50.
Although some of the classifications for poor countries may seem inappropriate for the present day (such as the rapidly growing countries of China and India), remember that the analysis covered 1960 to 2002, and as a result, the classification is based on the growth average during this period so as not to avoid building in successful growth performance. Many analyses do not address this comparative methodological problem and instead classify countries by current levels of development, even when historical levels may be more appropriate.
Market integration may be a better measure for modeling the effects associated with trade liberalization discussed in the recent public health literature (see Hawkes 2006; Rayner et al. 2006) because integration reflects the actual economic outcome of liberalization, as opposed to the process of liberalizing. Other measures for trade such as openness, or imports + exports/GDP, produced similar results.
Endnotes
This holds for all regions except for eastern Europe and Central Asia, where infectious diseases will also increase, albeit at less than one-sixth the amount expected for chronic diseases and primarily a result of the economic transitions in the former Soviet Union in the mid-1990s.
Although the World Bank commits more than US $1 billion to health each year, the cumulative total of loans for chronic noncommunicable diseases from 1997 to 2002 was US $110 million, nearly all of which was provided to eastern European and former Soviet countries. The World Bank argued that “any shift in attention from communicable diseases to non-communicable ailments … would work to the detriment of the poor … [and] the shift's primary beneficiaries would be the rich, who would therefore gain at the expense of the poor” (Gwatkin and Guillot 2000, p. 5). WHO spends only $1 on each chronic disease death in the developing world, compared with $7 for every HIV/AIDS death, yet chronic noncommunicable diseases are causing six times as many deaths in developing countries (WHO 2003). For more on why and how chronic diseases are a “neglected epidemic,” see Horton 2005 and the associated special issue of The Lancet, as well as Beaglehole and Yach 2003; Daar et al. 2007; Fuster and Voute 2005; Strong et al. 2006; and Suhrcke et al. 2006.
India, for example, has the world's worst iron deficiency levels and the world's largest diabetes pool. Exposure to stressors during early life-stages increases the risk of developing a chronic disease in the future (see Aboderin et al. 2001 and “thrifty phenotype”/“fetal origins” discussions; Reddy et al. 2005).
A market failure can be thought of as a circumstance when a competitive market's ability to translate individual rationality into collective rationality through individual market choice breaks down. For example, when one individual's choice affects another individual's well-being, such as in the case of environmental tobacco smoke, the individual's choice will not reflect the spillover onto the other individual, which, when aggregated via a market mechanism, leads to collective irrationality (an externality). Another circumstance is when an individual's choice does not equate to individual rationality from the outset, such as in the case of inadequate information or an individual's inability to use the available information, as seen with nutrition labeling. In this case, the market simply multiplies the existing mismatch between individual choice and individual rationality (an internality), which leads to collective irrationality at the population level. This latter “internality” category subsumes a large and growing literature on time-inconsistent preferences and psychological decision-making fallacies in behavioral economics.
In economic parlance, marketing affects the partial derivative: ∂R/∂I, or the change in chronic disease risk with respect to a change in income, all things being equal. In log form, this derivative is an income elasticity. Generally it appears that ∂2R/∂I2 < 0 (i.e., the function is concave) or that with rising income, the increase in risk levels starts diminishing—and, after a certain income level, even bends backward (the effect seen in rich countries). For a graphic depiction of chronic disease consumption curves, see Yach 2005, fig. 15.3.
Note that this method provides a full macroeconomic accounting for all the direct and indirect microeconomic channels of chronic disease's impact: health care costs, productivity costs, exit from the labor force, changes to savings, investment and consumption behavior, diminished education and returns to education, and likelihood of foreign direct investment, to name only a few. For a literature review of the evidence for each of these channels, see World Bank 2007 and Suhrcke et al. 2006. Removing savings rates from the model boosts the estimated coefficient of chronic noncommunicable disease working-age mortality rates to −5.37 at p < 0.001, suggesting that decreasing savings rates may be an important pathway of chronic disease's economic effects.
Recent studies have also identified significant interactions between the control of infectious diseases and of chronic diseases and their associated risk factors: TB, MDR-TB, and diabetes (Bashar et al. 2001; Stevenson et al. 2007), AIDS and TB incidence and tobacco use (Bates et al. 2007; Furber et al. 2007), and stunting and obesity (Popkin, Richards, and Montiero 1996), which further emphasize the need for a more coordinated approach to infectious and chronic disease interventions.
There are some glimmers of change: the UN recently adopted the first resolution on diabetes (61/225), designating November 14 as World Diabetes Day, which may serve as an entry point for broader action on chronic diseases; and Nature published “Grand Challenges in Chronic Non-Communicable Diseases” in November 2007, outlining the top twenty policy and research priorities for leading chronic diseases and marking the founding of a global partnership comprising OxHA, the UK Medical Research Council, the Canadian Institutes of Health Research, the U.S. National Institute of Health, and the Indian Council of Medical Research. However, unlike the grand (infectious disease) challenges in global health (http://www.gcgh.org), the chronic disease challenges were not linked to up-front funding commitments (Daar et al. 2007).
References
- Aboderin I, Kalache A, Ben-Shlomo Y, Lynch JW, Yajnik CS, Kuh D, Yach D. Life-Course Perspectives on Coronary Heart Disease, Stroke and Diabetes: Key Issues and Implications for Policy and Research. 2001. [accessed March 31, 2008]. Geneva: World Health Organization. Available at http://whqlibdoc.who.int/hq/2001/WHO_NMH_NPH_01.4.pdf. [Google Scholar]
- Bashar M, Alcabes P, Rom WN, Condos R. Increased Incidence of Multi-Drug Resistant Tuberculosis in Diabetic Patients on the Bellevue Chest Service, 1987 to 1997. Chest. 2001;120:1514–19. doi: 10.1378/chest.120.5.1514. [DOI] [PubMed] [Google Scholar]
- Bates MN, Khalakdina A, Pai M, Change L, Lessa F, Smith KR. Risk of Tuberculosis from Exposure to Tobacco Smoke: A Systematic Review and Meta-Analysis. Archives of Internal Medicine. 2007;167(4):335. doi: 10.1001/archinte.167.4.335. [DOI] [PubMed] [Google Scholar]
- Beaglehole R, Yach D. Globalisation and the Prevention and Control of Non-Communicable Disease: The Neglected Chronic Diseases of Adults. The Lancet. 2003;362(9387):903–8. doi: 10.1016/S0140-6736(03)14335-8. [DOI] [PubMed] [Google Scholar]
- Beck N, Katz JN. What to Do (and Not to Do) with Time-Series Cross-Section Data. American Political Science Review. 1995;89:634–47. [Google Scholar]
- Bowerman BL, O'Connell RT. Forecasting and Time Series: An Applied Approach. 3rd ed. Belmont, Calif: Duxbury Press; 1993. [Google Scholar]
- Centers for Disease Control (CDC) Public Health and Aging: Trends in Aging—United States and Worldwide. Morbidity and Mortality Weekly Report. 2003;52(6):101–6. [PubMed] [Google Scholar]
- Cutler D, Glaeser EL, Shapiro JM. Why Have Americans Become More Obese? Journal of Economic Perspectives. 2003;17:93–118. [Google Scholar]
- Daar AS, Singer PA, Persad DL, Pramming SK, Matthews DR, Beaglehole R, Bernstein A, et al. Grand Challenges in Chronic Non-Communicable Diseases. Nature. 2007;450:494–96. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Darmon N. The Economics of Obesity: Dietary Energy Density and Energy Cost. American Journal of Clinical Nutrition. 2005;82:S265–73. doi: 10.1093/ajcn/82.1.265S. [DOI] [PubMed] [Google Scholar]
- Edison HJ, Levine R, Ricci L, Sloek T. International Financial Integration and Economic Growth. IMF Working Paper. 2002:02/145. [Google Scholar]
- Fries J. The Compression of Morbidity. The Milbank Quarterly. 1983;61(3):397–419. [PubMed] [Google Scholar]
- Furber AS, Maheswaran R, Newell JN, Carroll C. Is Smoking Tobacco an Independent Risk Factor for HIV Infection and Progression to AIDS? A Systemic Review. Sexually Transmitted Infections. 2007;83:41–46. doi: 10.1136/sti.2005.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuster V, Voute J. MDGs: Chronic Diseases Are Not on the Agenda. The Lancet. 2005;366(9496):1512–14. doi: 10.1016/S0140-6736(05)67610-6. [DOI] [PubMed] [Google Scholar]
- Gilmore AB, Collin J, McKee M. Unless Health Decree 30 Is Amended Satisfactorily It Will Not Be Possible for This Transaction to Proceed”: British American Tobacco's Erosion of Health Legislation in Uzbekistan. British Medical Journal. 2006;332(7537):355–58. doi: 10.1136/bmj.332.7537.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AB, McKee M. Moving East: How the Transnational Tobacco Companies Gained Entry to the Emerging Markets of the Former Soviet Union. Part II: An Overview of Priorities and Tactics Used to Establish a Manufacturing Presence. Tobacco Control. 2004;13:151–60. doi: 10.1136/tc.2003.005207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AB, McKee M. Exploring the Impact of Foreign Direct Investment on Tobacco Consumption in the Former Soviet Union. Tobacco Control. 2005;14:13–21. doi: 10.1136/tc.2003.005082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwatkin D, Guillot M. The Burden of Disease among the Global Poor: Current Situation, Future Trends, and Implications for Strategy. Washington, D.C.: The World Bank; 2000. [accessed March 31, 2008]. Available at http://siteresources.worldbank.org/INTPAH/Resources/Publications/Seminars/burden.pdf. [Google Scholar]
- Hawkes C. The Role of Foreign Direct Investment in the Nutrition Transition. Public Health Nutrition. 2005;8(4):357–65. doi: 10.1079/phn2004706. [DOI] [PubMed] [Google Scholar]
- Hawkes C. Uneven Dietary Development: Linking the Policies and Processes of Globalization with the Nutrition Transition, Obesity and Diet-Related Chronic Diseases. Globalization and Health. 2006;2(4):1–18. doi: 10.1186/1744-8603-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton R. The Neglected Epidemic of Chronic Diseases. The Lancet. 2005;366(9496):1514. doi: 10.1016/S0140-6736(05)67454-5. [DOI] [PubMed] [Google Scholar]
- Jones A. Health Econometrics. In: Cuyler A, Newhouse JP, editors. Handbook of Health Economics. New York: Elsevier Science; 2000. pp. 265–344. [Google Scholar]
- Leeder S, Raymond S, Greenberg H, Liu H, Esson K. A Race against Time: The Challenge of Cardiovascular Disease in Developing Countries. New York: Earth Institute, Columbia University; 2004. [Google Scholar]
- Lopez AD. The Evolution of the Global Burden of Disease Framework for Disease, Injury and Risk Factor Quantification: Developing the Evidence Base for National, Regional and Global Public Health Action. Globalization and Health. 2005;1:5. doi: 10.1186/1744-8603-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks JS, McQueen DV. Chronic Diseases. In: Koop CE, Pearson CE, Schwarz MR, editors. Critical Issues in Global Health. San Francisco: Jossey-Bass; 2002. pp. 117–26. [Google Scholar]
- Mathers CD, Loncar D. Projections of Global Mortality and Burden of Disease from 2002 to 2030. PLoS Medicine. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Disease, Injuries and Risk Factors in 1990 and Projected to 2020. Harvard School of Public Health; 1996. World Health Organization, and the World Bank. Geneva: World Health Organization. [Google Scholar]
- Murray CJ, Lopez AD. Alternative Projections of Mortality and Disability by Cause 1990–2020: Global Burden of Disease Study. The Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- Nolte E, McKee M, editors. Caring for People with Chronic Conditions: A Health System Perspective. Buckingham: McGraw-Hill; 2008. [Google Scholar]
- Omran A. The Epidemiologic Transition: A Theory of the Epidemiology of Population Change. The Milbank Quarterly. 1971;49(4):509–38. [PubMed] [Google Scholar]
- Pang T, Guindon GE. Globalization and Its Risks to Health. European Molecular Biology Organisation Journal. 2004;5:S11–16. doi: 10.1038/sj.embor.7400226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin B. What Is Unique about the Experience in Lower- and Middle-Income Less-Industrialised Countries Compared with the Very-High Income Countries? The Shift in the Stages of the Nutrition Transition Differs from Past Experiences! Public Health Nutrition. 2002;5:205–14. doi: 10.1079/PHN2001295. [DOI] [PubMed] [Google Scholar]
- Popkin B, Horton S, Kim S, Mahal A, Shuigao J. Trends in Diet, Nutritional Status, and Diet-Related Noncommunicable Diseases in China and India: The Economic Costs of the Nutrition Transition. Nutrition Reviews. 2001;59:379–90. doi: 10.1111/j.1753-4887.2001.tb06967.x. [DOI] [PubMed] [Google Scholar]
- Popkin B, Richards MK, Montiero CA. Stunting Is Associated with Overweight in Children of Four Nations That Are Undergoing the Nutrition Transition. American Journal of Nutrition. 1996;126(12):3009–16. doi: 10.1093/jn/126.12.3009. [DOI] [PubMed] [Google Scholar]
- Rayner G, Hawkes C, Lang T, Bello W. Trade Liberalization and the Diet Transition: A Public Health Response. Health Promotion International. 2006;21(S1):67–74. doi: 10.1093/heapro/dal053. [DOI] [PubMed] [Google Scholar]
- Reddy K, Shah B, Varghese C, Ramadoss A. Responding to the Threat of Chronic Diseases in India. The Lancet. 2005;366(9498):1744–49. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- Roglic G, Unwin N. Global Mortality Attributable to Diabetes: Time for a Realistic Estimate. Diabetes Voice. 2005;50(10):33–34. [Google Scholar]
- Romer D. Advanced Macroeconomics. 2nd ed. New York: McGraw-Hill/Irwin; 2000. chaps. 1 and 2. [Google Scholar]
- Rosen S, Fox MP, Gill CJ. Patient Retention in Antiretroviral Therapy Programs in Sub-Saharan Africa: A Systematic Review. PLoS Medicine. 2007;4(10):1691–1701. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz T. An Economic Model of Family Planning and Fertility. Journal of Political Economy. 1969;77:153–80. doi: 10.1086/259506. [DOI] [PubMed] [Google Scholar]
- Stevenson CR, Forouhi NF, Roglic G, Williams BG, Lauer JA, Dye C, Unwin N. Diabetes and Tuberculosis: The Impact of the Diabetes Epidemic on Tuberculosis Incidence. BioMed Central Public Health. 2007;7:234. doi: 10.1186/1471-2458-7-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong K, Mathers C, Bonita R. Preventing Stroke: Saving Lives around the World. Lancet Neurology. 2007;6(2):182–87. doi: 10.1016/S1474-4422(07)70031-5. [DOI] [PubMed] [Google Scholar]
- Strong K, Mathers C, Epping-Jordan J, Beaglehole R. Preventing Chronic Disease: A Priority for Global Health. International Journal of Epidemiology. 2006;35(2):492–94. doi: 10.1093/ije/dyi315. [DOI] [PubMed] [Google Scholar]
- Stuckler D, Hawkes C, Yach D. Governance of Chronic Disease. In: Buse K, Drager N, editors. Making Sense of Global Health Governance—A Policy Primer. Palgrave Macmillan Press and World Health Organization; 2008. WHO Global Governance Working Group. in press. [Google Scholar]
- Suhrcke M, Nugent R, Stuckler D, Rocco L. Chronic Diseases: An Economic Perspective. London: OxHA Public Health and Economics Working Group; 2006. Oxford Health Alliance. [Google Scholar]
- Suhrcke M, Urban D. Are Cardiovascular Diseases Bad for Economic Growth? CESIFO Working Paper no. 1845. [DOI] [PubMed]
- United Nations (UN) New York: Population Division, United Nations; World Population Prospects: The 2004 Revision. [Google Scholar]
- Wang L, Kong L, Wu F, Bai Y, Burton R. Preventing Chronic Diseases in China. The Lancet. 2005;366:1514. doi: 10.1016/S0140-6736(05)67344-8. [DOI] [PubMed] [Google Scholar]
- Wanless D. Securing Our Future Health: Taking a Long-Term View. London: HM Treasury; 2002. [Google Scholar]
- Wanless D. Securing Good Health for the Whole Population. London: HM Treasury; 2004. [Google Scholar]
- Wiist WH. Public Health and the Anticorporate Movement: Rationale and Recommendations. American Journal of Public Health. 2006;96(8):1370–75. doi: 10.2105/AJPH.2005.072298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkowski TH. Food Marketing and Obesity in Developing Countries: Analysis, Ethics and Public Policy. Journal of Macromarketing. 2007;27(2):126–37. [Google Scholar]
- Wooldridge J. Econometric Analysis of Cross-Sectional and Panel Data. Cambridge, Mass: MIT Press; 2002. [Google Scholar]
- World Bank (WB) World Development Report: Investing in Health. New York: Oxford University Press; 1993. [Google Scholar]
- World Bank (WB) Public Policy and the Challenge of Chronic Noncommunicable Diseases. Washington, D.C.: 2007. [Google Scholar]
- World Health Organization (WHO) Declaration of Alma-Ata. Geneva: World Health Organization; 1978. [accessed March 31, 2008]. Available at http://www.who.int/social_determinants/links/events/alma_ata/en/index.html. [Google Scholar]
- World Health Organization (WHO) Ottawa Charter for Health Promotion; First International Conference on Health Promotion; 1986. [accessed March 31, 2008]. Available at http://www.who.int/hpr/NPH/docs/ottawa_charter_hp.pdf. [Google Scholar]
- World Health Organization (WHO) Financial Management Report: Expenditure on Implementation of Objectives in Programme Budget 2002–2003. Geneva: 2003. All sources of funds, from January 1, 2002, to December 31, 2002. [Google Scholar]
- World Health Organization (WHO) Preventing Chronic Diseases: A Vital Investment. Geneva: 2005. [Google Scholar]
- World Health Organization (WHO) Achieving Health Equity: From Root Causes to Fair Outcomes. 2007. [accessed March 31, 2008]. Commission on the Social Determinants of Health. Interim Statement. Available at http://whqlibdoc.who.int/publications/2007/interim_statement_eng.pdf. [Google Scholar]
- World Health Organization (WHO) Global Tuberculosis Control—Surveillance, Planning, Financing. 2008. [accessed March 31, 2008]. Available at http://www.who.int/tb/publications/global_report/2008/en/index.html. [Google Scholar]
- Yach D. Chronic Disease. In: Levy B, Sidel VW, editors. Social Injustice. Oxford: Oxford University Press; 2005. chap. 15. [Google Scholar]
- Yach D, Stuckler D, Brownell K. Epidemiologic and Economic Burden of the Global Epidemics of Obesity and Diabetes. Nature Medicine. 2006;12(1):62–66. doi: 10.1038/nm0106-62. [DOI] [PubMed] [Google Scholar]
- Yach D, Hawkes C, Gould CL, Hofman KJ. The Global Burden of Chronic Diseases: Overcoming Impediments to Prevention and Control. Journal of the American Medical Association. 2004;291:2616–22. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]


