Abstract
Study Objective:
To examine whether exposure to long working hours predicts various forms of sleep disturbance; short sleep, difficulty falling asleep, frequent waking, early waking and waking without feeling refreshed.
Design:
Prospective study with 2 measurements of working hours (phase 3, 1991–1994 and phase 5, 1997–1999) and 2 measurements of subjective sleep disturbances (phase 5 and phase 7, 2002–2004).
Setting:
The Whitehall II study of British civil servants.
Participants:
Full time workers free of sleep disturbances at phase 5 and employed at phases 5 and 7 (n = 937–1594) or at phases 3, 5, and 7 (n = 886–1510).
Measurements and Results:
Working more than 55 hours a week, compared with working 35–40 hours a week, was related to incident sleep disturbances; demographics-adjusted odds ratio (95% CI) 1.98 (1.05, 3.76) for shortened sleeping hours, 3.68 (1.58, 8.58) for difficulty falling asleep; and 1.98 (1.04, 3.77) for waking without feeling refreshed. Repeat exposure to long working hours was associated with odds ratio 3.24 (1.45, 7.27) for shortened sleep, 6.66 (2.64, 16.83) for difficulty falling asleep, and 2.23 (1.16, 4.31) for early morning awakenings. Some associations were attenuated after adjustment for other risk factors. To a great extent, similar results were obtained using working hours as a continuous variable. Imputation of missing values supported the findings on shortened sleep and difficulty in falling asleep.
Conclusion:
Working long hours appears to be a risk factor for the development of shortened sleeping hours and difficulty falling asleep.
Citation:
Virtanen M; Ferrie JE; Vahtera J; Elovainio M; Singh-Manoux A; Marmot MG; Kivimäki M. Long working hours and sleep disturbances: the whitehall II prospective cohort study. SLEEP 2009;32(6):737–745.
Keywords: Work hours, sleep, insomnia, overtime work, prospective
SURVEYS SUGGEST THAT 10% TO 15% OF ADULTS SUFFER FROM CHRONIC INSOMNIA, AND AN ADDITIONAL 25% TO 35% HAVE TRANSIENT OR OCCASIONAL sleeping disturbances.1 There is also evidence to show that a great number of people work long hours.2 One hypothesis is that long working hours are an important risk factor for sleep disturbances.3 However, the etiology behind sleep disturbances is complex, and the evidence to support the status of long working hours as an independent risk factor for incident sleeping disturbances remains insufficient.
In cross-sectional analyses, long working hours have been associated with sleep disturbances in some studies4,5 but null findings have also been reported.6,7 Others have reported associations between long working hours and fatigue symptoms.8–10 Prospectively, only one study has reported that past history, but not present overtime, increased the risk of incident sleep disorder.11 However, earlier studies are limited by their cross-sectional assessment of working hours and sleep, working hours assessment based on only one point in time, or retrospective analysis.
The Whitehall II study of British civil servants enabled us to address many of these methodological limitations. First, a strength of the study is the opportunity to determine average working hours at 2 time points over an interval of approximately 4 years and to take into account the influence of a range of covariates, such as workload, behavioral risk factors and health conditions.12–20 A further advantage is the possibility to assess incident sleep disturbances with baseline data on sleep at the time of the measurement of working hours and approximately 5 years later. As associations between working hours and sleep problems may be different depending on the type of problem, we focused on specific outcomes, such as short sleep, difficulty falling asleep, difficulty staying asleep, early waking, and waking without feeling refreshed (i.e., feeling tired after normal amount of sleep).
METHODS
Participants
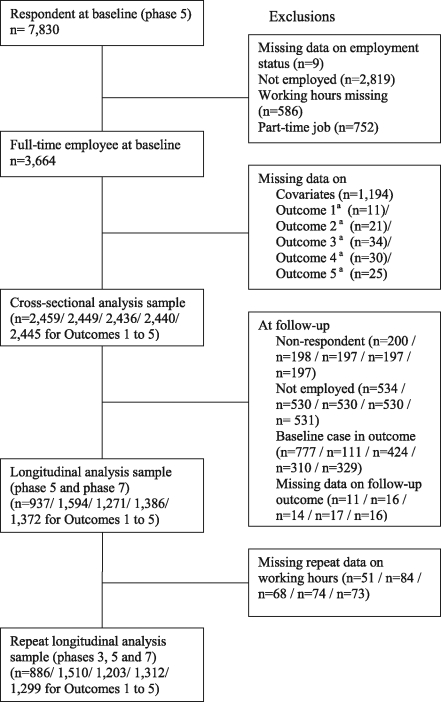
The Whitehall II study sample recruitment (phase 1) took place between late 1985 and early 1988 among all office staff, aged 35 to 55 years, from 20 London-based Civil Service departments.21 The response rate was 73% (6895 men and 3413 women); since recruitment there have been 7 further data collection phases. As we examined the association between working hours and sleep disturbances using 3 designs, the study comprises 3 separate samples: (1) for cross-sectional analyses, respondents with full-time work and data on all covariates at phase 5 (the baseline for this study) when sleep disturbances were first examined (n = 2,436 to 2,459 [depending on outcome]); (2) for prospective analyses with working hours measured once, all baseline respondents who were employed at baseline and at follow-up and free from sleep disturbance at baseline (n = 937 to 1,594); and (3) for prospective analyses with working hours measured at 2 time points; all above mentioned participants who had repeated measurements on working hours from phases 3 and 5 (n = 886 to 1,510; Figure 1). Informed consent was gained from all participants. The University College London Medical School Committee on the Ethics of Human Research approved the protocol.
Figure 1.
Sample selection procedure. aOutcome 1 = short sleep; outcome 2 = difficulty in falling asleep; outcome 3 = frequent waking during the night; outcome 4 = early waking; outcome 5 = waking without feeling refreshed.
Measures
Working hours were measured at phases 3 (1991–1994) and 5 (1997–1999), and sleep disturbances were measured at phases 5 and 7 (2002–2004). At phase 3, working hours were ascertained from the following question: “On an average weekday, approximately how many hours do you spend on the following activities: Work (daytime and work brought home)?” with response alternatives ranging from 1 to 12. At phase 5, working hours were ascertained from the following 2 questions: “How many hours do you work per average week in your main job, including work brought home?” and (for participants with more than one job), “How many hours do you work in an average week in your additional employment?” with response alternatives ranging from 0 to 100+ and 0 to 99, respectively. As there is no consensus regarding the definition of long working hours,14 we chose to follow a definition used in 2 recent studies showing an association between long working hours, poor sleep quality,22 and myocardial infarction.23 Thus the participants were divided into 3 groups: 1 = 35–40 hours; 2 = 41–55 hours; and 3 = more than 55 hours per week. For the measurement of repeated or long-term exposure to long working hours, an average of the 2 time points was calculated, and the participants were divided into 3 groups as described above. Further models with working hours entered as a continuous variable were also examined to asses whether the association between working hours and sleep disturbances was independent of the cut-points used.
Duration of sleep was assessed by asking the number of hours of sleep on an average week night. Less than 7 hours was considered as short sleep, as relatively short sleepers have been found to have an increased risk of mortality.24,25 The Jenkins Scale26 was used to indicate how often the participants had experienced sleep disturbances during the past month. This scale includes 4 questions on “having trouble falling asleep”, “waking up several times per night,” “having trouble staying asleep,” “waking up after the usual amount of sleep feeling tired and worn out” (i.e., waking without feeling refreshed); all items have a 6-point response scale (1 = not at all; 2 = 1–3 days; 3 = 4–7 days; 4 = 8–14 days; 5 = 15–21 days; 6 = 22–31 days). Each category of sleep disturbance was dichotomized as ≥ 8 days versus < 8 days. In our data, this cut-off point (corresponding at least 2–3.5 times /week) was chosen to approximate the ICD-10 diagnosis (F51.0)27 and other guidelines to assess insomnia,28 in which chronic insomnia is detected if the frequency of complaint is more than 2–3 times or ≥ 3 times a week.
Covariates
Sociodemographic factors, workload, behavioral factors and health conditions, found to be associated with sleep disturbances and/or working hours in previous research,12–20 were drawn from phase 5 and used as covariates in the analysis.12,13 Sociodemographics included sex, age, marital status (married/cohabited, single, divorced, or widowed), occupational grade level grouped into high (administrators, the top 7 unified grades), middle (executives, professionals and technical staff) and low (clerical and office support staff), and education (post-graduate, graduate, higher secondary, lower secondary, and no academic qualifications).
Psychological job demands,29 were assessed at phase 5, using 4 questions: “Do you have to work very fast?”; “Do you have to work very intensively?”; “Do you have enough time to do everything?”; “Do different groups at work demand things from you that you think are hard to combine?” Responses were given on a Likert scale of 1 = often to 4 = never / almost never. This scale (Cronbach α = 0.70) was calculated as the mean of reversed item scores, and the mean score was expressed as a percentage of the theoretical maximum (range from 0–100). Following the cut-points defined in previous papers from the Whitehall II study,30 participants were classified as having low, intermediate, or high job demands.
The (self-reported) health-related behaviors assessed were physical activity, alcohol consumption, and smoking. Body mass index (BMI, kg/m2), based on clinically assessed weight (in kg) and height (in m) according to standard guidelines, was used to classify individuals to the following 5 categories: 1 = BMI < 18.5 kg/m2; 2 = 18.5–24.9; 3 = 25.0–29.9; 4 = 30.0–34.9; 5 = ≥ 35.0.31 Twenty items were used to assess frequency and duration of participation in walking, cycling, sports, gardening, housework, home maintenance, and other activities. Frequency and duration of each activity were combined to compute hours per week of physical activity, and a compendium of activity energy costs was then used to assign each of the 20 physical activities assessed a metabolic equivalent.32 High, moderate, and low levels of physical activity were defined based on energy utilization as previously.32 Alcohol consumption was classified as up to 14 units/week for women and 21 units/week for men, and > 14 units for women and > 21 units for men.33 Smoking was assessed by a single question on whether the respondent was a current smoker.
Chronic physical disease was identified when at least one of the following conditions was present: (1) the participant reported any longstanding illnesses, diseases, or medical conditions for which he/she had sought treatment in the 12 months before the survey; (2) the participant had coronary heart disease (CHD) at phase 5 as previously defined30; (3) the participant had hypertension (systolic blood pressure ≥ 140 mm Hg and diastolic blood pressure ≥ 90 mm Hg or on antihypertensive treatment).30
Statistical Analysis
Differences in the covariates between the normal working hours and very long working hours at phase 5 were analyzed with the use of χ2 tests. Binary logistic regression analyses were used to calculate the odds ratios and their 95% confidence intervals (CIs) for prevalent and incident sleep disturbances. We examined cross-sectional associations between working hours and sleep disturbances among all full-time employed participants at phase 5. In subsequent analyses, only cases with no sleep disturbances at phase 5 were included to examine incident sleep disturbances at phase 7. First, we examined whether working hours measured at one time point (phase 5) predicted incident sleep disturbances at phase 7. Second, we examined whether working hours measured at 2 time points (phase 3 and phase 5) predicted incident sleep disturbances at phase 7. To examine linear trend in the association between working hours and sleep disturbances, we repeated the analysis treating working hours as a continuous variable and expressed as the effect per 10-hour increase in weekly working hours. We adjusted the analyses for covariates in a stepwise fashion; the first model was adjusted for sociodemographic factors (model I). Model I was then adjusted for physical health (model II) and then for health behaviors and body mass index (model III), and finally model III was also adjusted for job demands (model IV). The stepwise adjustment may allow us to assess the role of the covariates in the association between long working hours and sleep disturbances.
To explore potential bias due to missing data we undertook a sensitivity analysis in which we used multiple multivariate imputation34 using working hours, all covariates, and sleep disturbance variables to impute values for missing values in any variables with some missing data among all 3,664 eligible participants at baseline. We used switching regression in Stata as described by Royston,34 and carried out 20 cycles of regression switching and generated 20 imputation datasets. The multiple multivariate imputation approach creates a number of copies of the data (in this case 20 copies), each of which has values that are missing imputed with an appropriate level of randomness, using chained equations. The estimates are obtained by averaging across the results from each of these 20 datasets using Rubin's rules.34 The procedure takes account of uncertainty in the imputation as well as uncertainty due to random variation, as undertaken in all multivariable analyses.
We used SAS statistical software, version 9.1 (SAS Institute, Cary, NC) for all analyses, except the missing-data analysis which was carried out using STATA 9.0 statistical software.
RESULTS
Table 1 shows the characteristics of the participants according to their weekly working hours at phase 5. When compared with normal working hours, long working hours were more common in men, among those married or cohabiting, and those with high occupational grades, higher education, and job demands.
Table 1.
Characteristics of the Participants by Weekly Working Hours at Phase 5
| Working hours at phase 5 |
|||||
|---|---|---|---|---|---|
| Characteristics | All | 35–40 | 41–55 | >55 | P-value* |
| Age (years), Mean (SD) | 52.2 (4.2) | 52.6 (4.5) | 51.8 (3.9) | 52.5 (4.3) | 0.588 |
| Sex, n (%) | < 0.001 | ||||
| Men | 1,872 (76) | 680 (71) | 1,011 (78) | 181 (84) | |
| Women | 598 (24) | 282 (29) | 281 (22) | 35 (16) | |
| Marital status, n (%) | < 0.001 | ||||
| Married/cohabited | 1,930 (78) | 698 (73) | 1,049 (81) | 183 (85) | |
| Non-married/cohabited | 540 (22) | 264 (27) | 243 (19) | 33 (15) | |
| Occupational grade level, n (%) | < 0.001 | ||||
| High | 1,177 (48) | 264 (27) | 749 (58) | 164 (76) | |
| Middle | 1,075 (44) | 562 (58) | 465 (36) | 48 (22) | |
| Low | 218 (9) | 136 (14) | 78 (6) | 4 (2) | |
| Educational level, n (%) | < 0.001 | ||||
| I Post-graduate | 425 (17) | 116 (12) | 254 (20) | 55 (25) | |
| II Graduate | 628 (25) | 226 (23) | 340 (26) | 62 (29) | |
| III Higher secondary | 711 (29) | 275 (29) | 372 (29) | 64 (30) | |
| IV Lower secondary | 541 (22) | 259 (27) | 254 (20) | 28 (13) | |
| V No academic qualifications | 165 (7) | 86 (9) | 72 (6) | 7 (3) | |
| Physical disease, n (%) | 0.567 | ||||
| No | 1,292 (52) | 487 (51) | 691 (53) | 114 (53) | |
| Yes | 1,178 (48) | 475 (49) | 601 (47) | 102 (47) | |
| Body mass index (kg/m2), n (%) | 0.148 | ||||
| < 18.5 | 15 (1) | 6 (1) | 9 (1) | 0 (0) | |
| 18.5 < 25.0 | 1,031 (42) | 436 (45) | 513 (40) | 82 (38) | |
| ≥ 25.0 < 30.0 | 1,088 (44) | 402 (42) | 582 (45) | 104 (48) | |
| ≥ 30.0 < 35.0 | 274 (11) | 90 (9) | 156 (12) | 28 (13) | |
| ≥ 35.0 | 62 (3) | 28 (3) | 32 (2) | 2 (1) | |
| Exercise level, n (%) | 0.493 | ||||
| High | 1,183 (48) | 412 (43) | 671 (52) | 100 (46) | |
| Intermediate | 885 (36) | 368 (38) | 441 (34) | 76 (35) | |
| Low | 402 (16) | 182 (19) | 180 (14) | 40 (19) | |
| Alcohol use (units/week), n (%) | 0.064 | ||||
| 0–14 (women) / –21 (men) | 1,822 (74) | 739 (77) | 930 (72) | 153 (71) | |
| > 14 / 21 | 648 (26) | 223 (23) | 362 (28) | 63 (29) | |
| Smoking, n (%) | 0.608 | ||||
| No | 2,214 (90) | 857 (89) | 1162 (90) | 195 (90) | |
| Yes | 256 (10) | 105 (11) | 130 (10) | 21 (10) | |
| Job demands, n (%) | < 0.001 | ||||
| Low | 389 (16) | 241 (25) | 141 (11) | 7 (3) | |
| Intermediate | 1,102 (45) | 499 (52) | 543 (42) | 60 (28) | |
| High | 979 (40) | 222 (23) | 608 (47) | 149 (69) | |
P-value for difference between 35–40 hours and > 55 hours working groups
Table 2 presents cross-sectional associations between working hours and sleep disturbances at phase 5. In analyses adjusted for sex, marital status, occupational grade, and education, long ( > 55/week) working hours were related to an odds ratio of 2.63 for short sleep compared to normal working hours. The effect was slightly attenuated after adjustment for job demands. The result was replicated when working hours were entered into the models as a continuous variable: each extra 10 working hours per week increased the likelihood of short sleep by about 50%. We also found that working 41–55 hours per week, when compared to normal working hours, was related to a 35% greater likelihood of waking without feeling refreshed. We also found a linear association between working hours and waking without feeling refreshed, showing a 19% increase in risk per 10-hour increase in hours of work.
Table 2.
Cross-Sectional Associations Between Weekly Working Hours and Prevalent Sleep Disturbances at Phase 5
| Phase 5 | N / n of cases (%) |
Model I OR (95% CI)a |
Model II OR (95% CI)b |
Model III OR (95% CI)c |
Model IV OR (95% CI)d |
|---|---|---|---|---|---|
| Mean working hours | |||||
| Short sleep ( < 7 hours) | |||||
| 35–40 | 958/ 407 (42.5) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 1,287/ 622 (48.3) | 1.52 (1.27–1.82) | 1.52 (1.27–1.83) | 1.51 (1.26–1.81) | 1.39 (1.16–1.68) |
| > 55 | 214/ 128 (59.8) | 2.63 (1.92–3.62) | 2.64 (1.92–3.63) | 2.63 (1.91–3.63) | 2.25 (1.62–3.12) |
| Linear trende | 2,459/ 1,157 | 1.50 (1.34–1.69) | 1.50 (1.34–1.69) | 1.50 (1.33–1.68) | 1.39 (1.24–1.57) |
| Difficulty in falling asleep | |||||
| 35–40 | 952/ 64 (6.7) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 1,282/ 88 (6.9) | 1.26 (0.89–1.80) | 1.27 (0.89–1.81) | 1.24 (0.87–1.77) | 1.13 (0.78–1.64) |
| > 55 | 215/ 13 (6.1) | 1.28 (0.67–2.44) | 1.26 (0.66–2.41) | 1.28 (0.67–2.46) | 1.06 (0.54–2.06) |
| Linear trende | 2,449/ 165 | 1.17 (0.97–1.42) | 1.16 (0.96–1.41) | 1.17 (0.96–1.42) | 1.09 (0.88–1.34) |
| Frequent waking | |||||
| 35–40 | 951/ 265 (27.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 1,272 / 335 (26.3) | 1.00 (0.82–1.22) | 1.00 (0.82–1.23) | 1.00 (0.82–1.22) | 0.93 (0.76–1.15) |
| > 55 | 213/ 57 (26.8) | 1.03 (0.73–1.46) | 1.03 (0.72–1.46) | 1.03 (0.72–1.47) | 0.89 (0.62–1.28) |
| Linear trende | 2,436/ 657 | 1.00 (0.89–1.12) | 0.99 (0.88–1.12) | 0.99 (0.88–1.12) | 0.93 (0.82–1.06) |
| Early waking | |||||
| 35–40 | 948/ 170 (17.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 1,279/ 261 (20.4) | 1.30 (1.04–1.63) | 1.31 (1.04–1.64) | 1.31 (1.04–1.64) | 1.21 (0.96–1.53) |
| > 55 | 213/ 44 (20.7) | 1.40 (0.95–2.06) | 1.40 (0.94–2.06) | 1.41 (0.95–2.08) | 1.20 (0.81–1.80) |
| Linear trende | 2,440/ 475 | 1.10 (0.96–1.24) | 1.09 (0.96–1.24) | 1.10 (0.96–1.24) | 1.02 (0.89–1.17) |
| Waking without feeling refreshed | |||||
| 35–40 | 949/ 174 (18.3) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 1,282/ 269 (21.0) | 1.35 (1.07–1.69) | 1.36 (1.08–1.71) | 1.33 (1.06–1.67) | 1.19 (0.94–1.50) |
| > 55 | 214/ 42 (19.6) | 1.37 (0.93–2.04) | 1.37 (0.92–2.04) | 1.35 (0.91–2.01) | 1.06 (0.70–1.60) |
| Linear trende | 2,445/ 485 | 1.19 (1.05–1.35) | 1.19 (1.05–1.35) | 1.18 (1.04–1.34) | 1.08 (0.94–1.23) |
Model I: Adjusted for age, sex, marital status, occupational grade, and education;
Model II: Adjusted for Model I + chronic illness;
Model III: Adjusted for Model I + exercise level, body mass index, smoking, and alcohol use;
Model IV: Adjusted for Model I, II, III, and job demands;
Working hours entered into the model as a continuous variable (per 10-hour increase).
In cross-sectional analysis, several baseline covariates were associated with sleep disturbances. Short sleep was associated with, older age, female sex, lower occupational grade, higher BMI, moderate physical activity, and high job demands. Difficulty falling asleep was associated with female sex, smoking, and prevalent chronic disease. Frequent waking during the night was associated with age, female sex, prevalent chronic disease, heavy alcohol use, moderate physical activity, and high job demands. Early waking was associated with female sex, lower education, prevalent chronic disease, smoking, heavy alcohol use, and high job demands. Waking without feeling refreshed was associated with female sex, higher BMI, prevalent chronic disease, and high job demands. (Results not shown but available from authors).
Table 3 shows working hours at phase 5 as a predictor of incident sleep disturbances at phase 7. When compared to normal working hours, working > 55 hours a week was related to an odds ratio of 1.98 for incident short sleep, 3.68 for difficulty in falling asleep, and 1.98 for waking without feeling refreshed. Adjustment for covariates, especially job demands, attenuated these associations, except that for difficulty in falling asleep (final OR 4.12). When working hours was entered into the models as a continuous variable, a significant association was found with incident short sleep (OR 1.37), difficulty in falling asleep (OR 1.52), early waking (OR 1.23), and waking without feeling refreshed (OR 1.28). Of these, the association with short sleep and difficulty in falling asleep remained robust to adjustment for all covariates. Imputed analyses replicated the findings with regard to the association between the categorical and linear measure of working hours and difficulty in falling asleep, and with the linear (but not categorical) measure of working hours and early waking. Furthermore, an association between the categorical measure of working hours and early waking, which was not found in the original analysis, emerged in the imputed analysis (P-value 0.026). The association between working hours and incident waking without feeling refreshed was not replicated in the imputed data.
Table 3.
Longitudinal Associations of Mean Weekly Working Hours at Phase 5 with Incident Sleep Disturbances at Phase 7
| Phase 5 | N / n of cases(%) |
Model I OR (95% CI)a |
Model II OR (95% CI)b |
Model III OR (95% CI)c |
Model IV OR (95% CI)d |
|---|---|---|---|---|---|
| mean working hours | |||||
| Short sleep (< 7 hours) | |||||
| 35–40 | 386/ 78 (20.2) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 489/ 102 (20.9) | 1.09 (0.76–1.57) | 1.09 (0.76–1.57) | 1.06 (0.73–1.53) | 1.02 (0.70–1.49) |
| > 55 | 62/ 19 (30.7) | 1.98 (1.05–3.76) | 1.99 (1.05–3.77) | 1.86 (0.97–3.56) | 1.76 (0.90–3.45) |
| Linear trende | 937/ 199 | 1.37 (1.08–1.74) | 1.37 (1.08–1.74) | 1.33 (1.04–1.69) | 1.30 (1.01–1.68) |
| Difficulty in falling asleep | |||||
| 35–40 | 593/ 21 (3.5) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 856/ 34 (4.0) | 1.58 (0.88–2.82) | 1.63 (0.91–2.93) | 1.58 (0.88–2.84) | 1.69 (0.92–3.08) |
| > 55 | 145/ 10 (6.9) | 3.68 (1.58–8.58) | 3.82 (1.63–8.97) | 3.65 (1.55–8.56) | 4.12 (1.71–9.94) |
| Linear trende | 1,594/ 65 | 1.52 (1.19–1.95) | 1.54 (1.20–1.98) | 1.53 (1.19–1.96) | 1.57 (1.22–2.03) |
| Frequent waking | |||||
| 35–40 | 474/ 104 (21.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 686/ 148 (21.6) | 0.94 (0.69–1.27) | 0.94 (0.69–1.27) | 0.92 (0.67–1.25) | 0.87 (0.63–1.20) |
| > 55 | 111/ 23 (20.7) | 0.86 (0.50–1.46) | 0.85 (0.50–1.45) | 0.83 (0.48–1.42) | 0.77 (0.45–1.33) |
| Linear trende | 1,271/ 275 | 1.02 (0.85–1.22) | 1.01 (0.85–1.21) | 1.00 (0.84–1.20) | 0.97 (0.80–1.18) |
| Early waking | |||||
| 35–40 | 522/ 74 (14.2) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 741/ 101 (13.6) | 1.04 (0.73–1.46) | 1.06 (0.75–1.50) | 1.05 (0.74–1.48) | 1.01 (0.70–1.45) |
| > 55 | 123/ 23 (18.7) | 1.58 (0.91–2.73) | 1.60 (0.92–2.79) | 1.55 (0.89–2.70) | 1.44 (0.81–2.54) |
| Linear trende | 1,386/ 198 | 1.23 (1.02–1.47) | 1.24 (1.03–1.48) | 1.22 (1.02–1.46) | 1.19 (0.99–1.45) |
| Waking without feeling refreshed | |||||
| 35–40 | 518/ 52 (10.0) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 728/ 72 (9.9) | 1.14 (0.76–1.72) | 1.15 (0.77–1.73) | 1.14 (0.75–1.72) | 1.09 (0.72–1.67) |
| > 55 | 126/ 17 (13.5) | 1.98 (1.04–3.77) | 1.99 (1.05–3.79) | 1.94 (1.01–3.73) | 1.82 (0.93–3.54) |
| Linear trende | 1,372/ 141 | 1.28 (1.03–1.59) | 1.29 (1.04–1.60) | 1.27 (1.02–1.58) | 1.24 (0.99–1.56) |
Model I: Adjusted for age, sex, marital status, occupational grade, and education;
Model II: Adjusted for Model I + chronic illness;
Model III: Adjusted for Model I + exercise level, body mass index, smoking, and alcohol use;
Model IV: Adjusted for Model I, II, III, and job demands;
Working hours entered into the model as a continuous variable (per 10-hour increase)
Among participants with no sleep disturbances at baseline, several baseline covariates predicted incident sleep outcomes at follow-up: female sex, lower occupational grade, heavy alcohol use (decreased risk), higher BMI, and high job demands (P = 0.064) predicted shortened sleep; female sex and prevalent chronic disease predicted difficulty in falling asleep; higher occupational grade and higher BMI predicted frequent waking during the night; female sex and prevalent chronic disease predicted early waking; and younger age and female sex predicted waking without feeling refreshed. All sleep disturbances were more common in women except frequent waking during the night, which was equally common in both sexes (results not shown but available from authors).
Table 4 displays results for working hours measured at 2 time points (phase 3 and 5) as a predictor of incident sleep disturbances at phase 7. When compared with normal working hours, long working hours were associated with an odds ratio of 3.24 for shortened sleep among those who previously slept ≥ 7 hours per night, an odds ratio of 6.66 for difficulty in falling asleep, and 2.23 for early waking. When working hours were fitted into the models as a continuous variable, significant associations were found with shortened sleep (OR 1.64) and difficulty in falling asleep (OR 1.92). All these associations were attenuated to a certain degree after final adjustment for the covariates, but they remained statistically significant. Imputed analyses replicated the findings, except for early waking the statistical significance was marginal (p = 0.052).
Table 4.
Longitudinal Associations of Repeated Measures of Mean Weekly Working Hours at Phases 3 and 5 with Incident Sleep Disturbances at Phase 7
| Phase 3 and 5 | N / n of cases(%) |
Model IOR (95% CI)a |
Model IIOR (95% CI)b |
Model IIIOR (95% CI)c |
Model IVOR (95% CI)d |
|---|---|---|---|---|---|
| mean working hours | |||||
| Short sleep ( < 7 hours) | |||||
| 35–40 | 325/ 58 (17.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 525/ 122 (23.2) | 1.64 (1.11–2.41) | 1.64 (1.11–2.41) | 1.62 (1.09–2.41) | 1.55 (1.03–2.33) |
| > 55 | 36/ 12 (33.3) | 3.24 (1.45–7.27) | 3.26 (1.46–7.31) | 2.97 (1.30–6.77) | 2.80 (1.20–6.53) |
| Linear trende | 886/ 192 | 1.64 (1.21–2.23) | 1.64 (1.21–2.23) | 1.60 (1.17–2.19) | 1.56 (1.13–2.16) |
| Difficulty in falling asleep | |||||
| 35–40 | 488/ 18 (3.7) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 937/ 37 (4.0) | 1.63 (0.88–3.00) | 1.67 (0.90–3.09) | 1.62 (0.87–3.01) | 1.72 (0.91–3.25) |
| > 55 | 85/ 9 (10.6) | 6.66 (2.64–16.83) | 7.24 (2.82–18.54) | 6.82 (2.66-17.48) | 7.94 (2.97–21.25) |
| Linear trende | 1,510/ 64 | 1.92 (1.31–2.82) | 1.97 (1.33–2.91) | 1.94 (1.32–2.86) | 2.06 (1.37–3.08) |
| Frequent waking | |||||
| 35–40 | 390/ 80 (20.5) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 750/ 166 (22.1) | 1.08 (0.78–1.49) | 1.08 (0.78–1.49) | 1.04 (0.75–1.44) | 0.99 (0.71–1.39) |
| > 55 | 63/ 15 (23.8) | 1.17 (0.60–2.25) | 1.16 (0.60–2.25) | 1.10 (0.57–2.13) | 1.04 (0.53–2.03) |
| Linear trende | 1,203/ 261 | 1.05 (0.83–1.34) | 1.05 (0.82–1.33) | 1.02 (0.80–1.31) | 0.99 (0.77–1.28) |
| Early waking | |||||
| 35–40 | 419/ 55 (13.1) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 819/ 118 (14.4) | 1.26 (0.87–1.82) | 1.26 (0.87–1.82) | 1.28 (0.88–1.85) | 1.22 (0.83–1.80) |
| > 55 | 74/ 16 (21.6) | 2.23 (1.16–4.31) | 2.30 (1.19–4.46) | 2.16 (1.11–4.19) | 2.03 (1.03–4.02) |
| Linear trende | 1,312/ 189 | 1.26 (0.97–1.63) | 1.26 (0.97–1.64) | 1.25 (0.97–1.62) | 1.20 (0.92–1.58) |
| Waking without feeling refreshed | |||||
| 35–40 | 424/ 39 (9.2) | 1.00 | 1.00 | 1.00 | 1.00 |
| 41–55 | 800/ 87 (10.9) | 1.48 (0.96–2.28) | 1.48 (0.96–2.28) | 1.49 (0.96–2.31) | 1.41 (0.90–2.21) |
| > 55 | 75/ 8 (10.7) | 1.85 (0.79–4.34) | 1.87 (0.80–4.39) | 1.84 (0.78–4.35) | 1.71 (0.71–4.09) |
| Linear trende | 1,299/ 134 | 1.33 (0.98–1.81) | 1.33 (0.97–1.81) | 1.33 (0.98–1.82) | 1.28 (0.93–1.77) |
Model I: Adjusted for age, sex, marital status, occupational grade, and education;
Model II: Adjusted for Model I + chronic illness;
Model III: Adjusted for Model I + exercise level, body mass index, smoking, and alcohol use;
Model IV: Adjusted for Model I, II, III, and job demands;
Working hours entered into the model as a continuous variable (per 10-hour increase)
Table 5 summarizes the results of the associations between long working hours and incident sleep disturbances in the observed sample compared to the imputed sample. The most consistent evidence for the effects of working hours was found for difficulty in falling asleep. The evidence also indicates that repeat exposure to long working hours predicts shortened sleep. The associations with early morning wakening and waking without feeling refreshed were less consistent. Our findings indicate no association between long working hours and frequent waking during the night.
Table 5.
Summary of the Results from the Longitudinal Analyses of the Association Between Long Working Hours and Sleep Disturbances
| Incident sleep disturbance outcome |
Single exposure |
Repeat exposure |
||||||
|---|---|---|---|---|---|---|---|---|
| Categorical variable |
Continuous variable |
Categorical variable |
Continuous variable |
|||||
| Observed | Imputed | Observed | Imputed | Observed | Imputed | Observed | Imputed | |
| Shortened sleep | + | 0 | + | 0 | + | + | + | + |
| Difficulty in falling asleep | + | + | + | + | + | + | + | + |
| Frequent waking during the night | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Early waking | 0 | + | + | + | + | +a | 0 | 0 |
| Waking without feeling refreshed | + | 0 | + | 0 | 0 | 0 | 0 | 0 |
Note. + = positive association between long working hours and sleep disturbance (Model I)
0 = no association between long working hours and sleep disturbance (Model I)
P-value = 0.052
DISCUSSION
We examined long working hours as a predictor of disturbed sleep in a large occupational cohort of British civil servants. We found that > 55 working hours per week predicted incident sleep disturbances among employees free from such disturbance at baseline. The effects were slightly stronger for working hours measured repeatedly than at only one point in time suggesting a dose-response association between long work hours, incident shortened sleep, and difficulty in falling asleep (i.e., sleep-onset insomnia). We repeated all the analyses with working hours treated as a continuous variable and with datasets in which missing values were imputed. The results on long working hours and shortened sleep and difficulty in falling asleep were robust and not totally explained by known risk factors such as health behaviors or health status. However, adjustments suggested that high job demands may partially explain the association between long working hours and sleep disturbances. To our knowledge, this is the first prospective cohort study to examine the association between repeat exposure, i.e., long working hours measured at 2 time points, and subsequent sleep disturbances, independently of known risk factors.
A plausible causal pathway between long working hours and sleep disturbances may be poor recovery after work reflecting a lack of leisure time. At the end of a day at work, a certain time may be needed for recovery as a natural consequence of the fatigue resulting from efforts expended at work. Recovery after work may not only include sleep but also relaxation, such as spending time with family members and friends, resting, or reading. Relaxation has been recognized as an important prerequisite in the prevention of sleep-onset insomnia.35 As long working hours have been found to be associated with increased need of recovery after work,36 these employees would actually need more time to recover than workers with workdays of normal length. In our study, high job demands attenuated, but did not fully explain, the associations between long working hours and sleep disturbances. Indeed, adjustment for job demands might lead to overcontrolling because high demands and long hours may represent 2 indicators of the same stressful work environment rather than 2 distinct risk factors.
Our findings correspond with earlier research suggesting an association between long working hours and sleeping problems.2,4–7,11 As most of the earlier research has been cross-sectional, the temporal order between long working hours and sleep disturbances was unknown. Some studies have reported null findings.6,7 In our study, cross-sectional associations were found for short sleep and waking without feeling refreshed but not for difficulty in falling asleep and early waking, for which prospective associations were found. It is possible that some employees have been forced to shorten their working hours because of sleeping problems, and this may have diluted the associations in cross-sectional analysis.
At least 2 previous studies have examined working hours and sleep disturbances longitudinally. Ribet and Derriennic11 followed middle-aged French employees for 5 years and found that long working hours at baseline did not predict incident sleep disorders. However, participants who reported that they had worked overtime at some time in the past, but not at the time of the baseline survey, were at an increased risk of sleep disorder. A 4-year follow-up of Japanese manufacturing workers showed an association between increased overtime work and increased symptoms of fatigue assessed with the 36-item Short Form Medical Outcomes Survey (SF-36) vitality scale.10 However, that study had overlapping measurements of increase in fatigue and working hours. A strength of our study was the possibility to use non-overlapping measurements of working hours and sleep disturbances. Furthermore, examination of 5 distinct measures of sleep disturbances offered us the opportunity to consider whether long working hours are uniformly associated with sleep disturbances. This was not the case and the strongest effect was found for sleep-onset insomnia, with even stronger evidence generated by repeated or prolonged exposure to long working hours as opposed to working hours measured at one time point only.
Even though insomnia symptoms are associated with physical illnesses, insomnia has been shown to be a symptom of a psychological disorder 10 times as often as a physical illness.37,38 The most common diagnoses to which insomnia symptoms are related are the mood-, anxiety-, and substance-related disorders.38 In addition, some studies have shown an association between long working hours and mental ill health or fatigue symptoms.8–10,16 Because insomnia is a major symptom in depressive and anxiety disorders, we cannot exclude the possibility that the insomnia complaints in our study reflect symptoms of these disorders. Assessment of comorbidity between sleep disturbances and incidence of psychiatric disorders was beyond the scope of this study and should be considered as an important topic for future research. Further research should also clarify whether long working hours predict primary insomnia or organic sleep disorders such as somatic disease or sleep apnea, or whether insomnia is mainly a symptom of a mental disorder.
In our study, little evidence was found for the relationship between long working hours and “frequent waking during the night” or “waking without feeling refreshed”. Behavioral, psychiatric, and circadian disorders have been associated with trouble falling asleep and early awakening, whereas primary sleep disorders (such as sleep apnea) and other medical conditions have been more closely associated with frequent waking during the night and waking without feeling refreshed.35,37,39 Although there was no association between long working hours and chronic physical disease in our study and there is little evidence of that association in earlier studies,12,13 it is still possible that the association between long working hours and sleep complaints is partially accounted for by behavioral correlates (e.g., caffeine and alcohol) and comorbid organic disorders. We controlled for the effects of several confounding or mediating factors (body mass index, smoking, alcohol use, sociodemographic factors, longstanding illnesses, and job demands), but could not differentiate between sleep disturbances resulting from nonorganic insomnia and those related to organic sleep disorders, such as periodic limb movements, restless legs syndrome, or narcolepsy.40 However, the significant associations remained after we controlled for high body mass index, which is a correlate of obstructive sleep apnea. Measurements of organic sleep disorders would be needed in the future to further investigate these issues.
The interpretation of our results must take into account the reliability of self-reports of working hours and sleep disturbances. In the analyses using working hours measured at 2 time points, the phase 3 assessment was daily hours for weekdays while the phase 5 assessment included average number of work hours for the entire week, including weekends. Therefore the averaged measurement across these 2 time points cannot be considered as accurate as if exactly the same measures had been used at both phases. The strength of our design is, however, that the exposure and onset new sleep disorder were measured at different times; thus the potential for reversed causality was minimized.
We modeled sociodemographic, behavioral and biological covariates as time independent. This should be acknowledged as a potential limitation as it does not take into account the impact of possible changes in these factors on the risk of incident sleep disturbances. This may be a relevant question to address in future studies. Another issue involves potential bias arising from the fact that a relatively large proportion of participants had missing data and were excluded from the main analysis. However, similarity of the associations in the complete case analysis and multiple multivariate imputation analysis suggests that loss due to missing values is an unlikely source of major bias in this study.
In summary, this study indicates that long working hours predict onset of new sleep disturbances in a cohort of middle-aged employees, in particular sleep-onset insomnia and shortened sleep. Sleep disturbances can have a significant negative effect on an individual's quality of life, and the consequences associated with sleeping disturbances are serious including, for example, a higher risk of accidents due to fatigue, increased risk of all-cause mortality, cardiovascular diseases and mental disorders, increased sickness absence rates, and substantial medical care costs.25,41–45 The findings of the present study suggest that continued overtime work should be recognized as an independent risk factor for the development of sleep disturbances.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Financial support: The Whitehall II study has been supported by grants from the Medical Research Council; British Heart Foundation; Health and Safety Executive; Department of Health; National Heart Lung and Blood Institute (HL36310), US, NIH: National Institute on Aging (AG13196), US, NIH; Agency for Health Care Policy Research (HS06516); and the John D and Catherine T MacArthur Foundation Research Networks on Successful Midlife Development and Socio-economic Status and Health.
MK and JV are supported by the Academy of Finland (Projects no. 117604, 124271, 124322 and 129264); AS-M is supported by a ‘EURYI’ award from the European Science Foundation and MGM is supported by a MRC Research Professorship.
REFERENCES
- 1.Stewart R, Besset A, Bebbington P, et al. Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep. 2006;29:1391–7. doi: 10.1093/sleep/29.11.1391. [DOI] [PubMed] [Google Scholar]
- 2.Vaguer C, Van Bastelaer A. Working overtime. Statistics in Focus, Population and Social Conditions, European Communities. 2004 Nov [Google Scholar]
- 3.Åkerstedt T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. 2006;32:493–501. [PubMed] [Google Scholar]
- 4.Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: The Japanese Civil Servants Study. Sleep. 2006;29:206–16. doi: 10.1093/sleep/29.2.206. [DOI] [PubMed] [Google Scholar]
- 5.Kageyama T, Nishikido N, Kobayashi T, Kawagoe H. Estimated sleep debt and work stress in Japanese white-collar workers. Psychiatry Clin Neurosci. 2001 Jun;55:217–9. doi: 10.1046/j.1440-1819.2001.00831.x. [DOI] [PubMed] [Google Scholar]
- 6.Åkerstedt T, Fredlund P, Gillberg M, Jansson B. Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. J Psychosom Res. 2002;53:585–88. doi: 10.1016/s0022-3999(02)00447-6. [DOI] [PubMed] [Google Scholar]
- 7.Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours A cross-sectional study. J Psychosom Res. 2002;53:741–8. doi: 10.1016/s0022-3999(02)00333-1. [DOI] [PubMed] [Google Scholar]
- 8.Sasaki T, Iwasaki K, Mori I, Hisanaga N, Shibata E. Overtime, job stressors, sleep/rest, and fatigue of Japanese workers in a company. Ind Health. 2007;454:237–46. doi: 10.2486/indhealth.45.237. [DOI] [PubMed] [Google Scholar]
- 9.Park J, Kim Y, Chung HK, Hisanaga N. Long working hours and subjective fatigue symptoms. Ind Health. 2001;39:250–4. doi: 10.2486/indhealth.39.250. [DOI] [PubMed] [Google Scholar]
- 10.Yamazaki S, Fukuhara S, Suzukamo Y, et al. Lifestyle and work predictors of fatigue in Japanese manufacturing workers. Occup Med (Lond) 2007;57:262–9. doi: 10.1093/occmed/kqm006. [DOI] [PubMed] [Google Scholar]
- 11.Ribet C, Derriennic F. Age, working conditions, and sleep disorders: a longitudinal analysis in the French Cohort E.S.T.E.V. Sleep. 1999;22:491–504. [PubMed] [Google Scholar]
- 12.van der Hulst M. Long workhours and health. Scand J Work Environ Health. 2003;29:171–88. doi: 10.5271/sjweh.720. [DOI] [PubMed] [Google Scholar]
- 13.Sparks K, Cooper C, Fried Y, et al. The effects of hours of work on health: A meta-analytic review. J Occup Organ Psychol. 1997;70:391–408. [Google Scholar]
- 14.Caruso CC, Hitchcock EM, Dick RB, Russo JM, Schmit JM. Overtime and extended work shifts: Recent findings on illnesses, injuries, and health behaviors. NIOSH: Department of Health and Human Services. 2004 [Google Scholar]
- 15.Johnson JV, Lipscomb J. Long working hours, occupational health and the changing nature of work organization. Am J Ind Med. 2006;49:921–9. doi: 10.1002/ajim.20383. [DOI] [PubMed] [Google Scholar]
- 16.Fujino Y, Horie S, Hoshuyama T, Tsutsui T, Tanaka Y. A systematic review of working hours and mental health burden. Sangyo Eiseigaku Zasshi. 2006;48:87. doi: 10.1539/sangyoeisei.48.87. [DOI] [PubMed] [Google Scholar]
- 17.Raediker B, Janssen D, Schomann C, Nachreiner F. Extended working hours and health I. Chronobiol Int. 2006; 23:1305–16. doi: 10.1080/07420520601096245. [DOI] [PubMed] [Google Scholar]
- 18.Fletcher KE, Underwood W, Davis SQ, Mangrulkar RS, McMahon LF, Saint S. Effect of work hour reduction on residents' lives. A systematic review. JAMA. 2005;294:1088–100. doi: 10.1001/jama.294.9.1088. [DOI] [PubMed] [Google Scholar]
- 19.Owens JA. Sleep loss and fatigue in healthcare professionals. J Perinat Neonat Nurs. 2007;21:92–100. doi: 10.1097/01.JPN.0000270624.64584.9d. [DOI] [PubMed] [Google Scholar]
- 20.Shields M. Long working hours and health. Health Rep. 1999;11:33–48. [PubMed] [Google Scholar]
- 21.Marmot M, Brunner E. Cohort profile: The Whitehall II Study. Int J Epidemiol. 2005;34:251–6. doi: 10.1093/ije/dyh372. [DOI] [PubMed] [Google Scholar]
- 22.Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: The Japanese Civil Servants Study. Sleep. 2006;29:206–16. doi: 10.1093/sleep/29.2.206. [DOI] [PubMed] [Google Scholar]
- 23.Sokejima S, Kagamimori S. Working hours as a risk factor for acute myocardial infarction in Japan: case-control study. BMJ. 1998;317:775–80. doi: 10.1136/bmj.317.7161.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Dongen HPA, Vitellaro KM, Dinges DF. Individual differences in adult human sleep and wakefulness: Leitmotif for a research agenda. Sleep. 2005;28:479–96. doi: 10.1093/sleep/28.4.479. [DOI] [PubMed] [Google Scholar]
- 25.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;1;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jenkins D, Stanton BA, Niemcryk S, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–21. doi: 10.1016/0895-4356(88)90138-2. [DOI] [PubMed] [Google Scholar]
- 27.International statistical classification of diseases and related health problems, 10th revision. [(in Finnish, accessed December 17, 2008)];WHO. 2007 http://www.terveysportti.fi/terveysportti/icd10.koti.
- 28.Sateia MJ, Nowell PD. Insomnia. Lancet. 2004;364:1959–73. doi: 10.1016/S0140-6736(04)17480-1. [DOI] [PubMed] [Google Scholar]
- 29.Karasek RA, Theorell T. Stress, productivity, and the reconstruction of working life. New York: Basic Books; 1990. Healthy work. [Google Scholar]
- 30.Kivimäki M, Head J, Ferrie JE, et al. Hypertension is not the link between job strain and coronary heart disease in the Whitehall II Study. Am J Hypertens. 2007;20:1146–53. doi: 10.1016/j.amjhyper.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Obesity—Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity. Geneva: World Health Organization, WHO Technical Report Series. 2000;894 [PubMed] [Google Scholar]
- 32.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 33.White I, Altmann DR, Nanchahal K. Mortality in England and Wales attributable to any drinking, drinking above sensible limits and drinking above lowest risk level. Addiction. 2004;99:749–56. doi: 10.1111/j.1360-0443.2004.00710.x. [DOI] [PubMed] [Google Scholar]
- 34.Royston P. Multiple imputation of missing values. Stata J. 2004;4:227–41. [Google Scholar]
- 35.Viens M, De Koninck J, Mercier P, St-Onge M, Lorrain D. Trait anxiety and sleep-onset insomnia: Evaluation of treatment using anxiety management training. J Psychosom Res. 2003;54:31–7. doi: 10.1016/s0022-3999(02)00568-8. [DOI] [PubMed] [Google Scholar]
- 36.Jansen N, Kant I, van Amelsvoort L, Nijhuis F, van den Brandt P. Need for recovery from work: evaluating short-term effects of working hours, patterns and schedules. Ergonomics. 2003;46:664–80. doi: 10.1080/0014013031000085662. [DOI] [PubMed] [Google Scholar]
- 37.Harvey AG. Insomnia: symptom or diagnosis? Clin Psychol Rev. 2001;21:1037–59. doi: 10.1016/s0272-7358(00)00083-0. [DOI] [PubMed] [Google Scholar]
- 38.Ford D, Kamerow D. Epidemiologic study of sleep disturbances and psychiatric disorders. JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 39.Roth T, Roehrs T. Insomnia: epidemiology, characteristics, and consequences. Clin Cornerstone. 2003;5:5–15. doi: 10.1016/s1098-3597(03)90031-7. [DOI] [PubMed] [Google Scholar]
- 40.Aldrich M. Narcolepsy. N Engl J Med. 1990;323:389–94. doi: 10.1056/NEJM199008093230606. [DOI] [PubMed] [Google Scholar]
- 41.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–7. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 42.Partinen M, Putkonen PTS, Kaprio J, Koskenvuo M, Hilakivi I. Sleep disorders in relation to coronary heart disease. Acta Med Scand. 1982;660(Suppl.):69–83. doi: 10.1111/j.0954-6820.1982.tb00362.x. [DOI] [PubMed] [Google Scholar]
- 43.Vahtera J, Pentti J, Helenius H, Kivimäki M. Sleep disturbances as a predictor of long-term increase in sickness absence among employees after family death or illness. Sleep. 2006;29:673–82. doi: 10.1093/sleep/29.5.673. [DOI] [PubMed] [Google Scholar]
- 44.Walsh J, Engelhardt C. The direct economic costs of insomnia in the United States for 1995. Sleep. 1999;22(Suppl.2):S379–S93. [PubMed] [Google Scholar]
- 45.Westerlund H, Alexanderson K, Akerstedt T, Hanson LM, Theorell T, Kivimäki M. Work-related sleep disturbances and sickness absence in the Swedish working population, 1993-1999. Sleep. 2008;31:1169–77. [PMC free article] [PubMed] [Google Scholar]