Abstract
AIM: To assess the ability of 18F-fluorodeoxyglucose positron emission tomography/computer tomography (18F-FDG PET/CT) to differentiate between benign and malignant portal vein thrombosis in hepatocellular carcinoma (HCC) patients.
METHODS: Five consecutive patients who had HBV cirrhosis, biopsy-proven HCC, and thrombosis of the main portal vein and/or left/right portal vein on ultrasound (US), computer tomography (CT) or magnetic resonance imaging (MRI) were studied with 18F-FDG PET/CT. The presence or absence of a highly metabolic thrombus on 18F-FDG PET/CT was considered diagnostic for malignant or benign portal vein thrombosis, respectively. All patients were followed-up monthly with US, CT or MRI. Shrinkage of the thrombus or recanalization of the vessels on US, CT or MRI during follow-up was considered to be definitive evidence of the benign nature of the thrombosis, whereas enlargement of the thrombus, disruption of the vessel wall, and parenchymal infiltration over follow-up were considered to be consistent with malignancy. 18F-FDG PET/CT, and US, CT or MRI results were compared.
RESULTS: Follow-up (1 to 10 mo) showed signs of malignant thrombosis in 4 of the 5 patients. US, CT or MRI produced a true-positive result for malignancy in 4 of the patients, and a false-positive result in 1. 18F-FDG PET/CT showed a highly metabolic thrombus in 4 of the 5 patients. 18F-FDG PET/CT achieved a true-positive result in all 4 of these patients, and a true-negative result in the other patient. No false-positive result was observed using 18F-FDG PET/CT.
CONCLUSION: 18F-FDG PET/CT may be helpful in discriminating between benign and malignant portal vein thrombi. Patients may benefit from 18F-FDG PET/CT when portal vein thrombi can not be diagnosed exactly by US, CT or MRI.
Keywords: 18F-fluorodeoxyglucose, Positron emission tomography/computer tomography, Hepatocellular carcinoma, Portal vein tumor thrombus, Portal vein blood thrombus
INTRODUCTION
Hepatocellular carcinoma (HCC) carries a high risk of invasion of the portal vein. The detection and etiologic characterization of these thrombi are essential for treatment planning, particularly in patients with hepatic tumors, because malignant thrombosis is a negative factor in terms of prognosis[1,2]. Macroscopic tumor thrombi in the portal vein appear to occur during the terminal stage of HCC. The management of HCC with portal vein tumor thrombosis is complicated and controversial[3,4]. However, benign portal vein thrombi can usually be successfully managed with early identification[5]. Portal vein thrombosis (PVT) can be diagnosed noninvasively by using either real-time or duplex Doppler sonography, contrast-enhanced sonography, computer tomography (CT) or magnetic resonance imaging (MRI). Typical appearances of venous thrombosis include an intraluminal filling defect, peripheral ring-like enhancement and collateral venous channels[6,7]. Micro-invasive fine-needle aspiration (FNA) of a portal vein thrombus under ultrasound guidance also is an effective, well-tolerated method for the diagnosis of HCC patients with PVT[8,9] .
This pattern of 18F-FDG PET/CT has been reported in cases with different kinds of malignant tumor[10], while portal tumor growth and portal vein thrombosis identified by PET/CT in HCC patients have rarely been reported to date. We found highly metabolic thrombi of the portal vein on 18F-FDG PET/CT scans in four patients with HCC. 18F-FDG -avid lesions may represent malignant portal vein thrombosis. The importance of this finding for the diagnosis of and prognosis in HCC and the role of 18F-FDG PET/CT in the diagnosis of PVT are discussed.
MATERIALS AND METHODS
Patients
Between January 2007 and October 2007, five HCC patients with suspected portal vein tumor thrombus (PVTT) were assigned to PET/CT evaluation. Five consecutive patients who had HBV cirrhosis, biopsy-proven HCC, and thrombosis of the main portal vein and/or left/right portal vein on US, CT or MRI, were also studied by 18F-FDG PET/CT. PET/CT. US, CT or MRI results were compared with those at follow-up.
FDG PET/CT technique
The patients were asked to fast for at least 4 h before undergoing PET/CT. The blood glucose levels of these patients should have been within the normal range (0.7-1.2 g/L) prior to intravenous injection of 18F-FDG. The patients received an intravenous injection of 370-666 MBq (10-18 mCi) of 18F-FDG. Data acquisitions by an integrated PET/CT system (Discovery STE; GE Medical Systems, Milwaukee, WI, USA) were performed within 60 min after the injection. Data acquisition was performed as follows: CT scanning was performed first, from the head to the pelvic floor, with 110 kV, 110 mA, a tube rotation time of 0.5 s and a 3.3 mm section thickness, which was matched to the PET section thickness. Immediately after CT scanning, a PET emission scan that covered an identical transverse field of view was obtained. Acquisition time was 3 min per table position. PET image data sets were reconstructed iteratively by applying the CT data for attenuation correction, and co-registered images were displayed on a workstation.
Definitive diagnoses of thrombosis and thrombus malignancy
On integrated PET/CT images, thrombi were considered malignant if the maximum standardized uptake value (SUV) was greater than those of normal liver structures with a discrete margin and/or the 18F-FDG uptake was greater than that of the lumen of the descending aorta in the same axial slice. Thrombi were considered benign if the maximum SUV was lower than those of normal liver structures and/or the 18F-FDG uptake was lower than that of the lumen of the descending aorta in the same slice.
All patients were followed-up monthly by US, CT or MRI. Shrinkage of the thrombus and/or recanalization of the vessels on US, CT or MRI during follow-up was considered to be definitive evidence of the benign nature of the thrombosis, whereas enlargement of the thrombus, disruption of the vessel wall, and parenchymal infiltration over follow-up were considered to be consistent with malignancy.
RESULTS
Follow-up (1 to 10 mo) showed signs of malignant thrombosis in 4 out of 5 patients. US, CT or MRI produced a true-positive result for malignancy in 4 out of 5 patients, and a false-positive result in 1. 18F-FDG PET/CT was positive in four patients with malignant thrombi, and revealed a true-negative result in the remaining patient. 18F-FDG PET/CT showed highly metabolic thrombi in 4 of the 5 patients. No false-positive result was obtained using 18F-FDG PET/CT.
As shown in Figure 1, 2, 3, 4 and 5, the four malignant thrombi had SUVs of 3.0-11.5, which were higher than those of the normal liver parenchyma and the lumen of the descending aorta in the same axial slice. The SUVs of these malignant thrombi were lower than those of the HCC mass in the same axial slice. Thrombosis was significantly more common in patients with highly metabolic tumor lesions than in those with weakly metabolic tumor lesions. All four patients with malignant thrombi had advanced HCC. All of the malignant high metabolism thrombi had discrete margins in PET and PET/CT images.
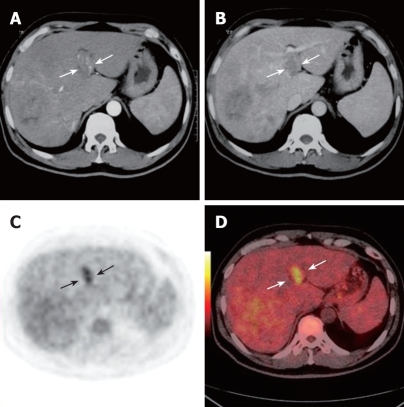
Figure 1.
Contrast CT scan showing right lobe and caudate lobe mass and portal vein thrombus in a 55-year-old man. During the arterial phase, the thrombus appears as an iso- to hypodense intraluminal area with dense linear enhancement (white arrows, A). A filling defect was detected in the left branch during the portal phases (white arrows, B). PET (black arrows, C) and PET/CT fused images (white arrows, D) reveal a highly metabolic thrombus in the left branch.
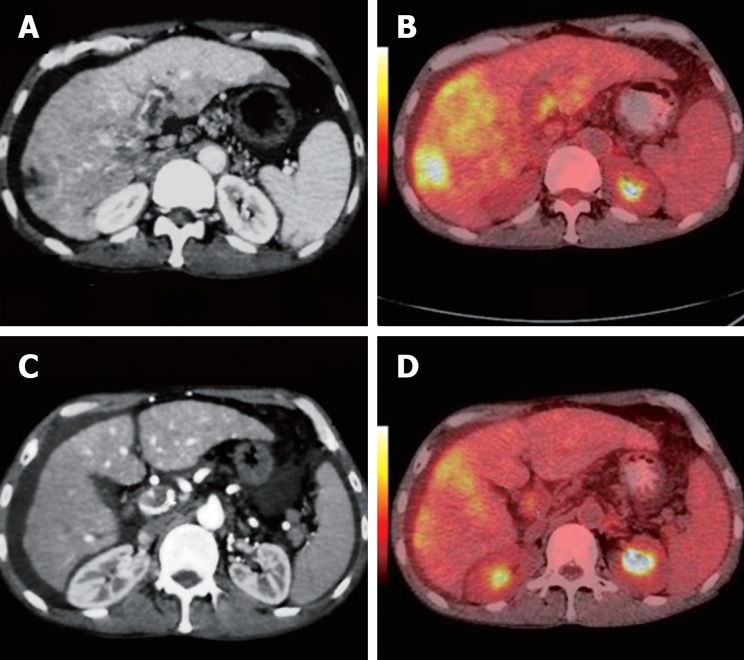
Figure 2.
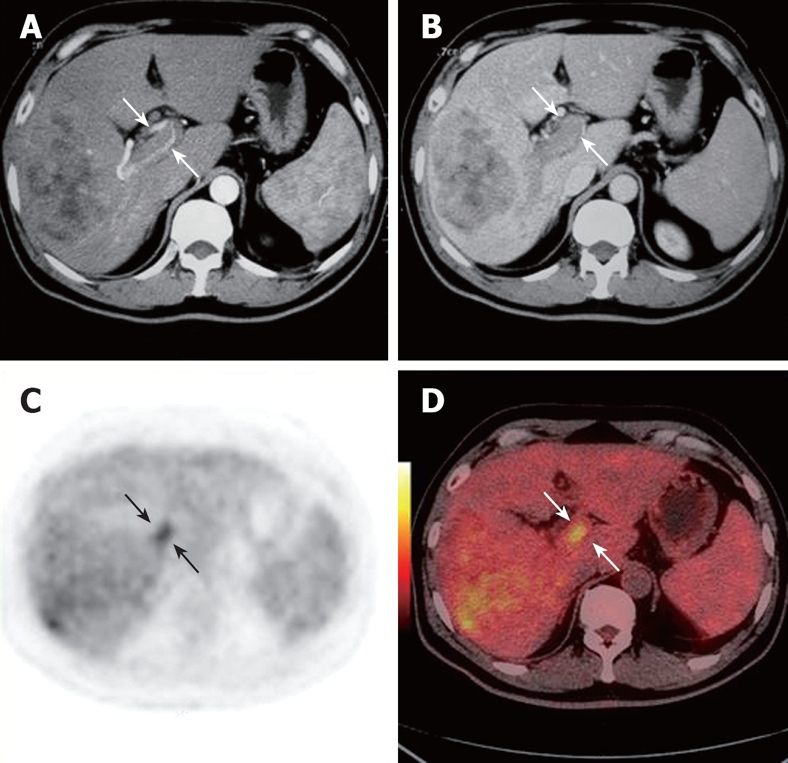
Contrast CT scan showing right lobe and caudate lobe mass and portal vein thrombus of the right branch in the same patient. During the arterial phase, the thrombus appears as an iso- to hypodense intraluminal area with dense linear enhancement (white arrows, A). A filling defect was detected in the right branch during the portal phases (white arrows, B). PET (black arrows, C) and PET/CT fused images (white arrows, D) reveal a highly metabolic thrombus in the left branch.
Figure 3.
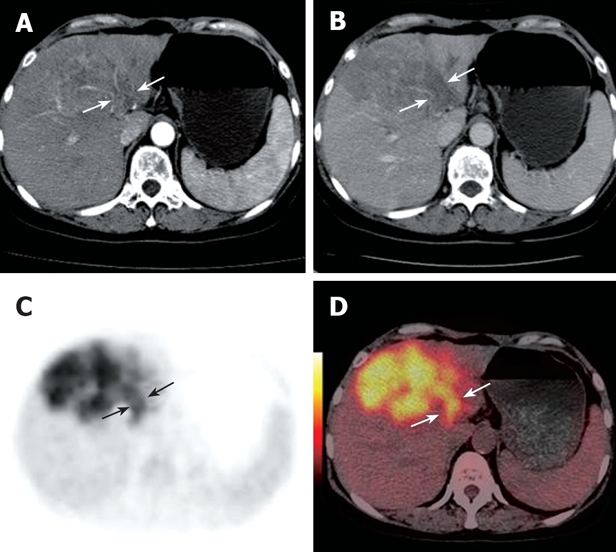
Contrast CT scan demonstrating a left lobe mass and portal vein thrombus in a 60-year-old woman. During the arterial phase, the thrombus appears as a hypodense intraluminal area with dense linear enhancement (white arrows, A). A filling defect was detected in the left branch during the portal phases (white arrows, B). PET (black arrows, C) and PET/CT fused images (white arrows, D) reveal a highly metabolic thrombus in the left branch.
Figure 4.
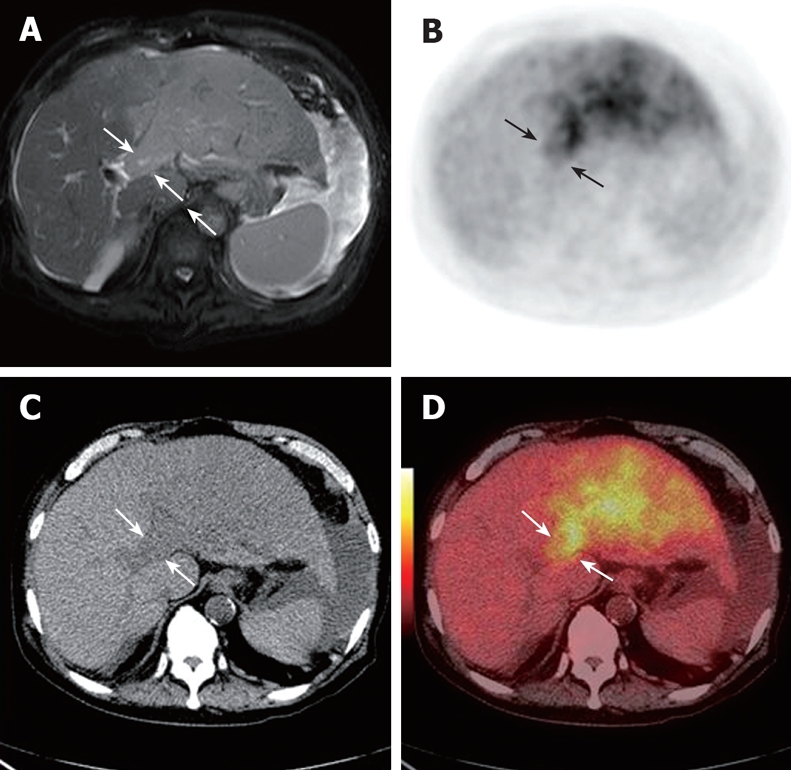
MRI scan showing a left lobe mass and portal vein thrombus in an 80-year-old man (white arrows, A). CT detected a low-density lesion in the left branch (white arrows, C). PET (black arrows, B) and PET/CT fused images (white arrows, D) reveal a highly metabolic thrombus in the left branch.
Figure 5.
Contrast CT scan showing a diffuse tumor and portal vein thrombus in a 44-year-old man. During the arterial phase, the thrombus appears as a hypodense intraluminal area with mild enhancement at the LV (white arrows, A) and PV (white arrows, C). PET/CT fused images reveal a highly metabolic mass and a highly metabolic thrombus at the LV and PV, respectively (white arrows, B, D).
The remaining patient was shown by ultrasound to have a portal thrombus in the left portal vein 6 mo after HCC resection. Malignant thrombus was suspected on contrast CT. Contrast-enhanced MRI demonstrated a thrombus in the left portal vein. In the PET/CT examination, the thrombus of the left portal vein had an SUV of 3.0, which was lower than those of the normal liver parenchyma and lumen of descending aorta. 18F-FDG PET/CT found no high 18F-FDG uptake in the left portal vein. The left portal vein was recanalized in the contrast MRI 10-mo follow-up (Figure 6). Finally, diagnosis of the left portal vein blood thrombus was established. Tables 1 and 2 summarize the clinical and image characteristics of the five patients.
Figure 6.
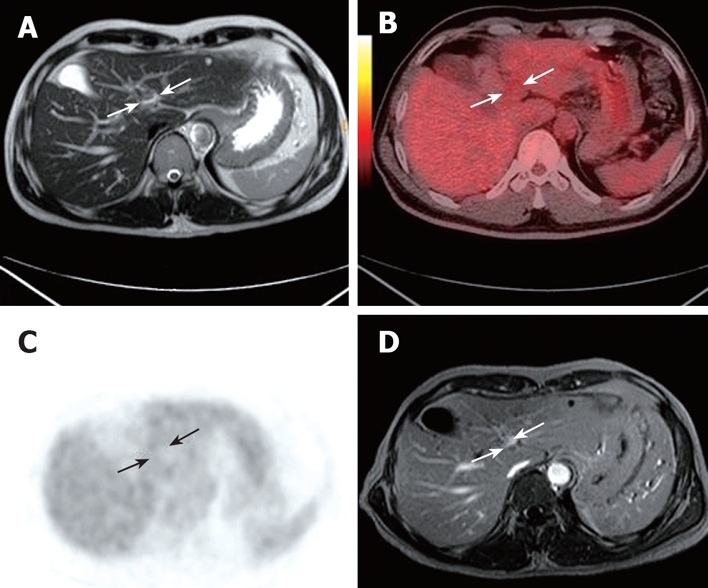
MRI showing a portal vein thrombus in a 44-year-old man six months after HCC resection (white arrows, A). PET/CT fused images (white arrows, B) and PET (black arrows, C) reveal no highly metabolic thrombus in the left branch. LP was recanalized in the contrast MRI at 10 mo follow-up (white arrows, D).
Table 1.
Clinical data on patients with high and low-metabolism thrombi of the portal vein
| Patient | Age (yr)/sex | Symptoms and signs | Laboratory data | Outcome |
| 1 | 55/M | No | AFP 5 ng/mL; abnormal HFT | Died of liver failure 2 mo after EPI |
| 2 | 60/F | Pain in right hypochondriac region | AFP > 1000 ng/mL; abnormal HFT | Died of hepatic failure 3 mo after TACE |
| 3 | 80/M | Cough | AFP 30 ng/mL; abnormal HFT | Died of renal failure 1 mo after admission |
| 4 | 65/M | Ascites | AFP > 1000 ng/mL; abnormal HFT | Died of liver failure 1 mo after admission |
| 5 | 44/M | Six mo after HCC resection | AFP normal; normal HFT | Recanalization |
AFP: Alpha-fetoprotein level; HFT: Hepatic function test.
Table 2.
Imaging data on patients with high and low-metabolism thrombi of the portal vein
| Patient |
US, CT, MRI findings |
FDG PET/CT SUV ratio |
|||
| Liver tumor location and size | Location of PV tumor thrombus | T/NT | Th/NT | Th/DAo | |
| 1 | Right and caudate lobe 11 cm × 13 cm | RPV | 4.8/3.0 | 5.2/3.0 | 5.2/2.1 |
| LPV | 4.8/5.9 | 5.9/3.0 | 5.9/2.1 | ||
| 2 | Right lobe 8.4 cm × 9.6 cm | LPV | 15.5/2.8 | 11.5/2.8 | 11.5/2.7 |
| 3 | Left lobe diffuse tumor | LPV | 9.0/3.6 | 7.9/3.6 | 7.9/2.4 |
| 4 | Both lobes diffuse tumor | LPV | 5.3/2.7 | 4.9/2.7 | 4.9/2.2 |
| PV | 5.3/2.7 | 3.4/2.7 | 3.4/2.2 | ||
| 5 | Six mo after right lobe lesion resection | LPV | - | 3. 0/3.0 | 3.0/2.0 |
SUV: Standardized uptake value; T: Tumor target; NT: Non tumor target; Th: Thrombi; Dao: Descending aorta; RPV: Right portal vein; LPV: Left portal vein; PV: Portal vein.
DISCUSSION
HCC tends to invade the intrahepatic vasculature, especially the portal vein. In clinically treated series, the rate of portal invasion is 34%-40%[11–13]. The natural history of untreated HCC is still poor, especially in patients with PVTT; the median survival of such patients was reported to be 2.7 mo, whereas survival in those without PVTT was 24.4 mo. PVTT causes acute portal hypertension, acute upper gastrointestinal hemorrhage, refractory ascites, and finally, acute liver function failure[14–16]. Our findings in the present study confirm portal vein thrombosis is a frequent complication of primary liver tumors, especially those with diameters larger than 3.0 cm, and diffuse tumors.
The reported increased sensitivity of PET/CT over CT has been attributed to the ability of FDG-PET to detect metabolic abnormalities that precede the morphologic changes seen by CT. The global (skull base to proximal thighs) nature of PET/CT study also contributes to increased sensitivity through the detection of distant metastases[17]. 18F-FDG PET/CT has become one of the standard imaging modalities in diagnosing and staging of tumors, and monitoring therapeutic efficacy in hepatic malignancies[18,19]. In this initial clinical experience, 18F-FDG PET/CT appears to be a reliable technique for evaluating the veins of the portal system thrombus. The main advantage of 18F-FDG PET/CT over conventional sonography techniques is its ability to assess the 18F-FDG metabolism activity of portal vein thrombi. Compared with US, the main limitations of no contrast 18F-FDG PET/CT is the absence of ability to observe the portal vein blood stream clearly along the main portal vein and its branch[20,21]. In the fourth patient, arterioportal shunt was confirmed by contrast CT. Thus, when 18F-FDG PET/CT-suspected PVTT is considered, a whole body 18F-FDG PET/CT examination combined with a contrast three-phase liver CT scan in the same PET/CT system is recommended.
Preliminary studies have already highlighted the potential value of 18F-FDG PET/CT in HCC staging and restaging for the TNM stage. It is helpful in early diagnosis and proper treatment, which are very important for patients with PVTT to prolong their lives[22–24]. The reported increased sensitivity of PET/CT over CT has been attributed to the ability of 18F-FDG PET to detect metabolic abnormalities that precede the morphologic changes seen by CT. The global (skull base to proximal thighs) nature of PET/CT study also contributes to increased sensitivity through the detection of distant metastases in HCC patients[25,26].
Dodd et al[27] reported that emboli might develop in the portal veins of hepatocirrhosis patients, and that these are mostly portal vein blood thrombi (PVBT), benign hepatic cells, or even bile duct epithelial cells. In recent years, some scholars have found that, during percutaneous ethanol injection, the alcohol that leaks out of the tumor and flows into the portal vein may cause a benign thrombus. 18F-FDG is not only uptaken by tumor cells, but also by normal cells[28–31] because benign hepatic cells and even bile duct epithelial cells in PVBT can uptake 18F-FDG, which may also have active metabolism in PET/CT images. Thus, further studies are needed to confirm the ability of 18F-FDG PET to discriminate PVTT and PVBT. The potential of this novel approach to characterize the veins of a portal system thrombus should be elucidated in large, ongoing clinical trials.
In conclusion, 18F-FDG PET/CT can be helpful in discriminating between benign and malignant portal vein thrombi. Patients may benefit from 18F-FDG PET/CT when portal vein thrombi can not be diagnosed exactly by US, CT or MRI.
COMMENTS
Background
To select an appropriate treatment regimen, it is essential to accurately characterize the nature of a thrombus in hepatocellular carcinoma (HCC) patients. This study investigated the ability of 18F-fluorodeoxyglucose positron emission tomography/computer tomography (18F-FDG PET/CT) to differentiate between benign and malignant portal vein thrombosis in HCC patients.
Research frontiers
PET and CT are becoming more and more widely available, and their application with 18F-FDG in oncology is beginning to be realized. However, the potential for 18F-FDG PET/CT in the diagnosis of benign and malignant portal vein thrombosis in HCC patients is undefined.
Innovations and breakthroughs
Thrombi with maximum standardized uptake values (SUVs) greater than those of normal liver structures with a discrete margin and/or an 18F-FDG uptake greater than that of the lumen of the descending aorta in the same axial slice were considered malignant. Thrombi with maximum SUVs lower than those of normal liver structures and/or an 18F-FDG uptake lower than that of the lumen of the descending aorta in the same slice were considered benign.
Applications
Our findings can be helpful in discriminating between benign and malignant portal vein thrombi, and can be used to select an appropriate treatment for HCC patients, especially when portal vein thrombi can not be diagnosed exactly by US, CT or MRI.
Peer review
In this study, the authors reported the clinical significance of 18F-FDG PET/CT for the discrimination between benign and malignant thrombi in advanced HCC. This manuscript arouses interest for readers and provides an important clue to diagnose or differentiate portal thrombus characteristics.
Peer reviewer: Akihito Tsubota, Assistant Professor, Institute of Clinical Medicine and Research, Jikei University School of Medicine, 163-1 Kashiwa-shita, Kashiwa, Chiba 277-8567, Japan
S- Editor Sun YL L- Editor McGowan D E- Editor Ma WH
References
- 1.Janssen HL, Wijnhoud A, Haagsma EB, van Uum SH, van Nieuwkerk CM, Adang RP, Chamuleau RA, van Hattum J, Vleggaar FP, Hansen BE, et al. Extrahepatic portal vein thrombosis: aetiology and determinants of survival. Gut. 2001;49:720–724. doi: 10.1136/gut.49.5.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou J, Tang ZY, Wu ZQ, Zhou XD, Ma ZC, Tan CJ, Shi YH, Yu Y, Qiu SJ, Fan J. Factors influencing survival in hepatocellular carcinoma patients with macroscopic portal vein tumor thrombosis after surgery, with special reference to time dependency: a single-center experience of 381 cases. Hepatogastroenterology. 2006;53:275–280. [PubMed] [Google Scholar]
- 3.Ikai I, Hatano E, Hasegawa S, Fujii H, Taura K, Uyama N, Shimahara Y. Prognostic index for patients with hepatocellular carcinoma combined with tumor thrombosis in the major portal vein. J Am Coll Surg. 2006;202:431–438. doi: 10.1016/j.jamcollsurg.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Minagawa M, Ikai I, Matsuyama Y, Yamaoka Y, Makuuchi M. Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,772 patients in Japan. Ann Surg. 2007;245:909–922. doi: 10.1097/01.sla.0000254368.65878.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radovich PA. Portal vein thrombosis and liver disease. J Vasc Nurs. 2000;18:1–5. doi: 10.1016/s1062-0303(00)90052-9. [DOI] [PubMed] [Google Scholar]
- 6.Shah ZK, McKernan MG, Hahn PF, Sahani DV. Enhancing and expansile portal vein thrombosis: value in the diagnosis of hepatocellular carcinoma in patients with multiple hepatic lesions. AJR Am J Roentgenol. 2007;188:1320–1323. doi: 10.2214/AJR.06.0134. [DOI] [PubMed] [Google Scholar]
- 7.Rogoveanu I, Vacaru D, Gheonea D, Georgescu CV, Comanescu V, Ciurea T. Diagnostic particularities in primitive diffuse form hepatocellular carcinoma associated with portal vein thrombosis. Rom J Morphol Embryol. 2005;46:317–321. [PubMed] [Google Scholar]
- 8.Lai R, Stephens V, Bardales R. Diagnosis and staging of hepatocellular carcinoma by EUS-FNA of a portal vein thrombus. Gastrointest Endosc. 2004;59:574–577. doi: 10.1016/s0016-5107(04)00007-0. [DOI] [PubMed] [Google Scholar]
- 9.Yang L, Lin LW, Lin XY, Gao SD, He YM, Yang FD, Xue ES, Lin XD. Ultrasound-guided fine needle aspiration biopsy in differential diagnosis of portal vein tumor thrombosis. Hepatobiliary Pancreat Dis Int. 2005;4:234–238. [PubMed] [Google Scholar]
- 10.Lai P, Bomanji JB, Mahmood S, Nagabhushan N, Syed R, Gacinovic S, Lee SM, Ell PJ. Detection of tumour thrombus by 18F-FDG-PET/CT imaging. Eur J Cancer Prev. 2007;16:90–94. doi: 10.1097/01.cej.0000220641.46470.77. [DOI] [PubMed] [Google Scholar]
- 11.Takizawa D, Kakizaki S, Sohara N, Sato K, Takagi H, Arai H, Katakai K, Kojima A, Matsuzaki Y, Mori M. Hepatocellular carcinoma with portal vein tumor thrombosis: clinical characteristics, prognosis, and patient survival analysis. Dig Dis Sci. 2007;52:3290–3295. doi: 10.1007/s10620-007-9808-2. [DOI] [PubMed] [Google Scholar]
- 12.Stuart KE, Anand AJ, Jenkins RL. Hepatocellular carcinoma in the United States. Prognostic features, treatment outcome, and survival. Cancer. 1996;77:2217–2222. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2217::AID-CNCR6>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 13.Fan J, Zhou J, Wu ZQ, Qiu SJ, Wang XY, Shi YH, Tang ZY. Efficacy of different treatment strategies for hepatocellular carcinoma with portal vein tumor thrombosis. World J Gastroenterol. 2005;11:1215–1219. doi: 10.3748/wjg.v11.i8.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grieco A, Pompili M, Caminiti G, Miele L, Covino M, Alfei B, Rapaccini GL, Gasbarrini G. Prognostic factors for survival in patients with early-intermediate hepatocellular carcinoma undergoing non-surgical therapy: comparison of Okuda, CLIP, and BCLC staging systems in a single Italian centre. Gut. 2005;54:411–418. doi: 10.1136/gut.2004.048124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martins A, Cortez-Pinto H, Marques-Vidal P, Mendes N, Silva S, Fatela N, Gloria H, Marinho R, Tavora I, Ramalho F, et al. Treatment and prognostic factors in patients with hepatocellular carcinoma. Liver Int. 2006;26:680–687. doi: 10.1111/j.1478-3231.2006.001285.x. [DOI] [PubMed] [Google Scholar]
- 16.Sakata H, Konishi M, Ryu M, Kinoshita T, Satake M, Moriyama N, Ochiai T. Prognostic factors for hepatocellular carcinoma presenting with macroscopic portal vein tumor thrombus. Hepatogastroenterology. 2004;51:1575–1580. [PubMed] [Google Scholar]
- 17.Czernin J, Allen-Auerbach M, Schelbert HR. Improvements in cancer staging with PET/CT: literature-based evidence as of September 2006. J Nucl Med. 2007;48 Suppl 1:78S–88S. [PubMed] [Google Scholar]
- 18.Messa C, Bettinardi V, Picchio M, Pelosi E, Landoni C, Gianolli L, Gilardi MC, Fazio F. PET/CT in diagnostic oncology. Q J Nucl Med Mol Imaging. 2004;48:66–75. [PubMed] [Google Scholar]
- 19.Sun L, Wu H, Guan YS. Positron emission tomography/computer tomography: challenge to conventional imaging modalities in evaluating primary and metastatic liver malignancies. World J Gastroenterol. 2007;13:2775–2783. doi: 10.3748/wjg.v13.i20.2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tarantino L, Francica G, Sordelli I, Esposito F, Giorgio A, Sorrentino P, de Stefano G, Di Sarno A, Ferraioli G, Sperlongano P. Diagnosis of benign and malignant portal vein thrombosis in cirrhotic patients with hepatocellular carcinoma: color Doppler US, contrast-enhanced US, and fine-needle biopsy. Abdom Imaging. 2006;31:537–544. doi: 10.1007/s00261-005-0150-x. [DOI] [PubMed] [Google Scholar]
- 21.Ueno N, Kawamura H, Takahashi H, Fujisawa N, Yoneda M, Kirikoshi H, Sakaguchi T, Saito S, Togo S. Characterization of portal vein thrombus with the use of contrast-enhanced sonography. J Ultrasound Med. 2006;25:1147–1152. doi: 10.7863/jum.2006.25.9.1147. [DOI] [PubMed] [Google Scholar]
- 22.Quaia E, Calliada F, Bertolotto M, Rossi S, Garioni L, Rosa L, Pozzi-Mucelli R. Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology. 2004;232:420–430. doi: 10.1148/radiol.2322031401. [DOI] [PubMed] [Google Scholar]
- 23.Sun L, Wu H, Pan WM, Guan YS. Positron emission tomography/computed tomography with (18)F-fluorodeo-xyglucose identifies tumor growth or thrombosis in the portal vein with hepatocellular carcinoma. World J Gastroenterol. 2007;13:4529–4532. doi: 10.3748/wjg.v13.i33.4529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.von Schulthess GK, Steinert HC, Hany TF. Integrated PET/CT: current applications and future directions. Radiology. 2006;238:405–422. doi: 10.1148/radiol.2382041977. [DOI] [PubMed] [Google Scholar]
- 25.Choi JY, Lee KS, Kwon OJ, Shim YM, Baek CH, Park K, Lee KH, Kim BT. Improved detection of second primary cancer using integrated [18F] fluorodeoxyglucose positron emission tomography and computed tomography for initial tumor staging. J Clin Oncol. 2005;23:7654–7659. doi: 10.1200/JCO.2005.01.4340. [DOI] [PubMed] [Google Scholar]
- 26.Fanti S, Franchi R, Battista G, Monetti N, Canini R. PET and PET-CT. State of the art and future prospects. Radiol Med (Torino) 2005;110:1–15. [PubMed] [Google Scholar]
- 27.Dodd GD 3rd, Memel DS, Baron RL, Eichner L, Santiguida LA. Portal vein thrombosis in patients with cirrhosis: does sonographic detection of intrathrombus flow allow differentiation of benign and malignant thrombus? AJR Am J Roentgenol. 1995;165:573–577. doi: 10.2214/ajr.165.3.7645473. [DOI] [PubMed] [Google Scholar]
- 28.Gorospe L, Raman S, Echeveste J, Avril N, Herrero Y, Herna Ndez S. Whole-body PET/CT: spectrum of physiological variants, artifacts and interpretative pitfalls in cancer patients. Nucl Med Commun. 2005;26:671–687. doi: 10.1097/01.mnm.0000171779.65284.eb. [DOI] [PubMed] [Google Scholar]
- 29.Metser U, Even-Sapir E. Increased (18)F-fluorodeoxyglucose uptake in benign, nonphysiologic lesions found on whole-body positron emission tomography/computed tomography (PET/CT): accumulated data from four years of experience with PET/CT. Semin Nucl Med. 2007;37:206–222. doi: 10.1053/j.semnuclmed.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum SJ, Lind T, Antoch G, Bockisch A. False-positive FDG PET uptake--the role of PET/CT. Eur Radiol. 2006;16:1054–1065. doi: 10.1007/s00330-005-0088-y. [DOI] [PubMed] [Google Scholar]
- 31.Kostakoglu L, Hardoff R, Mirtcheva R, Goldsmith SJ. PET-CT fusion imaging in differentiating physiologic from pathologic FDG uptake. Radiographics. 2004;24:1411–1431. doi: 10.1148/rg.245035725. [DOI] [PubMed] [Google Scholar]