Abstract
Insertion of percutaneous iliosacral screws with fluoroscopic guidance is associated with a relatively high screw malposition rate and long radiation exposure. We asked whether radiation exposure was reduced and screw position improved in patients having percutaneous iliosacral screw insertion using computer-assisted navigation compared with patients having conventional fluoroscopic screw placement. We inserted 26 screws in 24 patients using the navigation system and 35 screws in 32 patients using the conventional fluoroscopic technique. Two subgroups were analyzed, one in which only one iliosacral screw was placed and another with additional use of an external fixator. We determined screw positions by computed tomography and compared operation time, radiation exposure, and screw position. We observed no difference in operative times. Radiation exposure was reduced for the patients and operating room personnel with computer assistance. The postoperative computed tomography scan showed better screw position and fewer malpositioned screws in the three-dimensional navigated groups. Computer navigation reduced malposition rate and radiation exposure.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Treatment of unstable pelvic ring fractures by transiliosacral screw fixation after accurate reduction has gained general acceptance to rigidly stabilize pelvic fractures and posterior sacroiliac ligamentous injuries [6, 13, 15, 16, 19, 20, 22, 31]. Use of a percutaneous method avoids the high rate of wound necrosis and infection associated with open procedures [15, 19]. Routt et al. [19] described the advantages of this approach, particularly decreased blood loss and lower risk of infection [19]. To achieve proper screw fixation, various authors have used fluoroscopy [9, 20], computed tomography (CT) [9, 12, 17], fluoroscopic CT, and computer-assisted techniques [4, 11, 31]. Conventional fluoroscopy is the current standard for intraoperative observation [6, 12, 13, 15, 19, 20]. Lateral sacral images in combination with the anteroposterior, inlet, and outlet views are necessary. Patients and operating room personnel often are exposed to relatively high ionizing radiation [18]. Moreover, the image intensifier can only visualize one plane at a time, requiring the surgeon to perform a process of interpolation that may be associated with inherent errors. Identifying the correct entry point for the screw and the correct angle of implantation in all planes is crucial. However, proper implantation of the screws without perforation of the sacrum or sacral foramina is difficult and requires detailed anatomic knowledge and extensive surgical experience. The technical problems of screw placement are compounded by difficulties in radiographic interpretation and variations in the anatomy of the posterior pelvis [10].
Incorrect conventional placement of iliosacral screws may result in implant-related and neurovascular complications [1, 24, 25]. Screw malposition rates with fluoroscopic guidance have been reported to range from 2% to 15% [13, 28], with an incidence of neurologic injury between 0.5% and 7.7% [32]. Malposition of the screw by as little as 4° can cause damage to neurovascular structures [28].
Some authors have reported their clinical experiences or results of cadaver studies using navigated imaging systems [2, 7, 8, 14, 21, 23, 26, 27], but these navigation systems are not yet established for percutaneous iliosacral screw placement in pelvic surgery. Briem et al. [5] noted nine publications were listed concerning navigated surgery of the dorsal pelvic ring. In seven publications, the authors used two-dimensional fluoroscopic navigation and only two studies described three-dimensional computer-assisted screw placement in cadavers or plastic pelves [2, 11].
We therefore asked whether the transection until suture time and radiation exposure were reduced and screw position improved in patients having percutaneous iliosacral screw insertion using computer-assisted navigation compared with patients having conventional fluoroscopic screw placement.
Materials and Methods
We prospectively collected the data of our patients with unstable fractures of the posterior pelvic ring, including only Types B and C fractures according to the classification of Tile and Pennal [29]. Even with minimal or no dislocation, all Tile and Pennal Types B and C fractures are unstable and have a high risk of dislocation under weightbearing. We excluded patients with dislocated fractures who underwent open reduction and stabilization. Also excluded were patients who underwent additional operative procedures, patients who underwent revisions, or patients who had percutaneous screw placement attributable to other reasons (eg, pseudarthrosis). Twenty four patients (26 screws) with no or minimal dislocation of the posterior pelvic ring (after closed reduction, if necessary) were treated with navigated iliosacral screw placement from February 2006 to April 2008. We compared radiation exposure and screw position of these patients with those of 32 patients (35 screws) who had conventional fluoroscopy (conventional group) from December 2000 to February 2006 before the navigation system was available in our department. Patients in the navigated and conventional groups were treated with two different operative procedures and therefore divided into two subgroups for additional analysis: (1) patients receiving only an iliosacral screw (13 navigated screws versus 12 conventional screws), and (2) patients also receiving intraoperatively an external fixator for stability of the anterior pelvic ring (13 navigated screws versus 23 conventional screws).
The ages of patients in the navigated and conventional groups (mean ± standard deviation, 35 ± 23 years versus 46 ± 20 years) were similar (p = 0.017), as were gender ratios (male 60% versus 56%) (p = 0.015). The causes of accidents or fractures (navigated group versus conventional group) included car (39% versus 27%), fall greater than 3 m (36% versus 54%), pedestrian (18% versus 5%), crush (4% versus 2%), bicycle (4% versus 0%), and motorcycle (0% versus 15%). There were no differences between the navigated and conventional groups in Injury Severity Score [3] (31 ± 14 [range, 9–57] versus 26 ± 17 [range, 9–59]) (p = 0.088) or percentage of polytraumatized patients (Injury Severity Score of 16 or greater) (79% versus 62%) (p = 0.066). No difference (p = 0.087) was detected between the navigated and conventional groups regarding distribution of Tile and Pennal Types B and C fractures (75% Type B and 25% Type C versus 60% Type B and 40% Type C).
Seven trauma surgeons performed the implantations in the navigation group and nine trauma surgeons performed implantations in the conventional group. The level of expertise between surgeons in the two groups was not different (p = 0.24) (Table 1).
Table 1.
Number of screws implanted by surgeons in the navigation and conventional groups
| Surgeon | Number of screws implanted | Total number of screws implanted (screws included + screws excluded) | |||
|---|---|---|---|---|---|
| Navigated group | Conventional group | 2/2006–4/2008 (Navigation) | 12/2000–2/2006 (Conventional) | 12/2000–4/2008 (Total) | |
| 1 | 2 | — | 4 | — | 4 |
| 2 | 8 | 3 | 15 | 14 | 29 |
| 3 | 6 | 2 | 7 | 6 | 13 |
| 4 | 1 | 4 | 3 | 4 | 7 |
| 5 | 1 | 7 | 1 | 24 | 25 |
| 6 | 7 | 1 | 9 | 1 | 10 |
| 7 | 1 | 5 | 1 | 18 | 19 |
| 8 | — | 2 | — | 17 | 17 |
| 9 | — | 8 | — | 17 | 17 |
| 10 | — | 3 | — | 9 | 9 |
| Total | Total 26 | Total 35 | Mean ± SD 5.7 ± 5.1 | Mean ± SD 12.2 ± 7.6 | Mean ± SD 15.3 ± 9.4 |
| 7 (navigation) | |||||
| 9 (conventional) | |||||
There is no difference in the average screw implantation experience of surgeons in the navigated and conventional groups (p = 0.24); SD = standard deviation.
For navigated implantation, all screws were placed percutaneously with the patient in the supine position. The navigation system VectorVision® (BrainLAB, Munich, Germany) was connected to the Iso-C3D (Siremobil®; Siemens, Erlangen, Germany), which rotates 190° around the operative field and needs to be positioned isocentrically to the region of interest in anteroposterior and lateral projections. For a continuous accuracy check of the navigation system, the rigid body (reference clamp) was fixed either on the already placed external fixator or on two percutaneously placed 3.0-mm Kirschner wires in the iliac crest at the contralateral site. Afterward, Iso-C3D imaging was performed (duration approximately 90 seconds) after covering the operation field. During the Iso-C3D scan, the operating room personnel left the operating room. Afterward, multiplanar reconstructions were generated during one automated rotating scanning procedure. After the scans were performed, the images were transferred to the navigation system. In the next step, an accuracy check was performed by placing the tip of the navigation pointer on the ilium, checking the matching of the virtual navigation picture with the real touched bony surface. The screw position was planned using the three-dimensional data set. A trajectory was planned for guidance of the navigated drill guide based on the reconstructions, and afterward, drilling of a 3.2-mm hole controlled by navigation was performed. A guide wire was inserted 1 to 2 cm further. We then drilled holes with a cannulated 5-mm drill and inserted the screws using a 7.0-mm cannulated screw and removed the Kirschner wire.
For conventional fluoroscopy, all screws were placed percutaneously with the patient in the supine position according to the technique of Matta and Saucedo [16]. Standard lateral, inlet, and outlet fluoroscopic pelvic views were obtained. By rotating these views, a guide wire was placed across the ileum into the S1 vertebra. The inlet view shows the orientation of screws relative to the coronal plane and extraosseous screws extending anterior to the ala, whereas the outlet view elucidates placement of screws relative to the transverse plane and extraosseous screw tips extending into the sacral foramina or superior to the ala. The correct screw position was considered parallel to the superior S1 vertebral end plate midway between the S1 superior end plate and the S1 neuroforamina. Each guide wire was advanced just beyond the sacral midline. We then inserted a cannulated 5-mm drill followed by a 7.0-mm cannulated screw. The Kirschner wire then was removed.
A postoperative CT-based analysis of localization of the transiliosacral screw was evaluated by one independent radiologist (EK) not involved in the treatment. An ideal screw position was considered entirely within the cortical margins of the sacrum and parallel to the respective sacral end plate and the S1 neuroforamina. Perforations were graded according to an established classification method used for correct pedicle screw placement [23]: Grade 0, no perforation; Grade 1, perforation less than 2 mm; Grade 2, perforation between 2 and 4 mm; and Grade 3, perforation greater than 4 mm.
Differences in the transection until suture time and radiation time and dose between the groups were determined by the t test. Differences in the percentage of correct screw positions between the groups were determined by the Wilcoxon signed rank test. For statistical analysis (t test, Wilcoxon signed rank test), SigmaStat® 3.1 (Systat Software GmbH, Erkrath, Germany) was used and Microsoft® Excel® (Microsoft Corp, Redmond, WA) was used to create figures.
Results
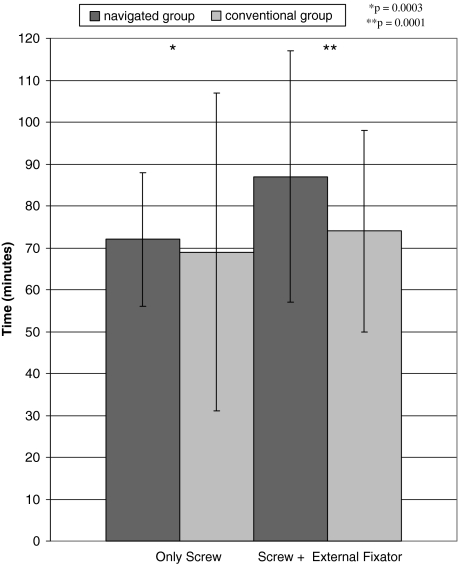
In the groups treated only by screw implantation, the time from transection until suture was similar (p = 0.42) in the navigated group (72 ± 16 minutes; range, 52–106 minutes) and conventional group (69 ± 38 minutes; range, 30–133 minutes) (Fig. 1). In the groups receiving an additional external fixator, the time from transection until suture was slightly longer (p = 0.077) in the navigated group (87 ± 30 minutes; range, 41–142 minutes) than in the conventional group (74 ± 24 minutes; range, 37–114 minutes) (Fig. 1).
Fig. 1.
A graph shows the transection until suture time in minutes in the navigated and conventional groups. In the groups of patients receiving only a screw, the times were similar (p = 0.42) in the navigation and conventional groups. In the groups receiving an additional external fixator, the time was slightly longer (p = 0.08) in the navigated group than in the conventional group.
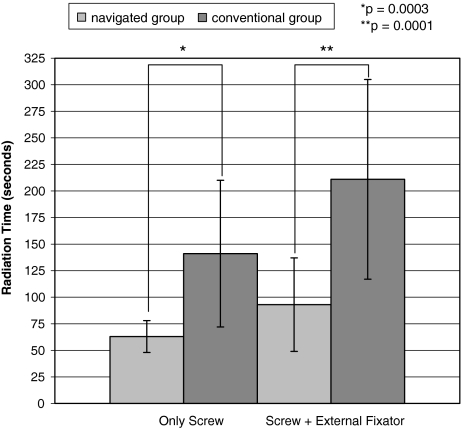
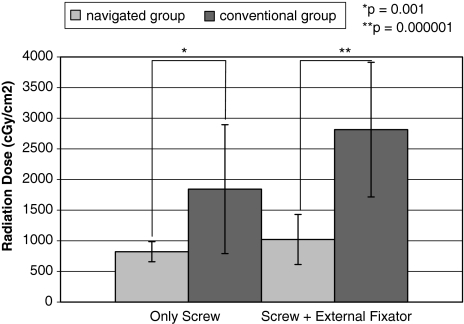
In the groups of patients receiving only a screw, the radiation time (p = 0.003) and dose (p = 0.001) were decreased in the navigated group (63 ± 15 seconds; range, 36–84 seconds; 822 ± 164 cGy/cm2; range, 542–1145 cGy/cm2) compared with time and dose in the conventional group (141 ± 69 seconds; range, 42–252 seconds; 1843 ± 1052 cGy/cm2; range, 600–3811 cGycm2) (Figs. 2, 3). In the groups receiving an additional external fixator, the radiation time (p = 0.0001) and dose (p = 0.000001) in the navigated group (93 ± 44 seconds; range, 46–216 seconds; 1021 ± 408 cGy/cm2; range, 479–1650 cGy/cm2) were decreased compared with time and dose in the conventional group (211 ± 94 seconds; range, 21–384 seconds; 2814 ± 1099 cGy/cm2; range, 1312–5464 cGy/cm2) (Figs. 2, 3).
Fig. 2.
A graph shows intraoperative radiation times measured in seconds in the navigated and conventional groups. In the groups of patients receiving only a screw, the time was shorter (p = 0.0003) in the navigated group than in the conventional group. In the groups receiving an external fixator, the time was shorter (p = 0.0001) in the navigated group than in the conventional group.
Fig. 3.
A graph shows the intraoperative radiation doses measured in cGy/cm2 in the navigated and conventional groups. In the groups of patients receiving only a screw, the dose was less (p = 0.001) in the navigated group than in the conventional group. In the groups receiving an external fixator, the dose was less (p = 0.000001) in the navigated group than in the conventional group.
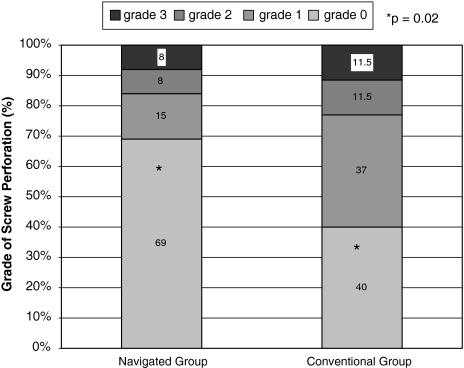
We observed a greater percentage of correct screw positions (p = 0.02) in the navigated group with Grade 0 in 69% (Grade 1, 15%; Grade 2, 8%; Grade 3, 8%) compared with correct screw position in the conventional group with Grade 0 in 40% (Grade 1, 37%; Grade 2, 11.5%; Grade 3, 11.5%) (Fig. 4).
Fig. 4.
A graph shows the screw position in the navigated and conventional groups. The results for correct screw position in the navigated group were greater (p = 0.02) than in the conventional group.
Discussion
Insertion of percutaneous iliosacral screws with fluoroscopic guidance is associated with a relatively high screw malposition rate and long radiation exposure. Navigation offers the possibility of reducing radiation exposure and improving screw position. We therefore asked whether radiation exposure for the patient and/or personnel could be achieved by a similar operation time and more precise screw positions and therefore fewer screw perforations would be expected.
Limitations of this study were the relatively small number of patients. We could include only pelvic fractures in which treatment with percutaneous screw implantation or implantation of an additional external fixator was indicated. All fractures needing open reduction therefore were excluded. Moreover, we had to exclude all screw implantations that were part of complex operative procedures because the specific parameters (operation time, skin-to-skin time, radiation time, and dose) for the single-screw implantation were not documented in the retrospective control group. However, the injury is relatively infrequent yet the number of patients was still high enough to show statistical differences in the analyzed parameters. Another limitation is the fact that the techniques were performed sequentially, so in theory the experience level of the surgeons involved would have been better for the navigated group, with that group having an advantage for proper placement. However, because our department is a teaching institution of a university hospital, there is a high fluctuation rate among surgeons. Therefore, only 50% of the surgeons participated in both groups (navigated/conventional). The average number of screws placed per surgeon by the time of implantation did not differ (p = 0.24) between 2000 to 2006 and 2006 to 2008 (Table 1). Whenever a novel intraoperative technique (eg, navigation) is introduced in clinical medicine, there are concerns about its increasing operating and overall setup times. Unfortunately, given our retrospective analysis, we found no data recorded regarding setup time in our records. Therefore, we cannot compare this parameter. Generally, it takes approximately 10 extra minutes to get the navigation system set up in the operating room and to prepare an additional sterile operation table for the navigation equipment.
The number of screws required for pelvic ring injuries remains controversial. Ebraheim et al. [9] suggested placement of one screw through the S1 pedicle into the vertebral body is safer, whereas others recommended placement of two screws [5, 8, 28]. In our treatment algorithm, we used only one screw in all patients. In the classification of Tile and Pennal [29], a Type B fracture is defined as unstable for rotational movement and a Type C fracture is defined as unstable for vertical and rotational movements because of the disturbance of the integrity of the pelvic ring. Even with no or minimal dislocation, these fractures are unstable and have a high risk of dislocation under weightbearing. Without operative stabilization, patients with these fractures have a high risk for fracture dislocation under weightbearing. Nonoperative treatment of an unstable fracture of the pelvic ring would result in a patient who is bedridden for several weeks. Nevertheless, early mobilization is an accepted primary goal of any kind of trauma treatment. In accordance with the literature, we therefore stabilize Tile and Pennal Types B and C fractures with no or minimal dislocation and then mobilize the patient immediately with partial weightbearing on the affected side. All screws are removed after 3 to 4 months to prevent continuous blocking of the iliosacral joint. All fractures in this study healed uneventfully with solid bony fusion of the pelvic ring at the time of implant removal.
We achieved reductions of the mean radiation dose and time using the navigation system. Correct positioning of the C-arm for projections described by Matta and Saucedo [16] during conventional fluoroscopy may be difficult to achieve. This may be associated with a high radiation time. These projections are not needed with the navigation system. This reduced the radiation dose for the patients, surgeons, and operating room personnel. Of note, the operating room personnel regularly left the operating room when the Iso-C3D scan was started, so they received no radiation dose at all during the scanning procedure. Radiation times for conventional screw placement have been reported to vary between 1.8 and 7.3 minutes [5, 7]. We found mean times of 141 and 211 seconds for the conventional group. In the navigated group, the times were reduced to 63 and 93 seconds. These data correspond to the results of earlier studies, which indicated lower radiation exposure using computer-assisted surgery [21, 30].
Retrospectively, we suspect the Grades 2 and 3 malpositions of the navigated group were the result of technical mistakes using the navigation system (eg, an unrecognized change of position of the data reference base that could result in a mismatch of the three-dimensional navigation pictures to the real position of the instruments). An unnoticed manipulation of the reference array can lead to a complete shift of the image.
Screw malposition rates with fluoroscopic guidance have been reported to range from 2% to 15% [13, 28], with an incidence of neurologic injury between 0.5% and 7.7% [32]. Accuracy of computer-guided transiliosacral screw implantation has been reported to be sufficiently effective and safe in preclinical work [4, 31] to warrant clinical trials. One cadaver study comparing fluoroscopic and computer-assisted surgery reported two of 10 screws penetrated the cortex equally in both groups [8]. Our data suggest better screw placement when using the navigation system. This was achieved with less radiation and similar operation time compared with the conventional procedure. For surgeons with no experience using the navigation system, we recommend initial practice with cadaver or animal models to achieve the needed safety for the complex technical steps and to be aware of possible pitfalls.
Using a navigation system for percutaneous iliosacral screw insertion reduces the malposition rate and radiation exposure for the patient and operating room personnel. However, use of a navigation system does not guarantee 100% correct screw placement. Therefore, we recommend using three-dimensional navigation to insert iliosacral screws in the presence of a surgeon who is experienced with navigation surgery. Also, correct placement of the screws should be controlled intraoperatively using the three-dimensional image intensifier.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution either has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Altman DT, Jones CB, Routt ML Jr. Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999;13:220–227. [DOI] [PubMed]
- 2.Arand M, Kinzl L, Gebhard F. Computer-guidance in percutaneous screw stabilization of the iliosacral joint. Clin Orthop Relat Res. 2004;422:201–207. [DOI] [PubMed]
- 3.Baker SP, O’Neill B, Haddon W Jr, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [DOI] [PubMed]
- 4.Barrick EF, O’Mara JW, Lane HE 3rd. Iliosacral screw insertion using computer-assisted CT image guidance: a laboratory study. Comput Aided Surg. 1998;3:289–296. [DOI] [PubMed]
- 5.Briem D, Windolf J, Rueger JM. [Percutaneous, 2D-fluoroscopic navigated iliosacral screw placement in the supine position: technique, possibilities, and limits] [in German]. Unfallchirurg. 2007;110:393–401. [DOI] [PubMed]
- 6.Cole JD, Blum DA, Ansel LJ. Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res. 1996;329:160–179. [DOI] [PubMed]
- 7.Collinge C, Coons D, Tornetta P, Aschenbrenner J. Standard multiplanar fluoroscopy versus a fluoroscopically based navigation system for the percutaneous insertion of iliosacral screws: a cadaver model. J Orthop Trauma. 2005;19:254–258. [DOI] [PubMed]
- 8.Day AC, Stott PM, Boden RA. The accuracy of computer-assisted percutaneous iliosacral screw placement. Clin Orthop Relat Res. 2007;463:179–186. [PubMed]
- 9.Ebraheim NA, Coombs R, Jackson WT, Rusin JJ. Percutaneous computed tomography-guided stabilization of posterior pelvic fractures. Clin Orthop Relat Res. 1994;307:222–228. [PubMed]
- 10.Ebraheim NA, Haman SP, Xu R, Stanescu S, Yeasting RA. The lumbosacral nerves in relation to dorsal S1 screw placement and their locations on plain radiographs. Orthopedics. 2000;23:245–247. [DOI] [PubMed]
- 11.Gautier E, Bachler R, Heini PF, Nolte LP. Accuracy of computer-guided screw fixation of the sacroiliac joint. Clin Orthop Relat Res. 2001;393:310–317. [DOI] [PubMed]
- 12.Goldberg BA, Lindsey RW, Foglar C, Hedrick TD, Miclau T, Hadad JL. Imaging assessment of sacroiliac screw placement relative to the neuroforamen. Spine. 1998;23:585–589. [DOI] [PubMed]
- 13.Hinsche AF, Giannoudis PV, Smith RM. Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res. 2002;395:135–144. [DOI] [PubMed]
- 14.Hufner T, Geerling J, Gansslen A, Kendoff D, Citak C, Grutzner P, Krettek C. [Computer-assisted surgery for pelvic injuries] [in German]. Chirurg. 2004;75:961–966. [DOI] [PubMed]
- 15.Keating JF, Werier J, Blachut P, Broekhuyse H, Meek RN, O’Brien PJ. Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma. 1999;13:107–113. [DOI] [PubMed]
- 16.Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989;242:83–97. [PubMed]
- 17.Nelson DW, Duwelius PJ. CT-guided fixation of sacral fractures and sacroiliac joint disruptions. Radiology. 1991;180:527–532. [DOI] [PubMed]
- 18.Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine. 2000;25:2637–2645. [DOI] [PubMed]
- 19.Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995;9:207–214. [DOI] [PubMed]
- 20.Routt ML Jr, Simonian PT. Closed reduction and percutaneous skeletal fixation of sacral fractures. Clin Orthop Relat Res. 1996;329:121–128. [DOI] [PubMed]
- 21.Schep NW, Haverlag R, van Vugt AB. Computer-assisted versus conventional surgery for insertion of 96 cannulated iliosacral screws in patients with postpartum pelvic pain. J Trauma. 2004;57:1299–1302. [DOI] [PubMed]
- 22.Shuler TE, Boone DC, Gruen GS, Peitzman AB. Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions. J Trauma. 1995;38:453–458. [DOI] [PubMed]
- 23.Smith HE, Yuan PS, Sasso R, Papadopolous S, Vaccaro AR. An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine. 2006;31:234–238. [DOI] [PubMed]
- 24.Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma. 1997;43:146–149. [DOI] [PubMed]
- 25.Stöckle U, König B, Hofstetter R, Nolte LP, Haas NP. [Navigation assisted by image conversion: an experimental study on pelvic screw fixation] [in German]. Unfallchirurg. 2001;104:215–220. [DOI] [PubMed]
- 26.Stöckle U, König B, Schäffler A, Zschernack T, Haas NP. [Clinical experience with the Siremobil Iso-C(3D) imaging system in pelvic surgery] [in German]. Unfallchirurg. 2006;109:30–40. [DOI] [PubMed]
- 27.Stöckle U, Krettek C, Pohlemann T, Messmer P. Clinical applications: pelvis. Injury. 2004;35(suppl 1):46–56. [DOI] [PubMed]
- 28.Templeman D, Schmidt A, Freese J, Weisman I. Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res. 1996;329:194–198. [DOI] [PubMed]
- 29.Tile M, Pennal GF. Pelvic disruption: principles of management. Clin Orthop Relat Res. 1980;151:56–64. [PubMed]
- 30.Tonetti J, Carrat L, Blendea S, Merloz P, Troccaz J, Lavallee S, Chirossel JP. Clinical results of percutaneous pelvic surgery: computer assisted surgery using ultrasound compared to standard fluoroscopy. Comput Aided Surg. 2001;6:204–211. [DOI] [PubMed]
- 31.Tonetti J, Carrat L, Lavallee S, Pittet L, Merloz P, Chirossel JP. Percutaneous iliosacral screw placement using image guided techniques. Clin Orthop Relat Res. 1998;354:103–110. [DOI] [PubMed]
- 32.van den Bosch EW, van Zwienen CM, van Vugt AB. Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma. 2002;53:44–48. [DOI] [PubMed]