Abstract
Computed tomography (CT) frequently is used to determine torsional abnormalities. However, its use in clinical practice may be limited. We present a new method for measuring tibial torsion using conventional radiographs. We compared the method with several clinical methods and with CT measurement in 44 lower extremities of 25 subjects. The radiographic method agreed well with all of the clinical methods, and this agreement was better than agreement between CT and clinical examination. The best agreement was between thigh-foot angle and the radiographic method. The proposed radiographic measurement is a practical method for evaluation of tibial torsion in outpatient clinics without the need for specialized equipment.
Level of Evidence: Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Tibial torsion is a term used to describe the physiologic twist of the distal relative to the proximal articular axis of the tibial bone in the transverse plane around its longitudinal axis [2, 4]. The first description of tibial torsion was made at the beginning of the 20th century [8, 12]. Subsequently, numerous authors have described various anthropometric, clinical, and radiographic methods to determine tibial torsion, including direct measurement of cadaver bones [7, 22], clinical assessment of patients’ limbs [5, 11, 18], and several imaging techniques using plain films [7, 15], fluoroscopy [2], CT [3, 8, 9, 13, 19], MRI [16], and ultrasound [6].
The most accurate technique for measuring tibial torsion is anthropometric measurement on necropsy specimens. Although this approach is useful for establishing normative data, it cannot be used clinically [8]. Normative values also have been reported using an anthropometer, which is a device using a fixed marker on the tibial tuberosity and a goniometer to measure the position of the malleoli [11, 14]. However, difficulty in centering the instrument on the mobile patella or the tibial tubercle decreases the accuracy of these methods [8]. In clinical practice, well-established indirect clinical methods include measurements of thigh-foot angle (TFA) and the thigh-transmalleolar angle (TMA) [10, 17]. However, these two measures rely on individual judgment rather than truly objective criteria and they depend in part on the particular posture assumed by the patient at the time [12].
No conventional radiographic technique for routine assessment of tibial torsion has yet gained acceptance. With the development of whole-body CT, it has been possible to accurately measure torsional deformities [8, 9]. However, its use in practice is limited because of expense, radiation, and availability. MRI and ultrasound also are impractical for most orthopaedic outpatient clinics. However, routine AP and lateral ankle and/or leg radiographs frequently are required for patients assessed in orthopaedic outpatient clinics because of lower-limb complaints.
We therefore describe a method using plain radiographs and the TMA for determining tibial torsion and compare the method with various clinical methods and CT.
Materials and Methods
We made all measurements on 25 healthy volunteers (44 lower extremities) between September 2007 and January 2008. Volunteers were selected from hospital personnel and patients seen in orthopaedic outpatient clinics. We excluded subjects with a history of tumor, the presence of lower-leg congenital or acquired deformities, and leg-length discrepancies. There were five women and 20 men. The measurements were made unilaterally in six (two right, four left) and bilaterally in 19 subjects. The average age of the subjects was 35.8 years (range, 24–50 years). All subjects signed an informed consent form that had been approved by the institution’s human subjects review board.
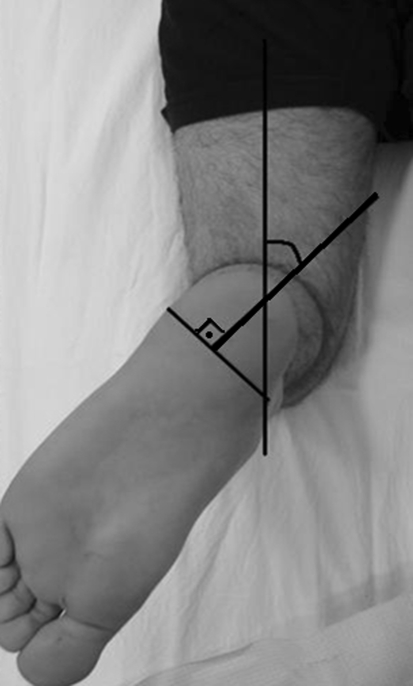
The subjects were assessed clinically and radiographically. Clinical evaluation included determination of the TFA and TMA using the prone goniometric method (TFA and TMA) [10, 17] and the footprint method (TMA) [5]. For the prone goniometric method, the patient was positioned prone, the knee on the side to be measured flexed 90°, and the ankle positioned in neutral dorsiflexion/plantar flexion. Care was taken to assure relaxation of the patient’s leg to eliminate tibiofibular rotation by the hamstring musculature during the measurements. We used a 1°-increment, manual goniometer with 30-cm arm length to take the measurements. We defined the TFA as the angular difference between the axis of the foot and the axis of the thigh. To measure TMA, we first marked the center point of each malleolus with a marking pen and these points were joined by a line across the plantar aspect of the heel, which approximated the transmalleolar axis (Fig. 1). The TMA was defined as the angular difference between the lines projected toward the heel at right angles to the transmalleolar axis and the axis of the thigh.
Fig. 1.
The photograph shows measurement of the TMA by the prone goniometric method.
The TMA also was measured with the footprint method [5]. The patient sat on an examining couch with the knee positioned at 90° flexion, the hip in neutral rotation, the tibial tubercle and patella facing forward, and the foot supported on a stool. The knee axis corresponded to the tibial transcondylar line, which was parallel to the edge of the examining couch. A piece of ruled paper was placed under the foot. The lines on the paper were parallel to the edge of the examining couch and perpendicular to the long axis of the thigh. The position of the malleoli projected downward onto the ruled paper using a small set square while the lines of the paper were aligned with the knee axis. A line was drawn between the two projected points of the malleoli and the angle was measured between this line and any line on the paper as TMA.
For the CT measurements [8], we used a LightSpeed Pro 16 model multislice scanner (General Electric Medical System, Milwaukee, WI). The patient was positioned supine and adhesive tape was used to stabilize the feet and thighs. The proximal reference line was determined by taking the axis through the widest transverse condylar diameter. The distal reference line was the transverse axis through the lower end of the tibia, which bisects the AP diameter and also passes through the anterior half of the lateral malleolus. The angle between these two axes was measured as TMA.
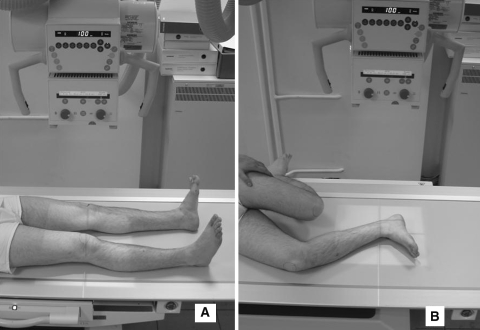
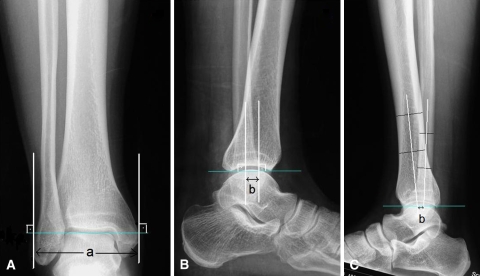
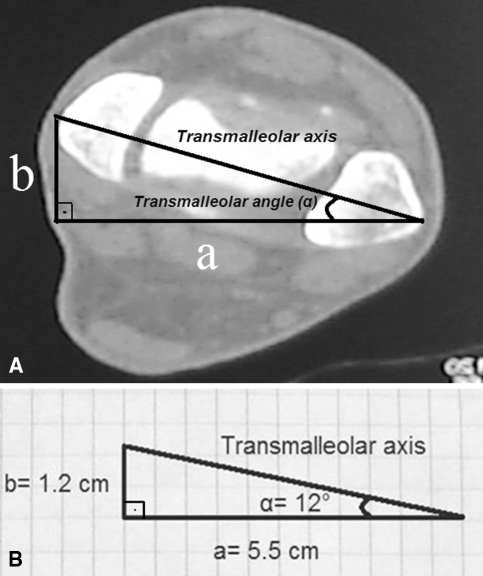
The radiographic evaluation was made with a digital radiograph (Axiom Aristos; Siemens AG, Erlangen, Germany). The patient was positioned supine. We took AP and lateral radiographs of the leg from a distance of approximately 100 cm. For AP radiographs of the leg, care was taken to centralize the patella. For lateral radiographs of the leg, the patient was placed in a lateral decubitus position with the measured side down and the knee was flexed 90° while the ankle was in neutral position. Care was taken that the lateral border of the thigh and the leg was in contact with the table (Fig. 2). The tibiotalar joint line was determined on the AP radiograph (Fig. 3A). We drew lines tangential to the medial and lateral malleoli and perpendicular to the tibiotalar joint line. The length between these two lines (a) was measured (Fig. 3A). On the lateral radiographs, the tibiotalar joint line was drawn between the anterior and posterior edges of the distal tibial articular surface. The lower ends of the medial and lateral malleoli were identified and the lines from these points, which were perpendicular to the tibiotalar joint line, were drawn. The length between these two lines (b) was measured (Fig. 3B). It was not always possible to identify the exact position of the medial and lateral malleoli on the lateral radiograph. In that situation, the middle points of the tibia and fibula in two different levels were determined on the lateral radiograph and the lines between these points were drawn. These two lines approximated the position of the malleoli at the ankle. The length between these two lines at the tibiotalar joint level was measured in the sagittal plane (Fig. 3C). These measurements in frontal and sagittal planes were transferred to the transverse plane assuming a and b were the orthogonal borders of a triangle. We defined the hypotenuse of this triangle as the transmalleolar axis (Fig. 4A). The TMA (α) can be computed with a trigonometric calculation using a simple handheld calculator. In the current study, it was measured on graph paper with a goniometer (Fig. 4B).
Fig. 2A–B.
The photographs show the position of the patient during (A) AP and (B) lateral radiographic examinations.
Fig. 3A–C.
The radiographs show the measurements on the (A) frontal and (B) sagittal planes. (C) The lateral radiograph shows the measurement on the sagittal plane for a patient in whom it was not possible to determine the exact position of the malleoli.
Fig. 4A–B.
(A) The transverse CT scan shows the geometric relationship between the measurements on the frontal (a) and sagittal (b) planes. (B) The TMA (α) can be measured on checkered paper with a goniometer.
All but the radiographic measurement were made by the same investigator. To examine reliability of the radiographic method, measurements were made twice with 2-week intervals independently by the first and last authors. Intraobserver and interobserver measurement variations were defined as the difference between the two measurements of one observer and the difference between two measurements of two observers, respectively. The mean differences of the intraobserver and interobserver measurements were 1.2° ± 0.9° (range, 0°–4°) and 2.2° ± 1.4° (range, 0°–6°), respectively. The radiographic measurement method had intraobserver and interobserver intraclass correlation coefficients of 0.869 (95% confidence interval, 0.770–0.926) and 0.768 (95% confidence interval, 0.691–0.868), respectively.
We computed descriptive statistics (mean and standard deviation). Dunnett’s test was used to compare the measurement methods. Differences between the clinical and radiographic measurement methods were determined by Mann-Whitney U test. Intraclass correlation coefficients and 95% confidence intervals were used to determine the agreement between measurement methods and intraobserver and interobserver reliability of the radiographic measurement method. The statistical analysis was performed using the NCSS 2007 program (NCSS Statistical Software, Kaysville, UT).
Results
The mean TMA measured radiographically was 10.05° ± 3.06° (range, 2°–17°) (Table 1). The radiographic measurement agreed well (p = 0.498) with the TFA, whereas the CT measurement agreed well (p = 0.358) with the TMA measured clinically (Table 2). The angles measured with CT were greater (p = 0.001) than the angles measured radiographically.
Table 1.
TMA measured by each method
| Method | TMA |
|---|---|
| TFA | 11.25° ± 3.17° (2°–22°) |
| Prone TMA | 15.80° ± 5.20° (2°–30°) |
| Footprint method | 13.05° ± 5.14° (5°–23°) |
| Radiographic measurement | 10.05° ± 3.06° (2°–17°) |
| CT measurement | 21.93° ± 8.36° (5°–40°) |
Values are expressed as mean ± standard deviation, with range in parentheses; TMA = thigh-transmalleolar angle; TFA = thigh-foot angle; CT = computed tomography.
Table 2.
Comparison of the methods according to Dunnett’s multiple comparison test
| Compared methods | p Value |
|---|---|
| TFA–prone TMA | 0.001 |
| TFA–footprint method | 0.430 |
| TFA–radiographic measurement | 0.498 |
| TFA–CT measurement | 0.001 |
| Prone TMA–footprint method | 0.128 |
| Prone TMA–radiographic measurement | 0.001 |
| Prone TMA–CT measurement | 0.358 |
| Footprint method–radiographic measurement | 0.037 |
| Footprint method–CT measurement | 0.001 |
| Radiographic measurement–CT measurement | 0.001 |
TFA = thigh-foot angle; TMA = thigh-transmalleolar angle; CT = computed tomography.
Correlation between CT and clinical measurement methods was lower than correlation between radiographic and clinical measurement methods (Table 3). The intraclass correlation coefficient between the radiographic and CT measurement methods was 0.63 (95% confidence interval, 0.32–0.79). We found the best agreement between the TFA and the TMA was measured radiographically.
Table 3.
Agreement between clinical and CT and radiographic measurement methods
| Clinical measurement method | Intraclass correlation coefficient (95% confidence interval) | |
|---|---|---|
| CT measurement | Radiographic measurement | |
| TFA | 0.43 (0.31–0.68) | 0.81 (0.66–0.89) |
| Prone TMA | 0.73 (0.50–0.85) | 0.70 (0.50–0.83) |
| Footprint method | 0.67 (0.40–0.82) | 0.71 (0.47–0.84) |
CT = computed tomography; TFA = thigh-foot angle; TMA = thigh-transmalleolar angle.
The differences between CT and clinical measurement methods were greater (p = 0.0001) than the differences between radiographic and clinical measurement methods (Table 4).
Table 4.
Differences between clinical and CT and radiographic measurement methods
| Clinical measurement method | CT measurement* | Radiographic measurement* | Mann-Whitney U test | p Value |
|---|---|---|---|---|
| TFA | 10.68° (7.64°) | −1.48° (2.37°) | 164 | 0.0001 |
| Prone TMA | 6.14° (6.46°) | −6.02° (3.4°) | 125.5 | 0.0001 |
| Footprint method | 8.88° (6.87°) | −3.00° (4.00°) | 153 | 0.0001 |
* Values are expressed as means, with standard deviations in parentheses; CT = computed tomography; TFA = thigh-foot angle; TMA = thigh-transmalleolar angle.
Discussion
Tibial torsion is defined as the relationship between the axis of rotation of the knee (flexion/extension) and the transmalleolar axis [17]. Previously reported radiographic methods to make this assessment [7, 15] generally are complicated and have not gained general clinical acceptance. These methods involve axial projection of the tibia with the patient in a sitting position. The results are considered unreliable and not reproducible because the reference points are uncertain [2]. We therefore developed a method using plain radiographs and the TMA for determining tibial torsion and compared the method with various clinical methods and CT. Our method differs from previous measurement methods because the evaluation of TMA is performed on frontal and sagittal planes. This geometric relationship can be introduced by taking AP and lateral radiographs in appropriate positions.
There are several limitations to this study. Our study group did not consist of patients with lower-leg deformities. There may be some difficulty evaluating patients with conventional radiographs because it may be difficult to obtain standard radiographs in appropriate positions. All subjects in our study were adults; similar measurements can be made in children although we cannot ensure the data presented would be similar. The evaluation of tibial torsion with CT is based on a measurement in the transverse plane that can decrease the value of this method in children because of incomplete ossification [2]. However, epiphysis lines do not interfere with the evaluation of TMA in the presented measurement method. Using this radiographic method in heavy patients may be difficult. Excessive soft tissue around the distal femur can prevent obtaining standard radiographs. Because of these limitations, we consider our study preliminary. Additional studies are needed to validate the use of this new method for patients who are skeletally immature, obese, or have coexisting sagittal or coronal plane deformities and to establish normative data with the method.
Tibial torsional abnormalities are considered possible causes of lower extremity disorders in adults, such as osteoarthritis [21], patellofemoral instability [20], and Osgood-Schlatter disease [20]. They also are responsible for gait abnormalities in childhood, such as toeing in or toeing out [18]. In most of these cases, routine AP and lateral radiographs are required. The proposed radiographic measurement method may help make an initial evaluation of tibial torsion and decrease consequent need for CT.
TFA and TMA are used in clinical practice to provide an estimation of underlying tibial torsion. TFA is a composite measurement that reflects rotation of the tibia and hind part of the foot [17]. However, it is easier to measure than TMA and is accepted as the most practical measurement method of tibial torsion. The average values of TFA and TMA are reportedly 10° (range, –5° to +30°) and 20° (range, 0° to +45°), respectively, with the mean value and the normal ranges of TMA being greater than those of TFA [17]. Another clinical measurement method for TMA is the footprint method [5]. The reported average value of TMA according to the footprint method was 12.6°. An error up to 5° is typical for goniometric measurements in normal subjects and a change of greater magnitude may be considered real [19]. Our clinical measurement results were similar to reported results but with no differences between each other, except TFA and TMA. However, a mean difference of 4° to 5° may not be clinically important, particularly because it is within measurement error.
There is general agreement that all clinical and radiographic methods for measuring tibial torsion allow only an approximation that ranges up to 15° from the true value [8]. For this reason, a technique using CT was developed with the goal of achieving the same accuracy as the direct measurements in necropsy specimens. In one study [1] comparing clinical methods with CT, the authors concluded goniometric measurements did not differ from the CT method of the determination of intraindividual torsional differences. Another study suggested goniometric measurements were within 5° to 10° of the CT measurements [19]. Our radiographic and clinical measurements, including TFA and the footprint method, were different from the CT measurements, with an average difference between radiographic and CT measurements of 12°. Therefore, the accuracy of our new radiographic method is not equal to that obtained with CT. However, our radiographic method agreed well with all of the clinical methods, and this agreement was better than agreement between CT and clinical examination.
The use of CT involves complicated and expensive equipment, which is not regularly available [2]. Otherwise, its use in practice may be limited because of the need for sedation or general anesthesia in the young child. It also may be of limited value in children because of incomplete ossification and disturbance of the image caused by implants and external fixation devices, especially at the level of the ankle [2, 17]. Precise, safe, and practical measurement of the tibial torsion is needed for clinical decision-making. The proposed radiographic measurement, which has results similar to those observed in previous clinical measurement studies, is a practical and reproducible method for evaluation of tibial torsion and can be used in orthopaedic outpatient clinics without the need for specialized equipment.
Acknowledgments
We thank the patients who participated in this study and Rana Konyalıoğlu (statistician) for contributing to the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bouchard R, Meeder PJ, Krug F, Libicher M. Evaluation of tibial torsion: comparison of clinical methods and computed tomography. Rofo. 2004;176:1278–1284. [DOI] [PubMed]
- 2.Clementz BG. Assessment of tibial torsion and rotational deformity with a new fluoroscopic technique. Clin Orthop Relat Res. 1989;245:199–209. [PubMed]
- 3.Eckhoff DG, Johnson KK. Three-dimensional computed tomography reconstruction of tibial torsion. Clin Orthop Relat Res. 1994;302:42–46. [PubMed]
- 4.Fabry G, Cheng LX, Molenaers G. Normal and abnormal torsional development in children. Clin Orthop Relat Res. 1994;302:22–26. [PubMed]
- 5.Hazlewood ME, Simmons AN, Johnson WT, Richardson AM, van der Linden ML, Hillman SJ, Robb JE. The footprint method to assess transmalleolar axis. Gait Posture. 2007;25:597–603. [DOI] [PubMed]
- 6.Hudson D, Roger T, Richards J. Ultrasound measurements of torsions in the tibia and femur. J Bone Joint Surg Am. 2006;88:138–143. [DOI] [PubMed]
- 7.Hutter CG Jr, Scott W. Tibial torsion. J Bone Joint Surg Am. 1949;31:511–518. [PubMed]
- 8.Jakob RP, Haertel M, Stüssi E. Tibial torsion calculated by computerized tomography and compared to other methods of measurement. J Bone Joint Surg Br. 1980;62:238–242. [DOI] [PubMed]
- 9.Jend HH, Heller M, Dallek M, Schoettle H. Measurement of tibial torsion by computer tomography. Acta Radiol Diagn (Stockh). 1981;22:271–276. [DOI] [PubMed]
- 10.King HA, Staheli LT. Torsional problems in cerebral palsy. Foot Ankle. 1984;4:180–184. [DOI] [PubMed]
- 11.Malekafzali S, Wood MB. Tibial torsion: a simple clinical apparatus for its measurement and its application to a normal adult population. Clin Orthop Relat Res. 1979;145:154–157. [PubMed]
- 12.Milner CE, Soames RW. A comparison of four in vivo methods of measuring tibial torsion. J Anat. 1998;193:139–144. [DOI] [PMC free article] [PubMed]
- 13.Reikaras O, Hoiseth A. Torsion of the leg determined by computed tomography. Acta Orthop Scand. 1989;60:330–333. [DOI] [PubMed]
- 14.Ritter MA, DeRosa GP, Babcock JL. Tibial torsion? Clin Orthop Relat Res. 1976;120:159–163. [PubMed]
- 15.Rosen H, Sandick H. The measurement of tibiofibular torsion. J Bone Joint Surg Am. 1955;37:847–855. [PubMed]
- 16.Schneider B, Laubenberger J, Jemlich S, Groenek K, Weber HM, Larger M. Measurement of femoral antetorsion and tibial torsion by magnetic resonance imaging. Br J Radiol. 1997;70:575–579. [DOI] [PubMed]
- 17.Staheli LT, Corbett M, Wyss C, King H. Lower extremity rotational problems in children: normal values to guide management. J Bone Joint Surg Am. 1985;67:39–47. [PubMed]
- 18.Staheli LT, Engel GM. Tibial torsion: a method of assessment and a survey of normal children. Clin Orthop Relat Res. 1972;86:183–186. [DOI] [PubMed]
- 19.Stuberg W, Temme J, Kaplan P, Clarke A, Fuchs R. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin Orthop Relat Res. 1991;272:208–212. [PubMed]
- 20.Turner MS, Smillie IS. The effect of tibial torsion on the pathology of the knee. J Bone Joint Surg Br. 1981;63:396–398. [DOI] [PubMed]
- 21.Yagi T, Sasaki T. Tibial torsion in subjects with medial type osteoarthritic knee. Clin Orthop Relat Res. 1986;213:177–182. [PubMed]
- 22.Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989;7:132–137. [DOI] [PubMed]