Abstract
Recurrent or persistent infection after two-stage exchange arthroplasty for previously infected total knee replacement is a challenging clinical situation. We asked whether a second two-stage procedure could eradicate the infection and preserve knee function. We evaluated 18 selected patients with failed two-stage total knee arthroplasty implantation treated with a second two-stage reimplantation between 1999 and 2005. Failure of treatment was defined as recurrence or persistence of infection. The minimum followup was 24 months (mean, 40 months; range, 24–83 months). Recurrent or persistent infection was diagnosed in four of 18 patients, two of whom were successfully treated with a third two-stage exchange arthroplasty. Knee Society score questionnaires administered at the last followup showed an average Knee Society knee score of 73 points (range, 24–100 points) and an average functional score of 49 points (range, 20–90 points). The data suggest repeat two-stage exchange arthroplasty is a reasonable option for eradicating periprosthetic infection, relieving pain, and achieving a satisfactory level of function for some patients.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Recurrent or persistent infection after two-stage exchange arthroplasty for the treatment of an infected total knee arthroplasty (TKA) is a dreaded problem with an incidence of 9% to 33% [8, 9, 11, 13–16, 19, 20]. Its complexity arises from the fact that it represents failure of the most commonly implemented and agreed upon strategy to treat TKA with established deep infection. Additionally, it poses a treatment dilemma to which clear-cut guidelines have not been instituted to date.
Careful assessment of the individual patient situation, taking into account the surgical history, virulence of the infecting organism, underlying medical conditions, bone stock and soft tissue integrity, and patient desires allow the surgeon to recommend the best option for treatment. Knee arthrodesis or above-the-knee amputation are two potential options for patients who are not deemed appropriate candidates for reconstruction using joint prostheses [10]. In a select group of patients, however, the surgeon may be inclined to attempt a second two-stage exchange arthroplasty in an effort to offer more optimal knee function to the patient. One report on the outcome of second two-stage exchange arthroplasty in nine patients eradicated the infection in all nine with functional scores (Hospital for Special Surgery) ranging from 53–97 [1].
To confirm those results the purpose of our study was (1) to evaluate the ability of a second two-stage exchange knee arthroplasty to eradicate infection; and (2) to measure the functional outcome after a second two-stage reimplantation for TKA reinfection.
Materials and Methods
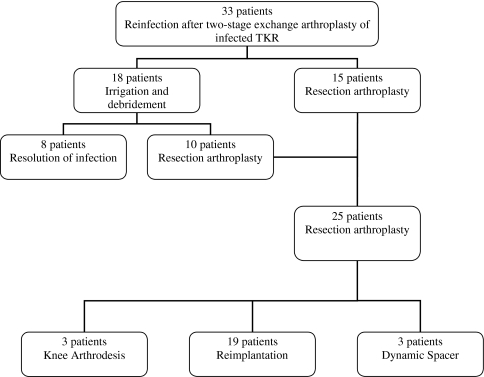
We retrospectively reviewed 33 patients with reinfection after two-stage reimplantation of TKA between 1999 and 2005 (Fig. 1). Reinfection was diagnosed at an average of 30 months following previous reimplantation. Twenty-six of the 33 patients had been treated with a two-stage exchange arthroplasty at our institution while the remaining seven patients had their initial two-stage treatment at an outside institution and were referred for further care. Irrigation and débridement with retention of prosthesis as the initial treatment was elected in 18 of the 33 patients. In the remaining 15 patients, infection was deemed severe and resection arthroplasty with intended delayed reimplantation was performed. Irrigation and débridement failed in 10 of the 18 patients undergoing irrigation and débridement, resulting in resection arthroplasty. This led to a total of 25 patients who had undergone resection arthroplasty with an intended delayed reimplantation. Severity of infection, extremely poor bone quality, condition of the soft tissue as well as the underlying medical condition resulted in a decision to perform knee arthrodesis as the second stage in three of 25 patients, and three others were deemed not to be candidates for further surgery. That left 19 patients (10 women and nine men) we considered candidates for a second reimplantation surgery. The average age was 67 years (range, 49–86 years) at the time of reimplantation. The mean body mass index was 29.7 kg/m2 (range, 21–46.6 kg/m2). The majority of patients in this cohort had preexisting comorbidities, including heart disease (six patients), diabetes (five patients), rheumatoid arthritis (three patients), chronic renal failure (two patients), and malignant disease (one patient). American Society of Anesthesiology (ASA) score was 3 (severe systemic disease) in 14 patients and 2 (mild systemic disease) in the other five. Patients were followed for a minimum of 2 years, until recurrence of infection, or until death. The minimum followup was 24 months (mean, 40 months; range, 24–83 months). There was one unrelated death after the 2-year followup. One of the 19 patients was lost to followup after the second reimplantation, leaving 18 for final evaluation.
Fig. 1.
A flowchart outlines the surgical treatment of 33 patients with reinfection after two-stage exchange knee arthroplasty at our institution between 1999 and 2005.
The symptoms and signs of reinfection varied in the cohort but mainly consisted of chronic pain, radiographic evidence of loosening, and clinical signs of infection which included swelling, joint tenderness, and erythema. Seven of the 19 patients considered for second reimplantation presented with symptoms and signs of acute infection, whereas 12 patients presented with chronic pain, five of whom had radiographic evidence of prosthetic loosening. Reinfection was confirmed with positive cultures in 17 of the 19 patients while the other two had at least one of the three criteria for infection: (1) abnormal serology (ESR > 30 mm/hr; CRP > 1 mg/dL); (2) joint aspiration leukocyte count over 1100 cells/μL and neutrophil percentage greater than 64%; (3) evidence of purulence during the subsequent surgical intervention [18]. The isolated organism was different from the previous infecting organism in only one of 17 patients while the same infecting organism as the initial infection was identified in 13 patients; the previous infecting organism could not be identified with routine cultures in the remaining three patients (Table 1).
Table 1.
Management of patients with persistent or recurrent infection following two stage exchange knee arthroplasty
| Patient No. | Age | Gender | Surgical treatment | Organism | Antibiotics following the second stage | Outcome | Treatment of reinfection | |
|---|---|---|---|---|---|---|---|---|
| First revision | Second revision | |||||||
| 1 | 69 | F | Second two-stage exchange arthroplasty | MSSE | MSSE | Vancomycin for 6 weeks followed by oral rifampin | Persistence or recurrence of infection | Third two-stage exchange arthroplasty |
| 2 | 49 | M | Second two-stage exchange arthroplasty | MRSE | MRSE | Vancomycin for 8 weeks | Persistence or recurrence of infection | Third two-stage exchange arthroplasty |
| 3 | 83 | F | Second two-stage exchange arthroplasty | No growth | MSSA | Vancomycin for 12 weeks | Persistence or recurrence of infection | Resection arthroplasty, patient deceased |
| 4 | 68 | F | I&D followed by a second two-stage exchange | Enterococcus faecalis Group D | Enterococcus faecalis Group D | Vancomycin for 12 weeks followed by oral cephalexin for 3 months | Infection control | |
| 5 | 75 | F | Second two-stage exchange arthroplasty | MRSA | MRSA | Vancomycin for 6 weeks | Infection control | |
| 6 | 61 | M | I&D followed by a second two-stage exchange | Oxacillin-resistant CoNS | Oxacillin-resistant CoNS | Vancomycin for 6 weeks followed by oral doxycycline for 2 years | Infection control | |
| 7 | 81 | M | Second two-stage exchange arthroplasty | Oxacillin-resistant CoNS | Oxacillin-resistant CoNS | Vancomycin for 12 weeks followed by oral cephalexin for 2 years | Infection control | |
| 8 | 80 | F | Second two-stage exchange arthroplasty | MRSA | MRSA | Vancomycin for 12 weeks followed by oral cephalexin for 3 years | Infection control | |
| 9 | 86 | F | I&D followed by a second two-stage exchange | MRSA | MRSA | Vancomycin for 2 weeks followed by oral doxycycline for 6 months | Infection control | |
| 10 | 51 | M | I&D followed by a second two-stage exchange | MRSE | MRSE | IV vancomycin for 6 weeks followed by oral cephalexin for 3 months | Infection control | |
| 11 | 59 | M | Second two-stage exchange arthroplasty | No growth | MSSA | IV cefazolin for 6 weeks followed by oral cephalexin for 3 months | Infection control | |
| 12 | 63 | F | Second two-stage exchange arthroplasty | Enterococcus faecalis Group D | Enterococcus faecalis Group D | Vancomycin for 6 weeks followed by oral cephalexin for 5 years | Infection control | |
| 13 | 63 | M | I&D followed by a second two-stage exchange | MRSE | No growth | IV cefazolin for 6 weeks followed by oral amoxicillin for 3 years | Infection control | |
| 14 | 71 | F | I&D followed by a second two-stage exchange | MSSE | MSSE | Rifampin for 3 months | Infection control | |
| 15 | 65 | M | Second two-stage exchange arthroplasty | MRSE | MRSE | Vancomycin for 6 weeks followed by oral cephalexin for 3 months | Infection control | |
| 16 | 60 | F | Second two-stage exchange arthroplasty | MRSA | No growth | Vancomycin for 12 weeks followed by oral doxycycline for 3 years | Infection control | |
| 17 | 52 | F | Second two-stage exchange arthroplasty | MRSA | MSSE | Tigecycline for 6 weeks followed by oral minocycline for 1 year | Infection control | |
| 18 | 67 | M | I&D followed by a second two-stage exchange | No growth | MRSA | IV vancomycin for 6 weeks followed by oral levaquin for 5 years | Infection control | |
| 19 | 79 | M | Second two-stage exchange arthroplasty | Oxacillin-resistant CoNS | Oxacillin-resistant CoNS | IV clindamycin followed by oral suppression with doxycycline | Persistence or recurrence of infection | Suppressive antibiotics |
| 20 | 74 | M | I&D followed by resection arthroplasty with insertion of a dynamic spacer | Oxacillin-susceptible CoNS | Group B streptococcus | Vancomycin for 12 weeks | Infection control | |
| 21 | 72 | F | Resection arthroplasty followed by knee arthrodesis | unknown | MRSA | Ciprofloxacin | Infection control | |
| 22 | 56 | M | Resection arthroplasty followed by knee arthrodesis | Serratia marcescens | Clostridium subterminale | Vancomycin for 6 weeks followed by ciprofloxacin | Infection control | |
| 23 | 42 | M | Resection arthroplasty with insertion of a dynamic spacer | Gram-negative organism | No growth | Vancomycin for 6 weeks followed by ciprofloxacin | Infection control | |
| 24 | 57 | F | I&D followed by resection arthroplasty with insertion of a dynamic spacer | MRSA | No growth | Vancomycin for 6 weeks followed by oral rifampin | Infection control | |
| 25 | 73 | M | I&D followed by knee arthrodesis | Pseudomonas + MRSA | No growth | Vancomycin for 6 weeks followed by ciprofloxacin | Infection control | |
| 26 | 71 | F | I&D | Klebsiella pneumoniae | MRSA | Vancomycin for 6 weeks followed by oral ciprofloxacin | Infection control | |
| 27 | 72 | F | I&D | Proteus mirabilis | Proteus mirabilis | Vancomycin for 6 weeks followed by oral ciprofloxacin | Infection control | |
| 28 | 71 | M | I&D | Oxacillin-resistant CoNS | Oxacillin-resistant CoNS | Vancomycin for 6 weeks followed by oral ciprofloxacin | Infection control | |
| 29 | 62 | F | I&D | MRSA | Oxacillin-resistant CoNS | Vancomycin for 6 weeks followed by oral doxycycline | Infection control | |
| 30 | 66 | M | I&D | Oxacillin-resistant CoNS | Oxacillin-resistant CoNS | Vancomycin for 6 weeks followed by oral doxycycline | Infection control | |
| 31 | 89 | F | I&D | Oxacillin-resistant CoNS | Oxacillin-resistant CoNS | Vancomycin for 6 weeks followed by oral cephalexin | Infection control | |
| 32 | 66 | F | I&D | Streptococcus mitis | MRSA | Vancomycin for 6 weeks followed by oral cephalexin | Infection control | |
| 33 | 83 | F | I&D | MSSA | Oxacillin-susceptible CoNS | Vancomycin for 6 weeks followed by oral doxycycline | Infection control | |
I&D = Irrigation and débridement; MRSA = methicillin-resistant Staphylococcus aureus; MRSE = methicillin-resistant Staphylococcus epidermidis; MSSA = methicillin-sensitive Staphylococcus aureus; MSSE = methicillin-sensitive Staphylococcus epidermidis; CoNS = Coagulase-negative staphylococcus.
In all 19 patients, antibiotics were discontinued at least 2 weeks prior to resection arthroplasty to allow for isolation of organisms in intraoperative cultures. Prior incisions and medial parapatellar arthrotomy were utilized to expose the knee joint. Quadriceps snip was utilized in two patients to facilitate exposure. Gross purulence was encountered in 16 patients. In each of the 19 patients, a total of five tissue specimens was collected intraoperatively and sent for Gram stain and culture. During resection arthroplasty all fragments of cement and the entire hardware, including the patellar button, were removed and extensive débridement of all necrotic soft tissues was carried out. At the conclusion of the procedure, a static spacer made of Palacos bone cement (Zimmer, Inc., Warsaw, Ind.) impregnated with 3.6 g of tobramycin and 3 g of vancomycin per pack was fashioned and interposed between the bony surfaces in 15 patients. A dynamic spacer, consisting of similar concentration of antibiotics, was used in four patients. All patients were treated with intravenous antibiotics, targeted against the isolated organism, for a period of 6 weeks.
Reimplantation was performed when clinical and serological confirmation of resolution of infection was available. Marked improvement in knee pain, absence of systemic symptoms and signs of inflammation, adequate wound healing, and a drop in inflammatory markers (ESR and CRP) were considered criteria for resolution of infection. At the time of reimplantation, the mean erythrocyte sedimentation rate was 28 mm/hr (range, 8–72 mm/hr) and the mean C-reactive protein was 0.7 mg/dL (range, 0.3–1.8 mg/dL). Reimplantation was performed at an average of 24 weeks (range, 9 weeks–26 months) after resection arthroplasty. Unwillingness of the surgeon and the patient to proceed earlier with a second reimplantation in some cases, longer time for inflammatory markers to substantially drop in others, and inability to obtain medical clearance for anesthesia for some patients delayed the time to reimplantation. Preoperative prophylactic antibiotics were administered and intraoperative cultures were obtained in all 19 patients during reimplantation. Prior to reimplantation, further débridement was performed and prosthesis reimplanted only if there was no suspicion for infection. Reimplantation was deferred in one patient due to persistently elevated inflammatory markers. This patient underwent further débridement and spacer exchange. Intraoperative cultures revealed no growth and reimplantation was performed 8 weeks later.
Intraoperative cultures were positive in two patients, both of whom were treated with extended intravenous antibiotics. The remaining patients received routine postoperative antibiotics. Nine patients were placed on suppressive oral antibiotics (Table 1) as they were deemed at high risk for recurrence of infection due to medical comorbidities, delayed wound healing or a coexisting septic focus.
The choice of implant was based on degree of bone loss, ligamentous integrity, and surgeon’s preference. Hinged prosthesis was used in 11 of 19 patients, one of which was a distal femoral replacement. All patients had Type III bone loss on the femoral side and either Type II (six patients) or Type III (five patients) bone loss on the tibial side, based on the Anderson Orthopaedic Research Institute (AORI) bone defect classification [6]. Eight patients had sufficient bone stock to support a semiconstrained prosthesis after restoration of the joint line with the use of augments (Fig. 2). Stems were used in all 19 patients.
Fig. 2.
This anteroposterior radiograph of a knee 6 years after second revision for sepsis shows a properly seated semiconstrained prosthesis.
Patients were followed at 6 weeks, 6, 12, 24 months after reimplantation, and every 2 years thereafter. Detailed clinical and radiographic data were collected prospectively for all patients. Knee Society scores [7] were obtained during followup visits. Successful outcome was defined as eradication of infection with presence of a functional prosthesis. The exact duration and doses of antibiotics received after hospital discharge were not consistently documented in medical records. Therefore, patients were contacted and asked about type of suppressive antibiotics.
We obtained anteroposterior and lateral radiographs of the treated joint at the time of the latest followup visit. Two of the authors (MA and JP) assessed the position and status of the components, any signs of loosening as well as the prevalence and size of radiolucent lines, if any. Preoperative radiographs were reviewed to assess bone stock.
Results
Infection was eradicated in 14 of 18 patients. Nine of the 14 patients were kept on suppressive oral antibiotics for 6 to 60 months (Table 1). The knee showed no signs of infection in one patient who died 3 years following second reimplantation. Recurrence of infection occurred in four patients. One patient developed recurrent knee pain 1 year after reimplantation. Cultures grew methicillin-sensitive coagulase-negative staphylococci, and copious amounts of purulent fluid as well as loose components were noted intraoperatively. Another patient presented with reinfection by vancomycin-resistant enterococci 8 weeks following reimplantation surgery. A third patient was diagnosed with recurrent staphylococcus aureus infection 3 years following reimplantation. Unfortunately, the latter patient, who had preexisting cardiac failure, suffered a complicated postoperative course and died 9 days following resection arthroplasty surgery secondary to complete lung atelectasis and cardiorespiratory failure. The fourth patient developed increasing swelling of the knee 2 weeks after reimplantation and aspiration revealed few colonies of enterococcus and was managed successfully with suppressive antibiotics. This means 15 of 18 patients successfully retained their prosthesis after the second reimplantation.
At last followup the average Knee Society knee score of the 14 patients whose infection was eradicated was 73 points (range, 24–100 points) with an average functional score of 49 points (range, 20–90 points). The KSS was between 80 and 100 in seven patients, between 70 and 79 in two patients, between 60 and 69 in one patient, and below 60 in four patients. Pain was absent in two patients, mild in six patients and moderate in six patients. Two years postoperatively, one patient developed new-onset knee pain and radiographs showed evidence of loosening around the tibial component but without any signs of infection and was subsequently lost to followup. Thus, eradication of infection with a functional prosthesis was achieved in 13 out of 18 patients followed at least two years. Radiographic evaluation of patients with no signs of infection after the second reimplantation at an average followup of 40 months showed proper tibiofemoral alignment in all patients. Definite signs of loosening were detected in one patient (mentioned above). A nonprogressive radiolucent line under the tibial component was noted in Zone 1 in one patient and in zones 3 and 4 in another [7], both of them were less than 2 mm. In-hospital complications occurred in three patients. Two had urinary tract infections that cleared with proper antibiotics and one had pancreatitis treated that resolved. One patient had a femoral fracture at the tip of the femoral stem after falling 2 months following the second reimplantation. He subsequently underwent open reduction and internal fixation. Radiographs taken at 3 years followup showed healing of the fracture and a well-fixed prosthesis.
A third two-stage exchange arthroplasty was performed in two of the four patients who had failed a second two-stage exchange (Fig. 3). Both remained infection-free at last followup (25 and 31 months). Their latest Knee Society knee scores were 73 and 40 and the functional scores were 45 and 35 respectively.
Fig. 3.

The radiograph shows a knee 2 years after third two-stage revision for sepsis. Distal femoral replacement was performed owing to extensive bone loss from multiple revisions.
Discussion
Despite being the most common treatment for infected TKA, two-stage exchange arthroplasty has a relatively high failure rate ranging from 9% to 20% [8, 9, 11, 13, 15, 19, 20]. When infection with resistant organisms is also included, the failure rate rises, between 24% and 33% [11, 14, 16]. Patients with a previously failed two-stage exchange arthroplasty present a challenge. Based partly on a previous report by Backe et al. [1], we presumed a second two-stage exchange arthroplasty is a reasonable treatment option for the majority of these patients with previous failures. We therefore examined the effectiveness of a second two-stage exchange arthroplasty in eradicating periprosthetic knee infection after a previously failed two-stage implantation.
Readers should be aware of several limitations. We evaluated only a select group of patients who were healthy enough to undergo a second reimplantation procedure and the outcomes would not likely apply to less healthy patients. We have no comparative data on whether knee arthrodesis similarly eradicates infection or provides comparable functional results. The retrospective nature of the study may introduce recall bias: doses and duration of antibiotics received after hospital discharge were not always accurately reported in the medical records. However, infection control and Knee Society scores were properly documented in a prospective database. Another limitation is that, despite being the largest reported cohort to date, the sample size was too small to allow meaningful statistical analyses to determine potential risk factors associated with treatment failure. However, the cohort is relatively large given the uncommon nature of the problem and we believe provides important information.
Our study shows that second two-stage exchange arthroplasty controlled periprosthetic knee infection in 14 of 18 patients in our cohort. There is relatively little literature on treatment of reinfection following two-stage exchange arthroplasty. Hanssen et al. [10] reported 24 knees presenting with reinfection following a previous two-stage exchange arthroplasty. Three patients were treated with a second two-stage exchange arthroplasty. Infection recurred in two patients, one of whom underwent an above-the-knee amputation. The third patient had no evidence of infection at a followup of 15 months. Other treatment modalities employed in this cohort included arthrodesis in 10 patients, above-the-knee amputation in four patients, resection arthroplasty or pseudarthroses in four patients, and suppressive antibiotic treatment in five patients. Mont et al. reported six reinfections in 69 cases treated with two-stage exchange arthroplasty including one patient treated with a second two-stage revision versus four patients with arthrodesis of the knee [15]. Wasielewski et al. reported five patients with reinfection among 50 knees treated with two-stage exchange arthroplasty; one of those patients underwent second two-stage exchange arthroplasty and subsequently became reinfected [19]. The outcome of a second two-stage exchange arthroplasty was dismal in one of the two patients treated for reinfection in another study, with one patient having an above-the-knee amputation [4]. Backe et al. followed nine patients treated for reinfection after total knee reimplantation with another two-stage exchange arthroplasty over 5 to 56 months and reported the infection was eradicated in all patients [1]. However, tibial component revision was performed in one patient 18 months postoperatively because of aseptic loosening. Although our results were not as uniformly successful in eradicating infection as reported by Backe et al. [1], we found second two-stage exchange arthroplasty eradicated the infection in 14 of 18 patients. The difference in outcome between our study and what was reported previously by Backe et al. [1] may be attributed to several reasons. Half of our patients had infection with methicillin-resistant organisms that persisted despite delayed reimplantation. Infection with such organisms compromises the treatment outcome [2, 13]. The majority of our patients also had medical comorbidities. None of the patients in the study by Backe et al. [1] were immunocompromised. Reinfection after the initial two-stage exchange arthroplasty caused by the same organism accounted for three out of the nine patients in their cohort as opposed to 13 out of 17 patients in ours and no specific reference was made to antibiotic sensitivity of the isolated organisms. Another reason for the difference could be that over ½ of our patients had extensive bone loss that necessitated the use of constrained hinged prosthesis. Finally, the smaller cohort and the shorter followup for patients in the cohort reported by Backe et al. [1] may be another important factor explaining the difference in outcome.
The functional outcome observed in our cohort is similar to what has been previously reported after a single two-stage revision for septic TKA. Barrack et al. [3] reported average Knee Society clinical and functional scores of 115 and 44 respectively after a single two-stage revision of 26 knees that was lower than that of aseptic revisions at 36 months followup. At an average followup of 4 years, Windsor et al. [20] noted poor outcome in seven of 37 patients (19%) who underwent two-stage exchange arthroplasty for periprosthetic knee infection. In the study by Backe et al. [1], the average Knee Society knee score was 79, and the average functional score was 73 after the second reimplantation.
Despite the failure in four of our 18 patients, we continue to advocate a second two-stage exchange arthroplasty for our patients as available salvage options are neither optimal nor easily acceptable to the patients. The salvage procedures available to address failure of a previous two-stage exchange arthroplasty include above-the-knee amputation and knee arthrodesis. Despite their success in eradicating infection, neither of these options is deemed acceptable by the patient and, if given the choice, would be turned down in favor of preserving the joint motion. Patients undergoing above-the-knee amputation often find it difficult to walk [12, 17] and those with knee arthrodesis can still suffer daily functional disability [5]. Successful eradication of infection accompanied by preservation of knee function has been reported following a second two-stage knee reimplantation [1]. Our data suggest a second two-stage exchange arthroplasty averts amputation or arthrodesis in the majority of the patients, despite the extensive bone loss, presence of medical comorbidities, and infection with resistant organisms.
Footnotes
The authors did not receive any outside funding or grants in support of their research for or preparation of this work. One of the authors (JP) receives payment from Stryker Orthopaedics (Mahwah, NJ) and Smith & Nephew (Memphis, TN).
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Backe HA, Jr., Wolff DA, Windsor RE. Total knee replacement infection after 2-stage reimplantation: results of subsequent 2-stage reimplantation. Clin Orthop Relat Res. 1996;331:125–131. [DOI] [PubMed]
- 2.Barberan J, Aguilar L, Carroquino G, Gimenez MJ, Sanchez B, Martinez D, Prieto J. Conservative treatment of staphylococcal prosthetic joint infections in elderly patients. Am J Med. 2006;119:993–1010. [DOI] [PubMed]
- 3.Barrack RL, Engh G, Rorabeck C, Sawhney J, Woolfrey M. Patient satisfaction and outcome after septic versus aseptic revision total knee arthroplasty. J Arthroplasty. 2000;15:990–993. [DOI] [PubMed]
- 4.Bengston S, Knutson K, Lidgren L. Treatment of infected knee arthroplasty. Clin Orthop Relat Res. 1989;245:173–178. [PubMed]
- 5.Benson ER, Resine ST, Lewis CG. Functional outcome of arthrodesis for failed total knee arthroplasty. Orthopedics. 1998;21:875–879. [DOI] [PubMed]
- 6.Engh GA: Bone defect classification. In: Engh GA, Rorabeck CH, eds. Revision Total Knee Arthroplasty. Baltimore, MD: Williams & Wilkins; 1997:63–120.
- 7.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed]
- 8.Goldman RT, Scuderi GR, Insall JN. Two-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res. 1996;331:118–124. [DOI] [PubMed]
- 9.Haleem AA, Berry DJ, Hanssen AD. Mid-term to long-term followup of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res. 2004;428:35–39. [DOI] [PubMed]
- 10.Hanssen AD, Trousdale RT, Osmon DR. Patient outcome with reinfection following reimplantation for the infected total knee arthroplasty. Clin Orthop Relat Res. 1995;321:55–67. [PubMed]
- 11.Hirakawa K, Stulberg BN, Wilde AH, Bauer TW, Secic M. Results of 2-stage reimplantation for infected total knee arthroplasty. J Arthroplasty. 1998;13:22–28. [DOI] [PubMed]
- 12.Isiklar ZU, Landon GC, Tullos HS. Amputation after failed total knee arthroplasty. Clin Orthop Relat Res. 1994;299:173–178. [PubMed]
- 13.Kilgus DJ, Howe DJ, Strang A. Results of periprosthetic hip and knee infections caused by resistant bacteria. Clin Orthop Relat Res. 2002;404:116–124. [DOI] [PubMed]
- 14.Mittal Y, Fehring TK, Hanssen A, Marculescu C, Odum SM, Osmon D. Two-stage reimplantation for periprosthetic knee infection involving resistant organisms. J Bone Joint Surg Am. 2007;89:1227–1231. [DOI] [PubMed]
- 15.Mont MA, Waldman BJ, Hungerford DS. Evaluation of preoperative cultures before second-stage reimplantation of a total knee prosthesis complicated by infection. A comparison-group study. J Bone Joint Surg Am. 2000;82:1552–1557. [DOI] [PubMed]
- 16.Salgado CD, Dash S, Cantey JR, Marculescu CE. Higher risk of failure of methicillin-resistant Staphylococcus aureus prosthetic joint infections. Clin Orthop Relat Res. 2007;461:48–53. [DOI] [PubMed]
- 17.Sierra RJ, Trousdale RT, Pagnano MW. Above-the-knee amputation after a total knee replacement: prevalence, etiology, and functional outcome. J Bone Joint Surg Am. 2003;85:1000–1004. [DOI] [PubMed]
- 18.Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steckelberg JM, Patel R. Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am J Med. 2004;117:556–562. [DOI] [PubMed]
- 19.Wasielewski RC, Barden RM, Rosenberg AG. Results of different surgical procedures on total knee arthroplasty infections. J Arthroplasty. 1996;11:931–938. [DOI] [PubMed]
- 20.Windsor RE, Insall JN, Urs WK, Miller DV, Brause BD. Two-stage reimplantation for the salvage of total knee arthroplasty complicated by infection. Further follow-up and refinement of indications. J Bone Joint Surg Am. 1990;72:272–278. [PubMed]