Abstract
The inset biconvex patella component is an alternative form of patella resurfacing in knee arthroplasty. We retrospectively reviewed 433 patients in whom 521 patella prostheses were implanted before April 1997 to determine survivorship, factors associated with failure of the implant, incidence of anterior knee pain, and factors that may be associated with the latter. We had clinical results for 204 surviving patients (242 knees) without failure of their implants with a minimum 10-year followup (mean, 11.4 years; range, 10–17 years). For the remaining 229 patients we used chart or radiographic review to determine if failure of their implant or other complications had occurred. At latest followup, 14 patella components had been revised for aseptic reasons or were radiographically loose. The 10-year Kaplan-Meier survivorship for the entire cohort for aseptic failure was 97.0%. Aseptic failure of the patella component was associated with the presence of osteonecrosis and the absence of a superior rim of bone radiographically. The incidence of anterior knee pain in surviving patients without failure of their implants was 7.8%. No factor examined was associated with anterior knee pain. Survivorship and clinical and radiographic results are equivalent, but not clearly superior, to those reported for other forms of patella resurfacing.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Routine resurfacing of the patella at TKA is controversial. Although some trials have concluded there is no advantage to routine patella resurfacing [2, 8, 9, 32], other studies [43, 44] and three recent meta-analyses [31, 33, 34] suggest a lower rate of anterior knee pain with routine patella resurfacing and either equivalent or lower rates of reoperation with routine resurfacing.
All-polyethylene patella components have proven more reliable than metal-backed patella components with time [15, 36]. There are various designs of all-polyethylene patellas, for example, domed versus anatomic, one or three pegs for fixation, and onlay versus inlay patellas.
Inlay patella implants have the potential advantages of more precise instrumentation for insertion, a larger area for cementation into the residual patella bone by virtue of creation of a cavity in the patella, and preservation of peripheral patella bone [22, 39]. Despite widespread use, there are relatively few reports of the results of these types of implants.
Based on our experience with the inset biconvex patella, we hypothesized the survivorship and clinical and radiographic findings of this implant would be at least equivalent to those of other types of patella components used for resurfacing. We specifically sought to determine (1) survivorship of the implant at 10 years, (2) factors associated with failure of the implant, (3) whether the patella tilt and tilt of the patella component in relation to the patella bone represented an improvement over historical controls of onlay patella components, (4) prevalence of anterior knee pain in surviving patients and what factors may be associated with anterior knee pain, and (5) whether an uncovered lateral facet of the patella articulating with the femoral component correlated with anterior knee pain.
Materials and Methods
We retrospectively identified 433 patients (521 knees) who underwent primary TKA before April 1997 with the Genesis® inset biconvex patella (Smith and Nephew, Inc, Memphis, TN) performed in association with either the Genesis® I or II knee system. This provided a potential minimum followup of 10 years for living patients. The design of the patella component remained unchanged throughout the study period. The inset patella component was the only type of patella resurfacing used with these knee systems, and the patella was resurfaced routinely at the time of knee arthroplasty. During the study period, other knee systems were used according to surgeon preference at our institution. These systems included inset patella components and other forms of patella resurfacing but were excluded to eliminate another variable. Of the 433 patients (521 knees), 182 (222 knees) had died at the time of review, and 31 (34 knees) were lost to followup. Of the surviving patients, two (three knees) had recent radiographs and were known to not have had revision surgery, but no clinical followup was available. An additional 14 patients (20 knees) had recent clinical reviews but had or were awaiting revision of femoral, tibial, or patella components or had radiographically loose femoral, tibial, or patella components. For those who had died or were lost to followup, chart records and radiographs, if available, were reviewed to ascertain if complications had occurred, and failures of patella components in those who had died are included in the results and analysis of failed patella implants. Clinical results and analysis of factors that may be associated with anterior knee pain are presented for the remaining 204 patients (242 knees). Of these, 144 patients (175 knees, 72%) had recent clinical and radiographic reviews (Group 1), and 60 (67 knees) had been sent a questionnaire or contacted by telephone, but complete Knee Society scores and radiographs could not be obtained for these patients (Group 2). All 433 patients (521 knees) are included in the survivorship analysis. As most of the complications that occur are detected radiographically, the description of complications pertains to all patients (surviving or not) with adequate radiographic followup, described below. The average age of the patients was 70.3 years (range, 29–96 years), and the average body mass index (BMI) was 30 kg/m2 (range, 15–63 kg/m2). There were 155 men and 278 women. Eighty-eight patients had bilateral procedures performed either under the same anesthetic or sequentially. The minimum followup for patients in Groups 1 and 2 was 10 years (mean, 11.4 years; range, 10–17 years). The study was approved by the ethics committee of our institution.
Thirty-three knees had Genesis® II femoral and tibial components at the primary surgery, and the remainder (488 knees) had the Genesis® I knee system. The primary diagnosis was osteoarthritis in 88%, inflammatory arthritis in 10%, posttraumatic arthritis in 2%, and osteonecrosis in less than 1%. Seventy-one percent of knees had a preoperative varus deformity, 25% had a valgus deformity, and 4% had neutral alignment. Ten knees had implantation through a lateral approach and the remainder through a medial approach. The posterior cruciate ligament was retained in 83% and sacrificed in 17%. Lateral release was performed in 22% of cases.
The patella component was implanted using the instrumentation provided. After exposure of the patella and removal of osteophytes, the appropriate diameter patella implant was chosen. The corresponding patella reamer collet was selected and placed on the reamer guide, which then was placed centrally or slightly medially on the patella articular surface. A patella depth gauge was used to set the reamer depth, and the reamer then was used to mill a cavity for the implant, maintaining an intact rim of bone. The patella component was cemented in after the femoral and tibial components using two mixes of Simplex® cement (Howmedica, Rutherford, NJ) for all three components. A patella clamp was applied to the component after it was implanted with the cement. The biconvex patella implant (Fig. 1) is available in different diameters, but all are the same thickness (13 mm).
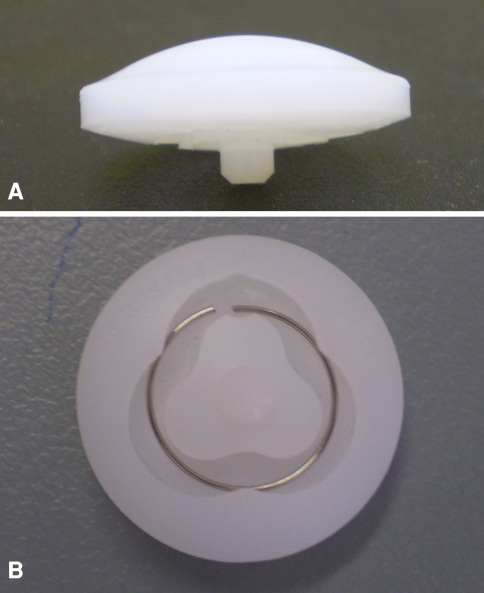
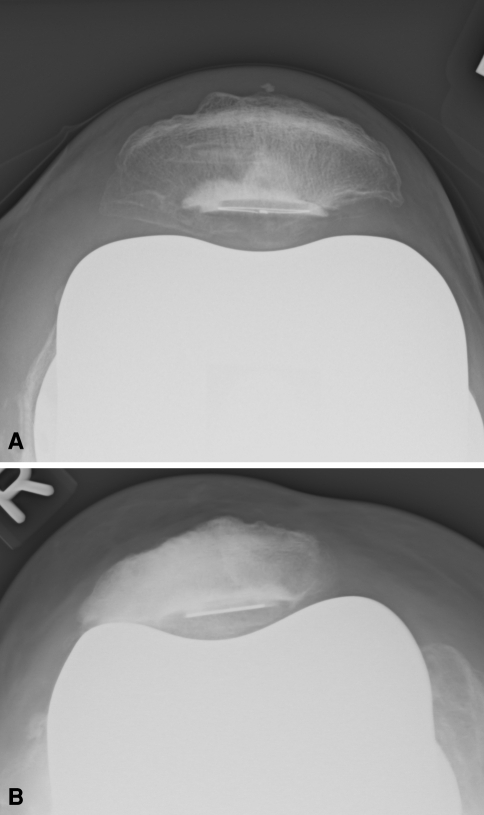
Fig. 1A–B.
(A) A side view and (B) a view of the underside of the biconvex inset patella implant are shown.
Patients were seen at 6 weeks, 3 months, 6 months, and 1 year postoperatively and then annually or biannually thereafter. Knee Society scores [17] were collected prospectively, and radiographs were taken at 6 weeks and 1 year and then at each subsequent visit. Radiographs consisted of standing anteroposterior, lateral, and skyline views (generally in 30° flexion). In addition, the presence of anterior knee pain was recorded, and, if present, the patient was asked by the doctor to record the severity on a visual analog scale from 1 to 10, with 10 representing the worst pain the patient had ever experienced. Patients who had not been seen recently and did not want to return to the clinic were sent a questionnaire asking whether they had pain in their knee, walking distance, ability to use stairs, and use of a walking aid as per the Knee Society score. They also were asked if they had any additional operations to their knee, if they were experiencing anterior knee pain, and, if so, the severity as outlined previously. Patients who did not respond to questionnaires were contacted by telephone and asked the same questions.
The patients’ most recent radiographs were reviewed. Radiographs were not available for 101 knees, and 11 knees had less than 6 months’ radiographic followup, leaving 409 for analysis. The minimum radiographic followup was 6 months (average, 7.6 years; range, 6 months to 15.5 years). All available radiographs were reviewed by one author not involved in the initial surgery (SE). Detailed radiographic analysis as outlined subsequently was done for knees in Group 1 (ie, with recent clinical and radiographic followups with a minimum of 10 years followup). For the remaining knees, the last available radiograph was examined for evidence of loosening of the patella, femoral, and tibial components; complications such as osteonecrosis or fracture; and whether the patella had an intact rim.
For the detailed radiographic analysis, one of us (SE) measured the diameter of the implant, articular surface, and thickness of the residual patella bone on the lateral and skyline views (Figs. 2, 3). The magnification of the radiograph was calculated using the measured diameter of the implant against the known diameter of the implant, and this magnification factor was used to correct the measured residual thickness of the patella bone. The percentage of the patella articular surface covered by the implant also was recorded. The diagnosis of osteonecrosis was indicated radiographically by fragmentation, collapse of the patella bone, and substantial change in the radiodensity of the patella [3, 41]. The presence of radiolucencies around the implant was noted on lateral and skyline views, and a note was made particularly of the size of the radiolucency (less or greater than 1 mm), if the radiolucencies were continuous around the implant, and if they were progressive. Radiographic loosening was defined as implant migration 3 mm or greater measured from the edge of the implant to the superficial and/or superior cortex of the patella or a continuous radiolucent line that had progressed in width or extent. The patella height was measured using the Insall-Salvati [16] and Blackburne-Peel [5] ratios. The tilt of the patella in relation to the femoral component and the tilt of the patella component in relation to the patella bone were measured on the skyline views (Fig. 4). A neutral range was defined as within −5° (medial tilt) and +5° (lateral tilt) [14]. Whether the patella implant had an intact superior rim also was recorded (Fig. 5). Note was made whether there was an uncovered portion of the patella articulating with the femoral component (Fig. 6).
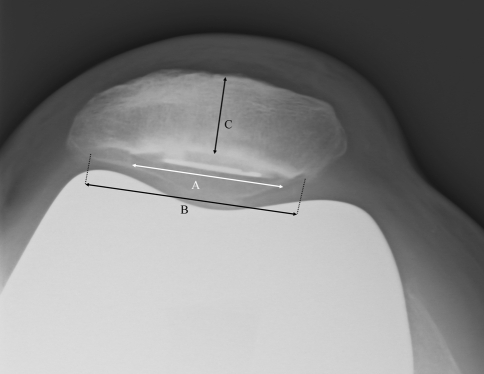
Fig. 2.
Radiographic measures on a lateral radiograph are shown. A = measured thickness of patella (later corrected for magnification). B = articular surface patella. C = measured diameter of patella implant. Percent covered by implant = C/B × 100. Magnification of radiograph = C/actual diameter patella implant. Thickness of residual patella = A/(magnification) × 100.
Fig. 3.
Radiographic measures on a skyline radiograph are shown. A = measured diameter of implant. B = articular surface patella. C = measured thickness patella. Percent covered by implant = A/B × 100. Magnification of radiograph = A/actual diameter patella implant. Thickness of residual patella = C/(magnification) × 100.
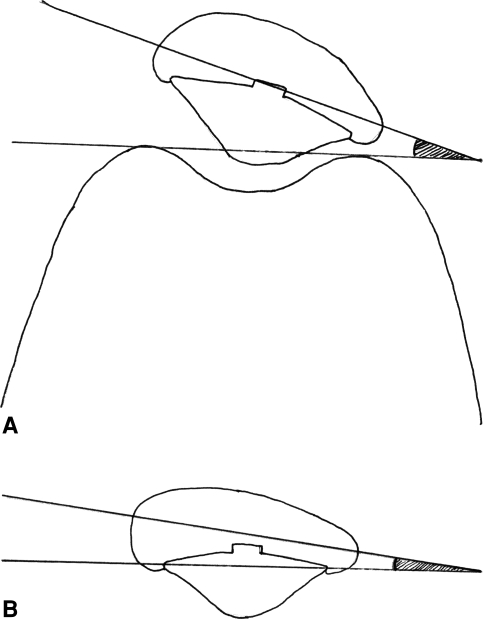
Fig. 4A–B.
The diagrams show radiographic measurements of (A) tilt of the patella to the femur and (B) tilt of the implant to the patella.
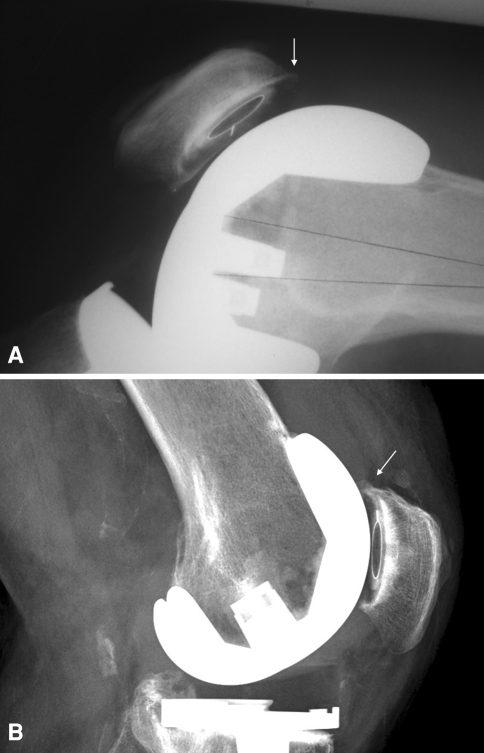
Fig. 5A–B.
The radiographs show the patella components (A) with no superior rim and (B) with an intact superior rim.
Fig. 6A–B.
The radiographs show the patella components with (A) central tracking and (B) the lateral facet of the patella articulating with the femur.
Kaplan-Meier survival curves [20] were generated for all patients enrolled in the study using aseptic revision of the patella component and aseptic revision or radiographic loosening as the end points. To determine whether there were differences between patients with and without aseptic failure of the implant, we used Fisher’s exact test (gender, type of knee replacement [Genesis® I or II], preoperative deformity [varus or valgus], approach [medial or lateral], use of a lateral release or not, posterior cruciate ligament retention or not, preoperative diagnosis [osteoarthritis or other], presence of avascular necrosis or not, preservation of a superior rim of bone or not) or nonpaired Student’s t test (age, BMI, height, weight, diameter of the implant). Factors that were significant either with Fisher’s exact test or Student’s t test were entered in a binary logistic regression model. To determine if there were differences between patients with and without anterior knee pain, we used Fisher’s exact test (gender, type of knee replacement [Genesis® I or II], preoperative deformity [varus or valgus], approach [lateral or medial], use of a lateral release or not, posterior cruciate ligament retention or not, preoperative diagnosis [osteoarthritis or other]) or nonpaired Student’s t test (age, height, weight, BMI). For patients in Group 1 (with recent clinical and radiographic followups), to determine if there were differences between patients with and without the presence of anterior knee pain, we used Fisher’s exact test (whether an uncovered lateral facet was articulating with the femoral component) or nonpaired Student’s t test (Insall-Salvati and Blackburne-Peel ratios, percentage cover of the implant of the patella on a lateral radiograph, tilt of the patella component, thickness of the residual patella bone). The Knee Society score and pain component of the Knee Society score also were compared between cases in which an uncovered lateral facet of the patella was articulating with the femoral component and those in which it was not using Student’s t test. Analyses were performed using SPPS® V10 for Windows® (SPSS Inc, Chicago, IL).
Results
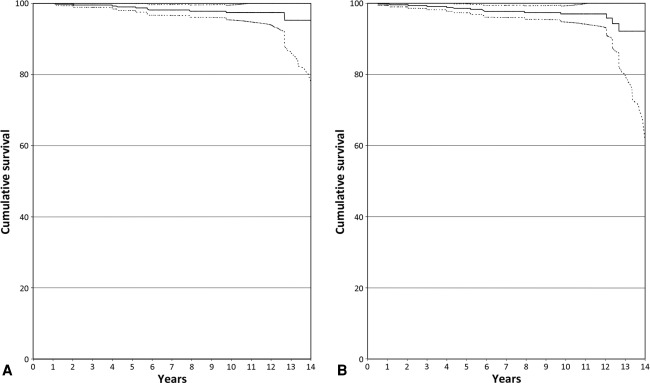
Ten patella components had been revised for aseptic reasons. Four implants were radiographically loose but had not been revised. Six had been revised or removed because of infection. Excluding patients with infection and those lost to followup, the rate of aseptic failure was 2.9%. Survivorship at 10 years using aseptic revision as the end point was 97.4% and using aseptic revision or radiographic loosening was 97.0% (Fig. 7). Eleven patella components had complete radiolucency on the most recent lateral, skyline, or both radiographs. In all cases, the radiolucencies measured 1 mm or less and were not progressive. These 11 cases were not judged as radiographically loose.
Fig. 7A–B.
Kaplan-Meier survivorship curves with (A) aseptic revision of the patella as the end point and (B) radiographic loosening or aseptic revision of the patella as the end point are shown. The data are based on the last available information available in the charts or most recent radiograph for the 213 patients either deceased or lost to followup, for whom only chart or radiographic followup was available. Dotted lines indicate 95% confidence intervals.
Osteonecrosis was a contributing factor involved in failure of the patella components in four patients (Table 1). The lack of a superior rim was observed in five cases and was potentially the major cause of failure in at least three cases. The presence of osteonecrosis and absence of a superior rim were independently associated with failure of the implant (p ≤ 0.01 and p = 0.03, respectively).
Table 1.
Factors potentially associated with aseptic failure of patella implants and outcomes of cases
| Mechanism of failure | Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Evidence of AVN | Fracture | Superior rim present? | Mechanism of failure | Treatment | Time to revision (years) | Revision of femoral and/or tibial component | Followup from time of primary surgery (years) | Presence of anterior knee pain | Pain component of Knee Society score (of 50) |
| Yes | Transverse | Yes | AVN; fracture | Observed | 15 | Yes weekly 8/10 | 45 | ||
| Yes | Fragmentation | Yes | AVN | Observed | 14 | No | 50 | ||
| No | No | Yes | ?Poorly supported on lateral and shear force form tilt | Observed | 13 | No | 45 | ||
| No | No | Yes | Unclear | Observed | 13 | No | 50 | ||
| No | No | No | No rim | Revised | 6 | 11 | No | 45 | |
| Yes | Longitudinal fracture, then fragments | No | AVN; fracture; no rim | Patellectomy | 1 | 5 (deceased) | Not recorded | “Ongoing pain” | |
| No | No | No | Revised for patella subluxation | Revised (and realignment) | 6 | 6 (demented) | Unknown | Unknown (patient demented, no further followup) | |
| No | No | No | No rim | Revised | 4 | 6 (deceased) | Not recorded | 45 | |
| Yes | Fragmentation | Unable to assess | AVN; fracture | Removed | 5 | 12 | No | 45 | |
| No | Longitudinal | Yes | Fracture | Removed; subsequent patellectomy 2 years later | 5 | Revised | 5 (deceased) | Not recorded | 20 |
| No | Longitudinal | Unable to assess | Fracture | Removed | 12 | Revised | 13 (deceased) | Not recorded | 45 |
| No | No | No | No rim | Revised | 10 | Revised (then further revision 1 year later) | 11 | Not recorded | 50 |
| No | No | Yes | Unclear | Revised | 14 | Revised | 14 | Recent revision | Recent revision |
| No earlier radiographs | No earlier radiographs | No earlier radiographs | Aseptic loosening, cause unclear | Removed | 5 | Revised for instability | 6 (deceased) | No | 50 |
AVN = avascular necrosis.
Average patella tilt in relation to the femoral component was 4.9° lateral, and the average tilt of the implant in relation to the patella was 1° medial (Table 2). Patella tilt in relation to the femur was within the neutral range in 63% of cases, and tilt of the component in relation to the patella was within the neutral range in 94% of cases.
Table 2.
Radiographic outcomes for cases in Group 1*
| Radiographic measurement | Value |
|---|---|
| Thickness patella bone on lateral radiograph (mm) | 12 (5–21) |
| Thickness patella bone on skyline radiograph (mm) | 13 (6–20) |
| Percent of patella covered by implant on lateral radiograph | 89 (68–101) |
| Percent of patella covered by implant on skyline radiograph | 77 (58–96) |
| Mean Insall-Salvati ratio | 1.00 (0.37–1.45) |
| Mean Blackburne-Peel ratio | 0.61 (0.26–1.19) |
| Average tilt patella to femur (degrees) (positive values = lateral tilt, negative values = medial tilt) | 4.9 (−11–18) |
| Average tilt implant to patella (degrees) | −1 (−10–8) |
* Excluding revisions and radiographic loosening of patella implant; values are expressed as means, with ranges in parentheses.
The prevalence of anterior knee pain was 7.8% for the 242 knees in Groups 1 and 2. The severity of anterior knee pain was recorded in 16 of the 19 knees with anterior knee pain; the mean severity was 4.2 on a scale of 1 to 10. We found no difference in any surgical, demographic, or radiographic factor examined between patients with anterior knee pain and those without anterior knee pain.
The average Knee Society knee score for patients in Group 1 was 92.2 (range, 37–100) at a mean of 11.2 years (range, 10–16 years), and the average function score was 61.9 (range, −10–100). Of this group, 48% had radiographic evidence of articulation of an uncovered portion of the lateral facet of the patella with the femoral component. The frequency of anterior knee pain, the mean pain component of the Knee Society score, and the mean Knee Society knee score were similar in patients who had an uncovered lateral facet articulating with the femoral component and in patients who did not (Table 3).
Table 3.
Comparison of radiographic and clinical outcomes between patellas in Group 1
| Outcome | Lateral facet patella articulates with component (48%)* | Central tracking of patella implant (35%)* | p Value |
|---|---|---|---|
| Percent with anterior knee pain | 5.1 | 6.7 | 0.73 |
| Pain component of Knee Society score | 47 | 45 | 0.10 |
| Knee Society score | 93 | 91 | 0.37 |
* Of the remaining cases: 4% articulation of medial facet of patella with femoral component; 13% indeterminate.
Dislocation of the patella component occurred in three cases (0.7%). Five patellas (1.2%) had evidence of osteonecrosis. In four of these five cases, there was associated loosening of the patella component either radiographically or at revision. A fracture that had the potential to disrupt the extensor mechanism or cause failure of the implant or fragmentation of the patella was noted in six cases (1.5%). In four of these cases, there was evidence radiographically of osteonecrosis. Two fractures were not clearly associated with osteonecrosis; there was subsequent failure of the patella components, which were treated with removal of the components.
Discussion
All-polyethylene patella implants have more favorable long-term results compared with most metal-backed patella implants [15, 36]. Most series have described the results of all-polyethylene patella components using an onlay design [1–4, 6, 12, 13, 24, 28, 30, 35, 37, 42, 44]. An alternative design is an inlay patella component. Potential advantages of the inlay patella component include increased area for cement-bone contact, preservation of peripheral patella bone stock, and more precise instrumentation and easier insertion [22, 39]. Previous reports have described satisfactory results in terms of anterior knee pain and failure rates at intermediate-term followup [10, 22, 25, 26]. Additionally, there is some biomechanical evidence supporting superior fixation strength of an inlay design over an onlay design [39]. Despite relatively widespread use, there are few long-term data on the survivorship or clinical results of inset biconvex patella components in knee arthroplasty. We have sought to present our experience with this implant at 10 years followup and to compare our results with those that have been historically reported for other types of patella implants, particularly regarding survivorship and anterior knee pain.
This study has numerous limitations. Selection bias exists as a result of incomplete followup for numerous surviving patients, those lost to followup, and the large number of patients who had died, although this is inevitable given the age of the patient cohort being studied and long duration of followup. We have presented the clinical results for 204 surviving patients with apparently well-fixed implants primarily to quantify the prevalence of anterior knee pain and review factors that may be associated with anterior knee pain. The description of the clinical results excludes 182 patients (42%) deceased at review, 31 patients (7.2%) lost to followup, two patients (0.5%) with recent radiographic review only (but no clinical followup), and 14 surviving patients (2.7%) with radiographically loose implants. However, chart records and the last available radiographs were reviewed for the entire cohort, and all known failures and complications are presented. All patients subsequently are included in the survivorship analysis. Followup was incomplete for numerous surviving patients who were unable to attend for radiographs or clinical examination; for patients in Group 2 (those with clinical followup by questionnaire but without a recent radiograph), this may underestimate the prevalence of complications that may be apparent radiographically only. Two differing designs of knee replacement were used (Genesis® I and II), which adds another confounding factor to the analysis. The study is retrospective, therefore data collection was incomplete in some areas, and imperfect radiographs in some cases were not included in the analysis. At the time of data collection, there was no universally accepted instrument for assessment of patellofemoral pain after TKA. The method we chose to assess anterior knee pain reflects information we collected prospectively in our database, being whether anterior knee pain was present and the severity on a visual analog scale, although the method has not been validated. We used prior publications on patella component outcomes as our control group. Comparison of survivorship, prevalence of anterior knee pain, and radiographic data involve referencing these historical controls, in which differing definitions of end points make direct comparison difficult. The strength of this study is that one reviewer collected all radiographic data and conducted the phone interviews, eliminating interobserver variability but potentially introducing systemic bias.
Our results suggest similar survivorship of this implant compared with those of other current and previous designs of cemented all-polyethylene patella components, although there is no clear advantage (Table 4). As in one other study [3], we found avascular necrosis is a major factor contributing to aseptic failure of cemented all-polyethylene patella components, although we could not correlate the use of lateral release to the occurrence of avascular necrosis. Failure to preserve an intact rim of bone around the implant, as indicated by the lack of a superior rim on lateral radiographs, also appears to be a factor in failure of this implant in some cases. With knee flexion we suppose a superiorly directed shear force is applied to the component, which can lead to failure of the implant, although there are no biomechanical studies to confirm or refute this. Although we could not correlate other factors to failure of this implant, a recent study of an onlay all-polyethylene patella component involving large numbers (8531) reported lateral release, BMI greater than 30 kg/m2, flexion greater than 100°, preoperative valgus alignment of 10° or greater, medial patella component position, and a tibial component greater than 12 mm were associated with aseptic loosening of the patella component [30]. The rate of fracture in our study was low, and most fractures occurred in relation to osteonecrosis.
Table 4.
Comparison of patella component failure and fracture in TKA
| Study | Number of cases | Mean followup (years) | Type of patella component* | Number of aseptic revisions and reasons | Number of radiographically loose cases | % of aseptic revisions and radiographic loosening | % of cases with fracture | % of cases with AVN |
|---|---|---|---|---|---|---|---|---|
| Rodricks et al. [37] | 145 | 15.8 | Onlay 3 peg |
3 loose 1 wear 2 dislocation 1 fracture |
0 | 4.8 | ||
| Vessely et al. [42] | 922 | 15.7 | Onlay 3 peg |
3 loose-revised 1 revised for dislocation 1 removal for fracture |
0.5 | 0.2 | ||
| Fetzer et al. [13] | 99 | 2.4–11.8 | Onlay 3 peg |
1 wear | 0 | 1 | 0 | |
| Berend et al. [3] | 4287 | 5.5 (for failed components) | Onlay 1 peg |
15 loose | 165 | 4.2 | 3.1 | Majority of failed components |
| Boyd et al. [6] | 396 | 6.5 | Onlay 1 peg |
5 | 1.2 | 0.7 | ||
| Kitsugi et al. [22] | 53 | 6.3 | Inset | 0 | 0 | 0 | 0 | |
| Ranawat [35] | 100 | 5–10 | Onlay 1 peg |
0 | 1 | 1 | 2 | 1 |
| Ewald et al. [12] | 240 | 10–14 | Onlay 1 peg |
10 loose | 4.1 | |||
| Laskin [25] | 93 | 10 | Inset | 1 loose | 0 | 1 | 0 | |
| Larson et al. [24] | 228 | 5.4 | Onlay 1 peg (37%) 3 peg (63%) |
0 | 0 | 0 | 3.1 | |
| Brick and Scott [7] | 2887 | Various, all loose were onlay, one peg, all polyethylene | 12 loose | 4 | 0.5 | 0.5 | ||
| Crites and Berend [11] | 296 | 10 | Metal backed | 18 poly dissociation/metallosis | 10 | 9.5 | ||
| Meding et al. [30] | 8531 | 7 | Onlay 1 peg | 25 | 384 | 4.8 | 5.2 | |
| Rosenberg et al. [38] | 122 | Metal backed | 8 loose (sheared pegs) | 4 | 9.8 | |||
| Jordan et al. [18] | 226 | 17 | Metal backed mobile bearing | 3 poly wear 1 “ improve range of motion” |
0 | 1.6 | 0 | |
| Current study | 481 | 7.7 | Inset | 10 | 4 | 2.9 | 1.5 | 1.2 |
* Unless otherwise stated, components were all-polyethylene; AVN = avascular necrosis.
Although one study showed improvement in patella tracking with an inset patella component over an onlay patella component [14], our data do not show any clear advantage of the inset patella with respect to patella tilt over that of other designs (Table 5). This finding is not unexpected given that, although accurate implantation of a patella component is important in satisfactory patella tracking, other factors such as femoral and tibial component rotation, femoral component size and morphology, and soft tissue tension also influence patella tracking. Our results, and those of previous studies of inset patella components [14, 22], do suggest, in the majority of cases, the component is implanted within a neutral range (between −5° and +5°) with respect to the patella bone. Newer techniques of patella resection and preparation of onlay patella components, however, also seem to provide satisfactory alignment of the patella [29].
Table 5.
Comparison of patella tilt in TKA
| Study | Number of cases | Type of component | Average tilt patella-femur (degrees) | % within neutral (patella-femur) | Average tilt implant-patella (degrees) | % within neutral (implant- patella) |
|---|---|---|---|---|---|---|
| Lewonowski et al. [28] | 62 | Onlay | 8.3 (for central placement) 11 (for medial placement) |
65 | ||
| Bindelgass et al. [4] | 234 | Onlay | 54.7 | |||
| Ledger et al. [27] | 80 | Dome | 2.3 | 92.5 | 2 | 88 |
| Kawano et al. [21] | 62 | Onlay | −1 | 81 | 3.2 | 76 |
| Gomes et al. [14] | 40 | Onlay and inset | 8.3 (onlay) | Not specified (onlay) | 5.9 (onlay) | 50 (onlay) |
| 1.8 (inset) | 90 (inset) | 1.4 (inset) | 90 (inset) | |||
| Larson et al. [24] | 228 | Onlay (2 different designs) | 4.5 | 70, 76 | ||
| Lombardi et al. [29] | 55 | Onlay | 1 | 89 | ||
| Baldini et al. [1] | 100 | Onlay | Not specified | 83 | ||
| Kitsugi et al. [22] | 53 | Inset | 3 | Not specified | 0 | 100 |
| Current study | 166 | Inset | 5 | 63.3 | 1.6 | 94 |
Comparison of anterior knee pain prevalence between different studies is difficult given there is no universally accepted outcome instrument for assessing patellofemoral pain. Previous studies have reported anterior knee pain rates between less than 1% [6] and 47% [9] for knee arthroplasties performed with an all-polyethylene patella component. Given this limitation, our results are broadly equivalent to those that have been described for this type of patella component and for those of other designs (Table 6). We could not find any demographic factor that correlated with the presence of anterior knee pain or pain scores. Other studies generally have had similar findings, although one study did find a correlation between weight and anterior knee pain [44]. Similar to others [4, 19, 23], we could not correlate any radiographic factor to anterior knee pain, particularly patella tilt. However, a recent study using a new patellofemoral scoring system and radiographic technique did report a correlation of anterior knee pain and patella tilt [1].
Table 6.
Comparison of anterior knee pain in TKA with patella resurfacing
| Study | Number of cases | Mean followup (years) | Type of implant | % with anterior knee pain |
|---|---|---|---|---|
| Baldini et al. [1] | 100 | 8.5 | Onlay | 19 |
| Barrack et al. [2] | 93 (47 resurfaced) | 5.8 | Onlay | 19 |
| Wood et al. [44] | 220 (92 resurfaced) | 4 | Onlay | 16 |
| Waters and Bentley [43] | 474 (243 resurfaced) | 5.3 | All polyethylene, type not stated | 5.3 |
| Larson et al. [24] | 228 | 5.4 | Onlay | 8.3 |
| Kaper et al. [19] | 300 | 1.6 | Inset | 5.3 |
| Kitsugi et al. [22] | 53 | 6.3 | Inset | 7.5 |
| Smith et al. [40] | 181 (87 resurfaced) | 4.4 | Inset | 30 |
| Current study | 242 | 11.4 | Inset | 7.8 |
One of the potential criticisms of this inset biconvex implant is, given the wider mediolateral dimensions of the native patella compared with the superoinferior dimensions, a portion of the lateral facet of the patella can remain uncovered by the implant, which could be a potential source of pain if it subsequently articulates with the femoral component. Our study, however, showed articulation of an uncovered portion of the patella with the femoral component did not correlate with the presence of anterior knee pain or a lower Knee Society score.
We did not attempt to address the question of whether routine patella resurfacing is warranted. If the decision has been made to resurface the patella, an inset biconvex patella component represents an alternative to onlay patella components. The technique and instrumentation give satisfactory alignment in terms of tilt of the component in relation to the patella bone in the majority of cases. The survivorship, complications, and clinical results are equivalent to those historically reported for other designs of patella replacement.
Acknowledgments
We thank Cecil Rorabeck, MD, FRCS, Jeff Guerin, BMath, and Julie Marr, RN, for their contributions to this study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Baldini A, Anderson JA, Zampetti P, Pavlov H, Sculco TP. A new patellofemoral scoring system for total knee arthroplasty. Clin Orthop Relat Res. 2006;452:150–154. [DOI] [PubMed]
- 2.Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty: a prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am. 2001;83:1376–1381. [PubMed]
- 3.Berend ME, Ritter MA, Keating EM, Faris PM, Crites BM. The failure of all-polyethylene patellar components in total knee replacement. Clin Orthop Relat Res. 2001;388:105–111. [DOI] [PubMed]
- 4.Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop Relat Res. 1993;286:103–109. [PubMed]
- 5.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241–242. [DOI] [PubMed]
- 6.Boyd AD Jr, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;75:674–681. [DOI] [PubMed]
- 7.Brick GW, Scott RD. The patellofemoral component of total knee arthroplasty. Clin Orthop Relat Res. 1988;231:163–178. [PubMed]
- 8.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res. 2004;428:12–25. [DOI] [PubMed]
- 9.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88:734–739. [DOI] [PubMed]
- 10.Chen AL, Mujtaba M, Zuckerman JD, Jeong GK, Joseph TN, Wright K, Di Cesare PE. Midterm clinical and radiographic results with the Genesis I total knee prosthesis. J Arthroplasty. 2001;16:1055–1062. [DOI] [PubMed]
- 11.Crites BM, Berend ME. Metal-backed patellar components: a brief report on 10-year survival. Clin Orthop Relat Res. 2001;388:103–104. [DOI] [PubMed]
- 12.Ewald FC, Wright RJ, Poss R, Thomas WH, Mason MD, Sledge CB. Kinematic total knee arthroplasty: a 10- to 14-year prospective follow-up review. J Arthroplasty. 1999;14:473–480. [DOI] [PubMed]
- 13.Fetzer GB, Callaghan JJ, Templeton JE, Goetz DD, Sullivan PM, Kelley SS. Posterior cruciate-retaining modular total knee arthroplasty: a 9- to 12-year follow-up investigation. J Arthroplasty. 2002;17:961–966. [DOI] [PubMed]
- 14.Gomes LS, Bechtold JE, Gustilo RB. Patellar prosthesis positioning in total knee arthroplasty: a roentgenographic study. Clin Orthop Relat Res. 1988;236:72–81. [PubMed]
- 15.Healy WL, Wasilewski SA, Takei R, Oberlander M. Patellofemoral complications following total knee arthroplasty: correlation with implant design and patient risk factors. J Arthroplasty. 1995;10:197–201. [DOI] [PubMed]
- 16.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. [DOI] [PubMed]
- 17.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 18.Jordan LR, Sorrells RB, Jordan LC, Olivo JL. The long-term results of a metal-backed mobile bearing patella. Clin Orthop Relat Res. 2005;436:111–118. [DOI] [PubMed]
- 19.Kaper BP, Woolfrey M, Bourne RB. The effect of built-in external femoral rotation on patellofemoral tracking in the Genesis II total knee arthroplasty. J Arthroplasty. 2000;15:964–969. [DOI] [PubMed]
- 20.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [DOI]
- 21.Kawano T, Miura H, Nagamine R, Urabe K, Matsuda S, Mawatari T, Moro-Oka T, Iwamoto Y. Factors affecting patellar tracking after total knee arthroplasty. J Arthroplasty. 2002;17:942–947. [DOI] [PubMed]
- 22.Kitsugi T, Gustilo RB, Bechtold JE. Results of nonmetal-backed, high-density polyethylene, biconvex patellar prostheses: a 5-7-year follow-up evaluation. J Arthroplasty. 1994;9:151–162. [DOI] [PubMed]
- 23.Larson CM, Lachiewicz PF. Patellofemoral complications with the Insall-Burstein II posterior-stabilized total knee arthroplasty. J Arthroplasty. 1999;14:288–292. [DOI] [PubMed]
- 24.Larson CM, McDowell CM, Lachiewicz PF. One-peg versus three-peg patella component fixation in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:94–100. [DOI] [PubMed]
- 25.Laskin RS. The Genesis total knee prosthesis: a 10-year followup study. Clin Orthop Relat Res. 2001;388:95–102. [DOI] [PubMed]
- 26.Laskin RS, Davis J. Total knee replacement using the Genesis II prosthesis: a 5-year follow up study of the first 100 consecutive cases. Knee. 2005;12:163–167. [DOI] [PubMed]
- 27.Ledger M, Shakespeare D, Scaddan M. Accuracy of patellar resection in total knee replacement: a study using the medial pivot knee. Knee. 2005;12:13–19. [DOI] [PubMed]
- 28.Lewonowski K, Dorr LD, McPherson EJ, Huber G, Wan Z. Medialization of the patella in total knee arthroplasty. J Arthroplasty. 1997;12:161–167. [DOI] [PubMed]
- 29.Lombardi AV Jr, Mallory TH, Maitino PD, Herrington SM, Kefauver CA. Freehand resection of the patella in total knee arthroplasty referencing the attachments of the quadriceps tendon and patellar tendon. J Arthroplasty. 1998;13:788–792. [DOI] [PubMed]
- 30.Meding JB, Fish MD, Berend ME, Ritter MA, Keating EM. Predicting patellar failure after total knee arthroplasty. Clin Orthop Relat Res. 2008;466:2769–2774. [DOI] [PMC free article] [PubMed]
- 31.Nizard RS, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, Sedel L. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432:196–203. [DOI] [PubMed]
- 32.Ogon M, Hartig F, Bach C, Nogler M, Steingruber I, Biedermann R. Patella resurfacing: no benefit for the long-term outcome of total knee arthroplasty: a 10- to 16.3-year follow-up. Arch Orthop Trauma Surg. 2002;122:229–234. [DOI] [PubMed]
- 33.Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2005;87:1438–1445. [DOI] [PubMed]
- 34.Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005;438:191–196. [DOI] [PubMed]
- 35.Ranawat CS. The patellofemoral joint in total condylar knee arthroplasty: pros and cons based on five- to ten-year follow-up observations. Clin Orthop Relat Res. 1986;205:93–99. [PubMed]
- 36.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85:259–265. [DOI] [PubMed]
- 37.Rodricks DJ, Patil S, Pulido P, Colwell CW Jr. Press-fit condylar design total knee arthroplasty: fourteen to seventeen-year follow-up. J Bone Joint Surg Am. 2007;89:89–95. [DOI] [PubMed]
- 38.Rosenberg AG, Andriacchi TP, Barden R, Galante JO. Patellar component failure in cementless total knee arthroplasty. Clin Orthop Relat Res. 1988;236:106–114. [PubMed]
- 39.Rosenstein AD, Postak PD, Greenwald AS. Fixation strength comparison of onlay and inset patellar implants. Knee. 2007;14:194–197. [DOI] [PubMed]
- 40.Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the Profix total knee system. J Bone Joint Surg Br. 2008;90:43–49. [DOI] [PubMed]
- 41.Smith PN, Parker DA, Gelinas J, Rorabeck CH, Bourne RB. Radiographic changes in the patella following quadriceps turndown for revision total knee arthroplasty. J Arthroplasty. 2004;19:714–719. [DOI] [PubMed]
- 42.Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat Award. Long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006;452:28–34. [DOI] [PubMed]
- 43.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2003;85:212–217. [DOI] [PubMed]
- 44.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84:187–193. [DOI] [PubMed]