Abstract
Due to the rise in prosthetic joint implantations, prosthetic joint infections (PJI) are increasing. Most PJI are treated outside the hospital setting via community-based parenteral antiinfective therapy (CoPAT) after initial surgical management, although little is reported about the short-term complications of CoPAT. We therefore ascertained the numbers of unanticipated readmissions, unplanned surgeries, and CoPAT complications within 12 weeks of hospital discharge in patients with PJI on CoPAT. We retrospectively reviewed the charts of 74 patients with PJI. Twenty-seven (73% of readmitted patients) were for unanticipated reasons within 12 weeks of hospital discharge; 16 (43% of readmitted) underwent an unplanned surgery. Nine patients (12% of total cohort) had CoPAT-related adverse events. Our data suggest patients with PJI on CoPAT represent a complex cohort that needs to be monitored closely for complications early after hospital discharge.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Prosthetic joint implantations (PJI) lead to pain relief and improved function in most patients with inflammatory and degenerative arthritis. More than 750,000 prosthetic joints are implanted in the United States annually [1]. PJI are one of the most common complications of joint arthroplasty, along with aseptic loosening [14] and dislocation of prosthetic components [6, 12]. Rates of PJI in most centers currently range between 0.5% to 1% for hip arthroplasties [2, 13], 0.5% to 2% for knee arthroplasties [2, 13], and less than 1% for shoulder arthroplasties [9]. PJI cause significant morbidity and account for a substantial proportion of health care expenditures [4, 10]. Recent data suggest more than $25 billion is spent annually on management of PJI [1].
Management of PJI is often difficult due to variable clinical presentations, a patient population with multiple comorbidities, and lack of high level studies on which to base standardized guidelines for therapy. Effective treatment of PJI requires a combined medical and surgical approach, usually with long courses of systemic antimicrobials. Often, intravenous antimicrobials are administered outside the acute care setting. Bone and joint infections are the most common indication for outpatient parenteral antiinfective therapy [3]. Zhan et al. have reported readmission rates of 12% after hip arthroplasty and 43% after knee arthroplasty at 1 year of followup [15]. To our knowledge, short term readmission rates in patients with PJI have not been evaluated.
We determined (1) the frequency of early unanticipated readmissions in patients with PJI on CoPAT, (2) the frequency of unplanned surgeries, and (3) CoPAT-related complications in these patients.
Materials and Methods
In July 2007, we created a specialized bone and joint infection service as part of a multidisciplinary team for study of diagnosis, management, and prevention of PJI. The Bone and Joint Infection Study Group comprises infectious disease (ID) physicians and orthopaedic surgeons, microbiologists, pathologists, infection control practitioners, and pharmacists. The Bone and Joint Infection Service works closely with the CoPAT Team of Excellence. This team, convened for study and improvement of CoPAT processes and outcomes, comprised ID physicians, the vascular access team, inpatient case managers, and home health pharmacy and nursing representatives.
We retrospectively reviewed the medical records of 74 patients obtained from a CoPAT registry maintained at our institution, who were treated for PJI using CoPAT between July 1, 2007 and December 31, 2007. PJI were defined as presence of one or more of the following: clinical signs/symptoms, purulence of synovial fluid or at the implant site, growth of the same microorganisms in two or more cultures of synovial fluid or periprosthetic tissue, acute inflammation on pathologic examination of periprosthetic tissue, and presence of a sinus tract communicating with the prosthesis [2, 11, 16]. CoPAT was defined as antiinfective therapy given intravenously in the community setting after hospital discharge; this designation in our institution is functionally equivalent to the term “OPAT” or outpatient parenteral antibiotic therapy. We included patients with at least 12 weeks of followup: 54 with outpatient followup and 20 who completed a telephone questionnaire. We considered only the first CoPAT episode per patient and excluded subsequent CoPAT episodes for the same patient. By protocol, laboratory monitoring was performed weekly and varied according to the antimicrobial agent used. All patients had outpatient followup scheduled before hospital discharge; timing of outpatient followup visits varied due to the geographic diversity of patient population and sites of outpatient care. Twenty patients were lost to followup after the index hospitalization; we located these 20 patients by phone to complete a voluntary questionnaire (Appendix 1) pertaining to readmission outside of our hospital system, reoperation and intravenous catheter related complications.
Data were collected from review of electronic health records. Patient demographic data included age, gender, body mass index (BMI), history of osteoarthritis, rheumatoid arthritis, diabetes mellitus (with HbA1c if available), immunosuppression, and prior history of PJI. Data were also collected about type of operative procedure during index hospitalization preceding CoPAT, type of joint involved with PJI, and microbial pathogens isolated in culture. CoPAT data included intravenous antimicrobials prescribed, duration of CoPAT and type of intravenous access. CoPAT complications assessed were timing and types of antimicrobial adverse effects and vascular access complications. Timing and reason for first readmission after index hospitalization were collected. Outcomes assessed were unanticipated readmissions, unplanned surgeries and CoPAT complications.
Index hospitalization was defined as the first hospital encounter when PJI were diagnosed during the study period. Immunosuppression was defined as presence of one or more of the following: underlying malignancy, posttransplant, autoimmune disease, being on 5 or more mg prednisone daily and/or other immunosuppressive agents at the time of index hospitalization. Acute kidney injury was defined as an abrupt (within 48 hours) absolute increase in the serum creatinine concentration of 0.3 mg/dL or more from baseline or a percentage increase in the serum creatinine concentration of 50% or higher [7]. Drug-induced hepatitis was defined as elevation of alanine aminotransferase (ALT) greater than two times the upper limit of normal from exposure to the presumed offending drug with no evidence of underlying liver disease, and normalization of ALT after stopping the drug [8]. Planned surgery was defined as a procedure that was expected to be performed at a defined interval after hospital discharge, for example the second stage of a two-stage arthroplasty. Unplanned surgery was defined as a procedure that was performed emergently or urgently after hospital discharge due to complications involving the prosthetic joint such as bleeding or infection. CoPAT start date was defined as the date of hospital discharge. CoPAT end date was defined as date of readmission to the hospital for any reason or date of completion of anticipated CoPAT.
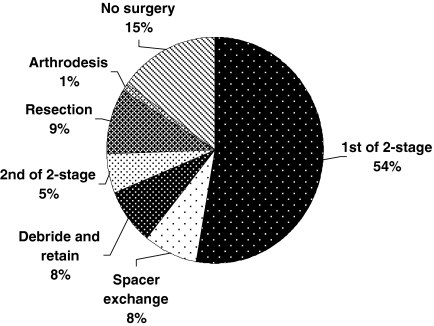
Median age of the study population was 64 years (range, 25–88 years) and 54% were men. Median BMI was 33 (range, 18–64). Twenty-five patients (34%) had diabetes mellitus with a mean HbA1c of 6.9 (measured in 17 patients at index hospitalization). Forty-three patients (58%) had a prior history of PJI in the same joint (Table 1). Most commonly involved prostheses were knees (47 patients, 63%), followed by hips (19 patients, 26%), shoulders (five patients, 7%), and others (three patients, 4%). Median CoPAT duration was 35 days (range, 2–80 days). Most patients had CoPAT administered via peripherally inserted central catheters (69 patients, 93%). The most common surgery performed immediately preceding CoPAT episode was first stage of a two-stage revision arthroplasty (39 patients, 54%) (Fig. 1).
Table 1.
Demographics of patients (n = 74)
| Variable | Value |
|---|---|
| Age in years | 64 (range, 25–88) |
| BMI | 33 (range, 18–64) |
| Osteoarthritis | 45 (61%) |
| Recurrent PJI—same joint | 43 (58%) |
| Male gender | 40 (54%) |
| Diabetes mellitus | 25* (34%) |
| Immunocompromised | 8 (11%) |
| Rheumatoid arthritis | 5 (7%) |
* Mean HbA1c—6.9.
Fig. 1.
The most common type of orthopaedic surgery performed immediately preceding CoPAT episode was 1st stage of a 2-stage revision arthroplasty (n = 74).
Pathogens identified were coagulase-negative staphylococcus species (25 isolates, 23%), Staphylococcus aureus (23 isolates, 22%), other Gram-positive bacteria (15 isolates, 15%), Gram-negative bacteria (15 isolates, 15%), and others (25 isolates, 25%). Twenty-two patients (30%) had polymicrobial PJI.
The most common antimicrobial used for CoPAT was vancomycin (49 courses, 56%). Other antimicrobials used were oxacillin (nine courses, 10%), daptomycin (eight courses, 9%), piperacillin-tazobactam (six courses, 7%), cephalosporins (five courses, 6%), ampicillin-sulbactam (three courses, 3%), and others (eight courses, 9%). Eleven patients (15%) had CoPAT with more than one antimicrobial agent.
JMP® 7.0 software (SAS Institute, Cary, NC) was used for generating survival curves using readmission as an endpoint. Planned readmissions were censored. We performed no other statistical analysis. Data were reported as numbers and percentages.
Results
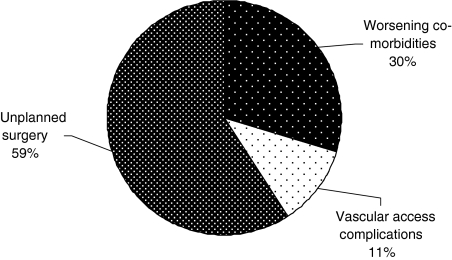
Thirty seven of the 74 patients (50% of total cohort) were readmitted within 12 weeks of index hospitalization. Twenty-seven (73% of readmissions) were for unanticipated reasons (Fig. 2), 10 (27% of readmissions) were for planned reoperation. Reasons for unplanned readmissions were: uncontrolled infection requiring unplanned surgery—16 patients (59% of unanticipated readmissions); worsening of existing comorbid conditions—eight patients (30% of unanticipated readmissions), which included altered mental status (two), heart failure exacerbation (one), hypertensive urgency (one), pancreatitis (one), acute renal failure (one), sickle cell crisis (one), systemic acidosis (one); and vascular access complications—three patients (11% of unanticipated readmissions). Nineteen (70% of unanticipated readmissions) occurred before CoPAT could be completed.
Fig. 2.
The most common reason for unanticipated readmission was an unplanned surgical procedure (n = 27).
Unplanned surgery for uncontrolled infection was performed in 16 patients (59% of unanticipated readmissions). The median time to unplanned surgery was 37 days from index hospitalization.
There were 3 CoPAT complications leading to readmission (11% of unanticipated readmissions): two for deep venous thrombosis related to peripherally inserted central catheter, and one for vascular access related bacteremia. There were no readmissions related to antimicrobial adverse effects. Five of the 74 patients (7%) had documented antibiotic adverse effects (2.15 per 1000 CoPAT days) and four (5%) had vascular access complications (1.72 per 1000 CoPAT days), occurring at a median of 22 days and 8 days after discharge, respectively (Table 2).
Table 2.
CoPAT complications
| Complication | Antimicrobial | Frequency/event(s) per 1000 CoPAT days | Time to event (days) |
|---|---|---|---|
| Antimicrobial related | |||
| Rash | Vancomycin | 1/0.4 | 30 |
| Nausea/vomiting | Vancomycin | 1/0.4 | 18 |
| Acute kidney injury | Vancomycin | 2/0.9 | 7,22 |
| Drug-induced hepatitis | Oxacillin | 1/0.4 | 42 |
| Vascular access related | |||
| Bacteremia | 1/0.4 | 9 | |
| DVT | 2/0.9 | 3,7 | |
| Occlusion | 1/0.4 | 7 | |
Discussion
PJI represent a rising problem due to an increase in prosthetic joint implantation. In an era of cost containment, patients usually complete their course of antibiotic therapy outside of the hospital. We determined the incidence and reasons for early unanticipated readmissions in patients with PJI on outpatient parenteral antiinfective therapy.
The limitations of our study include that our institution is a large referral center with a high degree of patient acuity and case complexity, thus decreasing the generalizability of our results to smaller centers. Our retrospective study design with limited subcohorts precludes statistical analysis of efficacy of specific surgical management plans and evaluation of risk factors for unanticipated readmissions in our patient cohort.
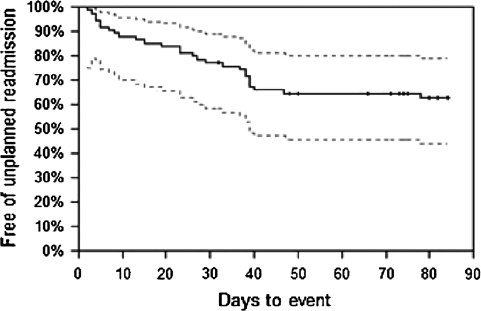
A high number of patients in our study had an unplanned readmission within 12 weeks of index hospitalization (Fig. 3). Unplanned readmission-free survival was 63% at 12 weeks of followup.
Fig. 3.
Study patients had an unanticipated readmission-free survival of 63% (solid line) at 12 weeks of followup. 95% confidence intervals are shown in dotted lines.
Long-term readmission rates in patients with PJI have been described. One such study looking at preoperative risks and outcomes after knee and hip arthroplasty in a population of Veterans Administration (VA) patients (from 1991 to 1997) reported readmission rates associated with PJI of 12% (n = 6876) in patients after hip arthroplasty and 43% (n = 11,710) in patients after knee arthroplasty at 12 months of followup, among other outcomes [15]. However, it is unclear how many of these readmissions occurred within 12 weeks of the index orthopaedic procedure.
A recent multicenter study found outpatient parenteral antimicrobial therapy suitable, cost-effective, and safe in bone and joint infections [5]. However, most of the population in this study received intravenous antimicrobials in hospital infusion centers rather than the community setting. Our study complements these prior data: none of our cohort received intravenous antimicrobials in infusion centers.
Taken as a whole, these findings underscore the complexity of management of PJI and the need for close monitoring and prompt management of early complications after hospital discharge. Our data suggest further investigation into risk factors leading to early complications during CoPAT for PJI, and for timely interventions to reduce these complications. According to a recent survey of ID physicians’ involvement and experiences in outpatient parenteral antimicrobial therapy, investigators reported variable role of ID consultants and heterogeneity in oversight and management practices [3]. It is our belief and practice that multidisciplinary teams, such as the ones we have assembled in our institution, can contribute toward a patient-centered, standardized approach to surgical, medical, and case management issues in PJI.
Acknowledgments
We thank Nabin K. Shrestha MD, MPH, Carlos M. Isada, MD, Steven M. Gordon, MD, David van Duin, MD (Department of Infectious Disease, Cleveland Clinic), and Viktor Krebs, MD, Robert Molloy, MD, and Ulf Knothe, MD (Department of Orthopedic Surgery, Section of Adult Reconstruction, Cleveland Clinic) for their input and advice.
Appendix 1
Phone script
Hello Mr/Ms…..
This is Dr Duggal calling from the Cleveland Clinic, Department of Infectious Disease. We are doing a research study to see how patients with bone and joint infections do after discharge from the hospital on IV antibiotics. You are receiving this call because you were recently treated for an infection by the Department of Infectious Disease. The study involves answering a few questions regarding your____infection. This will take approximately 5 minutes. Your participation in this study is completely voluntary. If you choose not to participate in the research your care at the Cleveland Clinic will not be affected in any way. Would you agree to participate in the research by answering a few questions?
Is this a good time?
[if no: ‘‘Thank you very much for your time’’]
[If yes: phone interviewer will go through items 1–4]
As you would recollect, you had an infection in_____ joint/bone while at Cleveland Clinic, and you were discharged on intravenous antibiotics. Have you had any surgery on the same_____joint/bone since your last infectious disease or surgery follow up visit?
[if no, go to next question]
[if yes, obtain date of surgery, hospital where surgery was performed]
Have you been admitted to a hospital other than the Cleveland Clinic for any reason since your last infectious disease or surgery follow up visit?
[if no, go to next question]
[if yes, obtain date, reason for admission, name of hospital]
Have you had any more infection(s) of the______ joint/bone for which you were treated by Cleveland Clinic Infectious Disease physician?
[if no, go to next question]
[if yes, obtain date of diagnosis, name of treating physician, antibiotic used, length of treatment, name of
the germ which caused the infection]
Since your last infectious disease or surgery follow up, have you had any clotting or infection of the long-term intravenous line placed to give the antibiotics?
[if no, go to end message]
[if yes, date of clotting or infection, name of hospital]
Thank you so much for answering these questions.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.American Academy of Orthopaedic Surgeons. Information about Orthopaedic Patients and Conditions. Available at: http://www.aaos.org/Research/stats/patientstats.asp. Accessed July 9, 2008.
- 2.Berbari EF, Hanssen AD, Duffy MC, Steckelberg JM, Ilstrup DM, Harmsen WS, Osmon DR. Risk factors for prosthetic joint infection: Case-control study. Clin Infect Dis. 1998;27:1247–1254. [DOI] [PubMed]
- 3.Chary A, Tice AD, Martinelli LP, Liedtke LA, Plantenga MS, Strausbaugh LJ. Experience of infectious diseases consultants with outpatient parenteral antimicrobial therapy: Results of an emerging infections network survey. Clin Infect Dis. 2006;43:1290–1295. [DOI] [PubMed]
- 4.Darouiche RO. Treatment of infections associated with surgical implants. N Engl J Med. 2004;350:1422–1429. [DOI] [PubMed]
- 5.Esposito S, Leone S, Noviello S, Ianniello F, Fiore M, Russo M, Foti G, Carpentieri MS, Cellesi C, Zanelli G, Cellini A, Girmenia C, De Lalla F, Maiello A, Maio P, Marranconi F, Sabbatani S, Pantaleoni M, Ghinelli F, Soranzo ML, Vigano P, Re T, Viale P, Scudeller L, Scaglione F, Vullo V. Outpatient parenteral antibiotic therapy for bone and joint infections: An Italian multicenter study. J Chemother. 2007;19:417–422. [DOI] [PubMed]
- 6.Lindberg HO, Carlsson AS, Gentz CF, Pettersson H. Recurrent and non-recurrent dislocation following total hip arthroplasty. Acta Orthop Scand. 1982;53:947–952. [DOI] [PubMed]
- 7.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A. Acute kidney injury network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. [DOI] [PMC free article] [PubMed]
- 8.Navarro VJ, Senior JR. Drug-related hepatotoxicity. N Engl J Med. 2006;354:731–739. [DOI] [PubMed]
- 9.Sperling JW, Kozak TK, Hanssen AD, Cofield RH. Infection after shoulder arthroplasty. Clin Orthop Relat Res. 2001;382:206–216. [DOI] [PubMed]
- 10.Steckelberg JM, Osmon DR. Prosthetic joint infections. In: Waldvogel FA, Bisno AL. Infections Associated with Indwelling Medical Devices, 3rd Ed. Washington, DC: ASM Press; 2000:173–177.
- 11.Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steckelberg JM, Patel R. Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am J Med. 2004:117:556–562. [DOI] [PubMed]
- 12.Vaughn BK. Managing chronic dislocated total hip arthroplasty. Semin Arthroplasty. 1993;4:16–24. [PubMed]
- 13.Widmer AF. New developments in diagnosis and treatment of infection in orthopedic implants. Clin Infect Dis. 2001;33 Suppl 2:S94–S106. [DOI] [PubMed]
- 14.Wroblewski BM, Siney PD, Fleming PA. Charnley low-frictional torque arthroplasty in patients under the age of 51 years Follow-up to 33 years. J Bone Joint Surg Br 2002;84:540–543. [DOI] [PubMed]
- 15.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89:526–533. [DOI] [PubMed]
- 16.Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351:1645–1654. [DOI] [PubMed]