Abstract
Although high-flexion TKA designs aim to safely accommodate deep flexion, it is unknown how often patients use deep flexion outside the laboratory. We used a validated smart-activity monitor to document the prevalence of knee flexion greater than 90° in 20 consecutive patients (21 knees) who had high-flexion TKAs, at a minimum of 2 years’ followup. Patients wore the device continuously for a mean of 35.7 ± 0.5 hours. The 21 knees flexed more than 90° for an average of 10 ± 3.8 minutes (0.5%). Activities performed with flexion greater than 90° were, on average, 70% in single-limb stance, 12% moving from sitting to standing, 8% walking, 7% moving from standing to reclining, 2% stepping, 0.9% moving from lying to standing, and 0.1% running. Eight knees flexed greater than 120° for an average of 2.2 minutes (range, 0.2–15 minutes), or 0.1% of the testing time. Activities performed with flexion greater than 120° were, on average, 90% in single-limb stance, 6% moving from sitting to standing, 3% walking, 0.6% moving from standing to reclining, 0.3% stepping, and 0.1% moving from lying to standing. Peak flexion used at any time during testing was, on average, 84% ± 11% of maximum postoperative flexion (125° ± 12°). These patients rarely used deep flexion.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA has evolved so that patients can expect long-term success rates of 85% at 10 to 15 years followup [14, 16, 17, 37, 46, 51]. Although the procedure was developed to relieve pain and restore function, the success of pain relief has been better than restoration of knee motion and kinematics [57]. Research efforts have focused on improving motion, as knee motion correlates with clinical outcome [34, 39, 43, 61]. In one study, 176 patients were interested in stretching, kneeling, and gardening (activities that require knee flexion greater than 90°), yet 54% to 72% of the patients found these activities difficult to perform after TKA [61].
The functional range of knee motion has been studied extensively [7, 30, 40, 49]. In general, gait and climbing slopes required greater than 90° knee flexion, using stairs and getting in and out of chairs required 90° to 120° flexion, and getting in and out of a bath required 135° flexion [40, 50]. Individuals typically need 111° to 165° knee flexion for kneeling, squatting, and sitting cross-legged [21, 39, 41]. Activities such as golf, catching in a softball game, meditation, yoga, and gardening often require knee flexion greater than 150° [39, 50]. Checking the line for a putt in golf, an activity enjoyed by many potential patients for TKA and one that requires squatting, may require greater than 120° knee flexion [33, 57].
Although the achievement of deep knee flexion (> 120°) after TKA in certain populations is considered an additional benefit from a successful operation, for some people, such motion postoperatively is a requirement of their interests or culture. Farmers, plumbers, and construction workers depend on deep knee flexion for their work [60]. Middle Eastern and Asian populations may require deep knee flexion for activities of daily living such as squatting to use Eastern-style toilets, and for kneeling during praying, sitting, and dining. Inability to perform these activities because of limited knee flexion would cause these groups of people to deviate from their cultural norms [28, 39].
In response to certain populations’ demands for deep knee flexion, orthopaedic implant manufacturers developed high-flexion total knee prostheses [1, 62]. These devices are designed to allow as much as 155° knee flexion without edge loading of the polyethylene posteriorly [31]. Although long-term clinical studies of these implants are limited, one device (Hy-Flex II; DePuy International, Inc, Leeds, UK) reportedly provides 72% of patients with peak passive knee flexion greater than 120° [62]. Another study reported increased average postoperative motion in the patients who received high-flexion prostheses (138° for NexGen® LPS-Flex versus 126° for NexGen® LPS; Zimmer, Inc, Warsaw, IN) at a minimum followup of 2 years [23]. A third study reported no difference in average postoperative knee flexion in 50 patients who underwent bilateral TKAs (138° for NexGen® LPS-Flex versus 135° for NexGen® LPS) [26]. To date, three of nine clinical studies suggest patients have increased postoperative flexion with high-flexion prostheses [6, 19, 20, 23, 26, 38, 42, 44, 45]. One of these studies reported patients with maximum flexion greater than 135° had a better functional WOMAC Osteoarthritis Index score than patients with maximum flexion of 135° or less (17.5 versus 14.3) [45].
Despite the potential benefits of safely accommodating deep knee flexion, there are theoretical problems associated with high-flexion designs. The first issue stems from the smaller radii of curvature found in some of the high-flexion prostheses. This change was made to increase the contact area between the posterior condyles and the tibial insert in deep flexion. However, if the contact area is not adequate, the end result may be increased polyethylene wear attributable to high contact stresses in terminal flexion [9, 41]. Also, the smaller radii of curvature require resection of an additional 2 to 4 mm of bone from the posterior condyles. In posterior-stabilized designs, additional bone also is taken from the intercondylar area to accommodate the increased box height. Resection of additional bone in these regions may lead to an increase in the complexity of revisions [47]. Second, the extremes of knee flexion are likely to produce high stresses in the patellofemoral joint. These high stresses may lead to pain, increased wear, fracture, and increased patellar loosening. One study of high-flexion TKAs reported a 38% rate of aseptic loosening at 32 months followup [20]. What is not known currently is how often patients will use, during daily activities, any additional safe flexion provided by the high-flexion TKA.
Traditionally, different methods to assess knee function are commonly used in the clinical setting. The first method relies on validated knee-scoring questionnaires such as the Knee Society Clinical Rating System and the WOMAC Osteoarthritis Index [4, 25]. The second method relies on biomechanical gait analysis. Knee-scoring questionnaires, although useful for determining overall patient outcomes, generally provide little objective data regarding use of the knee to perform functional activities. Analysis in a gait laboratory can provide detailed information regarding knee kinetics and loading for small samples of subjects performing one of several functional activities in limited, well-defined circumstances. However, the laboratory requires trained personnel and is time-consuming and costly. A third method, flexible electrogoniometry, was introduced as a promising outcome measure that evaluates functional range of motion of the knee in the clinical setting [40, 50]. One study of patients evaluated with flexible electrogoniometry before and after TKA concluded this cohort of patients failed to exploit the range of knee motion available to them while performing activities of daily living [40].
The Intelligent Device for Energy Expenditure and Activity system (IDEEA®; MiniSun, LLC, Fresno, CA) is a microcomputer-based portable physical activity measurement device that allows for detection of multiple physical activities (standing, sitting, walking, stepping, running, jumping, lying, reclining, transitions, ascending stairs, descending stairs, etc). The device can analyze gait, speed, distance, power, work, and energy expenditure. Investigations into the IDEEA® system’s accuracy show it is accurate for measuring energy expenditure, postures and limb movements, and speed of walking and running [58, 59, 64, 65]. The original IDEEA® system was modified for this experiment by adding two electrogoniometers. The modified IDEEA® system’s accuracy in detecting knee angles and activities was validated before starting this project [24]. Although knee flexion greater than 90° is important to patients who have had TKAs, we do not know how often patients actually flex their knee beyond 90° outside the gait laboratory.
In patients who received a high-flexion TKA, we documented (1) the frequency of knee flexion greater than 90° and (2) the activities performed while they flexed their knee greater than 90°. We presumed these patients would not use the maximum passive postoperative flexion available to them. We also examined the relationship between Knee Society scores and body mass index, age, and steps taken.
Materials and Methods
We recruited 20 patients (21 knees) who underwent elective TKA (10 cruciate-retaining and 11 posterior-stabilized) for varus osteoarthritis and then studied their ranges of motion with the modified IDEEA® system at a mean ± standard deviation of 27 ± 34 months (range, 24–29 months) after their surgery. Seven of the 20 patients had contralateral TKAs or unicompartmental knee arthroplasties performed with nonhigh-flexion total knee prostheses at a minimum of 2 years before having high-flexion TKA. At the time of testing, all prostheses were functioning well. None of the patients had any severe visual impairment, dementia, neurologic conditions, or abnormalities of the feet, ankles, contralateral knee, hips, or spine that caused substantial limitation or pain. The 21 surgically treated knees had varus deformities ranging from 1° to 9°. The 13 men and seven women had a mean age of 66 ± 10 years (range, 48–79 years). Their mean body mass index (BMI) was 31 ± 6 kg/m2 (range, 24–45 kg/m2).
All clinical and radiographic examinations, including calculation of Knee Society scores, were performed by one orthopaedic surgeon (JIH) who was not involved in the index procedure [25]. Preoperative Knee society scores were obtained by the attending surgeon before the index procedure. Each patient wore the modified IDEEA® device continuously for an average of 35 hours 40 minutes ± 30 minutes. The mean preoperative passive knee flexion contracture was 5° ± 4° (range, 0°–10°), and mean preoperative passive knee flexion was 113° ± 13°. The mean maximum postoperative passive knee flexion was 125° ± 12°. Fourteen knees had passive flexion greater than 120°. Our institutional review board approved the study and all patients provided written, informed consent.
All patients kept a log of their activities (Appendix 1). Fifteen patients listed their current occupation as retired or homemaker, and reported such activities as house cleaning, boat cleaning, riding a stationary bike, golf, and using a stepping machine. Three patients wore the device while at work. These three patients listed their occupations as administrative assistant, clinic-based medical assistant, and professor of political science.
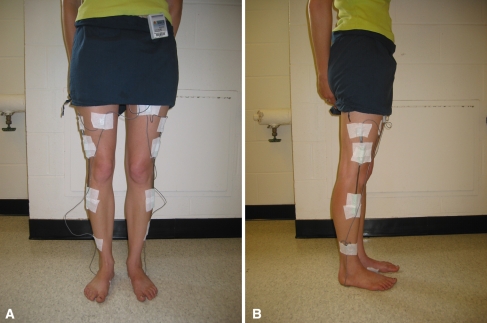
The IDEEA® system identifies 47 human physical activities based on limb movements, postures, transitions, and gaits; it quantifies these physical activities by type, duration, intensity, and expended energy. The mean and standard deviation for 18 measured parameters are calculated for the right foot, left foot, and both feet. The device includes five sensors (each 16 × 14 × 4 mm) (Figs. 1, 2). The sensors measure angles and acceleration of body segments in two orthogonal directions. One sensor was placed in the midline approximately 2 cm distal to the sternal notch, one was placed on the plantar aspect of each foot, proximal to the metatarsal heads, and one was placed on the anterior surface of each thigh at the mid-femur level. Hypoallergenic adhesive tape was used to secure the sensors to the skin. Output signals travel via 2-mm cables to a 33-MHz, 32-bit ARM microprocessor (ARM, Cambridge, UK) housed in a 7 × 5.4 × 1.7 cm plastic box. The box weighs 59 g and is worn on one’s belt. Flash memory allows recording of the data during activities of daily living without loss of data even if an unexpected power failure occurs. The device operates using one AA alkaline battery and consumes approximately 0.045 W during operation.
Fig. 1.
A photograph shows the modified IDEAA® device.
Fig. 2A–B.
The photographs show a subject with the modified IDEEA® device in place from (A) the front and (B) the side.
At our request, knee electrogoniometers (Penny + Giles™; Biometrics Ltd, Gwent, UK) were added to the system by MiniSun. The electrogoniometers measure knee flexion angles and were calibrated by MiniSun. One electrogoniometer was placed on the lateral surface of each knee, in line with the anatomic axes of the femur and tibia, and fixed to the skin with hypoallergenic tape with the knee in 0° extension (as measured by a conventional goniometer). Data collected are downloaded to a personal computer via a USB connection and a software interface (provided by MiniSun; the software also interprets the sensor output and determines activity type and other variables). With the addition of the electrogoniometers, the IDEEA® system can operate continuously for up to 48 hours and can store more than 60 million data points at 32 Hz. The output of the IDEEA® software gives the knee flexion angles and, simultaneously, identifies 47 different types of activities (walking, sitting, standing, running, stair climbing, reclining, transitions, etc) in charts, tables, and movielike animation. For a specific interval, as short as 1/32 of a second, it calculates the percentage of time each different physical activity was performed.
An experienced member of the research team applied the device to each patient; another team member confirmed proper placement. Before collecting data, the device was calibrated with the patient sitting in a chair with the ankles in neutral dorsiflexion and the knees and hips at 90° flexion, as per the manufacturer’s protocol. The proper electrogoniometer position also was confirmed by a conventional goniometer. Patients then were asked to walk around the laboratory to become acquainted with wearing the device. A detailed set of instructions regarding care of the device was read to each patient before their departure. The patients were asked to wear the device continuously for up to 48 hours. The only limitation of activity was that they were not allowed to get the device wet (thus eliminating the opportunity for a bath or shower). They were permitted to exercise. Patients were instructed to regularly check the position of the sensors and electrogoniometers. None of the patients reported any movement of the device during their testing periods. We encouraged the patients to proceed with their routine daily schedule. At the conclusion of their session, each patient removed the battery from the device and mailed the device back to the laboratory with the provided shipping materials.
Data were uploaded to a personal computer after testing each patient. A two-tailed Student’s t test, assuming unequal variances, was used to compare means of maximum passive postoperative knee flexion used for nonhigh-flexion versus high-flexion TKAs, and for cruciate-retaining versus posterior-stabilized TKAs. We used linear regression analyses to evaluate the relationships between Knee Society scores and BMI, age, and number of steps taken. Data analysis was performed with Microsoft® Excel® (Microsoft Corporation, Redmond, WA) and MATLAB® (MathWorks, Natick, MA).
Results
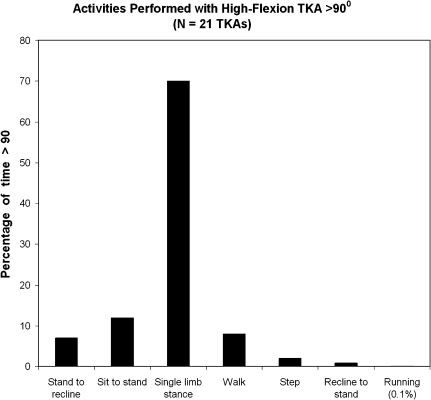
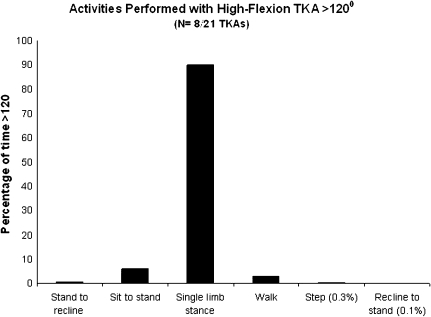
The 20 patients flexed their 21 knees with high-flexion TKAs greater than 90° for an average of 10 ± 3.8 minutes, or 0.5% of their average total data collection time. The activities performed while the patients flexed their knees greater than 90° were, on average, single-limb stance (70%), sitting/moving from sitting to standing (12%), walking (8%), moving from standing to reclining (7%), stepping (2%), moving from lying to standing (0.9%), and running (0.1%) (Figs. 3, 4). Eight knees with high-flexion TKAs were flexed greater than 120° for an average of 2.2 minutes (range, 0.2–15 minutes), or 0.1% of their average total data collection time. Thirteen knees with high-flexion TKAs were never flexed greater than 120°. Activities performed with flexion greater than 120° were, on average, 90% in single-limb stance, 6% sitting/moving from sitting to standing, 3% walking, 0.6% moving from standing to reclining, 0.3% stepping, and 0.1% moving from lying to standing (Fig. 5).
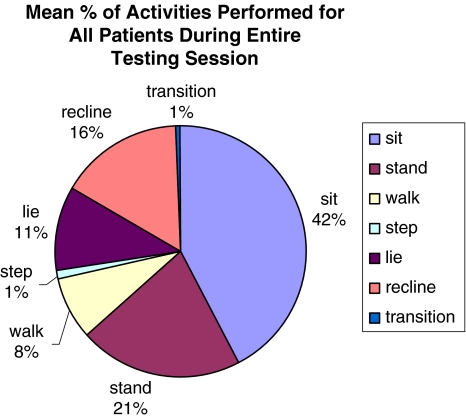
Fig. 3.
This graph illustrates the mean percentage of time all patients spent performing various activities during their entire data collection period.
Fig. 4.
Twenty patients flexed their 21 high-flexion knees greater than 90° for an average of 10 ± 3.8 minutes over the total data collection period. The most performed activity was single-limb stance (70%).
Fig. 5.
Eight knees flexed greater than 120° during data collection for an average of 2.2 minutes (range, 0.2–15 minutes). The most performed activity was single-limb stance (90%).
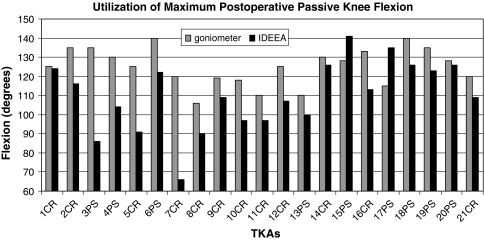
Peak flexion used at any time during the data collection period for the 21 knees with high-flexion TKAs was, on average, 84% ± 11% (range, 64%–100%) of their maximum passive postoperative flexion. There was no difference (p = 0.09) in the use of maximum passive postoperative flexion between the 11 high-flex posterior-stabilized TKAs (91% ± 15%) and the 10 high-flex cruciate-retaining TKAs (86% ± 8%) (Fig. 6).
Fig. 6.
Peak flexion used at any time during testing for the 21 high-flexion knees was, on average, 84% ± 11% (range, 64%–100%) of their maximum passive postoperative flexion. There was no difference (p = 0.09) in the use of maximum passive postoperative flexion between the 11 high-flex posterior-stabilized (PS) knees (91% ± 15%) and the 10 high-flex cruciate-retaining (CR) knees (86% ± 8%).
The average number of steps taken during the entire data collection period for the 20 patients was 12,125 ± 7607 steps. This translates to an estimated 1.2 million cycles per year. On average, the 20 patients walked 8.1 ± 4.7 km during the data collection period.
For the high-flexion TKAs, the average preoperative Knee Society knee and function scores were 37 ± 12 (range, 11–61) and 52 ± 15 (range, 25–82), respectively. The average postoperative Knee Society knee and function scores for the high-flexion TKAs were 88 ± 9 (range, 68–94) and 90 ± 9 (range, 65–96). Postoperatively, all patients had full extension and mean postoperative passive flexion was 125° ± 12°. We found no correlation (r2 < 0.2) between Knee Society scores and BMI, steps taken, or age. There was no correlation (r2 < 0.2) between steps and BMI or age.
Discussion
Although high-flexion TKA designs aim to safely accommodate deep flexion, it is unknown how often patients use deep flexion outside the laboratory. In patients who received a high-flexion TKA, we therefore documented (1) the frequency of knee flexion greater than 90° and (2) the activities performed while they flexed their knee greater than 90°.
In interpreting our results, one must remember the 20 patients in our study, in general, may not routinely use high flexion to perform their daily activities. We may have seen an increase in the time spent using deep knee flexion had the patients used the device on the weekends (during recreational activities such as golfing), if they had been permitted to bathe with the device in place (getting in and out of a bathtub), or if their employment required deep knee flexion (eg, mechanics, plumbers, or electricians). As such, our findings should not be generalized to other patient populations. Another potential limitation of this study is that the electrogoniometers were placed directly on the skin. In the past, human knee motion has been evaluated by in vitro (cadavers [15, 18, 22, 32, 35] and gait laboratories [2, 3, 29]) and in vivo (roentgen stereophotogrammetry and fluoroscopy[8, 10, 11, 13, 27, 55, 56]) approaches. One report that evaluated the effect of skin motion on the analysis of joint motion during running concluded knee motions other than flexion/extension (abduction/adduction and rotation) may be affected by substantial errors when using skin markers [48]. In that study, the average error relative to the range of motion was 21% for flexion and extension. Contrary to the findings of that investigation, we found a high degree of correlation (r2 = 0.97) for knee angles between the electrogoniometers used with the modified IDEEA® system and the data generated in our gait laboratory using a four-camera Selspot II® optoelectric light-emitting diode tracking system (Selective Electronics, Partille, Sweden) and two side-by-side Kistler® piezoelectric force platforms (Kistler Instruments, Winterthur, Switzerland) [24]. We therefore do not believe placement of the electrogoniometers directly on the skin affected our findings. Another limitation of the IDEEA® system is that it does not report which activities typically require weightbearing. Knowledge of weightbearing activities is important with regard to polyethylene insert wear and damage. A key question concerning the design of high-flexion total knee prostheses is how often patients will load their knee in flexion beyond 120°, as the deleterious effects from lift-off of the polyethylene insert at knee flexion angles greater than 120° have been documented [5, 12, 54]. Future versions of the IDEEA® system will be able to address this topic.
The average number of steps taken per day by the patients in our study (6078 ± 3806) represents a 22% increase over averages reported previously (4988 steps per day in 111 patients) [36, 52, 53, 63]. Although this increase is substantial, it does fall within the wide range of activity (395–17,718 steps per day) that has been described in the same studies. Sampling error from our small study group may contribute to this discrepancy. Also, the fact that seven of the 20 patients in our study had bilateral TKAs may have enabled them to be more active, as knee osteoarthritis is frequently bilateral.
At knee flexion greater than 90°, single-limb stance (variations of standing) was the most common activity performed by our patients. This begs the question: who needs more than 90° knee flexion to stand and walk? This can be explained by the fact that the IDEEA® system groups six different activities under the category “single-limb stance.” These six different activities include standing with weight supported (eg, foot forward on a bar), standing on the right foot with left leg moving, standing on the left foot with right leg moving, standing while supporting additional weight, standing with left hip abducted/adducted, and standing with right hip abducted/adducted. As defined by the IDEEA® system, a single-limb stance event typically occurs when all weight is supported on one limb with the knee extended and the other knee is flexed in one of the positions listed above. One thus can appreciate that knee flexion greater than 90° may be needed for single-limb stance when performing an activity such as tying one’s shoelaces, as this may require knee flexion to raise the foot onto a bench or a desktop. We also documented in the gait laboratory that knee flexion greater than 90° is used during walking when a subject picks an object off the floor without stopping completely to do so [24].
These patients with high-flexion TKA prostheses only infrequently used the maximum passive postoperative flexion available to them and spent only a small percentage of their testing time with their knees flexed beyond 90°. We were not surprised to find the patients did not fully use the available range of knee motion. The common gait adaptations seen in patients with hip and knee osteoarthritis (increased duration of swing phase, decreased step length, and decreased walking cadence), and the changes in the soft tissue envelope seen in osteoarthritis, may be difficult to overcome, even after the potential increased range of motion provided by TKA.
Although these 20 patients did not spend a high percentage of their data collection time using deep knee flexion, the small amount of time they spent using deep knee flexion is important. Patients who desire deep knee flexion for recreational and cultural reasons will be dissatisfied with their outcome if they are unable to perform these activities after TKA. Thus, it remains an attractive goal to provide patients with the opportunity to use deep knee flexion without risking damage to their prostheses, and there now are data supporting a positive correlation between flexion greater than 135° and function [45]. Given the theoretical problems associated with high-flexion designs discussed previously, surgeons may consider using high-flexion designs only in patients who have substantial knee flexion preoperatively.
Twenty patients flexed their 21 knees with high-flexion TKAs greater than 90° for an average of 0.5% of their data collection time. Eight of the 21 surgically treated knees were flexed greater than 120° for an average of 0.1% of their data collection time. Single-limb stance, sitting, and moving from sitting to standing were the most common activities performed during knee flexion greater than 90°. Peak flexion used by the 21 knees with high-flexion TKAs at any time during the testing averaged 84% of the maximum passive postoperative flexion available. Given the small amount of time spent using deep knee flexion by these patients and the theoretical concerns with the modifications present in the current high-flexion designs, surgeons may choose to use high-flexion designs only in patients who have a high degree of knee flexion preoperatively. Finally, longer followup of these patients is needed to determine if the design concerns become evident clinically.
Acknowledgments
We thank Harry E. Rubash, MD, and William H. Harris MD, DSc, for invaluable guidance and support in all aspects of this project. We also thank Aimee Mulkern, NP, for assistance in generating the data.
Appendix
Appendix 1.
Typical activity log kept by a patient
| Time | Predominant activity | Predominant posture(s) |
|---|---|---|
| 0800 | Driving, walking | Sitting, standing |
| 0900 | Working at desk | Sitting |
| 1000 | Working at desk | Sitting |
| 1100 | Working at desk | Sitting |
| 1200 | Eating/working at desk | Sitting |
| 1300 | Gym (step machine) | |
| 1400 | Gym (treadmill) | |
| 1500 | Working at desk | Sitting |
| 1600 | Cleaning boat | Standing, squatting |
| 1700 | Cleaning boat | Sitting, kneeling |
| 1800 | Cooking | Standing |
| 1900 | Eating | Sitting |
| 2000 | Cleaning | Standing |
| 2100 | Watching TV | Sitting |
| 2200 | Watching TV | Reclining |
| 2300 | Reading | Reclining |
| 2400 | Sleeping | Reclining |
| 0100 | Sleeping | Reclining |
| 0200 | Sleeping | Reclining |
| 0300 | Sleeping | Reclining |
| 0400 | Sleeping | Reclining |
| 0500 | Sleeping | Reclining |
| 0600 | Sleeping | Reclining |
| 0700 | Taking shower, dressing | Standing |
Footnotes
Dr. Freiberg has received consulting fees and royalties from Biomet Inc, Warsaw, IN, and Zimmer, Inc, Warsaw, IN. Dr. Malchau has received institutional research support from Zimmer.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Harris Orthopaedic Biomechanics and Biomaterials Laboratory and Stanford University Medical Center.
References
- 1.Akagi M, Nakamura T, Matsusue Y, Ueo T, Nishijyo K, Ohnishi E. The Bisurface total knee replacement: a unique design for flexion. Four-to-nine-year follow-up study. J Bone Joint Surg Am. 2000;82:1626–1633. [DOI] [PubMed]
- 2.Andriacchi TP. Functional analysis of pre and post-knee surgery: total knee arthroplasty and ACL reconstruction. J Biomech Eng. 1993;115:575–581. [DOI] [PubMed]
- 3.Andriacchi TP, Stanwyck TS, Galante JO. Knee biomechanics and total knee replacement. J Arthroplasty. 1986;1:211–219. [DOI] [PubMed]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed]
- 5.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty: influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. [DOI] [PubMed]
- 6.Bin SI, Nam TS. Early results of high-flex total knee arthroplasty: comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–355. [DOI] [PubMed]
- 7.Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756–759. [PubMed]
- 8.Chao EY. Justification of triaxial goniometer for the measurement of joint rotation. J Biomech. 1980;13:989–1006. [DOI] [PubMed]
- 9.Dahlkvist NJ, Mayo P, Seedhom BB. Forces during squatting and rising from a deep squat. Eng Med. 1982;11:69–76. [DOI] [PubMed]
- 10.Dennis DA, Komistek RD, Colwell CE Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res. 1998;356:47–57. [DOI] [PubMed]
- 11.Dennis DA, Komistek RD, Hoff WA, Gabriel SM. In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res. 1996;331:107–117. [DOI] [PubMed]
- 12.Dennis DA, Komistek RD, Mahfouz MR. In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res. 2003;410:114–130. [DOI] [PubMed]
- 13.Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38:241–253. [DOI] [PubMed]
- 14.Duffy GP, Trousdale RT, Stuart MJ. Total knee arthroplasty in patients 55 years old or younger: 10- to 17-year results. Clin Orthop Relat Res. 1998;356:22–27. [DOI] [PubMed]
- 15.Fukubayashi T, Torzilli PA, Sherman MF, Warren RF. An in vitro biomechanical evaluation of anterior-posterior motion of the knee: tibial displacement, rotation, and torque. J Bone Joint Surg Am. 1982;64:258–264. [PubMed]
- 16.Gill GS, Joshi AB. Long-term results of cemented, posterior cruciate ligament-retaining total knee arthroplasty in osteoarthritis. Am J Knee Surg. 2000;14:209–214. [PubMed]
- 17.Gill GS, Joshi AB. Long-term results of retention of the posterior cruciate ligament in total knee replacement in rheumatoid arthritis. J Bone Joint Surg Br. 2001;83:510–512. [DOI] [PubMed]
- 18.Goldberg VM, Henderson BT. The Freeman-Swanson ICLH total knee arthroplasty: complications and problems. J Bone Joint Surg Am. 1980;62:1338–1344. [PubMed]
- 19.Gupta SK, Ranawat AS, Shah V, Zikria BA, Zikria JF, Ranawat CS. The P.F.C. sigma RP-F TKA designed for improved performance: a matched-pair study. Orthopedics. 2006;29(9 suppl):S49-S52. [PubMed]
- 20.Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br. 2007;89:1457–1461. [DOI] [PubMed]
- 21.Hefzy MS, Kelly BP, Cooke TD. Kinematics of the knee joint in deep flexion: a radiographic assessment. Med Eng Phys. 1998;20:302–307. [DOI] [PubMed]
- 22.Hsieh HH, Walker PS. Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am. 1976;58:87–93. [PubMed]
- 23.Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty: a minimum of 2 years of follow-up. J Arthroplasty. 2005;20:674–679. [DOI] [PubMed]
- 24.Huddleston JI, Al Aiti A, Goldvasser D, Scarborough DM, Freiberg AA, Rubash HE, Malchau H, Harris WH, Krebs DE. Ambulatory measurement of knee motion and physical activity: preliminary evaluation of a smart activity monitor. J Neuroeng Rehabil. 2006;3:21. [DOI] [PMC free article] [PubMed]
- 25.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 26.Kim YH, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses: a prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470–1475. [DOI] [PubMed]
- 27.Komistek RD, Dennis DA, Mahfouz M. In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res. 2003;410:69–81. [DOI] [PubMed]
- 28.Koshino T, Saito T, Orito K, Mitsuhashi S, Takeuchi R, Kurosaka T. Increase in range of knee motion to obtain floor sitting after high tibial osteotomy for osteoarthritis. Knee. 2002;9:189–196. [DOI] [PubMed]
- 29.Lafortune MA, Cavanagh PR, Sommer HJ 3rd, Kalenak A. Three-dimensional kinematics of the human knee during walking. J Biomech. 1992;25:347–357. [DOI] [PubMed]
- 30.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52:34–43. [DOI] [PubMed]
- 31.Li G, Most E, Sultan PG, Schule S, Zayontz S, Park SE, Rubash HE. Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: an in vitro robotic experimental investigation. J Bone Joint Surg Am. 2004;86:1721–1729. [DOI] [PubMed]
- 32.Mahoney OM, Noble PC, Rhoads DD, Alexander JW, Tullos HS. Posterior cruciate function following total knee arthroplasty: a biomechanical study. J Arthroplasty. 1994;9:569–578. [DOI] [PubMed]
- 33.Mallon WJ, Callaghan JJ. Total knee arthroplasty in active golfers. J Arthroplasty. 1993;8:299–306. [DOI] [PubMed]
- 34.Maloney WJ, Schurman DJ. The effects of implant design on range of motion after total knee arthroplasty: total condylar versus posterior stabilized total condylar designs. Clin Orthop Relat Res. 1992;278:147–152. [PubMed]
- 35.Markolf KL, Finerman GM, Amstutz HC. In vitro measurements of knee stability after bicondylar replacement. J Bone Joint Surg Am. 1979;61:547–557. [PubMed]
- 36.McClung CD, Zahiri CA, Higa JK, Amstutz HC, Schmalzried TP. Relationship between body mass index and activity in hip or knee arthroplasty patients. J Orthop Res. 2000;18:35–39. [DOI] [PubMed]
- 37.Meding JB, Keating EM. Overview: long-term followup: predicting the success of a total knee arthroplasty. Clin Orthop Relat Res. 2001;388:7–9. [DOI] [PubMed]
- 38.Minoda Y, Aihara M, Sakawa A, Fukuoka S, Hayakawa K, Ohzono K. Range of motion of standard and high-flexion cruciate retaining total knee prostheses. J Arthroplasty. 2008 Jun 3. [Epub ahead of print]. [DOI] [PubMed]
- 39.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191–198. [DOI] [PubMed]
- 40.Myles CM, Rowe PJ, Walker CR, Nutton RW. Knee joint functional range of movement prior to and following total knee arthroplasty measured using flexible electrogoniometry. Gait Posture. 2002;16:46–54. [DOI] [PubMed]
- 41.Nagura T, Dyrby CO, Alexander EJ, Andriacchi TP. Mechanical loads at the knee joint during deep flexion. J Orthop Res. 2002;20:881–886. [DOI] [PubMed]
- 42.Ng FY, Wong HL, Yau WP, Chiu KY, Tang WM. Comparison of range of motion after standard and high-flexion posterior stabilised total knee replacement. Int Orthop. 2008;32:795–798. [DOI] [PMC free article] [PubMed]
- 43.Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165. [DOI] [PubMed]
- 44.Nutton RW, van der Linden ML, Rowe PJ, Gaston P, Wade FA. A prospective randomised double-blind study of functional outcome and range of flexion following total knee replacement with the NexGen standard and high flexion components. J Bone Joint Surg Br. 2008;90:37–42. [DOI] [PubMed]
- 45.Park KK, Chang CB, Kang YG, Seong SC, Kim TK. Correlation of maximum flexion with clinical outcome after total knee replacement in Asian patients. J Bone Joint Surg Br. 2007;89:604–608. [DOI] [PubMed]
- 46.Pavone V, Boettner F, Fickert S, Sculco TP. Total condylar knee arthroplasty: a long-term followup. Clin Orthop Relat Res. 2001;388:18–25. [DOI] [PubMed]
- 47.Ranawat CS. Design may be counterproductive for optimizing flexion after TKR. Clin Orthop Relat Res. 2003;416:174–176. [DOI] [PubMed]
- 48.Reinschmidt C, van den Bogert AJ, Nigg BM, Lundberg A, Murphy N. Effect of skin movement on the analysis of skeletal knee joint motion during running. J Biomech. 1997;30:729–732. [DOI] [PubMed]
- 49.Roaas A, Andersson GB. Normal range of motion of the hip, knee and ankle joints in male subjects, 30–40 years of age. Acta Orthop Scand. 1982;53:205–208. [DOI] [PubMed]
- 50.Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture. 2000;12:143–155. [DOI] [PubMed]
- 51.Schai PA, Thornhill TS, Scott RD. Total knee arthroplasty with the PFC system: results at a minimum of ten years and survivorship analysis. J Bone Joint Surg Br. 1998;80:850–858. [DOI] [PubMed]
- 52.Schmalzried TP, Szuszczewicz ES, Northfield MR, Akizuki KH, Frankel RE, Belcher G, Amstutz HC. Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am. 1998;80:54–59. [DOI] [PubMed]
- 53.Shepherd EF, Toloza E, McClung CD, Schmalzried TP. Step activity monitor: increased accuracy in quantifying ambulatory activity. J Orthop Res. 1999;17:703–708. [DOI] [PubMed]
- 54.Stiehl JB, Dennis DA, Komistek RD, Crane HS. In vivo determination of condylar lift-off and screw-home in a mobile-bearing total knee arthroplasty. J Arthroplasty. 1999;14:293–299. [DOI] [PubMed]
- 55.Stiehl JB, Dennis DA, Komistek RD, Keblish PA. In vivo kinematic analysis of a mobile bearing total knee prosthesis. Clin Orthop Relat Res. 1997;345:60–66. [DOI] [PubMed]
- 56.Stiehl JB, Komistek RD, Dennis DA, Paxson RD, Hoff WA. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br. 1995;77:884–889. [PubMed]
- 57.Sultan PG, Most E, Schule S, Li G, Rubash HE. Optimizing flexion after total knee arthroplasty: advances in prosthetic design. Clin Orthop Relat Res. 2003;416:167–173. [DOI] [PubMed]
- 58.Sun M, Hill JO. A method for measuring mechanical work and work efficiency during human activities. J Biomech. 1993;26:229–241. [DOI] [PubMed]
- 59.Sun M, Reed GW, Hill JO. Modification of a whole room indirect calorimeter for measurement of rapid changes in energy expenditure. J Appl Physiol. 1994;76:2686–2691. [DOI] [PubMed]
- 60.Trousdale RT, Thornhill TS, Engh GA, Gustke KA, Ranawat CS, Whiteside LA. Case challenges in knee surgery: what would you do? Orthopedics. 2002;25:987–988. [DOI] [PubMed]
- 61.Weiss JM, Noble PC, Conditt MA, Kohl HW, Roberts S, Cook KF, Gordon MJ, Mathis KB. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;404:172–188. [DOI] [PubMed]
- 62.Yamazaki J, Ishigami S, Nagashima M, Yoshino S. Hy-Flex II total knee system and range of motion. Arch Orthop Trauma Surg. 2002;122:156–160. [DOI] [PubMed]
- 63.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. [DOI] [PubMed]
- 64.Zhang K, Pi-Sunyer FX, Boozer CN. Improving energy expenditure estimation for physical activity. Med Sci Sports Exerc. 2004;36:883–889. [DOI] [PubMed]
- 65.Zhang K, Werner P, Sun M, Pi-Sunyer FX, Boozer CN. Measurement of human daily physical activity. Obes Res. 2003;11:33–40. [DOI] [PubMed]