Abstract
In situ gel-forming systems have drawn much attention of current researchers to overcome the poor bioavailability from the conventional eye drops. The present work described formulation and pharmacoscintigraphic evaluation of timolol-maleate-loaded chitosan/hydroxy propyl methyl cellulose (HPMC)-based polymer matrix for enhanced ocular retention. Chitosan and HPMC ratio was optimized and formulation was characterized for various in vitro parameters. The ocular retention was studied on New Zealand rabbits by gamma scintigraphy, which is a very simple and noninvasive technique. For scintigraphy study, the drug timolol maleate was radiolabeled 99mTc by direct labeling method using SnCl2·2H2O as reducing agent. The labeling procedure was optimized to get maximum labeling efficiency (>98%). In vitro stability of the radiolabeled drug (99mTc-timolol maleate complex) was checked and it was found to be stable for up to 24 h. Plain drug eliminates rapidly as significant activity was recorded in kidney and bladder after 2 h of ocular administration. It was evident from the scintigraphic images and the time–activity curve plotted from the data that the plain drug solution cleared very rapidly from the corneal region and reached into systemic circulation via nasolachrymal drainage system, as significant activity was recorded in kidney and bladder after 2 h of ocular administration. Developed formulation cleared at a slow rate and remained at corneal surface for longer time duration. No radioactivity was observed in systemic circulation after 2 h. Ocular irritation of the developed formulation was also checked by hen’s egg chorioallantoic membrane test and formulation was found to be practically nonirritant. The study signified the potential of gamma scintigraphy in evaluation of novel drug delivery systems in a noninvasive manner.
Key words: chitosan, gamma scintigraphy, in situ gel, radiolabeling, 99mTc, timolol maleate
INTRODUCTION
Drug delivery in ocular therapeutics is a challenging problem. Various ocular diseases like glaucoma, conjunctivitis, dry eye syndrome, etc. require frequent drug administration. The major problem encountered in drug delivery to eyes is the attainment of an optimum drug concentration at the site of action. Poor bioavailability of drugs from conventional eye drops is mainly due to the precorneal loss factors which include rapid tear turnover, nonproductive absorption, transient residence time in the cul-de-sac, and the relative impermeability of the drugs to corneal epithelial membrane. Sometimes, systemic absorption of the drug drained through the nasolachrymal duct may result in some undesirable side effects (1–3).
Due to these physiological and anatomical constraints, only a small fraction of the administered dose (<1%) is ocularly absorbed. This forces the clinician to recommend a frequent dosing at an extremely high concentration and pulse-type dosing results in several side effects of ophthalmic products. Novel ocular drug delivery systems offer some improvement over a conventional liquid dosage form but, because of blurred vision (e.g., ointments) (4,5) or lack of patient compliance (e.g., inserts), they have not been universally accepted (6,7). These problems may be overcome by the use of in situ gel-forming systems that are instilled as drops into the eye and undergo a sol-gel transition in the cul-de-sac. Different types of in situ gel-forming systems based on different mechanisms (temperature, pH, or ion activated) using different polymers have been explored for sustained ocular drug delivery as reviewed by Nanjawade et al. (8).Chitosan- and pluronic-F-127-based pH and temperature-triggered in situ gel for sustained ocular drug delivery have been reported by our group (9).
Present study employed combination of chitosan and hydroxyl propyl methyl cellulose (HPMC) for the development of sustained ocular drug delivery system. Chitosan is reported to act as penetration enhancer that increases transcorneal permeation of the drug. Besides this, other properties of chitosan like bioadhesiveness, viscous nature, and ability to convert into hydrogel at ocular pH make it the best suitable candidate for the development of such type of delivery systems. However, chitosan at higher concentration does not give clear solution and upon instillation into the eye, it forms hydrogel (white precipitate) due to precipitation of the polymer at pH 7–7.0 that can hamper the vision. Further, due its cationic nature, the polymer can cause ocular irritation. So we tried to reduce the concentration of chitosan by the addition of HPMC, a viscosifying polymer.
In the present study, the drug timolol maleate was radiolabeled with radioactive technetium (sodium pertechnetate; 99mTcO4−) and incorporated into the chitosan/HPMC-based developed polymeric system and precorneal retention and lacrimal clearance were studied by gamma scintigraphy, which is a noninvasive technique and is a powerful tool in the evaluation of new drugs/delivery systems and provides an insight into the in vivo fate of the delivery system (10).
MATERIALS AND METHODS
The drug timolol maleate was received as gift sample from M/s Ven Petrochem & Pharma (India) Pvt. Ltd., Mumbai, India. Chitosan (practical grade, 75–85% deacetylated, molecular weight 150 kDa) was obtained as kind gift from M/s, India Sea Foods, Cochin, India. HPMC K 100 and all other chemicals and solvents used were purchased from local suppliers and of analytical grade unless mentioned.
Labeling of Timolol Maleate with 99mTc
The timolol maleate was labeled with radioactive nuclide 99mTc which was obtained as sodium pertechnetate in normal saline eluted from molybdenum generator. It was procured from the regional center of the Board of Radiation and Isotopes Technology, INMAS, Delhi, India. For labeling, a 2.5 mg of the drug was dissolved in normal saline and mixed with stannous chloride (SnCl2 1 mg/ml in 10% acetic acid). The pH of the solution was adjusted by NaHCO3. To this, 99mTc (2–3 mci) was added and mixed properly. All the labeling operation was carried out in hot laboratory under lead shielding. Ultraviolet spectroscopy of 99mTc-labeled timolol maleate was taken to check any shift/changes from original molecule.
Determination of Labeling Efficiency
Labeling efficiency was checked using instant thin-layer chromatography (ITLC). A drop of the formulation was applied onto ITLC silica-gel-coated strips, which was run in 100% acetone as mobile phase. While reduced/hydrolyzed 99mTc (colloids) were estimated using pyridine–acetic acid–water (PAW = 3:5:1.5 v/v) as mobile phase. The strips were dried and cut into two equal halves and radioactivity was counted in each half using well-type gamma counter (CAPRAC-R, Capintec, USA). Labeling efficiency was calculated from the following formulae:
 |
Where: T = counts at top, B = counts at bottom
Optimization of Labeling Conditions (pH, SnCl2 Concentration)
Labeling efficiency of the drug molecules depends on amount of reducing agent (SnCl2 concentration) and the pH of the solution. Hence, to achieve maximum labeling efficiency, the two process variables were optimized. Labeling operation was carried out using different concentration of SnCl2 while keeping the pH constant. Labelling efficiency was determined as described previously (Table I). In another set of experiments, the amount of stannous chloride was kept constant and the pH of the solution was varied from 5 to 7.5 by adding 0.5-M NaHCO3 solution. The labeling efficiency at different pH was determined and optimum pH was selected (Table II).
Table I.
Effect of SnCl2 Concentration on Labeling Efficiency of Timolol Maleate
| Amount of SnCl2 (μg) | Percent of labeling efficiency | Percent of free Tc | Percent of colloids |
|---|---|---|---|
| 25 | 73.2 ± 0.4 | 26.1 ± 0.3 | 0.7 ± 0.2 |
| 50 | 84.5 ± 0.3 | 14.6 ± 0.13 | 0.9 ± 0.4 |
| 100 | 98.2 ± 0.2 | 0.7 ± 0.1 | 1.1 ± 0.1 |
| 200 | 87.8 ± 0.4 | 3.9 ± 0.5 | 8.3 ± 0.3 |
| 400 | 86.4 ± 0.2 | 1.5 ± 0.2 | 12.1 ± 0.2 |
All values are expressed as mean ± SD (n = 5)
Table II.
Effect of pH on Labeling Efficiency of Timolol Maleate
| pH | Percent of labeling efficiency | Percent of free Tc | Percent of colloids |
|---|---|---|---|
| 5 | 87 ± 0.2 | 12.3 ± 0.3 | 0.7 ± 0.3 |
| 5.5 | 90 ± 0.3 | 8 ± 0.2 | 2 ± 0.13 |
| 6.0 | 97.5 ± 0.1 | 2.0 ± 0.5 | 0.5 ± 0.12 |
| 6.5 | 98.2 ± 0.3 | 0.8 ± 0.12 | 0.2 ± 0.03 |
| 7.0 | 94 ± 0.2 | 5 ± 0.1 | 1 ± 0.3 |
| 7.5 | 90 ± 0.1 | 8 ± 0.3 | 2 ± 0.2 |
All values are expressed as mean ± SD (n = 5)
In Vitro Stability of Labeled Complex
In vitro stability of the labeled formulations was evaluated by ITLC. A 100 ml aliquot of the labeled formulation was mixed with 2.0 ml of phosphate-buffered saline (pH 7.4) and incubated at room temperature; change in labeling efficiency was monitored over a period of 24 h by ITLC as described above (Table III).
Table III.
In Vitro Stability of Radiolabeled Complex
| Time (hours) | Percent of labeling efficiency | Percent free |
|---|---|---|
| 0 | 98.8 ± 0.3 | 1.2 ± 0.2 |
| 1 | 98.7 ± 0.13 | 1.3 ± 0.1 |
| 2 | 98.6 ± 0.4 | 1.2 ± 0.13 |
| 4 | 97.4 ± 0.1 | 2.6 ± 0.32 |
| 24 | 94.5 ± 0.21 | 5.5 ± 0.21 |
All values are expressed as mean ± SD (n = 5)
Preparation of Placebo Formulation
Different combinations of placebo formulations were developed and evaluated for gelling capacity and other characteristics to identify the best suitable composition for final formulation. Chitosan was dissolved in saline solution, pH-adjusted to 5.5–6.0 by 1% v/v acetic acid. HPMC was also dissolved in normal saline (Table IV). The gelling capacity was determined by placing a drop of the system in a vial containing 2 ml of artificial tear fluid freshly prepared and equilibrated at 37°C and visually assessing the gel formation, noting the time of gelation and the time taken for the gel formed to dissolve. Viscosity of the formulation before and after gelation was measured using Brookfield’s viscometer (model DV II, spindle no. 02, at 20 rpm), while clarity was examined through visual inspection. The formulations are selected/rejected on the basis of their clarity, turbidity, and viscosity with change in pH. This method of measuring gelling capacity by visual inspection and measuring the viscosity using Brookfield viscometer is widely reported and adopted by different researchers with appropriate modification as per their laboratory setup (9,11–12).
Table IV.
Combinations of Chitosan/HPMC studied
| Formulation | Chitosan (% w/v) | HPMC(% w/v) | Gelling capacity |
|---|---|---|---|
| 1 | 0.25 | 2 | +++ |
| 2 | 0.5 | 2 | +++ |
| 3 | 1.0 | 2 | +++ |
| 4 | 0.25 | 1 | ++ |
| 5 | 0.5 | 1 | +++ |
| 6 | 1.0 | 1 | +++ |
| 7 | 0.25 | 0.5 | ++ |
| 8 | 0.5 | 0.5 | +++ |
| 9 | 1.0 | 0.5 | +++ |
| 10 | 0.25 | 0.25 | + |
| 11 | 0.5 | 0.25 | ++ |
| 12 | 1.0 | 0.25 | ++ |
Medicated Formulation
For antiglaucoma activity, timolol is prescribed as 0.25% to 0.5% w/v solution. Hence, a final drug concentration of 0.25% was used in formulation. Complete formula for the developed formulation is shown in Table V. The required quantity of timolol maleate (native or radiolabeled) to give a final drug concentration of 0.25% w/v was added to the previously optimized placebo formulation. Methyl paraben in a concentration of 0.1% w/v was used as preservative. Osmolarity of formulation was determined by osmometer (Fiske Associate, USA) and required quantity of sodium chloride after calculation was added to make the solution isotonic. The developed formulation was then filled in 10-ml-capacity amber-colored glass vials, with a cap and dropper with the teat. The formulation in its final pack was subjected to terminal sterilization by autoclaving at 121°C and 15 psi for 20 min. The sterilized formulations were stored in a refrigerator (4–8°C) until further use. Formulation was tested for different physicochemical properties as described and results are shown in Table VI.
Table V.
Formula of the Developed In Situ Formulation
| Ingredients | Concentration (w/v) |
|---|---|
| Timolol maleate | 0.25% |
| Chitosan | 0.5% |
| HPMC | 0.5% |
| NaCl | 0.45% |
| Methyl paraben | 0.1% |
| Water (q.s.) | 100% |
Table VI.
Physicochemical Properties of the Developed In Situ Gel Formulation
| Parameter | Inference |
|---|---|
| Clarity | Clear solution |
| pH | 6.0–6.2 |
| Osmolarity | 298–302 mOsmol |
| Gelation pH | 6.9–7.0 |
| Viscosity (at pH 6.0) | 40 ± 5 cps |
| Viscosity (at pH 7.2) | 150 ± 10 cps |
Values are expressed as mean ± SD (n = 5)
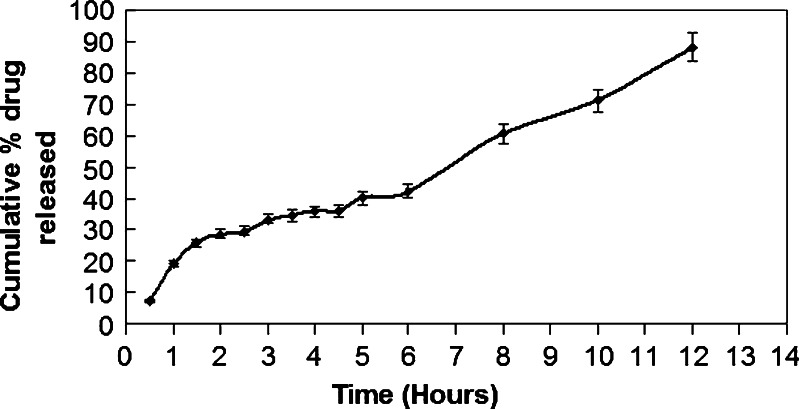
In Vitro Drug Release Profile
In vitro drug release kinetics from the prepared formulations was studied using a modified method reported earlier (13). Two milliliters of the test solution were placed in circular plastic cup (2.5-cm internal diameter and 1.2 cm in depth). This was placed on an inverted US Pharmacopeia basket which was kept inside a 250-ml beaker. Then, 100 ml of simulated tear fluid was added and stirred with a star-headed magnetic bead. Temperature of 37 ± 1°C was maintained throughout the study. Five-milliliter samples were withdrawn at regular time intervals and fresh media were added to replace the withdrawn samples. The samples were analyzed for drug content at 294 nm using an ultraviolet spectrophotometer. Results are shown in Fig. 1.
Fig. 1.
In vitro drug release profile of developed formulation. Values are expressed as mean ± SD (n = 5)
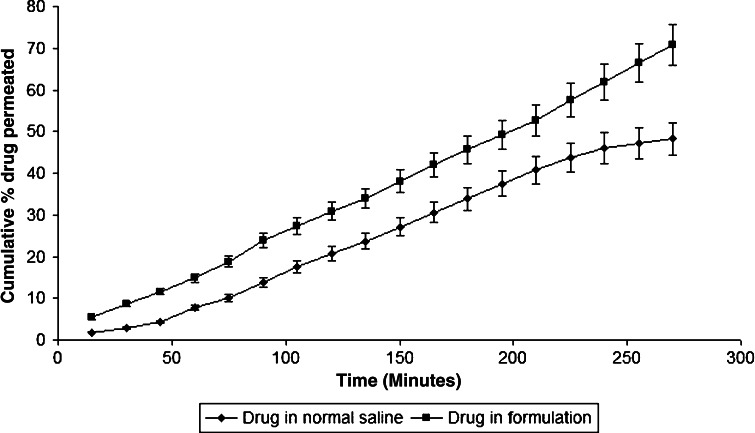
In Vitro Transcorneal Permeation Study
Goat corneas were used to study the permeation of timolol maleate across the corneal membrane. Whole eyeballs of goat were procured from a slaughter house and transported to laboratory in cold condition in normal saline maintained at 4°C. The corneas were carefully removed along with a 5–6 mm of surrounding scleral tissue and washed with cold saline. The washed corneas were kept in cold freshly prepared solution of tear buffer of pH 7.4. The study was carried out in modified Franz diffusion cells following the method reported by our group previously (9). It consisted of four cells and each cell consisted of upper and lower chambers. The upper chamber served as a donar compartment in which 100 μl of drug solution or formulation under study was placed. The composition of free drug solution was exactly the same as the composition of formulation except it did not contain any polymer. The upper and lower chambers were separated by goat cornea. The lower chamber served as a receiver compartment that was infused continuously with simulated tear fluid at the rate of 20 μl/min. The whole system was maintained at 37 ± 0.5°C. The perfusate was collected at periodic time intervals for up to 4 h in a preweighed microcentrifuge tubes and subjected to the quantification of timolol maleate using high-performance liquid chromatography method (14). Timolol maleate was freely soluble in water with octanol/water partition coefficient 1.8 and has pKa of 9.17.
Ocular Irritation Test (HET-CAM Test)
For the present study, modified hen’s egg chorioallantoic membrane (HET-CAM) test as reported by Velpandian et al. (15) was carried out. Briefly, fertilized hen’s eggs were obtained from poultry farm. Three eggs for each formulation weighing between 50 and 60 g were selected and candled in order to discard the defective ones. These eggs were incubated in humidified incubator at a temperature of 37 ± 0.5°C for 3 days. The trays containing eggs were rotated manually in a gentle manner after every 12 h. On day 3, egg albumin (3 ml) was removed by using sterile techniques from the pointed end of the egg. The hole was sealed by 70% alcohol-sterilized parafilm (American Can Company, USA) with the help of heated spatula. The eggs were kept in the equatorial position for the development of CAM away from the shell. The eggs were candled on the fifth day of incubation and everyday, thereafter, nonviable embryos were removed. On the tenth day, a window (2 × 2 cm) was made on the equator of the eggs through which formulations (0.5 ml) were instilled.
A 0.9% NaCl solution was used as a control as it is reported to be practically nonirritant. The scores were recorded according to the scoring schemes as shown in Table VII and score obtained was given in Table VIII.
Table VII.
Scoring Chart for HET-CAM Test
| Effect | Scores | Inference |
|---|---|---|
| No visible hemorrhage | 0 | Nonirritant |
| Just visible membrane discoloration | 1 | Mild irritant |
| Structures are covered partially due to membrane discoloration or hemorrhage | 2 | Moderately irritant |
| Structures are covered totally due to membrane discoloration or hemorrhages | 3 | Severe irritant |
Table VIII.
Scores Obtained in HET-CAM Test
| Formulations | Scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time (in minutes) | ||||||||||
| 0 | 5 | 15 | 30 | 60 | 120 | 240 | 480 | 1,440 | ||
| Normal saline as control | Egg1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Egg2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Egg3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Mean | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Developed formulation | Egg1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Egg2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Egg3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| Mean | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.33 | |
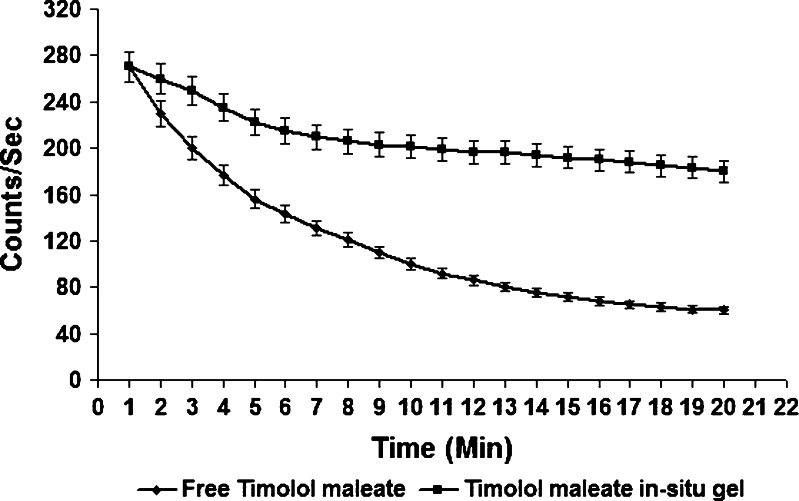
Gamma Scintigraphy
In vivo precorneal drainage of the developed formulation was assessed by gamma scintigraphy. Albino rabbits of either sex weighing 2–3 kg were used for the study. Animals were procured from the animal house of INMAS (Delhi, India) and having free access to food and water. The study was carried out under the guidelines compiled by the Committee for the Purpose of Control and Supervision of Experiments on Animals (Ministry of Culture, Govt. of India) and all the study protocols were approved by the local institutional Animal Ethics committee. Utmost care was taken to ensure that animals were treated in the most human and ethically acceptable manner.
Radiolabeled timolol maleate was incorporated into the optimized placebo formulation along with other ingredients as described previously. Gamma camera (Millennium VG, USA), autotuned to detect the 140-KeV radiation of 99mTc was used for scintigraphy study. Rabbits were anaesthetized using ketamine HCl injection given intramuscularly in a dose of 15-mg/kg body weight. The rabbits were positioned 5 cm in front of the probe and 25 μl of the radiolabeled formulation (100 μci) was instilled onto the left corneal surface of the rabbits. Recording was started 5 s after instillation and continued for 20 min using 128 × 128 pixel matrix. Individual 68 frames (68 × 16 s) were captured by dynamic imaging process. Region of interest was selected on the one frame of the image and time–activity curve was plotted to calculate the rate of drainage from eye. A single whole-body static image also was taken after 2 h of instillation of drug/formulation. Each formulation was tested on three rabbits.
RESULTS AND DISCUSSION
Gamma scintigraphy is a technique whereby the transit of a dosage form through its intended site of delivery can be noninvasively imaged in vivo via the judicious introduction of an appropriate short-lived gamma-emitting radioisotope. It provides an insight in to the fate of the delivery system. In the present work, we have used pharmacoscintigraphy as a powerful tool in the evaluation of our developed in situ formulation. Drug was labeled with radionuclide 99mTc. It was chosen for the purpose because of its moderate half-life (6 h). Further, it emits gamma rays, which have relatively low energy as compared to α and β rays, so it leads to no serious health hazards to the workers. Drug was instantaneously labeled with 99mTc. Ultraviolet spectrum of 99mTc-timolol maleate complex did not show any shift/changes from the original molecule; hence, timolol maleate was not affected therapeutically by labeling. Labeling efficiency was checked by ITLC using 100% acetone as mobile phase. The Rf value of free Tc is approximately 0.9, so it reached to the top of the ITLC strip while the drug–Tc complex, due to difference in molecular weight, retained at the base of ITLC strip. So from the difference in the top and bottom counts of the ITLC strips, efficiency could be calculated. The labeling procedure also leads to formation of reduced/hydrolyzed Tc (colloids); hence, to detect them, ITLC was run in another solvent system PAW. Colloids were retained at the base while drug–Tc complex traveled to the top of the ITLC strip.
Various labeling parameters, e.g., SnCl2 concentration and pH, were optimized and it was observed that at 100-μg SnCl2 concentration and at pH 6.5 the maximum labeling efficiency (98.2%) was obtained. At these conditions, minimum colloids (1.1%) were produced. In vitro stability of the labeled complex was also checked and the complex was found to be stable for up to 24 h.
The placebo formulations were developed using different combination of chitosan and HPMC which were evaluated for various physicochemical characteristics like gelling capacity, physical appearance, and viscosity at formulation pH (pH 6.0) and at ocular pH (pH 7.4). It was observed from the results that increasing the concentration of HPMC imparted viscosity to the formulation without affecting its clarity. Different combination of chitosan and HPMC were prepared and evaluated for its gelling capacity. It is prerequisite for an in situ gel system that it allows easy instillation into the eye as liquid drops which undergoes sol-to-gel transition, triggered by rise in pH. A concentration of 0.5% of both chitosan and HPMC was selected as it gave a colorless and transparent formulation (Table IV), which further gave the formulation prolonged resident time in cul-de-sac with no compromise with vision.
A medicated formulation was prepared from the selected placebo formulation. A dose of 0.25% of timolol maleate is prescribed for glaucoma therapy; hence, we also used the same concentration in our present formulation; 0.1% methyl paraben was added as preservative and NaCl in calculated amount was also added to maintain isotonicity of the final formulation (Table V). The amber-colored bottle closed with rubber closure and dropper with teat was used for packaging and was found to be appropriate packaging system for current formulation. The packaging was tested for resistance for autoclaving, leakage, and pourability. The packaging passed all the tests and proved to be a good choice for packaging of present ocular formulation. Sterilization of the product was done by autoclaving at 121°C for 20 min at 15 psig and test for sterility was performed on autoclaved packaging according to IP 1996 standards. There has been no growth/microbial contamination observed up to 14 days of incubation. Hence, the formulation passed the sterility test.
The developed formulations were further characterized for various physiological parameters, like clarity, gelation pH, viscosity, and osmolarity. The optimized formulation was isosmotic and gelation pH was found to be near 7.
In vitro drug release profile of the formulation was determined in simulated tear fluid (pH 7.4) and the formulation demonstrates a slow-release rate. Developed formulation shows 28.43% cumulative drug release after 2 h, 42.44% after 6 h, and 88.23% after 12 h as shown in Fig. 1.
In vitro transcorneal permeation studies were also conducted and a higher permeation across goat cornea was observed with chitosan/HPMC-based formulation as compared to plain drug solution (Fig. 2). This might be attributed to the well-known transmucosal enhancer property of chitosan.
Fig. 2.
In vitro transcorneal permeation profile of plain drug and drug in the developed formulation. Values are expressed as mean ± SD (n = 5)
Ocular irritation of the developed formulation was checked by hen’s egg chorioallantoic membrane test which is a rapid, sensitive, and inexpensive test. Testing with incubated eggs is a borderline case between in vivo and in vitro systems and does not conflict with the ethical and legal obligations. The chorioallantoic membrane of the chick embryo is a complete tissue including veins, arteries, and capillaries and is technically very easy to study. It responds to injury with a complete inflammatory process, a process similar to that induced in the conjunctival tissue of the rabbit eyes (15,16). Developed formulation was tested by this method and the result was compared with those obtained using normal saline, which was used as control that is supposed to be practically nonirritant. A means score of 0 was obtained for normal saline. Chitosan/HPMC-based formulation was nonirritant up to 12 h (mean score 0) while the mean score was found to be 0.33 up to 24 h (Table VII). The study shows that the formulation is nonirritant to mild irritant and is well tolerated.
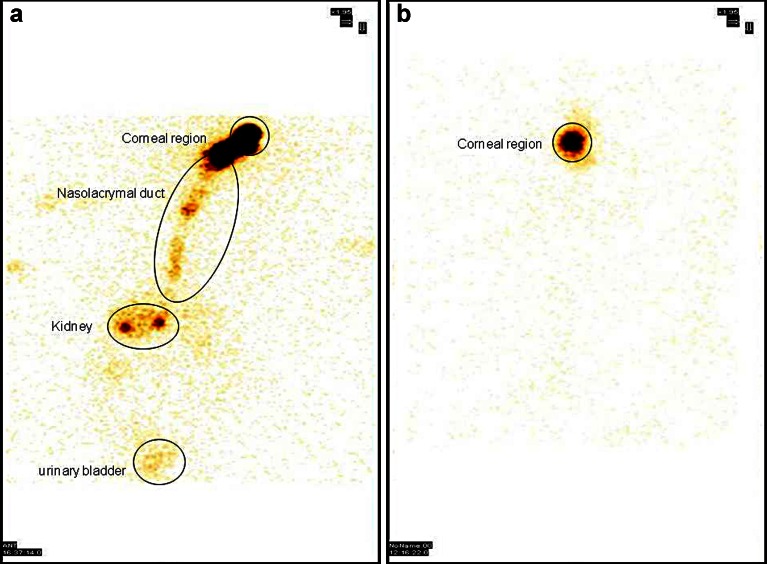
Scintigraphic studies were conducted on Albino New Zealand rabbits using radiolabeled timolol maleate in the formulation. The observation of the acquired gamma camera images showed good spreading over the entire precorneal area for developed in situ gelling system immediately after administration as compared with plain drug solution. The curve of the remaining activity on the corneal surface as a function of time (time–activity curve) was generated as shown in Fig. 3. Plain drug solution cleared very rapidly from the corneal region and reached into systemic circulation via nasolachrymal drainage system as significant activity was recorded in kidney and bladder after 2 h of ocular administration (Fig. 4a), whereas chitosan- and HPMC-based formulation was cleared at slow rate and retained at corneal surface for longer duration. No significant radioactivity was observed in systemic circulation (kidney and bladder) after 2 h (Fig. 4b). Chitosan is both viscous and bioadhesive. Further, viscosity of chitosan is increased as the pH of the formulation is raised (>7) upon instillation into eye as a result of buffering action of the tear fluid.
Fig. 3.
Time–activity curve shows precorneal drainage of various formulations
Fig. 4.
Static whole-body image after 2 h of drug administration a plain drug solution b developed in situ gel system
Conclusion
Drug was successfully radiolabeled with 99mTc for subsequent evaluation of the efficacy of the developed novel delivery system by pharmacoscintigraphy. This noninvasive technique has proved to be an important tool in evaluating ocular drug delivery system especially in evaluating retention and precorneal clearance. The developed chitosan/HPMC-based formulation was a nonirritant, enhanced transcorneal drug permeation, and prolonged the retention at corneal site. Formulation was found suitable for sustained topical drug delivery to eyes for rational drug therapy in case of various ocular diseases.
Contributor Information
Himanshu Gupta, Phone: +91-11-23824848, Email: himanshu18in@yahoo.com.
Sanyog Jain, Phone: +91-172-221468387, FAX: +91-172-2214692, Email: sanyogjain@niper.ac.in.
References
- 1.Maurice DM. Kinetics of topically applied drugs. In: Saettone MS, Bucci P, Padova S, editors. Ophthalmic drug delivery: biopharmaceutical, technological and clinical aspects. Fidia research series. Padova: Liviana; 1987. pp. 19–26. [Google Scholar]
- 2.Schoenwald RD. Ocular drug delivery: pharmacokinetic considerations. Clin Pharmacokinet. 1990;18:255–269. doi: 10.2165/00003088-199018040-00001. [DOI] [PubMed] [Google Scholar]
- 3.Middleton DL, Leung SS, Robinson JR. In: Bioadhesive drug delivery systems. Lenaerts V, Gurny R, editors. Boca Raton: CRC; 1990. pp. 179–202. [Google Scholar]
- 4.Swarbrick J, Boylan J. Ocular drug formulation and delivery. In encyclopedia of pharmaceutical technology. New York: Marcel Dekker; 1995. pp. 43–75. [Google Scholar]
- 5.Ranade VV, Hollinger MA. Intranasal and ocular drug delivery. In Drug delivery systems. Boca Raton: CRC; 1996. pp. 209–238. [Google Scholar]
- 6.Felt O, Baeyens V. Mucosal drug delivery: ocular. Encyclopedia of controlled drug delivery. Hoboken: Wiley; 1999. pp. 605–626. [Google Scholar]
- 7.Chiou GCY, Watanabe K. Drug delivery to the eyes. In: Ihler GM, editor. Methods of drug delivery: international encyclopedia of pharmacology and therapeutics. London: Pergamon; 1986. pp. 203–210. [Google Scholar]
- 8.Nanjawade BK, Manvi FV, Manjappa AS. In situ-forming hydrogels for sustained ophthalmic drug delivery. J Control Rel. 2007;122:119–134. doi: 10.1016/j.jconrel.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Gupta H, Jain S, Mathur R, Mishra P, Mishra AK, Velpandian T. Sustained ocular drug delivery from a temperature and pH triggered novel in situ gel system. Drug Deliv. 2007;14(8):507–515. doi: 10.1080/10717540701606426. [DOI] [PubMed] [Google Scholar]
- 10.Davis SS, Hardy JG, Newman SP, Wilding IR. Gamma scintigraphy in the evaluation of pharmaceutical dosage forms. Eur J Nucl Med. 1992;19(11):971–986. doi: 10.1007/BF00175865. [DOI] [PubMed] [Google Scholar]
- 11.Balasubramaniam J, Kant S, Pandit JK. In vitro and in vivo evaluation of the Gelrite® gellan gum-based ocular delivery system for indomethacin. Acta Pharm. 2003;53:251–261. [PubMed] [Google Scholar]
- 12.Srividya B, Cardoza RM, Amin PD. Sustained ophthalmic delivery of ofloxacin from a pH triggered in situ gelling system. J Control Rel. 2001;73:205–211. doi: 10.1016/S0168-3659(01)00279-6. [DOI] [PubMed] [Google Scholar]
- 13.Lin H, Sung KC. Carbopol/pluronic phase change solutions for ophthalmic drug delivery. J Control Rel. 2000;69(3):379–388. doi: 10.1016/S0168-3659(00)00329-1. [DOI] [PubMed] [Google Scholar]
- 14.Higashiyama M, Inada K, Ohtori A, Tojo K. Improvement of the ocular bioavailability of timolol by sorbic acid. Int J Pharm. 2004;272(1–2):91–98. doi: 10.1016/j.ijpharm.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 15.Velpandian T, Bankoti R, Humayun S, Ravi AK, Kumari SS, Biswas NR. Comparative evaluation of possible ocular photochemical toxicity of fluoroquinolones meant for ocular use in experimental models. Ind J Exp Biol. 2006;5:387. [PubMed] [Google Scholar]
- 16.Spielmann H. Ocular irritation. In: Castle JV, Gomez MJ, editors. In Vitro methods in pharmaceutical research. San Diego: Academic; 1997. pp. 265–287. [Google Scholar]