Abstract
Objective
To describe the method of incorporating an immunization certificate training program, such as the American Pharmacists Association's (APhA) Pharmacy-Based Immunization Delivery into a pharmacy curriculum.
Design
The program was delivered over 3 weeks in the spring semester of the third professional year (P3) as part of a required Pharmacy Care Lab sequence.
Assessment
Student response surveys and faculty input were used to evaluate the placement of the program in the curriculum.
Conclusion
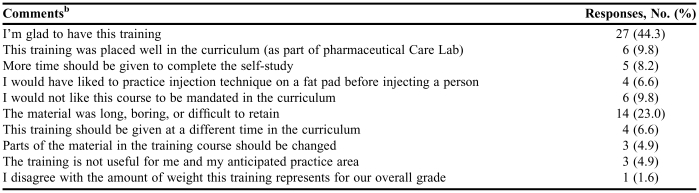
Optional comments yielded more than 44% of students providing positive open-ended feedback regarding the course while almost 10% felt the course should not be mandated in the curriculum.
Keywords: immunization, pharmacy curriculum, certificate program, public health
INTRODUCTION
On July 1, 2006, the Commonwealth of Pennsylvania updated the pharmacy scope of practice to give authority to pharmacists to administer injectable medications, biologics, and vaccines to adults.1 At the time of the change in the practice act, Pennsylvania was one of 44 states allowing pharmacists to administer immunizations.2 Registered pharmacists must apply for a license to administer injectable medications. The Pennsylvania State Board of Pharmacy voted on September 20, 2006, to approve the APhA's Pharmacy-Based Immunization Delivery certificate training program as the credential necessary for licensure. The application process involves completing an application form, providing proof of cardiovascular and pulmonary resuscitation certification (CPR), and submitting an application fee.
In 2005, Wilkes University contracted with APhA to become a licensed provider of the APhA Pharmacy-Based Immunization Delivery program. Six faculty members from Wilkes University were trained to teach Pharmacy-Based Immunization Delivery to other pharmacists and pharmacy students interested in becoming licensed to administer injectable medications in Pennsylvania.
The APhA Pharmacy-Based Immunization Delivery program is a certificate training course developed for pharmacists and provides comprehensive immunization education and training. According to APhA, the course is “an innovative and interactive training program that teaches pharmacists the skills necessary to become a primary source for vaccine information and administration. The program teaches the basics of immunology and focuses on practice implementation and legal/regulatory issues.”3 It consists of 20 hours of continuing education (CE) credit in the form of a self-study (12 hours) and a live training session (8 hours).3 Students may complete the program without receiving CE credit.
The knowledge and skills taught in the program are consistent with educational outcomes listed in the American Association of Colleges of Pharmacy's Center for the Advancement of Pharmaceutical Education (CAPE) in 2004.4 Immunization education and delivery addresses the third outcome of public health by promoting health improvement, wellness, and disease prevention. Educating pharmacy students about the role of immunization delivery in population-based care is also consistent with Standard 12 of the professional competencies listed in the Accreditation Standards 2007 for the doctor of pharmacy degree.5 The training program not only focuses on the public health outcome but also fosters the development of knowledge and skills in various areas of biomedical, pharmaceutical, administrative pharmacy, and clinical sciences.
The scope of practice for pharmacists is expanding in states across the country to include administration of medications or certain vaccines. As of March 2008, there were 48 states that authorized pharmacists to administer immunizations. More than 30,000 pharmacists in the United States have been trained through the APhA program.2 The administration of vaccines has become part of the scope of practice for pharmacists in almost every state.
The APhA certificate training course has been incorporated into the curriculum at other pharmacy schools. One such method of incorporation was offered to P2 (second professional year) students during influenza season and involved a modified lecture using small group, case discussions.6 However, this report appears to be the only published evidence to date on incorporating immunization training methods into the pharmacy curriculum.
DESIGN
The objective of this study was to describe h how one method of incorporating the certificate training program into the curriculum. The overall goal was to optimize immunization instruction in the curriculum.
The decision to incorporate the certificate course into the curriculum was approved at a department of pharmacy practice faculty retreat in May 2006. The faculty agreed that the course should be mandatory and that courses in infectious disease (Spring P2) and immunology (Spring P2) should be prerequisites. The decision to require the certificate course for all students was based on the changing scope of pharmacy practice in Pennsylvania and was consistent with the department and school's mission to provide a dynamic and innovative pharmacy curriculum. In addition, incorporating the course into the curriculum would enable students to meet the professional outcomes of promoting public health through public awareness of health and disease. Therefore, with departmental and administrative support, it was decided to require the certificate course over 3 Pharmacy Care Lab sessions in the spring P3 year.
Pharmacy Care Lab is a 5-semester course designed to give students the opportunity to apply the knowledge and skills they have gained throughout the pharmacy curriculum to practical patient care situations. Each week, the Care Lab assignments focus on different topics that have been covered in the didactic curriculum. In many laboratories, students have the opportunity not only to develop a therapeutic care plan but also to practice patient counseling through role playing. Simulated patient scenarios give students the opportunity to apply their skills and knowledge in “real life” situations. Furthermore, drug information, team building, critical thinking, problem solving, communication, and self and peer assessments are also emphasized throughout the five-semester sequence. Prior to the adoption of Pharmacy-Based Immunization Delivery into the curriculum, students received some immunization education in 2 laboratories within Pharmacy Care Lab V in the spring of the P3 year. However, these laboratories did not include specific immunization technique and assessment.
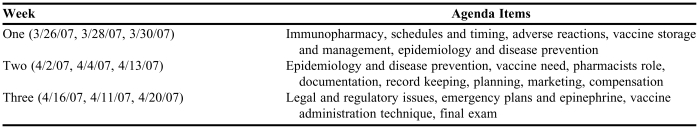
The Pharmacy Care Lab sequence seemed the most appropriate course in which to integrate the immunization training program because of the sequence's unique use of active learning and patient-case scenarios. Table 1 describes the schedule of topics for the 3 Care Labs dedicated to the delivery of the immunization program. Students were given the self-study materials during the first week of Care Lab and instructed to complete the 12 hours of self-study materials for submission during the final week of lab. Due to the university holiday schedule, students in the Monday and Friday sections had 3 weeks to complete the self-study materials, while those in the Wednesday section had 2 weeks. Cost of program materials was included in Pharmacy Care Lab fees as part of tuition expenses. The P4 advanced practice students wishing to take the program received the materials at cost and paid for them prior to participating in the course. Some students expressed anxiety and reservations about completing the injection technique as part of a required component of the curriculum. These students met with the instructors on an individual basis to discuss their concerns.
Table 1.
Schedule of Topics for Pharmacy-Based Immunization Deliverya
Each laboratory session was 2 hrs, 50 min.
Current CPR certification was required of students who wished to participate in the certificate training. The College of Pharmacy and Nursing coordinated the training through the American Red Cross. The certification course was offered during the spring semester of their P1 and P3 year. Students were financially responsible for the cost of the program.
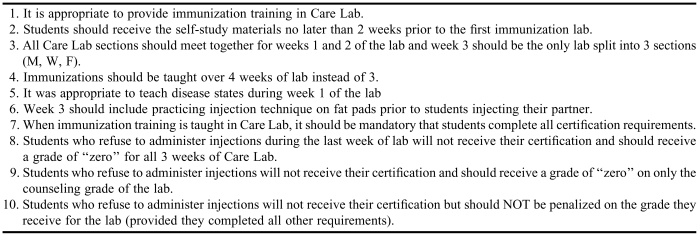
The Pharmacy-Based Immunization Delivery program included an evaluation form that students completed during the final hour of the live training seminar. This form asked participants to evaluate the program, the quality of the speakers, and the perceived impact of the material on clinical practice. The results were then compiled and sent to APhA. An additional survey was administered to students in WebCT (Blackboard, Inc., Washington, DC). The purpose of this survey was to evaluate all of the Care Labs in the second half of the spring semester. However, the survey included 2 questions that pertained specifically to the immunization laboratories. These questions were directed at determining whether students felt the instructors were knowledgeable and well prepared and whether students felt they had learned a lot in the laboratories. The responses were recorded on a Likert scale and asked students to strongly agree, somewhat agree, neither agree nor disagree, somewhat disagree, and strongly disagree. In addition, students were given an opportunity in the survey to add comments or suggestions for the particular laboratory or laboratory instructor. After students completed the Pharmacy Care Lab survey, another survey, sent to participating faculty members, focused on concerns that arose from the student survey. Results of the faculty survey could be used to improve the course the next year. Table 2 lists the 10 statements included in the faculty survey.
Table 2.
Survey to Faculty Instructorsa
The survey was administered to instructors after student comments were collected and analyzed. Faculty response options were on a Likert scale: strongly agree, somewhat agree, neither agree or disagree, somewhat disagree, and strongly disagree
ASSESSMENT
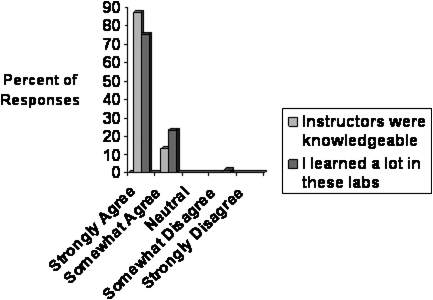
Eighty students completed the immunization instruction during Pharmacy Care Lab (73 P3 students and 7 P4 students who requested to take the course during their advance pharmacy practice experiences). There was a 100% pass rate, with a passing grade defined as a score of > 70% on the self-study materials and the final exam and by demonstrating appropriate injection technique. The WebCT survey was only administered to P3 students, and 69 students (95%) completed the survey. Figure 1 shows the results of the 2 survey questions that pertained to the immunization laboratories. Every student completing the survey agreed that the instructors were knowledgeable and well prepared. Nearly every student (99%) agreed that they learned a lot in the labs.
Figure 1.
Student responses to Web CT survey questions (n=69).
Of the 95% of students who completed the survey, 61 (88%) offered open comments. A summary of the comments is listed in Table 3. Some students commented on more than one issue. Overall, 27 students mentioned that they were happy to have completed the training compared to only 3 students who felt it would not be useful to them. Six students felt it was in the appropriate place in the curriculum and 6 students felt that the course should not be required. Of the 5 students who listed comments about wishing to receive the self-study materials earlier, 3 of those students were from the Wednesday section, which had less time between the labs to complete the work due to university holidays.
Table 3.
Open-Ended Student Survey Comments (N = 61)a
There were 69 students completing any portion of the survey out of 73 surveys sent. There were 61 students offering open-ended comments.
b Students' comments were classified into statements.
The results of the separate survey administered to faculty members (n=4) involved in teaching the program revealed a number of key issues. Three of the faculty members supported the placement of the immunization training in Pharmacy Care Lab. In addition, none of the faculty members felt that more than 3 laboratory periods should be used for the program. The participating faculty members had varying opinions about whether the certificate program should be mandatory (50% agreed, 25% did not agree, 25% were neutral). Every student completed all requirements of the course in the first year. Recognizing a potential situation where students may not wish to complete the requirements of the program, a majority of faculty members agreed (75% agreed, 25% were neutral) that the student's Care Lab grade would not be impacted for refusing to demonstrate administration technique. However, the student would not receive a certificate from APhA as per the association's requirements.
DISCUSSION
Pharmacy-Based Immunization Delivery or a similar program should be incorporated into pharmacy curricula across the country. Both students and faculty members supported the incorporation of immunization delivery training into the curriculum. Based on the survey results and feedback, all faculty instructors agreed that the following changes should be made for subsequent offerings. First, students will be provided the self-study materials 2 weeks prior to the first immunization laboratory to give them time to review the material prior to class. Second, for more efficient management of faculty time and workload, all 3 sections (Monday, Wednesday, and Friday groups) will be combined for the first 2 weeks of lab and only week 3 will be taught during the regularly scheduled laboratory sections. Third, during week 3, students will have the opportunity to practice injection technique on fat pads prior to injecting their partner. This strategy will help improve student confidence in injection technique and alleviate fears. The faculty agreed that it would also be helpful to have a P4 student, certified in immunization delivery, on hand to answer questions and prepare students while the faculty members observed injection technique.
This training program is an important addition to the pharmacy curriculum as it provides students the opportunity to review important material taught in other didactic courses and to participate in interactive case studies that allow them to learn and demonstrate new skills. The skills taught in the course are consistent with Educational Outcomes addressed by the CAPE and are important in the professional development of future pharmacists. Despite these benefits, the faculty expressed some concerns, particularly regarding the Care Lab time necessary to deliver the immunization program. Therefore, the faculty is considering alternative ways to deliver the didactic portion of the program while still retaining the injection/demonstration technique within the Care Lab. Regardless of how to deliver the didactic portion, the faculty unanimously agreed that immunization delivery is an important component of the pharmacy curriculum. The information and skills taught in the immunization program will provide students the opportunity to deliver alternative services and advanced patient care.
CONCLUSION
Pharmacy schools should explore various methods for incorporating immunization training into their individual curricula based on the professional needs of the students, student scheduling, and faculty workload. Requiring the program for all students in their P3 year in an application-based Care Lab or similar course may be one successful way to incorporate these skills into the curriculum. The skills learned in this program are valuable to students and will help prepare them for an evolving scope of practice in the pharmacy profession.
REFERENCES
- 1.Pennsylvania State Board of Pharmacy. Drug therapy and injectable medications, biologicals and immunizations. 49 PA. CODE, CH. 27. 7-1-0006. 36 Pa.B.3237. 6-26-2007.
- 2.States where pharmacists can immunize. American Pharmacists Association Web site. June 26, 2007. http://www.pharmacist.com/AM/Template.cfm?Section=Patient_Care_Services2&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=15864. Accessed January 26, 2009.
- 3.American Pharmacists Association. Pharmacy-Based Immunization Delivery. A continuing education program. Updated January 2007.
- 4.Center for the Advancement of Pharmaceutical Education – Educational Outcomes 2004. American Association of Colleges of Pharmacy Web site. http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE2004.pdf. Accessed December 10, 2008.
- 5.Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Accreditation Council for Pharmacy Education Web site. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Published July 1, 2007. Accessed December 10, 2008.
- 6.Hak EB, Foster SL, McColl MP, Bradberry JC. Evaluation of student performance in an immunization continuing education certificate program incorporated in a pharmacy curriculum. Am J Pharm Educ. 2000;64:184–7. [Google Scholar]