Abstract
In response to national trends for preceptor development, the University of Maryland School of Pharmacy conceived, developed, and implemented the Academy of Preceptors to foster preceptor development. The Academy's goals are to recognize preceptor excellence, improve experiential course delivery, develop preceptors' educational skills, and facilitate networking among preceptors.
In 2004, the Academy's initial focus was development of live continuing education programs for preceptor development. A CD-ROM format also was developed for those who could not attend live sessions. Preceptors were asked to suggest additional topics of interest for future programs.
In this paper, we describe our progress toward the goals, the School's benefits from the Academy, and the implications for the American Association of Colleges of Pharmacy (AACP).
Preceptors provide 30% of pharmacy curricula; thus, the need for their training and ongoing professional development has been increasingly emphasized within experiential education. Priorities are to train preceptors to become better educators and motivate these practitioners to improve pharmacy education by sharing their valuable expertise with students.
Keywords: preceptor development, experiential education, introductory pharmacy practice experience (IPPE), advanced pharmacy practice experience (APPE)
INTRODUCTION
The American Association of Colleges of Pharmacy (AACP) has identified preceptor development as a key component of quality experiential education.1 In January 2002, the Preceptor Development Task Force, formed by the Association's Pharmacy Practice Section/Professional Experience Programs Special Interest Group (PEPSIG), made the following recommendations:
Create a variety of programs for live or distance delivery;
Develop a series of programs (modules) leading to a preceptor certificate;
Update the Association booklet Training Pharmacy Preceptors to a Web-based or CD-ROM format;
Increase awareness of and define characteristics for successful programs;
Define the rubric for performance levels for Center for the Advancement of Pharmaceutical Education (CAPE) competencies to practice pharmacy;
Develop progressive modules, from general topics for new preceptors to advanced, more-detailed topics for experienced preceptors;
Facilitate combining and sharing programs;
Disseminate ideas to develop existing preceptors; and
Emphasize teaching skills, especially for assisting students with distinctive abilities, needs, and interests.
The expectation for preceptor development is clearly stated in the Accreditation Council for Pharmacy Education (ACPE) Standards.2 New preceptors are to be trained prior to precepting students, and programs should support professional development of volunteer preceptors. This presents ongoing challenges for experiential education in schools and colleges. New or expanding programs must continually recruit preceptors to meet future students' experiential learning requirements. All programs must recruit preceptors to offset attrition as preceptors experience career or life changes (eg, relocation, retirement). New preceptors need basic training so that they are familiar with students' didactic preparation and experiential course requirements. Ongoing development of experienced preceptors should also be addressed.
Based on these recommendations and requirements, the Experiential Learning Committee (ELC) at the University of Maryland School of Pharmacy recognized the need for a formalized method of providing education that would improve how preceptors teach as well as ensure that students benefitted from quality learning experiences. This paper describes the concept, development, and implementation of Academy of Preceptors and discusses future implications.
CONCEPT AND DESIGN
The rationale for the Academy was that preceptors represent 1 of the School's most important resources as supporters of the School's Experiential Learning Program (ELP), which now constitutes 30% of the curriculum. Each preceptor facilitates 1 or more of the School's 43 experiential learning courses, both required and elective.3 While their credentials are evaluated prior to their appointment as clinical faculty members, preceptors are often unfamiliar with the School's curriculum, strategic initiatives, expectations, and best practices in experiential education. Preceptors may work in isolation from other preceptors in similar School experiential courses, and they vary greatly in educational expertise, length of service, and pharmacy practice setting. Prior to 2004, their training was sporadic and often related to responsibilities for a specific course as there was no curriculum appropriate for all preceptors. Therefore, to capitalize on the strengths of existing preceptors and to offer a more complete curriculum for preceptor development, the School established the Academy of Preceptors.
The concept of the Academy of Preceptors provided an identity that did not previously exist for the collective pool of preceptors and is similar to that of major pharmacy organizations. For example, in the American Pharmacists Association (APhA), members are voluntarily organized into the Academy of Pharmacy Practice and Management, the Academy of Pharmaceutical Research and Science, and the Academy of Student Pharmacists. APhA provides the administrative support and resources for the Academies to convene and function. Similarly, at the University of Maryland School of Pharmacy, preceptors volunteer their service, and upon credentialing and academic appointment, become members of the Academy of Preceptors. However, unlike the academies within professional associations, there are no membership dues, no officer elections or self-directed governance, and no specialized sections.
The term academy was chosen as an honorific for the roster of preceptors. The term conveys the School's respect for preceptors and the collective prestige of clinical faculty appointments for experiential education. It also signifies inclusion in the academic environment. While the Academy of Preceptors members do not have voting privileges in the University's Faculty Assembly, they are included in many important functions of the School, from admissions interviews and accreditation visits to curricular updates and student organization events. By formalizing the role of preceptors within the School and giving them a collective title (ie, Academy of Preceptors), the esteem in which these professionals are held and their importance to achieving the School's mission is better conveyed, both to their faculty colleagues and the profession at large.
Taking place long before training or development, preceptor recruitment is as important to the pharmacy program's success as internal faculty recruitment. Preceptors are identified from professional organizations, site coordinators, referrals from faculty members and students, specialty settings, and self-nominations. Preceptor candidates submit an application, including a statement of character, along with a curriculum vitae and a copy of their current pharmacist license, as applicable. All candidates must belong to a professional organization and have access to e-mail. Course-specific preceptor criteria and requirements are included in course syllabi. For example, direct patient care experience is necessary for teaching several of the School's required and elective experiential courses. Once the School's experiential personnel have verified an applicant's information and recommended course assignments and clinical rank, the candidate's materials are forwarded to the Chair of the Department of Pharmacy Practice and Science and to the Dean of the School for approval. For preceptor appointments at the clinical associate professor or clinical professor level, the Faculty Affairs Committee must apply established promotion criteria and make recommendations prior to the Dean's approval. Official appointment letters to preceptors state the School's expectations that preceptors provide an environment conducive to successful student performance, participate in educational development to improve precepting skills, and support experiential learning policies and procedures. Preceptors indicate their agreement by signing and returning a copy of their appointment letter. Reappointments are completed every 3 years.
The primary purpose of the Academy of Preceptors is preceptor development, and the goals are to recognize practitioners who exhibit excellence in precepting; improve the delivery of experiential learning courses; develop preceptors' educational skills; and facilitate networking opportunities among preceptors.
The School perceives “preceptor development” as the constellation of educational and continuing education activities; resources (including faculty members and mentors); and preceptor events and recognition, which empowers preceptors to optimally facilitate experiential courses and nurtures professional satisfaction throughout their clinical faculty careers.
By definition, members of the Academy of Preceptors are preceptors for the University of Maryland School of Pharmacy. Preceptors generally are practicing pharmacists who have agreed to serve and who have received an appointment as clinical faculty members. In some cases, professionals other than pharmacists offer their expertise as appropriate for elective experiences. For example, an Annapolis-based lawyer serves as the preceptor for a legislative experience, and a physician at the Agency for Healthcare Research and Quality serves as a preceptor for a research experience.
DEVELOPMENT AND IMPLEMENTATION
Key Entities
Administration of the ELP is provided by a director, an assistant director, and 2 professional staff members. As head of a school-wide program, the ELP director reports to the Associate Dean of Academic Affairs. Internal faculty members (3 for introductory pharmacy practice experiences [IPPE] and 20 for advanced pharmacy practice experiences [APPE] from all 3 departments, but most from Pharmacy Practice and Science) serve as coursemasters (course managers) for academic experiential course responsibilities, such as syllabus preparation and grade submission. Required coursemasters and experiential personnel serve on the ELC, which forwards specific course recommendations to the Curriculum Committee prior to approval by the Faculty Assembly. Prior to inception of the Academy, individual course managers were responsible for training preceptors for their courses, and these labor-intensive efforts were not unified. Standardized basic training applicable to all preceptors was not provided, and incentives, such as continuing education credit, were not consistently offered.
A variety of individuals and groups were key entities necessary for the successful development and implementation of the Academy of Preceptors. School administrators provided funding to support programming that aligned with quality standards. The ELC provided programmatic oversight and recommendations. Course managers who developed experiential courses reviewed student evaluations as a basis for developing preceptor training topics. Students' cooperation in providing constructive feedback to preceptors after each experience remains essential and is now required. Stakeholders, such as the external entities that employ graduates, continue to assist with identification of exemplary practitioners for clinical appointment and facilitation of preceptor involvement.
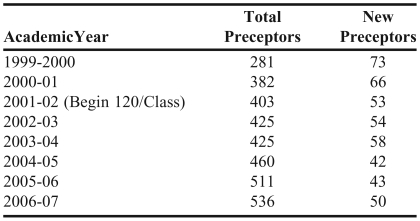
The expanding need for pharmacists has led the School to respond by increasing class enrollment, resulting in an increase in numbers and types of preceptors and experiential sites needed to support learning requirements. Specifically, the School increased enrollment from 100 to 120 students per class for fall 2001, and again expanded enrollment in fall 2007 to 160 by adding a cohort on the Universities of Shady Grove campus in Rockville, Maryland. Table 1 lists the annual number of preceptors as enrollment has increased.
Table 1.
Total Preceptors and New Preceptor Appointments in the University of Maryland School of Pharmacy by Academic Yeara
Numbers of preceptors change continually. Some preceptors are temporarily unavailable during leaves of absence or job changes. These individuals are reactivated, but not reappointed, when they resume precepting. The totals for this table were collected from various School reports provided at different times in the years identified. Examples of reports include ACPE self-study documents, annual reports, and the Dean's state of the school message.
Goal Timeline
For students to achieve competence as defined by educational goals, preceptors must also be competent to provide experiential education. Therefore, tactics were proposed by which the goals for the Academy of Preceptors (described above) could be achieved. The ELP director drafted a preceptor development plan for the Academy in March 2004. Feedback was provided by the ELC and comments were solicited from a fourth-year student focus group and a preceptor focus group in April 2004. In June 2004, course managers reviewed student evaluations from the previous semester's IPPEs and APPEs, with particular emphasis on areas pertinent to the training programs, as well as curriculum committee recommendations for skills-based assessment tools, including professionalism.4 In July 2004, the announcement of the formation of the Academy of Preceptors was included in a mailing to all preceptors.
Goal One: Recognize Preceptors' Excellence
To promote excellence in the ELP, outstanding preceptors were recognized and featured as role models and mentors or trainers through awards, presentations, and promotions. The annual Preceptor of the Year Awards were revised and finalized in April 2004 to include the more intensive peer-review process described below. These exemplary Preceptors of the Year were asked to present at Academy seminars that promoted best practices and lessons learned.
Growing Importance of Preceptors of the Year
Preceptors of the Year are increasingly important to the Academy, the ELP, and the School.5 In 2000, the School's Preceptor of the Year recognition awards were instituted for IPPE preceptor, APPE preceptor, and new preceptor in the first 3 years of academic appointment. The criteria include high standards of professionalism, spirit of cooperation with the School, and commitment to students as a professional mentor and teacher. The ELC subcommittee's decision is forwarded to the Chair of the Department of Pharmacy Practice and Science and the Associate Dean of Academic Affairs for approval prior to notification of recipients.
These preceptor honorees are now part of the fabric of the ELP during their year of recognition. The preceptors receive their awards at the School's convocation so that graduating students can honor them. They also speak at student events and are featured in School publications. Preceptors of the Year are asked to participate in the ELC for important considerations such as experiential course and policy revisions. Four of them have been invited to teach other preceptors at Academy seminars and to provide “precepting pearls” in the ELP newsletter, Maryland Mentor. Their experience, enthusiasm, influence, and insights have helped the ELP improve training and have encouraged high standards among preceptors. In fact, these preceptors have become ambassadors for recruiting new preceptors to the program.
The second tactic to achieve goal 1 is to streamline the preceptor promotion process. Even though promotion is included in basic training, most preceptors do not seek it. In 2004, among all preceptors, only 3 clinical professors and 7 clinical associate professors had earned promotions. Over 500 preceptors serve at the clinical assistant professor rank, and pharmacy residents are appointed annually as clinical instructors. Preceptors may self-assess against the promotion criteria, but they generally have found portfolio documentation overwhelming. With ELC input, the 2006-2007 Faculty Affairs Committee deliberated and approved a new timeline and an efficient process to mentor more preceptors toward promotion in recognition of their service and accomplishments (Appendix 1).
Goal 1, to recognize preceptors' excellence, has been met. First, all the preceptors were recognized collectively as the Academy of Preceptors to identify, brand, and convey esteem for these important educators. The Preceptor of the Year process was strengthened and has resulted in 9 Preceptors of the Year awards and 6 New Preceptors of the Year awards since 2004 (17 and 10 overall since 2000). Of these, only 2 preceptors have been honored more than once. Preceptor promotions also recognize teaching, service, and scholarly excellence; and through the more efficient process, the School should continue to meet or exceed the goal of 4 promotions annually.
Goal Two: Improve Management and Administration of Experiential Learning Courses
Experiential education is complex and involves many components, including students, preceptors, sites, administrative personnel, courses, calendars, regulations, insurance, and affiliation agreements. Improvement of operations for experiential course delivery was accomplished through the ELC programmatic coordination. Deadlines and policies varied throughout experiential courses. Therefore, consistent policies needed to be unified throughout the 4-year program to help students and preceptors navigate the expectations efficiently and fairly. A strategy to meet goal 2 was thorough review and revision of ELP policies and procedures. Also important was implementation of skills-based assessments in all IPPEs and APPEs to ensure documentation of students' performance and achievement of the School's terminal performance outcomes, which align with ACPE Standards.
An example of such a policy is the limitation of out-of-program APPEs to no more than one of the elective courses. Required APPEs must be completed with existing credentialed and trained preceptors. By setting this expectation, students can still develop unique experiences, and the ELP can manage the workload and maintain quality for course delivery. We seek to foster an exceptional program rather than a program of exceptions.
Goal 2 has been achieved. Skills-based assessments for all experiential courses have clearly defined expectations for students and have unified and standardized assessment forms by which preceptors evaluate students. The ELC continues to assist course managers with experiential course improvements and refinements that improve course delivery. This goal is met by an annual review and update of the policies and procedures, with input from students, preceptors, and faculty members, and by regular review of student evaluations of self, site, and preceptor, as now required for each IPPE and APPE. Future plans for goal 2 to improve course delivery and tracking of student assessments include a beta test of the SUCCESS competency assessment program.6
Goal Three: Develop Educational Skills of Preceptors
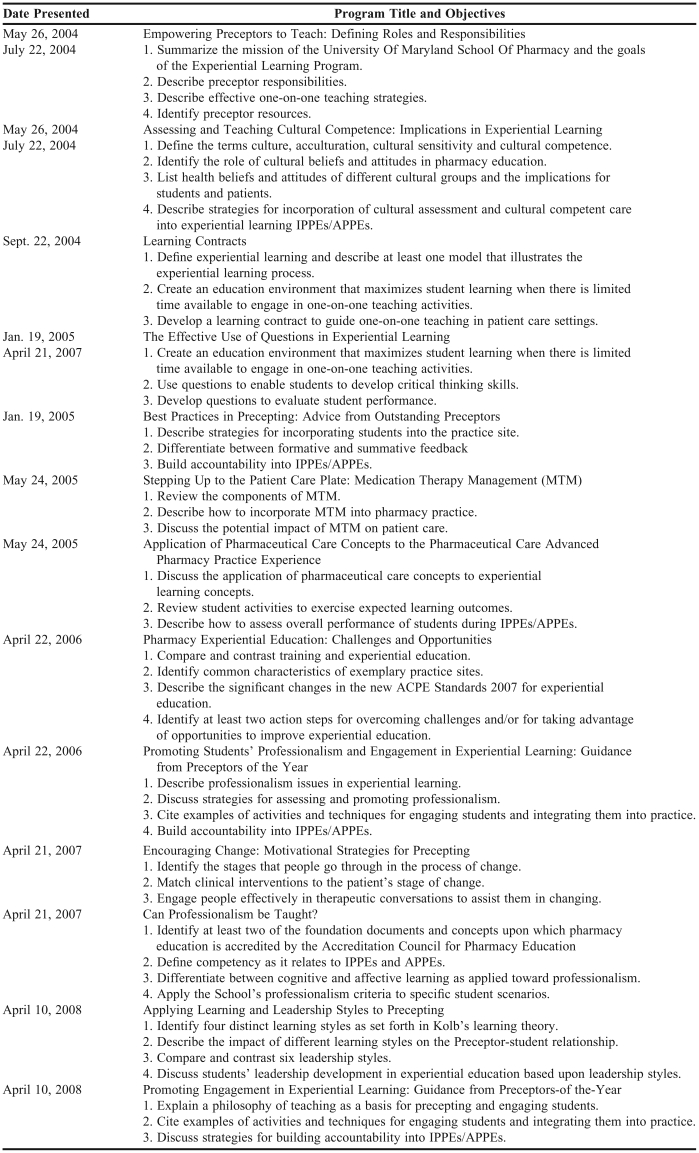
A major component of the Academy concept was development of preceptors' educational skills. Internal faculty members, preceptors, and invited speakers presented teaching modules on preceptor orientation, methodology for experiential learning, cultural competence in pharmaceutical care, professionalism, and other related topics pertinent to experiential learning. Appendix 2 lists programs to date, along with learning objectives. All programs were ACPE-accredited for continuing education, and preceptors were asked to recommend additional topics with each program evaluation. Preceptor program attendance has ranged from 18 to 54 participants; the audience size has promoted engagement among preceptors and enabled effective use of active-learning strategies. Almost without exception, preceptors agreed or strongly agreed that program objectives had been met, that speakers were effective, and that they were satisfied with the program and facility.
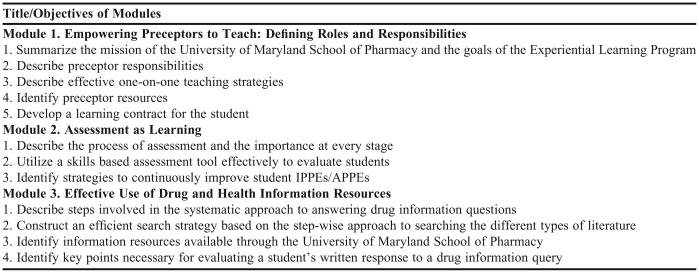
To improve access for preceptors who could not attend live training, the “Preceptor Survival Kit” was developed in 2006. It consists of the American Society of Health-System Pharmacists' (ASHP) Preceptor's Handbook for Pharmacists7 and a CD-ROM with content targeted to the basic training needs of all preceptors, regardless of practice setting (Table 2). The CD-ROM format was determined to be more user friendly than a Web-based program since some preceptors might not have access to a high-speed Internet connection. The survival kit was sent to all existing preceptors and is now provided to new preceptors with their appointment letters. With training available to all preceptors, development expectations have been emphasized for the clinical faculty reappointments since July 2005.
Table 2.
Lesson Modules in a CD-ROM on Basic Training for Pharmacy Preceptors at the University of Maryland
In many ways, goal 3 is the most important and most challenging, and we have made progress toward this goal in several ways. We have expressly stated the expectation “to participate in educational development to improve precepting skills” in each preceptor's appointment letter, and preceptors have indicated agreement by signing their appointment and reappointment acceptance letters. We have created a basic preceptor development curriculum and offered live and recorded training accredited for ACPE continuing education. Experienced Preceptors of the Year have shared best practices, and preceptors are satisfied that the training program objectives have been met, as evidenced by program evaluation responses. A new 2008 satisfaction survey of students in the first 3 professional years (IPPE) has yielded an internal benchmark by which to gauge future progress; 85% strongly agreed or agreed (N = 244) that preceptors provided individualized instruction, guidance, and evaluation that met the needs of doctor of pharmacy students.
Goal Four: Facilitate Preceptors' Networking Opportunities
The Academy provides unique networking opportunities that promote interactions between IPPE and APPE preceptors and among those who practice in various settings, rather than within a single organization or employer. Examples include an annual preceptor recognition event; an annual Academy symposium in the spring before the next academic cycle; preceptor focus groups at state association meetings; and various School events, such as convocation and student functions. For instance, the Gifts of Time Reception is held every year during the University's Founders Week to recognize all preceptors for their contributions to the ELP and to promote networking among preceptors as well as invited alumni.
Goal 4 has been met by coordinating planning and communications among the ELP, the Alumni Association, and the Office of External Affairs, and with the support of the Dean in funding and promoting networking events. School-wide events at which preceptors are recognized have increased from 1 to 3 per year, and other occasions such as receptions at national meetings also promote networking. Future plans include expanding networking opportunities in interest groups for practice specialty or service, such as Medication Therapy Management (MTM).
Benefits and Incentives for Preceptors in the Academy
Beyond the intrinsic benefits of working with students, preceptors are incentivized with continuing education credits for live and recorded programs. Development activities can be documented toward promotion and award criteria. Documentation may also support references and recognition applications such as Fellow of the American Society of Health-System Pharmacists or Fellow of the American Pharmacists Association. A recent 50% increase in honoraria payments was enacted as a benefit and incentive, but since this was offset by the increase in APPEs from 4 weeks to 5 weeks, honoraria payments may be adjusted again. It will be important to survey preceptors to evaluate their satisfaction with the Academy and their perceptions relative to the goals.
Resources
Prior to inception of the Academy, industry sponsorship supported preceptor recognition events. While these events promoted collegiality among preceptors, they did not advance educational goals. Unrestricted School funds were identified to support the annual preceptor symposia. Use of School facilities has limited expenses to food, parking, and materials.
Web-based or recorded modules were a high priority for preceptors who could not attend live programs. Since preceptor access to the campus Blackboard course platform was problematic and would have generated fees of $1,500 annually and $5 per module per preceptor, $15,000 was budgeted for module recording, CD-ROM production, and purchase of the ASHP handbook. In support of the entire plan, School administrators absorbed the associated costs for ACPE accreditation of the continuing education modules.
Given the increased workload, particularly for experiential course managers, it was essential to seek incentives, such as recognition and honoraria, for participating internal faculty members. The Chair for the Department of Pharmacy Practice and Science agreed to fund a $1,000 honorarium for 3 faculty members who developed and recorded a basic training module for the CD-ROM. In addition, ELP personnel provided significant support to these faculty members during the project. This honorarium will be important in recruiting faculty members to update existing programs or create new recorded modules.
Resources to assist with such training and development have been limited for experiential personnel who also have extensive administrative responsibilities.8 The Association convened the Academic–Practice Partnership Initiative (APPI) Summit to Advance Experiential Education in Pharmacy in 2005. A significant APPI benefit for experiential programs has been the PEPSIG Resource Library in which peer-reviewed preceptor development materials have been cataloged and made available to all programs.9
Benefits to the School and the State
The School and the state of Maryland may benefit by linking Academy programming to existing health initiatives such as Healthy People 2010, collaborative practice development, MTM, and smoking cessation. For example, a new MTM certificate program was offered in 2008 to help IPPE community preceptors develop practices that meet the requirements for community APPEs, which are in high demand. Eventually, collaborations initiated with other schools or colleges of pharmacy, such as a regional consortium, may help to conserve limited resources and maximize efficiencies where preceptors teach for multiple schools.
Limitations
Continuing education program evaluations have been thoroughly analyzed for program content development. Also, student evaluations, required for all courses, are a significant source of information for planning programs, both for lectures and workshop activities. In response to preceptors' suggestions and feedback, the ELC has provided live and recorded development programs on a variety of topics. Despite these efforts, the School has been able to achieve only 47% participation in School-sponsored programs. Only 1 preceptor attended a live training session and completed the CD-ROM modules, which leads us to conclude that both methods are needed. Many preceptors who have served since the ELP was initiated in the 1970s may not see the need for training. Also, there is now a variety of national association programs for preceptor training, but schools cannot easily access documentation of completion of other programs.
Some preceptors have decided not to accept reappointment because of the additional training requirements. In fact, in commenting on the Academy of Preceptors and the increased emphasis on training, one preceptor stated, “You take yourselves too seriously.” When preceptors did not return July 2007 reappointment letters, they were contacted as part of a quality review. Several indicated they could not meet the training deadline, which had been extended upon request. These comments and others cause serious concerns about sufficient numbers of academically oriented and effectively trained preceptors in the Academy, especially as the School is increasing enrollment.
Strategies to increase participation in development activities include offering more live sessions in a variety of locations across the state and collaborating with neighboring programs. The ELP is working with specific stakeholders to host training programs. New technology procured for the second campus may be deployed to record live sessions for Internet-savvy preceptors to view at any time. Also, preceptor development from national pharmacy meetings or programs could be better documented to meet training requirements; however, these programs do not obviate the need for School-specific orientation to the curriculum and policies. To offset any perception of unnecessary work or unreasonable expectations, it will be increasingly important to clarify for preceptors the basis for these development requirements.
CONCLUSIONS
The Academy of Preceptors has become a named and valued entity in the School. All 4 goals are being met, although documentation of training is not complete. As more regional schools and colleges collaborate for preceptor development and as more national training programs are disseminated, improved methods of documenting training will be needed. Emphasis will be placed on training new preceptors and offering advanced programs for experienced preceptors.
As the increasing number of schools and colleges of pharmacy prepare more students for more IPPEs and APPEs, preceptors will remain an important focus in experiential education. All will need not only basic orientation, but more importantly, ongoing development of teaching skills in experiential pharmacy education. Preceptors need resources, mentoring, and promotion opportunities, but they also deserve respect and recognition as the Academy of Preceptors. The Academy concept should be explored by the AACP. In particular, the Academy may assist schools and colleges in revising curricula or even providing didactic teaching when specific expertise does not exist among existing faculty members. In addition, preceptors—who provide 30% of pharmacy education—should be invited to join the AACP and participate in governance and policy development.
Meanwhile schools and colleges will need to promote efficiency to meet or exceed the current ACPE accreditation standards and to train and develop a growing number of preceptors. Standardization remains a recurring theme in national experiential programs/conferences/meetings.9 Regional experiential consortia are aligning calendars especially for APPEs, sharing site visitation tools, jointly conducting preceptor programs, and collaborating on assessments as part of the standardization trend. This trend may culminate in a national preceptor credential or certificate and possibly an ambitious mechanism by which pharmacy practice experiences could be matched from a national pool of credentialed preceptors.
Appendix 1. Preceptor Promotion Mentor Plan
Preceptor Promotion Mentor Plan
July 1, 2007
The goal of the Preceptor Promotion Mentor Plan is to develop and implement a “more proactive approach to the promotion of clinical volunteer faculty” as identified in the 2006 ACPE Self-Study Task Force recommendations (Standards for Faculty). The following administrative process is established to mentor and evaluate potential promotion candidates prior to submission to the Faculty Affairs Committee (FAC).
Timeline
Annually by June 1st, preceptors and coursemasters will be notified that nominations are open for clinical faculty promotions. Nominations may be made as a self-nomination from the preceptor or by faculty, especially experiential coursemasters. Interested preceptors will be directed to review the Clinical Track Faculty Appointment and Promotion Policies and Procedures (Rev. 4-9-07) and the Non-tenure Track CV Format (Rev. 11-19-01) which are available on the faculty development website at:. http://www2.pharmacy.umaryland.edu/faculty/development/index.html Candidates for promotion must submit a letter of intent for promotion to the Experiential Learning Program (ELP) Director or Department of Pharmacy Practice and Science (PPS) Chair by July 1st.
Identification of Nominees for Promotion
In addition to the self-nominations and nominations from faculty, the ELP Director and PPS Chair will identify suitable nominees.
Preliminary Review
Initially the PPS Chair and ELP Director will review nominees' information, including teaching documentation from ELP preceptor files. For those preceptors for whom promotion is recommended, letters of support may be solicited from the appropriate coursemaster(s) and peers, in addition to the letters from the ELP Director and PPS Chair. For those preceptors not yet prepared for promotion, a letter will be sent with specific suggestions for improvement. The FAC Chair, or his/her FAC designee, may be consulted to provide input during the preliminary review process. New preceptor applications will be reviewed upon submission for appropriate appointment rank.
Preceptor Resources
Those preceptors who have been promoted to clinical associate professor and clinical professor will be asked for their willingness to mentor nominees for promotion. Specific faculty may also be asked to mentor preceptors during the process.
Recommendation
The ELP Director or PPS Chair will forward all applicable materials to the FAC for review, preferably during the summer. Following FAC review, a recommendation letter will be provided to the Dean.
Recognition
Preceptors who are successfully promoted will be notified by letter and will receive a certificate. Promotions will be publicized through a variety of School media such as publications, web announcements, and the Academy of Preceptors.
Appendix 2. Live Continuing Education Sessions for University of Maryland School of Pharmacy Preceptors
REFERENCES
- 1.Boyle CJ, Carr-Lopez S, Kawahara NE, Kieser MA, See CJ, Smith GB. Report of the Preceptor Development Task Force Subcommittee Two. Am J Pharm Educ. 2002;66(4):42S–43S. [Google Scholar]
- 2.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree Adopted January 15, 2006.http://www.acpe-accredit.org/standards. Accessed March 20, 2009.
- 3.Experiential Learning Program Courses. http://www.pharmacy.umaryland.edu/elp Accessed March 20, 2009.
- 4.Boyle CJ, Beardsley RS, Morgan JA, et al. Professionalism: a determining factor in experiential learning. Am J Pharm Educ. 2007;7(2) doi: 10.5688/aj710231. Article 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preceptor of the Year Nomination Form. http://www2.pharmacy.umaryland.edu/administration/elp/forms.html Accessed March 20, 2009
- 6.Ried LD, Nemire R, Doty R, Brickler MP, Anderson HH, Frenzel-Shepherd E, Larose-Pierre M, Dugan D. An automated competency-based student performance assessment program for advanced pharmacy practice experiential programs. Am J Pharm Educ. 2007;71(6) doi: 10.5688/aj7106128. Article 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuellar LM, Ginsburg DB, editors. Preceptor's Handbook for Pharmacists. Bethesda, Maryland: American Society of Health-System Pharmacists; 2005. [Google Scholar]
- 8.Reynolds JR, Briceland LL, Carter JT, et al. Experiential education delivery- ensuring success through support and development of the faculty and administrative team: Report of the 2004-2005 Professional Affairs Committee. Am J Pharm Educ. 2005;69(5) Article S9. [Google Scholar]
- 9.Academic-Practice Partnership Initiative. Professional experience program resource library. http://www.aacp.org/resources/education/appi. Accessed March 20, 2009.