Abstract
Objective
To implement an active-learning methodology for teaching diabetes care to pharmacy students and evaluate its effectiveness.
Design
Laboratory instruction was divided into 4 primary areas of diabetes care, referred to by the mnemonic, the 4 M's: meal planning, motion, medication, and monitoring. Students participated in skill-based learning laboratory stations and in simulated patient experiences. A pretest, retrospective pretest, and posttest were administered to measure improvements in students' knowledge about diabetes and confidence in providing care to diabetes patients.
Assessment
Students knowledge of and confidence in each area assessed improved. Students enjoyed the laboratory session and felt it contributed to their learning.
Conclusion
An active-learning approach to teaching diabetes care allowed students to experience aspects of the disease from the patient's perspective. This approach will be incorporated in other content areas.
Keywords: diabetes, active-learning techniques, practice laboratory
INTRODUCTION
Diabetes affects almost 24 million children and adults, or approximately 8% of the US population. While almost 18 million of those people have been diagnosed, nearly a third remain undiagnosed.1-3 Furthermore, there are 57 million people in the United States who have blood glucose levels that are higher than normal, a condition often referred to as “pre-diabetic.”1,4 Both genetics and environmental factors, such as lack of exercise, poor dietary habits, and resultant obesity, play important roles in the development of the disease. Through appropriate education and management, it is possible to delay complications or even prevent some cases of type 2 diabetes, which accounts for over 90% of diagnosed cases.1,5
Pathophysiology, diagnostic methods, and treatment modalities are often taught to pharmacy students through traditional classroom lectures, but more diabetes educators are realizing the importance of pharmacy students gaining hands-on experience with the vast array of new diagnostic and monitoring devices and the benefits of using new patient instruction techniques.6-9 By instructing simulated patients, students can develop an understanding of adherence issues and an empathetic attitude toward the difficulties involved in managing the disease. The laboratory setting is ideal for providing students with hands-on experience in a low-risk environment, there by instilling both confidence and competence before students assist actual patients in practice settings.
The 2007 Accreditation Council for Pharmacy Education (ACPE) Standards and Guidelines address the need for active-learning techniques in every phase of pharmacy students' education and in pharmacists' continuing professional development.10 Active-learning techniques can effectively bridge the gap between licensure and actual patient experience. Hands-on skill-based training empowers pharmacists to develop medication therapy management skills, potentially resulting in transformation of practice.11
As the practice of pharmacy progresses towards its vision of pharmaceutical care, students should be taught and encouraged to provide these patient-care--centered services.10,11
In addition to mastering diabetes curricular content and skill-based training, students should develop empathy for their patients. Part of a pharmacist's responsibility is to be an effective communicator and compassionately respond to what the patient is experiencing.12,13 Empathy is a component of effective communication.14-16 In relation to diabetes care, students who have never injected themselves or monitored their blood glucose often find it difficult to effectively deal with the fears and anxieties of diabetes patients.
At Purdue University, second-year pharmacy students receive didactic instruction on the management of diabetes through a series of lectures and multimedia demonstrations. Upon completion of the didactic portion of the diabetes curriculum, students participate in a hands-on, skill-based laboratory that uses a variety of communication simulations, calculations, self-injection and monitoring techniques, and Web-based instruction. A comprehensive written examination follows completion of the laboratory experience to ensure that students understand the pathophysiology, methods of prevention, treatment, and monitoring of diabetes. The laboratory experience described below involved 157 pharmacy students who were assigned to 1 of 5 laboratory sections, with approximately 32 students in each laboratory section. One 3-hour laboratory section was scheduled each day of the week. The goal of the laboratory was to increase pharmacy students' competency and confidence in primary areas of diabetes care (the 4 Ms): meal planning, motion (exercise), monitoring, and medication. This training would serve as a basis for provision of medication therapy management services to improve patient outcomes.
Two faculty members at Purdue University, including a certified diabetes educator and the introductory pharmacy practice experience (IPPE) director, designed the active-learning laboratory and implemented the new approach. Additional faculty members, a Purdue pharmacy resident with Type 1 diabetes, and pharmacy students who had completed advanced pharmacy practice experiences (APPEs) in diabetes care also provided input on the laboratory content. Each individual's expertise was used in formulating the new design. The following description illustrates the instructional approach and assessment methods used.
DESIGN
After reviewing a variety of teaching and learning methods, the instructors delineated skill-based learning into 4 basic areas and developed a mnemonic device, “The 4 Ms,” (which stands for meal planning, motion, medication, and monitoring) based on methodology endorsed by Bartol.17-19 Not all pharmacists are diabetes care specialists, but pharmacists must still provide holistic, point-of-care diabetes counseling, and therefore need to have knowledge and skill in the 4 basic areas of care. Laboratory activities were designed to enhance didactic learning and provide progressive skill training, culminating in the higher levels of learning (ie, analysis, synthesis, and evaluation) described in Bloom's taxonomy.20,21
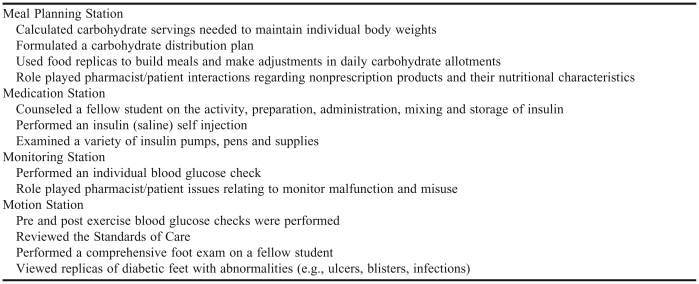
Table 1 outlines the activities performed by students at each laboratory station. Prior to laboratory participation, students were required to read background information pertaining to each laboratory station and view 2 Web-based instructional videos on insulin injection techniques and blood glucose monitoring. Students also were required to complete worksheets on the Web-based instruction. Students were informed in lecture and through e-mail reminders that they would be self-injecting saline solution and performing finger-stick tests to measure their blood glucose. They were asked to wear loose-fitting clothing, eat a light snack before participating in the 3-hour laboratory, and have clean feet in preparation for conducting diabetic foot checks.
Table 1.
Station Activities Conducted in an Active-Learning Laboratory Used to Teach Pharmacy Students the Four M's of Diabetes Care
Approximately 20 minutes of laboratory time was devoted to detailing the objectives and logistics of station-to-station operations. Following prelaboratory instructions, each section of 32 students was divided into 4 random groups of 8 students. Each group of 8 students rotated through one of 4 separate stations every 45 minutes. The evaluation method for this laboratory was approved by the University's Institutional Review Board.
Meal Planning Station
At the meal planning station, the instructor reviewed basic nutritional components of a balanced diet and how to calculate patient-specific nutritional requirements.22,23 The instructor then led discussion on the rationale behind carbohydrate counting, specifically why health care providers focus on carbohydrates as opposed to daily intake of fats and proteins. Students discussed the didactic lecture on how carbohydrates rapidly and effectively raise blood glucose levels.
Students were assigned a carbohydrate counting book and instructed on basic carbohydrate counting rules. A discussion using the carbohydrate counting book helped familiarize students with resources and demonstrated how carbohydrates from vegetables could outnumber those in candy. The instructor and students discussed methodologies of adjusting medications and incorporating exercise in relation to carbohydrate intake. In the first activity, students learned how to count carbohydrates. Although both methods were discussed, the focus of the discussion was on carbohydrate servings rather than counting grams of carbohydrates. Students used their actual body weights, an estimate of their daily energy expenditures, and an adjustment factor to reach ideal body weight to determine servings of carbohydrates needed to reach or maintain their individual body weights. Students determined the distribution of their individual number of carbohydrate servings between meals and snacks and how to make adjustments when needed. Students then formulated a carbohydrate distribution plan for the day based on their personal requirements.
Based on their distribution plans, students were asked to select a meal (breakfast, lunch, or dinner) and were then escorted to a food and drink replica buffet (products obtained from Nasco at www.enasco.com/nutrition, Modesto, CA). Food and drink replicas were identical in weight and potion size to actual food products. Students were instructed to choose foods they would normally eat for the selected meal and to disregard carbohydrate counting. They were then instructed to use a carbohydrate counting book to analyze their meal for carbohydrate content. Electronic scales were available for weighing foods. Next, students were told to assume the role of a patient with diabetes, and based on their carbohydrate calculation, make necessary additions or deletions from their drinks and food plate by changing either the type or the quantity of food. Students were told to adhere to their personally allowed carbohydrate servings determined for the meal selected. The instructor reminded students that patients with diabetes often have co-morbid disease states, such as hypercholesterolemia or hypertension, that further limit their selection of low-carbohydrate foods. After experiencing the complexity and frustration of meal planning, instructors discussed the role of dieticians in diabetes management.
The next exercise at the meal planning station compared nutritional values of widely consumed nonprescription products such as cough syrups, lozenges, and candies, along with their sugar-free counterparts. Students compared number and type of carbohydrates, calorie content, cost per serving, and taste, using information from package labels, cash register receipts, and a food scale. Students paired off for role-playing scenarios that involved a patient with diabetes approaching a pharmacist with a request for a product recommendation. For example, a patient asks a pharmacist: “I have diabetes, but I hate the taste of this sugar-free cough syrup. What do you recommend?” During their role-play exercises, students were required to scientifically defend their recommendations. Peers and the station instructor provided verbal feedback on the students' counseling techniques.
Medication Station
Goals for students working at the medication station included developing an understanding of the physical technique of self-injection, gaining a sense of the diabetes patient's apprehension over self-injection, and developing sensitivity to the experience of the diabetes patient.
Prior to the laboratory, students were instructed to watch an online video about self-injection that covered insulin mixing, proper use of syringes, site selection and preparation, and administration. The instructor reinforced the concepts and demonstrated the techniques presented in the video.
Students paired off for role-playing as patients and pharmacists. In the first simulation, students in patient roles were handed a prescription for an insulin analog, which they presented to their pharmacists. Students in pharmacist roles dispensed the appropriate vial and provided patient education on insulin activity, preparation, administration technique, storage, and other pertinent issues. Upon conclusion of the pharmacist-patient counseling, the faculty instructor observed the patients preparing, withdrawing, and administering the saline by self-injection. Immediate instructor feedback was provided. Students were given the opportunity to self-evaluate their performance. Upon satisfactory performance, the faculty instructor signed the students' worksheets, indicating adequate provision of care to their patients and understanding of correct injection technique.
In the second simulation, students reversed roles. Students in pharmacist roles were required to teach patients how to mix insulin (simulated with saline) in a syringe and how to self-administer the dose. The process and evaluation for the second simulation was the same as reported for the first.
The final activity at this station involved examination of a variety of insulin pens, insulin pumps, and other supplies. A pharmacy practice resident who used an insulin pump demonstrated pump use and answered questions from other students.
Monitoring Station
Prior to laboratory attendance, students viewed an online video of commonly used blood glucose meters. Students then completed a worksheet that outlined aspects of the meters, including relative advantages and disadvantages of each meter, activation and calibration, required blood amounts, capillary action on the strip, reading times, meter sizes, and dexterity issues involving the strips. At the station, the instructor reviewed the worksheets to ensure that students had recorded accurate information. The faculty instructor then verbally quizzed students about blood glucose testing and the appropriate use of lancet devices. Discussion included processes to prepare fingers and hands for testing, appropriate skin sites for using a lancet, alternate testing sites, normal blood glucose ranges and goal setting, frequency of monitoring, and Hemoglobin A1c testing. The students then performed a blood glucose test on themselves. The instructor observed the students for appropriate technique.
Students then paired off for role-playing as patients and pharmacists. Scenarios depicting common monitoring issues, including problems with technique or the blood glucose meter, were distributed to the student pairs. Students playing pharmacists resolved the issue by using appropriate questioning techniques with their patients, and then counseled their patients on appropriate use of the meter. The roles were then reversed and a new scenario was provided with an alternative meter.
Motion Station
At the motion station, students and the instructor discussed patient cases as well as benefits of exercise to the patient, such as lowered blood glucose levels, weight loss, decreased insulin resistance, raised high-density lipoprotein (HDL), lower blood pressure, and improved mental health and self-esteem. To demonstrate the impact of exercise on blood glucose, 2 students were selected to jog in place for 10 to 15 minutes. The students' blood glucose were tested before and after jogging. Students and the instructor discussed results from the activity as well as the inherent risks of exercise such as hypoglycemia, foot blisters, injuries such as sprains and strains, cardiac events, and retinal hemorrhage or detachment. Students then taste-tested a variety of blood glucose tablets and gels, and the instructor addressed the appropriate use of these products.
This station's activities began with a review of national standards of medical care with a focus on prevention and management of diabetic complications.24,25 A variety of pictures and photographs were used to demonstrate the types of target organ damage commonly seen with diabetes. Also discussed was the frequency and importance of preventive care such as eye and dental examinations, immunizations, and microalbuniuria screenings.
Another primary focus of discussion involved preventive diabetes foot checks since studies demonstrate the value of student involvement in preventive diabetes foot care evaluations.26 A Nasco Common Foot Problems Display (http://www.enasco.com/product/WA22223HR, Modesto, CA) helped students visualize the variety of foot ailments commonly seen in patients with diabetes. A variety of graphic representations of a diabetic foot (ie, ulcerated tissue, gangrene, amputations, and infections) were distributed to student pairs. Using these pictorials, students completed the Diabetes Foot Screen worksheet (http://www.hrsa.gov/leap/levelonescreening.htm). Students then performed comprehensive foot examinations on one another using monofilaments, alcohol wipes, and latex gloves.
Assessment Methods
Students completed 3 instruments pertaining to the laboratory activities: (1) knowledge of diabetes, (2) confidence in providing diabetes care, and (3) a laboratory evaluation. The knowledge and confidence instruments were completed prior to and after the conclusion of the laboratory activities. The laboratory evaluation was completed at the conclusion of the laboratory activities. The knowledge instrument contained 14 open-ended items and true-or-false questions about diabetes and diabetes management. The maximum score possible was 17 points.
The confidence instrument consisted of 15 items assessing students' perceptions of their confidence in providing diabetes care to patients. For each item, students ranked their confidence on a Likert-type scale with 1 = not at all confident, 2 = not very confident, 3 = moderately confident, 4 = very confident, and 5 = extremely confident. A retrospective pretest was added to the posttest instrument, which allowed students to evaluate their prelaboratory confidence at the conclusion of the laboratory.
A pretest, retrospective pretest, and posttest design was utilized to determine students' ability to accurately assess their confidence prior to being exposed to skills-based content. On a pretest, students sometimes are unable to determine what they do not know and cannot accurately assess themselves. The retrospective pretest also asks students to assess what they did not know at the beginning of the laboratory, but since the laboratory activities have taken place, students are better able to identify what they did not know.
Students also completed a laboratory evaluation at the conclusion of the laboratory. The laboratory evaluation consisted of 10 items, using a Likert scale with 1 = strongly disagree, 3 = undecided, and 5 = strongly agree. In addition, students were asked to rate the laboratory as excellent, good, fair, poor, or very poor. Students also were asked to comment on what they liked and disliked about the laboratory.
Descriptive statistics were calculated for all instruments. An a priori level of significance was established at α = 0.05. Student responses were linked for all comparisons using a student identifier. A paired t test was performed to compare overall pretest and posttest scores on the knowledge instrument. Wilcoxon sign-ranked test was used to determine statistical significance between pretest and posttest answers for individual questions on the knowledge instrument. Repeated measures ANOVA was performed to compare the pretest, retrospective pretest, and posttest responses on the confidence questionnaire. The Greenhouse Geisser correction was used when the assumption of sphericity was violated for repeated measures ANOVA.27 Bonferroni post hoc comparisons were conducted when statistical significance was detected in the repeated measures ANOVA.
ASSESSMENT
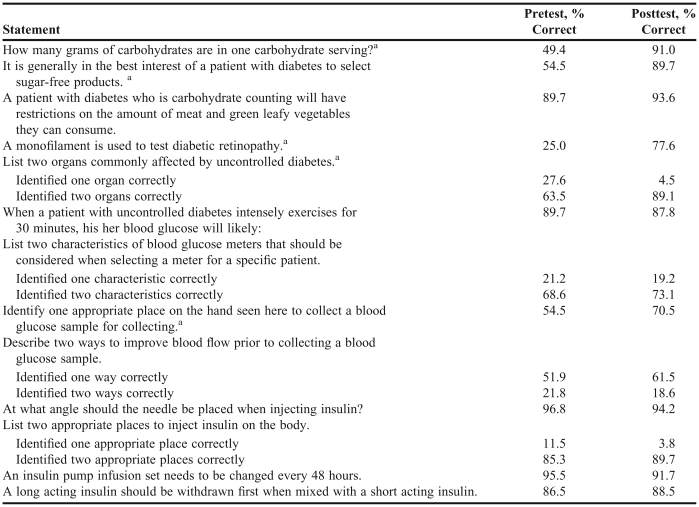
Of the 157 students, 155 completed the knowledge assessment. The results of the knowledge assessment are reported in Table 2. The mean score for the pretest was 12.3 ± 2.7 and for the posttest was 14.2 ± 3.5, which was statistically different (t = 5.79, p < 0.01. The following items were determined to be significant between pretest and posttest scores: (1) How many grams of carbohydrates are in 1 carbohydrate serving? (49.4% vs. 91%, p < 0.01); (2) It is generally in the best interest of the patient to select sugar-free products (54.5% vs. 89.7%, p < 0.01); (3) A monofilament is used to test diabetic retinopathy (25% vs. 77.6%, p < 0.01); (4) List 2 organs commonly affected by uncontrolled diabetes (63.5% vs. 89.1%, p = 0.00); and (5) Identify 1 appropriate place on the hand seen here to collect a blood glucose sample for testing (54.5% vs. 70.5%, p = 0.001).
Table 2.
Pharmacy Students' Knowledge of Diabetes Care Assessed Before and After Completing an Active-Learning Laboratory on the Four M's of Diabetes Care, N = 155
a Pretest vs. posttest scores, p < 0.01
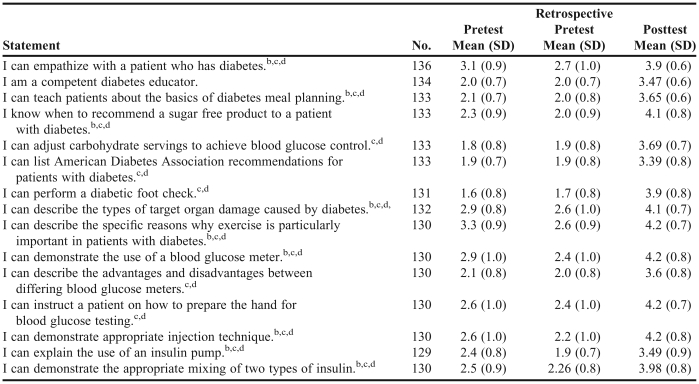
Not all students completed all 3 components (pretest, retrospective pretest, and posttest) of the confidence assessment (Table 3). The score for every item on the confidence instrument was significant, with improved confidence found between pretest and posttest scores. Significant declines in confidence also were seen between pretest and retrospective pretest scores except for the following items: (1) I am a competent diabetes educator, (2) I can adjust carbohydrate servings to achieve blood glucose control, (3) I can list the American Diabetes Association's recommendations for patients with diabetes, (4) I can perform a diabetes foot check, (5) I can describe the advantages and disadvantages between differing blood glucose meters, and (6) I can instruct a patient on how to prepare the hand for blood glucose testing.
Table 3.
Students' Confidence in Providing Diabetes Care Before and After Completing an Active-Learning Laboratory on the Four M's of Diabetes Care a
Rating scale used: 1 = not at all confident, 2 = not very confident, 3 = moderately confident, 4 = very confident, and 5 = extremely confident
b Pretest vs. retrospective pretest, p < 0.05
c Pretest vs. posttest, p < 0.01
d Retrospective pretest vs. posttest, p < 0.01
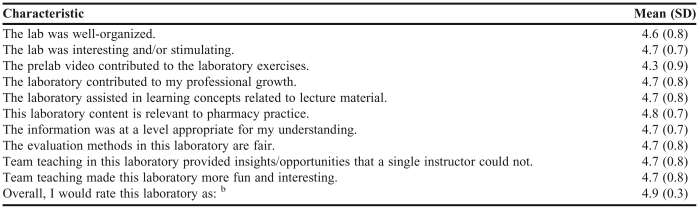
The laboratory evaluation was completed by 143 students (Table 4). The students indicated that the laboratory experience contributed to their learning (4.7 ± 0.8) and was relevant to pharmacy practice (4.8 ± 0.7). In addition, the students rated their overall laboratory experience positively with a mean of 4.9 ± 0.3.
Table 4.
Evaluation of an Active-Learning Laboratory Used to Teach Pharmacy Students the Four M's of Diabetes Care , N = 143a
Rating scale used: 1 = strongly disagree, 2 = disagree, 3 = undecided, 4 = agree, and 5 = strongly agree
b Rating scale used: 1 = very poor, 2 = poor, 3 = fair, 4 = good, and 5 = excellent
Prior to the laboratory, the instructors requested that an assessment of the laboratory instructional techniques be performed by the University's Center for Instructional Excellence (CIE). The CIE evaluator stated that (1) the laboratory instructors provided a friendly, informal atmosphere, essential to this type of laboratory; (2) instruction was personalized, with students in close proximity to the instructor; (3) the level of instruction was uniformly excellent; (4) the students were involved and enjoyed the activities; (5) the use of props made each lesson more effective; and (6) the hands-on activities engaged students at a level as close as possible to real experiences with patients.
DISCUSSION
The purpose of this manuscript was to describe a unique instructional approach based on active-learning methodology when teaching diabetes care to pharmacy students. In addition, students' attitudes pertaining to the instructional approach were evaluated. The primary laboratory goals were to increase pharmacy students' competence and confidence with patient care skills within 4 primary areas of diabetes care (the 4 Ms): meal planning, motion (exercise), monitoring, and medication. Evidence exists that the addition of active-learning strategies greatly enhances the understanding of didactic material provided through lectures, as well as students' ability to retain information and apply it to real-life situations. 28,29 Since this approach was not compared to a traditional teaching methodology, it cannot be determined whether it is the superior approach to teaching this material.
By incorporating active-learning techniques through a series of transitional experiences, students are better prepared to provide diabetes medication therapy management services to their patients. The hands-on activities appeared to be effective, since the students' knowledge increased in areas that were specific to these activities. Overall, the students' confidence in providing care to diabetes patients improved. Their overall empathy for patients with diabetes also improved, suggesting they gained a better understanding of what a patient with diabetes faces (eg, blood glucose testing, self-injection, meal planning, and conducting foot checks). Students' confidence scores could be considered conservative, with many of the mean responses in the moderately confident range. Students, however, may have recognized that this laboratory was a first step in learning. The difference in the pretest and retrospective pretest scores indicated that students reassessed their abilities to provide this type of patient care. Students seemed to realize that more learning and practice was needed before becoming totally confident in providing diabetes management services. Many advanced experiences involve diabetes management care with preceptor supervision, which provides students with additional experiences before becoming independent providers.30 The laboratory activities improved students' confidence in their diabetes care skills and therefore prepared them for these APPE activities.
Using a pretest, retrospective pretest, and posttest methodology appeared to be effective in assessing students' confidence in their diabetes care skills. For some items, students appeared to overestimate their abilities on the pretest. On further evaluation, however, students recognized that they did not know as much as they thought they did before coming to the laboratory. This is evidenced by students' lower confidence ratings on the retrospective pretest. Accurately reflecting on abilities is an essential part of becoming a health care professional. Having students evaluate themselves prior to and at the conclusion of a laboratory experience helps students learn to assess their abilities and confidence in future activities.
Beyond the effectiveness of meeting educational goals, the students appeared to enjoy the hands-on activities in the laboratory. They indicated that their laboratory activities were stimulating and at a level appropriate for their understanding. In addition, the students appreciated the team teaching/station-based approach, and agreed that insights from activities at the stations were beyond what a single instructor could provide and made the laboratory more fun and interesting.
Student comments revealed several limitations in learning that will be addressed in future laboratories. For example, students noted that one 3-hour laboratory seemed insufficient to provide the skills training necessary in all 4 aspects of diabetes care. When under time constraints, it is imperative for instructors to carefully examine content to determine what could be taught as effectively in a traditional lecture format instead of individualized hands-on instruction in small groups. Several small content areas were identified that could be omitted or provided in lecture or through Web-based training prior to the laboratory.31 Adding an additional laboratory section would necessitate an increased teaching load for current instructors, the addition of other qualified instructors, and adjustment of an already full curriculum.
Faculty Observations for Improvement
Students performed skills at each station, sometimes in pairs and sometimes on an individual basis. The station instructor provided feedback and suggested changes to improve the students' performance. Students were required to repeat the exercise until proficiency was attained. An improvement to the laboratory might be the use of an observed structured clinical examination (OSCE) to measure application of content.32
The addition of an IPPE could help students become more empathetic with patients and improve their skills in injection and blood glucose monitoring. While “living the life” of a diabetic patient for several days, students in the IPPE would be required to self-inject insulin (simulated with saline), take medications (simulated with placebos) on a scheduled basis, monitor their blood glucose several times per day, count their carbohydrates while adhering to a patient-specific diet, and exercise daily. “Living the life” of a patient with diabetes would help students become problem-solvers and providers of holistic diabetes care. Similar learning activities could be extrapolated to a variety of difficult-to-manage disease states.
Another appropriate addition to the laboratory could be a station termed “motivation,” such as that described by Bartol.17 In order for patients with diabetes to assume control of care for their disease, self-motivation to comply with medical guidelines is essential. Bartol discusses motivation and compliance as communication issues and explains how health care providers should deliver information in manageable pieces over several patient visits: “If you (the provider) are doing more than 5% of the work to manage a patient's diabetes, the patient isn't pulling his share of the workload.”17 A simulated patient could be utilized at the laboratory station to encourage students to address motivational and behavioral issues that go beyond those addressed in a typical medication counseling session.
SUMMARY
Overall, students were positive in their evaluations of instructional content and methods. Over 90% of the students strongly agreed that the laboratory was interesting, helped them learn key concepts presented in lectures, and would help them apply skills in the “real” world. Students improved in their confidence and knowledge of diabetes care. Aspects of this teaching method will be incorporated into other content areas.
REFERENCES
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates of diabetes in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services. http://www.cdc.gov/diabetes/pubs/factsheet07.htm. Accessed March 2, 2009.
- 2.American Diabetes Association. Diabetes statistics. Last updated May 17, 2007. http://diabetes.org/diabetes-statistics.jsp. Accessed January 14, 2009.
- 3.National Diabetes Information Clearinghouse. National diabetes statistics. Last updated 2007. http://diabetes.niddk.nih.gov/dm/pubs/statistics/. Accessed January 14, 2009.
- 4.American Diabetes Association. All about diabetes. Last updated May 15, 2007. http://www.diabetes.org/about-diabetes.jsp. Accessed January 14, 2009.
- 5.Ohio State University Medical Center. Statistics about diabetes. Last updated 2007. http://medicalcenter.osu.edu. Accessed February 19, 2009.
- 6.Johnson JF, Chesnut RJ, Tice BP. An advanced diabetes care course as a component of a diabetes concentration. Am J Pharm Educ. 2003;67(1) Article 21. [Google Scholar]
- 7.Odegard PS. A diabetes education program for pharmacy students. Am J Pharm Educ. 2002;66:391–5. [Google Scholar]
- 8.Shane-McWhorter L, Oderda GM. Providing diabetes education and care to underserved patients in a collaborative practice at a Utah community health center. Pharmacotherapy. 2005;25:96–109. doi: 10.1592/phco.25.1.96.55623. [DOI] [PubMed] [Google Scholar]
- 9.Koda-Kimble MA, Batz FR. Diabetes care as an active learning model of postgraduate education and training for pharmaceutical care. Am J Pharm Educ. 1994;58:382–5. [Google Scholar]
- 10.Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Accreditation Council for Pharmacy Education. Effective July 1, 2007. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed January 14, 2009.
- 11.American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education (CAPE), Educational Outcomes 2004. Adopted 1994; revised 2004. http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE2004.pdf. Accessed January 14, 2009.
- 12.Professional outcome ability goals. Purdue University School of Pharmacy and Pharmaceutical Sciences. Adopted April 1993; revised May 2007.
- 13.Beardsley RS. Communication skills development in colleges of pharmacy. Am J Pharm Educ. 2001;65:307–14. [Google Scholar]
- 14.O'Keefe M, Sawyer M, Roberton D. Medical students taking the role of the mother in paediatric interview evaluation. Med Educ. 2004;38:294–301. doi: 10.1111/j.1365-2923.2004.01768.x. [DOI] [PubMed] [Google Scholar]
- 15.Lust E, Moore FC. Emotional intelligence instruction in a pharmacy communications course. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700106. Article 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evans S, Lombardo M, Belgeri M, et al. The geriatric medication game in pharmacy education. Am J Pharm Educ. 2005;69(3) Article 46. [Google Scholar]
- 17.Bartol T. How do I get them to do what they're supposed to do? Program and abstracts of the 6th American College of Nurse Practitioners National Clinical Symposium; October 20-24, 2004; Philadephia, Pennsylvania. Session T6. [Google Scholar]
- 18.Exubera Official Site. Managing diabetes. February 2006. http://www.exubera.com. Accessed February 19, 2009.
- 19.Bartol T. Putting a patient with diabetes in the driver's seat. Nursing. 2002;32(2):53–55. doi: 10.1097/00152193-200202000-00052. [DOI] [PubMed] [Google Scholar]
- 20.Forehand M. (2005) Bloom's taxonomy: Original and revised. In M Orey,ed, Emerging perspectives on learning, teaching, and technology. http://www.coe.uga.edu/epltt/bloom.htm. Accessed January14, 2009.
- 21.Krathwohl D. A revision of bloom's taxonomy: an overview. Theory Pract. 2002;41(4):212–8. [Google Scholar]
- 22.U.S. Department of Health and Human Services and U.S. Department of Agriculture. 6th Edition. Washington, DC: U.S. Government Printing Office; Dietary guidelines for Americans, 2005. January 2005. [Google Scholar]
- 23.United States Department of Agriculture. MyPyramid.gov. Last updated May 17, 2007. http://www.mypyramid.gov/. Accessed January 14, 2009.
- 24.American Diabetes Association. Standards of medical care in diabetes-2006. Diabetes Care. 2006;(Suppl 1):S4–42. 29. [PubMed] [Google Scholar]
- 25.Martin C, Daly A, McWhorter LS, et al. American Association of Diabetes Educators. The scope of practice, standards of practice, and standards of professional performance for diabetes educators. Diabetes Educ. 2005;31:487–512. doi: 10.1177/0145721705279719. [DOI] [PubMed] [Google Scholar]
- 26.Sifuentes F, Chang L, Nieman LZ, et al. Evaluating a diabetes foot care program in a preceptorship for medical students. Diabetes Educ. 2002;28(6):930–7. doi: 10.1177/014572170202800608. [DOI] [PubMed] [Google Scholar]
- 27.Field A. Discovering Statistics Using SPSS for Windows. London: Sage Publications; 2004. pp. 326–358. [Google Scholar]
- 28.Lo C. Integrating nutrition as a theme throughout the medical school curriculum. Am J Clin Nutr. 2000;72(3):882s–9s. doi: 10.1093/ajcn/72.3.882s. [DOI] [PubMed] [Google Scholar]
- 29.Faro B, Ingersoll G, Fiore H, et al. Improving students' diabetes management through school-based diabetes care. J Pediatr Health Care. 2005;19(5):301–8. doi: 10.1016/j.pedhc.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Condren M. Diabetes camp as an experiential clerkship site. Am J Pharm Educ. 2003;67(4) Article 119. [Google Scholar]
- 31.Buchowski MS, Plaisted C, Fort J, et al. Computer-assisted teaching of nutritional anemias and diabetes to first-year medical students. Am J Clin Nutr. 2002;75(1):154–61. doi: 10.1093/ajcn/75.1.154. [DOI] [PubMed] [Google Scholar]
- 32.Austin Z, Marini A, Tabak D. Toronto, Canada: Leslie Dan Faculty of Pharmacy, University of Toronto; OSCE-ology Workshop. June 14-16, 2006. [Google Scholar]