Abstract
Objective
To assess the effectiveness of a single educational intervention, followed by patient education training, in pharmacists retaining their inhaler technique skills.
Methods
A convenience sample of 31 pharmacists attended an educational workshop and their inhaler techniques were assessed. Those randomly assigned to the active group were trained to assess and teach correct Turbuhaler and Diskus inhaler techniques to patients and provided with patient education tools to use in their pharmacies during a 6-month study. Control pharmacists delivered standard care. All pharmacists were reassessed 2 years after initial training.
Results
Thirty-one pharmacists participated in the study. At the initial assessment, few pharmacists demonstrated correct technique (Turbuhaler:13%, Diskus:6%). All pharmacists in the active group demonstrated correct technique following training. Two years later, pharmacists in the active group demonstrated significantly better inhaler technique than pharmacists in the control group (p < 0.05) for Turbuhaler and Diskus (83% vs.11%; 75% vs.11%, respectively).
Conclusion
Providing community pharmacists with effective patient education tools and encouraging their involvement in educating patients may contribute to pharmacists maintaining their competence in correct inhaler technique long-term.
Keywords: community pharmacists, dry powder inhalers, asthma, education
INTRODUCTION
Poor inhaler technique is a major problem in managing asthma because the patient does not receive an optimal dose of the prescribed drug, resulting in reduced response to treatment and poor asthma control.1,2
Community pharmacists have become more active in patient care, and the benefits of pharmacists counseling patients about medications have been recognized.3 Pharmacists are in an excellent position to identify patients whose asthma may not be well controlled due to poor inhalation technique.4,5 Pharmacists are the last link in the therapy chain prior to the patients' self-administration of inhalation therapy and therefore have an obligation to their patients to ensure they are using their inhalers correctly. However, many pharmacists lack the skills needed to adequately demonstrate correct inhaler technique.6,7 This has been found to be true even with dry powder inhaler devices, which are easier to use than pressurized metered dose inhalers (pMDIs).8,9
Patients using inhalation therapies need careful instruction, including step-by-step demonstration and observation of their technique when dispensing the medication.5,10 In addition, inhaler technique tends to decline without routine review, highlighting the importance of periodic follow-up and reinstruction.11 Pharmacists are available not just when patients obtain their first inhaler, but also when they obtain refill inhalers, giving pharmacists the ideal opportunity to assess and educate their patients on an ongoing basis regarding correct inhaler technique.
However, most patients are rarely assessed or educated by community pharmacists on inhaler administration technique.10,12 This could be due partly to a lack of knowledge and skills by pharmacists in this subject, affecting their confidence and willingness to perform inhaler technique education.6,13 Hence, ensuring that pharmacists are able to demonstrate correct inhaler technique is crucial as a first step towards correcting patients' inhaler technique and achieving optimal asthma management.
We previously reported a study in which we developed, implemented, and evaluated the effectiveness of a model by which community pharmacists could improve patients' inhaler technique. The objectives of the present study were to evaluate the short- and long-term effects of this model on the participating pharmacists' own inhaler technique demonstration skills.
METHODS
Approval for this study was obtained from the University of Sydney Human Ethics Committee. The study of pharmacists' inhaler technique skills was carried out over 6 months in conjunction with a randomized controlled study which investigated the effect on clinical and humanistic outcomes of an educational intervention on dry powder inhaler technique delivered by community pharmacists to patients with asthma.14,15 The first phase of the study involved the development and implementation of an educational workshop for pharmacists on inhaler technique education conducted in Sydney University, Faculty of Pharmacy in April 2003.
A convenience sample of 120 registered community pharmacists was identified from the Sydney metropolitan area and contacted by telephone. Pharmacists were excluded if they were involved in another clinical study or were not able to complete the study, or if a pharmacist assistant would not be present in the pharmacy at all times to allow the pharmacist to deliver the intervention to patients without interruptions.
Those selected were randomly allocated to active or control groups using a computer-generated list and asked to give informed written consent for participation.
All participants attended 1 evening workshop which lasted 3 hours for pharmacists in the active group and 2 hours for pharmacists in the control group. At the beginning of the workshop, all participants completed a questionnaire on demographic characteristics, including years in practice as a community pharmacist, location of pharmacy, source of education and years since most recent education on peak flow meters (PFM), Turbuhaler, and Diskus.
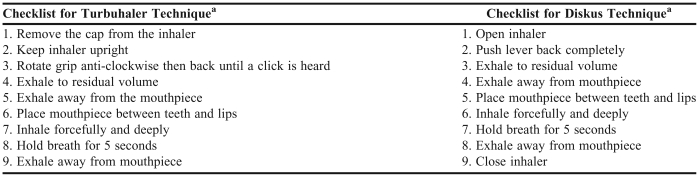
The educational workshop was designed to provide the skills which pharmacists would need for their participation in the randomized controlled follow-up study.14,15 During the workshop, which was based on comprehensive consideration of adult learning principles, all pharmacists received initial training covering basic asthma management, inhaled medications, and PFM technique, each delivered by appropriate experts. After the educational session, pharmacists were assessed on PFM technique on a scale of 0-11 (scoring checklist available from the corresponding author upon request). All pharmacists were assessed on Turbuhaler and Diskus technique using placebo inhaler devices; however, no feedback was given. Turbuhaler and Diskus inhaler techniques were assessed using previously published checklists for scoring (Table 1), each on a scale of 0-9.10,16 For each device, 1 researcher assessed all pharmacists. Pharmacists in the active and control groups then were separated for the rest of the workshop and advised they would be taught 1 of 2 different ways of managing asthma in the community pharmacy, but blinded to the true nature of the educational interventions.
Table 1.
Technique Checklists Used to Assess the Skills of Community Pharmacists Prior to and After an Educational Intervention
Checklists based on previous published literature.10,16
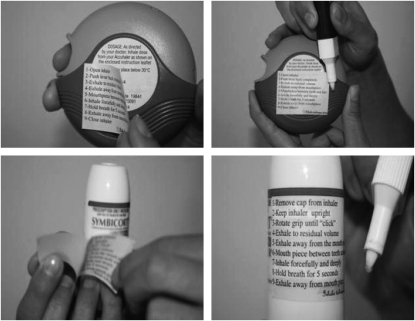
Pharmacists in the control group received training on how to teach PFM technique to patients and on data form completion. Pharmacists in the active group received the same training, plus training on how to assess and educate patients on Turbuhaler and Diskus technique. Pharmacists in the active group were reassessed on their Turbuhaler and Diskus technique post-education, and any problems were corrected before patient recruitment commenced. Pharmacists in the active group were provided with data collection forms and study materials. These included patient-centered educational tools for inhaler technique education,15 including checklists for assessing technique and novel “inhaler technique labels” (Figure 1), which were preprinted along with the relevant checklists (Table 1). Pharmacists in the control group were not provided with any education about Turbuhaler and Diskus technique.
Figure 1.
Inhaler Technique Labels. At each visit, the Inhaler Technique Label was highlighted by the pharmacists with any steps which the patient performed incorrectly at initial assessment at that visit.
After the workshop, pharmacists in both the active and control groups recruited customers with asthma who were using Turbuhaler or Diskus. Patients were asked to come back to the pharmacy on a monthly basis for 3 months following a baseline visit, and for 1 last visit 6 months after study began. These visits were not linked to scheduled medication refills. At each visit, pharmacists in the active group assessed and educated their patients on correct inhaler technique using the inhaler technique checklists provided to them. A highlighter pen was used on the inhaler technique labels (Figure 1) to identify any incorrect steps demonstrated by the patients on the first assessment. Patients were educated using a “show and tell” inhaler technique counseling method, which was repeated up to 3 times if necessary.10 At the completion of counseling, the pharmacist attached the highlighted inhaler technique label to the patient's controller inhaler (not the box), without covering any essential information printed on the inhaler device.
At each subsequent patient visit, a similar process was followed, and a new inhaler technique label was placed on the patient's replacement inhaler (or on the old one if still in use). If no steps were incorrect on the initial assessment at any visit, the label was attached to the patient's inhaler with no highlighting. Pharmacists in the control group only taught their patients how to measure and record peak flow.
Pharmacists in the active group were assessed on their Turbuhaler and Diskus technique at 3 and 6 months during the follow-up study using placebo devices. Pharmacists were not informed in advance that they would be assessed. After each assessment, pharmacists were corrected on their inhaler technique if they performed any of the steps incorrectly. Assessments were completed in the counseling area of the pharmacists' own pharmacy. Pharmacists in the control group were not assessed on their inhaler technique during the study. All pharmacists were assessed on their inhaler technique 1 year after all patients completed the follow-up study (2 years from initial training). Inhaler technique assessment was completed using the same checklists used in the initial assessment. One researcher assessed all pharmacists. Pharmacists in the control group were educated on correct inhaler technique following their final assessment.
Statistical Analysis
Sample size determination was based on results obtained from a previous study which showed an improvement in pharmacists' mean inhaler technique scores of 23% ± 19% for the Turbuhaler and 38% ± 20% for the Diskus after receiving education.7 With 80% power, 5% risk of a type I error and a 20% drop out rate, it was determined that 29 pharmacists should be recruited.
Data were analyzed using SPSS (version 12, Chicago, IL). Comparisons between groups were performed by independent sample t test or Wilcoxon signed rank test, and by chi-square test for binary outcome variables. For all statistical analyses, p values of ≤0.05 were considered significant.
RESULTS
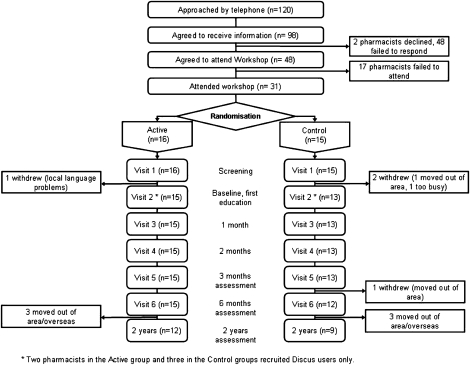
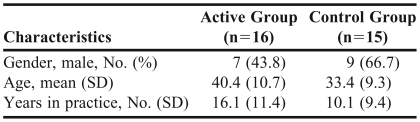
Of the 120 pharmacists invited by telephone to participate in the randomized controlled trial, 98 agreed to receive the information, and 31 (26%) attended the workshop (Figure 2). Sixteen pharmacists were randomized to the active group and 15 to the control group. There were no significant differences between pharmacists in the active and control groups in terms of gender, age, and years in practice (Table 2). There was no significant difference in the proportion of pharmacists practicing in different geographical or socioeconomic locations, with most pharmacies located in shopping areas.
Figure 2.
CONSORT diagram for pharmacists, showing disposition and retention throughout the workshop, followup 6-month study, and 2 years post initial training (educational workshop).
Table 2.
Characteristics of Pharmacists Participating in a Study of Inhaler Technique and Education
Eighty-seven percent of pharmacists reported that they had received past education on PFM, Turbuhaler, and Diskus use; however, the education on using any of these asthma devices was not recent (2 to 4 years). The main source of inhaler technique education had been pharmaceutical industry representatives.
The majority of pharmacists were able to demonstrate correct PFM technique following education, with no significant difference in mean PFM technique scores (out of 11) between the pharmacists in the active and control groups (active: 9.9 ± 0.8; control: 9.5 ± 1.1, p = 0.4, independent sample t test).
At baseline, pharmacists' inhaler technique demonstration skills were poor, with no significant difference in mean inhaler technique scores between the pharmacists in the active and the control groups for either the Turbuhaler or the Diskus (Turbuhaler: 5.6 ± 1.8 vs. 5.5 ± 1.9; Diskus: 5.6 ± 1.8 vs. 5.7 ± 1.1 (p > 0.05, Mann-Whitney test).
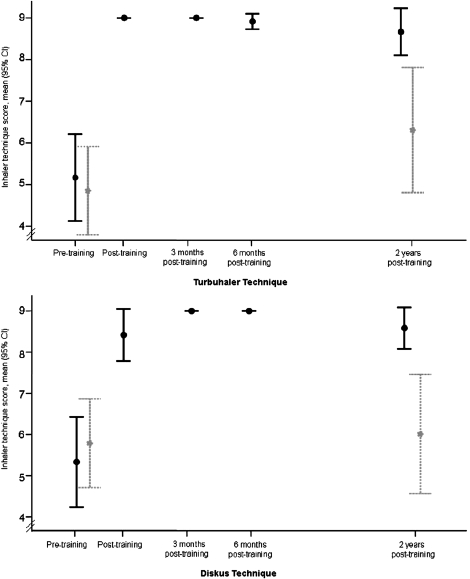
For pharmacists in the active group, inhaler technique scores improved significantly post-education to 9.0 ± 0.0 for the Turbuhaler and 8.6 ± 0.9 for the Diskus (p = 0.001, Wilcoxon signed rank test, for both devices) (Figure 3). Two pharmacists required minor correction in their Diskus technique before patient recruitment commenced. Three pharmacists (1 from the active group and 2 from the control group) withdrew before recruiting any patients. Fifteen pharmacists from the active group and 12 from the control group completed the follow-up 6-month study.
Figure 3.
Mean score of inhaler technique (Turbuhaler and Diskus) for pharmacists in the Active group (n=16) and Control group (n=15), pre and post education in the educational workshop; 3 and 6 months during the follow-up 6-month study, and 2 years post initial training (educational workshop).
During the 6-month follow-up study, a score of 9/9 for both inhalers was maintained by all pharmacists in the active group at 3 months and 6 months (Figure 3), except for 1 pharmacist on Turbuhaler at 6 months (score was 8 because step 4, “exhale to residual volume,” was not demonstrated correctly).
Participating pharmacists recruited 1-5 patients for each type of inhaler. During the course of the study, each of the pharmacists in the active group went through the items on the inhaler technique checklist approximately 15 times per patient for Turbuhaler users, and 12 times per patient for Diskus users (including the initial assessment of inhaler technique at each visit, any required repeats of demonstration and re-checking of technique from later in the study), and then marking faulty steps on the inhaler technique label with a highlighter pen.
One year after the randomized controlled 6-month follow-up study was completed (2 years from initial training), pharmacists in the active group had significantly higher inhaler technique scores (out of 9) than pharmacists in the control group, for both the Turbuhaler and the Diskus (Turbuhaler: active group, 8.7 + 0.9 vs. control group, 6.3 + 1.9; Diskus: active group, 8.6 ± 0.8 vs. control group, 6.0 ± 1.9; p = 0.002, Mann-Whitney test used for all comparisons).
DISCUSSION
Community pharmacists' participation in a workshop followed by provision of repeated inhaler technique education to patients has been shown to result in the long-term optimization of the pharmacists' own inhaler technique skills. As expected from previous studies, the pharmacists' inhaler technique skills were initially corrected by a single brief workshop session based on adult learning principles. In this study, these skills were found to be maintained 2 years later without any further education. Pharmacists' use of patient-centered educational tools when counseling their asthma patients about correct inhaler technique may have served to maintain their own inhaler technique skills on a long-term basis. If confirmed, these findings would have important implications for professional education of pharmacists, in that with appropriate tools, pharmacists can function as effective educators on an ongoing basis without further training. This could potentially magnify the clinical improvements that were observed in the patients whom the pharmacists educated.14,15
This is the first study to show long-term retention of correct inhaler technique by health care professionals after only a brief intervention. Although many studies have shown that health care professionals can be trained to demonstrate the correct use of inhalers correctly, several studies have demonstrated that inhaler technique demonstration skills decline within a few weeks or months after the training/intervention. For example, Resnick and colleagues showed that, of housestaff physicians educated to achieve correct pMDI technique, only 26% had correct technique when reassessed 2 months later.17 In the present study, the training workshop was based on comprehensive consideration of adult learning principles, including didactic presentations, physical demonstrations, hands-on training with inhalers, peer assessment, and immediate feedback.18,19 Nevertheless, even when similar principles were followed in the study by Jackevicius and Chapman, with a 1-hour hands-on workshop leading to an increase in the proportion of hospital pharmacists who could demonstrate correct technique with a Turbuhaler from 0% to 65%, the proportion with correct technique had fallen to 35% after 3 months.20 By contrast, in the present study, correct technique was retained by almost all pharmacists 2 years after a single training workshop.
In view of this previously observed decline in inhaler technique, the development of the present workshop and intervention tools was based on specific educational theory to promote long-term retention of pharmacist skills.18,19 Based on the approach of Pike, a process of “overview, teach and review” was built into the workshop, to help pharmacists retain information longer.19 The work of Pike would also suggest that the more frequently the pharmacists were exposed to the inhaler technique education tools while educating their patients, the more information they would retain,19 and this may have applied in the present study. Although pharmacists attended only 1 evening workshop, and recruited only 1-5 patients for each type of inhaler in the follow-up study, each pharmacist in the active group subsequently went through the items on the inhaler technique checklist many times for both the Turbuhaler users and Diskus users, each time reminding themselves of the correct steps. In addition, anecdotal comments suggested that pharmacists broadened their use of the study methods by educating non-study patients during and after the study, thereby practicing their technique even more and perhaps more effectively maintaining their own skills.15 This suggests that the provision of appropriate training modules and simple education tools to community pharmacists to use in educating their patients may provide a feasible, low-cost, and sustainable way of improving asthma outcomes.
Although more than 80% of the pharmacists reported receiving previous education on inhaler technique, only about 10% of the pharmacists demonstrated correct technique with the Turbuhaler and Diskus prior to the educational portion of the workshop, possibly due to not having any inhaler technique education in the previous 2 to 4 years. Despite the potential for pharmacists to have a positive impact on asthma management,14 previous studies have shown that pharmacists rarely review or educate asthma patients on correct inhaler technique.9,10, 21 Pharmacists' lack of knowledge and skills can be identified as the main reason hindering them from fulfilling their role in asthma management.6,22 More alarming is that pharmacists' own lack of correct inhaler technique may result in the provision of incorrect instructions to patients with asthma. The implication of this problem can be enormous in that asthma patients may continue to use their inhaler devices incorrectly between the time of prescription and the time they complete all their refill inhalers and go back to see their doctor. Because of the resulting lack of symptom control, the patients' doctors may prescribe increased doses of their asthma medication, increasing prescription costs and the potential for side effects.
The educational intervention used for pharmacists in this study was based on the classic “train the trainer” concept. The workshop was run by 4 experts in the field of inhaler technique who first trained the study pharmacists to use the inhalers correctly themselves, and then how to teach correct technique to others. Given that the best outcomes in inhaler technique education arise from a hands-on demonstration,20 a train the trainer approach is an efficient method of education, with a potential impact on a much larger population than could be reached by a few experts.
This study also points to the importance of the source of information to pharmacists on inhaler technique. Pharmacists indicated that prior to the workshop, pharmaceutical representatives were their main source of education on inhaler technique. Information from pharmaceutical companies (either in the form of a package insert or other information supplied) and observation of pharmaceutical representatives are the most common sources of information on inhalers and inhaler technique.6,23,24 We are not aware of any studies examining the inhaler technique skills of pharmaceutical manufacturer representatives, but the present findings suggest that they also may need follow-up education in correct inhaler technique.6,7,9,22
Small sample size and selection bias are the main limitations of this study as only 31 of the 120 pharmacists contacted attended the workshop. Thus, pharmacists who attended the workshop may have been more motivated and had a greater predisposition to learn correct inhaler technique. The low response rate could limit the generalizability of the findings. In addition, the assessments of pharmacists' inhaler technique at 3 and 6 months after the workshop may have reinforced correct techniques. However, the pharmacists in the active group were not told in advance that assessments would take place, and when assessed, only 1 pharmacist needed any correction, suggesting that the follow-up assessments did not significantly contribute to the pharmacists' ability to maintain their correct technique demonstration skills.
CONCLUSION
A single brief workshop on proper inhaler technique following the train-the-trainer approach, and with the provision of effective patient-centered tools to educate patients about correct inhaler technique, resulted in pharmacists maintaining proper technique 2 years later. This approach could provide a feasible, low-cost and sustainable way of maintaining pharmacists' competence in demonstrating correct inhaler technique long-term. This study confirms the findings of many previous studies conducted in different countries6,7,9,22: that many pharmacists and other health care professionals involved in asthma management have poor inhaler technique, and without specific education, they will continue to lack the skills necessary to play an effective role in educating patients about correct inhaler technique.
ACKNOWLEDGMENTS
This study was funded by the Faculty of Pharmacy, University of Sydney. Also, the work of one of the authors, Helen K. Reddel, PhD, was funded by the Asthma Foundation of NSW.
REFERENCES
- 1.Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respir Care. 2005;50:1360–74. [PubMed] [Google Scholar]
- 2.Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J. 2002;19:246–51. doi: 10.1183/09031936.02.00218402. [DOI] [PubMed] [Google Scholar]
- 3.Ballantyne PJ. The role of pharmacists in primary care. BMJ. 2007;334:1066–7. doi: 10.1136/bmj.39213.660394.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ekedahl A. ‘Open-ended questions’ and ‘show-and-tell’–a way to improve pharmacist counselling and patients' handling of their medicines. J Clin Pharm Ther. 1996;21:95–9. doi: 10.1111/j.1365-2710.1996.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 5.Cordina M, McElnay JC, Hughes CM. Assessment of a community pharmacy-based program for patients with asthma. Pharmacotherapy. 2001;21:1196–203. doi: 10.1592/phco.21.15.1196.33894. [DOI] [PubMed] [Google Scholar]
- 6.Kesten S, Zive K, Chapman KR. Pharmacist knowledge and ability to use inhaled medication delivery systems. Chest. 1993;104:1737–42. doi: 10.1378/chest.104.6.1737. [DOI] [PubMed] [Google Scholar]
- 7.Cain WT, Cable G, Oppenheimer JJ. The ability of the community pharmacist to learn the proper actuation techniques of inhaler devices. J Allergy Clin Immunol. 2001;108:918–20. doi: 10.1067/mai.2001.119153. [DOI] [PubMed] [Google Scholar]
- 8.Melani AS, Zanchetta D, Barbato N, et al. Inhalation technique and variables associated with misuse of conventional metered-dose inhalers and newer dry powder inhalers in experienced adults. Ann Allergy Asthma Immunol. 2004;93:439–46. doi: 10.1016/s1081-1206(10)61410-x. [DOI] [PubMed] [Google Scholar]
- 9.Chopra N, Oprescu N, Fask A, Oppenheimer J. Does introduction of new “easy to use” inhalational devices improve medical personnel's knowledge of their proper use? Ann Allergy Asthma Immunol. 2002;88:395–400. doi: 10.1016/S1081-1206(10)62371-X. [DOI] [PubMed] [Google Scholar]
- 10.Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respir Care. 2005;50:617–23. [PubMed] [Google Scholar]
- 11.Skaer TL, Wilson CB, Sclar DA, et al. Metered-dose inhaler technique and quality of life with airways disease: assessing the value of the Vitalograph in educational intervention. J Int Med Res. 1996;24:369–75. doi: 10.1177/030006059602400409. [DOI] [PubMed] [Google Scholar]
- 12.Nimmo CJ, Chen DN, Martinusen SM, Ustad TL, Ostrow DN. Assessment of patient acceptance and inhalation technique of a pressurized aerosol inhaler and two breath-actuated devices. Ann Pharmacother. 1993;27:922–7. doi: 10.1177/106002809302700721. [DOI] [PubMed] [Google Scholar]
- 13.Pronk M, Blom L, Jonkers R, Bakker A. Community pharmacy and patient-oriented activities: the Dutch case. Patient Educ Counseling. 2002;46:39–45. doi: 10.1016/s0738-3991(01)00148-3. [DOI] [PubMed] [Google Scholar]
- 14.Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol. 2007;119:1537–8. doi: 10.1016/j.jaci.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 15.Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ Counseling. 2008;72:26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 16.van der Palen J, Klein JJ, Schildkamp AM. Comparison of a new multidose powder inhaler (Diskus/Accuhaler) and the Turbuhaler regarding preference and ease of use. J Asthma. 1998;35:147–52. doi: 10.3109/02770909809068202. [DOI] [PubMed] [Google Scholar]
- 17.Resnick DJ, Gold RL, Lee-Wong M, Feldman BR, Ramakrishnan R, Davis WJ. Physicians' metered dose inhaler technique after a single teaching session. Ann Allergy Asthma Immunol. 1996;76:145–8. doi: 10.1016/S1081-1206(10)63413-8. [DOI] [PubMed] [Google Scholar]
- 18.Caffarella RS. Planning Programs for Adult Learners. A Practical Guide for Educators, Trainers and Staff Developers. 2nd ed. San Francisco, Calif: Jossey-Bass Publications; 2002. pp. 176–351. [Google Scholar]
- 19.Pike RW. Creative Training Techniques Handbook. Tips, tactics, and how to's for delivering effective training. 2nd ed. Minneapolis, MN: Lakewood Publications; 1994. pp. 1–41. [Google Scholar]
- 20.Jackevicius CA, Chapman KR. Inhaler education for hospital-based pharmacists: how much is required? Can Respir J. 1999;6:237–44. doi: 10.1155/1999/695365. [DOI] [PubMed] [Google Scholar]
- 21.Mehuys E, Van Bortel L, Annemans L, et al. Medication use and disease control of asthmatic patients in Flanders: a cross-sectional community pharmacy study. Respir Med. 2006;100:1407–14. doi: 10.1016/j.rmed.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Mickle TR, Self TH, Farr GE, Bess DT, Tsiu SJ, Caldwell FL. Evaluation of pharmacists' practice in patient education when dispensing a metered-dose inhaler. Ann Pharmacother. 1990;24:927–30. doi: 10.1177/106002809002401003. [DOI] [PubMed] [Google Scholar]
- 23.Guidry GG, Brown WD, Stogner SW, George RB. Incorrect use of metered dose inhalers by medical personnel. Chest. 1992;101:31–3. doi: 10.1378/chest.101.1.31. [DOI] [PubMed] [Google Scholar]
- 24.Hanania NA, Wittman R, Kesten S, Chapman KR. Medical personnel's knowledge of and ability to use inhaling devices. Metered-dose inhalers, spacing chambers, and breath-actuated dry powder inhalers. Chest. 1994;105:111–6. doi: 10.1378/chest.105.1.111. [DOI] [PubMed] [Google Scholar]