Abstract
Introduction
One aspect of clinical integration involves case managers' tools and particularly the individualized service plan.
Methods
We examined individualized service plan content and use in the PRISMA experiment. We analyzed 50 charts, and conducted and recorded interviews regarding individualized service plan use with all the case managers concerned (n=13).
Results
Delays between starting case management and writing the individualized service plan were long and varied (0–596 days, mean: 117 days). During the interviews, the individualized service plan was described as the ‘last step’ once the active planning phase was over. The reasons for formulating plans were mainly administrative. From a clinical viewpoint, individualized service plans were used as memoranda and not to describe services (842 interventions not mentioned in the plans) or needs (694 active problems not mentioned). Case managers felt uncomfortable with the individualized planning task and expected a tool more adapted to their needs.
Conclusion
Although a majority of the case managers' charts contained an individualized service plan, implementation of this tool seems tenuous. Because of the discrepancy between the potential usefulness expected by case managers and their actual use, a working committee was created to develop proposals for modifying the instrument.
Keywords: case management tool, individualized service plan, clinical integration, gerontology, qualitative research
Introduction and background
A number of recent literature reviews emphasize the pivotal role played by case management in the efficacy of integration experiences for older adults around the world [1–3]. The case management process can be defined as comprising the following key steps [4–14]: case identification according to predefined criteria, standardized multidimensional assessment, individualized service plan, resource identification, implementation, monitoring, and plan reassessment. Some include the concept of advocacy, which combines advice and representation [10, 13, 15]. While case management was being developed, it became apparent that tools were needed to support the tasks of identification, assessment, and planning. To a great extent, case identification depends on the eligibility criteria for case management. As a result, the tools used in the various experiments varied substantially. The assessment task led to the development of many different tools, such as the Outil d'evaluation multiclientele (OEMC or multiclientele assessment tool), including the Systeme de mesure de l'autonomie fonctionnelle (SMAF or Functional Autonomy Measurement System) in Quebec and the Resident Assessment Instrument (RAI) in the US and then Europe. These instruments have undergone many validation studies [16, 17].
However, the planning task, which appears to be essential since it governs implementation, monitoring, and reassessment, has not yet received the same kind of attention. Yet many authors view the formulation of an individualized service plan as an essential component in integrating services for frail elders [1, 4]. For some, it represents case management quality criteria [12, 18]. As with assessment, the plan is both a set of processes and a product in the form of a written document placed in the person's chart. To our knowledge, no such planning document has ever been validated scientifically. Consequently, the tools used for planning are usually derived from that used for assessment. In Quebec, the definition of individualized service plan used by the Ministère de la Santé et des Services sociaux refers to the process designed to achieve social integration and to provide an individualized response to the person's needs. It requires that the person or the person's representative attend a meeting aimed at cooperation and collaboration [9]. This definition, like others around the world [1, 12, 14, 18] based on major consensual principles, does not, however, explicitly state how the individualized service plan leads to clinical integration and how important developing the plan document is to integration. This is also observed in the literature: while the individualized service plan is often cited as an important feature of integration, its design, expected content, size, usefulness, and use are not defined [9]. The PRISMA integration experiment, in which case managers were asked to develop individualized service plans, enabled us to clarify these individualized service plan aspects using qualitative methods.
Methods and theory
The PRISMA program
PRISMA (Program of Research on the Integration of Services for the Maintenance of Autonomy) [4] is an integration model implemented in three experimental areas. The research program comprised, on the one hand, a study of the impact integration has on independence, satisfaction, and use of services for older adults in the experimental areas compared to the control areas and, on the other, ongoing monitoring of the model's effective implementation [19]. This program proposes a coordination-type approach to the integration model as defined by Leutz [20]. In this kind of model, all health and social service organizations are involved, whether public, private, volunteer, or community. Each organization maintains its structure but takes part in integration by adapting its operations and resources. The outcome is that individuals no longer have to search for the proper resource for their needs. Rather, it is up to the integrated system to provide a continuum of services that respond to people's needs. The PRISMA model, designed after reviewing the literature, comprises six components: 1) coordination at all levels of decision-making, 2) a single entry point, 3) case management, 4) individualized service plans, 5) a unique standardized assessment tool, and 6) a computerized clinical chart. Each of these points have been described in detail elsewhere [4, 19]. There are different case management models [9]. In the PRISMA model, case managers are under the responsibility of and remunerated by Quebec's public health care and services system. Each full-time case manager has to manage about 45 people. Case management was defined as a new role for different professionals (social workers, nurses and psychologists) already involved in the public health care and service system for older persons in Quebec. Professionals received special training on the different case management tasks before they became case managers. Individual eligibility corresponded to a great need for coordination because of the number of caregivers and providers involved (greater than two, in addition to the attending physician and meal services) or the degree of loss of independence measured with a standardized assessment instrument (need for assistance exceeding that provided for domestic needs). Case managers had to have or perform a comprehensive assessment of the individuals' needs. They had to be in close contact with patients and be familiar with their home settings. In interacting with patients, families and attending physicians, case managers had to develop an individualized service plan resulting from a cooperative interdisciplinary process with the various caregivers and providers. Afterwards, they were responsible for the follow-up and reassessment of the plan over time, thereby guaranteeing the diachronic continuity of management.
In the PRISMA model, therefore, the individualized service plan represented one of the key elements in effectively implementing integration at the clinical level. Since electronic medical charts were gradually introduced [19], case managers soon had an electronic version of the same form. No databases (needs or services) were associated with the individualized service plans. No tasks were automated and the text was written freely on paper or electronically. The overall PRISMA research program included an implementation analysis that evaluates the quality of the individualized service plan in each patient chart [19]. The entire PRISMA research program and each of the PRISMA studies including the one described here were approved by the Ethics Committee of the Sherbrooke Geriatric University Institute.
Analysis methods
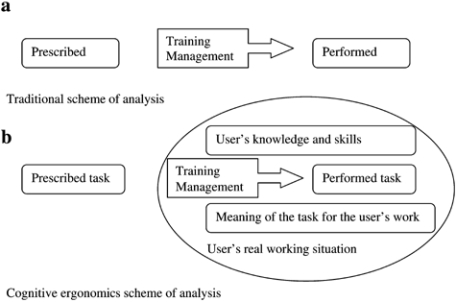
Our analysis of the individualized service plan is based on the conceptual framework of cognitive ergonomics [21], where the focus is on the discrepancies between what is prescribed, said, and done. Traditionally, a task has to be performed as prescribed by managers and if this is not the case, a deficiency in training or management must be found. In contrast, cognitive ergonomics research is based on the assumption that users have specific (but not necessarily the best) knowledge on how and why an activity is to be done during their work (Figure 1). Studies in cognitive ergonomics develop an analysis framework to take into account the prescribed task and the performed task. To understand the discrepancies, the performed task has to be assessed in a real situation (not a simulation or a ‘performance’ test), and in parallel an assessment of cognitive activities linked to the task has to be done, usually by users' comments on this task. This approach is pragmatic and aims to develop recommendations that meet both organizational needs and reflect professional reality. In our research on individualized service plans, the prescribed task (case managers have to develop individualized service plans in order to achieve clinical integration) was compared to the task actually performed (individualized service plan production and use) and what the case managers had to say about it (which reflects both their knowledge about the task prescribed and performed, and their expectations). The discrepancies between the task prescribed and performed, and what the case managers had to say are not viewed here as deficiencies. Indeed, as we have said, knowledge about the need for individualized service plans for integration was vague. Accordingly, we will discuss these discrepancies as a source of information about the work done by the case managers related to individualized service plans and as a source of potential information about the usefulness of these plans in terms of integration.
Figure 1.
Illustration of the cognitive ergonomics scheme of analysis 21 compared to a more traditional view.
For this study, we used a sequential schema with multiple investigative methods in order to achieve a certain degree of triangulation. The research team that examined methods and interview grids was comprised of researchers in the area of health services and social sciences. Different professions were represented in the research team including physicians, social workers and psychologists.
Our analysis of the implementation context focused on the documentation used to train the case managers, to which we had complete access. This material was analyzed for information that would yield the most precise description of the ‘prescribed’ task of developing the individualized service plan, its expected contents, and its practical use. From this, we attempted to identify the rules indicated in these documents that case managers were supposed to follow to develop an individualized service plan.
Interviews
The criteria for including case managers in the interviews for the qualitative study about what the case managers “said” about the individualized service plan were as follows:
Participation in the PRISMA program
Having a minimum caseload of five
Having been a case manager for at least six months
Having signed an informed consent form to take part in the study.
All the case managers meeting these criteria were invited to take part. None of them refused to participate.
The interview plan was developed through multidisciplinary cooperation. It was based on the theoretical framework of cognitive ergonomics and a literature survey [9]. The following issues were addressed:
- In order to examine case managers' knowledge of individualized service plans (that is, case managers' representation of the ‘prescribed task’:
- individualized service plan usefulness and function(s) in the case managers' work
- In order to examine the individualized service plan ‘activity’ in the case managers' work from the perspective of ‘what is said’:
- Time-related aspects of the individualized service plan in the case managers' work
- Factors fostering or hindering individualized service plan formulation development
- Distribution of the instrument to other professionals in the system
The interview plan enabled interviewers to systematically address the various issues and elicit further information if necessary. Case managers could also bring up points of interest outside the plan as long as the interview remained focused on the individualized service plan as a case management tool. All the interviews were carried out face-to-face at the case managers' workplaces by the same person and recorded without intermediate analysis or modification of the interview plan prior to being transcribed verbatim.
Each interview was coded in two ways: descending, that is, starting with the interview plan described above, for the most unequivocal coding possible; and ascending, that is, starting with the analysis of interview content outside the plan in order to add value to the analysis plan while maintaining an ergonomic approach. The interviews were all coded by the same individual without any cross-coding. A preliminary grouping of the codes emerging from the ascending approach was made. The grouping was discussed by the multidisciplinary team and modified to generate a reasonably stable theoretical framework for analyzing the interviews. This made it possible to code the entire corpus of interviews a second time. The second encoding revealed that the first-round codes were quite stable. The codes that came up during the process served mainly to encode passages that had not been coded in the first round. Data organization and encoding was facilitated by using NVivo® software (QSR International), which can be used to encode, assign multiple codes, and reorganize the corpus according to code or category.
Chart analysis
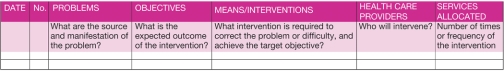
We analyzed the contents of 50 charts managed by the 13 case managers in order to develop a description of the task actually done. Charts were selected randomly except for ensuring that there were at least two charts from each case manager interviewed. The drafting date had to be as close as possible to but no later than the start of our study of individualized service plans, which the case managers were aware of. The elements that we looked for in the case manager charts were defined by the multidisciplinary team, after the ‘prescribed task’ was analyzed at a time close to when the interviews were conducted in order to grasp the significance of the individualized service plan as a tool. Since managers required each ISP to be reassessed every six months, each chart could contain more than one ISP. As for the individualized service plan itself, we used the date the individualized service plan was written compared to the case management start date (date on which the case manager signed the consent to exchange information) and the date written in the assessment tool. Since a service could be delivered long before documentation of the ISP, this delay is not of the same as a delay in service production. The individualized service plan's readability was assessed by the number of lines and various kinds of information it contained. The individualized service plan form is structured as a series of columns (Appendix 1); the lines (rows) depend on how the case managers fill it out. Consequently, a single line may contain a number of problems, objectives, and interventions and thus involve a number of caregivers and frequencies. The analysis took into account the fact that the rows on the electronic individualized service plan form are predetermined. In the case of paper forms, the numbering along the left-hand side, used by certain case managers, or a skipped line were considered separators for analysis purposes. In the electronic and traditional charts, the plan was filed in plain text so that several issues were often put on the same line since the average number of issues could exceed the number of lines.
With the electronic individualized service plans, we were able to determine the number of consultations and the professional categories of the individuals with access to individualized service plans. We also attempted to determine to what degree the case managers followed the development rules that we identified based on our analysis of the training documentation. We also carried out a qualitative study of the vocabulary used in the individualized service plans by certain key caregivers, such as general practitioners and case managers. Lastly, we examined the charts for indications of individualized planning (progress notes, conclusions of the standardized case management assessment).
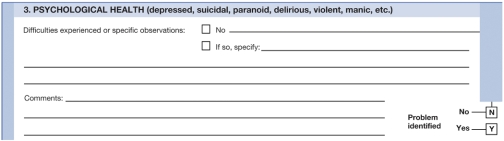
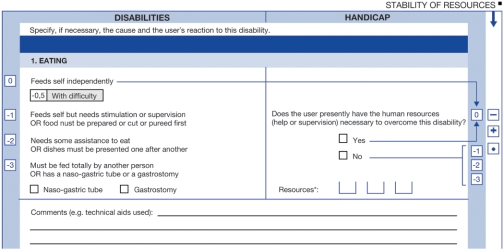
Individualized service plan—assessment comparison
The assessment instrument used in Quebec is the Multiclientele Assessment Tool, which includes 25 dimensions assessed as to whether or not the patient was experiencing a problem (or if means were used to compensate for the difficulty) (Appendix 2). Functional autonomy was assessed with a standardized tool, the Système de mesure de l'autonomie fonctionnelle or SMAF [22], which assesses 29 dimensions of independence based on whether the patient does or does not have a disability and, if so, whether it appears as a handicap (Appendix 3). Both instruments make it possible to identify difficulties and often many of the resources that respond to these disabilities at the time of assessment. We therefore compared the contents of each individualized service plan with that of the most recent standardized assessment in order to determine how well the individualized service plan corresponded to the summary of all the problems noted in the assessment (with or without solutions), and if the individualized service plan contained all the resources indicated in the assessment as compensating for the person's handicap or difficulty. If so, the individualized service plan could be viewed as a snapshot of the person's services, even if they did not address all of the needs.
Results
Contextual analysis (‘prescribed task’)
No individualized service plan documents were created when the integrated networks were implemented. Instead, the forms used to plan home care services, called the ‘individual service allocation plan’ (Appendix 1), were used. This document was designed at the same time as the Multiclientele Assessment Tool to plan professional services. Evolving out of similar documents used in nursing, it had been used as a guide in multidisciplinary team work well before the creation of integrated networks. However, it was not designed for higher-level coordination (that is, of more than one group of professionals). Four training documents were analyzed. All of these documents have an indirect or direct connection to the book by D. Boisvert on the individualized service plan [23]. The individualized service plan definitions given in all four documents refer to a ‘process’. None of the documents dealt with the opportunities and means that case managers can or must use in their work. These documents give prominence to major consensual values (such as fairness, justice, equality, solidarity, social integration, and primacy of the individual), whose definitions constituted part of the training. Two documents stressed the importance of organizing the multidisciplinary meeting (as in Boisvert's book [23]). For the Objective section, the rule was to record observable or measurable behaviors with a threshold and an observation delay; action verbs had to be used. One document included a four-page list of verbs to use as help in drafting the objective. Moreover, it was indicated that instructional verbs (maintain, reduce, promote, improve, etc.) should be avoided. No specific rule was provided about the other sections of the form. The written comments of the case managers who received training—which were kept—revealed dissatisfaction with the individualized service plan section, although they considered the overall training very satisfactory. They felt that the individualized service plan training was too theoretical: “How do you adapt a tool made for planning services over the medium and long-term to a clientele whose health and needs change rapidly?” or “Why does someone in the network still not use an individualized service plan after several years of training and awareness?”
Interviews: what was said
Our main results as compared to the prescribed and the performed task are synthesized in Table 1. In regards to using the individualized service plan (ISP), case managers indicated that it usually comes after planning, since the individualized service plan is described as the last step in a chart that has achieved a certain degree of stability: “The ISP is the final act…. That's how I see it, once I have all the information I need…” (case manager 5); “I don't put anything into the ISP until the client's situation has stabilized. Once the client is set up, I use the ISP” (case manager 3). In fact, 12 of the 13 case managers made similar comments. The only one that did not say he didn't use the individualized service plan at all: “It's a step that I often skip…because it just doesn't seem useful to me…it's just one more step if you have to write up the intervention plan or ISP” (case manager 12).
Table 1.
Synthesized table of results on the principal axis of analysis of the utilization of ISP as a clinical integration tool by case managers
| ‘Prescribed’ task | What was said | ‘Performed’ task | |
|---|---|---|---|
| ISP as a planning tool | Not clearly defined | ‘Final step’ | Long delay |
| Motivation | ‘The case manager's tool’ | Predominance of administrative motives | Impossible to determine |
| Content of the problem section | All problem must be noted | Not consistent | Not consistent |
| Content of the objective section | Precise rules | Not consistent but never in accordance with rules | Not consistent |
| Content of other sections | Not clearly defined | Not consistent | Not consistent |
| Access | Not clearly defined | Concern about insufficient access and clarity | Rare access to ISP Poor readability of the ISPs |
| Clinical function | Not clearly defined | Reminder, contract, multidisciplinary support | Notes about planning were found in all the charts but not in ISP |
| Link between ISP and case management | Clear | Clear | Impossible to determine |
Moreover, the case managers cited motives for producing the individualized service plan that reinforced the impression of it being an administrative task. For example they said: “It's one of our tasks. We knew when we were hired…that it had to be done” (case manager 5) or “One goes into every chart” (case manager 3) or “Well, there is an ISP, but it hasn't been finished…. I'm going to update it because I have to submit it to the allocation committee next week” (case manager 6). Some thought the research program itself had an influence: “If I hadn't read the research now, I'm not sure that there would be ISPs in the charts” (case manager 1). Five case managers mentioned the research protocol either directly or indirectly, referring to the PRISMA model as a motivation for developing the individualized service plan.
The case managers were not in agreement about the expected contents of an individualized service plan: “I put down all services” (case manager 10); “No, I didn't put down everything, and I won't in the future” (case manager 8); “Every handicap and disability must be included in the ISP” (case manager 5). It is interesting to note that the individualized service plans did not always reflect the expressed intentions. For example, case manager 5 only managed to follow his rule of mentioning all needs in 2 of the 12 individualized service plans analyzed, while case manager 8 complied with the same rule in 3 cases out of 4.
The case managers were concerned about the fact that few people in the network appear to want to read individualized service plans. Case manager 8, whose individualized service plans had the highest average access rate (average of 3 in addition to the case manager), stated: “I've already looked at the history. Not too many people are going to do that.”
The case managers also took different positions about the usefulness of the individualized service plan for the case manager: “The first thing I do…is to see what's in the plan” (case manager 12); “sometimes I'll look at the chart, but rarely the ISP” (case manager 1). Plan access could serve case managers as a reminder of the services in place, the steps already taken, or as a help in managing schedules. Given that the individualized service plan aims at determining an individual's needs and planning the services to respond to them, it is paradoxical that the only clinical motivation mentioned by two case managers was related to limiting services for people who were considered overly demanding: “The ISPs for manipulative people…contain tons of details…because they tend to always ask for more” (case manager 7). The individualized service plan has been described as an element fostering multidisciplinary team joint action. With the exception of this latter function, the others could be replaced by reviewing progress notes or concluding the assessment without an individualized service plan. Consequently, no functions related to the case managers' clinical work appeared to specifically devolve to the individualized service plan.
All the case managers described the individualized service plan as being very strongly related to their work: “It's THE case manager's tool” (case manager 11). No case managers raised the idea of case management without an individualized service plan. On the contrary, the difficulties encountered were explained by the innovativeness of integration: “An integrated network…and case management are new” (case manager 7); lack of partner computer access: “The system…must be accessible elsewhere” (case manager 7); lack of definition of confidentiality rules: “I tell myself to be careful not to put too much into the ISP because the information can be shared” (case manager 13). They also emphasized a lack of clarity about the concept: “No one has a clear idea of what the ISP is all about” (case manager 7). Four case managers had very similar perceptions: “Everything goes into our ISPs today, like disciplinary intervention plans and service plans; everything is thrown together” (case manager 10). Case managers also pointed out the lack of training or, more accurately, the inappropriateness of training: “I don't think they were clear enough about ISP contents” (case manager 13).
Case managers felt that the form used for individualized service plans had problems, specifically its lack of clarity: “It's clear to me, but I don't think it is for the others” (case manager 5); its static appearance “You know that you can't exchange? with an ISP. An ISP doesn't budge?” (case manager 9); and the burden of writing: “I often wrack my brains trying to write the objective” (case manager 9). The clash of these expectations with reality made case managers uneasy: “My own plans bother me sometimes…but I don't know what else to do” (case manager 10). There were, in fact, many expectations and they concerned, in particular, the concept itself: “What use is it? Why are we doing this? What should it contain?” (case manager 10); training: “I think that training on this is needed” (case manager 10); and form simplification: “I think that ISPs should be easy to develop” (case manager 1).
Chart analysis
Our analysis involved all of the individualized service plans (n=101) in the 50 charts. The average time between the start of management and the first individualized service plan varied greatly: 0 to 598 days for the 50 individualized service plans we examined. The average time lapse was relatively high (117 days). The case managers themselves were not consistent with individualized service plan production, except for two who appeared to try to do the individualized service plan within the first 30 days. These two case managers, who worked at the same location, had been instructed by their superior that the charts had to conform to the integration model (i.e. contain an individualized service plan). Another case manager at the same site, however, had an average production time for the first individualized service plan of 71 days from the start of case management (ranging from 0 to 267 days). The time lapse between assessment and individualized service plan production was similarly variable: 0 to 524 days, for an average of 68 days. Lastly, the time between assessment and individualized service plan production shortened: from 138 days in 2001–2002 to 39 days in 2003.
Other characteristics of the ISP related to readability are summarized in Table 2. Nevertheless, the number of interventions was not directly related to the number of caregivers since many interventions were performed by the same caregiver. To illustrate, in individualized service plan 2, Chart 47, the visiting homemaker did all of the following: “Help with hygiene, help with clipping nails, meal preparation, support with home maintenance, and grocery shopping”. Conversely, several caregivers provided the same intervention: for example, in individualized service plan 2, Chart 38, seven caregivers provided spouse respite: day centre, temporary placement centre, two social workers from these organizations, the case manager, a community organization, and a private resource.
Table 2.
Characteristics of the 101 individualized services plans (ISP)
| Characteristics of ISP | Mean | Range |
|---|---|---|
| Lines (n) | 5.5 | [1–19] |
| Issues (n) | 7.1 | [1–20] |
| Objectives (n) | 6.9 | [1–20] |
| Interventions (n) | 10.6 | [2–33] |
| One-month access count (n)* | 11 | [0–30] |
These data were based on 73 computerized charts.
Case managers accounted for the large majority (91%) of individualized service plan accesses and specifically the writer in 70% of cases. For the remaining 9%, administrative purposes were the reason for at least 5 instances of access: program managers (n=2) and archivists (n=3). Access by other caregivers in the system was rare: individualized service plans were mailed to the family physicians concerned in 27 cases out of 101. No other recipients were mentioned in the charts.
No specific guideline was followed in writing up problems or needs; the recommended structure was never used. None of the 699 objectives appearing in the individualized service plans could be considered as observable or measurable behaviors with a threshold and observation delay, as presented during training. In contrast, 80.7% of the objectives corresponded to directions for actions continuing over time expressed with verbs that were supposed to be avoided (compensate, improve, maintain, monitor, learn, etc.). The family physician was mentioned in 73 of the 101 individualized service plans. Since the document is structured so that the caregiver is mentioned depending on the problems identified, the family physician sometimes repeatedly appeared in the same individualized service plan. It is also possible that he was not the only caregiver mentioned on a single line for a problem. As a result, we analyzed such individualized service plans on a per-line basis. When mentioned on an individualized service plan line, the problems that the family physician should be able to resolve were health issues in 58 cases out of 80, loss of independence in 17 cases, and psychosocial disorders in 5 cases. The objectives were often quite vague, related to the medical profession in a general way: “Provide medical management,” “Maintain state of health” and “The patient will have the required medication and care”. More specific objectives were used much more rarely: “Reduce the micturitional frequency and redness associated with incontinence”.
We also studied the lines in the individualized service plans where the case manager was mentioned as caregiver. There were often multiple problems, possibly of different types, but mainly psychosocial and related to the loss of independence, such as: “Precarious recovery from fractures” or “Needs help in managing appointments and contacts with the system.” Moreover, we also noted that the objective was often a fairly general description of the case manager's function: “Enable service use and reduce management burden”; “The patient will have advice enabling him to live in his home as long as possible”; “Maintain a presence and be supportive, while providing support to the natural caregiver.” A more individualized description of the task was rarely encountered. It is interesting to note, however, that, when the objective was mentioned, it always health-related and did not always correspond to the case manager's previous profession: “Avoid increasing pain, avoid falls or increased pain during bathing” (case manager was initially a nurse); “Investigate incontinence and identify adequate compensation” (case manager initially a psychologist); “Ensure that the patient has adequate dietary intake (no weight loss), monitor problem with constipation” (case manager initially a social worker). Frequency was stated in the form of “as needed,” without describing the process for identifying need recurrence in 37.5% of cases. As a result, this did not make it possible to establish an accurate schedule for delivery or the actual service frequency.
The qualitative analysis of the charts highlighted the fact that individualized planning did indeed exist but was not supported by the individualized service plan, which means that it provided only partial representation. Indications that individualized planning actually occurred appear in the progress notes: “Contact with family physician reveals that pain clinic physicians did not recommend infiltration and suggested morphine…He is in agreement with swimming and the day centre…”; or in assessment conclusions: “As for housekeeping, Mr. X refused system help; he will ask his family to play a greater role…. He accepts help with grooming and some financial aid to purchase these services.”
Individualized service plan—assessment comparison
Three individualized service plans were written with no trace of a previous or current assessment while seven were written after a limited assessment to determine loss of autonomy. It was therefore possible to compare individualized service plan and assessment data in nearly all cases. The comparison of individualized service plans and multiclientele assessment data showed that the individualized service plans as a whole did not inventory all of the individuals' problems since only 716 problems were identified in the ISPs and 695 were not (Table 3) or the services they used (Table 4).
Table 3.
Comparison of the number and type of problems and handicaps in the individualized service plan and multidimensional assessment
| Problems or handicaps | Indicated in the individualized service plan | Not in the individualized service plan but in the assessment | Total |
|---|---|---|---|
| Health problems | 141 | 225 | 366 |
| Prevention problems (diet, smoking, alcohol, safety) | 2 | 29 | 31 |
| Problems with loss of independence (handicap or instability of the resource offsetting the handicap) | 424 | 271 | 695 |
| Psychosocial problems | 132 | 132 | 264 |
| Financial problems | 11 | 15 | 26 |
| Other problems | 6 | 23 | 29 |
| Total | 716 | 695 | 1411 |
Table 4.
Comparison of the number and types of caregivers in the individualized service plans and multidimensional assessment (Family physician is a given in both cases, which is analyzed in the text)
| Service providers other than family physician | Indicated in the individualized service plan | Not in the individualized service plan but in the assessment | Total |
|---|---|---|---|
| Patient | 17 | 67 | 84 |
| Family and significant others | 159 | 513 | 672 |
| Private resources | 109 | 176 | 285 |
| Community organizations | 67 | 14 | 81 |
| Public services (medical and social) | 461 | 81 | 542 |
| Public institutional resources (day centre, temporary placement) | 116 | 5 | 121 |
| Others and poorly defined | 29 | 14 | 43 |
| Total | 958 | 870 | 1828 |
The problems most often missing from the individualized service plans related to health; the services most often omitted were non-professional in nature such as services provided by the family. We attempted to discover if case managers adhered to the same writing logic from one individualized service plan to the next. None of the 13 case managers consistently followed the same rule in drafting all of his or her individualized service plans. Nevertheless, while seven followed no rule in more than 50% of their individualized service plans, two case managers inventoried needs in more than 50% of their individualized service plans and four listed professional services.
Discussion
This qualitative study found problems with implementation of individualized service plans in an experiment in which quantitative assessment alone indicated successful implementation of the tool [19]. The PRISMA program offered a rare opportunity to highlight this aspect because it is a successful experiment of implementation of a model of integration in Quebec [19]. Moreover, this model of integration was successful in the pilot study in preventing the loss of autonomy [24]. Nevertheless, despite the fact that the charts contained individualized service plans for the most part, our analysis showed that they were rarely put to practical use and that their usefulness remained mostly theoretical. Specifically, the motivations underlying its development and use were vague when written. The clinical chart as a whole attested to real individualized planning carried out by case managers, but the individualized service plan appeared to be only an accessory in the process at best. The conceptual framework guiding the trainers [23] was based on another clientele (specifically, individuals with intellectual impairments) with needs and disabilities that remained stable over long periods of time. Moreover, the dynamic nature of the individualized service plan was not essential for this target group. The form itself was developed for planning a fairly limited number of interventions over a relatively short period of time (intervention plan derived from nursing and adapted to the care team's work). It appears limited in its usefulness over the longer term with a significant number of problems and caregivers. Consequently, the individualized service plans were primarily produced to document the chart or for administrative purposes, although they may occasionally serve a clinical purpose in summarizing the chart. Nevertheless, case managers expressed a need for a planning tool, which they thought that the individualized service plan should have been.
It should be noted that any tool or instrument used in an integrated system often has both clinical as well as management and guidance functions. This is the case with assessment tools (Système de mesure de l'autonomie fonctionnelle SMAF in Québec) that are tied to classification systems (case mix) (Iso-SMAF profiles [25]) and therefore used to manage resources (personnel, budget, etc.) as well as to plan services and develop integrated networks. From this viewpoint, the fact that individualized service plan information was not used for management and guidance is symptomatic of its inappropriateness for integration in its current form. When integration was being developed in Quebec, the choice of assessment tools gave rise to very serious rethinking that led to the first instrument (named CTMSP) being abandoned for failing to take into consideration certain environmental factors deemed essential for integrated networks [26].
Our results call into question the adequacy of individualized service plans as a clinical integration tool. If case manager feedback is taken into consideration, there appears to be a need to support and facilitate this complex task of individualized planning within an integrated service network. All our interviews and analyses of charts (particularly assessment conclusions and progress notes) showed a good understanding of the individualized planning task as described in the literature [9] and of training materials and case management in general, with a central role for coordination (not only in terms of time but also in consistency between interventions) and continuity of information (conciseness and accuracy). There was also an expectation that the writing task would be simplified and that the dynamic aspect of the tool would give case managers an ‘instrument panel,’ rapidly indicating the needs, the services in place, and those either pending or unavailable (and the solution arrived at). With such a tool, the objectives do not need to be observable behaviors with a threshold and a waiting time, but rather overall directions. That is premised on the directions being taken into account by each caregiver or team of caregivers when drafting its intervention plan (with observable or measurable objectives in each of these plans, with a timeline and threshold). Modifying the drafting guidelines in this way would respond to case managers' concerns about making the individualized service plan much more user-friendly. Moreover, it is based on an intuitive adaptation of case managers who were already using such verbs in more than 80% of cases when drafting their objectives. It could be noted in passing that an instrument panel documenting the discrepancies between people's needs and the services actually available in the integrated network would be useful for management and guidance purposes, which is what makes it a comprehensive integration tool. Of course, certain prerequisites seem necessary. The case managers insist, in particular, on adequate training for themselves and the other network caregivers in order to develop the habit of looking for information in the individualized service plan. In this regard, computerizing the tool also appears necessary, as does improving access to the electronic tool with networks. Nevertheless it seems that even with precise rules and adequate tools, a certain degree of flexibility is necessary to achieve clinical integration.
Based on the quality criteria for qualitative research developed by Mays et al. [27], our study includes many factors making it possible to judge its validity. The qualitative methods we deployed (contextual analysis, documentary analysis and discussions) enabled us to triangulate our research methods on our objective and, through congruence analysis, increase our degree of confidence in our results. This triangulation also enables the reader to judge our level of interpretation of the corpus. The principal investigator's field is very different from that of this study. A hospital geriatrician from France, he joined the research group when the impact and implementation study was in its third year. He brought an unbiased perspective of the individualized service plan since he had no prior knowledge of Quebec's health and social services system. Indeed, while French legislation refers to the planning task in developing an assistance plan, responsibility for it never falls on a hospital physician. Such plans in France are purely social in nature and do not involve physicians. Lastly, unlike Quebec health care providers, their French counterparts have no tradition of viewing the plan and techniques for developing it as being important. The researcher's distance from the study topic and from the people who provided opinions reduces the personal and intellectual bias inherent in this type of research.
We approached the study from the standpoint developed in the literature that case managers needed individualized service plans to do their jobs. By paying particular attention to the opposite of this assumption, we came to the conclusion that the instrument currently used in the networks examined was not directly useful to case managers in their planning tasks. We also tried to get respondent validation by presenting our research results initially to small groups of professionals (case managers) and then larger groups (conference open to the public, with invitations to case managers and managers of the health and services network), and finally conferences at the provincial and international levels. During these encounters, our results appear to have revealed the working reality of case managers, not just in the three target areas in our study but well beyond.
Our study's main limitation is that it involves a single planning tool. Nevertheless, this is the only tool recognized under the regulations governing Quebec's health and social services system. Moreover, it is structurally quite similar to tools described in various case management manuals elsewhere in the world (in particular, France [28] and the US [14]). We are not aware of other tools that have been developed and scientifically validated to help case managers with individualized planning. Our work provided food for thought in Quebec about individualized planning practices and produced recommendations about the tool's evolution [29]. The work situation is an essential part of the explanation of why a tool can be used in a task (Figure 1); nevertheless, we think that the PRISMA experiment has many strengths that make these results significant for other integration contexts. All of the study areas attempted to implement integration according to the PRISMA model defined a priori, with one of the constituent criteria being the use of the individualized service plan. Consequently, it could be considered that there was initially a certain degree of homogeneity in the implementation of each aspect of the model, including the individualized service plan. This homogeneity of intent was found in contrasting study sites (rural, semi-rural and urban). In our study, we did not examine the influence that location at one site or another may have on individualized service plan effectiveness. Conversely, practices may differ slightly anecdotically depending on instructions regarding the drafting date or systematically entering the family physician as caregiver. Moreover, while the case managers came from different professional backgrounds (social workers, nurses, psychologists), the influence of background on individualized service plans was not examined. Lastly, the fact that the case managers came from different organizations in the Quebec health and social services system (hospitals, local community service centres and community organizations, in particular) had no impact on these parameters. Consequently, our conclusions should be applicable to a very broad range of integration contexts.
Conclusion
Individualized service plans appear to constitute a significant instrument for case managers, which should help in performing individualized planning because they are dynamic and provide for information exchange. However, the forms with five major columns (other than the date), as used in the PRISMA experiment and in other care contexts, do not appear to be satisfactory. As the result of a strong push towards implementation, there has been an increase in the number of charts containing individualized service plans. However, they do not reflect people's individual needs or the services they receive in general. Case managers' motivation in filling out such instruments is mainly administrative in nature, and the level of use by individuals and the system is low. Because of the discrepancy between the potential usefulness expected by case managers and actual use, a working committee was created by the Ministère de la Santé et des Services sociaux to develop concrete proposals for modifying the instrument. Should a new tool be implemented, our results emphasize the importance of providing adequate training in its use. Moreover, we consider that our qualitative methodology based on the conceptual framework of cognitive ergonomics would be appropriate for assessing its usefulness in achieving genuine and effective clinical integration.
Acknowledgments
This project was made possible through the financial support of PRISMA, the Canadian Health Services Research Foundation, the Ministère des Affaires Étrangères français, as part of the Bourse Lavoisier program and Assistance-Publique Hôpitaux de Paris.
Appendix 1. Titles of document columns used at the outset of implementation to produce individualized service plans
Appendix 2. Sample item from the Multiclientele Assessment Tool
Appendix 3. Sample item from the Functional Autonomy Measurement System
Contributor Information
Dominique Somme, Hôpital Européen Georges Pompidou, Service de Gériatrie, Paris, France.
Réjean Hébert, Doyen, Faculté de médecine et des sciences de la santé, Université de Sherbrooke, Quebec, Canada.
Gina Bravo, Institut Universitaire de Gériatrie de Sherbrooke, Quebec, Canada.
François Blanchard, Service de Médecine Interne et Gérontologie, CHRU de Reims, Hôpital Sébastopol, Reims, France.
Olivier Saint-Jean, Hôpital Européen Georges Pompidou, Service de Gériatrie, Paris, France.
Reviewers
Henk Nies, PhD, director, Vilans, Netherlands Centre of expertise for long-term care, Utrecht, The Netherlands.
Giovanni Gambassi, Professor, MD, Catholic University of the Sacred Heart, Rome, Italy.
One anonymous reviewer.
References
- 1.Kodner DL. The quest for integrated systems of care for frail older persons. Aging Clinical and Experimental Research. 2002 Aug;14(4):307–13. doi: 10.1007/BF03324455. [DOI] [PubMed] [Google Scholar]
- 2.Kodner DL, Kyriacou CK. Fully integrated care for frail elderly: two American models. International Journal of Integrated Care [serial online] 2000 Nov 1;1 doi: 10.5334/ijic.11. Available from: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. International Journal of Geriatrics and Psychiatry. 2003 Mar;18(3):222–35. doi: 10.1002/gps.819. [DOI] [PubMed] [Google Scholar]
- 4.Hébert R, Durand PJ, Dubuc N, Tourigny A. PRISMA: a new model of integrated service delivery for frail older people in Canada. International Journal of Integrated Care [serial online] 2003 Mar 18;3 doi: 10.5334/ijic.73. Available from: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Applebaum RA, Wilson NL. Training needs for providing case management for the long-term care client: lessons from the national channeling demonstration. The Gerontologist. 1988 Apr;28(2):172–6. doi: 10.1093/geront/28.2.172. [DOI] [PubMed] [Google Scholar]
- 6.Bernabei R, Landi F, Gambassi G, Sgadari A, Zuccala G, Mor V, et al. Randomised trial of impact of model of integrated care and case management for older people living in the community. British Medical Journal. 1998 May 2;316(7141):1348–51. doi: 10.1136/bmj.316.7141.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newcomer R, Harrington C, Kane R. Challenges and accomplishments of the second-generation social health maintenance organization. The Gerontologist. 2002 Dec;42(6):843–52. doi: 10.1093/geront/42.6.843. [DOI] [PubMed] [Google Scholar]
- 8.Tourigny A, Durand PJ, Bonin L, Hébert R, Rochette L. Evaluation of the effectiveness of an integrated service delivery (ISD) network for frail elderly. In: Hébert R, Tourigny A, Gagnon M, editors. Integrated service delivery to ensure persons' functional autonomy. Québec: EDISEM; 2004. pp. 51–71. [Google Scholar]
- 9.Somme D, Hébert R, Bravo G, Blanchard F. Individualized service plan (ISP) concept and utilization: a review of experiments on integrated services for the elderly in Québec and elsewhere. In: Hébert R, Tourigny A, Gagnon M, editors. Integrated service delivery to ensure persons' functional autonomy. Québec: EDISEM; 2004. pp. 271–89. [Google Scholar]
- 10.Challis D, Darton R, Johnson L, Stone M, Traske K. An evaluation of an alternative to long-stay hospital care for frail elderly patients: I. The model of care. Age and Ageing. 1991 Jul;20(4):236–44. doi: 10.1093/ageing/20.4.236. [DOI] [PubMed] [Google Scholar]
- 11.Pacala JT, Boult C, Hepburn KW, Kane RA, Kane RL, Malone JK, et al. Case management of older adults in health maintenance organizations. Journal of the American Geriatrics Society. 1995 May;43(5):538–42. doi: 10.1111/j.1532-5415.1995.tb06102.x. [DOI] [PubMed] [Google Scholar]
- 12.Riley PA, Fortinsky RH, Coburn AF. Developing consumer-centered quality assurance strategies for home care. A case management model. Journal of Case Management. 1992 Summer;1(2):39–48. [PubMed] [Google Scholar]
- 13.Capitman J, Sciegaj M. A contextual approach for understanding individual autonomy in managed community long-term care. The Gerontologist. 1995 Aug;35(4):533–40. doi: 10.1093/geront/35.4.533. [DOI] [PubMed] [Google Scholar]
- 14.Moxley DP. The practice of case-management. Newbury Park, CA: Sage Publications Inc; 1989. (Sage Human Services Guide: 58) [Google Scholar]
- 15.Genrich SJ, Neatherlin JS. Case manager role. A content analysis of published literature. Care Management Journals. 2001 Fall;3(1):14–9. [PubMed] [Google Scholar]
- 16.Landi F, Tua E, Onder G, Carrara B, Sgadari A, Rinaldi C, et al. Minimum data set for home care: a valid instrument to assess frail older people living in the community. Medical Care. 2000 Dec;38(12):1184–90. doi: 10.1097/00005650-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Hébert R, Guilbeault J, Desrosiers J, Dubuc N. The Functional Autonomy Measurement System (SMAF): A clinical-based instrument for measuring disabilities and handicaps in older people. Geriatrics today: Journal of the Canadian Geriatrics Society. 2001;4(9):141–7. [Google Scholar]
- 18.Geron SM, Chassler D. Advancing the state of the art: establishing guidelines for long-term care case management. Journal of Case Management. 1995 Spring;4(1):9–14. [PubMed] [Google Scholar]
- 19.Hébert R, Veil A. Monitoring the degree of implementation of an integrated delivery system. International Journal of Integrated Care [serial online] 2004 Sep 20;4 doi: 10.5334/ijic.106. Available from: http://www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leutz WN. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank, Quarterly. 1999;77(1):77–110. doi: 10.1111/1468-0009.00125. iv–v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montmollin M. de. L'ergonomie. 3rd. [Ergonomics]. Paris: La Découverte; 1996. (Reperes 43). [in French] [Google Scholar]
- 22.Hébert R, Carrier R, Bilodeau A. The Functional Autonomy Measurement System (SMAF): description and validation of an instrument for the measurement of handicaps. Age and Ageing. 1988 Sep;17(5):293–302. doi: 10.1093/ageing/17.5.293. [DOI] [PubMed] [Google Scholar]
- 23.Boisvert D. Le plan de services individualisé: participation et animation. rev. ed. [The individualized services plan: participation and animation]. Cap-Rouge, QC: Presses Inter Universitaires; 1995. [in French] [Google Scholar]
- 24.Kodner DL. Whole-system approaches to health and social care partnerships for the frail elderly: an exploration of North American models and lessons. Health & Social Care in the Community. 2006 Sep;14(5):384–90. doi: 10.1111/j.1365-2524.2006.00655.x. [DOI] [PubMed] [Google Scholar]
- 25.Dubuc N, Hébert R, Desrosiers J, Buteau M, Trottier L. Disability-based classification system for older people in integrated long-term care services: the Iso-SMAF profiles. Archives of Gerontology and Geriatrics. 2006 Mar-Apr;42(2):191–206. doi: 10.1016/j.archger.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Comité aviseur sur l'adoption d'un outil d'évaluation intégré des besoins des personnes en perte d'autonomie et de détermination des services requis, notamment en institution ou à domicile. [Advisory, Committee on the adoption of a tool for integrated assessment of the needs of people in loss of autonomy and determination of required services, in the institution or in community]. Québec: Ministère de la Santé et des Services sociaux; 2000. [in French]. Available from: http://www.msss.gouv.qc.ca/documentation/index.php. [Google Scholar]
- 27.Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. British Medical Journal. 2000 Jan 1;320(7226):50–2. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Notice d'information sur l'allocation personnalisée pour l'autonomie. [Information notice on the personalized allowance for autonomy]. Paris, France: Ministère des affaires sociales, du travail et des solidarités, Ministère de la santé de la famille et des personnes handicapées; 2001. [in French] [Google Scholar]
- 29.Groupe de travail sur la planification des services. [Working group on the planning of the services]. Québec: Ministère de la Santé et des Services sociaux; 2006. [in French] [Google Scholar]