Abstract
Objectives
To assess the effectiveness of a service-learning advanced pharmacy practice experience (APPE) in a diabetes camp to improve student confidence in diabetes knowledge and related skills
Design
Pharmacy students assisted medical staff during a week-long diabetes camp for children. Students participated in all aspects of diabetes care, as well as wrote pre- and post-camp reflection papers, completed online quizzes, presented an educational training session, and completed pre- and post-camp survey instruments.
Assessment
Students' confidence in their diabetes knowledge and patient care skills increased as a result of participating in the camp.
Conclusion
A diabetes camp APPE improved students' confidence in their knowledge and ability to manage diabetes, and allowed them to gain experience working with an interdisciplinary team in a unique real-world environment.
Keywords: service-learning, diabetes, camp, advanced pharmacy practice experience
INTRODUCTION
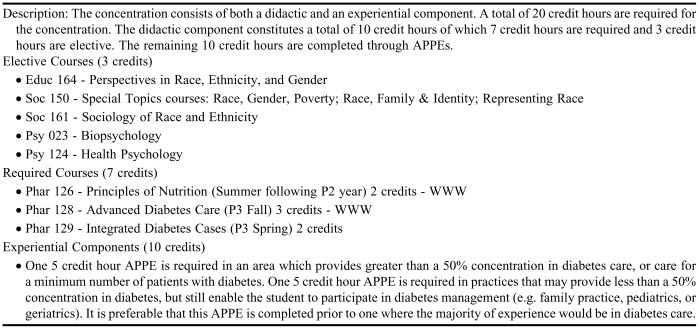
An advanced pharmacy practice experience (APPE) at Camp Hertko Hollow (CHH), a diabetes camp for children in Iowa, has been offered as a component of the diabetes concentration at Drake University College of Pharmacy & Health Sciences since 2001. The diabetes concentration, first implemented in 1999, requires completion of didactic courses and APPEs focused on diabetes. The didactic portion consists of 3 professional elective courses and 1 general education elective. The curricular content of one of the core professional elective courses in the diabetes concentration has been previously published.1 The experiential portion for fourth-professional year students consists of 1 APPE that is less than 50% focused and 1 APPE that is greater than 50% focused on diabetes (Table 1). The diabetes camp APPE serves to fulfill the latter of these experiential requirements.
Table 1.
Outline of Requirements for a Diabetes Concentration Within a Doctor of Pharmacy Degree Program
The reasons for offering the diabetes camp APPE were fourfold. First, faculty members wanted this to serve as a capstone course that would require students to apply and integrate the information they had learned in their diabetes coursework. This APPE is described to students as immersion learning within an environment that requires students to live the life of patients with the disease. Second, we wanted students to increase their confidence and build their skills in caring for people with diabetes. The complexity and growing prevalence of this disease requires graduates to have both breadth and depth of understanding not only of the principles but also the practices of diabetes care. Third, we needed the students to understand the caring aspect of pharmaceutical care and to develop empathy for people affected by diabetes. In the case of this diabetes camp, students interact directly with young patients and their families who share the unrelenting demands imposed on them by the disease. Finally, we wanted to demonstrate our commitment to service-learning, given its importance to the mission of our University and College, and the attention focused on it by the American Association of Colleges of Pharmacy (AACP). Beyond service-learning, this APPE fills an important need for the Camp by providing a trained student pharmacist for their staff. Students become part of an interprofessional team that provides care to the campers.
Institutions of higher learning have expressed a commitment to educate students to be socially responsible citizens, to be engaged in partnerships that benefit their communities, and to help students connect academic learning to meeting societal needs.2 According to the 2004-05 AACP Argus Commission Report titled “Engaging Communities,” service-learning can be simply defined as outreach, or more extensively defined as follows:
“…a method under which students learn and develop through thoughtfully organized service that: is conducted in and meets the needs of a community and is coordinated with an institution of higher education, and with the community; helps foster civic responsibility; is integrated into and enhances the academic curriculum of the students enrolled; and includes structured time for students to reflect on the service experience.”3
This article will describe how the components of a diabetes camp APPE satisfy this more extensive description of service-learning.
DESIGN
Description of Camp Hertko Hollow
Camp Hertko Hollow is a non-profit organization that was founded in 1968 by Dr. Ed Hertko, an endocrinologist. The Camp is centrally located in Boone, IA, at the site of a year-round YMCA camp.4 Children with diabetes are rarely accepted into regular camp programs due to the careful monitoring and care their medical condition requires. CHH provides the safety and security these children need to enjoy a camping experience similar to that enjoyed by children without the disease. These camps also give families a respite from the demands of diabetes management in a secure environment provided by a competent and caring diabetes staff. The notion that “it takes a village” certainly applies to this camp as it creates a safe village of supporters to offer a successful diabetes camp experience.5
The camp provides cabins, a dining hall, conference center, newly renovated health lodge, and other buildings for education sessions or arts and crafts. Annual attendance at the camp has grown from 37 the first year to more than 300, now with different sessions held for different age groups. Kindergarten through the fifth grade attend camp the first week (end of June) while children and teenagers in the sixth through twelfth grades attend the second week (early July). A 3-day “Mini-Camp” is also offered for younger children who may feel uncomfortable being away from home for an extended period. The camp director holds the only full-time salaried position at CHH. A camp committee and over 100 medical and other staff volunteers, including physicians, nurses, dieticians, pharmacists, students in these health professions, and counselors, assist with the planning and operations for CHH. YMCA staff members and administration also provide support. Both CHH and the YMCA camp must meet over 300 national standards for safety and quality required for American Camping Association (ACA) accreditation. A volunteer Board of Directors and a paid Executive Director coordinate fundraising to support camperships for families that need financial assistance and to pay for required operational expenses.
Student Recruitment
Students were alerted to the diabetes camp APPE through electronic student announcements, advisors, a link on the College and experiential office web pages, the annual fall preceptor showcase, student organization fundraising efforts for the camp, and presentations to various student professional organizations. Students who had completed the diabetes concentration were given preference when selecting students for this APPE, but a few students who had completed at least 1 of the professional diabetes elective courses were also considered after the diabetes concentration students had been enrolled. A maximum of 4 students were allowed to enroll for each camp session due to preceptor workload and the desire to closely monitor student performance during the camp. This allowed for continual feedback and mentoring by the preceptor who served as a medical staff volunteer at CHH. If the faculty preceptor was not able to stay at the camp the entire week, other licensed pharmacists who had adjunct faculty appointments and were volunteering as medical staff for camp served as preceptors for the remaining time.
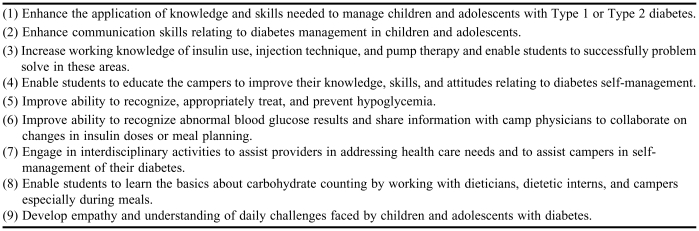
Goals for the Diabetes Camp APPE
Table 2 lists the goals for this APPE, which is offered towards the beginning of the fourth-professional year. These goals were included in the course syllabus and served as the basis for student survey instruments completed before and after camp. Attendance at an orientation to the diabetes camp APPE was mandatory and included review of the syllabus, goals, student responsibilities and activities at camp, required pre- and post-camp assignments, and methods of performance evaluation. The Academic Affairs Committee approved this 1-week APPE as equivalent to the College's other APPEs due to the time required to: (1) complete assignments before and after camp; (2) attend the 24-hour ACA-required staff orientation the day before camp, (3) spend 24-hours a day for 6 days with their campers; and (4) enter activities and interventions into the College's standardized web-based performance evaluation tool through the Pharmacy Educational Management System (PEMS).6
Table 2.
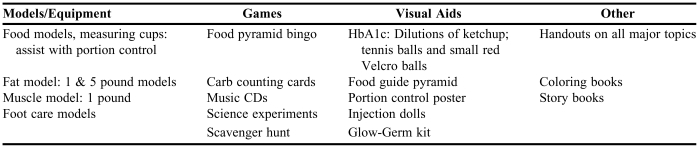
Educational Resources Provided at Camp Hertko Hollow
Student Roles at Camp
Students attended a mandatory staff orientation on the Saturday immediately prior to the first day of camp. Topics covered during this orientation included introduction of all key staff members, review of all personnel and responsibilities, review of camp protocols and camp safety, and educational “round robins” that reviewed insulin injection, information on insulin pumps, glucose meter operation, and the education sessions during camp. Pharmacy students were assigned to a group of campers who they would accompany during all daily program activities. Students slept in their group's cabin whenever appropriate.
Pharmacy students' primary function for the entire week was to assist the other CHH medical staff assigned to their cabin. During the evening, the faculty preceptor reviewed the camper profiles for each student's cabin and assisted students in gathering information related to the care of each camper. The following day, students assisted the faculty member or adjunct pharmacy preceptor at a medication station table during registration. Camper's medications were logged in, regimens properly transcribed, and individual camper medication drawers were set up for the medication cart. The cart was conveniently located at the entrance to the dining hall to serve as a visual reminder that medications were available for campers needing scheduled medications.
Students were responsible for distributing medications for 1 full day during camp. Administration of medications was documented on a medication distribution form and included the camper's name, time of medication administration, and the initials of the individual giving out the medication. At all times when medications were distributed, a licensed pharmacist was present to monitor and supervise this activity.
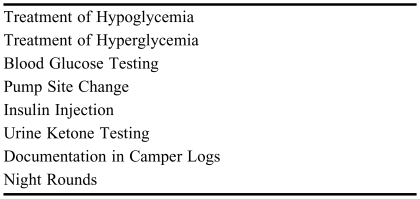
The pharmacy students monitored all aspects of diabetes care including testing camper's blood glucose, reinforcing proper insulin injection technique, accurately counting carbohydrates, accurately documenting blood glucose levels in campers' logbooks, and checking urine ketones, as well as performed basic problem-solving regarding insulin pumps, and observed campers for signs of hypo- and hyperglycemia. Students arranged time to review the logbooks for the campers in their cabin during the afternoon when the physicians were reviewing the books to make insulin adjustments. Students were required to sign-up for at least one session of night rounds. Night rounds consisted of small teams of medical staff members that visited cabins between 1:00 am and 3:00 am to check the blood glucose levels of campers flagged by the camp physicians or by the cabin staff. Students were assigned to 1 of 3 roles on the night rounds team: checking blood glucose, treating hypoglycemia per camp protocol, or documenting all team activities in each camper's logbook. Students were encouraged to sign up with a team that visited the student's cabin in order to gain a better understanding of the problems encountered with the children in their cabin and learn to anticipate problems before they occur.
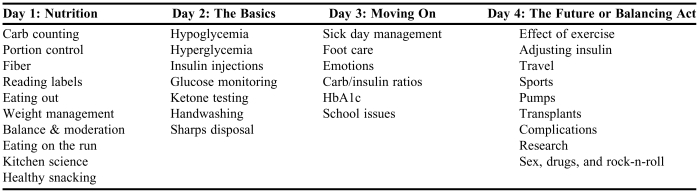
Students were assigned to teach at least one education session topic such as foot care, recognition and treatment of low blood sugar, how to properly inject insulin, and carbohydrate counting (Table 3). Prior to attending the camp, the preceptor forwarded materials to the students that would help them prepare for their session and additional materials were available at camp.
Table 3.
Daily Educational Sessions and Topics Presented to Campers During a Diabetes Camp APPE
Finally, students spent time at the health lodge organizing the medication cupboards, checking for outdated drugs, observing insulin pump changes, and assisting in first-aid situations as appropriate for their educational level.
Camper Program
Activity sessions constituted the core of the daily schedule and were interspersed among regularly scheduled meals and snacks, blood sugar monitoring, and insulin injections. Blood sugar monitoring with glucose meters was performed a minimum of 4 times a day, typically before meals and before bedtime. Activity sessions included recreational activities such as canoeing, horseback riding, and swimming, as well as daily formal diabetes education. Diabetes educators and other medical staff members provided these 45-minute sessions using a variety of educational resources, including models, interactive tools, and printed materials (Table 4). Pharmacy students had to present at least 1 topic and act as teaching assistants as needed during all other sessions. Daily themes encompassed specific topics for each of the 4 days when campers attended educational sessions. Topic themes for each day were: Day 1, Nutrition; Day 2, The Basics; Day 3, Moving On; Day 4, The Future or Balancing Act, depending on the age group (Table 3). The content and format of the sessions was kept flexible to accommodate different age groups attending a specific week. Day 5 was a general assembly for the entire camp and featured a speaker who shared his/her personal story of success despite having diabetes.
Table 4.
List of Protocols for a Diabetes Camp for Children and Teenagers
Other learning opportunities (teachable moments) for campers occurred during each meal when food items and their nutritional value were posted in the dining room to assist campers in counting carbohydrates. Dietetic interns and registered dieticians assisted campers with accurate estimation of carbohydrate intake and documented actual intake in the camper's logbooks. Pharmacy students assisted the dieticians during meal times as they worked with individual campers on meal calculations and recording results. In order to educate campers on proper testing and action steps needed based on test results, CHH staff closely monitored campers at other times, such as when they were testing their blood glucose or checking their urine for ketones.
Camp protocols guide situations related to clinical management such as when to check ketones, when and how to treat hypoglycemia, and procedures to follow for hyperglycemia (Table 5). Prandial insulin injection was performed in a separate air-conditioned building, referred to by campers as the “Shoot ‘em Up Shack,” which was close to the dining hall to take into account the rapid glycemic lowering effect of the newer bolus insulin analogs. Physicians and nurses were scheduled to monitor camper's insulin injection technique during every injection time. Pharmacy students observe campers during this activity and made suggestions for improvement when needed. Children using insulin pumps (affectionately called “pumpers”) self-administered their insulin boluses at the beginning of their meal, though some were allowed by camp physicians to inject the insulin immediately after their meal. Pumpers were monitored during the meal to ensure that boluses were not missed and to ensure the correct match of insulin to carbohydrate intake. Problems with insulin pumps or skin insertion site changes were handled by nurses and physicians in the Good Health Lodge.
Table 5.
Goals for Pharmacy Students Participating in a Diabetes Camp APPE
Assessment Methods
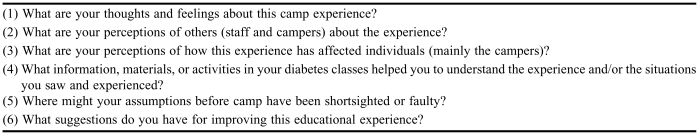
Students had to write both a pre-camp and a post-camp reflection paper. The guided list of questions for the post-camp paper is included in Table 6. These papers were not graded on strict criteria but had to be submitted for the student to receive credit for the APPE, as did all diabetes camp APPE assignments. The reflection papers were intended to have students explore their own thoughts and feelings about this unique experience, assist them in their mental preparation, and allow them to gain a deeper meaning of how they grew as a result of the camp experience.
Table 6.
Guided Questions for Post-Camp Reflection Paper*
Adapted from reference 13
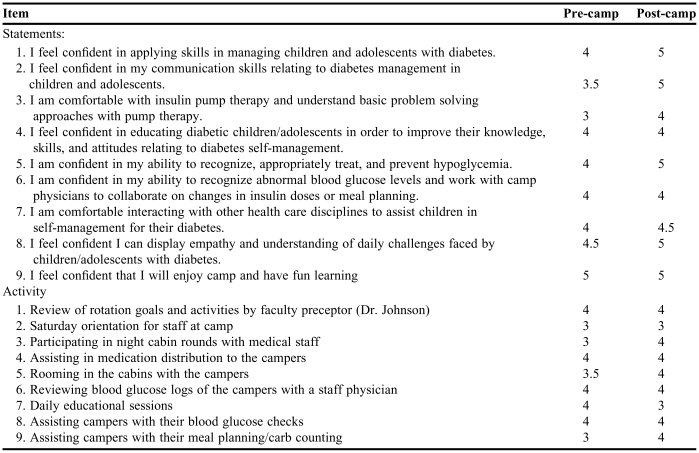
Students were also required to complete a pre- and post-camp self-assessment survey of their confidence level regarding their knowledge and performance of skills related to diabetes camp responsibilities and the value of the planned activities.
Their final assessment was conducted using the web-based PEMS system, the same instrument used for rating student performance in all of the College's APPEs. Students entered their activities and the interventions they performed for each day, and these were rated 1 through 5 by the faculty preceptor based on how well the student performed and how much assistance or prompting was needed from the preceptor.
In addition to the reflection papers and self-assessment surveys, students had to complete a series of educational modules and test questions developed by CHH diabetes educators and linked to the CHH web site. This assured that core areas were understood by all camp staff members and provided a foundation for principles that were reinforced during the mandatory staff orientation. Students also had to read the articles “Diabetes Care at Diabetes Camps”7 and “Celiac Disease: Wheat Ails You?”8 and were encouraged to review their class notes particularly in areas of insulin activity profiles, insulin administration technique, operation of various glucose meters, and management of hypo- and hyperglycemia. Links to the web sites of manufacturers of the glucose meters used at the camp were provided to enable students to review proper operation of the meters. Students had already received meter operation information and training either in the diabetes concentration or in professional diabetes electives, but refreshing student's knowledge immediately prior to camp gave them greater confidence in meter operation. Video tapes were available for students regarding insulin injection, glucose meter operation, and insulin pump operation if additional review was needed before camp. Each week the team of students was asked to brainstorm on 1 or 2 fun educational games for the campers that could be included during the formal education sessions or at other times.
During camp, students were advised to keep brief notes on their daily activities and interventions, which had to be entered into PEMS within the week following camp. The faculty preceptor met with students as a group at the end of every day for a debriefing session and to discuss interesting cases that arose during the day.
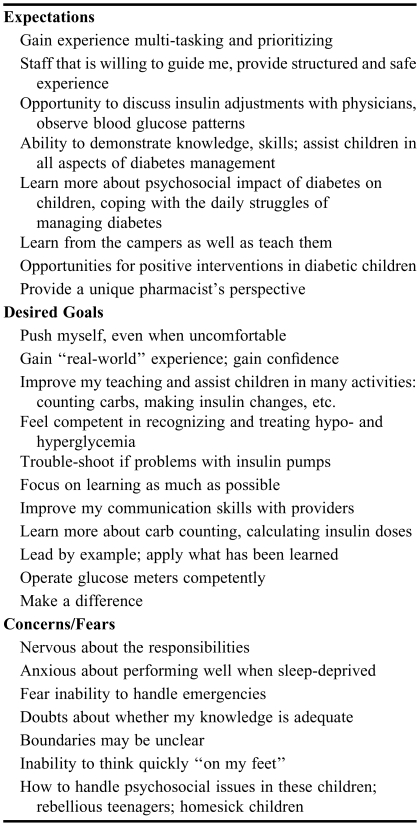
ASSESSMENT
Thirty-five pharmacy students have completed the CHH diabetes camp APPE since 2001. In 2006, 8 pharmacy students participated in the camp and completed reflection papers. A summary of themes extracted from pre-camp reflection papers is included in Table 7. Students recognized that they would play dual roles as teacher and student during the camp, and were open to learning about diabetes from both the providers and the campers. They also expected to play active teaching roles and to offer a pharmacist's perspective on diabetes care and education. The most common concerns students expressed were that they would not be able to handle an emergency or would not be able to respond as quickly as needed, and that they would be challenged by teenage campers and have to deal with behavioral issues.
Table 7.
Summary of Themes from 2006 Pre-Camp Reflection Papers
Post-camp reflection papers revealed a transformation of student's attitudes, knowledge, and self-confidence. Post-camp reflection papers showed improvement in student's attitudes about the physical limitations of diabetes, as reflected by several students' observation of how much children with diabetes behaved “just like normal kids.” The papers also showed an improved level of confidence in many areas of diabetes management.
Prior to and at the completion of camp, students completed a survey instrument that asked them to rank 9 statements on a 1-5 Likert scale regarding their confidence in and knowledge of specific areas of diabetes management encountered at camp. They were also asked to rank 9 different activities that they would be completing during camp based on their perceived value of the activity. A summary of pre- and post-camp survey results that relate to student's level of confidence in their knowledge and skills at baseline and as a result of the camp experience is included in the first section of Table 8. These results were consistent with comments shared by previous students and results of previous post-camp surveys. Responses to 6 of the 8 statements were higher after camp than before camp. Students had more confidence in their skills in diabetes management, communication, insulin pump therapy, hypoglycemia recognition and treatment, interaction with other health disciplines, and in their ability to display empathy and an understanding of the daily challenges of diabetes management. Activities that students rated higher in value after completing the APPE were night rounds, rooming with the campers in cabins, and assisting campers with carbohydrate counting. Activities that were rated lower after attending the camp included daily education sessions and assisting in the health lodge.
Table 8.
Pharmacy Students' Responses* to Pre- and Post-Camp Surveys (N = 8)
Responses are stated as the median
Likert scale used: 1 = strongly disagree 2 = disagree 3 = neutral 4 = agree 5 = strongly agree
DISCUSSION
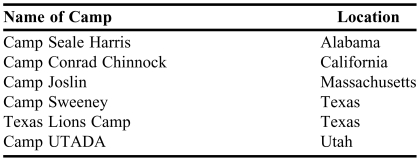
The development of empathy is essential to pharmacists in relating to the needs of patients.9 Imbedding students in the highly interactive experience of a diabetes camp can greatly assist in deepening this professional trait as well as enhancing their knowledge and abilities in working directly with people affected by this chronic condition. Yet, there are few published articles that highlight medical camps in general as a service-learning APPE option for pharmacy students. Kirwin et al described an asthma camp that served as a service-learning APPE and how 40% of participating students believed their attitudes had changed as a result of the experience.10 Condren et al described a diabetes camp experience and reported positive evaluations by students in addition to an increased interest in the APPE over time.11 This APPE differs from these in that it requires enrollment in the diabetes concentration as a prerequisite for participation, is self-contained and not a portion of another APPE, grants students credits equivalent to other APPEs, and requires completion of pre- and post-camp reflection papers and survey instruments. Other camps include pharmacists on their staff, and a few other colleges are affiliated with diabetes camps across the country (Table 9). The Diabetes Education and Camping Association (DECA) has a list of contacts for colleges who may desire further information on availability of camps in their state.12
Table 9.
Diabetes Camps With Pharmacist, Pharmacy Faculty Members, and/or Pharmacy Student Involvement11
This was also an excellent opportunity for interprofessional development for students as they worked with physicians and nurses to better understand how insulin adjustments are made in real-world situations where changes in meals and exercise patterns in a camp environment can have a significant impact on insulin requirements. Students benefitted from committed preceptors who were comfortable managing diabetes and served as role models for the interdisciplinary care provided during this experience. Daily group and individual meetings with students ensured that students received frequent feedback and support in this unique experiential environment.
The activities rated highest both before and after camp and those activities for which ratings improved will be retained in this APPE. The lower rating in the post-camp survey instrument regarding the daily educational sessions will help us to better prepare students to participate in the education sessions and will encourage camp leadership to provide better guidance to all staff regarding the organization of the education sessions. This observation was made not only by students but also by many staff members who had responsibility for teaching during these sessions. Operational and personnel changes are already being planned for future camps. The other activity rated lower after camp by students was assisting in the health lodge. Students did not feel this was a productive use of their time, which could have been better spent supervising insulin injections before meals or participating in other activities.
The data analysis was restricted to that of a pilot analysis and is mainly descriptive in nature given the small sample size. As we accumulate more students in the pre/post comparisons, we hope to be able to more rigorously analyze the differences between confidence in knowledge and abilities before and after camp in the future.
Interest in the diabetes camp APPE has remained high among students and continues to grow. The only limitation is the number of students one preceptor can adequately supervise and mentor. The current faculty preceptor will encourage other faculty members to consider volunteering as medical staff and precepting students in order to expand opportunities for this APPE.
The camp leadership also feels it is essential to grow the next generation of camp medical staff volunteers by exposing students to the diabetes camp, thereby sustaining the essential core of volunteers needed to ensure safe and competent care of the campers. Every year at least 1 student from the previous year who has graduated and become a licensed pharmacist volunteers to work at the diabetes camp, and some return for several years after that.
CONCLUSION
A diabetes camp APPE improved student's confidence in their knowledge and ability to manage diabetes. Activities highly rated by students will be continued and other activities rating lower will be reassessed. Interest in the APPE continues to grow. All colleges are encouraged to consider developing a service-learning experience or APPE at/around a diabetes camp to better prepare students to serve patients with this disease.
ACKNOWLEDGEMENTS
Thanks to Denise Soltis, BS, RPh, and Ed Bell, PharmD, for review of this manuscript. Thanks also to the leadership and volunteers of Camp Hertko Hollow; the YMCA staff.; my dedicated students; and the kids with diabetes and their families who teach us every day.
REFERENCES
- 1.Johnson JF, Chesnut R, Tice BP. An advanced diabetes care course as a component of a diabetes concentration. Am J Pharm Educ. 2003;67(1):160–70. Article 21. [Google Scholar]
- 2.Chapdelaine A, Ruiz A, Warchal J, Wells C, editors. Service-learning Code of Ethics. Bolton, Mass: Anker Publishing Company; 2005. Overview of service-learning. [Google Scholar]
- 3.Smith RE, Kerr RA, Nahata MC, Roche VF, Wells BG, Maine LL. Engaging communities: academic pharmacy addressing unmet public health needs. Report of the 2004-05 Argus Commission. Am J Pharm Educ. 2005;69(5) Article S22. [Google Scholar]
- 4.Camp Hertko Hollow: Iowa's camp for children with diabetes. Des Moines, IA: Camp Hertko Hollow; 2007. Available at: www.Camphertkohollow.com. Accessed February 17, 2007.
- 5.Butler DA, Lawlor MT. It takes a village: helping families live with diabetes. Diabetes Spectrum. 2004;17:26–31. [Google Scholar]
- 6.Education Management Systems. Glendale, Az: ROI Solutions Group; 2007. Available at: http://www.memsweb.com/. Accessed February 23, 2007.
- 7.American Diabetes Association. Diabetes care at diabetes camps. Diabetes Care. 2006;29(Supplement 1):S56–8. [PubMed] [Google Scholar]
- 8.American Diabetes Association. Celiac disease: wheat ails you? Available at: http://www.diabetes.org/type-1-diabetes/celiac-disease.jsp. Accessed February 15, 2007.
- 9.Barner JC. Implementing service-learning in the pharmacy curriculum. Am J Pharm Educ. 2000;64:260–5. [Google Scholar]
- 10.Kirwin JL, VanAmburgh JA, Napoli KM. Service-learning at a camp for children with asthma as part of an advanced pharmacy practice experience. Am J Pharm Educ. 2005;69(3):321–9. Article 49. [Google Scholar]
- 11.Condren M. Diabetes camp as an experiential clerkship site. Am J Pharm Educ. 2003;67(4) Article 119. [Google Scholar]
- 12.Diabetes Education and Camping Association. Available at: www.diabetescamps.org. Accessed February 17, 2007.
- 13.Eyeler J. Nashville, Tenn: Vanderbilt University; 1996. A practitioner's guide to reflection in service-learning. [Google Scholar]