Abstract
Objectives
To assess pharmacy faculty members' perceptions of the Rx for Change tobacco cessation program materials and train-the-trainer program.
Methods
Pharmacy faculty members attended a 14.5 hour train-the-trainer program conducted over 3 days. Posttraining survey instruments assessed participants' (n = 188) characteristics and factors hypothesized to be associated with program adoption.
Results
Prior to the training, 49.5% of the faculty members had received no formal training for treating tobacco use and dependence, and 46.3% had never taught students how to treat tobacco use and dependence. Participants' self-rated abilities to teach tobacco cessation increased posttraining (p < 0.001). The curriculum materials were viewed as either moderately (43.9%) or highly (54.0%) compatible for integration into existing curricula, and 68.3% reported they were “highly likely” to implement the program in the upcoming year.
Conclusions
Participation in a national train-the-trainer program significantly increased faculty members' perceived ability to teach tobacco-related content to pharmacy students, and the majority of participants indicated a high likelihood of adopting the Rx for Change program at their school. The train-the-trainer model appears to be a viable and promising strategy for promoting adoption of curricular innovations on a national scale.
Keywords: tobacco cessation education, train-the-trainer, faculty development, assessment
INTRODUCTION
Over the past 3 decades, extensive research has led to the documentation of considerable evidence-based knowledge in feasible and effective treatments for tobacco use and dependence.1 Timely and effective dissemination of this information to health practitioners, who are well positioned to render tobacco cessation counseling to their patients, remains an important public health priority. Previous evaluations of tobacco-related curricular content suggest that most graduates of health professional schools receive limited training and are ill-equipped to treat tobacco use and dependence.2-6 Indeed, surveys of practicing clinicians suggest few healthcare providers have received comprehensive training for providing tobacco cessation counseling to patients.7-10
The train-the-trainer model has been increasingly used in the education of students in the healthcare professions11-16 and for continuing education of licensed clinicians.17-20 The approach appears to be useful in meeting the educational needs of the health care system by increasing the knowledge and skills of providers. Furthermore, staff development programs may improve employee retention.17 Recent evaluations of physician train-the-trainer programs in preventive medicine,11 evidence-based medicine,12 managed care,13 and end-of-life care14 have reported significant improvements in faculty participants' knowledge and self-assessed ability to teach these content areas.
The train-the-trainer approach has become a promising method for disseminating tobacco counseling knowledge. In a large-scale initiative cosponsored by the National Cancer Institute, 53 seminars were conducted with 2,098 health professional volunteers from 22 states to enhance their ability to train their colleagues in smoking cessation techniques.19 This initiative demonstrated the advantages of the train-the-trainer approach when training a large number of participants. Heath and colleagues conducted a national train-the-trainer program for 30 nurse practitioner faculty members and observed significant improvements in the participants' self-assessed ability to teach tobacco-related content. Twelve-month follow-up evaluations revealed a significant increase in the curricular hours devoted to tobacco education in acute care nurse practitioner programs. The percentage of programs teaching at least 3 hours of tobacco-related content increased from 22.2% to 74.1% (p < 0.001).21
In 2000, faculty members from 3 schools of pharmacy in California developed Rx for Change: Clinician-Assisted Tobacco Cessation, a comprehensive tobacco cessation curriculum for pharmacy students.22 Early success with the program in California22,23 and extensive interest from other health disciplines led to subsequent expansion of the program to enhance applicability for other health disciplines, and to development of a national faculty training program with the goal of promoting broad-scale dissemination using a train-the-trainer approach. Through funding from the National Institutes of Health, we conducted a series of 5 train-the-trainer programs during the summers of 2003-2005 for faculty members from schools of pharmacy across the United States. To our knowledge, this was the first systematic attempt within any health discipline to target broad-scale dissemination and evaluation of a shared curricular resource among all accredited colleges. As such, the uniqueness of this initiative affords an unprecedented opportunity to study the process of diffusion of an innovation across a discipline, and to explore predictors of adoption of that innovation. In this report, we present evaluation data from the important first step of this initiative: our faculty train-the-trainer programs.
METHODS
Prior to submission of our grant application, faculty investigators attempted to identify 1 to 2 faculty members at each school of pharmacy who (1) were interested in attending a train-the-trainer program on use of a shared curriculum for treating tobacco use and dependence, (2) either currently taught tobacco use and dependence or planned to teach it in the near future (pharmacy practice and behavioral science faculty were targeted), and (3) were capable of incorporating the Rx for Change program22 into an existing course or a new course at their school of pharmacy. These faculty members were asked to complete a baseline survey instrument assessing the tobacco content in their school's curriculum during the 2001-2002 academic year.4 Two faculty members from the 81 (of 82; 98.8% response) schools that completed the baseline survey then were recruited to the larger dissemination study. As new pharmacy schools opened during the funding period, our target population for dissemination increased to 91 schools. Recruited faculty members completed an informed consent document that delineated the study procedures, which included attending a train-the-trainer program, completing a posttraining survey (described here), implementing the Rx for Change program at their school, administering pretraining and posttraining survey instruments to students, and completing annual survey instruments for 3 years to assess the tobacco content in their pharmacy school curriculum on an ongoing basis. Because our program advocates team-teaching, we encouraged faculty members from the same school to attend a train-the-trainer session together. Costs associated with travel and participation in the program were covered by grant funds. Continuing education credit (14.5 hours) and all program materials were provided to participants at no charge. All study procedures and measures have been approved by the Committee on Human Research at the University of California San Francisco, the Committee on Human Research at Yale University (prior institution of the Principal Investigator), and the Committee on the Use of Human Research Subjects at Purdue University.
Each train-the-trainer program was conducted over a 3-day period, beginning late Saturday afternoon and ending at noon on Monday. The opening session included introductions, a motivational speech by a key leader in either pharmacy or public health, and a presentation describing the history and vision of the Rx for Change program. The remainder of the training program focused on presenting the Rx for Change material (described elsewhere)22 with an emphasis on the delivery and implementation aspects of the program. Faculty members who had been involved in the development and had been teaching the Rx for Change program for the previous 4 years were speakers for the sessions. Presentations consisted of the core modules of the Rx for Change program (including hands-on training with the various pharmaceutical agents for cessation), the “Forms of Tobacco” module, the introductory video segment, role playing with case scenarios, and trigger tapes. A separate session addressed the logistics of course implementation and study procedures and an overview of the Rx for Change web site (http://rxforchange.ucsf.edu). At the end of the program, through a group brainstorming session, participants explored possible methods for implementation at each participating school.
At the conclusion of the training, participants completed an 8-page survey instrument assessing key factors hypothesized to be associated with adoption of the Rx for Change program. Sociodemographic factors that were assessed included sex, age, race/ethnicity, academic level, area of expertise, years in current position, whether the participant had ever smoked (smoked 100 or more cigarettes in lifetime), and current tobacco use status. The survey instrument also assessed whether participants had previously received formal training in treating tobacco use and dependence, or in teaching students how to treat tobacco use and dependence. Response options for each item included no prior training, some training, and extensive training. Additionally, we assessed whether participants previously had taught class lectures, class laboratories or programs (eg, role playing with case studies), or continuing education programs for tobacco cessation, or had facilitated tobacco cessation group programs for patients, worked as a clinician in a setting that specialized in providing tobacco cessation counseling to patients, and/or served as a preceptor for students in a setting that specialized in providing tobacco cessation counseling to patients. Perceived changes in teaching ability, as a result of participation in the train-the-trainer program, were assessed by asking participants how they would have rated their overall ability to teach comprehensive tobacco cessation to students before the training, and how they would rate their ability “now,” after the training. Finally, participants were asked to estimate the percentage of the program content that was (1) completely new, (2) taught before but a necessary review, and (3) an unnecessary review (so that the estimated percentages for 1 through 3 totaled 100%).
For each of the following components, the survey instrument assessed overall quality (1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent), overall usefulness (1 = not at all, 2 = a little, 3 = moderately, 4 = very, 5 = extremely useful), and overall likelihood of use (1 = not at all, 2 = a little, 3 = moderately, 4 = very, 5 = extremely likely) of the following: PowerPoint lecture slides, instructor notes that accompany the PowerPoint lecture slides, case scenarios for role playing, instructor guidelines that accompany case scenarios, introductory video segment, trigger tapes, ancillary student handouts, the Rx for Change web site (which had not yet been launched prior to the 2003 trainings, but was described to participants, in concept). Scores are presented for videotaped counseling sessions only for the 2004 participants, as these were not available at the time of the 2003 trainings.
Three principal components analyses were conducted, omitting the “videotaped counseling sessions” item, to determine the appropriateness of forming a scale for the perceived overall quality, overall usefulness, and overall likelihood of use constructs. Each of the 3 solutions presented as single-component scales, accounting for 57.3%, 60.7%, and 47.0% of the variance, respectively. All component loadings were at least 0.59, and Cronbach alpha estimates of internal consistency were 0.89, 0.91, and 0.83, respectively. Given these results, we computed scale scores for each of these constructs as an average of the constituent items. Detailed psychometric data are available from the authors upon request.
Using Rogers' Diffusion of Innovations as a theoretical framework,25 we assessed participants' perceptions associated with adoptability of the Rx for Change program: (1) compatibility for integration into the existing curriculum structure, (2) relative advantage over other tobacco cessation training programs that are available, (3) relative advantage over other tobacco cessation content that currently is taught in the curriculum, (4) acceptability of the complexity of implementing Rx for Change, (5) comprehensiveness of content, (6) appropriateness of teaching methodologies used, (7) clarity of the Faculty Coordinator's Guide in terms of its ability to facilitate program implementation, (8) confidence in their skills for teaching the Rx for Change materials and (9) likelihood of adoption of Rx for Change. Response options included 0 = none, 1 = low, 2 = moderate, 3 = high.
For each of the curriculum modules (core and optional), we assessed perceived importance (1 = not at all, 2 = a little, 3 = moderately, 4 = very, and 5 = extremely important) and perceived likelihood of adoption (1 = definitely not, 2 = probably not, 3 = not sure, 4 = probably yes, 5 = definitely yes) during the upcoming academic year. We also specifically asked participants if they personally had the ability to determine whether the Rx for Change materials would be integrated into their school's curriculum. Response options included yes, no, and not sure.
Using a 5-point scale (1 = not at all, 2 = a little, 3 = moderately, 4 = very, and 5 = extremely important), we assessed a series of perceived potential barriers to program adoption. These included lack of available curriculum time, financial resources, faculty expertise for this topic, faculty interest in tobacco-related issues, faculty's perceived importance of tobacco-related issues as applicable to a pharmacist's practice, access to comprehensive, evidence-based resources for teaching tobacco-related content, and available clinical training sites that focus primarily on tobacco cessation interventions.
Additional measures included (1) the anticipated total number of hours that would be dedicated to the Rx for Change materials in the upcoming academic year, (2) whether participants anticipated any major barriers to administering pretraining and posttraining survey instruments to students and (3) whether participants would recommend the train-the-trainer program to (a) other pharmacy faculty members and (b) other health professional faculty members (outside of pharmacy) who might be interested in teaching comprehensive tobacco cessation to their students.
Statistical analyses involved computation of simple summary statistics to characterize the questionnaire responses. Group comparisons were made using chi-squared tests of independence and comparisons of group means, as appropriate. In all cases, comparisons of means were made using both parametric and nonparametric tests, and the conclusions were the same; as such, parametric results were chosen for presentation to aid interpretability. Analyses were conducted using SPSS for Windows, Version 10.1.3 (SPSS, Inc, Chicago, Ill).
RESULTS
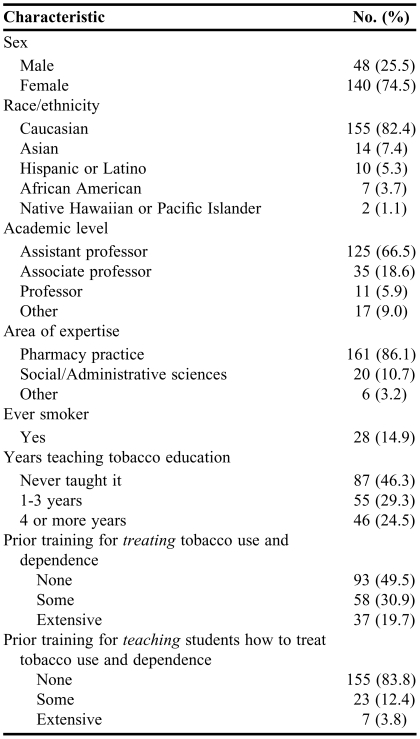
From 2003-2005, 191 pharmacy faculty members (Table 1) representing 89 of the 91 targeted schools of pharmacy (98%) consented and participated in our dissemination study and attended 1 of our 5 train-the-trainer programs. Of these participants, 188 (98.4%) completed the posttraining survey instrument. Most were women, at the assistant professor level, with pharmacy practice as their area of expertise. The median age was 32 years (range, 25-67 years), and participants had been working in their current position for a median of 3 years (range, 0-37 years). Fewer than half (41.5%) had previously taught class lectures on tobacco, 26.1% had taught class laboratories or class programs (eg, role playing with case studies) on tobacco cessation, 16.0% had taught continuing education programs on tobacco, 25.0% had facilitated tobacco cessation group programs for patients, 37.2% had worked as a clinician in a setting that specialized in providing tobacco cessation counseling to patients, and 28.2% had served as a preceptor for students in a setting that specialized in providing tobacco cessation counseling to patients. Approximately half (50.5%) had prior training for treating tobacco use and dependence, and 16.2% had prior training for teaching this topic.
Table 1.
Characteristics of Faculty Members Who Participated in a Train-the-Trainer Program for Tobacco Cessation
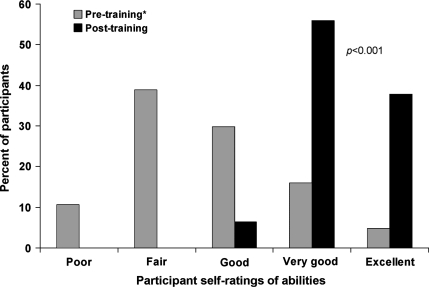
On average, participants reported that 30.3% of the training program content was new to them, 46.0% was a necessary review, and 23.6% was an unnecessary review. After the training, the proportion of faculty members rating their confidence for teaching the Rx for Change program as “high,” or “moderate” was 73.3% and 26.7%, respectively. Overall, we observed a significant increase (2.65 ± 1.03 versus 4.31 ± 0.59; t 187 = 27.7, p < 0.001) in self-reported abilities to teach tobacco cessation training to pharmacy students (Figure 1). Significantly higher change scores (p < 0.001) were observed for faculty members with no prior training for treating tobacco use and dependence (n = 93; mean change, 1.87 ± 0.80) versus faculty members with some or extensive prior training (n = 95; mean change, 1.45 ± 0.80). Similarly, we observed higher change scores (p < 0.001) for faculty members with no prior training for teaching this topic (n = 155; mean change, 1.77; SD, 0.78) versus faculty members with some or extensive prior training (n = 30; mean change, 1.17 ± 0.83).
Figure 1.
Faculty self-ratings of overall ability to teach comprehensive tobacco cessation to pharmacy students (n = 188). *Assessed posttraining: “Before the conference, how would you have rated your overall ability to teach comprehensive tobacco cessation to your students?”
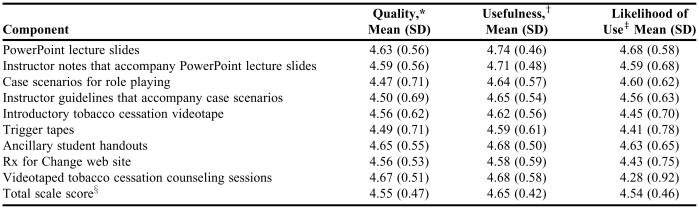
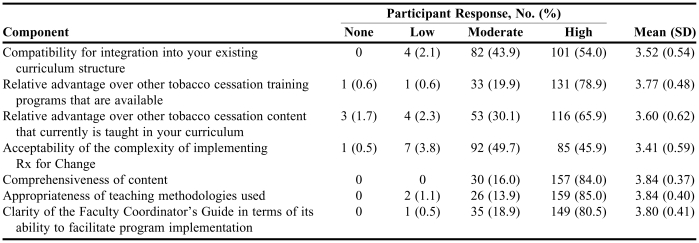
Table 2 presents the perceived quality, usefulness, and likelihood of use of the Rx for Change program components. Mean ratings, which ranged from 1 to 5 for each item, were at least 4.47 for perceived quality, at least 4.58 for perceived usefulness, and at least 4.28 for likelihood of use. The scale scores for each of these constructs were significantly (all p values < 0.001) interrelated: perceived quality and perceived usefulness, r = 0.72; perceived quality and perceived likelihood of use, r = 0.45, and; perceived usefulness and perceived likelihood of use, r = 0.59. Perceived attributes of the Rx for Change program (according to Rogers' Diffusion of Innovations Theory) are presented in Table 3.
Table 2.
Faculty Perceived Quality, Usefulness, and Likelihood of Using the Rx for Change Program Components (n = 188)
*Rating scale used: 1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent
†Rating scale used: 1 = not at all useful, 2 = a little useful, 3 = moderately useful, 4 = very useful, 5 = extremely useful
‡Rating scale used: 1 = not at all likely, 2 = a little likely, 3 = moderately likely, 4 = very likely, 5 = extremely likely
§Omits videotaped tobacco cessation counseling sessions item for 2003 participants, as this component was not available at that time
Table 3.
Rating scale: 1 = none, 2 = low, 3 = moderate, 4 = high
Values might not sum to 188 because of missing data
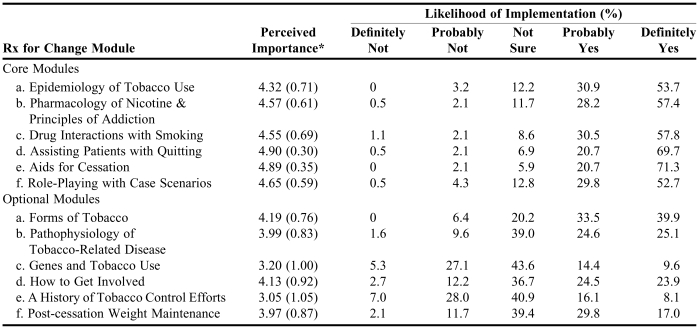
Just over two thirds (68.3%) of respondents indicated a high likelihood of adopting Rx for Change at their institution during the upcoming academic year; 29.0% indicated moderate likelihood, 2.2% indicated low likelihood, and 0.5% indicated no likelihood. Table 4 presents respondents' perceived importance of implementing each curriculum module into the required curriculum at their institution, and likelihood of implementation in the upcoming academic year. The modules perceived to be most important were Assisting Patients with Quitting, Aids for Cessation, and Role Playing with Case Scenarios.
Table 4.
Faculty Perceptions of the Likelihood of Implementing the Individual Rx for Change Modules During the Upcoming Academic Year (n = 188)
*Mean (standard deviation); 1 = not at all important, 2 = a little important, 3 = moderately important, 4 = very important; 5 = extremely important
Of 7 potential barriers to program adoption, lack of available curriculum time was rated most highly; 26.1% and 33.0% of respondents rated this barrier as very or extremely important, respectively. Other potential barriers, and the corresponding percentage of respondents who perceived the barrier to be very or extremely important (combined), included lack of clinical training sites that focus primarily on tobacco cessation interventions (31.4%), lack of financial resources (14.9%), lack of faculty perceived importance of tobacco-related issues as applicable to a pharmacist's practice (11.7%), lack of faculty interest in tobacco-related issues (10.7%), lack of faculty expertise for this topic (9.1%), and lack of access to comprehensive, evidence-based resources for teaching tobacco-related content (6.4%).
More than half (57.8%) of participants reported that they personally had the ability to influence or determine whether the Rx for Change materials would be integrated into their institution's curriculum; 25.1% were not sure, and 17.1% did not have the ability. When asked how many total hours of tobacco cessation content they anticipated teaching at their school during the upcoming academic year, the median was 6.0 hours (interquartile range, 4 hours to 8 hours), with the distribution of responses as follows: 0 hours, 2.8%; 2 to 3 hours, 15.6%; 4 hours, 12.2%; 5 hours, 5.6%; 6 hours (the minimum recommended), 25.6%; 7 hours, 2.2%; 8 hours, 21.1%; more than 8 hours, 15.0%. While the scale scores for perceived likelihood of use of the materials were associated with the anticipated number of minutes of teaching (Kendall's tau-b = 0.17, p < 0.005); the scale scores for perceived quality and usefulness of the materials were not. Lack of available curriculum time was the only barrier that was associated with the anticipated number of minutes to be implemented in the upcoming academic year (p < 0.05).
Nearly all (97.3%) participants indicated that they would recommend the program to other pharmacy faculty members who might be interested in teaching comprehensive tobacco cessation to their students (2.7% were unsure), and 97.9% would recommend the program to faculty members from other health professional schools (eg, medical, nursing, dental) who might be interested in teaching comprehensive tobacco cessation to their students (2.1% were unsure).
DISCUSSION
In this nationwide evaluation, we observed a significant increase in faculty members' self-rated confidence and ability to provide comprehensive tobacco cessation training to pharmacy students following participation in the train-the-trainer program. Nearly all (93.6%) of the participants rated their overall ability to teach comprehensive tobacco cessation to pharmacy students as very good or excellent following completion of the training. This finding is notable because the program attendees, in general, were relatively inexperienced in the area of tobacco cessation. Forty-six percent of the participants had never taught tobacco-related content previously, and nearly half had never received formal training for treating tobacco use and dependence.
As described elsewhere, Rx for Change incorporates varied interactive instructional techniques (role playing, “hands-on” demonstration exercises, and trigger tape exercises) and visually stimulating content (videos with interviews of tobacco users, and “model” cessation counseling sessions) to address different learning styles and to facilitate skills development. The vast majority of faculty participants rated the interactive instructional components of the curriculum as “very” or “extremely” useful and indicated they were “very” or “extremely” likely to incorporate all of these instructional methods when teaching tobacco cessation at their institution. These data are encouraging given that interactive, skills-based training programs have been shown to be more effective in developing professional skills and promoting behavioral change compared to traditional didactic lecture programs.24
The Rx for Change tobacco cessation curriculum, its national dissemination plan, and the evaluation of the dissemination process were developed and grounded in Everett Rogers' Diffusion of Innovations Theory. The theory characterizes the process by which an innovation is communicated through various channels, over time, among the members of a social system.25 In brief, stages through which an innovation is put into practice include knowledge (the extent to which a target population is aware of the innovation and have at least basic understanding of its functions), persuasion (forming a favorable attitude toward the innovation), decision (a member of the target population engages in activities that lead to the choice to adopt or reject an innovation), implementation (the innovation is put to use), and confirmation (reinforcement based positive outcomes associated with use of the innovation). With a curricular innovation, factors influencing the rate of program adoption include attributes of the curriculum—relative advantage, compatibility, complexity, trialability (the extent to which the innovation can be experimented with), and observability—and characteristics of the faculty members responsible for teaching the materials, as well as the channels of communication used to disseminate the curriculum and the underlying educational system. In applying the Diffusion of Innovations concept to dissemination of the Rx for Change program, the relative advantage of the Rx for Change curriculum is that turnkey, evidence-based teaching materials and training were provided at no cost to faculty members, thereby reducing the amount of time and effort that individual instructors would put forth in order to develop similar content. The program's modular format is conducive to the program's adoption (addressing compatibility with existing coursework), in that the program can be either incorporated within one course or spread across different courses (such as a therapeutics or communication course and patient care skills laboratory). Additionally, the curriculum web site offers faculty and student support (thereby reducing perceived complexity). Because the program was pilot tested extensively in California from 2000 to 2003, the trialability of the curriculum was well established prior to nationwide dissemination (this factor usually affects the early adopters of an innovation). Through newsletters, presentations, and publications, the observability of the Rx for Change program was enhanced on a national level prior to and during the dissemination phase. Based on posttraining measures specifically designed to assess factors associated with diffusion of an innovation, we anticipate high level adoption of the Rx for Change program nationwide. Faculty participants consistently rated the curriculum high in terms of comprehensiveness and quality of materials. Importantly, the majority of faculty members indicated the curriculum was compatible for integration within their existing curricular structure. Nearly 70% of participants indicated they were “highly” likely to implement the Rx for Change program, and overall, they estimated they would teach a median of 360 minutes of tobacco-related content in the upcoming academic year. This compares favorably with data we obtained from a 2001-2002 survey of 82 schools of pharmacy (98.8% response rate) where a median of 170 minutes of tobacco education was provided to students during the entire doctor of pharmacy degree program.
While our data suggest the train-the-trainer model appears to be a viable approach for effective broad-scale dissemination of a comprehensive tobacco cessation curriculum, our future years of data collection will yield data to further characterize the usefulness of the model in promoting our primary endpoint of interest, which is program adoption (and maintenance of adoption). An important area for future research is to validate self-reported data with observational data, such as actual ability (versus perceived ability) to teach tobacco cessation. Strengths of this study include its large sample size, relative to other train-the-trainer initiatives, and careful consideration of relevant theory at the stages of (1) innovation development, (2) dissemination planning, and (3) evaluation. Regardless, our study is not without limitations. To enhance the rate of adoption at each school of pharmacy, members of our research team directly contacted instructors responsible for teaching the courses most relevant to tobacco cessation counseling. In doing so, we achieved high levels of participation (89 of 91 targeted schools) and identified motivated faculty members with a vested interest in the Rx for Change training program, and this likely influenced participant reports for constructs such as “perceived importance” of the content. However, pursuant to Diffusion of Innovations Theory, we conversely could assert that this potential for item response bias was an acceptable risk given the positive tradeoff of identifying faculty champions (ie, what Rogers would term “change agents”) at each school, and these change agents would subsequently strive for program adoption. Improvements in faculty members' self-assessed teaching abilities and plans for increased tobacco-related instruction were reported, and objective, long-term follow-up data (collected annually for 3 years) to document these changes are forthcoming. Furthermore, because our measurements relied on self-reported ratings, our results are inherently susceptible to social desirability bias.
Our evaluation of improvement in the participants' perceived ability to teach tobacco-related content was assessed by a retrospective pretraining and posttraining self-evaluation of teaching abilities. While a posttest-only design typically is considered to be a less powerful assessment of an intervention than is a pretest/posttest design for single-group studies, the educational literature suggests that retrospective pretest/posttest self-assessment ratings might be a more sensitive measure of assessing the the impact of a training program12,14,26-28 by controlling for response-shift bias.26 Response-shift bias refers to the change in the study participants' knowledge or understanding of the material as a result of the educational intervention. That is, participants may provide elevated pretraining assessments of their abilities because they do not yet fully appreciate their lack of knowledge in a given content area until after participation in an education program. A retrospective self-evaluation of pretraining/posttraining abilities might therefore be a more accurate measure of the impact of an education training program. Indeed, we observed this phenomenon in our study of students participating in Rx for Change training programs.23 We observed a significant difference between students' pretraining assessment of their overall ability to counsel for tobacco cessation and their subsequent posttraining assessment of their pretraining ability. The self-reported pretraining and posttraining overall ability to help patients quit using tobacco increased significantly (p < 0.001), from an average of 1.89 to 3.53, and posttraining assessments of pretraining abilities (mean = 1.5; “Before attending this class, how would you have rated your overall ability to help patients quit using tobacco?”) were significantly lower than were pretraining assessments of the same ability (p < 0.001).
CONCLUSION
We have developed and implemented a national faculty training program to promote dissemination and adoption of a comprehensive, evidence-based tobacco cessation curriculum for pharmacy students. Participation in the train-the-trainer program significantly increased faculty members' perceived ability to teach tobacco-related content to pharmacy students, and the majority of participants indicated a high likelihood of adopting the Rx for Change program at their institution. As such, the train-the-trainer model appears to be a viable and effective strategy for promoting adoption of shared, curricular innovations on a national scale. In this time of limited resources, and with recent increases in the number of pharmacy schools despite a shortage and high turnover of qualified pharmacy faculty, shared, evidence-based curricula are needed.
ACKNOWLEDGMENTS
The authors would like to acknowledge Eunice Chung, Berit Gunderson, and Leanne Sakamoto for their significant contributions during the early development and implementation of the Rx for Change curriculum and train-the-trainer programs. Bruce Berger, Ken Lem, Beth Martin, Steven Schroeder, Mary Kate Sullivan, and Frank Vitale also were instrumental to the success of the programs. Finally, we would like to thank Rx for Change faculty members across the country for their thoughtful and constructive feedback, continued enthusiasm, and assistance in promoting tobacco cessation counseling education for pharmacy students nationwide.
This study was made possible through funding from the National Cancer Institute (grant R25 90720 to K. Hudmon). The hands-on portion of the Aids for Cessation module was made possible in part through product donations from Pfizer, Inc., GlaxoSmithKline, and PICS, Inc. Harriett Bennett at the Agency for Healthcare Research and Quality kindly provided all participants with copies of the full and abbreviated Clinical Practice Guideline for Treating Tobacco Use and Cessation.
REFERENCES
- 1.Fiore MC, Bailey WC, Cohen SJ, et al. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2000. Treating tobacco use and dependence. Clinical practice guideline. [Google Scholar]
- 2.Grinstead CL, Dolan TA. Trends in U.S. dental schools' curriculum content in tobacco use cessation 1989-93. J Dent Educ. 1994;58:663–7. [PubMed] [Google Scholar]
- 3.Heath J, Andrews J, Thomas SA, et al. Tobacco dependence curricula in acute care nurse practitioner education. Am J Crit Care. 2002;11:27–33. [PubMed] [Google Scholar]
- 4.Hudmon KS, Bardel K, Kroon LA, et al. Tobacco education in U.S. schools of pharmacy. Nicotine Tob Res. 2005;7:225–32. doi: 10.1080/14622200500055392. [DOI] [PubMed] [Google Scholar]
- 5.Spangler J, George G, Foley K, et al. Tobacco intervention training: current efforts and gaps in US medical schools. JAMA. 2002;288:1102–9. doi: 10.1001/jama.288.9.1102. [DOI] [PubMed] [Google Scholar]
- 6.Wewers ME, Kidd K, Armbruster D, et al. Tobacco dependence curricula in U.S. baccalaureate and graduate nursing education. Nurs Outlook. 2004;52:95–101. doi: 10.1016/j.outlook.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Hu S, Pallonen U, McAlister AL, et al. Knowing how to help tobacco users. Dentists' familiarity and compliance with the clinical practice guideline. J Am Dent Assoc. 2006;137:170–9. doi: 10.14219/jada.archive.2006.0141. [DOI] [PubMed] [Google Scholar]
- 8.Hudmon KS, Prokhorov AV, Corelli RL. Tobacco cessation counseling: pharmacists' opinions and practices. Patient Educ Couns. 2006;61:152–60. doi: 10.1016/j.pec.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Sarna LP, Brown JK, Lillington L, et al. Tobacco interventions by oncology nurses in clinical practice: report from a national survey. Cancer. 2000;89:881–9. [PubMed] [Google Scholar]
- 10.Cantor JC, Baker LC, Hughes RG. Preparedness for practice. Young physicians' views of their professional education. JAMA. 1993;270:1035–40. doi: 10.1001/jama.270.9.1035. [DOI] [PubMed] [Google Scholar]
- 11.Albright CL, Farquhar JW, Fortmann SP, et al. Impact of a clinical preventive medicine curriculum for primary care faculty: results of a dissemination model. Prev Med. 1992;21:419–35. doi: 10.1016/0091-7435(92)90051-i. [DOI] [PubMed] [Google Scholar]
- 12.Green ML. A train-the-trainer model for integrating evidence-based medicine training into podiatric medical education. J Am Podiatr Med Assoc. 2005;95:497–504. doi: 10.7547/0950497. [DOI] [PubMed] [Google Scholar]
- 13.Peters AS, Ladden MD, Kotch JB, et al. Evaluation of a faculty development program in managing care. Acad Med. 2002;77:1121–7. doi: 10.1097/00001888-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Stratos GA, Katz S, Bergen MR, et al. Faculty development in end-of-life care: evaluation of a national train-the-trainer program. Acad Med. 2006;81:1000–7. doi: 10.1097/01.ACM.0000242475.41549.66. [DOI] [PubMed] [Google Scholar]
- 15.Barratt MS, Moyer VA. Effect of a teaching skills program on faculty skills and confidence. Ambulatory Pediatr. 2004;4(1 Suppl):117–20. doi: 10.1367/1539-4409(2004)004<0117:eoatsp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 16.Scherrer CS, Dorsch JL, Weller AC. An evaluation of a collaborative model for preparing evidence-based medicine teachers. J Med Libr Assoc. 2006;94:159–65. [PMC free article] [PubMed] [Google Scholar]
- 17.Bess CA, LaHaye C, O'Brien CM. Train-the-Trainer Project meets organization's strategic initiative for retention and continuous learning. J Nurses Staff Dev. 2003;19:121–7. doi: 10.1097/00124645-200305000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Burr CK, Storm DS, Gross E. A faculty trainer model: increasing knowledge and changing practice to improve perinatal HIV prevention and care. AIDS Patient Care STDs. 2006;20:183–2. doi: 10.1089/apc.2006.20.183. [DOI] [PubMed] [Google Scholar]
- 19.Epps RP, Manley MW, Husten CG, et al. Transfer of preventive health programs to physicians' practices through medical organizations. Am J Prev Med. 1998;14:25–30. doi: 10.1016/s0749-3797(97)00011-1. [DOI] [PubMed] [Google Scholar]
- 20.Robinson K, Sutton S, von Gunten CF, et al. Assessment of the Education for Physicians on End-of-Life Care (EPEC) Project. J Palliat Med. 2004;7:637–45. doi: 10.1089/jpm.2004.7.637. [DOI] [PubMed] [Google Scholar]
- 21.Heath J, Kelley FJ, Andrews J, et al. Evaluation of a tobacco cessation curricular intervention among acute care nurse practitioner faculty members. Am J Crit Care. 2007;16:284–9. [PubMed] [Google Scholar]
- 22.Hudmon KS, Corelli RL, Chung E, et al. Development and implementation of a tobacco cessation training program for students in the health professions. J Cancer Educ. 2003;18:142–9. doi: 10.1207/S15430154JCE1803_07. [DOI] [PubMed] [Google Scholar]
- 23.Corelli RL, Kroon LA, Chung EP, et al. Statewide evaluation of a tobacco cessation curriculum for pharmacy students. Prev Med. 2005;40:888–95. doi: 10.1016/j.ypmed.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 24.Davis D, O'Brien MA, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 25.Rogers EM. Diffusion of Innovations. 5th ed. New York: Free Press; 2003. [Google Scholar]
- 26.Howard GS, Daily PR. Response-shift bias: a source of contamination of self-report measures. J Appl Psychol. 1979;64:144–50. [Google Scholar]
- 27.Skeff KM, Stratos GA, Bergen MR. Evaluation of a medical faculty development program. A comparison of traditional pre/post and retrospective pre/post self-assessment ratings. Eval Health Professions. 1992;15:350–66. [Google Scholar]
- 28.Bray JH, Howard GS. Methodological considerations in the evaluation of a teacher-training program. J Educ Psychol. 1980;72:62–70. [Google Scholar]