Abstract
A case of a left small finger tumour that was diagnosed on histopathological review as Nora’s lesion (bizarre parosteal osteochondromatous proliferation) is reported. There have been fewer than 150 cases reported in the literature to date and its pathophysiology is yet to be defined. Due to its rare presentation, Nora’s lesion can easily go unrecognized and therefore inappropriately managed.
Keywords: Bizarre parosteal osteochondromatous proliferation, Nora’s lesion
Abstract
Les auteurs présentent ici un cas de tumeur de l’auriculaire dont le diagnostic à l’examen histopathologique est une tumeur de Nora (ou prolifération ostéochondromateuse parostéale bizarre). À ce jour, moins de 150 cas de cette nature ont été répertoriés dans la littérature et sa physiopathologie n’a pas encore été bien définie. En raison de sa rareté, la tumeur de Nora peut facilement passer inaperçue et par conséquent, le traitement adéquat risque de n’être pas instauré.
Nora’s lesion, also known as bizarre parosteal osteochondromatous proliferation (BPOP), is a rare, benign, exostotic osteochondromatous tumour of the hands and feet that is uncommonly related to trauma (1–5). There have been fewer than 150 cases reported in the literature to date and its pathopathology is yet to be defined (1–4,6–8). Due to its rare presentation, Nora’s lesion can be easily unrecognized and treated inappropriately.
We report a case of left small finger mass that, on histopathological review, revealed Nora’s lesion. The patient’s presentation was delayed, requiring aggressive surgical management in the form of a ray amputation, and he remains recurrence-free two years postoperatively. We present a case history of a patient with BPOP, review the pertinent literature and offer a treatment strategy for the management of BPOP.
CASE PRESENTATION
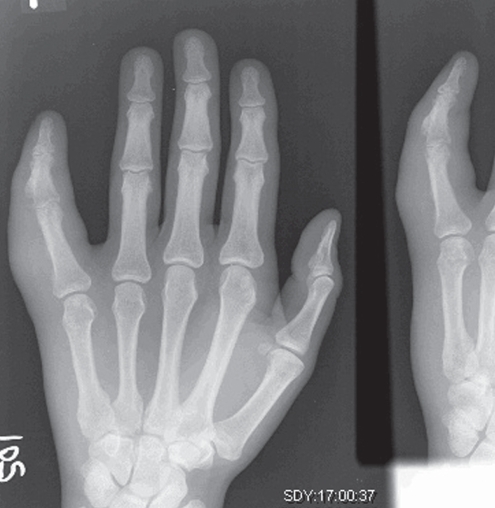
A 32-year-old man was referred to plastic surgery with a history of an enlarging mass in the left small finger. The patient reported having suffered a penetrating laceration in the same anatomic location 10 years earlier, which was managed with primary wound closure. Approximately two months before presenting to the Section of Plastic Surgery at Wayne State University, Detroit, Michigan, he was evaluated at a community hospital for pain in the left small finger and gradual, progressive limitation of range of motion. A radiograph was performed and a bone density exostosis of the left small digit, middle phalanx, was noted (Figure 1). The mass was biopsied and histopathology revealed proliferative and haphazardly arranged spindle cells and chondrocytes, with new and calcified bone, suggestive of BPOP, whereupon the patient was referred for further management.
Figure 1).
Radiograph demonstrating bone density exostosis of proximal middle phalanx of the left small finger
Upon presentation approximately two months following biopsy, the patient’s symptoms included increased swelling and further loss of digital function. On clinical evaluation, the tumour was located in the dorsal ulnar aspect of the left small finger’s middle phalanx, extending toward the proximal phalanx (Figure 2). There was limited extension of the small finger and the tumour was firm and fixed to the underlying tissues and bone.
Figure 2).
Initial clinical presentation with left small finger tumour
Due to the progressive swelling and functional limitations, magnetic resonance imaging (MRI) of the left hand was performed, results of which were suggestive of tumour involvement of the middle phalanx, extending proximally with involvement of the proximal phalanx (Figure 3). Due to the aggressive presentation, the patient underwent amputation of his left fifth ray (Figure 4). Grossly, the tumour measured 3.5 cm × 2.5 cm × 2.0 cm, and histopathological review of the specimen confirmed the diagnosis of Nora’s lesion (Figure 5) and tumour-free margins. No complications were observed postoperatively and the patient remained disease-free on two-year follow-up. The patient had a full range of motion of the remaining digits of the left hand and was able to participate with all activities of daily living, without limitation (Figures 6A and 6B).
Figure 3).
Magnetic resonance image revealing tumour progression to involve the medullary canal of the proximal phalanx
Figure 4).
Amputation of fifth ray
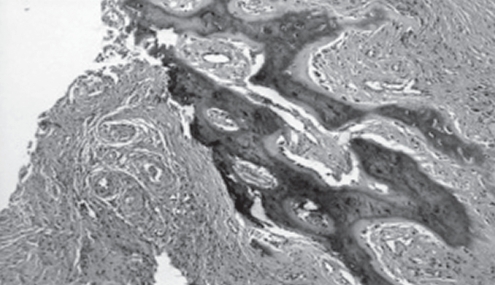
Figure 5).
Histopathology revealing proliferative and haphazardly arranged spindle cells, chondrocytes, with new and calcified bone, diagnostic of bizarre parosteal osteochondromatous proliferation
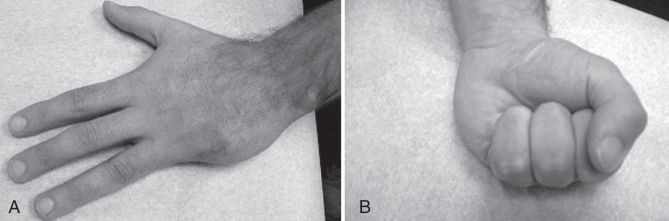
Figure 6).
A and B Two-year postoperative clinical presentation demonstrating full range of motion without tumour recurrence
DISCUSSION
BPOP is a lesion of osteochondromatous origin that was first described in 1983 by Nora et al (4). It remains a challenging diagnosis due to the extremely rare presentation and its clinical and radiological similarity to more common osteochondromatous tumours (6,9). This lesion is seldom related to trauma; however, it is purported that trauma played a role in the lesion’s etiology in our patient (1,3,10). Patients are most commonly in their third to fourth decades, and both sexes are affected equally (3,6). The tumour generally affects bones of the distal extremities (hands and feet), but can be found in the mandible and long bones (1,3). It usually presents as a minimally painful pedunculated mass that grows slowly over months or years (2,3); however, our patient demonstrated an aggressive growth pattern.
Both computed tomography and MRI may be effective in identifying Nora’s lesion (6,10). It can be differentiated from osteogenic tumours by the absence of cortical flaring of the affected bone, and from chondromatous tumours by the lack of communication with the underlying medullary canal (2–4,9). The MRI in our patient demonstrated some of these periosteal findings in the middle phalanx, although aggressive tumour involvement of the medullary space of the proximal phalanx was also demonstrated.
Histopathology clearly delineates this process from others. Nora’s lesion has three components in varying amounts: cartilage, bone and fibrous tissue (3,4). The cartilage usually forms a cap; less frequently, it is arranged in lobules separated by dense fibrous tissue with irregular maturation into bone (endochondral ossification) (3,4). The bone that is produced has a characteristic dark blue tinctorial quality, especially at the interface with the cartilage (3,4). The intertrabecular spaces contain proliferating spindle cells that lack cytological atypia (3,4). The cartilaginous component is hypercellular and contains irregular groups of binucleated and ‘bizarre’ chondrocytes (3,4). Although double-nucleated chondrocytes are common, hyperchromasia and cytological atypia are not present (3,4).
Due to the proliferative osteochondromatous composition and location of these lesions, the differential diagnosis includes osteochondroma, parosteal osteosarcoma, subungual exostosis, myositis ossificans and florid reactive periostitis. Furthermore, while osteochrondromas are the most common benign bone tumours, they are extremely uncommon in the distal extremities and are more likely to be found in long bones (1,3–5). Histologically, osteochondromas do not exhibit cytological atypia and show more regular alignment of chondrocytes (3,4). Parosteal osteosarcoma has been described in the hands, but is more common in long bones. Nora’s lesion can be differentiated from parosteal osteosarcoma by its lobular architecture, distinct blue tinctorial characteristic of their osteoid, small size, and slender, short and irregular bony trabeculae (3,4). Most importantly, the tumour lacks invasion into the adjacent muscle.
Although Nora’s lesion does not typically show metastatic capability, it can be locally aggressive and produce loss of vital hand functions, as illustrated with our patient (2). The literature is replete with reports suggestive of curative surgical resection when detected early; however, recurrence is seen in more than one-half of the cases and generally occurs between two months and two years postoperatively (2,3,6,8,9). Neither metastatic lesions nor death attributable to the tumour have previously been reported (3,6). Additionally, at the present time, there is no standardized screening protocol or follow-up regimen, given the rare presentation of this tumour.
CONCLUSIONS AND TREATMENT STRATEGY
BPOP is a diagnostic and therapeutic challenge. Although rare, it should always be considered in the differential diagnosis of any osteogenic or chrondromatous growth found in the hand. Following diagnostic confirmation with incisional biopsy, lesions presenting early are most appropriately treated with early excision of the pseudocapsule and periosteal tissue with decortication of any bony abnormalities (6). For tumours presenting in a delayed fashion, aggressive wide local resection and/or ray amputation are required to limit lesion progression and to restore function.
REFERENCES
- 1.Abramovici L, Steiner GC. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion): A retrospective study of 12 cases, 2 arising in long bones. Hum Pathol. 2002;33:1205. doi: 10.1053/hupa.2002.130103. [DOI] [PubMed] [Google Scholar]
- 2.Bandiera S, Bacchini P, Bertoni F. Bizarre osteochondromatous proliferation of bone. Skeletal Radiol. 1998;27:154. doi: 10.1007/s002560050355. [DOI] [PubMed] [Google Scholar]
- 3.Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion) Am J Surg Pathol. 1993;17:691. doi: 10.1097/00000478-199307000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Michelsen H, Abramovici L, Steiner G, Posner MA. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) in the hand. J Hand Surg. 2004;29A:520. doi: 10.1016/j.jhsa.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol. 1983;7:245. doi: 10.1097/00000478-198304000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Oviedo A, Simmons T, Benya E, Gonzales-Crussi F. Bizarre parosteal osteochondromatous proliferation: Case report and review of the literature. Ped Path. 2001;4:496. doi: 10.1007/s10024001-0048-8. [DOI] [PubMed] [Google Scholar]
- 7.Saygi B, Karadag-Saygi E, Erzik C, Erkan M, Yildirim Y. Bizarre parosteal osteochondromatous proliferation of the little toe. J Am Podiatr Med Assoc. 2006;96:158–61. doi: 10.7547/0960158. [DOI] [PubMed] [Google Scholar]
- 8.Soon JL, Chang HC, Sim CS, Teoh LC, Low CO. A case of bizarre parosteal osteochondromatous proliferation of the hand. Singapore Med J. 2003;44:27. [PubMed] [Google Scholar]
- 9.Brien EW, Mirra JM, Luck JV. Benign and malignant cartilage tumors of bone and joint: Their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. II. Juxtacortical tumors. Skeletal Radiol. 1999;28:1. doi: 10.1007/s002560050466. [DOI] [PubMed] [Google Scholar]
- 10.Resnick D, Kyriakos M, Greenway GD. Tumors and tumor-like lesions of bone: imaging and pathology of specific lesions. In: Resnick D, editor. Diagnosis of Bone and Joint Disorders. 3rd edn. Philadelphia: WB Saunders Co; 1995. pp. 3725–79. [Google Scholar]