Abstract
While previous research has consistently shown an association between depression and disability in the elderly, less is known about the mechanisms linking the two. Recent longitudinal population studies showed considerable inconsistency in the criteria used to establish causality and terms such as mediation and effect modification were frequently incorrectly applied in terms of the inferences drawn.
We underlines the necessity to adopt more stringent theoretical criteria for the establishment of intermediary effects in the relationship between depression and disability in order to better identify cross-validated potential intervention points for reducing the risk of disablement and depression.
Keywords: Aged, Longitudinal studies, Disability evaluation, Depression
While a considerable body of literature confirms the high co-occurrence of depression and disability in the elderly (Lenze et al., 2001), much less is known about the mechanisms linking the two. The increasing number of longitudinal observations now available makes the exploration of temporal pathways possible, however, such studies have also identified a large number of intervening factors which potentially modulate the relationship between the two, making health outcomes following either depression or disability difficult to predict or prevent. Failure to take into account the innate complexity of the cause-effect relationships involved has led to considerable confusion in our present understanding of the relationship between depression and disability. The conceptual framework (if any) used by most studies to establish mediating effects is seldom discussed in publications thus leading to considerable confusion in terminology and the use of inappropriate statistical methods.
Theoretical criteria for the establishment of mediation and moderation
Depression, like many other mental disorders, cannot be attributable to a single cause, but is increasingly recognized to lie along multiple causal chains involving, environmental, social, and biological risk factors which mediate the relationship with activity limitations. Causal chains are often complex in the case of psychiatric disorders as the pathology may both cause and be the result of the same mediating factors such as social, biological disturbances or at risk behaviours. Kraemer et al (Kraemer et al., 2008, Kraemer et al., 2001) have proposed a worthwhile theoretical model of this type of complex causal chain which may be used to validate causality and risk factor mediation within longitudinal data sets. In this model a mediator or intermediate variable is defined as a variable that occurs in a causal pathway from an independent to a dependent variable. It “causes” variation in the dependent variable (Y), and itself is subject to variation by the independent variable (X). The independent variable precedes the mediator (Me), it is correlated to Me and when X and Me are jointly analyzed either Me “dominates” X (total mediation) or X and Me codominate (partial mediation). Proving that X precedes Me is thus a key point in demonstrating mediation. A moderator or effect modifier refers to variations in the magnitude of the effect of the independent variable across levels of another variable. Mo moderates the association between X and Y, if Mo precedes X, Mo and X are not correlated and Mo and X codominate. Mo identifies subpopulations in which different causal chains operate or one causal chain operates differently (Kraemer et al., 2001). Moderators may thus be considered in relation to susceptibility or resiliency or buffering factors. A mediator is in a causal sequence between two variables, whereas a moderator is not part of this causal sequence (figure 1a and 1b).
Figure 1.
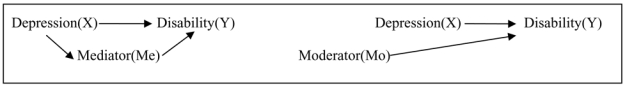
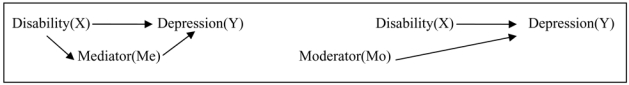
Figure 1a. Depression as risk factor for disability
Figure 1b. Disability as risk factor for depression
Establishment of mediating and moderating effects
Of the 24 longitudinal population studies which have been published to our knowledge since 2001 examining the association between depression or depressive symptomatology and activity limitation, 11 examined depressive symptomatology as a risk factor for activity limitation, 11 examined activity limitations as a risk factor for depressive symptomatology and 2 examined the reciprocal relationship. We found considerable inconsistency in the criteria used to establish causality and terms such as mediation and effect modification were frequently incorrectly applied in terms of the inferences drawn. Adjusting for a covariable measured at baseline and observing a decrease in the strength of the association between the main factor and the outcome does not prove that this covariable represents a mediating effect. Mediating effects should be defined as new events occurring during follow-up or as changes since baseline, and associations should be established by appropriate statistical models such as linear mixed models, generalized mixed models or multi-state models applied to longitudinal data. However, it should be noted that the use of linear mixed models may be questionable as the scales used to measure depression or disability are seldom normally distributed in the general population. We also observed that bias due to cohort attrition has rarely been taken into account in research in this area. Depression as well as disability may induce early dropouts and sensitivity analyses need to be undertaken to test the robustness of the results.
To illustrate the problem of defining effect mediators let us consider concomitant illnesses. Depression in late-life is frequently influenced by other conditions present at baseline: depression is common in older persons recovering from myocardial infarction or stroke and in those suffering from cancer, diabetes, hip fracture and cognitive impairment (Blazer, 2003). Depression may also induce physical illness including cardio- and cerebro-vascular disorders. Depressed individuals may have detrimental health habits (poor nutrition, smoking, alcohol, lack of exercise), which are risk factors for vascular illness. Immune dysfunction associated with depression may also be associated with increased risk of other pathologies such as cancer (Lenze et al., 2001). To demonstrate that diseases are mediating effects in the pathway leading from depression to disability, only new or worsening diseases occurring after depression onset and before disability should be considered. Pre-existing depression risk factors cannot be considered as mediators but rather as confounding factors. Such a distinction is important to explain the mechanism leading to disability and to find targets for intervention to prevent or postpone disability in depressed elderly persons.
Mediating and effect modification between depression and activity limitations
A number of potential factors have been proposed by previous studies but all require more stringent evaluation of their mediating effect: namely loss of motivation leading to self neglect, decrease in physical activity, poor nutrition inducing sarcopenia. Depression is also observed to induce lack of compliance with medical treatment (Bruce, 2001), isolation, and difficulties in coping with life events which in turn determine depression. Conversely, beneficial intermediate effects are observed due to psychiatric care, antidepressant prescription, improvement of social support and correction of sensorial impairment all of which may break the on-going chain to disability.
Several effect modifiers were found to be significant: pre-existing chronic disease (Geerlings et al., 2001), time (Lenze et al., 2005), cognition (Mehta et al., 2002) and baseline functional limitations (van Gool et al., 2005). Other factors have to be considered: gender, education, genetic and environmental factors, and history of pathologies. In particular women are known to have more depressive symptoms than men but seem to be less liable to depressive symptoms when suffering from physical health problems (Piccinelli and Wilkinson, 2000). High level of education is also associated with reduced rates of depression, but loss of functional capacities may be less accepted by educated people. On the other hand people with high income may more easily access help and home adaptations, thus decreasing the consequences of functional impairment. History of depression may also be an effect modifier rendering people less able to cope with loss of functional activity and conversely, the impact on disability of chronic depression being possibly stronger.
Mediating and effect modification between activity limitations and depression
Certain factors namely availability of a confidant, satisfaction with support, sense of control and self-esteem have been validated as mediators between activity limitations and depression incidence using appropriate analytic techniques (Yang, 2006). Dependency in daily tasks is a persistent chronic stressor leading to negative psychological outcomes such as loss of self-esteem which may also be symptoms of depression. Disability may also lead to restriction in social and leisure activities, and isolation which are important precipitants of depression. Anticipated support may be the key element for buffering the effects of this stressor and perceived support has in some cases been demonstrated to have a more significant mediating effect as opposed to objective support (Yang, 2006). With ageing and increased risk of multiple chronic disorders, the role of the caregiver may become more onerous and time consuming, creating tension between ageing parents, adult children, and spouses, with possible role inversion. Other potential mediators require further research, in particular physical rehabilitation was anticipated to change the course of both disability and depression (Bruce, 2001).
With regard to effect modifiers and possible stratifications, time or age (Anstey et al., 2007, Schnittker, 2005) and gender, race and social economic status (Schieman and Plickert, 2007) were found to be significant. But most of the effect modifiers suggested above for the reverse association should be considered providing that they precede activity limitation onset.
Conclusion
Recent longitudinal studies have identified a large number of factors which may impinge on the causal relationship between depression and disability. These mediating and moderating factors may vary according to the direction of the relationship being examined. Given the persistent variability in measures used for both depression and disability it is not currently possible to validate findings from one study by other observations or to conduct meta-analyses. We underline the necessity for future studies to adopt more stringent theoretical criteria for the establishment of intermediary effects in the relationship between depression and disability, to adopt a common language with regard to mediating and moderating effects and to work towards uniformity in case-identification in order to better identify cross-validated potential intervention points for reducing the risk of disablement and depression.
Acknowledgments
This work was supported in part by a grant from the Institut de Recherche en Santé Publique (IReSP), Paris, France.
Footnotes
Declaration of Interest: None
References
- Anstey KJ, von Sanden C, SargentCox K, Luszcz MA. Prevalence and risk factors for depression in a longitudinal, population-based study including individuals in the community and residential care. American Journal of Geriatric Psychiatry. 2007;15:497–505. doi: 10.1097/JGP.0b013e31802e21d8. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: review and commentary. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2003;58:249–65. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Bruce M L. Depression and disability in late life: directions for future research. American Journal of Geriatric Psychiatry. 2001;9:102–12. [PubMed] [Google Scholar]
- Geerlings SW, Beekman AT, Deeg DJ, Twisk JW, Van Tilburg W. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. Psychological Medicine. 2001;31:1361–71. doi: 10.1017/s0033291701004639. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27:S101–8. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–56. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, Schulz R, Reynolds CF., 3rd The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9:113–35. [PubMed] [Google Scholar]
- Lenze EJ, Schulz R, Martire LM, Zdaniuk B, Glass T, Kop WJ, Jackson SA, Reynolds CF., 3rd The course of functional decline in older people with persistently elevated depressive symptoms: longitudinal findings from the Cardiovascular Health Study. Journal of the American Geriatrics Society. 2005;53:569–75. doi: 10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- Mehta KM, Yaffe K, Covinsky KE. Cognitive impairment, depressive symptoms, and functional decline in older people. Journal of the American Geriatrics Society. 2002;50:1045–50. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. British Journal of Psychiatry. 2000;177:486–92. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Schieman S, Plickert G. Functional limitations and changes in levels of depression among older adults: a multiple-hierarchy stratification perspective. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62:S36–42. doi: 10.1093/geronb/62.1.s36. [DOI] [PubMed] [Google Scholar]
- Schnittker J. Chronic illness and depressive symptoms in late life. Social Science & Medicine. 2005;60:13–23. doi: 10.1016/j.socscimed.2004.04.020. [DOI] [PubMed] [Google Scholar]
- van Gool CH, Kempen GI, Penninx BW, Deeg DJ, Beekman AT, van Eijk JT. Impact of depression on disablement in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Social Science & Medicine. 2005;60:25–36. doi: 10.1016/j.socscimed.2004.04.021. [DOI] [PubMed] [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. Journal of Health and Social Behavior. 2006;47:355–72. doi: 10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]


