Abstract
AIM: To examine the long-term results of endoscopic treatment in a prospective study conducted over a period of 10 years, 1997 to January 2007.
METHODS: A total of 25 patients (20 female and five male: aged 18-75 years), with at least one symptom of stricture not passable with the standard colonoscope and with a confirmed scarred Crohn’s stricture of the lower gastrointestinal tract, were included in the study. The main symptom was abdominal pain. The endoscopic balloon dilatation was performed with an 18 mm balloon under endoscopic and radiological control.
RESULTS: Eleven strictures were located in the colon, 13 at the anastomosis after ileocecal resection, three at the Bauhin valve and four in the ileum. Four patients had two strictures and one patient had three strictures. Of the 31 strictures, in 30 was balloon dilatation successful in a single endoscopic session, so that eventually the strictures could be passed easily with the standard colonoscope. In one patient with a long stricture of the ileum involving the Bauhin valve and an additional stricture of the ileum which were 15 cm apart, sufficient dilatation was not possible. This patient therefore required surgery. Improvement of abdominal symptoms was achieved in all cases which had technically successful balloon dilatation, although in one case perforation occurred after dilatation of a recurrent stricture. Available follow-up was in the range of 54-118 mo (mean of 81 mo). The relapse rate over this period was 46%, but 64% of relapsing strictures could be successfully dilated again. Only in four patients was surgery required during this follow-up period.
CONCLUSION: We conclude from these initial results that endoscopic balloon dilatation, especially for short strictures in Crohn’s disease, can be performed with reliable success. Perforation is a rare complication. It is our opinion that in the long-term, the relapse rate is probably higher than after surgery, but usually a second endoscopic treatment can be performed successfully, leading to a considerable success rate of the endoscopic procedure.
Keywords: Crohn’s disease strictures, Balloon dilatation, Endoscopy, Morbidity, Mortality
INTRODUCTION
Strictures of the gastrointestinal tract are common complications of Crohn’s disease. Medical treatment can improve acute inflammation, but is ineffective in the presence of chronic scarred strictures. These strictures are mainly treated surgically. As well as techniques of surgical resection, especially for less extended strictures, reconstructive surgery (strictureplasty) is recommended, in order to minimize the risk of short bowel syndrome[1,2]. Strictureplasty is a bowel-conserving operation technique, requiring anesthesia and minimally invasive surgery or laparotomy. Regardless of which surgical technique is chosen, the reoperation rate for new strictures or recurrence of strictures is between 15% and 45% within 5 years[3,4].
For some time, it has been possible to treat benign strictures of the upper gastrointestinal tract with endoscopic balloon dilatation. Over the past 20 years, this method has become increasingly used for symptomatic Crohn’s strictures in the ileum or colon[5–16]. The available results indicate equal technical effectiveness of the endoscopic procedures when compared to surgical therapy. Up till now the method has not been standardized, for example regarding balloon diameters or possible concomitant medical treatment.
Valid long-term studies of 5 years or more, which would permit a statement regarding recurrence of strictures and a better comparison with surgical techniques[3,4], are available so far only in casuistic form and with limited numbers[8,17–19].
We report on our own prospective 10-year long-term study of endoscopic balloon dilatation of strictures in Crohn’s disease using a relatively thin balloon (18 mm) and additional treatment with prednisolone.
MATERIALS AND METHODS
In our prospective long-term study, conducted since 1997, we included patients who had at least one symptomatic ileal or colonic stricture which could not be passed with the standard colonoscope (external diameter 13 cm), in the presence of histologically documented Crohn’s disease. Additional inclusion criteria were: (1) obstructive symptoms (especially abdominal pain), refractory to medical treatment; (2) no or low inflammatory disease activity (CDAI < 200); (3) age over 18 years; (4) no fistulas connecting to the stricture; (5) length of the stenosis no more than 10 cm; (6) patient’s consent after being informed about the uncertain success of the method, with regard to current knowledge; (7) Either an enteroclysis (Sellink) or a colon contrast imaging examination was performed to exclude the presence of fistulas and determine the length of the stricture.
Patients were prepared for endoscopy with 4 L of Golytely solution. Premedication consisted of 2.5-5 mg midazolam and 50 mg meperidine. After the dilatation patients were monitored in the hospital for at least 24 h.
The balloon dilatation was carried out through the placed endoscope, under endoscopic and radiological control using a balloon of 55 mm in length and 18 mm in diameter (Olympus BC4). In a safe position within the stricture, the balloon was filled with diluted contrast medium for at least 2 min with a pressure of 2.0 at (= 19 6133 bar).
The dilatation was judged technically successful if the stricture appeared conspicuously larger during radiological control of the balloon diameter, and if it could be passed with the standard colonoscope.
Twenty five patients (20 female, five male) between the age of 18 and 75 years and with a disease duration of between 2 and 35 years (mean 13.3 years) were included in the study. There were 11 strictures located in the colon, 13 strictures at the anastomosis after ileocecal resection, three at the Bauhin’s valve and four in the ileum. Four patients had two, one patient had three strictures (Table 1). The length of the strictures was between 1 and 10 cm.
Table 1.
Patient characteristics
| Case number | Age/sex | Disease duration (yr) | Previous bowel surgery | Stricture localisation |
| 1 | 38/F | 17 | Ileocecal resection | Anastomosis |
| 2 | 22/F | 5 | None | Transverse colon |
| 3 | 23/F | 7 | None | Sigmoid, ileum |
| 4 | 23/M | 7 | appendectomy | Ileum |
| 5 | 33/F | 14 | None | Rectum/sigmoid |
| 6 | 33/F | 12 | Ileocecal resection | Anastomosis |
| 7 | 32/F | 9 | Anal fistula | Ileocecal valve |
| 8 | 46/F | 19 | Anal fistula | Colon |
| 9 | 28/F | 16 | Ileocecal resection, bowel perforation | Anastomosis |
| 10 | 35/F | 15 | Ileocecal resection | Anastomosis |
| 11 | 26/M | 7 | None | Ileocecal valve |
| 12 | 42/F | 20 | Right hemicolectomy anal fistula | Anastomosis |
| 13 | 48/F | 15 | None | Colon |
| 14 | 50/F | 10 | None | Colon |
| 15 | 50/F | 14 | Ileocecal resection | Anastomosis |
| 16 | 24/F | 6 | Ileocecal resection | Anastomosis |
| 17 | 55/F | 11 | Ileocecal resection, terminal ileum | Anastomosis |
| 18 | 43/F | 25 | Ileocecal resection, sigmoid resection | Anastomosis |
| 19 | 49/F | 35 | Ileocecal resection, right hemicolectomy | Anastomosis (2) |
| 20 | 75/M | 3 | None | Ileum |
| 21 | 42/M | 6 | Right hemicolectomy | Anastomosis |
| 22 | 34/F | 13 | Anal fissure | Anal channel, rectum, sigmoid |
| 23 | 26/F | 6 | None | Rectum, sigmoid |
| 24 | 18/F | 2 | None | Ileocecal valve |
| 25 | 26/M | 20 | Total colectomy, ileoanal pouch | Pouchanal anastomosis |
Regardless of pre-existing medical treatment, after the dilatation all patients received 3 g of peroral mesalamine and initially 50 mg of prednisolone, reducing the dosage gradually over a period of 2 mo.
Our follow-up period was between 54 and 118 mo (mean 81 mo). All patients were last seen in outpatient settings in January 2007 (recent medical history, clinical examination). The study was carried out in accordance with the Helsinki declaration.
RESULTS
In 30 of 31 strictures (24 of 25 patients) balloon dilatation was successful in one endoscopic session. Eventually the stricture could be passed easily with the standard colonoscope. Only in one patient with a long (about 10 cm) stricture of the ileum, involving the ileocecal valve, and an additional stricture of the ileum 15 cm distant, was the dilatation unsuccessful, so that surgery (ileocecal resection) had to be performed.
With the above mentioned premedication, 10 of 25 patients complained of moderate pain during the dilatation. In one patient with a recurrence of stricture, the second balloon dilatation was complicated by perforation (3%), and consequently the patient had to be operated on. Bleeding requiring treatment or rise of body temperature after dilatation were not observed.
With technical success, the treatment caused immediate improvement of abdominal pain, which was the main symptom in all 24 patients with successful dilatation.
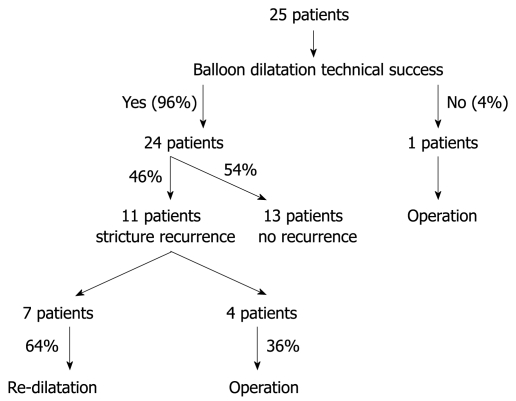
The follow-up period of the successfully dilated patients was between 54 and 118 mo (mean 81 mo). Thirteen of the successfully dilated patients did not have any symptoms indicating a stricture relapse up to the last follow-up in January 2007. In 11 cases, 3 to 77 mo (mean 32 mo) after successful dilatation, a stricture relapse developed which could not be passed with the colonoscope. Accordingly, after a mean follow-up of more than 6.5 years, the relapse rate was 46%. In seven patients with recurrent strictures, a second endoscopic balloon dilatation could be performed successfully, and in only four patients was surgery required (Figures 1 and 2). Thus the long-term success rate of balloon dilatation was 80% over a mean follow-up period of 81 mo.
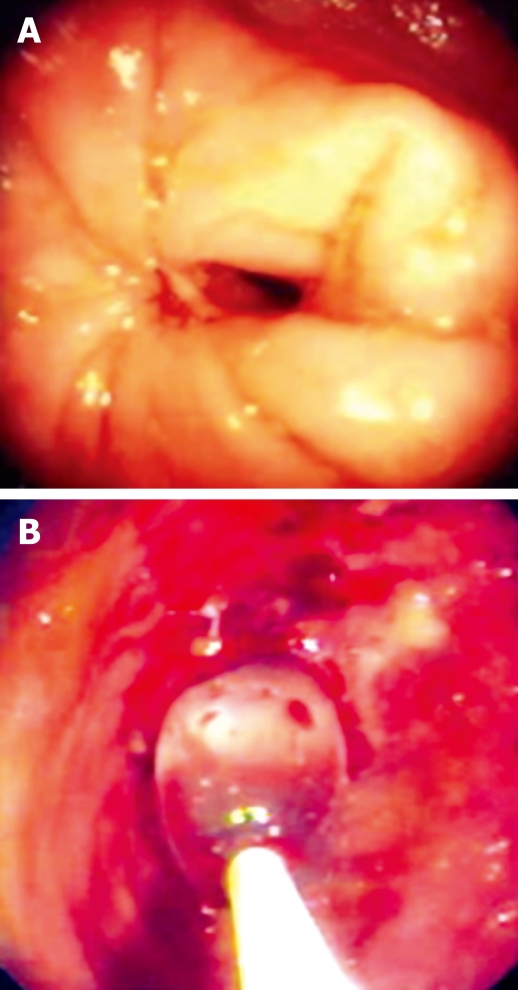
Figure 1.
Endoscopic view of a non-passable stricture. A: Ileum; B: An anastomosis, balloon in the stricture.
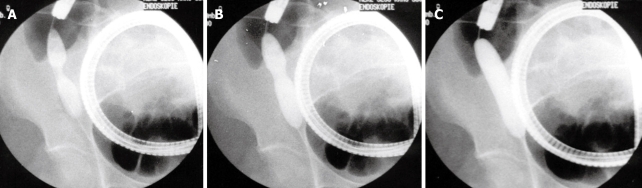
Figure 2.
Radiological image of the endoscopic dilatation of a short stricture in the ileum. A: Before dilatation; B: Beginning dilatation; C: Completed dilatation.
As accompanying medical treatment all patients received 3 g of peroral mesalamine and initially 50 mg of prednisolone, reducing the dosage gradually over a period of 2 mo. The results of all patients are summarized in Table 2 and Figure 3.
Table 2.
Results
| Case number | Stricture number | Complications | Follow-up (mo) | Time to relapse (months & method of therapy) |
| 1 | 1 | None | 118 | 77, dilatation |
| 2 | 1 | None | 112 | No relapse |
| 3 | 2 | None | 106 | Sigmoid: 10, dilation ileum: no relapse |
| 4 | 1 | None | 106 | 37, operation |
| 5 | 1 | None | 101 | No relapse |
| 6 | 1 | None | 99 | 30, dilatation |
| 7 | 1 | None | 97 | Unsuccessful dilatation, operation |
| 8 | 1 | None | 97 | No relapse |
| 9 | 1 | None | 89 | No relapse |
| 10 | 1 | None | 86 | No relapse |
| 11 | 1 | None | 84 | 15, operation |
| 12 | 1 | None | 79 | No relapse |
| 13 | 1 | None | 75 | No relapse |
| 14 | 1 | None | 75 | 24, operation |
| 15 | 1 | None | 73 | 55, dilatation |
| 16 | 1 | None | 73 | 40, dilatation |
| 17 | 1 | None | 71 | 48, dilatation |
| 18 | 1 | None | 67 | No relapse |
| 19 | 2 | None | 66 | No relapse |
| 20 | 2 | None | 65 | No relapse |
| 21 | 1 | None | 63 | 14, dilatation |
| 22 | 3 | None | 62 | No relapse |
| 23 | 2 | None | 57 | No relapse |
| 24 | 1 | Perforation | 54 | 4, operation |
| 25 | 1 | None | 54 | No relapse |
Figure 3.
Overview of all patients treated.
DISCUSSION
Endoscopic balloon dilatation has been used over a long period of time in the treatment of strictures of the upper gastrointestinal tract, sporadically also for Crohn’s strictures of the duodenum[20,21]. Balloon catheters suitable for transendoscopic dilatation of ileal and colonic strictures have made it possible to dilate Crohn’s strictures of the lower gastrointestinal tract.
In the studies published so far, balloons with an external diameter of 18-25 mm have been used, in order to enable the endoscopic dilatation of strictures of the lower gastrointestinal tract. The technical success rate, defined as achieving an endoscopically passable residual stricture, is between 70% and 90 %, independent of the balloon’s diameter[5–16]. Usually more than one dilatation session is required for every stricture. Complications such as hemorrhages are rare, while perforations are reported mostly in studies in which 25 mm balloons are used[5,8].
In the present study, single-session dilatations using an 18 mm balloon were technically successful in 97% of cases. In one case perforation occurred during attempted dilatation of a relapsing stricture (3%). Ramboer et al[12] exclusively used 18 mm balloons in 52 sessions involving 13 patients, without complications. This technique has the additional advantage that the dilatation set can be easily inserted through a standard colonoscope with a working channel of 3.2 mm in diameter. On the other hand, when using balloon catheters with a diameter of 25 mm, therapeutic colonoscopes with a larger working channel are required.
Unfortunately, results of comparative studies on the effectiveness of different balloon diameters and balloon lengths, on differences in duration and pressure of the dilatation, as well as on the number of dilatations per session in the treatment of Crohn’s strictures are still lacking. The accomplishment of achieving an endoscopically passable residual stricture seems to be important for the outcome. Couckuyt et al[8] found a statistically significant correlation between this achievement and the number of patients being free of symptoms over a longer observation period.
In our experience, intravenous midazolam and meperidine usually are sufficient as accompanying medication. Patients did not complain about a lot of pain during the intervention. Alternatively, in cases of painful procedures, the application of propofol can be considered.
At the moment, it is difficult to define the relapse risk after endoscopic balloon dilatation, as the published studies[8,17–19] are based on very different follow-up periods, and often do not represent structured prospective long-term studies.
In the present prospective long-term study, after a mean follow-up of more than 6.5 years, stricture relapses were observed in 11 patients (46%) after a mean of 32 mo. The other 13 successfully dilated patients were free of symptoms and stricture relapse over the complete follow-up period.
Endoscopic re-dilatation was successful in 64% of the patients with relapsing strictures. The long-term success rate was 80%. Our data indicate that long-term results of endoscopic balloon dilatation, repeated if necessary, are comparable to the results of surgical treatment[3,4]. The relapse rate after a single balloon dilatation is probably higher than after surgical intervention[3,4].
Whether additional medical treatment, such as steroid injection into the stricture, as suggested in case reports[7,11,12], or treatment with steroids after dilatation, can influence the recurrence rate is unknown. Follow-up studies after surgical bowel resection have shown that, after surgical treatment of Crohn’s strictures, local inflammatory signs develop rapidly at the anastomosis without clinical signs of a relapse[22].
Raedler et al[23] treated 30 patients after successful dilatation of ileocecal strictures with azathioprine 100 mg/d and budenoside 9 mg/d or with a placebo. After 6 and 12 mo, a statistically significantly greater number of symptoms due to strictures and more necessary surgical interventions were found in the placebo group.
In the present study, under hypothetic considerations, a 2-mo steroid treatment was performed after dilatation, aimed at reducing the early relapse rate. With one exception there were no early relapsing strictures in the first 6 mo, and only one repeat dilatation was necessary over this period. Definite conclusions, however, cannot be drawn from these data.
Considering all available results, the endoscopic balloon dilatation seems suitable for the treatment of Crohn’s strictures in the lower gastrointestinal tract especially in presence of scarred, short strictures. Our considerable clinical experience has shown us that in cases of multiple strictures, only one stricture should be dilated in each session. Strictures of more than 5 cm in length should instead be treated surgically. Fistulas originating from the stricture are considered contraindications for balloon dilatation.
The relapse rate after single endoscopic balloon dilatation, according to the results of the present long-term study, is probably somewhat higher than after surgery. But by repeatedly dilating relapsing strictures, surgery often can be avoided or delayed. The long-term success rate of endoscopic dilatation (repeated if necessary) of 80% is remarkable and has to be considered when comparing balloon dilatation with surgery.
COMMENTS
Background
Strictures of the gastrointestinal tract are common complications of Crohn’s disease. Medical treatment can improve acute inflammation, but is ineffective in the presence of chronic scarred strictures. These strictures are mainly treated surgically.
Innovations and breakthroughs
The available results indicate equal technical effectiveness of the endoscopic procedures, compared to surgical therapy. This is one of few studies to report prospective 10-year results. Furthermore, our study would suggest that endoscopic balloon dilatation seems suitable in the treatment of Crohn’s strictures, especially in presence of scarred, short strictures.
Applications
When considering treatment options for patients with Crohn’s disease, this study may show a safe and feasible alternative for therapeutic intervention in the treatment of patients with short, scarred strictures.
Peer review
The authors examined a total of 25 patients with at least one symptom of stricture, not passable with the standard colonoscope and with a scarred Crohn’s stricture of the lower gastrointestinal. The study revealed that endoscopic balloon dilatation especially for short strictures in Crohn’s disease, can be performed with reliable success. Perforation is a rare complication. The long-term relapse rate may probably be higher than after surgery, but usually a second endoscopic treatment can be performed successfully. The results are interesting and may show a safe and feasible alternative for therapeutic intervention in the treatment of patients with short, scarred strictures.
Peer reviewers: Naohiko Harada, PhD, Department of Gastroenterology, Fukuoka Higashi Medical Center, Chidori 1-1-1, Koga, Fukuoka 811-3195, Japan; Jamie S Barkin, MD, Professor of Medicine, Chief, Sinai Medical Center Division of Gastroenterology, Mt. Sinai Medical Center, University of Miami, School of Medicine, 4300 Alton Road, Miami Beach, FL 33140, United States
S- Editor Li LF L- Editor Logan S E- Editor Ma WH
References
- 1.Alexander-Williams J, Haynes IG. Conservative operations for Crohn‘s disease of the small bowel. World J Surg. 1985;9:945–951. doi: 10.1007/BF01655400. [DOI] [PubMed] [Google Scholar]
- 2.Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn's disease. Ann R Coll Surg Engl. 1982;64:229–233. [PMC free article] [PubMed] [Google Scholar]
- 3.Legnani PE, Kornbluth A. Therapeutic options in the management of strictures in Crohn’s disease. Gastrointest Endosc Clin N Am. 2002;12:589–603. doi: 10.1016/s1052-5157(02)00015-6. [DOI] [PubMed] [Google Scholar]
- 4.Tichansky D, Cagir B, Yoo E, Marcus SM, Fry RD. Strictureplasty for Crohn's disease: meta-analysis. Dis Colon Rectum. 2000;43:911–919. doi: 10.1007/BF02237350. [DOI] [PubMed] [Google Scholar]
- 5.Blomberg B, Rolny P, Jarnerot G. Endoscopic treatment of anastomotic strictures in Crohn's disease. Endoscopy. 1991;23:195–198. doi: 10.1055/s-2007-1010654. [DOI] [PubMed] [Google Scholar]
- 6.Breysem Y, Janssens JF, Coremans G, Vantrappen G, Hendrickx G, Rutgeerts P. Endoscopic balloon dilation of colonic and ileo-colonic Crohn’s strictures: long-term results. Gastrointest Endosc. 1992;38:142–147. doi: 10.1016/s0016-5107(92)70379-4. [DOI] [PubMed] [Google Scholar]
- 7.Brooker JC, Beckett CG, Saunders BP, Benson MJ. Long-acting steroid injection after endoscopic dilation of anastomotic Crohn’s strictures may improve the outcome: a retrospective case series. Endoscopy. 2003;35:333–337. doi: 10.1055/s-2003-38145. [DOI] [PubMed] [Google Scholar]
- 8.Couckuyt H, Gevers AM, Coremans G, Hiele M, Rutgeerts P. Efficacy and safety of hydrostatic balloon dilatation of ileocolonic Crohn’s strictures: a prospective longterm analysis. Gut. 1995;36:577–580. doi: 10.1136/gut.36.4.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferlitsch A, Reinisch W, Puspok A, Dejaco C, Schillinger M, Schofl R, Potzi R, Gangl A, Vogelsang H. Safety and efficacy of endoscopic balloon dilation for treatment of Crohn's disease strictures. Endoscopy. 2006;38:483–487. doi: 10.1055/s-2006-924999. [DOI] [PubMed] [Google Scholar]
- 10.Junge U, Zuchner H. [Endoscopic balloon dilatation of symptomatic strictures in Crohn's disease] Dtsch Med Wochenschr. 1994;119:1377–1382. doi: 10.1055/s-2008-1058848. [DOI] [PubMed] [Google Scholar]
- 11.Lavy A. Triamcinolone improves outcome in Crohn's disease strictures. Dis Colon Rectum. 1997;40:184–186. doi: 10.1007/BF02054985. [DOI] [PubMed] [Google Scholar]
- 12.Ramboer C, Verhamme M, Dhondt E, Huys S, Van Eygen K, Vermeire L. Endoscopic treatment of stenosis in recurrent Crohn’s disease with balloon dilation combined with local corticosteroid injection. Gastrointest Endosc. 1995;42:252–255. doi: 10.1016/s0016-5107(95)70101-x. [DOI] [PubMed] [Google Scholar]
- 13.Dear KL, Hunter JO. Colonoscopic hydrostatic balloon dilatation of Crohn’s strictures. J Clin Gastroenterol. 2001;33:315–318. doi: 10.1097/00004836-200110000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Singh VV, Draganov P, Valentine J. Efficacy and safety of endoscopic balloon dilation of symptomatic upper and lower gastrointestinal Crohn’s disease strictures. J Clin Gastroenterol. 2005;39:284–290. doi: 10.1097/01.mcg.0000155128.31208.44. [DOI] [PubMed] [Google Scholar]
- 15.Thomas-Gibson S, Brooker JC, Hayward CM, Shah SG, Williams CB, Saunders BP. Colonoscopic balloon dilation of Crohn's strictures: a review of long-term outcomes. Eur J Gastroenterol Hepatol. 2003;15:485–488. doi: 10.1097/01.meg.0000059110.41030.bc. [DOI] [PubMed] [Google Scholar]
- 16.Williams AJ, Palmer KR. Endoscopic balloon dilatation as a therapeutic option in the management of intestinal strictures resulting from Crohn’s disease. Br J Surg. 1991;78:453–454. doi: 10.1002/bjs.1800780421. [DOI] [PubMed] [Google Scholar]
- 17.Sabate JM, Villarejo J, Bouhnik Y, Allez M, Gornet JM, Vahedi K, Modigliani R, Lemann M. Hydrostatic balloon dilatation of Crohn's strictures. Aliment Pharmacol Ther. 2003;18:409–413. doi: 10.1046/j.1365-2036.2003.01715.x. [DOI] [PubMed] [Google Scholar]
- 18.Solt J, Hertelendi A, Szilagyi K. [Balloon catheter dilatation of lower gastrointestinal tract stenoses: long-term results] Orv Hetil. 2002;143:1835–1840. [PubMed] [Google Scholar]
- 19.Morini S, Hassan C, Lorenzetti R, Zullo A, Cerro P, Winn S, Giustini M, Taggi F. Long-term outcome of endoscopic pneumatic dilatation in Crohn’s disease. Dig Liver Dis. 2003;35:893–897. doi: 10.1016/j.dld.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Kelly SM, Hunter JO. Endoscopic balloon dilatation of duodenal strictures in Crohn’s disease. Postgrad Med J. 1995;71:623–624. doi: 10.1136/pgmj.71.840.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsui T, Hatakeyama S, Ikeda K, Yao T, Takenaka K, Sakurai T. Long-term outcome of endoscopic balloon dilation in obstructive gastroduodenal Crohn’s disease. Endoscopy. 1997;29:640–645. doi: 10.1055/s-2007-1004271. [DOI] [PubMed] [Google Scholar]
- 22.Michelassi F, Balestracci T, Chappell R, Block GE. Primary and recurrent Crohn's disease. Experience with 1379 patients. Ann Surg. 1991;214:230–238; discussion 238-240. doi: 10.1097/00000658-199109000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raedler A, Peters J, Schreiber S. Treatment with azathioprin and budenosid prevents recurrence of ileocolonic stenosis after endoscopic dilatation in Crohn´s disease. Gastroenterology. 1997;112:A1067. [Google Scholar]