Abstract
Objectives:
This is a prospective study of psychiatric patients presenting to the emergency department (ED) to determine the value of routine laboratory studies used to attempt to exclude concomitant medical illness.
Methods:
Physical exams and laboratory tests were performed on 375 psychiatric patients presenting for “medical clearance” in the ED. Upon completion of these tests, the percentage and impact of abnormal physical exams and laboratory results were assessed.
Results:
Fifty-six of 375 patients (14.9%) had a non-substance-induced laboratory abnormality. Forty-two of these 56 patients (75.0%) also had abnormal history or physical exam findings indicating laboratory screening. Ten had normal history and physical exams with insignificant laboratory abnormalities. The four (1.1% [95% CI 0.3–2.7%]) remaining patients with normal history and physical exams had abnormal urinalyses which did not affect final disposition or contribute to altered behavior.
Conclusion:
Patients presenting to the ED with psychiatric chief complaints, benign histories and normal physical exams have a low likelihood of clinically significant laboratory findings.
INTRODUCTION
In the United States, 4.3 million psychiatric-related emergency department (ED) visits occur each year.1 This constitutes 5.4% of ED patients and is the fastest growing segment, increasing 15% over the last decade.2 The emergency physician (EP) excludes significant medical illness that might cause or contribute to these patients’ abnormal behavior prior to psychiatric hospitalization. This process is termed “medical clearance.”
Historically, EPs have ordered many diagnostic tests to screen for medical conditions.3 One of the first studies of routine medical screening by Hall4 showed that 46% of psychiatric inpatients had a medical problem that accompanied, exacerbated or caused their psychiatric condition. Henneman5 reported similarly that 63% of patients with new onset psychosis had an organic rather than a functional cause. Conversely, lower rates of organic illness have been reported by Koran6 in 1988 and Dolan7 in 1985. These suggested organic illness rates of 12% and 4%, respectively. In a retrospective chart review of 80 patients with a prior history of psychiatric illness and an isolated psychiatric chief complaint, Korn8 reported that routine laboratory studies did not change final disposition on any patient. The clinical significance of laboratory or radiographic findings has not been reported in a prospective series, to our knowledge.
A commonly held belief has been the presumed inability of psychiatric patients to relate an accurate history or report signs and symptoms to guide testing; however, there is no literature to support this view. Conversely, Korn8 demonstrated that the patient’s initial complaint correlated directly with the need for laboratory and radiographic testing. Nevertheless, this belief persists and is used as rationale to continue performing routine laboratory screening.
The purpose of this study is to determine the value of routine laboratory testing in the “medical clearance” of patients with known psychiatric disorders who present to the ED with a normal history and physical exam. Our hypothesis was that in the absence of abnormal vital signs, history or chart review reflecting significant medical problems, or abnormal physical exam, laboratory testing rarely yields significant findings.
METHODS
The study hospital ED evaluates approximately 53,000 patients per year and serves as the regional psychiatric facility. Approximately 3,000 (5.6%) are psychiatric patients. We performed a prospective, unblinded study of a convenience sample of patients from December 2004 through September 2006. Inclusion criteria were: 1) primary psychiatric complaint (i.e., homicidal, gravely disabled, delusional, hallucinating or agitated/bizarre behavior), 2) documented pre-existing psychiatric disorder, 3) alert and oriented mental status, and 4) laboratory tests were performed. We excluded suicidal patients with or without intentional medication overdoses. The local Institutional Review Board approved the study protocol.
All potential psychiatric patients were initially evaluated by an emergency medicine (EM) resident under supervision of a board-certified emergency physician (EP). The assessment included a history from the patient, corroborated by family, friends, or their psychiatrist, a report from the referring agency, a chart review history, as well as a physical exam. A general physical exam with focus on neurological and psychiatric systems was done. The physician noted whether abnormalities in history or physical exam indicated laboratory testing. Regardless of whether these were indicated laboratory panels, they were performed as agreed upon by the psychiatric and ED services. These included a combination of the following: complete blood count, basic metabolic panel, urine analysis, urine toxicology screen, thyroid panel, liver panel, and urine pregnancy test. Additional laboratory testing or radiographic workup was performed at the discretion of the individual physician.
After “medical clearance,” patients were admitted to the psychiatry service or discharged home, dependent on their psychiatric evaluation. Significant abnormal laboratory values, medical intervention, and final disposition were noted. We defined “significant” operationally as resulting in change in management or prompting further investigations. These data were confirmed by chart and laboratory review, by the primary investigator and entered into a custom database (FilemakerPro 7.0), and analyzed using Excel 2002. Confidence intervals were calculated using STATA 9.2 statistical software (Statacorp, College Station TX).
RESULTS
Four hundred patients were enrolled by 21 EM residents (Post Graduate Year 2–4). We recorded data on 375 (93.7%) patients due to incomplete data forms. The age distribution of psychiatric patients demonstrated by the National Hospital Ambulatory Medical Care Survey, 2000 (NHAMCS)1 compared to our study population are as follows: age 18–24 (11.6% NHAMCS, 20.8% study), 25–44 (47.2% NHAMCS, 47.5% study), 45–64 (26.2% NHAMCS, 30.4% study), 65+ (15.1% NHAMCS, 1.3% study). Our study population was younger than the national benchmark. All of the patients in our study were alert, oriented and able to give a history. The spectrum of psychiatric disturbance in these patients ranged from normal mental status to florid psychosis.
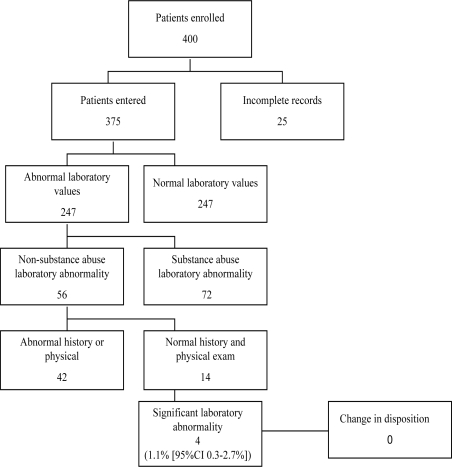
One hundred twenty-eight of 375 patients (34.1% [95%CI 29 – 39%]) had abnormal laboratory values. Seventy-two (56.2%) of these abnormal values were positive urine drug screens, managed by observation and, hydration. Of the 56 other patients with abnormal laboratory values (14.9% [95%CI 10 – 17%]), 42 had indications for further testing due to abnormal history (16/42, 38.1%) or physical exam including vital signs (26/42, 61.9%). Of the remaining 14 patients, only four (1.1% [95% CI 0.3 – 2.7%]) had a significant laboratory abnormality which received medical treatment. See Figure 1.
Figure 1.
Flowchart of study patients
The lab abnormality in each of these four patients was a positive urine analysis suggesting infection (bacteria, white blood cells, leukocyte esterase). Three patients were female, age 35, 57 and 60. The fourth patient was a 60-year-old male. All four received oral antibiotics. Urine cultures were obtained only on one of these patients, and it was a contaminated sample. After evaluation by psychiatry, none of these patients’ dispositions were altered by results of their laboratory tests.
DISCUSSION
Our results demonstrate that, in a selected group of patients presenting with behavioral complaints, physical examination and history are effective screening methods for significant laboratory abnormalities. We suggest that the high percentages of missed organic diagnosis reported in other studies may be due to the lack of a complete history and physical exam as reported by Reeves,9 Tintinalli,10 and Riba.11 Only 1.1% of our patients had results that would not have been suggested by a focused clinical evaluation. All four of these had positive urine analyses. The significance of this laboratory finding, asymptomatic pyuria, is not relevant as it has been shown to neither require nor benefit from treatment.12,13 Furthermore, the U.S. Preventive Services Task Force does not recommend screening non-pregnant women or men for asymptomatic bacteriuria.14 Hence, it is unlikely that significant morbidity would have occurred, if these findings were not discovered.
Korn8 reported similar findings to our study in their retrospective chart review. Our study was the first prospective study to address this issue. Hall4 and Henneman5 reported higher rates of organic illness than our study because they included patients presenting with psychosis without prior psychiatric illness. Henneman only studied patients with new onset psychosis. For that reason cranial computed tomography (CT) was a standard part of his study protocol. In our study only two patients underwent cranial CT.
Chronic conditions such as hypertension, migraine headaches and acne vulgaris were reported by Koran,6 resulting in an organic illness rate of 12%. Koran may have reported lower rates of physical illness if a distinction were made between acute and chronic medical conditions. In Dolan’s study patients were initially admitted to the psychiatric ward without a physical examination or medical history.7 Dolan also may have reported lower rates of organic illness if patients were first medically evaluated for organic verses psychiatric illness. Furthermore, these studies did not fully distinguish between abnormal laboratory findings and those significant enough to require treatment or change in disposition.
LIMITATIONS
Our study was not randomized or blinded, and enrolled a convenience sample with inherent potential for selection bias. The level of training of physicians varied. Our study population was significantly younger than those described by NHAMCS, and therefore, these results may not apply to older patients. The depth of history and completeness of physical examination was not proscribed by the protocol, and likely varied. Furthermore, after “medical clearance” a psychiatrist also evaluated the patient. That is uncommon in most community EDs. Lastly, although our study population was small, this is the largest prospective study to date addressing medical clearance. A large multi-centered study is needed to derive and then validate a clinical decision rule.
CONCLUSION
Our study demonstrates that patients presenting to the ED with a primary psychiatric complaint, a documented previous psychiatric history and normal medical history and physical exam, have a very low likelihood of clinically significant laboratory findings. Therefore, mandatory laboratory testing may not be necessary.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Supervising Section Editor: Eric D. Isaacs, MD
Reprints available through open access at www.westjem.org
REFERENCES
- 1.Ly N, McCaig LF. Advance data from vital and health statistics. 326 Hyattsville, Maryland: National Center for Health Statistics; 2002. National Hospital Ambulatory Medical Care Survey: 2000 emergency department summary. [Google Scholar]
- 2.Hazlett B, McCarthy ML, Londer MS, Onyike CU. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004;11:193–195. [PubMed] [Google Scholar]
- 3.Lagomasino I, Daly R, Stoudemire A. Medical assessment of patients presenting with psychiatric symptoms in the emergency setting. Psychiatr Clin North Am. 1999;22:819–850. doi: 10.1016/s0193-953x(05)70128-3. [DOI] [PubMed] [Google Scholar]
- 4.Hall RCW, Gardner ER, Popkin MK, et al. Unrecognized physical illness prompting psychiatric admission: A prospective study. Am J Psychiatry. 1981;138:629–635. doi: 10.1176/ajp.138.5.629. [DOI] [PubMed] [Google Scholar]
- 5.Henneman PL, Mendoza R, Lewis RJ. Prospective evaluation of emergency department medical clearance. Ann Emerg Med. 1994;24:672–677. doi: 10.1016/s0196-0644(94)70277-2. [DOI] [PubMed] [Google Scholar]
- 6.Koran LM, Sox HL, Martin KI, et al. Medical evaluation of psychiatric patients: Results in a state mental health system. Arch Gen Psychiatry. 1989;46:733–740. doi: 10.1001/archpsyc.1989.01810080063007. [DOI] [PubMed] [Google Scholar]
- 7.Dolan JG, Mushlin AI. Routine laboratory testing for medical disorders in psychiatric patients. Arc Intern Med. 1985;145:2085–2088. [PubMed] [Google Scholar]
- 8.Korn CS, Currier GW, Henderson SO. Medical clearance of psychiatric patients without medical complaints in the emergency department. J Emerg Med. 2000;18:173–176. doi: 10.1016/s0736-4679(99)00191-2. [DOI] [PubMed] [Google Scholar]
- 9.Reeves RR, Pendarvis EJ, Kimble R. Unrecognized Medical Emergencies Admitted to the Psychiatric Units. American J of Emerg Med. 2000;18:390–393. doi: 10.1053/ajem.2000.7318. [DOI] [PubMed] [Google Scholar]
- 10.Tintinalli JE, Peacock FW, Wright MA. Emergency medical evaluation of psychiatric patients. Ann Emerg Med. 1994;23:859–862. doi: 10.1016/s0196-0644(94)70326-4. [DOI] [PubMed] [Google Scholar]
- 11.Riba M, Hale M. Medical clearance: fact or fiction in the hospital emergency room. Psychosomatic. 1990;31:400–404. doi: 10.1016/S0033-3182(90)72134-2. [DOI] [PubMed] [Google Scholar]
- 12.Colgan R, Nicolle LE, McGlone A, Hooton TM. Asymptomatic bacteriuria in adults. Am Fam Physician. 2006;74:985–990. [PubMed] [Google Scholar]
- 13.Nicolle LE, Bradley S, Clogan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643–654. doi: 10.1086/427507. [DOI] [PubMed] [Google Scholar]
- 14.U. S. Preventative Services Task Force. Screening for asymptomatic bacteriuria in adults: U.S. Preventive Service Task Force Reaffirmation Recommendation Statement. Ann Intern Med. 2008;149:43–47. doi: 10.7326/0003-4819-149-1-200807010-00009. [DOI] [PubMed] [Google Scholar]