Abstract
While the supraclavicular approach to the subclavian vein has been described since 1965, it is generally employed much less often than the “traditional” infraclavicular approach. Although randomized trials are lacking, the best evidence suggests that the supraclavicular approach has a number of important advantages to the infraclavicular approach. The landmarks and relative merits of the procedure are described in this paper.
INTRODUCTION
Central venous catheterization is a vital intervention in critically ill patients for a variety of purposes, including volume resuscitation, central venous pressure monitoring, transvenous cardiac pacing, hemodialysis access, and hypertonic or irritant substance infusion. Central lines are typically introduced into the internal jugular, subclavian, or femoral veins. The proper choice of insertion site is essential for success. Various methods of placement have evolved, each with its own advantages and potential complications.
Several anatomic advantages of the subclavian vein for central access include its large diameter, absence of valves, and ability to remain patent and in a relatively constant position.1,2 Subclavian catheterization also carries a lower risk of catheter-related infection and thrombosis than femoral or internal jugular vein catheterization.3
Since Aubaniac’s original description in 1952,4 subclavian vein catheterization via the infraclavicular approach has become a well-established technique. In 1965 an alternate supraclavicular approach was described by Yoffa.1 This supraclavicular route to the subclavian vein has some distinct advantages over the infraclavicular approach; however it is less often taught and utilized for reasons that are not clear.
Advantages of the Supraclavicular Approach
Advantages of the supraclavicular approach over the infraclavicular technique include: a well-defined insertion landmark (the clavisternomastoid angle); a shorter distance from skin to vein; a larger target area; a straighter path to the superior vena cava; less proximity to the lung; and fewer complications of pleural or arterial puncture.1,2,5–8 In addition, the supraclavicular approach less often necessitates interruption of CPR or tube thoracostomy than the infraclavicular method.9,10
Approach
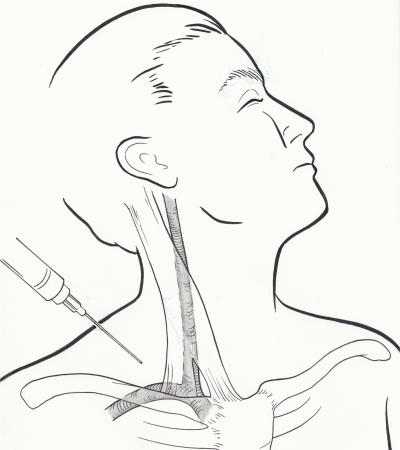
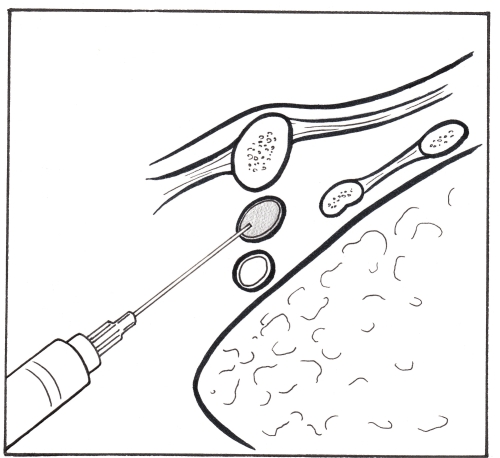
The objective of the supraclavicular technique is to puncture the subclavian vein in its superior aspect just as it joins the internal jugular vein. The key to success, according to Yoffa,1 is correct identification of the clavisternomastoid angle formed by the junction of the lateral head of the sternocleidomastoid muscle and the clavicle. Active raising of the patient’s head may make this landmark more apparent. The needle is inserted 1 cm lateral to the lateral head of the sternocleidomastoid muscle and 1 cm posterior to the clavicle and directed at a 45-degree angle to the sagittal and transverse planes and 15 degrees below the coronal plane aiming toward the contralateral nipple.5 The needle bisects the clavisternomastoid angle as it is advanced in an avascular plane, away from the subclavian artery and the dome of the pleura, entering the junction of the subclavian and internal jugular veins.1,5,6 See Figures 1 and 2.
Figure 1.
Figure 2.
The right side is preferred because of the lower pleural dome, more direct route to the superior vena cava, and absence of thoracic duct. The Trendelenberg position is recommended to decrease risk of air embolus and to potentially help distend the vein, as the subclavian vein is not bound by fascia on its superior aspect.5 To further minimize complications the needle bevel should be facing down prior to insertion, attempts should cease after 2–3 unsuccessful tries, and most importantly, the clavisternomastoid angle must be clearly identified prior to insertion.11
THE DATA
Most clinical studies on the supraclavicular approach are in the form of prospective case series. Only a few well designed, randomized prospective trials comparing the infraclavicular and supraclavicular methods have been described in the literature.
Dronen et al.9 conducted a randomized prospective comparison of the supraclavicular and infraclavicular techniques in 76 patients undergoing CPR. Forty-four supraclavicular attempts and 45 infraclavicular attempts were evaluated. Rates of successful cannulation with the two approaches were comparable (90% with the supraclavicular approach and 84% with the infraclavicular approach, p>0.05). The mean number of needle sticks for cannulation was similar with both techniques (1.38 +/− 0.69 with the supraclavicular approach and 1.46 +/− 0.89 with the infraclavicular approach, p>0.05). The incidence of technical difficulties in threading the catheter also did not differ significantly (18% and 21% with the supraclavicular and infraclavicular approaches, respectively, p>0.05). However, the incidence of malpositioning or kinking of the catheter was significantly higher with the infraclavicular technique (26% versus 7% in the supraclavicular group, p<0.05). In addition, excessive interruption of CPR (five seconds or greater) occurred in 20% of supraclavicular attempts and in 40% of infraclavicular attempts (p<0.025). No patient had CPR interrupted for more than 10 seconds with the supraclavicular method, while CPR interruption exceeded 10 seconds in 9% of cases with the infraclavicular method. There were no major complications with either approach. According to this small study, the supraclavicular approach to subclavian vein catheterization is probably the technique of choice when central venous access is required during CPR.9
In a larger study, Sterner et al.12 conducted a randomized, prospective comparison of the supraclavicular and infraclavicular approaches in 500 patients. Two hundred forty-five patients were in the supraclavicular group and 255 patients in the infraclavicular group. The rates of successful cannulation were similar between the two groups (84.5% for the supraclavicular group and 80% for the infraclavicular group, p=0.23). When catheterization by the designated approach failed, catheterization by the alternate approach was successful in all but seven cases, resulting in an overall success rate of 98.6%. The incidence of catheter malpositioning was significantly higher in the infraclavicular group (9% vs. 0.5% in the supraclavicular group, p<0.01). Overall there were 18 complications (3.6%), and no differences were observed between the groups in the instances of pneumothorax, arterial punctures, or kinked catheters (p=0.13). According to this study, using an alternate approach to subclavian vein catheterization if the initial approach is unsuccessful yields a very high overall success rate and a very low overall complication rate. Sterner concluded that familiarity with both approaches is the key to successful subclavian vein catheterization.
Lu et al.13 conducted a prospective comparison of four different approaches to subclavian catheterization in 91 infants. There were 21 right supraclavicular (RSC), 24 left supraclavicular (LSC), 24 right infraclavicular (RIC), and 22 left infraclavicular (LIC) catheterization attempts. The operator decided on the site of skin puncture. The success rate was 95.2% in the RSC group, 91.7% in the LSC group, 87.5% in the RIC group, and 86.4% in the LIC group. No statistically significant differences were detected in the rates of success or complications. There were six cases of arterial puncture (five supraclavicular and one infraclavicular, p=0.09), two cases of pneumothorax (one RSC and one RIC), and two cases of malpositioned catheter (one RSC and one RIC). Authors concluded that subclavian vein catheterization is a safe procedure for infants.
OTHER METHODS
Numerous permutations of Yoffa’s original supraclavicular technique have been developed and tested in cadaver studies and prospective case series. The modifications range from simply changing the angle of needle insertion to using a completely different set of anatomical landmarks than the “clavisternomastoid angle.”
Garcia et al.14 evaluated 83 attempts at subclavian vein catheterization using a modified supraclavicular approach. Successful catheterization was achieved in 98.6% of the attempts. The complication rate was 6% with two pneumothoraces and three subclavian artery punctures. This modification used the same landmarks as Yoffa;1 however, the needle was directed at a 5-degree angle from the coronal plane, 50 degrees from the sagittal plane and 40 degrees from the transverse plane. This adaptation was based on a cadaver study in which authors noted that a wider “sling” target formed by the confluence of the internal jugular and subclavian veins could be easily cannulated with a more superficial needle trajectory than the original approach.14
In a large case series published in 1974, Haapaniemi and Slatis15 introduced an alternative technique with a puncture site 2–3 cm above the clavicle near the posterior border of the sternocleidomastoid muscle. The needle was then advanced caudad at an angle of 35 degrees towards the sagittal plane and slightly upwards from the coronal plane between the sternocleidomastoid and anterior scalene muscles. The site of venipuncture was the confluence of the subclavian and internal jugular veins. In a series of 600 patients, this technique had a 94% success rate and a 5% complication rate with two cases of pneumothorax, four arterial punctures, and six thoracic duct punctures.
Over a decade later, Conroy et al.16 studied the supraclavicular junctional or “central” approach in which the needle pierced the skin 1 cm medially and superiorly to the midpoint of the clavicle at a 20-degree angle from the transverse plane and a 20-degree angle from the coronal plane and was advanced toward the sternoclavicular joint. In the study population of 100 patients, only two failures and no complications occurred.
Using the approach described by Conroy et al.,16 Jones and Walters17 reported successful cannulation in 27 of 34 patients (79%) requiring temporary hemodialysis access. Two arterial punctures transpired and no pneumothorax or hemothorax occurred.
In 1992, MacDonnell et al.18 evaluated another modification of the supraclavicular technique in 35 human cadavers. The new landmark for needle insertion was the junction of the middle and medial thirds of the clavicle. The needle entered the skin at this point just posterior to the clavicle and was advanced parallel to the coronal plane toward the ipsilateral sternoclavicular joint. Cannulation was successful in 33 cases (94%) with one subclavian artery cannulation.
In 1997, Muhm et al.7 studied an adaptation of Yoffa’s approach in 175 patients requiring hemodialysis access. With this method, the needle was introduced at the lateral margin of the clavicular insertion of the sternocleidomastoid muscle and was then directed toward the sternal end of the right-sided second intercostal space 20 degrees cephalad to the transverse plane and 20 degrees anterior to the coronal plane. During an 18-month period, 208 large bore catheters were successfully placed in 164 patients (success rate, 93.8%). Complications included one pneumothorax, seven arterial punctures, two thoracic duct punctures, and two catheter malpositions without sequelae.
Gorchynski et al.10 evaluated another variation of the supraclavicular technique in 2004. With the “pocket approach,” the needle was inserted at the midpoint between the sternal and clavicular heads of the sternocleidomastoid muscle just posterior to the clavicle and was then advanced toward the ipsilateral nipple at a 45-degree angle. In the initial phase of this study, the “pocket approach” was attempted in 28 cadavers with a 100% success rate. The second phase, a chart review of 68 patients who underwent attempted central venous access using the “pocket approach,” yielded a 90% success rate. There were two cases of catheter misplacement. No pneumothoraces, arterial punctures, or other complications were reported. The “pocket shot” has been used by intravenous drug users when they have exhausted their peripheral veins.19
Supraclavicular Central Lines in The Ultrasound Era
The use of ultrasound guidance during internal jugular catheterization has been shown to reduce the time required for insertion, the number of complications and the rates of unsuccessful catheterization.20,21 However, evidence supporting its use in subclavian venous access is sparse.22 Real-time ultrasound guidance with the supraclavicular approach is technically difficult because little room is available to position the transducer while inserting the needle. One alternative is to identify the vessel with ultrasound and mark the puncture site on the skin overlying the center of the vessel.23 Another option is the ultrasound-guided low internal jugular vein approach in which the inferior portion of the internal jugular is cannulated approximately 2 cm above the clavicle between the sternal and clavicular insertions of the sternocleidomastoid muscle. Silberzweig and Mitty24 evaluated 116 ultrasound-guided low internal jugular vein approaches in 109 patients. Successful catheterization occurred in 100% of the attempts with an average of 1.2 passes (range 1–3) to obtain access. One common carotid artery puncture occurred with no adverse outcome. Another potential alternative described in a recent article by Maeken and Grau22 is the “notch position” for ultrasound-guided central venous puncture of the innominate vein; although this procedure has not been studied in detail.
While ultrasound is an enormous advance in the placement of central lines, it is not always available. For this reason alone landmark based central line access will remain a skill physicians need to have in their armamentarium. The supraclavicular line offers another approach that appears at least as safe and possibly easier to perform with less misplacement than more frequently used lines.
CONCLUSIONS
The literature clearly demonstrates the effectiveness of the supraclavicular approach using Yoffa’s original technique as well as modifications to landmarks, angles, and patient position (see Table). No central venous access is without potential complications and no one technique is ideal for every patient. In conclusion, a thorough knowledge of anatomy and familiarity with multiple approaches is the route to successful central venous catheterization.
Table.
Summary of current evidence for supraclavicular approach to the subclavian vein.
| Year/Author | Total cases | Method | Versus infraclavicular | Success rate | Complication rate |
|---|---|---|---|---|---|
| 1965 Yoffa1 | 130 | Yoffa | No | 97.7% | 0.8% |
| 1972 Garcia14 | 72 | Garcia | No | 98.6% | 6.0% |
| 1972 James25 | 3000 | Yoffa | No | 95.0% | 1.2% |
| 1974 Haapaniemi15 | 600 | Other | No | 94.0% | 5.0% |
| 1976 Neale26 | 64 | Garcia | No | 97.0% | 3.0% |
| 1977 Brahos5 | 100 | Yoffa | No | 95.0% | 2.0% |
| 1981 Brahos6 | 250 | Yoffa | No | 95.0% | 1.2% |
| 1982 Dronen9 | 89 | Yoffa | Yes | 90.0% supra 84.0% infra |
2.2% supra 0.0% infra |
| 1985 Helmkamp11 | 99 | Yoffa | No | 91.0% | 3.0% |
| 1986 Sterner12 | 500 | Yoffa | Yes | 84.5% supra 80.0% infra |
2.0% supra 5.1% infra |
| 1990 Conroy16 | 100 | Central | No | 98.0% | 0.0% |
| 1992 Jones17 | 34 | Central | No | 79.0% | 7.0% |
| 1992 MacDonnell18 | 35 | Other | No | 94.0% | 2.9% |
| 1997 Muhm7 | 219 | Other | No | 93.8% | 8.2% |
| 1997 Nevarre27 | 128 | Yoffa | No | 97.8% | 0.6% |
| 1998 Apsner8 | 81 | Yoffa | No | 97.5% | 4.9% |
| 2000 Laczika28 | 17 | Yoffa | No | 100.0% | 0.0% |
| 2004 Gorchynski10 | 68 | No | 90.0% | 0.0% | |
| 2006 Lu13 | 91 | Other | Yes | 93.3% supra 87.0% infra |
13.3% supra 4.3% infra |
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Supervising Section Editor: Jeffrey Sankoff, MD
Reprints available through open access at www.westjem.org
REFERENCES
- 1.Yoffa D. Supraclavicular subclavian venepuncture and catheterization. Lancet. 1965;2:614–7. doi: 10.1016/s0140-6736(65)90519-2. [DOI] [PubMed] [Google Scholar]
- 2.Defalque R. Subclavian venipuncture: A review. Anesth Analg. 1968;47:677–82. [PubMed] [Google Scholar]
- 3.McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123–33. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- 4.Aubaniac R. A new route for venous injection or puncture: the subclavicular route, subclavian vein, brachiocephalic trunk. Sem Hop. 1952;28:3445–7. [PubMed] [Google Scholar]
- 5.Brahos GJ. Central venous catheterization via the supraclavicular approach. J Trauma. 1977;17:872–7. doi: 10.1097/00005373-197711000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Brahos GJ, Cohen M. Supraclavicular central venous catheterization: technique and experience in 250 cases. Wisconsin Med J. 1981;80:36–8. [PubMed] [Google Scholar]
- 7.Muhm M, Sunder-Plassmann G, Apsner R, Kritzinger M, Hiesmayr M, Druml W. Supraclavicular approach to the subclavian/innominate vein for large-bore central venous catheters. Am J Kidney Dis. 1977;30:802–6. doi: 10.1016/s0272-6386(97)90085-8. [DOI] [PubMed] [Google Scholar]
- 8.Apsner R, Schulenburg A, Sunder-Plassmann G, Muhm M, Keil F, Malzer R, Kalhs P, Druml W. Routine fluoroscopic guidance is not required for placement of Hickman catheters via the supraclavicular route. Bone Marrow Transplant. 1998;21:1149–52. doi: 10.1038/sj.bmt.1701250. [DOI] [PubMed] [Google Scholar]
- 9.Dronen S, Thompson B, Nowak R, Tomlanovich M. Subclavian vein catheterization during cardiopulmonary resuscitation: a prospective comparison of the supraclavicular and infraclavicular percutaneous approaches. JAMA. 1982;247:3227–30. [PubMed] [Google Scholar]
- 10.Gorchynski J, Everett WW, Pentheroudakis E. A modified approach to supraclavicular subclavian vein catheter placement: The pocket approach. Calif J Emerg Med. 2004;5:50–4. [PMC free article] [PubMed] [Google Scholar]
- 11.Helmkamp BF, Sanko SR. Supraclavicular central venous catheterization. Am J Obstet Gynecol. 1985;153:751–4. doi: 10.1016/0002-9378(85)90339-4. [DOI] [PubMed] [Google Scholar]
- 12.Sterner S, Plummer DW, Clinton J, Ruiz E. A comparison of the supraclavicular approach and the infraclavicular approach for subclavian vein catheterization. Ann Emerg Med. 1986;15:421–4. doi: 10.1016/s0196-0644(86)80179-2. [DOI] [PubMed] [Google Scholar]
- 13.Lu WH, Yao ML, Hsieh KS, Chiu PC, Chen YY, Lin CC, Huang TC, Chen CC. Supraclavicular versus infraclavicular subclavian vein catheterizatin in infants. J Chin Med Assoc. 2006;69:153–6. doi: 10.1016/S1726-4901(09)70196-0. [DOI] [PubMed] [Google Scholar]
- 14.Garcia JM, Mispireta LA, Pinho RV. Percutaneous supraclavicular superior vena caval cannulation. Surg Gynecol Obstet. 1972;134:839–41. [PubMed] [Google Scholar]
- 15.Haapaniemi L, Slatis P. Supraclavicular catheterization of the superior vena cava. Acta Anaesth Scand. 1974;18:12–22. doi: 10.1111/j.1399-6576.1974.tb00694.x. [DOI] [PubMed] [Google Scholar]
- 16.Conroy JM, Rajagopalan PR, Baker JD, et al. A modification of the supraclavicular approach to the central circulation. South Med J. 1990;83:1178–81. doi: 10.1097/00007611-199010000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Jones CE, Walters GK. Efficacy of the supraclavicular route for temporary hemodialysis access. South Med J. 1992;85:725–8. doi: 10.1097/00007611-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 18.MacDonnell JE, Perez H, Pitts SR, et al. Supraclavicular subclavian vein catheterization: Modified landmarks for needle insertion. Ann Emerg Med. 1992;21:421–4. doi: 10.1016/s0196-0644(05)82663-0. [DOI] [PubMed] [Google Scholar]
- 19.Cherubin CE, Sapira JD. The medical complications of drug addiction and the medical assessment of the intravenous drug user: 25 years later. Ann Intern Med. 1993;119:1017–28. doi: 10.7326/0003-4819-119-10-199311150-00009. [DOI] [PubMed] [Google Scholar]
- 20.Teichgraber UK, Benter T, Gebel M, et al. A sonographically guided technique for central venous access. Am J Roentgenol. 1997;169:731–3. doi: 10.2214/ajr.169.3.9275887. [DOI] [PubMed] [Google Scholar]
- 21.Randolph AG, Cook DJ, Gonzalez CA, et al. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24:2053–8. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- 22.Maecken T, Grau T. Ultrasound imaging in vascular access. Crit Care Med. 2007;35:S178–85. doi: 10.1097/01.CCM.0000260629.86351.A5. [DOI] [PubMed] [Google Scholar]
- 23.Abboud PA, Kendall JL. Ultrasound guidance for vascular access. Emerg Med Clin N Am. 2004;22:749–73. doi: 10.1016/j.emc.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Silberzweig JE, Mitty HA. Central venous access: low internal jugular vein approach using imaging guidance. AJR. 1998;170:1617–20. doi: 10.2214/ajr.170.6.9609184. [DOI] [PubMed] [Google Scholar]
- 25.James PM, Myers RT. Central venous pressure monitoring: Misinterpretation, abuses, indications and a new technique. Ann Surg. 1972;175:693–701. doi: 10.1097/00000658-197205000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Neale TJ. Experience in the use of central venous cannulation. N Z Med J. 1976;83:13–14. [PubMed] [Google Scholar]
- 27.Nevarre DR, Domingo OH. Supraclavicular approach to subclavian catheterization: review of the literature and results of 178 attempts by the same operator. J Trauma. 1997;42:305–9. doi: 10.1097/00005373-199702000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Laczika K, Thalhammer F, Locker G, et al. Safe and efficient emergency transvenous ventricular pacing via the right supraclavicular route. Anesth Analg. 2000;90:784–9. doi: 10.1097/00000539-200004000-00003. [DOI] [PubMed] [Google Scholar]