Abstract
BACKGROUND:
Peripheral arterial disease (PAD) is a common manifestation of systemic atherosclerosis and is associated with a high risk of stroke, myocardial infarction and cardiovascular death. PAD also fosters major morbidity by causing claudication, functional impairment, disability and amputation. PAD is largely unrecognized and under-treated compared with other cardiovascular diseases. The public health impact of PAD, as a contributor to Canadian national rates of heart attack, stroke, amputation, death and disability, will be challenging to address if the public is unaware of this common cardiovascular disease.
OBJECTIVE:
To assess public knowledge of PAD in Canada.
METHODS:
A cross-sectional, population-based telephone survey of 501 adults 50 years of age and older (mean age 64.4 years) was conducted using random digit dialing. The survey assessed demographics and risk factors of the study population and knowledge of PAD causes and consequences.
RESULTS:
Survey respondents reported a high prevalence of atherosclerotic risk factors including high blood pressure (43%), high blood cholesterol (37%), diabetes (12%) and smoking history (18% current and 49% former smokers). Only 36% of respondents reported familiarity with PAD, which was significantly lower than other cardiovascular diseases or risk factors. Knowledge of perceived consequences of PAD was low and knowledge gaps were more pronounced in older, less educated and lower income respondents.
CONCLUSIONS:
The Canadian public is largely unaware of PAD as a prevalent systemic manifestation of atherosclerosis and its associated morbidity and mortality. National PAD awareness programs should be instituted to increase PAD knowledge to levels comparable with other cardiovascular diseases and risk factors.
Keywords: Cardiovascular disease, Claudication, Myocardial infarction, Peripheral arterial disease, Prevention, Risk factors
Abstract
HISTORIQUE :
La maladie des artères périphériques (MAP) est une manifestation courante de l’athérosclérose systémique et s’associe à un risque élevé d’accident vasculaire cérébral (AVC), d’infarctus du myocarde et de décès cardiovasculaire. La MAP entraîne également une importante morbidité, y compris une claudication, une atteinte fonctionnelle, une invalidité et une amputation. Elle est largement méconnue et sous-traitée par rapport à d’autres maladies cardiovasculaires. Les répercussions de la MAP sur la santé publique, à titre de facteur contribuant aux taux canadiens de crise cardiaque, d’AVC, d’amputation, de décès et d’invalidité, seront difficiles à déterminer si le public ne connaît pas cette maladie cardiovasculaire courante.
OBJECTIF :
Évaluer la sensibilisation du public à la MAP au Canada.
MÉTHODOLOGIE :
Les auteurs ont procédé à une enquête téléphonique transversale en population auprès de 501 adultes de 50 ans et plus (âge moyen de 64,4 ans) au moyen de la composition aléatoire. L’enquête a permis d’évaluer les facteurs démographiques et les facteurs de risque de la population à l’étude ainsi que leur connaissance des causes et des conséquences de la MAP.
RÉSULTATS :
Les répondants à l’enquête ont déclaré une forte prévalence de facteurs de risque d’athérosclérose, y compris l’hypertension (43 %), un taux élevé de cholestérol sanguin (37 %), du diabète (12 %) et des antécédents de tabagisme (18 % de fumeurs et 49 % d’anciens fumeurs). Seulement 36 % des répondants ont déclaré connaître la MAP, un taux considérablement plus faible que pour les autres maladies ou facteurs de risque cardiovasculaires. Les connaissances quant aux conséquences perçues de la MAP étaient faibles, et cette lacune était plus prononcée chez les répondants plus âgés, moins instruits et au revenu moins élevé.
CONCLUSIONS :
Le public canadien connaît très peu la MAP à titre de manifestation systémique prévalente de l’athérosclérose ainsi que la morbidité et la mortalité qui s’y rapportent. Il faudrait entreprendre des programmes nationaux de sensibilisation à la MAP pour faire connaître la MAP à des taux comparables aux autres maladies et facteurs de risque cardiovasculaires.
Peripheral arterial disease (PAD) is a common manifestation of systemic atherosclerosis (1). PAD is usually caused by atherosclerotic disease of the arteries that supply the lower extremities, and is a powerful predictor of atherosclerotic disease in other arterial beds (2,3). The primary ischemic symptom of PAD is intermittent claudication, which markedly impairs quality of life and functional status (4). In its most severe form, PAD may lead to limb-threatening ischemia requiring revascularization or amputation. Patients with PAD, defined by an ankle-brachial index of less than 0.90, suffer a fivefold increased short-term risk of a nonfatal heart attack or stroke, and a total mortality that is two- to threefold greater than that observed in individuals without PAD (4,5). This increased hazard is essentially identical for asymptomatic and symptomatic individuals with PAD (6).
PAD is widely prevalent, affecting approximately 800,000 Canadians, as many as nine million Americans and 12% to 29% of the elderly (1,7,8). The incidence of PAD increases with age and exposure to atherosclerosis risk factors. Previous investigations have documented that PAD is often underdiagnosed and undertreated (9,10). Therefore, PAD is widespread within the population as a ‘silent’ cardiovascular disease, and tens of thousands of Canadians remain at risk for preventable heart attacks and strokes. Approximately one-half of all individuals with PAD are asymptomatic (3,9). Although leg symptoms may not be prominent, the atherosclerotic disease burden is high. Data from the Edinburgh Artery Study (11) have demonstrated that at least one-third of individuals with asymptomatic PAD will have at least one complete occlusion of a major artery to the leg, as documented by duplex arterial ultrasound evaluation. In Canada, the population-based prevalence of PAD has not been directly assessed. However, it is estimated that 4% of the population older than 40 years of age in comparable developed nations have PAD (12). Canadian and American clinical practice guidelines (12–15) designate PAD as a coronary artery disease risk equivalent.
Public awareness of common diseases and their associated risks can lead to health benefits. The Canadian Hypertension Education Program has been very successful at educating the public about the dangers of hypertension. Recent studies suggest hypertension treatment and control is improving (16). The Canadian cardiovascular health professional societies have therefore considered PAD public awareness to represent an important opportunity to foster improved Canadian cardiovascular population-based health (12).
A recent publication by Hirsch et al (17) described the results of an American PAD public awareness survey of a national probability sample of 2501 adults 50 years of age and older. The survey highlighted the profound lack of PAD-related awareness and detailed specific PAD-related knowledge gaps (17). The present survey was concurrently performed, and used comparable methodology to determine the level of PAD public awareness in Canada.
The purpose of the present baseline Canadian PAD awareness survey was to assess PAD awareness in a national sample of adults 50 years of age and older. The survey was designed to measure knowledge of factors that increase the risk for PAD and the clinical risk consequences of having PAD. These data will provide useful information to guide future regional (provincial) and Canadian national public cardiovascular educational efforts.
METHODS
Sample and survey design
The present cross-sectional, population-based descriptive survey was conducted between June 5, 2006, and July 5, 2006. An independent, interdisciplinary academic steering committee from the nonprofit Peripheral Arterial Disease Coalition, with expertise in survey research, developed the survey instrument. Before initiating the main survey in the United States, a cognitive pretest was performed on 25 respondents on May 3, 2006, and May 4, 2006, to ensure reliability and validity. The purpose of the pretest was to obtain a better understanding of how respondents interpreted the questions and to decide if any questions required revisions. Only minor edits were required in clarifying the survey instrument. Data were collected via telephone, using a list-assisted random digit dialing sample design (18). Methodological details of the survey were published previously (17). The measurement of PAD awareness was defined by a positive response to the following question: “Have you ever been told by a health care professional that you had: blockage in your leg arteries; circulation problems in your legs; problems in the flow of blood to your legs; decreased blood pressure in your ankles; or claudication, which is leg pain when walking or exercising that disappears after a few minutes of rest?” The survey instrument will be published independently.
In total, 501 adults 50 years of age and older who were living in Canada were interviewed in English or French. The Canadian national probability sample was weighted by age (coded into four 10-year categories: 50 to 59 years; 60 to 69 years; 70 to 79 years; and 80 years and older) and sex to reflect Canadian census estimates for 2006 (19). The response rate was 35.8% and was determined by inputting the number of screen outs (Canadians younger than 50 years) in the final disposition report.
Statistical analysis
Data are reported as percentages. The sample size of 501 is associated with a margin of error of less than 4.5%. Differences in responses between each ethnic and age group were analyzed to assess pairwise significance as calculated using Pearson’s χ2 test. Statistical significance was set at p<0.05.
RESULTS
Demographic characteristics
Demographic characteristics are presented in Table 1. The survey population consisted of 501 individuals 50 years of age and older. The mean age was 64.4 years, with 41.6% of subjects aged 50 to 59 years, 27.2% aged 60 to 69 years, 20.6% aged 70 to 79 years, and 10.5% 80 years of age and older. The survey population was 93.0% Caucasian, 0.7% black, 1.6% First Nations and 1.9% Asian. Compared with the prevalence of these groups in the Canadian population, First Nations and Asians were under-represented. Women comprised 53.6% of the sample and 38.7% of respondents had completed some college education. Of those surveyed, 46.6% had an annual household income of less than $40,000. Geographically, the present survey represented all provinces and territories, with the largest survey population from Quebec and Ontario (58.5%), followed by western Canada (32%) and eastern Canada (9.6%).
TABLE 1.
Demographic characteristics of the Canadian peripheral arterial disease awareness sample
| n (%) | |
|---|---|
| Sex | |
| Male | 233 (46.4) |
| Female | 268 (53.6) |
| Age, years | |
| 50–59 | 209 (41.6) |
| 60–69 | 136 (27.2) |
| 70–79 | 103 (20.6) |
| 80 or older | 53 (10.5) |
| Race | |
| Caucasian | 466 (93.0) |
| Black | 3 (0.7) |
| Aboriginal | 8 (1.6) |
| Asian | 10 (1.9) |
| Other | 8 (1.6) |
| Education | |
| ≤ high school | 301 (60.1) |
| > high school | 194 (38.7) |
| Annual income | |
| <$40,000 | 233 (46.6) |
| ≥ $40,000 | 192 (38.3) |
| Total | 501 (100.0) |
Note: Distributions in some groups do not add up to 100% due to missing data
Leg symptoms and signs
The survey classified leg symptoms in all respondents by their presence at rest or with ambulation, regardless of whether there had been a previous, confirmed diagnosis of PAD. Thirty per cent of the survey respondents reported leg symptoms (Table 2). No validated PAD-specific survey instrument was used to define both typical claudication and/or atypical leg symptoms. The survey was designed to determine whether any leg symptoms prompted consideration of a diagnosis of PAD. Leg symptoms were more frequently reported by women (31.7%), individuals 70 years of age and older (35.9%) and those with lower education levels (35.5%) or annual income less than $40,000 (37.6%). Nonhealing foot wounds or sores (1.4%) were infrequently reported.
TABLE 2.
Leg symptoms by demographics
| Leg symptoms |
Sex |
Age, years |
Education |
Annual income |
Total (n=501) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=233) | Female (n=268) | 50–69 (n=345) | 70+ (n=156) | ≤ High school (n=301) | > High school (n=194) | <$40,000 (n=233) | ≥ $40,000 (n=192) | ||
| Persistent or recurring pain in your legs | 48 (20.6) | 62 (23.1) | 74 (21.5) | 35 (22.4) | 79 (26.2) | 30 (15.5) | 67 (28.8) | 27 (14.1) | 110 (22) |
| Frequent pain in your legs when you walk | 40 (17.2) | 53 (19.8) | 56 (16.3) | 37 (23.7) | 71 (23.6) | 21 (10.8) | 57 (24.4) | 16 (8.3) | 93 (18.6) |
| Frequent pain in your legs or feet when sitting | 29 (12.5) | 38 (14.2) | 50 (14.5) | 17 (10.9) | 50 (16.6) | 18 (9.3) | 38 (16.3) | 17 (8.9) | 67 (13.4) |
| Frequent pain in your legs or feet when elevated | 18 (7.7) | 34 (12.7) | 34 (9.9) | 17 (10.9) | 38 (12.6) | 13 (6.7) | 30 (12.8) | 12 (6.3) | 52 (10.4) |
| Wound or sore on your foot that would not heal | 3 (1.3) | 4 (1.5) | 3 (0.9) | 3 (1.9) | 4 (1.3) | 3 (1.5) | 5 (2.1) | 1 (0.5) | 7 (1.4) |
| Any one or more symptoms | 66 (28.3) | 85 (31.7) | 95 (27.5) | 56 (35.9) | 107 (35.5) | 41 (21.1) | 88 (37.6) | 34 (17.7) | 151 (30.1) |
| None of these | 167 (71.7) | 183 (68.3) | 250 (72.5) | 100 (64.1) | 194 (64.5) | 153 (78.9) | 146 (62.4) | 158 (82.3) | 350 (69.9) |
Data presented as n (%). Note: Values in bold denote pairwise significance from the associated value
Knowledge of risk factors, cardiovascular diseases and other illnesses
Awareness of atherosclerotic risk factors, cardiovascular diseases and other illness was defined as the combination of ‘somewhat’ or ‘very’ familiar responses and is presented in Table 3. Among the study population, awareness of risk factors, including high blood pressure (80.2%), high blood cholesterol (78.6%) and diabetes (73.5%), was high. Many respondents also reported familiarity with stroke (71.7%), coronary artery disease (51.1%) and heart failure (47.9%). PAD awareness was determined by a positive response to either PAD or peripheral vascular disease. Awareness of PAD (35.5%) was low. Multiple sclerosis, a much less prevalent disease, was better known than PAD, with 43.0% reporting that they were at least somewhat familiar with the condition. PAD awareness was lowest in men (31.8%), adults 70 years of age and older (33.3%), and those with lower education levels (28.6%) and lower income (30.9%).
TABLE 3.
Awareness of atherosclerosis risk factors, cardiovascular diseases and other diseases by demographic characteristics (combining ‘very familiar’ and ‘somewhat familiar’ responses)
| Risk factors |
Sex |
Age, years |
Education |
Annual income |
Total (n=501) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=233) | Female (n=268) | 50–69 (n=345) | 70+ (n=156) | ≤ High school (n=301) | > High school (n=194) | <$40,000 (n=233) | ≥ $40,000 (n=192) | ||
| High blood pressure | 185 (79.4) | 217 (81.0) | 285 (82.6) | 117 (74.5) | 236 (78.4) | 162 (83.5) | 180 (76.9) | 162 (84.4) | 402 (80.2) |
| High cholesterol | 187 (80.6) | 206 (76.9) | 289 (83.8) | 105 (67.3) | 222 (73.8) | 166 (85.6) | 180 (76.9) | 159 (82.8) | 393 (78.6) |
| Diabetes | 171 (73.4) | 197 (73.5) | 272 (78.8) | 96 (61.5) | 205 (67.9) | 159 (82.0) | 161 (69.1) | 152 (79.2) | 368 (73.5) |
| Coronary disease | |||||||||
| Stroke | 165 (70.8) | 195 (72.5) | 267 (77.4) | 93 (59.6) | 190 (62.9) | 167 (86.1) | 158 (67.5) | 156 (81.3) | 360 (71.7) |
| Coronary artery disease | 126 (54.1) | 130 (48.5) | 192 (55.8) | 64 (41.0) | 124 (41.2) | 129 (66.5) | 105 (44.9) | 112 (58.6) | 256 (51.1) |
| Congestive heart failure | 108 (46.4) | 132 (49.3) | 182 (52.8) | 58 (37.2) | 120 (39.9) | 116 (59.8) | 102 (43.8) | 109 (56.8) | 240 (47.9) |
| Peripheral arterial disease | 74 (31.8) | 104 (38.8) | 126 (36.5) | 52 (33.3) | 86 (28.6) | 90 (46.4) | 72 (30.9) | 77 (40.1) | 178 (35.5) |
| Other diseases | |||||||||
| Multiple sclerosis | 97 (41.6) | 119 (44.2) | 166 (48.1) | 49 (31.4) | 106 (35.2) | 107 (55.2) | 80 (34.2) | 103 (53.6) | 216 (43.0) |
| Lou Gehrig’s disease (ALS) | 72 (30.9) | 84 (31.3) | 113 (32.8) | 43 (27.6) | 66 (21.9) | 87 (44.8) | 59 (25.3) | 75 (39.1) | 156 (31.1) |
| Cystic fibrosis | 65 (27.9) | 76 (28.4) | 114 (33.0) | 27 (17.3) | 67 (22.3) | 72 (37.1) | 52 (22.2) | 67 (34.9) | 141 (28.1) |
Data presented as n (%). Note: Values in bold denote pairwise significance from the associated value. ALS Amyotrophic lateral sclerosis
Risk factors and cardiovascular diseases
The prevalence of atherosclerotic risk factors and cardiovascular diseases in the study population was comparable with the prevalence of these conditions in the Canadian population (Table 4). For risk factors, 43.4% of respondents reported a history of high blood pressure, 36.7% had high blood cholesterol, 12.0% had diabetes, 18.2% were current smokers and 40.5% were former smokers. Chest pain or angina was reported in 18.2% of respondents, and 10.0% of the population previously suffered a heart attack. Approximately 7.6% of subjects reported a prior coronary angioplasty or coronary artery bypass surgery. Stroke (4.2%), transient ischemic attack symptoms (5.8%), and carotid artery surgery or stenting (1.8%) were reported less frequently.
TABLE 4.
Risk factors, smoking history, and associated cardiovascular diseases by demographic characteristics of the study population
|
Sex |
Age, years |
Education |
Annual income |
PAD symptoms |
Total (n=501) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n=233) | Female (n=268) | 50–69 (n=345) | 70+ (n=156) | ≤ High school (n=301) | > High school (n=194) | <$40,000 (n=233) | ≥$40,000 (n=192) | One or more (n=151) | None (n=350) | ||
| High blood pressure | 81 (34.8) | 137 (50.9) | 132 (38.3) | 85 (54.5) | 144 (47.8) | 71 (36.6) | 110 (47.2) | 73 (38) | 79 (52.3) | 138 (39.4) | 218 (43.4) |
| High cholesterol | 90 (38.8) | 94 (34.9) | 135 (39.1) | 49 (31.4) | 110 (36.5) | 70 (36.1) | 90 (38.6) | 63 (32.8) | 74 (49) | 110 (31.4) | 184 (36.7) |
| Diabetes | 31 (13.3) | 29 (10.8) | 36 (10.5) | 23 (14.7) | 42 (14) | 17 (8.8) | 36 (15.4) | 14 (7.3) | 28 (18.4) | 32 (9.1) | 60 (12.0) |
| Chest pain or angina | 55 (23.6) | 36 (13.4) | 55 (16) | 36 (22.9) | 62 (20.6) | 27 (13.9) | 48 (20.5) | 28 (14.6) | 48 (31.8) | 43 (12.3) | 91 (18.2) |
| Heart attack | 35 (15) | 15 (5.6) | 31 (9) | 19 (12.2) | 37 (12.3) | 12 (6.2) | 30 (12.8) | 13 (6.8) | 24 (15.9) | 26 (7.4) | 50 (10.0) |
| Coronary bypass surgery or angioplasty | 26 (11.2) | 12 (4.5) | 22 (6.4) | 16 (10.3) | 29 (9.6) | 9 (4.6) | 23 (9.8) | 10 (5.2) | 18 (11.8) | 20 (5.7) | 38 (7.6) |
| Stroke | 7 (3) | 14 (5.2) | 13 (3.8) | 8 (5.1) | 12 (4) | 10 (5.2) | 14 (6) | 4 (2.1) | 12 (7.9) | 10 (2.9) | 21 (4.2) |
| Mini-stroke or TIA | 12 (5.2) | 17 (6.3) | 13 (3.8) | 16 (10.3) | 17 (5.6) | 13 (6.7) | 16 (6.9) | 10 (5.2) | 15 (9.9) | 14 (4) | 29 (5.8) |
| Carotid artery surgery or stenting | 5 (2.1) | 4 (1.5) | 5 (1.4) | 5 (3.2) | 7 (2.3) | 2 (1) | 7 (3) | 1 (0.5) | 7 (4.6) | 2 (0.6) | 9 (1.8) |
| Smoking history | |||||||||||
| Current | 48 (20.6) | 43 (16) | 82 (23.8) | 9 (5.8) | 56 (18.6) | 34 (17.5) | 52 (22.2) | 32 (16.7) | 35 (23.2) | 56 (16) | 91 (18.2) |
| Past | 113 (48.5) | 90 (33.6) | 129 (49.2) | 74 (50.3) | 127 (51.8) | 75 (46.9) | 96 (52.7) | 77 (48.1) | 61 (52.6) | 142 (48.3) | 203 (49.6) |
| Never | 71 (30.6) | 135 (50.4) | 133 (38.6) | 73 (46.8) | 118 (39.2) | 85 (43.8) | 86 (36.9) | 83 (43.2) | 55 (36.4) | 152 (43.4) | 206 (41.2) |
Data presented as n (%). Note: Values in bold denote pairwise significance from the associated value. PAD Peripheral arterial disease; TIA Transient ischemic attack
Knowledge of PAD among the ‘PAD aware’ cohort
The survey assessed more specific descriptors of PAD knowledge among the 178 survey respondents who reported to be somewhat or very familiar with PAD. Among this group, knowledge of known PAD risk factors was poor (Table 5). Nearly one-half did not know that diabetes could lead to PAD, and 41.6% did not link smoking with PAD. Many did not know that high blood pressure (48.9%) and high cholesterol (51.4%) can cause PAD. Current scientific evidence has not established a causal relationship between obesity or lack of exercise and PAD, yet most survey respondents cited both as potential causes of PAD. Knowledge of known risk factors was lower in respondents 70 years of age and older, and in those with less education and lower income.
TABLE 5.
Perceived causes of peripheral arterial disease (PAD) among those aware of PAD by demographic characteristics (combining ‘a lot’ and ‘a moderate’ amounts). Question: “Do the following increase the risk of getting PAD/PVD?”
|
Sex |
Age, years |
Education |
Annual income |
Total (n=178) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n=74) | Female (n=104) | 50–69 (n=126) | 70+ (n=52) | ≤ High school (n=86) | > High school (n=90) | <$40,000 (n=71) | ≥ $40,000 (n=77) | ||
| Cigarette smoking | 39 (52.7) | 65 (62.5) | 79 (62.7) | 25 (48.1) | 43 (50.0) | 59 (65.6) | 36 (50.0) | 57 (75.0) | 104 (58.4) |
| Being overweight | 43 (58.1) | 59 (56.2) | 82 (64.6) | 20 (38.5) | 46 (52.9) | 54 (60.0) | 37 (51.4) | 53 (69.7) | 102 (57.0) |
| Lack of exercise | 37 (50.0) | 60 (57.7) | 76 (60.3) | 20 (39.2) | 39 (44.8) | 56 (62.9) | 31 (43.7) | 53 (68.8) | 97 (54.5) |
| High blood pressure | 34 (45.9) | 57 (54.8) | 70 (55.1) | 21 (41.2) | 41 (47.1) | 48 (53.9) | 30 (41.7) | 50 (64.9) | 91 (51.1) |
| Diabetes | 34 (45.9) | 56 (53.8) | 65 (51.6) | 25 (48.1) | 36 (41.4) | 53 (58.9) | 34 (47.2) | 45 (58.4) | 90 (50.6) |
| High cholesterol | 33 (45.2) | 53 (51.0) | 67 (52.8) | 19 (37.3) | 37 (42.5) | 48 (53.3) | 32 (44.4) | 46 (59.7) | 86 (48.6) |
| Heart attack or stroke | 28 (37.8) | 50 (48.1) | 63 (49.6) | 16 (30.8) | 35 (40.2) | 43 (47.8) | 27 (37.5) | 44 (57.1) | 78 (43.8) |
| Having a close family member who has had a heart attack or stroke | 19 (25.7) | 46 (44.2) | 50 (39.7) | 14 (27.5) | 28 (32.6) | 35 (39.3) | 25 (34.7) | 34 (44.2) | 65 (36.5) |
| Drinking alcohol | 19 (26.0) | 44 (42.3) | 49 (38.9) | 14 (26.9) | 27 (31.4) | 34 (38.2) | 26 (36.6) | 29 (37.7) | 63 (35.6) |
Data presented as n (%). Note: Values in bold denote pairwise significance from the associated value. PVD Peripheral vascular disease
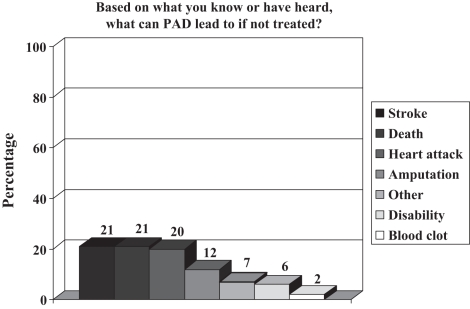
Knowledge of potential consequences of PAD among the ‘PAD aware’ group was also poor (Figure 1). Few respondents associated PAD with a risk of stroke (21.3%), death (20.8%), heart attack (19.8%) and amputation (12.4%). Only 6.7% of respondents knew that PAD could lead to disability or diminished ability to walk. Knowledge of potential consequences was lowest in those 70 years of age and older.
Figure 1).
Perceived consequences of peripheral arterial disease (PAD) among those who are ‘PAD aware’
The ‘PAD aware’ group was also surveyed regarding their sources of PAD information. Broadcast or cable television (25.3%) was the leading source of information, followed by family members or friends (18.5%), or other miscellaneous sources (15.6%). Other sources included books, brochures, medical journals and reading material at the doctors’ office. Few respondents reported receiving PAD information from a physician (13.5%), nurse (1.7%) or other health care professional (1.7%). Media information sources, such as the newspaper (8.4%), internet (5.1%) or radio (1.1%), were less frequently cited.
DISCUSSION
Key findings
The first Canadian survey of public knowledge of PAD confirms that the nation has significant knowledge gaps regarding this widespread atherosclerotic disease. Most Canadians do not know that PAD is a major risk marker of heart attack, stroke and death. Canadians are also unaware that PAD can cause major leg ischemia symptoms, disability, a reduced quality of life and amputation. Furthermore, knowledge of PAD risk factors and symptoms is poor. A recent publication (20) demonstrated that the Chinese Canadian population has a low awareness of heart disease and stroke. In addition, low Canadian public awareness of hypertension and its association with other cardiovascular diseases (21) is consistent with our findings.
Lack of public knowledge regarding PAD poses a major barrier that contributes to diagnosis and treatment rates. When individuals with, or at risk for, PAD are not aware of key symptoms or signs of the disease, efforts to prevent morbid, mortal and expensive cardiovascular ischemic events are compromised. Comparably low public awareness of PAD has also recently been demonstrated in the United States in a similar PAD public awareness survey (17). To our knowledge, no other countries have reported PAD public awareness rates (22).
The prevalence of PAD is expected to increase as the population ages (2,3). Research has shown that current PAD diagnosis and treatment rates are much lower than for other forms of atherosclerotic arterial disease (23). To improve PAD outcomes, the Prevention of Atherothrombotic Disease Network issued a “Call to Action” (24) that outlined five key unmet needs: increase awareness of PAD and its consequences (myocardial infarction, stroke, vascular death); improve the identification of patients with symptoms of PAD; initiate screening for patients at high risk for PAD (eg, smokers, people with diabetes and people with a history of myocardial infarction and/or stroke); improve treatment rates among patients who have been diagnosed with PAD; and increase the rate of early detection among the high-risk population. PAD is most often asymptomatic, and yet these patients are at very high short-term cardiovascular risk. These data support the use of targeted PAD diagnostic efforts via use of the physical examination and ankle-brachial index on high-risk patients. These ‘high-risk’ PAD patients are presently unaware of their increased risk of heart attack and stroke, and are therefore unable to take action to reduce their risk.
Socioeconomic status, sex and health disparities
The present data illustrate that PAD-related knowledge gaps were more significant in the elderly, less educated and lower income respondents. Also, a robust database (25) documents that there is a higher incidence of amputation related to PAD in the diabetic population. Socioeconomic status, Aboriginal identity, sex and geographical location are important factors associated with health disparities in Canada (26). Men in the lowest income quintile live an average of five years less than men in the highest income quintile; the gap among women is two years (26).
Unlike the United States, Canada has a universal access health care system through which primary care availability and access to all residents are addressed. However, public funding of health care in Canada currently does not fully prevent these health disparities. Furthermore, the current shortage of physicians is associated with the risk of many individuals being without access to a primary care physician. When the health care system is not organized to proactively detect prevalent PAD in communities, it may be particularly prudent and cost-effective for public awareness and education efforts to help individuals at risk identify their risk and, therefore, prevent atherosclerotic events. Therefore, our data suggest that new and major national efforts need to be initiated and should use strong, culturally appropriate PAD risk messages to increase awareness of PAD.
PAD information sources
Respondents who were familiar with PAD primarily learned about the disease from television, friends, family members and magazines, rather than through health care professionals. Few individuals reported to receive information on PAD from a physician (14%), nurse (2%) or other health care professional (1.7%). While the Internet is a source for quickly accessible medical information, only 5% of survey respondents obtained PAD information online. This is in contrast to other reports on how people obtain heart health information, but is consistent with other sources of medical information (27,28). Most importantly, the data that define current sources of public PAD health information suggest an opportunity to use each potential source (eg, health care provider, television and print media) to create awareness of PAD. Physicians and other health care professionals should play a larger role in disseminating cardiovascular risk information to the public.
Cardiovascular health campaigns
Cardiovascular disease knowledge and awareness programs have been well implemented for more than three decades (29,30). Inadequate knowledge of hypertension risk has been linked to low rates of blood pressure control, and improvements in blood pressure have been demonstrated with programs of public education (29,30). In the United States, campaigns designed to increase awareness of heart disease risk among women have demonstrated measurable improvements (31). The Heart and Stroke Foundation assesses Canadian awareness of specific heart health issues annually and is launching a heart awareness campaign targeting women. To date, however, PAD has not been a priority in Canadian cardiovascular public health programs. A national awareness program could be effective in raising awareness of PAD, as well as its symptoms, risk factors and consequences (32). National efforts should provide benefit to both sexes, which remain at nearly equal relative risk for PAD-associated ischemic events and target particularly high-risk populations such as the elderly. Data from the present survey can be used to strategically develop campaign approaches and serve as a baseline for assessing future changes in PAD knowledge.
Many theories of behaviour change rely on a person’s risk awareness and access to information (33,34). One finding evident from our work is that health promotion campaigns should consider individual differences and include distinct messages for subgroups of the population, at least those defined by age and education level. Other variables identified as determinants in the communication process (eg, method of disseminating information or source of information) should also be considered. It seems that cardiovascular disease awareness programs have been successful in reaching some segments of the population, but programs need to be developed for the most disadvantaged sectors of the population (21,35).
The Peripheral Arterial Disease Coalition, coordinated by the nonprofit Vascular Disease Foundation, is an international alliance of 71 cardiovascular and vascular health care professional societies, health advocacy groups, corporations and government agencies working to improve the health and health care of people with, or at risk for, PAD (36). In September 2006, the Peripheral Arterial Disease Coalition and the United States Department of Health and Human Services’ National Heart, Lung and Blood Institute launched a national PAD awareness campaign titled “Stay in Circulation: Take Steps to Learn about PAD” (37). A national PAD awareness campaign was considered to be key in achieving cardiovascular health prevention goals because it would foster improved public access to scientifically accurate health information and facilitate an effective patient-clinician partnership to improve PAD-related health. Clinical practice tools, including slides and patient resources, are available on the Coalition’s Web site (www.padcoalition.org).
Clinical implications
A recent survey of vascular surgery bypass patients who were admitted to a large Canadian tertiary care centre indicated that a significant care gap exists in the use of life-saving medications among patients with PAD (38,39). Many of these patients had established coronary or cerebrovascular disease or the presence of two or more cardiovascular risk factors, and were poorly treated (39,40). Achievement of target risk reduction goals is known to improve cardiovascular outcomes (39). The Canadian Cardiovascular Society and Inter-Society Consensus (TASC II) documents, and the ACC/AHA guidelines for the management of patients with PAD recommend aggressive risk factor management in this patient population (12,13,40). Many risk management clinics for the PAD patient population have been initiated across Canada to ensure this patient population is managed aggressively. Distribution of PAD resources to clinicians, patients and the general public can reduce the current knowledge gap and help informed individuals work with informed clinicians to improve PAD outcomes.
Study limitations
The response rate of the present study was relatively low compared with some previous Canadian surveys (33,21). We note that there is evidence that survey response rates may be declining in many countries (41). Also, a volunteer response bias may exist because it is possible that the PAD awareness of the cohort sampled was greater than that of a more representative general population. However, these results were consistent with a larger study in the United States (17) and likely provide a reasonable representation of true deficiencies in knowledge of PAD in the Canadian public. The limited study sample size and use of a list-assisted random digit dialing method resulted in a sample not fully representative of all Canadian ethnic groups. There were few minority respondents in the study, which may limit the generalizability of results to these important populations. As noted in the United States study, no previous Canadian efforts have led to the use of a common PAD nomenclature among clinicians or the public. Before the 2006 publication of the guidelines for the management of patients with PAD, differing terminology was used to describe PAD to the public, which could diminish efforts to improve public PAD awareness (12,13). However, anticipating this, we designed our survey to be maximally inclusive of common terms used by the public to define PAD and likely represents the best available estimate of public PAD awareness.
CONCLUSION
The present survey demonstrates that public knowledge of the causes or consequences of PAD is low in Canada. Knowledge gaps are more pronounced in the elderly and in individuals with lower income and lower education levels. PAD-related knowledge is far below that of other cardiovascular diseases and risk factors, making it an important public health concern. These findings reinforce the need for national educational efforts on PAD. A larger and more inclusive sample size representing all ethnic groups is required. Health professionals, the media, the health care industry and the government share a responsibility to work together to inform the public about this very prevalent cardiovascular disease that affects thousands of Canadians.
Acknowledgments
The authors acknowledge the contributions of Eileen Harwood PhD, Assistant Professor of Epidemiology and Community Health, University of Minnesota School of Public Health (Minneapolis, Minnesota), for reviewing the manuscript.
Footnotes
SOURCES OF FUNDING: Unrestricted educational grants to the Peripheral Arterial Disease Coalition to support the independent design and performance of this survey were provided by sanofi-aventis Canada Inc, the Bristol-Myers Squibb/sanofi-aventis Partnership and Cordis Endovascular, a division of Cordis Corporation.
DISCLOSURES: M Lovell served on the sanofi-aventis Canadian Peripheral Arterial Disease Advisory Board. Dr Harris has received research grant support from sanofi-aventis. Dr Hirsch has received research support from the National Institutes of Health, the Bristol-Myers Squibb/sanofi-aventis Partnership, sanofi-aventis, Omron Healthcare and AstraZeneca. Dr Mohler has received research grant support from the Bristol-Myers Squibb/sanofi-aventis Partnership and GlaxoSmithKline Inc, and serves on speakers bureaus for AstraZeneca, the Bristol-Myers Squibb/sanofi-aventis Partnership, and Merck Frosst. Dr Abramson has received research support from AstraZeneca, Eli Lilly Canada, sanofi-aventis, Boehringer Ingelheim (Canada) Ltd and Merck Frosst, and serves on national advisory boards for AstraZeneca, Boehringer Ingelheim (Canada) Ltd, Novartis Pharmaceuticals Canada Inc and sanofi-aventis. G Twillman, P Schroder and Drs Criqui, Forbes and Galloway report no conflicts.
NOTE: The opinions expressed in the present article are those of the author(s) and do not necessarily reflect the views of the United States Department of Health and Human Services’ Office of Public Health and Science or the United States government.
REFERENCES
- 1.Rosamond W, Flegal K, Furie K, et al. for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics – 2008 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Criqui MH. Peripheral arterial disease – epidemiological aspects. Vasc Med. 2001;6(Suppl 1):3–7. doi: 10.1177/1358836X0100600i102. [DOI] [PubMed] [Google Scholar]
- 3.Diehm C, Schuster A, Allemberg R, et al. High prevalence of peripheral arterial disease and comorbidity in 6880 primary care patients: Cross sectional study. Atherosclerosis. 2004;172:95–105. doi: 10.1016/s0021-9150(03)00204-1. [DOI] [PubMed] [Google Scholar]
- 4.Meru AV, Mittra S, Thyagarajan B, Chugh A. Intermittent claudication: An overview. Atherosclerosis. 2006;187:221–37. doi: 10.1016/j.atherosclerosis.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 5.Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381–6. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- 6.Steg G, Bhatt DL, Wilson PWF, et al. for the REACH Registry Investigators One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–206. doi: 10.1001/jama.297.11.1197. [DOI] [PubMed] [Google Scholar]
- 7.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: Results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2004;110:738–43. doi: 10.1161/01.CIR.0000137913.26087.F0. [DOI] [PubMed] [Google Scholar]
- 8.Allison MA, Ho E, Denenberg JO, et al. Ethnic specific prevalence of peripheral arterial disease in the United States. Am J Prev Med. 2007;32:328–33. doi: 10.1016/j.amepre.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Hirsch AT, Criqui MH, Treat-Jacobsen D, et al. Peripheral arterial disease detection, awareness and treatment in primary care. JAMA. 2001;286:1317–24. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 10.Lange S, Diehm S, Darius H, et al. High prevalence of peripheral arterial disease and low treatment rates in elderly primary care patients with diabetes. Exp Clin Endocrinol Diabetes. 2004;112:566–73. doi: 10.1055/s-2004-830408. [DOI] [PubMed] [Google Scholar]
- 11.Fowkes FG, Housley E, Cawood EH, Macintyre CC, Ruckley CV, Precott RJ. Edinburgh Artery Study: Prevalence of asympomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1991;20:384–92. doi: 10.1093/ije/20.2.384. [DOI] [PubMed] [Google Scholar]
- 12.Abramson BL, Huckell V, Anand S, et al. Canadian Cardiovascular Society Consensus Conference: Peripheral arterial disease – executive summary. Can J Cardiol. 2005;21:997–1006. [PubMed] [Google Scholar]
- 13.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): Executive summary – a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines. J Am Coll Cardiol. 2006;47:1239–312. doi: 10.1016/j.jacc.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 14.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 15.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure National High Blood Pressure Education Program Coordinating Committee. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.McAlister FA, Wooltorton E, Campbell NRC, for The Canadian Hypertension Education Program The Canadian Hypertension Education Program (CHEP) recommendations: Launching a new series. CMAJ. 2005;173:508–9. doi: 10.1503/cmaj.050737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirsch AT, Murphy TP, Lovell MB, et al. for the Peripheral Arterial Disease Coalition Gaps in public knowledge of peripheral arterial disease: The first national PAD public awareness survey. Circulation. 2007;116:2086–94. doi: 10.1161/CIRCULATIONAHA.107.725101. [DOI] [PubMed] [Google Scholar]
- 18.Brick JM, Waksberg J, Kulp D, Starer A. Bias in list-assisted telephone samples. Public Opin Q. 1995;59:218–35. [Google Scholar]
- 19.Health Canada Statistics Population<http://www41.statcan.ca/2007/3867/ceb3867_000_e.htm> (Version current at November 18, 2008).
- 20.Chow C-M, Chu JY, Tu JV, Moe GW. Lack of awareness of heart disease and stroke among Chinese Canadians: Results of a pilot study of the Chinese Canadian Cardiovascular Health Project. Can J Cardiol. 2008;24:623–8. doi: 10.1016/s0828-282x(08)70650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petrella RJ, Campbell NR. Awareness and misconception of hypertension in Canada: Results of a national survey. Can J Cardiol. 2005;21:589–93. [PubMed] [Google Scholar]
- 22.Clement DL, Belch JJF. Vascular disease public education: The mandate is international. Int Angiol. 2004;23:1–4. [PubMed] [Google Scholar]
- 23.Ismal HM, Jackosn K, Smith D. Diagnosis and treatment of peripheral arterial disease compared with other atherosclerotic vascular diseases in a university primary care clinic. J Investig Med. 2006;54:255–61. doi: 10.2310/6650.2006.05049. [DOI] [PubMed] [Google Scholar]
- 24.Belch JJF, Topol EJ, Agnelli G, et al. Critical issues in peripheral arterial disease detection and management: A call to action. Arch Int Med. 2003;163:884–92. doi: 10.1001/archinte.163.8.884. [DOI] [PubMed] [Google Scholar]
- 25.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: Epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–81. doi: 10.1001/jama.287.19.2570. [DOI] [PubMed] [Google Scholar]
- 26.Public Health Agency of Canada. Reducing Health Disparities – Roles of the Health Sector: Recommended Policy Directions and Activities <http://www.phac-aspc.gc.ca/ph-sp/disparities/dr_policy_1_e.html> (Version current at November 18, 2008).
- 27.Wong B, Yung BM, Chow CM, Boswell KM, Abramson BL. Increasing internet use among cardiovascular patients: New opportunities for heart health promotion. Can J Cardiol. 2005;21:349–54. [PubMed] [Google Scholar]
- 28.Chan RH, Kwan K, Abramson BL. Complimentary alternative medicine use in patients with CV disease: A breakdown in patient-physician communication. Program and Abstracts of the American Heart Association Scientific Seminar; Dallas: Nov 13 to 16, 2005. (Abst 2520) [Google Scholar]
- 29.Burt VL, Cutler JA, Hoggins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population: Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26:60–9. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- 30.Muntner P, DeSalvo KB, Wildman RP, Raggi P, He J, Whelton PK. Trends in the prevalence, awareness, treatment and control of cardiovascular disease risk factors among noninstitutionalized patients with a history of myocardial infarction and stroke. Am J Epidemiol. 2006;163:913–20. doi: 10.1093/aje/kwj124. [DOI] [PubMed] [Google Scholar]
- 31.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women’s awareness of heart disease: An American Heart Association national study. Circulation. 2004;109:573–9. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- 32.Hirsch AT, Gloviczki P, Drooz A, Lovell M, Creager MA, on behalf of the Trustees of the Vascular Disease Foundation The Mandate for Creation of a National PAD Public Awareness Program: An opportunity to improve cardiovascular health. J Vasc Surg. 2004;39:474–81. doi: 10.1016/j.jvs.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 33.Potvin L, Richard L, Edwards AC. Knowledge of cardiovascular disease risk factors among the Canadian population: Relationships with indicators of socioeconomic status. CMAJ. 2000;162(9 Suppl):S5–11. [PMC free article] [PubMed] [Google Scholar]
- 34.Janz N, Becker MH. The health belief model: A decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 35.Onysko J, Maxwell C, Eliaszaw M, Zhang JH, Johansen H, Campbell NR. Large increases in hypertension diagnosis and treatment in Canada after a healthcare professional program. Hypertension. 2006;48:853–60. doi: 10.1161/01.HYP.0000242335.32890.c6. [DOI] [PubMed] [Google Scholar]
- 36.Peripheral Arterial Disease Coalition <http://www.padcoalition.org/wp/> (Version current at November 18, 2008).
- 37.National Heart, Lung, and Blood Institute. Stay in Circulation Campaign <http://www.nhlbi.nih.gov/health/public/heart/pad/stay/index.html> (Version current at November 18, 2008).
- 38.Kundhal MD, Chin SL, Harrison L, et al. Patterns of medical therapy in patients with peripheral arterial disease in a tertiary care centre in Canada. Can J Cardiol. 2007;23:357–61. doi: 10.1016/s0828-282x(07)70768-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Omran M, Lindsay TF, Major J, Jawas A, Leiter LA, Verma S, Systematic Assessment of Vascular Risk Investigators Perceptions of Canadian vascular surgeons toward pharmacological risk reduction in patients with peripheral arterial disease. Ann Vasc Surg. 2006;20:555–63. doi: 10.1007/s10016-006-9110-3. [DOI] [PubMed] [Google Scholar]
- 40.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, on behalf of the TASC II Working Group Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) J Vasc Surg. 2007;45(1 Suppl):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 41.Tolonen H, Helakorpi S, Talala K, Helasoja V, Martelin T, Prattala R. 25-year trends and socio-demographic differences in response rates: Finnish adult health behaviour survey. Eur J Epidemiol. 2006;21:409–15. doi: 10.1007/s10654-006-9019-8. [DOI] [PubMed] [Google Scholar]