Abstract
BACKGROUND:
Octogenarians are the fastest growing population in Canada and have also been referred for coronary artery bypass grafting (CABG) with increasing frequency during the past decade.
OBJECTIVE:
To examine the changing trends in preoperative risk profiles, postoperative outcomes and hospital resource use in the octogenarian population.
METHODS:
A retrospective review was conducted to identify all patients 80 years of age or older who underwent isolated CABG at the Toronto General Hospital (Toronto, Ontario) between 1990 and June 2005. To examine the effect of time on preoperative risk, patients were divided into three groups based on year of operation: 1990 to 1994, n=92; 1995 to 1999, n=202; and 2000 to June 2005, n=314.
RESULTS:
The preoperative risk profile of octogenarians undergoing CABG has changed over the years. The percentage of patients with diabetes, dyslipidemia, hypertension and left main disease increased over time (P<0.05). However, the requirement for urgent/emergent operations decreased. In-hospital mortality declined from 7.1% (1990 to 1999) to 3.2% (2000 to June 2005, P=0.02). The prevalence of low cardiac output syndrome, intra-aortic balloon pump insertion and stroke decreased over time. Preoperative myocardial infarction (OR 4, P=0.0004), left main disease (OR 3.7, P=0.0013) and year of operation (1990 to 1994 [OR 3.3, P=0.03]; 1995 to 1999 [OR 2.9, P=0.02]) independently predicted in-hospital mortality. Hospital resource use in terms of hours on ventilator, length of stay in the intensive care unit and postoperative length of stay decreased over time (P<0.0001).
CONCLUSION:
Despite a changing risk profile, hospital outcomes of octogenarians were improved over time with a reduction in hospital resource use. The results suggest that CABG can and should be performed in this expanding population.
Keywords: Aging, Cardiopulmonary bypass
Abstract
HISTORIQUE :
Les octogénaires constituent la population qui croît le plus rapidement au Canada et ils sont de plus en plus nombreux à subir des pontages coronariens depuis une dizaine d’années.
OBJECTIF :
Analyser l’évolution des tendances en ce qui concerne le risque pré-opératoire, l’issue post-opératoire et l’utilisation des ressources hospitalières chez la population octogénaire.
MÉTHODES :
Les auteurs ont procédé à une analyse rétrospective pour recenser tous les patients de 80 ans ou plus qui ont subi un pontage coronarien à l’Hôpital Général de Toronto (Toronto, Ontario) entre 1990 et juin 2005. Pour mesurer l’effet du temps sur le risque pré-opératoire, les patients ont été scindés en trois groupes selon l’année de leur intervention : 1990 à 1994 n = 92, 1995 à 1999 n = 202 et 2000 à juin 2005 n = 314.
RÉSULTATS :
Le profil de risque pré-opératoire des octogénaires devant subir un pontage coronarien a évolué au cours des ans. Le pourcentage de patients souffrant de diabète, de dyslipidémie, d’hypertension et d’atteinte du tronc de la coronaire gauche a augmenté (p < 0,05). Toutefois, les critères appliqués aux interventions urgentes/très urgentes ont diminué. La mortalité en cours d’hospitalisation est passée de 7,1 % (1990 à 1999) à 3,2 % (entre 2000 et juin 2005, p = 0,02). La prévalence du syndrome de bas débit cardiaque, le recours à la pompe à ballonnet intra-aortique et les AVC ont aussi diminué avec le temps. L’infarctus du myocarde pré-opératoire (RC 4, p = 0,0004), la maladie du tronc coronaire gauche (RC 3,7, p = 0,0013) et l’année de l’intervention 1990 à 1994 (RC 3,3, p = 0,03) et 1995 à 1999 (RC 2,9, p = 0,02) se sont révélés des prédicteurs indépendants de la mortalité en cours d’hospitalisation. L’utilisation des ressources hospitalières en termes d’heures sous ventilation mécanique, de durée des hospitalisations aux soins intensifs et de durée des séjours post-opératoires a diminué avec le temps (p < 0,0001).
CONCLUSION :
Malgré l’évolution du profil de risque, le prognostic hospitalier des octogégenaires s’est amélioré avec le temps, ce qui s’est accompagné d’une réduction de l’utilisation des ressources hospitalières. Selon ces résultats, le pontage coronarien peut et doit être offert à cette population dont le nombre est en hausse.
Seniors are one of the fastest growing population groups in Canada. Patients 85 years of age and older are the fastest growing segment of the overall senior population. Approximately one in 10 Canadian seniors are now 85 years of age or older, up from one in 20 in the early 1920s. Statistics Canada (1) has projected that there will be almost two million Canadians 85 years of age and older in 2051, almost five times the current figure. The life expectancy of Canadian seniors has also risen substantially during the past century. Rapid growth of the octogenarian population, combined with increased life expectancy, is expected to increase the number of octogenarians being referred for coronary artery bypass grafting (CABG).
Age has traditionally been an independent predictor of mortality in patients undergoing either isolated CABG or valvular surgery (2–7). At the Toronto General Hospital (Toronto, Ontario), elderly patients (older than 80 years of age) continue to be offered surgery primarily for symptomatic relief of angina or dyspnea. Usually, this necessitates hospital admission with intravenous drug therapy before surgical intervention is considered. However, with improved results in the elderly population, we began to offer ‘elective’ surgery to appropriately selected patients (2). The purpose of the present study was to examine the trends in surgical outcomes following isolated CABG in patients 80 years of age or older, with a particular emphasis on the changing demographic profile and the impact on hospital resource use.
METHODS
The study population included all patients 80 years of age or older who underwent isolated CABG between 1990 and June 2005 at the Toronto General Hospital. All patient data were entered prospectively into an institutional database by a trained database management group. Preoperative, intraoperative and postoperative data were collected on standard variables. The details of this database have been published previously (5,7).
Hospital resource use was defined using the following three variables: the length of time on mechanical ventilation before postoperative tracheal extubation; the duration of stay in the intensive care unit (ICU); and the postoperative length of stay, which did not include ICU length of stay. The primary outcome of interest in the study was operative mortality (OM). OM was defined as any postoperative death occurring within the same hospital admission or within 30 days of surgery.
Statistical analysis
All statistical analyses were conducted using SAS 8.1 software (SAS Institute Inc, USA) (8). Categorical variables were analyzed using the χ2 test and are expressed as percentages. Continuous variables were analyzed by ANOVA methods and are reported as mean ± SD. Multivariable logistic regression techniques were used to determine independent predictors of OM, and to calculate factor-adjusted ORs. Model discrimination was evaluated by the area under the receiver operating characteristic (ROC) curve, and the upper and lower CIs for the ROC curve were calculated by using an SAS Macro program. Model calibration was assessed with the Hosmer-Lemeshow goodness-of-fit statistic (9).
RESULTS
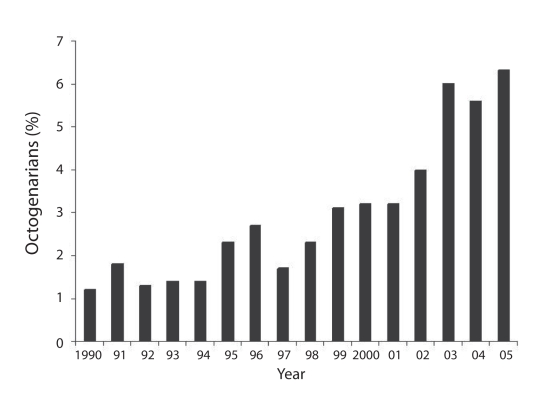
To examine outcomes over time, patients were divided into three groups based on year of operation (1990 to 1994, n=92; 1995 to 1999, n=202; 2000 to June 2005, n=314). The percentage of octogenarians among the overall CABG population gradually increased over the years and it was highest in the most recent year (Figure 1). Even in the most recent year, octogenarians represented only approximately 6% of the annual CABG population.
Figure 1).
Percentage of octogenarians among the overall coronary artery bypass graft cohort
The changing preoperative risk profiles of patients in the three time periods are shown in Table 1. The percentage of patients with diabetes, dyslipidemia, hypertension and left main disease increased over time. However, the requirement for urgent/emergent operations and the percentage of patients with chronic obstructive pulmonary disease and renal failure decreased. The percentage of women who underwent CABG was similar among the three time groups (Table 1).
TABLE 1.
Distribution of preoperative variables
| Variable |
Year of operation |
P | ||
|---|---|---|---|---|
| 1990 to 1994 | 1995 to 1999 | 2000 to June 2005 | ||
| Number of patients | 92 | 202 | 314 | |
| Age, years, mean ± SD | 82±2.5 | 82.1±2.3 | 82.1±1.81 | 0.9 |
| Body surface area, m2, mean ± SD | 1.77±0.2 | 1.79±0.2 | 1.8±0.2 | 0.2 |
| Women, % | 37 | 35.2 | 30.9 | 0.4 |
| Hypertension, % | 51.1 | 55 | 67.8 | 0.001 |
| Dyslipidemia, % | 27.5 | 40.6 | 65.8 | <0.0001 |
| Diabetes mellitus, % | 23.9 | 19.3 | 28.7 | 0.05 |
| LVEF, % | ||||
| ≥60 | 26.1 | 29.7 | 40.8 | 0.007 |
| 40 to 60 | 44.6 | 48.5 | 35 | |
| <40 | 29.3 | 21.8 | 24.2 | |
| Urgency of surgery, % | ||||
| Elective | 21.7 | 32.7 | 38.7 | <0.0001 |
| Same hospital | 44.6 | 49.5 | 48.5 | |
| Urgent/emergent | 33.7 | 17.8 | 12.8 | |
| NYHA class, % | ||||
| I or II | 7.6 | 7 | 17.3 | 0.0003 |
| III | 28.3 | 17.3 | 22.8 | |
| IV | 64.1 | 75.7 | 59.9 | |
| Triple-vessel disease, % | 80.4 | 82.2 | 85.0 | 0.5 |
| Left main disease, % | 30.4 | 28.7 | 39.2 | 0.03 |
| Number of diseased vessels, mean ± SD | 2.78±0.5 | 2.8±0.5 | 2.84±0.4 | 0.4 |
| Congestive heart failure, % | 22 | 12.9 | 17.2 | 0.1 |
| Peripheral vascular disease, % | 24.2 | 22.3 | 30.3 | 0.1 |
| COPD, % | 17.4 | 7.4 | 6.4 | 0.003 |
| Myocardial infarction, % | 27.2 | 23.8 | 26.4 | 0.7 |
| Stroke, % | 8.7 | 12.9 | 12.7 | 0.5 |
| Renal failure, % | 9.8 | 5.5 | 0 | <0.0001 |
| Previous angioplasty, % | 5.4 | 6.9 | 6.1 | 0.9 |
| Previous thrombolysis, % | 3.4 | 11.4 | 3.8 | 0.001 |
| Atrial fibrillation, % | 1.1 | 2.5 | 6.1 | 0.04 |
| Any reoperative surgery, % | 3.3 | 5 | 1 | 0.02 |
COPD Chronic obstructive pulmonary disease; LVEF Left ventricular ejection fraction; NYHA New York Heart Association
Intraoperative details for the study population are listed in Table 2. Use of the left internal thoracic artery increased over time, while use of the right internal thoracic artery did not change significantly. The total number of arteries bypassed per patient was similar in the first two time periods and decreased in the most recent era. The mean cross-clamp time did not change significantly, but the mean duration of cardiopulmonary bypass decreased over the three time periods.
TABLE 2.
Distribution of intraoperative variables
| Variable |
Year of operation |
P | ||
|---|---|---|---|---|
| 1990 to 1994 | 1995 to 1999 | 2000 to June 2005 | ||
| Use of left internal thoracic artery, % | 40.2 | 60 | 66 | <0.0001 |
| Use of right internal thoracic artery, % | 2.2 | 1 | 1.9 | 0.7 |
| Number of arteries bypassed | 3.4±0.8 | 3.5±0.9 | 3.2±0.8 | 0.02 |
| Duration of CPB, min | 87±29 | 78±33 | 78±33 | 0.03 |
| Duration of XCL, min | 59±20 | 57±21 | 58±26 | 0.7 |
| Off-pump surgery, % | 0* | 4 | 8 | – |
Data are presented as mean ± SD unless otherwise specified.
Off-pump surgeries were not performed in the 1990 to 1994 time cohort. CPB Cardiopulmonary bypass; XCL Aortic cross clamp
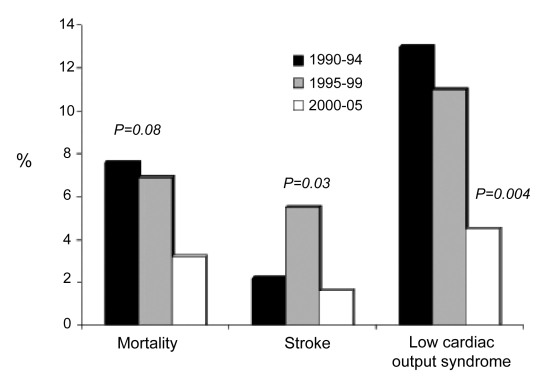
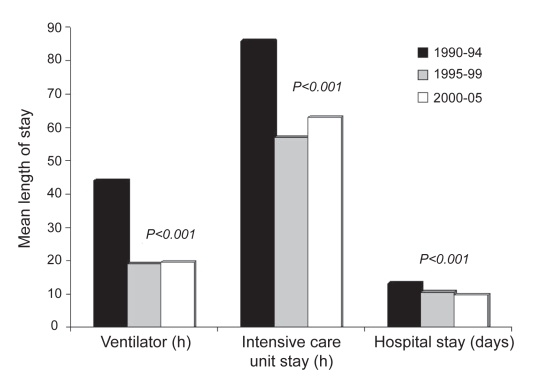
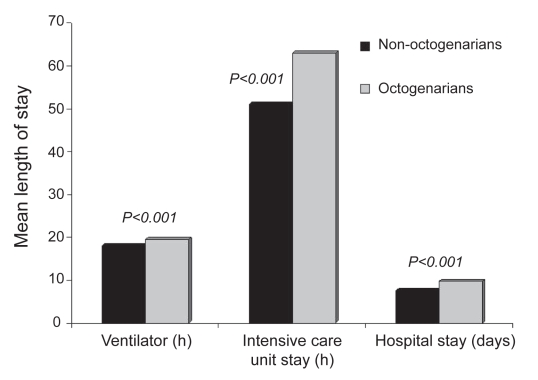
Data on postoperative outcomes and hospital resource use are shown in Figures 2 and 3. The OM rate was 5.1% (n=31). OM declined from 7.1% (1990 to 1999) to 3.2% (2000 to June 2005, P=0.02). However, hospital mortality did not change over the years in the female population (5.9% versus 7% versus 4.1%, respectively; P=0.7). The incidence of postoperative stroke and low cardiac output syndrome were significantly lower in the most recent time cohort than in the other time cohorts (Figure 2). Also, a decreasing trend was observed in the percentage of leg infections (4.4% versus 0.5% versus 1%, respectively; P=0.02) and the need for intra-aortic balloon pump support (6.5% versus 8.9% versus 1.9%; P=0.005). Hospital resource use, defined in terms of hours on ventilator, ICU length of stay and postoperative length of stay, was highest in the early group and decreased in the later two groups (Figure 3). When examining the most recent cohort, resource use was higher in octogenarians than in their younger counterparts (Figure 4). While statistically significant differences were observed in all three outcome measures, only ICU stay appears to represent a clinically significant difference and, again, was likely influenced by physician bias.
Figure 2).
Postoperative hospital outcomes
Figure 3).
Mean length of stay
Figure 4).
Mean length of stay (2000 to 2005)
Multivariable logistic regression analysis of the 608 patients who underwent an operation during the study period showed that preoperative myocardial infarction, left main disease and year of operation independently predicted mortality (Table 3). The model for logistic regression has an area under the ROC curve of 0.76 (95% CI 0.67 to 0.85) and a Hosmer-Lemeshow goodness-of-fit probability value of 0.98, indicating model discrimination and calibration.
TABLE 3.
Multivariable predictors of operative mortality
| Variable | Regression coefficient ± standard error | OR | 95% CI | P |
|---|---|---|---|---|
| Constant | −4.8±0.5 | – | – | – |
| Year of operation | ||||
| 1990 to 1994* | 1.2±0.5 | 3.3 | 1.1–9.4 | 0.03 |
| 1995 to 1999* | 1.1±0.5 | 2.9 | 1.2–7.1 | 0.02 |
| Myocardial infarction | 1.4±0.4 | 4 | 1.9–8.7 | 0.0004 |
| Left main disease | 1.3±0.4 | 3.7 | 1.7–8.1 | 0.001 |
ORs were calculated by comparing against the 2000 to June 2005 cohort
DISCUSSION
The present study examined the clinical outcomes of 608 patients 80 years of age or older who underwent CABG during a period of 15 years. The proportion of octogenarians as a percentage of all patients undergoing CABG increased steadily over time from 1% to more than 6%. The study demonstrates that, despite the changing risk profile of patients, OM declined over time, which is consistent with previously published reports (2,3,10–12). We also found that the incidence of stroke and low cardiac output syndrome decreased over time, further adding evidence to our previously documented reports of improving cardiac surgical outcomes over time (2,4,5,7). Hospital resource use expressed as length of ventilatory support, duration of stay in the ICU and postoperative length of stay also decreased over time.
In the present study population, we found that the most dominant predictor of OM was the incidence of preoperative myocardial infarction with an OR of 4. The prevalence of preoperative myocardial infarction did not change over time. Nonetheless, the mortality among patients who had preoperative myocardial infarction decreased over time from 12% in the first time cohort to 7.2% in the most recent time cohort. This may be due to improved perioperative care or the increased expertise and familiarity of surgeons operating on more octogenarians over time. Our results are in agreement with Peterson et al (10), who reported preoperative myocardial infarction to be one of the independent predictors of three-day or 30-day in-hospital mortality after CABG in a large clinical series of 24,461 patients 80 years of age or older. Similarly, Alexander et al (11) identified preoperative myocardial infarction as one of the independent predictors of OM in 4743 octogenarians undergoing CABG.
The prevalence of left main disease increased from 30.4% in the first time cohort to 39.2% in the final time cohort. The mortality associated with left main disease decreased from 17.8% to 5.7% during the 15-year period. However, left main disease was an independent predictor of mortality with an OR of 3.7. This result is in contrast to the literature in which the most contemporary and powerful predictors of hospital mortality in octogenarians included previous CABG, left ventricular dysfunction (11,12), recent myocardial infarction, shock, New York Heart Associatation (NYHA) class III to IV symptoms and advancing age (11).
As expected, year of operation was a significant predictor of OM. In the current series of patients, OM decreased from 7.6% in the 1990 to 1994 time cohort to 3.2% in 2000 to 2005, a reduction of approximately 50%. Baskett et al (3) found a similar decrease in octogenarian mortality over time. In a multicentre study of very elderly patients, Peterson et al (12) reported a reduction in hospital mortality from 5.9% in 1991 to 4.98% in 1998. An interesting finding of the present study was that the proportion of octogenarians undergoing urgent or emergent surgery decreased over time. This is likely due to the improved results of elective surgery in elderly patients (the OM for the 1990 to 1994 cohort was 5% and the OM for the 2000 to June 2005 cohort was 0.8%), with a resultant shift in philosophy over time. In the earlier time period, octogenarians were probably only offered surgery as a ‘salvage’ situation when they suffered from intractable angina or dyspnea. As operative results improved, surgical revascularization was offered to elderly patients in a more elective fashion, thereby reducing the proportion of octogenarians undergoing CABG in an urgent or emergent fashion.
Limitations
Our study is limited by the fact that it is retrospective in nature and reflects the experience of a single institution. Also, our outcomes are limited to in-hospital events, and follow-up outcomes on long-term survival or quality of life are not available. Furthermore, the sample size of each time cohort was not adequate for risk stratification of the study population. Risk stratification would have allowed us to determine whether a similar reduction in OM observed in the study population could be seen in high-risk subgroups.
CONCLUSIONS
CABG is increasingly common in octogenarians, with steadily improving outcomes over time. Compared with a younger patient population, the increased hospital resource use appears to be acceptable and justified. The present study represents the largest single-centre experience with octogenarians in the contemporary Canadian literature and serves to emphasize the fact that these patients should not be refused surgery due to age alone. Further studies examining the long-term results of revascularization in octogenarians will be useful to provide further justification for surgical intervention in this expanding patient population.
Acknowledgments
The authors thank Ms Susan Collins, database manager of cardiovascular surgery at the Toronto General Hospital, for her meticulous data collection and management skills.
REFERENCES
- 1.Statistical snapshots of Canada’s Seniors Ottawa: Statistics Canada, for the Divison of Aging and Seniors, Health Canada; 2000. <http://www.phac-aspc.gc.ca/seniors-aines/pubs/factoids/2001/toc_e.htm> (Version current at January 7, 2009). [Google Scholar]
- 2.Ivanov J, Weisel RD, David TE, Naylor CD. Fifteen-year trends in risk severity and operative mortality in elderly patients undergoing coronary artery bypass graft surgery. Circulation. 1998;97:673–80. doi: 10.1161/01.cir.97.7.673. [DOI] [PubMed] [Google Scholar]
- 3.Baskett R, Buth K, Ghali W, et al. Outcomes in octogenarians undergoing coronary artery bypass grafting. CMAJ. 2005;172:1183–6. doi: 10.1503/cmaj.1041342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borger MA, Ivanov J, Weisel RD, et al. Decreasing incidence of stroke during valvular surgery. Circulation. 1998;98(19 Suppl):II137–43. [PubMed] [Google Scholar]
- 5.Rao V, Ivanov J, Weisel RD, Ikonomidis JS, Christakis GT, David TE. Predictors of low cardiac output syndrome after coronary artery bypass. J Thorac Cardiovasc Surg. 1996;112:38–51. doi: 10.1016/s0022-5223(96)70176-9. [DOI] [PubMed] [Google Scholar]
- 6.Davierwala PM, Maganti M, Yau TM. Decreasing significance of left ventricular dysfunction and reoperative surgery in predicting coronary artery bypass grafting-associated mortality: A twelve-year study. J Thorac Cardiovasc Surg. 2003;126:1335–44. doi: 10.1016/s0022-5223(03)00936-x. [DOI] [PubMed] [Google Scholar]
- 7.Maganti MD, Rao V, Borger MA, Ivanov J, David TE. Predictors of low cardiac output syndrome after isolated aortic valve surgery. Circulation. 2005;112(9 Suppl):I448–52. doi: 10.1161/CIRCULATIONAHA.104.526087. [DOI] [PubMed] [Google Scholar]
- 8.SAS Institute . SAS/STAT User’s Guide, version 8. Cary: SAS Institute; 1988. [Google Scholar]
- 9.Hosmer D, Lemeshow S. Applied logistic regression. New York: John Wiley and Sons; 1989. [Google Scholar]
- 10.Peterson ED, Cowper PA, Jollis JG, et al. Outcomes of coronary artery bypass graft surgery in 24,461 patients 80 years of age or older. Circulation. 1995;92(9 Suppl):II85–91. doi: 10.1161/01.cir.92.9.85. [DOI] [PubMed] [Google Scholar]
- 11.Alexander KP, Anstrom KJ, Muhlbaier LH, et al. Outcomes of cardiac surgery in patients > or = 80 years: Results from the National Cardiovascular Network. J Am Coll Cardiol. 2000;35:731–8. doi: 10.1016/s0735-1097(99)00606-3. [DOI] [PubMed] [Google Scholar]
- 12.Peterson ED, Alexander KP, Malenka DJ, et al. American Heart Association Chronic CAD Working Group. Multicenter experience in revascularization of very elderly patients. Am Heart J. 2004;148:486–92. doi: 10.1016/j.ahj.2004.03.039. [DOI] [PubMed] [Google Scholar]