Abstract
This study investigated the link between exposure to early life trauma, sensitivity to current daily stressors, and cocaine dependence. Individuals with (n = 105) or without (n = 53) cocaine dependence completed the Early Trauma Inventory and the Daily Hassles Scale. In comparison to controls, cocaine-dependent individuals reported almost twice as many daily hassles and perceived those hassles more negatively (p < .001). For participants with cocaine dependence, a significant relationship between exposure to early life trauma and negative perception of current daily hassles was observed (p < .01), whereas no such relationship was observed for participants without cocaine dependence. Adverse childhood events may lead to an altered view of the environment that contributes to increased irritability with daily life events among cocaine-dependent individuals.
Keywords: Childhood, cocaine, daily hassles, stress, trauma
INTRODUCTION
A strong relationship between exposure to early life trauma and increased risk for adverse outcomes, such as substance abuse, has been documented in clinical and preclinical studies (1–4). Life events need not be traumatic nor qualify for a Criterion A PTSD event in order to influence substance use. “Daily hassles” (e.g., misplacing things, auto maintenance) are also associated with substance abuse. Seeman and Seeman (5) examined the influence of “life strains” (e.g., changes in marital status, economic strain) among 505 men and found that the frequency of stressful life events was significantly related to drinking problems (e.g., missing work, family quarrels about drinking). More recently, among 195 outpatients enrolled in an alcohol and drug treatment program, individuals who experienced ongoing stress (i.e., >2 weeks) were 2.5 times more likely to resume substance use following treatment as compared to individuals who did not experience ongoing stress (6). While research has documented that both early life trauma and daily hassles can influence substance use, the relationship between these two variables has not yet been explored.
Chronic, non-traumatic stress may result in repeated exposure to negative emotional states, which then increase the risk of using alcohol and drugs to self-medicate (7, 8). Individuals with substance use disorders (SUDs) often lead chaotic and stress-filled lives. With repeated exposure to stressors and negative affect, less provocation may be required over time to activate the psychobiological stress response system (i.e., the threshold for activation becomes minimal). Thus, events that were not previously appraised as stressful may, with repeated exposure, be perceived as threatening, and have a more negative physiological, neurobiological, and subjective impact. In addition, exposure to childhood trauma may impact the cognitive appraisal of everyday interactions through similar mechanisms.
In a previous study, our group found that cocaine-dependent men and women used cocaine more frequently in response to negative situations and temptation when they were reporting greater distress from day-to-day stressors (9). The current study aimed to preliminarily examine the relationship between exposure to early life trauma and frequency/perception of recent daily hassles in individuals with and without cocaine-dependence.
METHOD
Participants and Procedure
Participants were 158 non-treatment-seeking individuals with cocaine dependence (n = 105) or healthy controls (n = 53) enrolled in a larger study investigating the HPA axis, stress, and cocaine dependence. Participants were 18 years or older and medically stable. General exclusion criteria included psychiatric or medical conditions that could affect HPA axis functioning (e.g., major depressive disorder, posttraumatic stress disorder, diabetes, AIDS), pregnancy, or obesity. Individuals taking psychotropic medications were required to be on a stable dose for at least eight weeks before enrollment in the study. Participants in the cocaine group met DSM-IV diagnostic criteria for current (i.e., last three months) cocaine dependence. Other substance use disorders were allowed if cocaine was the primary substance of choice. Among individuals in the cocaine group, 10% had a current alcohol use disorder, 7% marijuana abuse or dependence, and 8% past history on other substances (e.g., sedatives, opiates). Participants in the control group had no current substance abuse or dependence (other than nicotine and caffeine). Approximately 9% had a history of an alcohol use disorder and 2% a history of marijuana abuse.
Participants answered an advertisement for research and were initially screened over the phone. After IRB-approved informed consent was obtained, eligible participants were interviewed and administered a battery of assessments.
Assessments
Cocaine dependence and other psychiatric diagnoses were assessed with the Structured Clinical Interview for DSM-IV (10). The Early Trauma Inventory (ETI) (11), a 56-item self-report form, evaluated childhood (i.e., before the age Z of 18) physical, sexual, emotional, and general trauma. In order to examine severe early trauma, six clinicians (3 M.D.s, 3 Ph.D.s) rated the items as “severe” or “not severe,” and a binary composite variable was created. For the purposes of this study, items that were rated as “severe” by all six clinicians were considered severe trauma items. The Daily Hassles Scale (DHS) (12) evaluated the frequency of 117 irritating or frustrating events that characterize everyday interactions with the environment (e.g., misplacing things, auto maintenance, traffic) in the past month. Participants rated how severe they perceived the hassle to be (i.e., somewhat, moderately, or extremely severe).
Statistical Analysis
Continuous response variables were modeled using cocaine status and gender as categorical predictors. When appropriate, the response was transformed to address issues with normality. In a number of the analyses, cocaine-dependent subjects were found to exhibit more variability in the response than control subjects. This was addressed by allowing the estimation of a separate variance parameter for each group (13). Dichotomous response variables were modeled using cocaine status and gender as predictors in a logistic regression model, with significant main effects interpreted using an odds ratio. Type I error rate was controlled using a Bonferroni family-wise correction.
RESULTS
Demographic Characteristics
Approximately half of the sample were men (54%), African American (56%), and single (84%). The average age was 38 years (SD = 11) and the majority (65%) were employed. Between-group comparisons revealed that cocaine-dependent individuals were more likely than controls to be male, unemployed, and African American (ps ≤ .05). These differences were statistically controlled in all of the analyses.
Baseline Frequency of Early Life Trauma History and Daily Hassles
A between-group comparison of the total number of early life traumatic events endorsed on the ETI was examined. Cocaine-dependent individuals reported experiencing an average of 11 early life traumas (SD = 6.7), and control group participants reported an average of 10 (SD = 6.7), which was not significantly different. As previously described, ETI items were rated for severity, and the following items were identified by expert consensus as severe early life traumas: being a victim rape; witnessing a murder; being a prisoner of war or held hostage; combat exposure; being victim of assault; being tied up or locked in a closet; forced genital, oral, or anal intercourse. Logistic regression was used to predict the probability of endorsing exposure to at least one severe early life trauma, using cocaine status, gender, and demographic variables as predictors. A main effect of gender was revealed (p < .001), indicating that women were 1.7 times more likely than men to endorse exposure to at least one Severe early life trauma.
Comparison of the total number of daily hassles reported revealed a significant main effect of cocaine status, F(1,110) = 12.93, p = .001. Individuals in the cocaine group reported experiencing almost twice as many daily hassles (M = 25.0, SD = 24.5) than individuals in the control group (M = 14.0, SD = 19.6). No other significant differences were observed.
Perception of Daily Hassles
Cocaine-dependent individuals perceived daily hassles as being more negative (M = 1.7, SD = .6) than did controls [M = 1.2, SD = .3; F(1,139) = 27.55, p < .001]. No other significant differences were observed.
Relationship between Early Life Trauma and Frequency of Daily Hassles
The association between exposure to early life trauma and the number of daily hassles reported differed by gender, F(1,91.9) = 5.28, p = .05. For males, a positive relationship between the number of early life traumas experienced and the number of daily hassles reported was revealed. No significant relationship between these two variables was revealed for females.
Relationship between Early Life Trauma and Perception of Daily Hassles
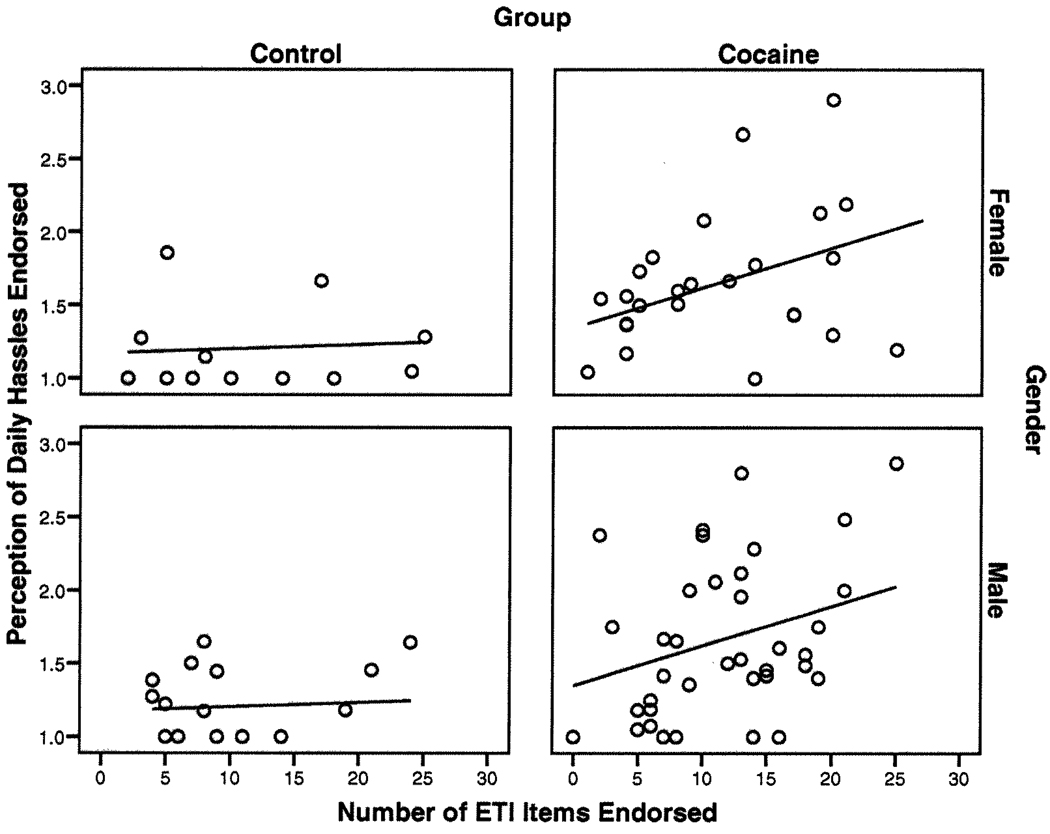
As can be seen in Figure 1, among individuals in the cocaine group, a significant relationship between the number of early traumas experienced and the perception of daily hassles reported was observed, F(1,60) = 7.94, p = .01. Thus, cocaine-dependent individuals who had a greater number of early life traumas perceived current daily hassles as more negative. In comparison, no significant relationship was revealed for the control group, F(1,28) = .18, p > .10. Finally, no gender differences were observed, F(1,59.4) = .86, p > .10.
Figure 1.
Relationship between the cumulative frequency of early life traumas (ETI) and perception of recent daily hassles among men and women with and without cocaine dependence. Among individuals in the cocaine group, a significant relationship between the number of early traumas experienced and the perception of daily hassles reported was observed, p = .01. No significant relationship was revealed for the control group.
DISCUSSION
In this study, the relationship between early life trauma and vulnerability to current daily hassles was examined among individuals with and without cocaine dependence. The findings revealed significantly higher rates of daily stressors and more negative perceptions of those stressors among individuals with, as compared to without, cocaine dependence. Cocaine-dependent individuals reported almost twice as many daily hassles as compared to controls. In addition, as the amount of early childhood trauma increased, so did the degree of sensitivity to current daily hassles among cocaine-dependent individuals. This relationship was not observed among non-cocaine-dependent participants.
Clinical and preclinical studies demonstrate that repeated early life stress leads to neurobiologic alterations, particularly in the HPA axis and corticotrophin releasing factor systems that then lead to increased responsiveness to stress (14–16). However, little research has examined the impact of early life trauma on daily experience of life events among individuals with substance use disorders (SUDs). In a recent study of 90 patients who presented frequently at their general practitioner’s office, Glaser et al. (17) used Experience Sampling Method (a diary approach) to assess the relationship between childhood trauma and emotional reactivity to daily life stress. An interaction between childhood trauma and daily stress was found, indicating that childhood trauma moderated the emotional impact of daily life events (17). SUDs, however, were excluded. The current study is the first to our knowledge to examine this phenomenon among individuals with SUDs.
Questions remain concerning the mechanisms linking childhood trauma and sensitivity to daily hassles. Regulation of negative affect via chronic substance use, which can result in alterations of the neuroendocrine stress response systems, executive brain functioning, information processing patterns, and cognitive appraisal of events (18), may help explain the stronger association of early trauma and sensitivity to current stressors observed among individuals with cocaine dependence. This is an important issue as it provides a possible behavioral mediator for the ongoing influence of early trauma on day-to-day functioning and may also be a target for treatment intervention.
Consistent with previous research, women were more likely to report exposure to severe early traumas (19, 20). Gender differences were also observed in the relationship between early life trauma and the frequency of daily hassles. Among men, there was a positive relationship between the number of early life traumas and the number of daily hassles reported. Although it is unclear why this relationship was not observed among women, the findings from a research study examining brain activation to acute stress suggests that women may use more verbal coping strategies than men do in dealing with stress (21), which may help in moderating the impact of early trauma on daily hassles. Future research with a larger sample size is needed to confirm the findings.
An unexpected finding was the similarity in reports of early life trauma among individuals with and without cocaine. The fact that PTSD was an exclusion criterion is likely to have influenced these results. Both female gender and cocaine dependence are associated with risk for PTSD (22). As such, it is likely that many cocaine-dependent individuals with trauma histories, and in particular women, were excluded because they had PTSD, so the group included in the study may “under represent” childhood trauma in cocaine-dependent individuals.
Limitations
The sample size was small, which limits generalizability and statistical power. Self-report measures were used and are subject to bias. Because this study was not designed specifically to examine the relationship between early life trauma and daily hassles, the results are preliminary in nature.
Conclusions
In summary, the findings extend previous research by examining the influence of exposure to early life trauma on sensitivity to current daily hassles among individuals with SUDs. Early life trauma appears to place cocaine-dependent individuals at risk of a) increased frequency of current daily hassles and b) negatively perceiving such hassles. As both trauma and negative affect may increase risk of relapse, routine screening of trauma history and daily hassles among cocaine-dependent individuals is warranted. Further investigation is needed to help elucidate why and how exposure to early life trauma places some individuals at greater risk of experiencing and being negatively affected by current daily hassles.
ACKNOWLEDGMENTS
Supported by National Institute on Drug Abuse grants P50 AR049551 and K25 DA00435 awarded to Dr. Kathleen Brady.
REFERENCES
- 1.Kikusui T, Faccidomo S, Miczek KA. Repeated maternal separation: Differences in cocaine-induced behavioral sensitization in adult male and female mice. Psychopharmacology. 2005;178(2–3):202–210. doi: 10.1007/s00213-004-1989-1. [DOI] [PubMed] [Google Scholar]
- 2.Levine S. Developmental determinants of sensitivity and resistance to stress. Psychoneuroendocrinology. 2005;30(10):939–946. doi: 10.1016/j.psyneuen.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Lynch WJ, Mangini LD, Taylor JR. Neonatal isolation stress potentiates cocaine seeking behavior in adult male and female rats. Neuropsychopharmacology. 2005;30:322–329. doi: 10.1038/sj.npp.1300594. [DOI] [PubMed] [Google Scholar]
- 4.Rounsaville BJ, Weissman MM, Wilber CH, Kleber HD. Pathways to opiate addiction: an evaluation of differing antecedents. Br J Psychiatry. 1982;141:437–446. doi: 10.1192/bjp.141.5.437. [DOI] [PubMed] [Google Scholar]
- 5.Seeman M, Seeman AZ. Life strains, alienation, and drinking behavior. Alcohol Clin Exp Res. 1992;16(2):199–205. doi: 10.1111/j.1530-0277.1992.tb01364.x. [DOI] [PubMed] [Google Scholar]
- 6.Tate SR, McQuaid JR, Brown SA. Characteristics of life stressors predictive of substance treatment outcomes. J Subst Abuse Treat. 2005;29(2):107–115. doi: 10.1016/j.jsat.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry. 1998;55(3):259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- 8.Miller WR, Westerberg VS, Harris RJ, Tonigan JS. What predicts relapse? Prospective testing of antecedent models. Addiction. 1996;91 Suppl:155–172. [PubMed] [Google Scholar]
- 9.Waldrop AE, Back SE, Brady KT, Upadhyaya HP, McRae AL, Saladin SE. Daily stressor sensitivity, abuse effects, and cocaine use in cocaine dependence. Addictive Behaviors. doi: 10.1016/j.addbeh.2007.07.006. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders-Research Version. New York, NY: New York State Psychiatric Institute, Biometrics Research Department; 2001. [Google Scholar]
- 11.Bremner JD, Vermetten E, Mazure CM. Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: The Early Trauma Inventory. Depress Anxiety. 2000;12(1):1–12. doi: 10.1002/1520-6394(2000)12:1<1::AID-DA1>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 12.Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. J Behav Med. l981;4(1):1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- 13.Brown H, Prescott R. Applied Mixed Models in Medicine. Chichester: John Wiley and Sons; 1999. [Google Scholar]
- 14.Heim C, Newport J, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- 15.Nemeroff CB. Neurobiological consequences of childhood trauma. J Clin Psychiatry. 2004;65 Suppl 1:18–28. [PubMed] [Google Scholar]
- 16.Penza KM, Heim C, Nemeroff CB. Trauma and depression. In: Keyes C, Goodman S, editors. Women and depression: A handbook for the social, behavioral, and biomedical sciences. New York, NY: Cambridge University Press; 2006. pp. 360–381. [Google Scholar]
- 17.Glaser JP, van Os J, Portegijs PJM, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J Psychosomatic Res. 2006;61:229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 18.Olff M, Langeland W, Gersons BP. The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology. 2005;30(10):974–982. doi: 10.1016/j.psyneuen.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 19.Putnam F. Ten-year research update review: Child sexual abuse. J Am Acad Child Adolesc Psychiatry. 2003;42(3):269–278. doi: 10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Nelson EC, Heath AC, Madden PA. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Arch Gen Psychiatry. 2002;59(2):139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- 21.Li CS, Kosten TR, Sinha R. Antisocial personality and stress-induced brain activation in cocaine-dependent patients. Neuroreport. 2006;17(3):243–247. doi: 10.1097/01.wnr.0000199471.06487.a2. [DOI] [PubMed] [Google Scholar]
- 22.Cottler LB, Compton WM, Mager D, Spitznagel EL, Janca A. Posttraumatic stress disorder among substance users from the general population. Am J Psychiatry. 1992;149(5):664–670. doi: 10.1176/ajp.149.5.664. [DOI] [PubMed] [Google Scholar]