Abstract
Traumatic brain injury (TBI) results in a cerebral metabolic crisis that contributes to poor neurologic outcome. The aim of this study was to characterized changes in oxidative glucose metabolism in early periods after injury in the brains of immature animals. At 5 hours after controlled cortical impact TBI or sham surgery to the left cortex, 21-22 day old rats were injected intraperitoneally with [1,6-13C]glucose and brains removed 15 min, 30 min and 60 min later and studied by ex vivo 13C-NMR spectroscopy. Oxidative metabolism, determined by incorporation of 13C into glutamate, glutamine and GABA over 15 to 60 min, was significantly delayed in both hemispheres of brain from TBI rats. The most striking delay was in labeling of the C4 position of glutamate from neuronal metabolism of glucose in injured, ipsilateral hemisphere which peaked at 60 min, compared to the contralateral and sham-operated brains, where metabolism peaked at 30 and 15 min, respectively. Our findings indicate that 1) neuronal specific oxidative metabolism of glucose at 5-6h after TBI is delayed in both injured and contralateral sides compared to sham brain; 2) labeling from metabolism of glucose via the pyruvate carboxylase pathway in astrocytes was also initially delayed in both sides of TBI brain compared to sham brain; 3) despite this delayed incorporation, at 6 hours after TBI, both sides of brain showed apparent increased neuronal and glial metabolism, reflecting accumulation of labeled metabolites, suggesting impaired malate aspartate shuttle activity. The presence of delayed metabolism, followed by accumulation of labeled compounds is evidence of severe alterations in homeostasis that could impair mitochondrial metabolism in both ipsilateral and contralateral sides of brain after TBI. However, ongoing oxidative metabolism in mitochondria in injured brain suggests that there is a window of opportunity for therapeutic intervention up to at least 6 hrs after injury.
Keywords: traumatic brain injury, immature brain, glucose, metabolism, 13C NMR spectroscopy, PDHC, PC, glutamate, GABA
Introduction
Traumatic brain injury (TBI) is the leading cause of morbidity and mortality in children (Keenan and Bratton 2006). TBI is characterized by depressed cerebral metabolism, which is attributed to mitochondrial dysfunction induced by increased production of reactive oxygen species (ROS) after trauma, alterations in intracellular calcium homeostasis and dissipation of transmembrane potential (Fiskum 2000; Verweij et al. 2007). Numerous adult animal and human investigations demonstrated that the decreased oxidative metabolism is non-ischemic, suggesting that it is due to mitochondrial alterations per se, and not solely a result of lack of oxygen and glucose supply due to decreased cerebral perfusion pressure to the injured tissue (Xiong et al. 1998; Soustiel and Sviri 2007; Marcoux et al. 2008). A decrease in oxidative metabolism after TBI results in shift to anaerobic metabolism, tissue lactate accumulation, decreased pH and further mitochondrial impairment.
Mitochondria are important for energy production, maintaining redox state in brain, detoxification of ROS and intracellular calcium homeostasis (Robertson et al. 2006a). Production of glutamate and γ-amino butyric acid (GABA), the major excitatory and inhibitory neurotransmitters in brain, respectively, involves oxidative metabolism via the tricarboxylic acid (TCA) cycle in neurons (Waagepetersen et al. 2000). Mitochondrial metabolism is finely tuned to fluctuations in the concentrations of key metabolites in the intra- and extracellular milieu under normal conditions (McKenna 2007). However, following TBI mitochondria are injured and many of these normal functions are disrupted (Robertson et al. 2006a; Opii et al. 2007; Robertson et al. 2007; Casey et al. 2008).
Using 13C NMR spectroscopy Bartnik et al. (Bartnik et al. 2005) reported significant increases in brain lactate and glutamine production as early as 3.5 h after TBI in immobilized adult rats. . Investigations on the effects of TBI on energy metabolism of the immature brain are limited, despite the prevalence of TBI in children. Nevertheless, brain mitochondrial respiration and pyruvate dehydrogenase complex activity levels are reduced within 4 hr after TBI in immature rats (Robertson et al. 2007). A recent 1H-NMR study reported increased lactate at 4 hr, and decreased N-acetylaspartate at 24 hr and 7 days after TBI providing further evidence of mitochondrial dysfunction after TBI in immature brain (Casey et al. 2008).
The aim of this study was to determine glycolytic and oxidative glucose metabolism and neurotransmitter synthesis using 13C NMR spectroscopy to further clarify the alterations in immature brain 5-6 hours after TBI.
Materials and Methods
Animals
This study was approved by the University of Maryland, Baltimore, Animal Care and Use Committee; all care and handling of rats were in compliance with the National Institutes of Health guidelines. Immature (postnatal day (PND) 21-22), male Sprague-Dawley rats (Charles River Laboratories, Wilmington, MA, USA) were used in all studies. The animals were weaned away from the dam on PND 19 and housed with littermates before surgery and after recovery from anesthesia.
TBI model
The injury paradigm for immature rats was previously described by Robertson et al. (Robertson et al. 2007). Anesthesia was induced in a plexiglass chamber with 4% isoflurane. The head was fixed in a stereotactic device and isoflurane (2-2.5%) with oxygen (30%) was administered via a nose cone for the duration of surgery. Rectal temperature was maintained at 37.0 ± 0.5°C. A midline scalp incision was made, and a left parietal craniotomy performed. Traumatic brain injury was performed using the controlled cortical impact (CCI) device (Pittsburgh Precision Instruments, Pittsburgh, PA, USA) as previously described (Dixon et al. 1991; Robertson et al. 2006b). CCI injury was produced with a 6-mm metal impactor tip with a 1.5 mm depth of penetration, 5.5 ± 0.3 m/s velocity, and 50 ms duration of deformation. Following injury, the bone flap was replaced, craniotomy sealed, and the scalp incision closed with sutures. Isoflurane was discontinued and, after regaining consciousness, the rats were returned to their cages with littermates. Sham rats had identical surgeries, without CCI injury. Rats were not randomized, but treatment (TBI and sham) was alternated between rats on each day of study.
At 5 hours following surgery rats were given i.p. injections of [1,6-13C]glucose (200mg/kg; 99% 13C enriched, Cambridge Isotope Laboratories, Woburn, MA, USA). Rats were euthanized by decapitation 15min, 30min and 60min after injection. Brains were rapidly dissected into injured (left, ipsi) and contralateral (right, contra) sides (cortex, including the immediate subcortical structures, i.e. hippocampus, thalamus, hypothalamus, parietal and motor areas) and snap-frozen in liquid nitrogen. The time from decapitation to freezing brain was <40 sec, and the order of freezing left and right sides of brain was alternated to avoid any bias from freezing time. All samples were stored at -80°C until extraction.
Tissue extraction
Each frozen tissue sample was homogenized in 2 ml ice-cold 7% perchloric acid (PCA), and processed as described by Richards et al. (Richards et al. 2007). The neutralized, lyophilized extracts were stored at -20°C.
NMR spectroscopy
Lyophilized samples were reconstituted in deuterium oxide (D2O) with 0.4% dioxane added as an internal standard for quantification, adjusted to pH 6.8-7.0. Proton-decoupled 125.5-MHz 13C NMR spectra were obtained at the NMR Center, University of Maryland Baltimore, on a Varian Inova 500 MHz spectrometer with a broad band detection probe. Spectra were acquired at 25°C using a 35° pulse angle, 25 KHz spectra width, and 64K data points. Acquisition time and relaxation times were 1.3s and 4.3s, respectively. The number of scans was typically 11,000-13,000. Spectra were corrected for nuclear Overhauser effects (Richards et al. 2007). A line broadening of 5 Hz was used. Chemical shifts are reported relative to the dioxane peak at 67.4 ppm, and peak assignments were made by comparison spectra from 13C standards and literature values.
Protein and amino acid quantification
The protein content of the pellets from the PCA extracts of the brains was determined using the Pierce BCA microreagent assay (Smith et al. 1985). Amino acids were determined by HPLC (Richards et al. 2007).
Statistical analyses
Data are expressed as mean ± SEM for n= 5 for the15 and 30 min post-injection groups, and n=7 for the 60 min group. Data were analyzed by one-way ANOVA with p<0.05 as the level of significance, using SigmaStat software.
Labeling from metabolism of [1,6-13C]glucose in brain
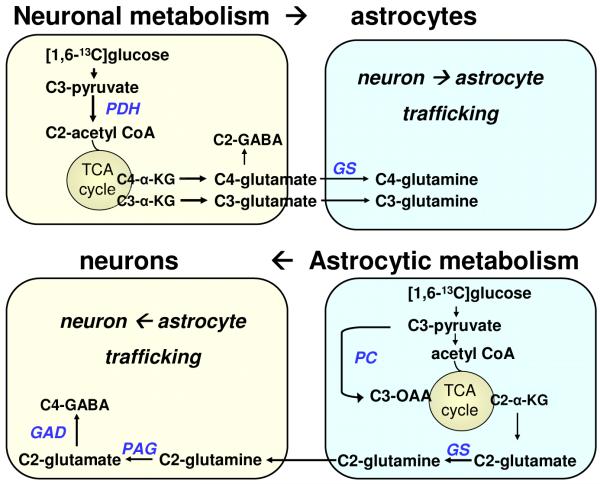
The labeling pattern of brain metabolites after infusion of [1,6-13C]glucose is the same as [1-13C]glucose, which has been documented in many studies (Haberg et al. 2001) (Figure 1). [1,6-13C]glucose enters glycolysis forming [3-13C]pyruvate, which can be converted to [3-13C]lactate or be metabolized via the TCA cycle, giving rise [4-13C]α-ketoglutarate in the first turn, which is converted to [4-13C]glutamate (GLU C4) in neurons and the corresponding [4-13C]glutamine (GLN C4) in astrocytes. GLN C3 and GLU C3 are formed in the next turn of the cycle, and due to randomization of the label in the symmetrical fumarate step some labeling in GLU C2 and GLN C2 also occurs. GLU C4 can be converted directly to [2-13C]GABA (GABA C2) in neurons. [3-13C]Oxaloacetate formed in the first turn of the TCA cycle can be converted to [3-13C]aspartate (ASP C3).
Figure 1.
Labeling and neuronal glial interactions from metabolism of [1,6-13C]glucose in rat brain. Details of the labeling are given in methods section. Abbreviations PDH, pyruvate dehydrogenase complex; PC, pyruvate carboxylase; GS, glutamine synthetase; PAG, phosphate activated glutaminase.
In astrocytes glucose metabolism occurs primarily via pyruvate carboxylase (PC) leading to formation of GLU C2 and GLN C2 in astrocytes. Labeling in GLU C3 can also occur in from PC in astrocytes due to the subsequent equilibration of oxaloacetate with fumarate (Hassel et al. 1995). Via the activity of phosphate activated glutaminase (PAG), GLU C2 can be synthesized in neurons from astrocytic GLN C2. These precursors can be converted to GABA C4 in neurons. Labeling in GABA C3 reflects both neuronal metabolism of GLU C3 as well as extensive metabolism of the glial derived precursors.
Cycling ratios, which show the relative amount of labeling from the second turn/first turn of the TCA cycle, were calculated for glutamate glutamine and GABA using the amount in GLU C3/GLU C4, GLN C3/GLN C4 and GABA C3/GABA C2 (Qu et al. 2003).
Results
Swelling of tissue from the ipsi side of TBI brain was apparent at 5- 6 hr after injury. Hematomas were not usually seen. Incorporation of label from the metabolism of [1,6-13C]glucose into metabolites in the ipsilateral (ipsi) and contra sides of brain of TBI rats was compared at 15, 30 and 60 minutes after injection of the labeled 13C-precursor to determine the extent and pathways of glucose metabolism. These time points corresponded to 5hr 15min, 5hr 30min and 6hrs after the TBI injury. Since sham operated controls underwent craniotomy and skull closure in the ipsi side, metabolism was determined separately in both sides of brains from sham-operated rats.
Incorporation of 13C into lactate after TBI
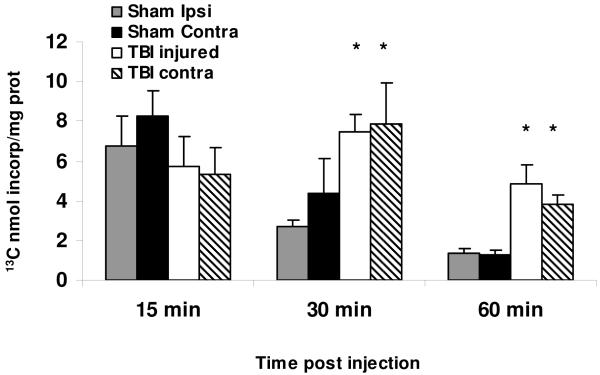
At 15min after i.p. injection of [1,6-13C]glucose the concentration of unmetabolized brain glucose, and incorporation of label into LAC C3 was not different in TBI and sham rats suggesting that glucose delivery to the brain 5h 15 min post injury was essentially preserved (Figure 2). Initial labeling of LAC C3 was comparable to values of 5.95 ± 0.47 reported for adult rat brain (Hassel et al. 1995; Qu et al. 2003). There was a significantly increased labeling of LAC C3 in both ipsi and contra sides of TBI rats at 30 min and 60 min (p<0.05) compared to shams.
Figure 2.
Delayed increase in formation [3-13C]lactate (Lac C3) in ipsi and contra sides of brain from young TBI rats at 15, 30 and 60 min after i.p. injection of [1,6-13C]glucose. These time points represent 5h 15 min, 5h 30 min, and 6hr after the TBI injury. Spectra we obtained on PCA extracts of brain as described in methods. Values are mean ± S.E. of data for nmol 13C incorporated/mg protein, from 6 TBI and 5 sham rats at each time point. Data were analyzed using one-way ANOVA. *p<0.05 significant difference between ipsi and contra sides of TBI and sham brain as indicated the horizontal lines over the bars.
Incorporation of 13C into metabolites in 21-22 day old rat brain
In sham rat brain label from metabolism of [1,6-13C]glucose was incorporated into glutamate, glutamine, GABA, aspartate and lactate. Incorporation of label in sham brain was highest at 15 min post-injection, consistent with reports that metabolism of 13C-glucose in brain peaks at 15 min after injection of the precursor in adult mice and rats (Hassel and Sonnewald 1995). The incorporation of label into GLU C4 and GLN C4 in the contra side of sham rat brain (essentially normal side; Fig 3A and Fig 3B) was comparable to values reported for GLU C4, (4.88 (calculated from concentration and percent enrichment) and 4.18), and GLN C4 (0.99 and 1.0) in normal mouse and rat brain (Hassel et al. 1995; Qu et al. 2003). In the contra side of brain of sham rats labeling of GLU C 3 was comparable to that of GLU C4 at 15 and 30 min. This is in contrast to reports of higher labeling in GLU C4 than GLU C3 in adult mouse and rat brain (Hassel et al. 1995; Qu et al. 2003). Labeling of GLU C2 and GLN C2 (Fig 4) via the PC pathway in astrocytes was higher in immature brain than values reported for adult brain (GLU C2, 2.96; GLN C2, 0.7 recalculated from (Hassel et al. 1995; Qu et al. 2003)). Indeed, the high labeling in GLU C3 noted above may also reflect increased formation from the PC pathway. Incorporation of label from glucose metabolism into GABA C2 was also comparable to values of 1.04 and 0.85 for adult mouse and rat brain, respectively (Hassel et al. 1995; Qu et al. 2003). Consistent with adult brain, labeling was higher in GABA C2> GABA C4>GABA C3 (Figs. 3C and Fig 4).
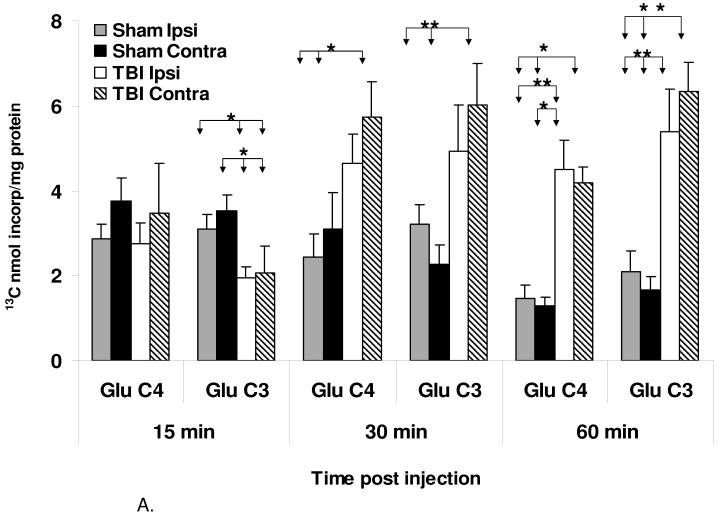
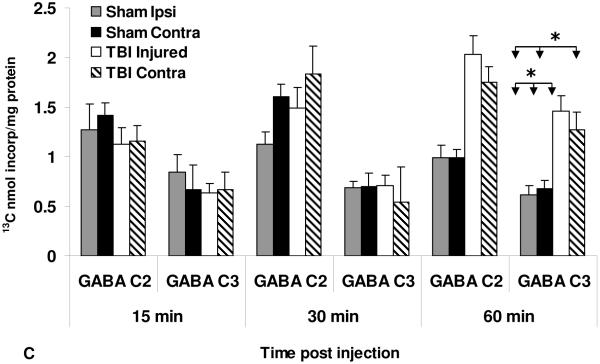
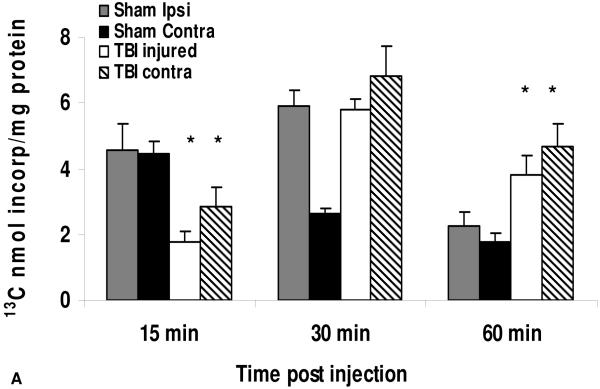
Figure 3.
Delayed increase in labeling of (A) [4-13C]glutamate(GLU C4) and [3-13C]glutamate (GLU C3), (B) [4-13C]glutamine (GLN C4) and [3-13C]glutamine (GLN C3) and [2-13C]GABA (GABA C2) and (C) [3-13C]GABA (GABA C3) in ipsi and contra sides of the brain from young TBI rats at 15, 30 and 60 min after i.p. injection of [1,6-13C]glucose. These time points represent 5h15min, 5h30min and 6h post TBI injury. Values are mean ± S.E. of data for nmol 13C incorporated/mg protein from 6 TBI and 5 sham rats at each time points. Data were analyzed using one-way ANOVA. *p<0.05 significant difference between ipsi and contra sides of TBI and sham brain as indicated the horizontal lines over the bars.
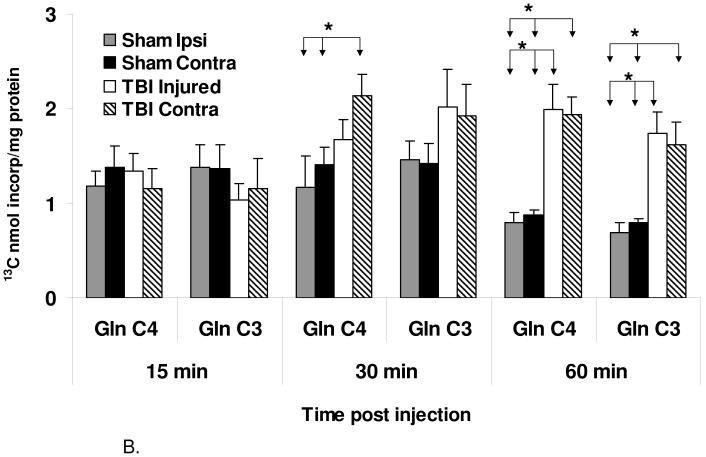
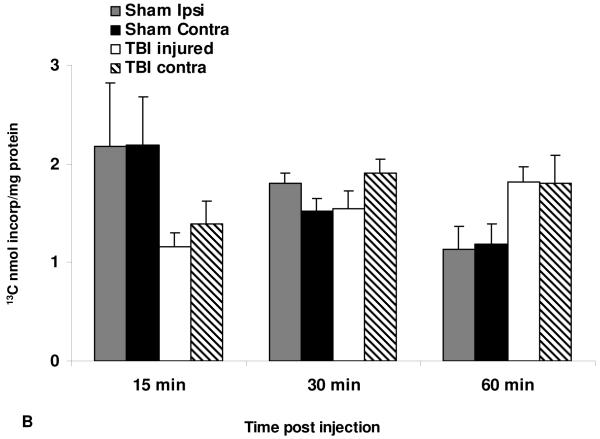
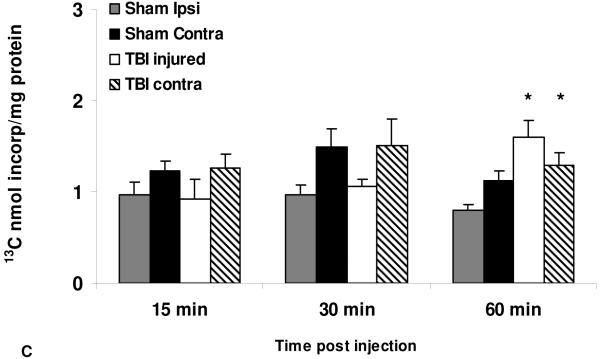
Figure 4.
Formation of [2-13C]glutamate (GLU C2) and [2-13C]glutamine (GLN C2) via the anaplerotic pyruvate carboxylase pathway, and [4-13C]GABA (GABA C4) formed from these metabolites, in ipsi and contra sides of the brain from young TBI rats at 15, 30 and 60 min after i.p. injection of [1,6-13C]glucose. These time points represent 5h15 min, 5h 30 min and 6h post TBI injury. Values are mean ± S.E. of data for nmol 13C incorporated/mg protein from 6 TBI and 5 sham rats at each time points. Data were analyzed using one-way ANOVA. *p<0.05 significant difference between ipsi and contra sides of TBI and sham brain as indicated the horizontal lines over the bars.
Incorporation of 13C into GLU and GLN in brain after TBI
At 15 min after injection there was no difference in labeling of GLU C4 in the ipsi and contra sides of brain from TBI rats and sham operated controls as shown in Figure 3A. However, labeling of GLU C3 was significantly decreased (p <0.05) in both ipsi and contra sides of brain from TBI rats. The significantly decreased cycling ratio (p < 0.03, supplemental Table 1) for GLU at 15 min indicated decreased TCA cycle activity in ipsi side of TBI brain. At 30 min labeling of GLU C4 and C3 was significantly higher in both sides from TBI brain compared to shams. At 60 min (6 hr after TBI) labeling of GLU C4 and C3 was increased more than 2-fold in both sides of TBI brain compared to shams.
In sham and TBI rat brain 15 min after injection of [1,6-13C]glucose there were no differences in labeling of GLN C4 and GLN C3, which are formed from the GLU C4 and GLU C3 synthesized in neurons, (Figure 3B). At 30 min labeling of GLN C4 was significantly increased only in the contra side, and there was a trend towards an increase in GLN C3 in both sides of TBI rat brain. At 60 min, labeling of GLN C4 and GLN C3 was increased more than 2-fold in both ipsi and contra sides of TBI brain compared to shams, in parallel with the increase in labeling of the precursors GLU C4 and GLU C3 formed in neurons.
Incorporation of 13C into GABA after TBI
At 15 min and 30 min after injection of [1,6-13C]glucose there were no significant differences in labeling of GABA C2, which is formed directly from the GLU C4 derived from metabolism of glucose in neurons (Figure 3C). However, at 60 min (6 hr after TBI), there was significantly more labeling of GABA C2 in both ipsi and contra sides in TBI rats compared to shams, that paralleled the increased GLU C4. GABA C3 reflects labeling from both neuronally derived (GLU C3, GLN C3) and astrocytic precursors (GLU C2, GLN C2). At 15 and 30 min, labeling of GABA C3 was not different from shams; however, at 60 min there was significantly (p<0.05) increased GABA C3 in both sides of brain from TBI rats.
Alterations in metabolism via the pyruvate carboxylase pathway
At 15 min and 30 min after injection of [1,6-13C]glucose there was a tendency towards decreased GLN C2 formed from metabolism of glucose via the pyruvate carboxylase (PC) pathway in astrocytes (Figure 4). The corresponding GLU C2 formed from GLN C2 was significantly decreased at 15 min. At 60 min labeling of GLU C2 was significantly increased in both ipsi and contra side of TBI brains compared to shams. At 60 min, in ipsi TBI brain there was significantly increased GABA C4 (Figure 4C), that is derived from the GLU C2 and GLN C2 formed via PC in astrocytes.
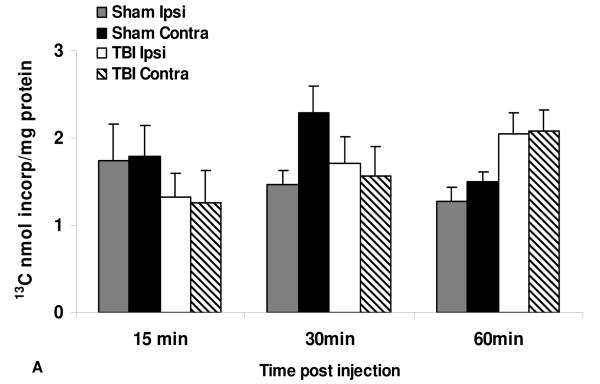
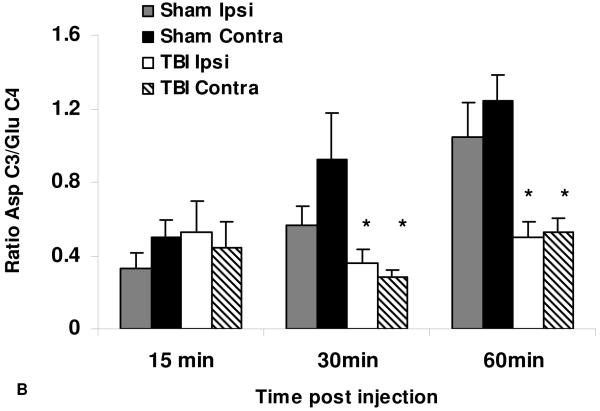
Incorporation of 13C into Aspartate
There was no significant difference in labeling of ASP C3 formed primarily from metabolism via the first turn of the TCA cycle in neurons (Figure 5A). However, the ratio of ASP C3/GLU C4 was significantly decreased (p<0.05) at 30 and 60 min in both ipsi and contra sides of TBI brain compared to shams (Figure 5B).
Figure 5.
TBI leads to decrease of Asp C3/GLU C4 in both ipsi and contra hemispheres of TBI rats. (A) There was no significant differences in 13C incorporation into [3-13C]aspartate (ASP C3) between ipsi and contra sides of the brain from young TBI rats at 15, 30 and 60 min after i.p. injection of [1,6-13C]glucose. These time points represent 5h 15 min, 5h 30 min and 6 h post TBI injury. Values are mean ± S.E. of data for nmol 13C incorporated/mg protein from 6 TBI and 5 sham rats at each time points. Data were analyzed using one-way ANOVA. (B) Ratio of Asp C3/GLU C4 decreased at 30 and 60min post injection. Values are mean ± S.E. of data from 6 TBI and 5 sham rats at each time points. Data were analyzed using one-way ANOVA. *p<0.05 significant difference between ipsi and contra sides of TBI and sham brain as indicated the horizontal lines over the bars.
Discussion
This is, to our knowledge, the first study that determined oxidative glucose metabolism in immature brain following TBI. Multiple animal and clinical studies have provided evidence of decreased oxidative metabolism accompanied by rise in lactate following TBI in adults (Siesjo 1984; Schroder et al. 1996). In those studies the decreased oxidative metabolism was attributed to hypotension after the brain injury and decreased oxygen and glucose supply. However, in immature brain the hypoperfusion state is short lived and rapidly converts to prolonged hyperemia (Biagas et al. 1996). The results of the present study showing comparable levels of unmetabolized glucose and labeling in LAC C3 and GLU C4 in the ipsi and contra sides of TBI brain and shams at 15 min post injection suggests that there was adequate blood supply 5-6 hr after moderate TBI in young rats.
A number of animal and clinical studies have implicated glutamate excitotoxicity in the pathophysiology of TBI (Bullock et al. 1998; Zhong et al. 2006). Although these studies using brain microdialysis probes demonstrated a surge in glutamate in the interstitial fluid within the first hours after TBI, the mechanism of this rise in glutamate is not completely clear. Up to 20-fold increase in glutamate and smaller alterations in aspartate within 15-30min after TBI have been reported (Zhong et al. 2006). Cerebral ischemia, which can occur as a secondary injury following TBI, is also associated with glutamate rise and accompanying mitochondrial impairment (Globus et al. 1995; Takeuchi et al. 2008); however, the mechanisms underlying these changes are not fully understood. During energy failure glutamate can be released from neurons or from astrocytes by vesicular release or reversal of transporters (Montana et al. 2004; Haydon and Carmignoto 2006). Although we found no difference in total brain glutamate concentration at any of the time points after TBI (supplemental Figure 6), measurements of total amount in brain extracts cannot distinguish between intra- and extracellular glutamate. However, results of the present study showed an initial decrease in labeling of GLU C3, and decreased GLU cycling ratio, both of which are consistent with impaired oxidative metabolism. Our findings are consistent with Robertson et al. (Robertson et al. 2007) who found a lower ispi/contra ratio of PDHC activity 4 hr after TBI in immature rat brain compared to shams. They also reported elevated state 4 mitochondrial respiration rates and uncoupling of respiration indicating a loss of mitochondrial integrity at 1 hr after TBI. Impairment of PDHC after TBI in immature rats may be prolonged for weeks (Kochanek et al. 2006). The decreased formation of GLU C2 in the present study is evidence of impaired astrocyte mitochondrial function. Several other recent studies attribute the metabolic changes in adult TBI to altered mitochondrial function (Lifshitz et al. 2003; Opii et al. 2007; Pandya et al. 2007). Since the results of Robertson et al. (Robertson et al. 2007) were obtained with the same immature TBI model used in the present study, it is likely that mitochondrial dysfunction is responsible for the observed delayed glucose metabolism.
Although labeling of ASP C3 was not changed, the increased incorporation of 13C into GLU C4 led to a significantly decreased ratio of ASP C3/GLU C4 at 30 and 60min after glucose injection (5 ½ h and 6 hr after TBI). Aspartate is formed from the TCA cycle intermediate oxaloacetate, and labeling in ASP C3 reflects primarily formation from neuronal metabolism (Oz et al. 2004). The decreased ASP/GLU ratio could be due, in part, to decreased activity of α-ketoglutarate dehydrogenase, an enzyme that is subject to damage by oxidative stress (Starkov et al. 2004). Intramitochondrial aspartate has a key role in the malate-aspartate shuttle, the most important mechanism for transferring reducing equivalents from the cytosol to the mitochondria in brain (McKenna et al. 2006). Oxidative metabolism of glutamate requires entry into the mitochondria via the aspartate-glutamate carrier (AGC), which occurs as an electrogenic exchange with intramitochondrial aspartate (McKenna et al. 2006; McKenna 2007; Satrustegui et al. 2007; Xu et al. 2007). Thus, an imbalance in ASP/GLU could limit entry of glutamate into mitochondria and subsequent conversion to α-ketoglutarate. The apparent hypermetabolism and increased GLU C4 and GLU C3 at 30 and 60 min in the present study may reflect, in part, accumulation of glutamate subsequent to impaired entry into mitochondria and/or subsequent oxidative metabolism that would normally provide energy when entry of pyruvate into the TCA cycle is impaired (McKenna et al. 2006; McKenna 2007).
Astrocytes have a number of crucial roles in brain including uptake and disposal of glutamate from the synaptic cleft, maintaining the pH and appropriate concentrations of K+ and other ions in the interstitial milieu and providing neurons with energy substrates. Metabolism of glucose via the anaplerotic PC pathway in astrocytes fulfills the crucial role of carboxylating pyruvate to form oxaloacetate, thereby adding net carbons to the astrocytic TCA cycle. This serves to ultimately replenish the neuronal TCA cycle which is continuously depleted by synthesis of neurotransmitters (Oz et al. 2004). Thus glutamine labeled in C2 position from metabolism via PC in astrocytes, is released, taken up by neurons and used as a substrate for synthesis of glutamate C2 and GABA C4, and replenishing neuronal TCA cycle intermediates. Metabolism via PC is important in developing brain and hypomyelination and lactic acidosis are found in clinical PC deficiency (Higgins et al. 1994). Data from the present study show an initial decrease in labeling of GLU C2, followed by increased labeling at 5 ½ - 6 hr after TBI in young rats. The significantly decreased GLU C2 may reflect energy impairment in astrocytes since label can be ‘trapped’ in GLU C2 if there is insufficient ATP for glutamine formation via glutamine synthetase in astrocytes. Since synthesis of GLN and GLU via the PC pathway in astrocytes provides important substrates for replenishing the neuronal TCA cycle, even transient impairment of this process and the associated glial → neuronal trafficking could lead to ongoing alterations in metabolism after TBI in developing brain.
Our findings differ to a large extent with those reported by Bartnik et al. (Bartnik et al. 2005) who showed that 3.5h and 24h after CCI TBI in adult rats, entry of [1,2-13C]glucose into the TCA cycle was not inhibited and oxidative metabolism in glutamatergic neurons was maintained. The same investigators reported that labeling of GLU C3 and GLU C2 (via PC) were not altered, indicating intact function of the TCA cycle in both injured and contralateral mitochondria in adult rats brain at 3.5h and 24h after TBI. In contrast, the results of the present study showed that 5-6 hours post TBI there were profound alterations in both ipsi and contra sides of brain, with an initial decrease, and subsequently apparent increased glucose metabolism in neurons and via the PC pathway in astrocytes. There are several explanations for the differences between the present study and those reported in adult brain (Bartnik et al. 2005). First, in the present study metabolism was determined in immature brain between 5h 15min and 6h after TBI injury. Clinically, the first 6h after severe pediatric TBI may represent a critical window for improving the outcome (Samant et al. 2008). Robertson at al. (Robertson et al. 2007), demonstrated that young animals have abnormal mitochondrial function early (< 4h), thus it is important to determine oxidative metabolism that occurs via the TCA cycle after these early abnormal states of the mitochondria. Second, while direct evidence for alterations in mitochondrial energy metabolism after TBI in the developing brain is limited, pre-clinical investigations showed that alterations in cerebral glucose metabolism are characterized by early (first 30 min) increased cerebral metabolic rates and secondary metabolic depression 1-3 days after TBI (Thomas et al. 2000). The pattern of alterations in developing brain is different from adult rats, which show an acute increase in cerebral glucose metabolism for hours (Yoshino et al. 1991), followed by a subsequent metabolic depression and decreased cytochrome oxidase activity for 10 days after injury (Hovda et al. 1991). The increased labeling of GLN reported 3.5 h after injury by Bartnik et al. (Bartnik et al. 2005) is consistent with the hypermetabolism reported by Hovda et al. (Hovda et al. 1991) and suggests intact, overactive glial metabolism early after injury in adult brain. In contrast, results from the present study show that the metabolic alterations in immature brain differ from those in adult brain, particularly with respect to the impaired glutamine formation and metabolism via PC in astrocytes. The decreased labeling of GLU C3 and GLU C2 at 15 min after glucose administration demonstrates that significantly decreased neuronal and glial metabolism occurs early after TBI in young rats, followed by an apparent hypermetabolism in both neuronal and glial pathways at 5 ½ to 6 h after injury. However, an important conclusion drawn from the present study is that 5-6 hours after moderate-severe TBI in young rats there is still considerable metabolism of glucose via the TCA cycle in brain. Our results suggest that the altered metabolism is due to a combination of early impairment in the TCA cycle, specifically at the level of PDHC and possibly at α-ketoglutarate dehydrogenase, coupled with impairment of malate-aspartate shuttle activity and utilization of glutamate and glutamine that leads to accumulation of labeled metabolites. The temporal duration of these metabolic alterations in immature brain needs to be studied further. It is important to note that any long lasting metabolic alterations superimposed on the intense biosynthetic requirements of the developing brain could contribute significantly to poor outcome.
Overall, the present studies show that severe alterations in cerebral metabolism occur from 5-6 h after TBI in immature brain. 13C-NMR spectroscopy is a valuable tool for determining the extent of metabolic changes as well as for identifying the specific pathways altered in neuronal and glial metabolism. Further experiments determining the specific alterations in key enzymes after TBI are warranted and may lead to development of new targeted therapeutic interventions to improve both neuronal and glial cerebral oxidative metabolism after pediatric TBI.
Supplementary Material
References
- Bartnik BL, Sutton RL, Fukushima M, Harris NG, Hovda DA, Lee SM. Upregulation of pentose phosphate pathway and preservation of tricarboxylic acid cycle flux after experimental brain injury. J Neurotrauma. 2005;22:1052–1065. doi: 10.1089/neu.2005.22.1052. [DOI] [PubMed] [Google Scholar]
- Biagas KV, Grundl PD, Kochanek PM, Schiding JK, Nemoto EM. Posttraumatic hyperemia in immature, mature, and aged rats: autoradiographic determination of cerebral blood flow. J Neurotrauma. 1996;13:189–200. doi: 10.1089/neu.1996.13.189. [DOI] [PubMed] [Google Scholar]
- Bullock R, Zauner A, Woodward JJ, Myseros J, Choi SC, Ward JD, Marmarou A, Young HF. Factors affecting excitatory amino acid release following severe human head injury. J Neurosurg. 1998;89:507–518. doi: 10.3171/jns.1998.89.4.0507. [DOI] [PubMed] [Google Scholar]
- Casey PA, McKenna MC, Fiskum G, Saraswati M, Robertson CL. Early and sustained alterations in cerebral metabolism after traumatic brain injury in immature rats. J Neurotrauma. 2008;25:603–614. doi: 10.1089/neu.2007.0481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon CE, Clifton GL, Lighthall JW, Yaghmai AA, Hayes RL. A controlled cortical impact model of traumatic brain injury in the rat. J Neurosci Methods. 1991;39:253–262. doi: 10.1016/0165-0270(91)90104-8. [DOI] [PubMed] [Google Scholar]
- Fiskum G. Mitochondrial participation in ischemic and traumatic neural cell death. J Neurotrauma. 2000;17:843–855. doi: 10.1089/neu.2000.17.843. [DOI] [PubMed] [Google Scholar]
- Globus MY, Alonso O, Dietrich WD, Busto R, Ginsberg MD. Glutamate release and free radical production following brain injury: effects of posttraumatic hypothermia. J Neurochem. 1995;65:1704–1711. doi: 10.1046/j.1471-4159.1995.65041704.x. [DOI] [PubMed] [Google Scholar]
- Haberg A, Qu H, Saether O, Unsgard G, Haraldseth O, Sonnewald U. Differences in neurotransmitter synthesis and intermediary metabolism between glutamatergic and GABAergic neurons during 4 hours of middle cerebral artery occlusion in the rat: the role of astrocytes in neuronal survival. J Cereb Blood Flow Metab. 2001;21:1451–1463. doi: 10.1097/00004647-200112000-00010. [DOI] [PubMed] [Google Scholar]
- Hassel B, Sonnewald U. Glial formation of pyruvate and lactate from TCA cycle intermediates: implications for the inactivation of transmitter amino acids? J Neurochem. 1995;65:2227–2234. doi: 10.1046/j.1471-4159.1995.65052227.x. [DOI] [PubMed] [Google Scholar]
- Hassel B, Sonnewald U, Fonnum F. Glial-neuronal interactions as studied by cerebral metabolism of [2-13C]acetate and [1-13C]glucose: an ex vivo 13C NMR spectroscopic study. J Neurochem. 1995;64:2773–2782. doi: 10.1046/j.1471-4159.1995.64062773.x. [DOI] [PubMed] [Google Scholar]
- Haydon PG, Carmignoto G. Astrocyte control of synaptic transmission and neurovascular coupling. Physiol Rev. 2006;86:1009–1031. doi: 10.1152/physrev.00049.2005. [DOI] [PubMed] [Google Scholar]
- Higgins JJ, Glasgow AM, Lusk M, Kerr DS. MRI, clinical, and biochemical features of partial pyruvate carboxylase deficiency. J Child Neurol. 1994;9:436–439. doi: 10.1177/088307389400900421. [DOI] [PubMed] [Google Scholar]
- Hovda DA, Yoshino A, Kawamata T, Katayama Y, Becker DP. Diffuse prolonged depression of cerebral oxidative metabolism following concussive brain injury in the rat: a cytochrome oxidase histochemistry study. Brain Res. 1991;567:1–10. doi: 10.1016/0006-8993(91)91429-5. [DOI] [PubMed] [Google Scholar]
- Keenan HT, Bratton SL. Epidemiology and outcomes of pediatric traumatic brain injury. Dev Neurosci. 2006;28:256–263. doi: 10.1159/000094152. [DOI] [PubMed] [Google Scholar]
- Kochanek AR, Kline AE, Gao WM, Chadha M, Lai Y, Clark RS, Dixon CE, Jenkins LW. Gel-based hippocampal proteomic analysis 2 weeks following traumatic brain injury to immature rats using controlled cortical impact. Dev Neurosci. 2006;28:410–419. doi: 10.1159/000094167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifshitz J, Friberg H, Neumar RW, Raghupathi R, Welsh FA, Janmey P, Saatman KE, Wieloch T, Grady MS, McIntosh TK. Structural and functional damage sustained by mitochondria after traumatic brain injury in the rat: evidence for differentially sensitive populations in the cortex and hippocampus. J Cereb Blood Flow Metab. 2003;23:219–231. doi: 10.1097/01.WCB.0000040581.43808.03. [DOI] [PubMed] [Google Scholar]
- Marcoux J, McArthur DA, Miller C, Glenn TC, Villablanca P, Martin NA, Hovda DA, Alger JR, Vespa PM. Persistent metabolic crisis as measured by elevated cerebral microdialysis lactate-pyruvate ratio predicts chronic frontal lobe brain atrophy after traumatic brain injury. Crit Care Med. 2008;36:2871–2877. doi: 10.1097/CCM.0b013e318186a4a0. [DOI] [PubMed] [Google Scholar]
- McKenna MC. The glutamate-glutamine cycle is not stoichiometric: fates of glutamate in brain. J Neurosci Res. 2007;85:3347–3358. doi: 10.1002/jnr.21444. [DOI] [PubMed] [Google Scholar]
- McKenna MC, Waagepetersen HS, Schousboe A, Sonnewald U. Neuronal and astrocytic shuttle mechanisms for cytosolic-mitochondrial transfer of reducing equivalents: current evidence and pharmacological tools. Biochem Pharmacol. 2006;71:399–407. doi: 10.1016/j.bcp.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Montana V, Ni Y, Sunjara V, Hua X, Parpura V. Vesicular glutamate transporter-dependent glutamate release from astrocytes. J Neurosci. 2004;24:2633–2642. doi: 10.1523/JNEUROSCI.3770-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opii WO, Nukala VN, Sultana R, Pandya JD, Day KM, Merchant ML, Klein JB, Sullivan PG, Butterfield DA. Proteomic identification of oxidized mitochondrial proteins following experimental traumatic brain injury. J Neurotrauma. 2007;24:772–789. doi: 10.1089/neu.2006.0229. [DOI] [PubMed] [Google Scholar]
- Oz G, Berkich DA, Henry PG, Xu Y, LaNoue K, Hutson SM, Gruetter R. Neuroglial metabolism in the awake rat brain: CO2 fixation increases with brain activity. J Neurosci. 2004;24:11273–11279. doi: 10.1523/JNEUROSCI.3564-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandya JD, Pauly JR, Nukala VN, Sebastian AH, Day KM, Korde AS, Maragos WF, Hall ED, Sullivan PG. Post-Injury Administration of Mitochondrial Uncouplers Increases Tissue Sparing and Improves Behavioral Outcome following Traumatic Brain Injury in Rodents. J Neurotrauma. 2007;24:798–811. doi: 10.1089/neu.2006.3673. [DOI] [PubMed] [Google Scholar]
- Qu H, Eloqayli H, Muller B, Aasly J, Sonnewald U. Glial-neuronal interactions following kainate injection in rats. Neurochem Int. 2003;42:101–106. doi: 10.1016/s0197-0186(02)00051-7. [DOI] [PubMed] [Google Scholar]
- Richards EM, Fiskum G, Rosenthal RE, Hopkins I, McKenna MC. Hyperoxic reperfusion after global ischemia decreases hippocampal energy metabolism. Stroke. 2007;38:1578–1584. doi: 10.1161/STROKEAHA.106.473967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson CL, Saraswati M, Fiskum G. Mitochondrial dysfunction early after traumatic brain injury in immature rats. J Neurochem. 2007;101:1248–1257. doi: 10.1111/j.1471-4159.2007.04489.x. [DOI] [PubMed] [Google Scholar]
- Robertson CL, Soane L, Siegel ZT, Fiskum G. The potential role of mitochondria in pediatric traumatic brain injury. Dev Neurosci. 2006a;28:432–446. doi: 10.1159/000094169. [DOI] [PubMed] [Google Scholar]
- Robertson CL, Puskar A, Hoffman GE, Murphy AZ, Saraswati M, Fiskum G. Physiologic progesterone reduces mitochondrial dysfunction and hippocampal cell loss after traumatic brain injury in female rats. Exp Neurol. 2006b;197:235–243. doi: 10.1016/j.expneurol.2005.09.014. [DOI] [PubMed] [Google Scholar]
- Samant U. B. t., Mack CD, Koepsell T, Rivara FP, Vavilala MS. Time of hypotension and discharge outcome in children with severe traumatic brain injury. J Neurotrauma. 2008;25:495–502. doi: 10.1089/neu.2007.0491. [DOI] [PubMed] [Google Scholar]
- Satrustegui J, Contreras L, Ramos M, Marmol P, del Arco A, Saheki T, Pardo B. Role of aralar, the mitochondrial transporter of aspartate-glutamate, in brain N-acetylaspartate formation and Ca(2+) signaling in neuronal mitochondria. J Neurosci Res. 2007;85:3359–3366. doi: 10.1002/jnr.21299. [DOI] [PubMed] [Google Scholar]
- Schroder ML, Muizelaar JP, Kuta AJ, Choi SC. Thresholds for cerebral ischemia after severe head injury: relationship with late CT findings and outcome. J Neurotrauma. 1996;13:17–23. doi: 10.1089/neu.1996.13.17. [DOI] [PubMed] [Google Scholar]
- Siesjo BK. Cerebral circulation and metabolism. J Neurosurg. 1984;60:883–908. doi: 10.3171/jns.1984.60.5.0883. [DOI] [PubMed] [Google Scholar]
- Smith PK, Krohn RI, Hermanson GT, Mallia AK, Gartner FH, Provenzano MD, Fujimoto EK, Goeke NM, Olson BJ, Klenk DC. Measurement of protein using bicinchoninic acid. Anal Biochem. 1985;150:76–85. doi: 10.1016/0003-2697(85)90442-7. [DOI] [PubMed] [Google Scholar]
- Soustiel JF, Sviri GE. Monitoring of cerebral metabolism: non-ischemic impairment of oxidative metabolism following severe traumatic brain injury. Neurol Res. 2007;29:654–660. doi: 10.1179/016164107X240017. [DOI] [PubMed] [Google Scholar]
- Starkov AA, Fiskum G, Chinopoulos C, Lorenzo BJ, Browne SE, Patel MS, Beal MF. Mitochondrial alpha-ketoglutarate dehydrogenase complex generates reactive oxygen species. J Neurosci. 2004;24:7779–7788. doi: 10.1523/JNEUROSCI.1899-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi H, Jin S, Suzuki H, Doi Y, Liang J, Kawanokuchi J, Mizuno T, Sawada M, Suzumura A. Blockade of microglial glutamate release protects against ischemic brain injury. Exp Neurol. 2008 doi: 10.1016/j.expneurol.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Thomas S, Prins ML, Samii M, Hovda DA. Cerebral metabolic response to traumatic brain injury sustained early in development: a 2-deoxy-D-glucose autoradiographic study. J Neurotrauma. 2000;17:649–665. doi: 10.1089/089771500415409. [DOI] [PubMed] [Google Scholar]
- Verweij BH, Amelink GJ, Muizelaar JP. Current concepts of cerebral oxygen transport and energy metabolism after severe traumatic brain injury. Prog Brain Res. 2007;161:111–124. doi: 10.1016/S0079-6123(06)61008-X. [DOI] [PubMed] [Google Scholar]
- Waagepetersen HS, Sonnewald U, Larsson OM, Schousboe A. Compartmentation of TCA cycle metabolism in cultured neocortical neurons revealed by 13C MR spectroscopy. Neurochem Int. 2000;36:349–358. doi: 10.1016/s0197-0186(99)00143-6. [DOI] [PubMed] [Google Scholar]
- Xiong Y, Peterson PL, Verweij BH, Vinas FC, Muizelaar JP, Lee CP. Mitochondrial dysfunction after experimental traumatic brain injury: combined efficacy of SNX-111 and U-101033E. J Neurotrauma. 1998;15:531–544. doi: 10.1089/neu.1998.15.531. [DOI] [PubMed] [Google Scholar]
- Xu Y, Ola MS, Berkich DA, Gardner TW, Barber AJ, Palmieri F, Hutson SM, LaNoue KF. Energy sources for glutamate neurotransmission in the retina: absence of the aspartate/glutamate carrier produces reliance on glycolysis in glia. J Neurochem. 2007;101:120–131. doi: 10.1111/j.1471-4159.2006.04349.x. [DOI] [PubMed] [Google Scholar]
- Yoshino A, Hovda DA, Kawamata T, Katayama Y, Becker DP. Dynamic changes in local cerebral glucose utilization following cerebral conclusion in rats: evidence of a hyper- and subsequent hypometabolic state. Brain Res. 1991;561:106–119. doi: 10.1016/0006-8993(91)90755-k. [DOI] [PubMed] [Google Scholar]
- Zhong C, Zhao X, Van KC, Bzdega T, Smyth A, Zhou J, Kozikowski AP, Jiang J, O’Connor WT, Berman RF, Neale JH, Lyeth BG. NAAG peptidase inhibitor increases dialysate NAAG and reduces glutamate, aspartate and GABA levels in the dorsal hippocampus following fluid percussion injury in the rat. J Neurochem. 2006;97:1015–1025. doi: 10.1111/j.1471-4159.2006.03786.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.