Abstract
Purpose of Review
To summarize recent work from clinical and epidemiological studies which describe how, and at what stage, glaucoma affects the performance of important vision-related activities.
Recent Findings
Difficulties with the extremes of lighting are the most frequent complaint in glaucoma. Individuals with bilateral glaucoma also self-report difficulty with a broad array of tasks including reading, walking, and driving. Bilateral glaucoma is associated with driving cessation and limitation, bumping into objects, slower walking, and falls. Some, but not all, studies also demonstrate higher accident rates in glaucoma. Measurable effects on reading speed have only been observed with field damage severe enough to affect binocular central acuity.
Summary
Glaucoma with bilateral visual field loss is associated with increased symptoms and a measurable decline in mobility and driving. Further work is necessary to establish whether unilateral glaucoma has a significant impact on patients, to determine whether reading difficulty is common in subjects with bilateral glaucoma, and to establish the effects of lighting conditions on task performance in glaucoma.
Keywords: Glaucoma, disability, mobility, driving, reading, quality of life
Introduction
Since quality of life in glaucoma was first examined 10 years ago [1,2], more research has focused on the impact of glaucoma on patients. Many population-based studies [3–5], and multi-center clinical trials [6] have evaluated self-reported disability occurring as a result of glaucoma. Research from the population-based Salisbury Eye Evaluation (SEE), and from other clinic-based studies, have directly examined how individuals with glaucoma perform important tasks such as driving, walking, and reading, and also looked into the mechanism by which glaucoma produces disability. This research has led to a better understanding of how, and at what stage of disease, glaucoma impacts the activities of daily living in adults with the disease.
Importance of relating glaucomatous damage to disability
Glaucoma affects approximately 2% of adults over the age of 40 [7], and disease prevalence increases dramatically with age [8,9]. Aging of the population worldwide will lead to substantially more individuals with glaucoma in coming years [7,10], which may result in dramatically more individuals with glaucoma-related visual disability.
Knowledge of when and how glaucoma produces disability will help decide which patients should be treated and how aggressive treatment should be. This knowledge will also help to determine the level of disease at which the benefit of screening outweighs costs. In addition, measurement of disability from glaucoma can define guidelines to increase patient safety (i.e. avoid crashes in drivers), identify subjects who might benefit from rehabilitative interventions, and test the efficacy of rehabilitative interventions.
Glaucoma and Disability – Which tasks to study?
Studies have suggested that glaucoma affects a broad array of activities [2,6,11–13], raising the question of which vision-related activities are most important for study. Ideally, investigations should focus on activities which are both important to individuals with glaucoma and are likely to be affected by the disease.
Recent work has assessed which activities are most important to subjects with glaucoma by asking them to choose amongst hypothetical scenarios in which they had different levels of difficulty with different tasks [14**,15**]. Subjects gave the greatest importance to tasks involving central and near vision (i.e. reading), with high scores also given to mobility outside the home (i.e. driving and walking outside) [14**,15**]. Less importance was given to glare, bumping into objects, and performing household chores [15**].
Focus groups [16–19], and clinical trial-based questionnaires [20] have examined the complementary question of which tasks are most affected by glaucoma. Difficulties related to lighting, such as glare [17,20] and difficulty adapting to different levels of light [17,20], consistently ranked as the most frequent complaint. Other common complaints included difficulty with walking or stair climbing, reading, and face recognition/social relations [16,17,19]. Driving was not discussed in most of these glaucoma focus groups, but was the most frequent complaint in the group used to create the NEI-VFQ questionnaire [16]. Altangerel and Spaeth directly tested the performance of glaucoma subjects on an index of activities, and identified searching for objects, reading, and manual tasks (placing a stick into holes of different sizes) as most related to the extent of VF loss [21].
Criteria for evaluating studies relating glaucoma to disability
It is clear that glaucoma affects all vision-related activities in the most advanced cases, but less clear how severe disease must be before significant difficulty is first detected. Therefore, this review will give priority to studies which yield insight into when glaucomatous VF damage has an effect on functional impairment, and how the level of disability relates to stage of disease (Figure 1). VF damage can also occur from a variety of eye conditions, and has been noted as an artifact of testing in 15% of individuals without eye disease [22]. Other eye diseases produce different spatial patterns of VF loss than glaucoma and also have distinct effects on other aspects of vision (acuity, contrast sensitivity, etc.). Therefore, studies which relate VF damage independent of cause to disability have been excluded from this review.
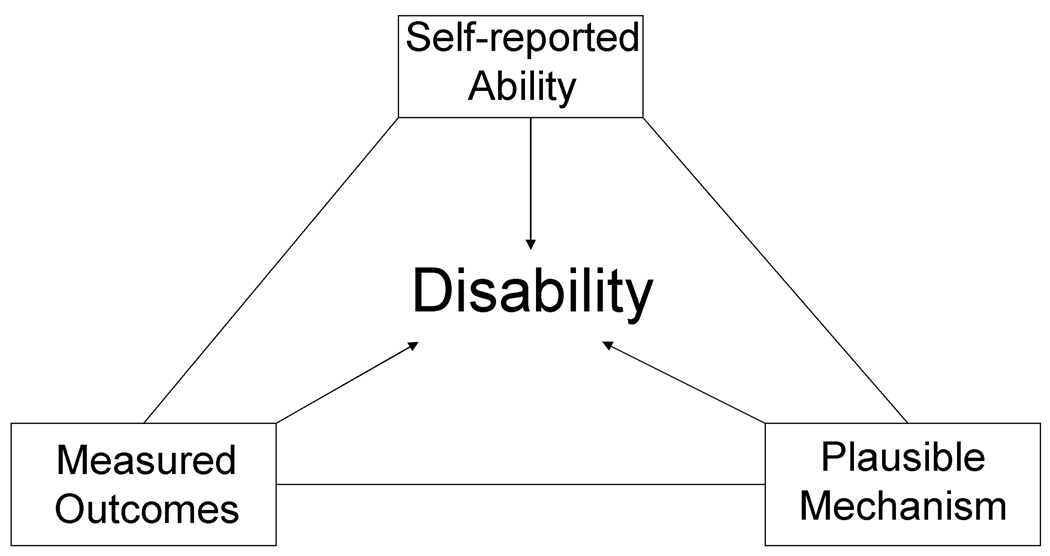
Figure 1.
Many distinct relationships between disease severity and disability are possible. Grouping of patients over a range of severity can demonstrate increased disability for the group, while ignoring that the extent of disability may vary drastically over the range of disease severity studied.
Numerous non-ocular factors (i.e. race, cognitive ability, education, and comorbid illness) differ between subjects with and without glaucoma, and strongly influence reading, mobility or driving [23**,24**,25**]. Not adjusting for these important covariates can result in drastically different results. In SEE for example, bilateral glaucoma subjects read more slowly than subjects without glaucoma in the unadjusted analysis, but no difference in reading speed persisted after adjusting for age, race, education, and cognitive ability (except in those with the most advanced glaucoma) [25**]. Therefore, we will focus on studies that have attempted to account for other potentially confounding variables.
Staging glaucoma for purposes of disability
To relate difficulty with a given task with disease severity, an appropriate disease severity scale must be used. Several glaucoma staging systems have been previously described, though nearly all focus on staging disease for a single eye [26–29]. Overlapping VF loss in both eyes may be most relevant to disability. Therefore, systems to directly test the binocular VF were developed, such as the Esterman binocular suprathreshold field [30]. Others have devised methods to simulate the binocular VF by combining data from separate right and left monocular VF tests [31,32].
The best metric of glaucoma damage to relate disease severity to disability still remains unclear. Overlapping VF loss has not been shown to produce more disability than non-overlapping VF loss. Additionally, Esterman VFs are not routinely ordered, and no “bedside” method for combining right and left VFs is available. Thus, metrics which use the individual monocular field data, such as the mean deviation (MD) of the better or worse eye, have been most common employed. Further work is needed to more easily measure or generate binocular fields, and to further explore their utility as a metric for disability.
Understanding when Disability is Present
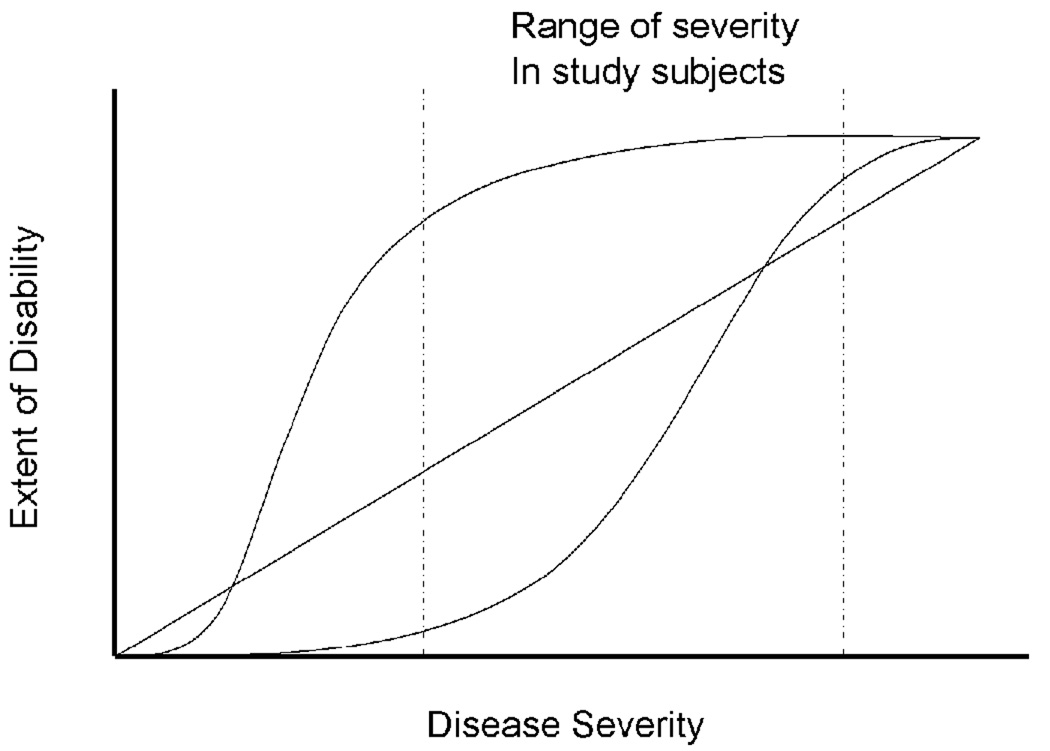
The strongest evidence for the presence of disability exists when multiple lines of evidence link visual impairment from a certain disease (and of a given severity) to difficulty in a specific functional domain (i.e. reading, walking, or driving). Ideally, self-reported difficulty with a task, measured task performance, and a mechanism linking disease and disability would all support the association of disability with a given stage of disease (Figure 2). For example, if bilateral glaucomatous VF loss truly affects the ability to read, then individuals with bilateral glaucoma should describe more difficulty reading, read measurably more poorly, and demonstrate a plausible mechanism for their disability (i.e. greater time finding the next line of text) when compared to similar individuals without glaucoma.
Figure 2.
The strongest evidence linking disability to eye disease occurs when self-reported ability, measured outcomes, and a plausible mechanism for disability in a given functional domain (i.e. reading, driving, or walking) are all observed to occur at the same level of disease severity.
All methods to evaluate disability have strengths and weaknesses, and no single method of study can, by itself, demonstrate disability (Table 1). Direct measures of task performance may fail to recapitulate how the task is performed in real-world settings. On the other hand, studies that measure disability through self-reported answers to questions are subject to bias. Knowledge that one’s eye is not normal may lead individuals to report more symptoms or difficulty with tasks. For example, one-third of subjects in the Collaborative Initial Glaucoma Treatment Study (CIGTS) attributed symptoms such as burning, irritation, eye pain and redness to their glaucoma though they had yet to receive treatment [33]. In other situations, knowledge of disease may make subjects less likely to report adverse events. For instance, one study demonstrated that patients with glaucoma were less likely to self-report a state-recorded automobile accident than subjects without glaucoma, and this reporting bias produced different conclusions about whether or not glaucoma is associated with more accidents [34]. Other individuals may under-report disability that they have accepted and by which they are no longer troubled. For example, only ¼ of those in the SEE cohort who read slower than 80 words per minute (the cutoff for reading impairment) reported moderate or extreme difficulty reading [35].
Table 1.
Merits of self-reported impairment and direct measurement of outcomes in assessing vision-related disability
| Self-reported Impairment |
Directly measured outcomes |
|
|---|---|---|
| Strengths | Captures patients’ perception of disease |
Tests ability under standardized conditions |
| Simple to perform | Less subject to reporting bias | |
| Assesses task difficulty under real-world settings |
Yield quantitative results | |
| Weaknesses | Bias introduced by knowledge of disease |
Difficult to recapitulate real- world activity setting |
| Clinical significance of differences in self-report scores unclear |
Hard to capture rare events. | |
| Impairment may not be reported when activities are given up |
More laborious to perform. |
Walking and balance
Walking and balance are important to healthy living. Elderly subjects with difficulty walking are more likely to enter into assisted living or nursing homes [36]. Furthermore, when walking becomes difficult or is accompanied by fear of falling, patients may restrict their physical activity [37], producing decreased quality of life [38,39], higher morbidity [40–42], and increased mortality [43–49]. In a glaucoma focus group, difficulty with walking was the most common complaint after difficulty with lighting, with 49% describing difficulties with steps, 42% describing difficulty going shopping, and 36% describing difficulty crossing the road [17]. Similarly, questionnaires given to glaucoma subjects demonstrated that two of the strongest correlates with binocular VF loss were difficulty with stairs and bumping into objects [19].
Overall, subjects with glaucoma walk more slowly than similarly-aged controls [50], and walking speed is strongly correlated with MD in the worse-eye VF [50]. A population-based comparison of walking in subjects with and without glaucoma demonstrated that subjects with bilateral, but not unilateral, glaucoma walked slower, and bumped into objects more frequently [24**]. No difference in performance was observed going up and down a short staircase [24**]. Slower walking speeds and more frequent bumps were also observed when the field of vision was artificially constricted in normal individuals [51]. Walking may be slower in glaucoma subjects because it requires greater care and concentration. Indeed, response to a secondary task slowed in walking glaucoma subjects as VF damage worsened [52*].
Glaucoma also has been noted to lead to impairment of balance. In SEE, subjects with bilateral, but not unilateral, glaucoma had more trouble performing balance tasks such as semi-tandem and tandem stands - where the heel of one foot is placed next to or in front of the big toe of the second foot [24**]. Other studies have demonstrated that individuals with glaucoma sway more when standing than normal individuals [53], and that greater sway is associated with increasing VF damage in the better eye [54*]. No differences in sway were observed when testing was performed with eyes closed, which strongly suggests that the observed changes in balance were due to loss of visual input [53,54*].
The end result of bumps and poor balance may be more frequent falls. In the Blue Mountains Eye Study, falls were twice as likely when subjects were using a glaucoma medicine [55]. Similarly, glaucoma subjects in the Singapore Malay Eye Study had four-fold higher odds of falling than non-glaucoma subjects after adjusting for visual acuity, though this conclusion was limited by the small number of glaucoma subjects [56]. A four-fold higher risk for falling was reported by patients in a clinic-based study by Haymes. However, non-glaucoma controls in that report seemed poorly matched to the glaucoma subjects, as they were more frequently employed, had fewer medical conditions, and had better acuity [57].
Glaucoma-related falls may produce serious fractures in elderly patients. Amongst Medicare recipients, glaucoma subjects coded as visually impaired were more likely to have had a fall or accident (OR=1.6) and to have had a femur fracture (OR=1.6) when compared to glaucoma patients not coded to have visual loss [58]. Colón-Emeric examined risk factors for entry into a skilled nursing facility because of a hip fracture, and noted that glaucoma was a risk factor in men, but not women [59].
Reading
Difficulty with central and near vision tasks in general, and with reading specifically, are the most frequent complaint amongst subjects with eye disease [16]. Near vision tasks such as reading are also the most valued visual function amongst subjects with glaucoma [14**]. While reading is clearly dependent on visual acuity [16,60], complaints of difficulty reading are also commonplace amongst subjects with glaucoma, and were noted in over 40% of the glaucoma subjects in a glaucoma focus group [17].
In the SEE study, subjects with bilateral glaucoma were almost 5 times more likely to report severe difficulty with near activities than subjects without glaucoma [4]. This confirms several clinic-based studies that demonstrate more vision-related difficulty with near vision tasks in the presence of glaucoma-related VF loss [1,2,11,13,61]. Data from SEE, however, demonstrated significant discordance between measured reading speed and self-reported reading difficulty, particularly amongst subjects who read poorly. This disparity between measured reading speed and self-assessment highlights the need to utilize both questionnaire and direct testing methods to assess reading [35].
When reading speed was directly measured in the SEE study, only the most advanced glaucoma patients had significantly decreased reading speed [25**]. However, reading speed was measured over a short 15 second test interval that may not capture difficulty with sustained reading or with reading-related tasks such as searching pages for information. A second study identified the reading of small print as one of the most visually demanding tasks for glaucoma subjects, and noted a moderate correlation between reading speed and the extent of Esterman binocular VF loss [21]. In another study, glaucoma subjects with worse Esterman scores described more difficulty following a line of print or finding the next line when reading [19], providing a plausible mechanism by which VF loss could lead to reading difficulty. Further testing of reading under more realistic reading is required to address these contradictory findings and to firmly establish when glaucoma results in difficulty reading.
Driving
Mobility outside the home is cited as the one of the two most important visual functions by subjects with glaucoma [14**,15**], and is particular important in the United States where the elderly rely upon driving as the primary means of transportation [62]. Elderly persons who stop driving are nearly 5 times more likely to move to a long-term care facility [63], have higher rates of depression [64], and report a lower quality of life [65]. Large numbers of subjects with very advanced VF loss continue to drive [23**], even after a previous collision [66], subjecting both themselves and society at large to increased mortality [67].
Previous analyses of accident rates among those with glaucoma provide mixed evidence for an association. McGwin found that glaucoma subjects had a 3-fold increase in the odds of a state-reported accident when compared to controls without glaucoma [34]. A subsequent case-control study also noted higher crash rates with worsening levels of glaucomatous VF loss [68]. Haymes found a high rate of vehicle accidents among glaucoma subjects when compared to controls (OR = 6.6), though controls were partially recruited from an employee pool that was healthier and had better visual acuity than the glaucoma subjects [69]. Hu, on the other, hand, found that crash rates were not higher in women with glaucoma, while men with glaucoma had only a slightly higher rate of state-recorded accidents (OR=1.7) [70]. One report even noted fewer state-recorded accidents amongst individuals with glaucoma (OR = 0.67) [71].
Subjects with glaucoma perceive more difficulty driving than control subjects without glaucoma [12,72], and perceived difficulty increases with worsening VF damage in the better eye [2]. SEE subjects with bilateral, but not unilateral glaucoma, had worse self-reported scores with regards to driving at night, suggesting that disability may occur primarily in subjects with bilateral disease [4]. One study found that driving ability was self-reported to be worse among glaucoma subjects with worse than 12 dB mean loss in the more affected eye. Yet, the same investigation reported that there were significant differences in perceived ability to drive between subjects with treated and untreated ocular hypertension, suggesting that reported difficulty may be more related to perceived disease severity than actual disability [72].
As a result of perceived difficulty with their vision, individuals with glaucoma may also limit or stop driving. Subjects in the SEE study with bilateral glaucoma were nearly 3 times as likely to have stopped driving than individuals without glaucoma, and unilateral glaucoma was noted to also possibly result in more frequent driving cessation [23**]. Glaucoma was more frequently associated with driving cessation in the Blue Mountains Eye Study (OR=2.2) as well, though the likelihood of driving cessation was not separately analyzed for different levels of VF loss [73]. Others with glaucoma likely restrict their driving without stopping altogether. Subjects with glaucoma are twice as likely to avoid driving at night, in fog, in the rain, in rush hour, or in highway traffic when compared to subjects without glaucoma [71]. Another investigation found that glaucoma subjects were more likely to limit their driving at night and in unfamiliar areas, but not on highways, in bad weather, or during rush hour [74]. We found that elderly subjects had similar rates of night driving cessation, driving frequency, and cessation of driving in unfamiliar areas whether they had glaucoma or not. However, our data suggest that subjects with bilateral glaucoma do report more driving limitation attributable to visual difficulty [23**].
A plausible mechanism for difficulty driving among glaucoma patients is that they have more difficulty seeing peripheral objects. Indeed, one study found that subjects with glaucoma were less likely to see pedestrians on the side of the road during actual road tests, and were more likely to require an intervention by the driving evaluator [75*]. Subjects with glaucoma also experienced more accidents in a wide-field driving simulator than subjects without glaucoma, and the likelihood of a simulated accident correlated with the degree of constriction in the binocular horizontal VF [76]. However, a separate study did not find that glaucoma subjects differed from controls in any of 8 driving measures performed in a driving simulator, though less than 30 subjects were in each group [76].
The Importance of Lighting Conditions
The lighting conditions under which tasks are performed may be even more important than the task itself. Seventy percent of patients in a focus group complained of glare with bright lights, while over half described difficulty adapting to different levels of lighting [17]. Another study noted that 82% of glaucoma subjects described trouble seeing in the dark as compared to only 32% of controls [18]. Two studies have also noted that the greatest change in self-reported ability with worsening VF damage occurs in the domain of lighting and glare [14**,17]. Simulated VF constriction in normal individuals has also been observed to have a more profound effect under scotopic conditions [51], though direct testing of task performance in glaucoma subjects relative to light level remains largely unexplored.
Other Effects of Glaucoma
Medicare data has suggested that subjects severely impaired from glaucoma are more likely to develop depression (OR=1.6), though other studies have noted no association of depressive symptoms and glaucoma [77,78]. The diagnosis of glaucoma may by itself increase anxiety, and up to 80% of patients describe negative emotions such as anxiety upon receiving the diagnosis of glaucoma [79]. In CIGTS, nearly 50% of subjects worried about possible blindness as a result of their diagnosis [33].
Conclusion
Individuals with bilateral VF loss from glaucoma have worse self-reported visual abilities and measurably worse task performance, particularly for driving and mobility. Much less evidence supports the idea that unilateral VF loss results in significant disability. More research is also needed to determine how increasing VF damage from glaucoma affects other important domains such as reading, face recognition, and task performance with very bright or very dim lighting. It will be important to conduct studies that directly assess driving and mobility under real world conditions.
Acknowledgments
Work funded by NEI grant EY015025.
REFERENCES
- 1.Gutierrez P, Wilson MR, Johnson C, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch.Ophthalmol. 1997;115:777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 2.Parrish RK, 2nd, Gedde SJ, Scott IU, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–1455. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 3.McKean-Cowdin R, Varma R, Wu J, et al. Severity of visual field loss and health-related quality of life. Am.J.Ophthalmol. 2007;143:1013–1023. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freeman EE, Munoz B, West SK, et al. Glaucoma and quality of life: the Salisbury Eye Evaluation. Ophthalmology. 2008;115:233–238. doi: 10.1016/j.ophtha.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 5.Ivers RQ, Mitchell P, Cumming RG. Visual function tests, eye disease and symptoms of visual disability: a population-based assessment. Clin.Experiment.Ophthalmol. 2000;28:41–47. doi: 10.1046/j.1442-9071.2000.00236.x. [DOI] [PubMed] [Google Scholar]
- 6.Mills RP, Janz NK, Wren PA, Guire KE. Correlation of visual field with quality-of-life measures at diagnosis in the Collaborative Initial Glaucoma Treatment Study (CIGTS) J.Glaucoma. 2001;10:192–198. doi: 10.1097/00061198-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Friedman DS, Wolfs RC, O'Colmain BJ, et al. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122:532–538. doi: 10.1001/archopht.122.4.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman DS, Jampel HD, Munoz B, West SK. The prevalence of open-angle glaucoma among blacks and whites 73 years and older: the Salisbury Eye Evaluation Glaucoma Study. Arch.Ophthalmol. 2006;124:1625–1630. doi: 10.1001/archopht.124.11.1625. [DOI] [PubMed] [Google Scholar]
- 10.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ringsdorf L, McGwin G, Jr, Owsley C. Visual field defects and vision-specific health-related quality of life in African Americans and whites with glaucoma. J.Glaucoma. 2006;15:414–418. doi: 10.1097/01.ijg.0000212252.72207.c2. [DOI] [PubMed] [Google Scholar]
- 12.Gutierrez P, Wilson MR, Johnson C, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 13.Broman AT, Munoz B, Rodriguez J, et al. The impact of visual impairment and eye disease on vision-related quality of life in a Mexican-American population: proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:3393–3398. [PubMed] [Google Scholar]
- 14. Burr JM, Kilonzo M, Vale L, Ryan M. Developing a preference-based Glaucoma Utility Index using a discrete choice experiment. Optom. Vis. Sci. 2007;84:797–808. doi: 10.1097/OPX.0b013e3181339f30. ** Examined which functions are most important to subjects with glaucoma using discrete choice modeling.
- 15. Aspinall PA, Johnson ZK, Azuara-Blanco A, et al. Evaluation of quality of life and priorities of patients with glaucoma. Invest.Ophthalmol.Vis.Sci. 2008;49:1907–1915. doi: 10.1167/iovs.07-0559. ** Identified the vision-related functions that were most important to subjects with glaucoma.
- 16.Mangione CM, Berry S, Spritzer K, et al. Identifying the content area for the 51-item National Eye Institute Visual Function Questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol. 1998;116:227–233. doi: 10.1001/archopht.116.2.227. [DOI] [PubMed] [Google Scholar]
- 17.Nelson P, Aspinall P, O'Brien C. Patients' perception of visual impairment in glaucoma: a pilot study. Br.J.Ophthalmol. 1999;83:546–552. doi: 10.1136/bjo.83.5.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee BL, Gutierrez P, Gordon M, et al. The Glaucoma Symptom Scale. A brief index of glaucoma-specific symptoms. Arch.Ophthalmol. 1998;116:861–866. doi: 10.1001/archopht.116.7.861. [DOI] [PubMed] [Google Scholar]
- 19.Viswanathan AC, McNaught AI, Poinoosawmy D, et al. Severity and stability of glaucoma: patient perception compared with objective measurement. Arch.Ophthalmol. 1999;117:450–454. doi: 10.1001/archopht.117.4.450. [DOI] [PubMed] [Google Scholar]
- 20.Janz NK, Wren PA, Lichter PR, et al. The Collaborative Initial Glaucoma Treatment Study: interim quality of life findings after initial medical or surgical treatment of glaucoma. Ophthalmology. 2001;108:1954–1965. doi: 10.1016/s0161-6420(01)00874-0. [DOI] [PubMed] [Google Scholar]
- 21.Altangerel U, Spaeth GL, Steinmann WC. Assessment of function related to vision (AFREV) Ophthalmic Epidemiol. 2006;13:67–80. doi: 10.1080/09286580500428500. [DOI] [PubMed] [Google Scholar]
- 22.Coleman AL. Sources of binocular suprathreshold visual field loss in a cohort of older women being followed for risk of falls (an American Ophthalmological Society thesis) Trans.Am.Ophthalmol.Soc. 2007;105:312–329. [PMC free article] [PubMed] [Google Scholar]
- 23. Ramulu PY, West SK, Munoz B, et al. Driving Cessation and Driving Limitation in Glaucoma: The Salisbury Eye Evaluation Project. 2008 doi: 10.1016/j.ophtha.2009.03.033. Submitted for publication. ** Demonstrated more frequent driving cessation with bilateral glaucoma in a population-based sample elderly drivers.
- 24. Friedman DS, Freeman E, Munoz B, et al. Glaucoma and mobility performance: the Salisbury Eye Evaluation Project. Ophthalmology. 2007;114:2232–2237. doi: 10.1016/j.ophtha.2007.02.001. ** Directly tested a population-based sample of elderly individuals with known glaucoma status in a mobility course.
- 25. Ramulu PY, West SK, Munoz B, et al. Glaucoma and Reading Speed: The Salisbury Eye Evaluation Project. Archives of Ophthalmology. doi: 10.1001/archophthalmol.2008.523. In Press; ** Directly tested reading speed in a population-based sample of elderly individuals with known glaucoma status.
- 26.Mills RP, Budenz DL, Lee PP, et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am.J.Ophthalmol. 2006;141:24–30. doi: 10.1016/j.ajo.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 27.Hodapp E, Parrish RK, Anderson DR. Clinical decisions in glaucoma. St. Louis: Mosby; 1993. [Google Scholar]
- 28.Katz J. Scoring systems for measuring progression of visual field loss in clinical trials of glaucoma treatment. Ophthalmology. 1999;106:391–395. doi: 10.1016/S0161-6420(99)90052-0. [DOI] [PubMed] [Google Scholar]
- 29.Musch DC, Lichter PR, Guire KE, Standardi CL. The Collaborative Initial Glaucoma Treatment Study: study design, methods, and baseline characteristics of enrolled patients. Ophthalmology. 1999;106:653–662. doi: 10.1016/s0161-6420(99)90147-1. [DOI] [PubMed] [Google Scholar]
- 30.Esterman B. Functional scoring of the binocular field. Ophthalmology. 1982;89:1226–1234. doi: 10.1016/s0161-6420(82)34647-3. [DOI] [PubMed] [Google Scholar]
- 31.Nelson-Quigg JM, Cello K, Johnson CA. Predicting binocular visual field sensitivity from monocular visual field results. Invest.Ophthalmol.Vis.Sci. 2000;41:2212–2221. [PubMed] [Google Scholar]
- 32.Crabb DP, Fitzke FW, Hitchings RA, Viswanathan AC. A practical approach to measuring the visual field component of fitness to drive. Br.J.Ophthalmol. 2004;88:1191–1196. doi: 10.1136/bjo.2003.035949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janz NK, Wren PA, Lichter PR, et al. Quality of life in newly diagnosed glaucoma patients: The Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2001;108:887–897. doi: 10.1016/s0161-6420(00)00624-2. discussion 898. [DOI] [PubMed] [Google Scholar]
- 34.McGwin G, Jr, Owsley C, Ball K. Identifying crash involvement among older drivers: agreement between self-report and state records. Accid.Anal.Prev. 1998;30:781–791. doi: 10.1016/s0001-4575(98)00031-1. [DOI] [PubMed] [Google Scholar]
- 35.Friedman SM, Munoz B, Rubin GS, et al. Characteristics of discrepancies between self-reported visual function and measured reading speed. Salisbury Eye Evaluation Project Team. Invest.Ophthalmol.Vis.Sci. 1999;40:858–864. [PubMed] [Google Scholar]
- 36.Yu MS, Chan CC, Tsim RK. Usefulness of the Elderly Mobility Scale for classifying residential placements. Clin.Rehabil. 2007;21:1114–1120. doi: 10.1177/0269215507080789. [DOI] [PubMed] [Google Scholar]
- 37.Deshpande N, Metter EJ, Lauretani F, et al. Activity restriction induced by fear of falling and objective and subjective measures of physical function: a prospective cohort study. J.Am.Geriatr.Soc. 2008;56:615–620. doi: 10.1111/j.1532-5415.2007.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garatchea N, Molinero O, Martinez-Garcai R, et al. Feelings of well being in elderly people: Relationship to physicial activity and physical function. Archives of Gerontology. doi: 10.1016/j.archger.2008.02.010. In Press. [DOI] [PubMed] [Google Scholar]
- 39.Lynch BM, Cerin E, Owen N, et al. Prospective relationships of physical activity with quality of life among colorectal cancer survivors. J.Clin.Oncol. 2008;26:4480–4487. doi: 10.1200/JCO.2007.15.7917. [DOI] [PubMed] [Google Scholar]
- 40.Leon AS, Connett J, Jacobs DR, Jr, Rauramaa R. Leisure-time physical activity levels and risk of coronary heart disease and death. The Multiple Risk Factor Intervention Trial. JAMA. 1987;258:2388–2395. [PubMed] [Google Scholar]
- 41.Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS., Jr Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N.Engl.J.Med. 1991;325:147–152. doi: 10.1056/NEJM199107183250302. [DOI] [PubMed] [Google Scholar]
- 42.Cummings SR, Kelsey JL, Nevitt MC, O'Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol.Rev. 1985;7:178–208. doi: 10.1093/oxfordjournals.epirev.a036281. [DOI] [PubMed] [Google Scholar]
- 43.Paffenbarger RS, Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N.Engl.J.Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 44.Kaplan GA, Seeman TE, Cohen RD, et al. Mortality among the elderly in the Alameda County Study: behavioral and demographic risk factors. Am.J.Public Health. 1987;77:307–312. doi: 10.2105/ajph.77.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grand A, Grosclaude P, Bocquet H, et al. Disability, psychosocial factors and mortality among the elderly in a rural French population. J.Clin.Epidemiol. 1990;43:773–782. doi: 10.1016/0895-4356(90)90237-j. [DOI] [PubMed] [Google Scholar]
- 46.Rakowski W, Mor V. The association of physical activity with mortality among older adults in the Longitudinal Study of Aging (1984–1988) J.Gerontol. 1992;47:M122–M129. doi: 10.1093/geronj/47.4.m122. [DOI] [PubMed] [Google Scholar]
- 47.Simonsick EM, Lafferty ME, Phillips CL, et al. Risk due to inactivity in physically capable older adults. Am.J.Public Health. 1993;83:1443–1450. doi: 10.2105/ajph.83.10.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ruigomez A, Alonso J, Anto JM. Relationship of health behaviours to five-year mortality in an elderly cohort. Age Ageing. 1995;24:113–119. doi: 10.1093/ageing/24.2.113. [DOI] [PubMed] [Google Scholar]
- 49.Bijnen FC, Caspersen CJ, Feskens EJ, et al. Physical activity and 10-year mortality from cardiovascular diseases and all causes: The Zutphen Elderly Study. Arch.Intern.Med. 1998;158:1499–1505. doi: 10.1001/archinte.158.14.1499. [DOI] [PubMed] [Google Scholar]
- 50.Turano KA, Rubin GS, Quigley HA. Mobility performance in glaucoma. Invest Ophthalmol Vis Sci. 1999;40:2803–2809. [PubMed] [Google Scholar]
- 51.Hassan SE, Hicks JC, Lei H, Turano KA. What is the minimum field of view required for efficient navigation? Vision Res. 2007;47:2115–2123. doi: 10.1016/j.visres.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 52. Geruschat DR, Turano KA. Estimating the amount of mental effort required for independent mobility: persons with glaucoma. Invest.Ophthalmol.Vis.Sci. 2007;48:3988–3994. doi: 10.1167/iovs.06-1193. * Assessed response time to a secondary task in subjects with glaucoma while they walked in different environments.
- 53.Shabana N, Cornilleau-Peres V, Droulez J, et al. Postural stability in primary open angle glaucoma. Clin.Experiment.Ophthalmol. 2005;33:264–273. doi: 10.1111/j.1442-9071.2005.01003.x. [DOI] [PubMed] [Google Scholar]
- 54. Black AA, Wood JM, Lovie-Kitchin JE, Newman BM. Visual impairment and postural sway among older adults with glaucoma. Optom.Vis.Sci. 2008;85:489–497. doi: 10.1097/OPX.0b013e31817882db. * Tested how balance was affected in glaucoma subjects with a range of VF loss.
- 55.Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J.Am.Geriatr.Soc. 1998;46:58–64. doi: 10.1111/j.1532-5415.1998.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 56.Lamoureux EL, Chong E, Wang JJ, et al. Visual impairment, causes of vision loss, and falls: the singapore malay eye study. Invest.Ophthalmol.Vis.Sci. 2008;49:528–533. doi: 10.1167/iovs.07-1036. [DOI] [PubMed] [Google Scholar]
- 57.Haymes SA, Leblanc RP, Nicolela MT, et al. Risk of falls and motor vehicle collisions in glaucoma. Invest.Ophthalmol.Vis.Sci. 2007;48:1149–1155. doi: 10.1167/iovs.06-0886. [DOI] [PubMed] [Google Scholar]
- 58.Bramley T, Peeples P, Walt JG, et al. Impact of vision loss on costs and outcomes in medicare beneficiaries with glaucoma. Arch.Ophthalmol. 2008;126:849–856. doi: 10.1001/archopht.126.6.849. [DOI] [PubMed] [Google Scholar]
- 59.Colon-Emeric CS, Biggs DP, Schenck AP, Lyles KW. Risk factors for hip fracture in skilled nursing facilities: who should be evaluated? Osteoporos.Int. 2003;14:484–489. doi: 10.1007/s00198-003-1384-5. [DOI] [PubMed] [Google Scholar]
- 60.West SK, Rubin GS, Broman AT, et al. How does visual impairment affect performance on tasks of everyday life? The SEE Project. Salisbury Eye Evaluation. Arch Ophthalmol. 2002;120:774–780. doi: 10.1001/archopht.120.6.774. [DOI] [PubMed] [Google Scholar]
- 61.Sherwood MB, Garcia-Siekavizza A, Meltzer MI, et al. Glaucoma's impact on quality of life and its relation to clinical indicators. A pilot study. Ophthalmology. 1998;105:561–566. doi: 10.1016/S0161-6420(98)93043-3. [DOI] [PubMed] [Google Scholar]
- 62.Foley DJ, Heimovitz HK, Guralnik JM, Brock DB. Driving life expectancy of persons aged 70 years and older in the United States. Am.J.Public Health. 2002;92:1284–1289. doi: 10.2105/ajph.92.8.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Freeman EE, Gange SJ, Munoz B, West SK. Driving status and risk of entry into long-term care in older adults. Am.J.Public Health. 2006;96:1254–1259. doi: 10.2105/AJPH.2005.069146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marottoli RA, Mendes de Leon CF, Glass TA, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J.Am.Geriatr.Soc. 1997;45:202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 65.Eberhard JW. Driving is transportation for most older adults. Geriatrics. 1998;Suppl 1:S53–S55. [PubMed] [Google Scholar]
- 66.Dellinger AM, Sehgal M, Sleet DA, Barrett-Connor E. Driving cessation: what older former drivers tell us. J.Am.Geriatr.Soc. 2001;49:431–435. doi: 10.1046/j.1532-5415.2001.49087.x. [DOI] [PubMed] [Google Scholar]
- 67.Evans L. Risk of fatality from physical trauma versus sex and age. J.Trauma. 1988;28:368–378. doi: 10.1097/00005373-198803000-00013. [DOI] [PubMed] [Google Scholar]
- 68.McGwin G, Jr, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest.Ophthalmol.Vis.Sci. 2005;46:4437–4441. doi: 10.1167/iovs.05-0750. [DOI] [PubMed] [Google Scholar]
- 69.Haymes SA, Leblanc RP, Nicolela MT, et al. Risk of falls and motor vehicle collisions in glaucoma. Invest.Ophthalmol.Vis.Sci. 2007;48:1149–1155. doi: 10.1167/iovs.06-0886. [DOI] [PubMed] [Google Scholar]
- 70.Hu PS, Trumble DA, Foley DJ, et al. Crash risks of older drivers: a panel data analysis. Accid.Anal.Prev. 1998;30:569–581. doi: 10.1016/s0001-4575(98)00019-0. [DOI] [PubMed] [Google Scholar]
- 71.McGwin G, Jr, Mays A, Joiner W, et al. Is glaucoma associated with motor vehicle collision involvement and driving avoidance? Invest.Ophthalmol.Vis.Sci. 2004;45:3934–3939. doi: 10.1167/iovs.04-0524. [DOI] [PubMed] [Google Scholar]
- 72.Bechetoille A, Arnould B, Bron A, et al. Measurement of health-related quality of life with glaucoma: validation of the Glau-QoL(c) 36-item questionnaire. Acta Ophthalmol.Scand. 2007 doi: 10.1111/j.1600-0420.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 73.Gilhotra JS, Mitchell P, Ivers R, Cumming RG. Impaired vision and other factors associated with driving cessation in the elderly: the Blue Mountains Eye Study. Clin.Experiment.Ophthalmol. 2001;29:104–107. doi: 10.1046/j.1442-9071.2001.00411.x. [DOI] [PubMed] [Google Scholar]
- 74.Adler G, Bauer MJ, Rottunda S, Kuskowski M. Driving habits and patterns in older men with glaucoma. Soc.Work Health Care. 2005;40:75–87. doi: 10.1300/J010v40n03_05. [DOI] [PubMed] [Google Scholar]
- 75. Haymes SA, LeBlanc RP, Nicolela MT, et al. Glaucoma and on-road driving performance. Invest.Ophthalmol.Vis.Sci. 2008;49:3035–3041. doi: 10.1167/iovs.07-1609. * Directly examined subjects with and without glaucoma in on-road driving.
- 76.Szlyk JP, Taglia DP, Paliga J, et al. Driving performance in patients with mild to moderate glaucomatous clinical vision changes. J.Rehabil.Res.Dev. 2002;39:467–482. [PubMed] [Google Scholar]
- 77.Wilson MR, Coleman AL, Yu F, et al. Functional status and well-being in patients with glaucoma as measured by the Medical Outcomes Study Short Form-36 questionnaire. Ophthalmology. 1998;105:2112–2116. doi: 10.1016/S0161-6420(98)91135-6. [DOI] [PubMed] [Google Scholar]
- 78.Wilson MR, Coleman AL, Yu F, et al. Depression in patients with glaucoma as measured by self-report surveys. Ophthalmology. 2002;109:1018–1022. doi: 10.1016/s0161-6420(02)00993-4. [DOI] [PubMed] [Google Scholar]
- 79.Odberg T, Jakobsen JE, Hultgren SJ, Halseide R. The impact of glaucoma on the quality of life of patients in Norway. I. Results from a self-administered questionnaire. Acta Ophthalmol.Scand. 2001;79:116–120. doi: 10.1034/j.1600-0420.2001.079002116.x. [DOI] [PubMed] [Google Scholar]