Abstract
Intolerance of uncertainty (IU), or the increased affective response to situations with uncertain outcomes, is an important component process of anxiety disorders. Increased IU is observed in panic disorder (PD), obsessive compulsive disorder (OCD) and generalized anxiety disorder (GAD), and is thought to relate to dysfunctional behaviors and thought patterns in these disorders. Identifying what brain systems are associated with IU would contribute to a comprehensive model of anxiety processing, and increase our understanding of the neurobiology of anxiety disorders. Here, we used a behavioral task, Wall of Faces (WOF), during functional magnetic resonance imaging (fMRI), which probes both affect and ambiguity, to examine the neural circuitry of IU in fourteen (10 females) college age (18.8 yrs) subjects. All subjects completed the Intolerance of Uncertainty Scale (IUS), Anxiety Sensitivity Index (ASI), and a measure of neuroticism (i.e. the NEO-N). IUS scores but neither ASI nor NEO-N scores, correlated positively with activation in bilateral insula during affective ambiguity. Thus, the experience of IU during certain types of emotion processing may relate to the degree to which bilateral insula processes uncertainty. Previously observed insula hyperactivity in anxiety disorder individuals may therefore be directly linked to altered processes of uncertainty.
INTRODUCTION
Anxiety disorders, the most common type of mental illness in the United States [27], profoundly impact quality of life [35] and can lead to other mental disorders such as depression [2, 20]. Both behavioral and functional neuroimaging studies have shown that subjects with various anxiety disorders processing emotionally ambiguous information differently than do healthy subjects [23]. Ambiguity processing involves evaluation of complex stimuli, leading to uncertainty about the classification of these stimuli. This process has been hypothesized to play a critical role in anxiety disorders [23].
Intolerance of uncertainty (IU) has been defined as stress, discomfort, and avoidance induced by uncertainty [6]. An greater IU has been associated with anxiety disorders – notably obsessive compulsive disorder (OCD) and generalized anxiety disorder (GAD), and may be an important component process underlying the pathological thinking and behavior in these individuals as they attempt to gain control over perceived aversive conditions [7, 21, 26, 53]. Individuals with increased anxiety often experience heightened subjective stress during situations when error is possible. For example, previous investigations reveal that anxious individuals [24, 39, 49] show altered biases when attempting to disambiguate affective information. In one study, OCD checkers had greater IU than both OCD non-checkers and non-anxious controls [53]. In another study, IU was positively associated with pathological worry [21], a finding that is consistent with the notion that worry may function as a means of avoiding aversive somatic arousal, images, thoughts, and/or emotions [3]. Despite these studies, relatively little is known about the neural circuitry involved in IU. Identifying the neural substrates of IU may provide therapeutic targets for anxiolytic therapies that can decrease morbidity in patients suffering from anxiety disorders.
Neuroimaging research has shown that altered functional status of the amygdala [4, 25, 42, 45, 50, 52], medial prefrontal gyrus (MPFG) and anterior cingulate cortex (ACC) [1, 19, 39, 44, 49] and insula [38, 46, 57] are critically involved in affective processing in individuals with anxiety disorders and those with anxious personality types. The MPFG and ACC support important cognitive processes such as response inhibition and error monitoring [9, 32–34, 54], and are critically involved in making classification decisions about complex ambiguous stimuli [37, 47]. In comparison, insula function has been described as processing how the value of stimuli might affect the body state (or interoception). In particular, the anterior insular cortex provides information about future aversive body states associated with conditional stimuli, and relays this information to brain areas that are critical for the allocation of attention and the execution of actions [40].
In a prior study [47], we designed a Wall of Faces task (WOF) to examine the neural substrates underlying ambiguity processing, and found that healthy volunteers exhibited increased activation in the ventral ACC when processing stimuli that contained groups of affective faces with no predominant affect (i.e., ambiguous affective stimuli) relative to stimuli that contained groups of faces with no predominant gender (i.e., ambiguous gender stimuli). Increased activation in the dorsal ACC related to processing all ambiguous sets (i.e., both gender and affective sets) was also observed [47]. The activation pattern observed when subjects determine the predominant affect of an ambiguous group of faces was very similar to activation seen in other ambiguous facial expression tasks, such as ambiguous morphed or composite faces [37, 56]. The benefit of this design in the context of IU is that we can parametrically modulate the probability that the selected response is incorrect, by providing an ambiguous response set. As the ambiguity of the stimulus set increases, so does the likelihood of error, which is a negative outcome. We hypothesized that trials with a greater likelihood of an uncertain outcome would be more distressing to those with higher reported IU. If the ambiguous set is related to social or emotional context this has greater ecological validity as those individuals with greater anxiety and IU are often more agitated by affective than cognitive aspects of a situation. As the MFPC, insula, and amygdala appear important for affectively processing the ambiguity and uncertain outcome we hypothesized that individuals with greater intolerance of uncertainty would exhibit relatively greater activation in these structures.
METHODS AND MATERIALS
Subjects
This study was approved by the University of California San Diego (UCSD) and San Diego State University (SDSU) Institutional Review Boards and all subjects provided written informed consent to participate. Fourteen subjects were studied (10 females) with an average age of 18.8 years +/− 0.7 (range 18–20) and an average education level of 13.4 +/− 0.5 years (range 13–14). Subjects consumed less than 400 mg of caffeine daily. All subjects were trained on the task prior to fMRI. Subjects were paid to participate. All subjects completed the Intolerance of Uncertainty Scale (IUS) [6] (27 items; scores can range from 27–135); Anxiety Sensitivity Index (ASI) [43] (16 items; scores can range from 0 to 64), and a multifactor personality measure, NEO-PIR [11] from which the neuroticism facet (NEO-N) (subscale of 240 items; t-scores with mean of 50 and standard deviation of 15) was considered in analyses.
Subjects completed the Structured Clinical Interview for DSM-IV (SCID) [22] in order to establish the presence or absence of current and lifetime psychiatric diagnoses. No subjects had substance dependence, they were not seeking treatment and none were taking psychiatric medications. Four individuals had psychiatric diagnoses: Major Depression Disorder (n=2), GAD (n=1), or both (n=1).
Procedure
During each trial of the Wall of Faces (WOF) task [47] the subject sees an array of 32 faces from a standardized set [31] against a black background for 3 seconds and is instructed to decide whether more faces were “Angry or Happy” (affective trials) or whether more faces were “Female or Male” (gender trials) by pressing the LEFT or RIGHT button, respectively. The options “Angry or Happy” or “Male or Female” remained on the screen for 4.5 seconds. Four trial types (i.e. ambiguous affective, ambiguous gender, unambiguous affective and unambiguous gender) were presented, based on the ratio of angry to happy or male to female faces (see supplementary information). The response (LEFT or RIGHT button) and the response latency were recorded for each trial (see supplementary information).
FMRI analysis pathway
The data were preprocessed and analyzed with the software AFNI [12]. The echoplanar images were realigned to a central slice, time-corrected for slice acquisition order, and normalized to Talairach coordinates. The preprocessed time series data for each individual were analyzed using a multiple regression model consisting of 11 regressors. There were 6 task-related regressors, which identified the time-series for the three ratios (6/26, 16/16, and 26/6) of gender (female-male) and emotion (angry-happy). Each regressor was created using a reference function corresponding to the 3 seconds during a trial during which subjects viewed the array of faces. These regressors were convolved with a prototypical hemodynamic response function prior to inclusion in the regression model. In addition, three regressors were used to account for residual motion (in the roll, pitch, and yaw direction), and a baseline regressor and linear trends regressor were used to eliminate slow signal drifts. A 6 mm full-width half-maximum Gaussian filter was applied to the voxel-wise percent signal change data to account for individual variations of anatomical landmarks.
Initially, a whole brain analysis was preformed. It was determined via simulations that a voxel-wise a-priori probability of 0.05 would result in a corrected cluster-wise activation probability of 0.05 if a minimum volume of 1408 μl and 22 connected voxels. In addition, a priori analysis of regions of interest (ROIs) was conducted using masks (defined by the AFNI Talairach Atlas) [28] in the bilateral amygdala, insula, and ventromedial prefrontal cortex (vmPFC). Based on these areas of interests, it was determined via simulations that a voxel-wise a-priori probability of 0.05 would be retained within the ROIs if a minimum volume of 128 μl (in the amygdala) or 512 μl (in all other ROIs) was used. Only activations within the areas of interest, which also satisfied the volume and voxel connection criteria were extracted and used for further analysis. The corrected voxel-wise probabilities are: amygdala p < 0.012, insular cortex p < 0.00006859, and medial prefrontal cortex p < 0.00014493.
Statistical Analyses
To measure the contribution of IU to brain activation during affective uncertainty voxel-based correlations were calculated between IUS and ambiguous affective minus ambiguous gender trials using the AFNI program 3dRegAna. Similar analyses were also performed with the ASI and NEO-N.
Behavioral analyses were carried out with SPSS 10.0 (Norusis MJ, 1990). Simple t-tests were used to measure the task effects and a mixed model ANOVA (fixed factors: task conditions (gender versus affect; ambiguous versus non-ambiguous), random factor: subjects) was used to analyze differences in the behavioral measures.
RESULTS
Behavioral Findings
The ratio of angry or happy and of male or female faces significantly affected response latency (F(2,11)=15.983, p<.001 and F(2,11)=93.204, p<.0001, respectively) such that ambiguous ratios (i.e., 16/16) resulted in significantly longer response latencies than unambiguous ratios (i.e., 6/26 or 26/6) in both emotional and gender contrasts (t(12)= 3.963, p<.005, and t(12)=3.759, p<.005, respectively; see supplemental Figure 1). In comparison, there was no difference in response latency between affective or gender trials (F(2,11)=.761, NS and F(2,11)=.394, NS, respectively). Finally, the degree to which the ratio of affect or gender affected response latency did not differ across trial types, i.e., there was no significant interaction between trial type and ratio (F(2,11)=1.191, NS and F(2,11)=.159, NS, respectively). The degree of inter-correlation between personality measures (IUS, NEO, and ASI) was calculated (see supplemental Table 1).
Functional Neuroimaging Findings
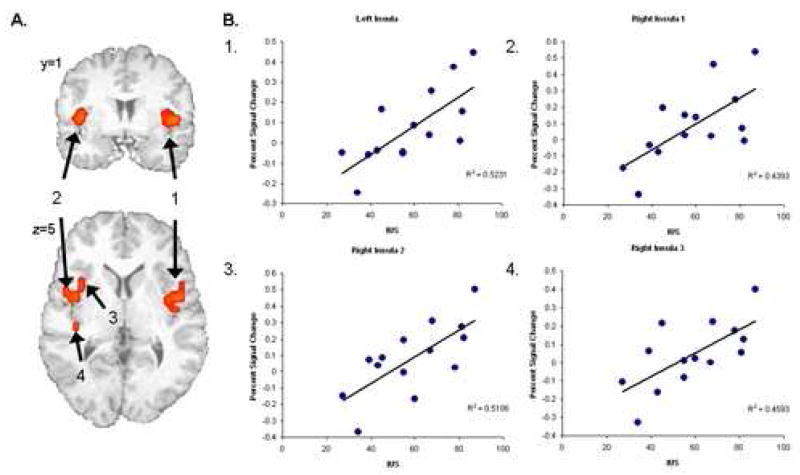
Based on prior research [47] the contrast of primary interest was ambiguous affective trials versus ambiguous gender trials. An initial whole brain analysis found the activation during this contrast correlated significantly with IUS in several regions including posterior cingulate, left insula, right superior temporal gyrus, and right putamen (correlating at r values ranging from .71-.82; see supplemental Table 2). The ROI analysis found significant surviving clusters of activation in the bilateral insula correlating with IUS at r values ranging from 0.66–0.72 (see Figure 2, p > .01). There was a significant correlation between the NEO-N and one of the right insula clusters (r=.554, p<.05) that did not survive when taking into account the multiple comparisons, and no other correlations with NEO-N or ASI neared significance (see Table 1). There was no significant correlation between behavior on the task (response latency and response selection) and activation in the resulting clusters. There were no significant correlations between task performance and anxiety or personality measures (IUS, ASI, and NEO-N). Correlations between other functional contrasts and the acquired ROI were calculated (see supplemental Table 3). Several post-hoc analyses were completed to better delineate the relationship between IUS, NEO-N and insula activation (see supplementary information).
Table 1.
Locations and correlations of Insula Activation during Amgbiguous Affect –Ambiguous Gender with Intolerance of Uncertainty Scale (IUS), Anxiety Sensitivity Index (ASI), and a measure of neuroticism (NEO-N).
| Location | Volume | x | y | z | IUS | NEON | ASI |
|---|---|---|---|---|---|---|---|
| Left Insula | 2304 | −40 | −1 | 5 | 0.723*** | 0.414 | 0.420 |
| Right Insula (#1) | 1088 | 40 | 1 | 6 | 0.663** | 0.441 | 0.208 |
| Right Anterior Insula (#2) | 576 | 33 | 12 | 6 | 0.715*** | 0.558* | 0.369 |
| Right Posterior Insula (#3) | 256 | 38 | −16 | 10 | 0.678** | 0.320 | 0.363 |
Note. = p>.05,
= p>.01,
= p>.005.
DISCUSSION
This investigation yielded four main findings. First, the activation during affective uncertainty was significantly related to IU in several regions including posterior cingulate, left insula, right superior temporal gyrus, and right putamen. Second, by using an ROI analysis, we were able to identify several specific subregions within the insula that displayed significant correlations with IU. Third, no clusters of activation were identified which significantly covaried with scores on the ASI or NEO-N. Fourth, behavioral performance did not correlate with activation in the insula or with performance on the IUS. These findings are consistent with the hypothesis that insula activation during an ambiguous situation is related to the degree to which uncertainty is processed as being aversive, further confirming the role of this structure in uncertainty processing and anxiety [40].
Altered insula activation has been observed in numerous anxiety disorders [41]. Social phobia patients have shown increased activation during a public speaking task [29], specific phobia subjects have shown increased response to fearful faces [57], OCD patients have shown more activation with greater contamination/washing symptoms [30], and GAD patients have shown reduced activation due to effect treatment with citalopram [55]. In addition, we found that non-treatment seeking young adults with high trait anxiety had greater activation in the insula when matching emotional faces [51] and during anticipation of a negative image [48]. The insula has also been conceptualized as a key area for processing one’s own physiological state [13, 14, 18, 48, 51]. Insula response has shown sensitivity to changes in heart rate [15, 17] and galvanic skin response [16, 36], as well as vagus nerve stimulation [10]. Some anxiety reactions, such as worry or IU, conceptually link physiological and affective processing. The current study adds to the existing literature by relating the subjective degree of aversion related to uncertainty to the degree of insula activation during the processing of ambiguous situations. Moreover, the current findings help to explain the link between neuroticism and insula activation, because individuals with high neuroticism have been shown to also exhibit high IUS scores. It is important to note that it is not uncertainty per se but affective uncertainty that relates to activation in the bilateral insula. If the proposed insula function of a prediction signal indicating the possibility of future aversive interoception is correct, then IUS may quantify the magnitude of such a prediction signal, which, in turn, results in the initiation of behavioral responses aimed at reducing this signal. Future investigations should examine this model further by delineating whether affectively uncertain stimuli, relative to other types of ambiguous stimuli, differentially influence insular cortex activity.
While the findings within the insula was the main focus of this research a whole brain analysis was performed as this was the first report on the relationship of IU with brain functioning. This revealed that beyond the insula several regions such as the posterior cingulate, superior temporal gyrus, and putamen related to IU during affective uncertainty. It may be that these areas are indicative of heightened arousal as all three have been shown to be related to attention and arousal networks in prior literature [5, 8]. However, additional research is required to explain a link between these areas and affectively driven homeostatic systems.
A notable limitation should be considered in the interpretation of these data. In this study, our aim was to assess the full spectrum of IU, by using this measure as a continuous variable. This approach is optimal for examining the neural substrates of IU. However, these findings require replication in samples of individuals with PD, GAD, or OCD before extrapolation can be made to these clinical conditions.
The process of making judgments of an ambiguous affective stimulus appears to be instantiated within a specific neural substrate. This relationship between IU and insula activation is consistent with prior literature in that the insula appears important in monitoring changes in physiological status or homeostasis and IU is itself a hallmark of the inability of patients with anxiety disorders to tolerate the sensations that are evoked by ambiguous situations. Discomfort with ambiguous affective judgments is especially characteristic of patients with certain anxiety disorders such as GAD [21], raising the possibility that insular dysfunction may be more prominent in some anxiety disorders than others. This hypothesis can be tested in future studies that compare insular function across patients with different anxiety disorders during various types of emotion processing. Such information would contribute to a comprehensive neural systems-based classification of anxiety disorders.
Supplementary Material
Figure 1.
Correlations of Insula Activation during during Amgbiguous Affect –Ambiguous Gender with Intolerance of Uncertainty Scale (IUS). Four Regions in the Insula survived masking (A) with significant clusters of correlation with IUS (B).
Acknowledgments
We would like to acknowledge the invaluable help of Carla Hitchcock. This work was supported by grants from NIMH (MH65413, MBS), support from the Veterans Administration via Merit Grants (MPP and MBS), and an NIH training grant (5T32MH18399: ANS and SCM).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bishop S, Duncan J, Brett M, Lawrence AD. Prefrontal cortical function and anxiety: controlling attention to threat-related stimuli. Nat Neurosci. 2004 doi: 10.1038/nn1173. [DOI] [PubMed] [Google Scholar]
- 2.Bittner A, Goodwin RD, Wittchen HU, Beesdo K, Hofler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? J Clin Psychiatry. 2004;65:618–626. doi: 10.4088/jcp.v65n0505. quiz. [DOI] [PubMed] [Google Scholar]
- 3.Borkovec TD, Lyonfields JD, Wiser SL, Deihl L. The role of worrisome thinking in the suppression of cardiovascular response to phobic imagery. Behav Res Ther. 1993;31:321–324. doi: 10.1016/0005-7967(93)90031-o. [DOI] [PubMed] [Google Scholar]
- 4.Breiter HC, Etcoff NL, Whalen PJ, Kennedy WA, Rauch SL, Buckner RL, Strauss MM, Hyman SE, Rosen BR. Response and habituation of the human amygdala during visual processing of facial expression. Neuron. 1996;17:875–887. doi: 10.1016/s0896-6273(00)80219-6. [DOI] [PubMed] [Google Scholar]
- 5.Britton JC, Phan KL, Taylor SF, Welsh RC, Berridge KC, Liberzon I. Neural correlates of social and nonsocial emotions: An fMRI study. NeuroImage. 2006 doi: 10.1016/j.neuroimage.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 6.Buhr K, Dugas MJ. The Intolerance of Uncertainty Scale: psychometric properties of the English version. Behav Res Ther. 2002;40:931–945. doi: 10.1016/s0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- 7.Buhr K, Dugas MJ. Investigating the construct validity of intolerance of uncertainty and its unique relationship with worry. J Anxiety Disord. 2006;20:222–236. doi: 10.1016/j.janxdis.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 8.Cabeza R, Nyberg L. Imaging cognition II. Journal of Cognitive Neuroscience. 2000;12:1–47. doi: 10.1162/08989290051137585. [DOI] [PubMed] [Google Scholar]
- 9.Carter CS, Botvinick MM, Cohen JD. The contribution of the anterior cingulate cortex to executive processes in cognition. Rev Neurosci. 1999;10:49–57. doi: 10.1515/revneuro.1999.10.1.49. [DOI] [PubMed] [Google Scholar]
- 10.Conway CR, Sheline YI, Chibnall JT, George MS, Fletcher JW, Mintun MA. Cerebral blood flow changes during vagus nerve stimulation for depression. Psychiatry Res. 2006;146:179–184. doi: 10.1016/j.pscychresns.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Costa PT, Jr, McCrae RR. Overview: innovations in assessment using the revised NEO personality inventory. Assessment. 2000;7:325–327. doi: 10.1177/107319110000700402. [DOI] [PubMed] [Google Scholar]
- 12.Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res. 1996;29:162–173. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- 13.Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13:500–505. doi: 10.1016/s0959-4388(03)00090-4. [DOI] [PubMed] [Google Scholar]
- 14.Critchley HD. The human cortex responds to an interoceptive challenge. Proc Natl Acad Sci USA. 2004;101:6333–6334. doi: 10.1073/pnas.0401510101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Critchley HD, Corfield DR, Chandler MP, Mathias CJ, Dolan RJ. Cerebral correlates of autonomic cardiovascular arousal: a functional neuroimaging investigation in humans. J Physiol. 2000;523(Pt 1):259–270. doi: 10.1111/j.1469-7793.2000.t01-1-00259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Critchley HD, Elliott R, Mathias CJ, Dolan RJ. Neural activity relating to generation and representation of galvanic skin conductance responses: a functional magnetic resonance imaging study. J Neurosci. 2000;20:3033–3040. doi: 10.1523/JNEUROSCI.20-08-03033.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Critchley HD, Rotshtein P, Nagai Y, O’Doherty J, Mathias CJ, Dolan RJ. Activity in the human brain predicting differential heart rate responses to emotional facial expressions. NeuroImage. 2005;24:751–762. doi: 10.1016/j.neuroimage.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Critchley HD, Wiens S, Rotshtein P, Ohman A, Dolan RJ. Neural systems supporting interoceptive awareness. Nat Neurosci. 2004;7:189–195. doi: 10.1038/nn1176. [DOI] [PubMed] [Google Scholar]
- 19.Davidson RJ. Anxiety and affective style. Biological Psychiatry. 2002;51:68–80. doi: 10.1016/s0006-3223(01)01328-2. [DOI] [PubMed] [Google Scholar]
- 20.de Graaf R, Bijl RV, Spijker J, Beekman AT, Vollebergh WA. Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders--findings from the Netherlands Mental Health Survey and Incidence Study. Soc Psychiatry Psychiatr Epidemiol. 2003;38:1–11. doi: 10.1007/s00127-003-0597-4. [DOI] [PubMed] [Google Scholar]
- 21.Dugas MJ, Ladouceur R. Treatment of GAD. Targeting intolerance of uncertainty in two types of worry. Behav Modif. 2000;24:635–657. doi: 10.1177/0145445500245002. [DOI] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams JBW, editors. Structured Clinical Interview for DSM-IV Axis I Disorders - Clinician Version (SCID-1) American Psychiatric Press, Inc.; Washington, D.C.: 1997. [Google Scholar]
- 23.Gilboa-Schechtman E, Presburger G, Marom S, Hermesh H. The effects of social anxiety and depression on the evaluation of facial crowds. Behav Res Ther. 2005;43:467–474. doi: 10.1016/j.brat.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez-Bono E, Moya-Albiol L, Salvador A, Carrillo E, Ricarte J, Gomez-Amor J. Anticipatory autonomic response to a public speaking task in women: the role of trait anxiety. Biol Psychol. 2002;60:37–49. doi: 10.1016/s0301-0511(02)00008-x. [DOI] [PubMed] [Google Scholar]
- 25.Hariri AR, Mattay VS, Tessitore A, Kolachana B, Fera F, Goldman D, Egan MF, Weinberger DR. Serotonin transporter genetic variation and the response of the human amygdala. Science. 2002;297:400–403. doi: 10.1126/science.1071829. [DOI] [PubMed] [Google Scholar]
- 26.Holaway RM, Heimberg RG, Coles ME. A comparison of intolerance of uncertainty in analogue obsessive-compulsive disorder and generalized anxiety disorder. J Anxiety Disord. 2006;20:158–174. doi: 10.1016/j.janxdis.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L, Kochunov PV, Nickerson D, Mikiten SA, Fox PT. Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp. 2000;10:120–131. doi: 10.1002/1097-0193(200007)10:3<120::AID-HBM30>3.0.CO;2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lorberbaum JP, Kose S, Johnson MR, Arana GW, Sullivan LK, Hamner MB, Ballenger JC, Lydiard RB, Brodrick PS, Bohning DE, George MS. Neural correlates of speech anticipatory anxiety in generalized social phobia. Neuroreport. 2004;15:2701–2705. [PubMed] [Google Scholar]
- 30.Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive-compulsive disorder. Arch Gen Psychiatry. 2004;61:564–576. doi: 10.1001/archpsyc.61.6.564. [DOI] [PubMed] [Google Scholar]
- 31.Matsumoto D, Ekman P. Japanese and Caucasian facial expressions of emotion (JACFEE) and neutral faces (JACNeuF) San Francisco State University; San Francisco: 1998. [Google Scholar]
- 32.Matthews SC, Simmons AN, Arce E, Paulus MP. Dissociation of inhibition from error processing using a parametric inhibitory task during functional magnetic resonance imaging. Neuroreport. 2005;16:755–760. doi: 10.1097/00001756-200505120-00020. [DOI] [PubMed] [Google Scholar]
- 33.Mayberg HS. Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry Clin Neurosci. 1997;9:471–481. doi: 10.1176/jnp.9.3.471. [DOI] [PubMed] [Google Scholar]
- 34.Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, Schwalb JM, Kennedy SH. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–660. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 35.Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. The American journal of psychiatry. 2000;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- 36.Nagai Y, Critchley HD, Featherstone E, Trimble MR, Dolan RJ. Activity in ventromedial prefrontal cortex covaries with sympathetic skin conductance level: a physiological account of a “default mode” of brain function. NeuroImage. 2004;22:243–251. doi: 10.1016/j.neuroimage.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 37.Nomura M, Iidaka T, Kakehi K, Tsukiura T, Hasegawa T, Maeda Y, Matsue Y. Frontal lobe networks for effective processing of ambiguously expressed emotions in humans. Neurosci Lett. 2003;348:113–116. doi: 10.1016/s0304-3940(03)00768-7. [DOI] [PubMed] [Google Scholar]
- 38.Paulus MP, Feinstein JS, Castillo G, Simmons AN, Stein MB. Dose-dependent decrease of activation in bilateral amygdala and insula by lorazepam during emotion processing. Arch Gen Psychiatry. 2005;62:282–288. doi: 10.1001/archpsyc.62.3.282. [DOI] [PubMed] [Google Scholar]
- 39.Paulus MP, Feinstein JS, Simmons A, Stein MB. Anterior cingulate activation in high trait anxious subjects is related to altered error processing during decision making. Biol Psychiatry. 2004;55:1179–1187. doi: 10.1016/j.biopsych.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 40.Paulus MP, Stein MB. An insular view of anxiety. Biol Psychiatry. 2006;60:383–387. doi: 10.1016/j.biopsych.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 41.Rauch SL, Savage CR, Alpert NM, Fischman AJ, Jenike MA. The functional neuroanatomy of anxiety: a study of three disorders using positron emission tomography and symptom provocation. Biol Psychiatry. 1997;42:446–452. doi: 10.1016/S0006-3223(97)00145-5. [DOI] [PubMed] [Google Scholar]
- 42.Rauch SL, Shin LM, Wright CI. Neuroimaging studies of amygdala function in anxiety disorders. Ann N Y Acad Sci. 2003;985:389–410. doi: 10.1111/j.1749-6632.2003.tb07096.x. [DOI] [PubMed] [Google Scholar]
- 43.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 44.Shin LM, Whalen PJ, Pitman RK, Bush G, Macklin ML, Lasko NB, Orr SP, McInerney SC, Rauch SL. An fMRI study of anterior cingulate function in posttraumatic stress disorder. Biol Psychiatry. 2001;50:932–942. doi: 10.1016/s0006-3223(01)01215-x. [DOI] [PubMed] [Google Scholar]
- 45.Shin LM, Wright CI, Cannistraro PA, Wedig MM, McMullin K, Martis B, Macklin ML, Lasko NB, Cavanagh SR, Krangel TS, Orr SP, Pitman RK, Whalen PJ, Rauch SL. A functional magnetic resonance imaging study of amygdala and medial prefrontal cortex responses to overtly presented fearful faces in posttraumatic stress disorder. Arch Gen Psychiatry. 2005;62:273–281. doi: 10.1001/archpsyc.62.3.273. [DOI] [PubMed] [Google Scholar]
- 46.Simmons A, Matthews SC, Stein MB, Paulus MP. Anticipation of emotionally aversive visual stimuli activates right insula. Neuroreport. 2004;15:2261–2265. doi: 10.1097/00001756-200410050-00024. [DOI] [PubMed] [Google Scholar]
- 47.Simmons A, Stein MB, Matthews SC, Feinstein JS, Paulus MP. Affective ambiguity for a group recruits ventromedial prefrontal cortex. NeuroImage. 2006;29:655–661. doi: 10.1016/j.neuroimage.2005.07.040. [DOI] [PubMed] [Google Scholar]
- 48.Simmons A, Strigo I, Matthews SC, Paulus MP, Stein MB. Anticipation of aversive visual stimuli is associated with increased insula activation in anxiety-prone subjects. Biol Psychiatry. 2006;60:402–409. doi: 10.1016/j.biopsych.2006.04.038. [DOI] [PubMed] [Google Scholar]
- 49.Simpson JR, Jr, Drevets WC, Snyder AZ, Gusnard DA, Raichle ME. Emotion-induced changes in human medial prefrontal cortex: II. During anticipatory anxiety. Proc Natl Acad Sci USA. 2001;98:688–693. doi: 10.1073/pnas.98.2.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stein MB, Goldin PR, Sareen J, Zorrilla LT, Brown GG. Increased amygdala activation to angry and contemptuous faces in generalized social phobia. Arch Gen Psychiatry. 2002;59:1027–1034. doi: 10.1001/archpsyc.59.11.1027. [DOI] [PubMed] [Google Scholar]
- 51.Stein MB, Simmons AN, Feinstein JS, Paulus MP. Increased Amygdala and Insula Activation During Emotion Processing in Anxiety-Prone Subjects. Am J Psychiatry. 2007;164:318–327. doi: 10.1176/ajp.2007.164.2.318. [DOI] [PubMed] [Google Scholar]
- 52.Thomas KM, Drevets WC, Dahl RE, Ryan ND, Birmaher B, Eccard CH, Axelson D, Whalen PJ, Casey BJ. Amygdala response to fearful faces in anxious and depressed children. Arch Gen Psychiatry. 2001;58:1057–1063. doi: 10.1001/archpsyc.58.11.1057. [DOI] [PubMed] [Google Scholar]
- 53.Tolin DF, Abramowitz JS, Brigidi BD, Foa EB. Intolerance of uncertainty in obsessive-compulsive disorder. J Anxiety Disord. 2003;17:233–242. doi: 10.1016/s0887-6185(02)00182-2. [DOI] [PubMed] [Google Scholar]
- 54.van Veen V, Carter CS. The anterior cingulate as a conflict monitor: fMRI and ERP studies. Physiol Behav. 2002;77:477–482. doi: 10.1016/s0031-9384(02)00930-7. [DOI] [PubMed] [Google Scholar]
- 55.Willour VL, Yao SY, Samuels J, Grados M, Cullen B, Bienvenu OJ, III, Wang Y, Liang KY, Valle D, Hoehn-Saric R, Riddle M, Nestadt G. Replication study supports evidence for linkage to 9p24 in obsessive-compulsive disorder. Am J Hum Genet. 2004;75:508–513. doi: 10.1086/423899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Winston JS, O’Doherty J, Dolan RJ. Common and distinct neural responses during direct and incidental processing of multiple facial emotions. Neuroimage. 2003;20:84–97. doi: 10.1016/s1053-8119(03)00303-3. [DOI] [PubMed] [Google Scholar]
- 57.Wright CI, Martis B, McMullin K, Shin LM, Rauch SL. Amygdala and insular responses to emotionally valenced human faces in small animal specific phobia. Biol Psychiatry. 2003;54:1067–1076. doi: 10.1016/s0006-3223(03)00548-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.