Abstract
Objectives
Two randomized Phase I studies in separate populations of healthy adult volunteers investigated the pharmacokinetics, safety and tolerability of daptomycin (Cubicin®; Novartis Pharma AG, Basel, Switzerland) administered as a 2 min intravenous (iv) injection, relative to the currently licensed 30 min iv infusion.
Methods
Study 1 was an open-label, single-dose, two-period, crossover study in which each subject received 6 mg/kg daptomycin administered as a 30 min iv infusion (n = 15) and as a 2 min iv injection (n = 16). In Study 2, a single-blind, multiple-dose, parallel-group study, subjects received a once-daily 2 min iv injection of 6 mg/kg daptomycin (n = 12), 4 mg/kg daptomycin (n = 8) or placebo (n = 4) for 7 days. Single-dose pharmacokinetics were assessed at various timepoints up to 36 and 24 h post-dose in Study 1 and Study 2, respectively, and multiple-dose pharmacokinetics were assessed in Study 2 at day 7 for 48 h post-dose.
Results
In Study 1, pharmacokinetic comparability between the two administration regimens was demonstrated by meeting the bioequivalence criteria for the exposure parameters, AUC0–t, AUC0–∞ and Cmax. In Study 2, time-invariant pharmacokinetic properties as well as dose-proportional pharmacokinetics were demonstrated for the daptomycin 2 min iv injection regimen. In both studies, daptomycin was well tolerated and the majority of treatment-emergent adverse events were of mild intensity and considered to be unrelated to daptomycin.
Conclusions
The similar pharmacokinetic and safety profiles of the two administration regimens suggest that the 2 min iv injection may be a convenient treatment option for both patients and healthcare professionals.
Keywords: open-label, crossover, antibiotic, Gram-positive, Staphylococcus aureus
Introduction
Daptomycin (Cubicin®; Novartis Pharma AG, Basel, Switzerland) is an antibacterial agent indicated for the treatment of complicated skin and soft tissue infections (cSSTIs) caused by susceptible strains of Gram-positive microorganisms. Additionally, daptomycin is approved for the treatment of Staphylococcus aureus bloodstream infections (bacteraemia), including those with right-sided infective endocarditis (RIE) in the USA, and in the European Union for RIE due to S. aureus and S. aureus bacteraemia when associated with RIE or with cSSTI.1,2
Daptomycin has rapid, concentration-dependent bactericidal activity against clinically relevant Gram-positive bacteria including methicillin-resistant S. aureus (MRSA). The potency of daptomycin against S. aureus has remained consistent throughout 7 years of surveillance studies (2001–2007) in both North America and Europe.3–9
The currently approved method of administration for daptomycin is as a once-daily 30 min intravenous (iv) infusion, and the efficacy, safety and pharmacokinetics of this dosing regimen have been established in healthy subjects10,11 as well as in patients with Gram-positive infections.12 In Phase III clinical trials, the majority of adverse events (AEs) experienced by patients were of mild or moderate intensity and not attributed to the study drug.13,14 Daptomycin pharmacokinetics are linear after the administration of single or multiple doses of up to 12 mg/kg by 30 min iv infusion, with a t1/2 of ∼8 h; steady state is reached by day 3, independent of dose.10 Daptomycin has a low volume of distribution (V; averaging ∼0.1 L/kg) and is 90–93% protein bound, independent of the daptomycin concentration.10 Renal excretion is the major elimination pathway; urinary recovery over a 24 h period ranges from ∼34% to ∼68% of the administered dose in healthy subjects.15–17
Administration of antibiotics by rapid injection is attractive because of advantages over infusion such as cost-effectiveness, greater flexibility in the management of fluid balance and suitability for administration as outpatient parenteral antibiotic therapy.18 This paper presents the results from two clinical studies that evaluated the pharmacokinetics, safety and tolerability of daptomycin administered as a 2 min iv injection, compared with a 30 min iv infusion in healthy adult volunteers.
Materials and methods
Study designs
Study 1 was a randomized, open-label, single-dose, two-period, crossover study. Each subject received 6 mg/kg daptomycin administered as a 30 min iv infusion and as a 2 min iv injection. The order of administration was randomized and each dose was separated by a washout period of 5 days.
Study 2 was a randomized, single-blind, multiple-dose, parallel-group, placebo-controlled study. Subjects were randomized in a 3:2:1 ratio to receive 6 mg/kg daptomycin, 4 mg/kg daptomycin or placebo administered as a 2 min iv injection once daily for 7 days.
For both studies, the 2 min iv injection was administered by peripheral iv administration using a Medex Medfusion 3010a (Medex Inc., Duluth, GA, USA) or equivalent syringe driver. The 30 min iv infusion was administered using a Graseby 500 Modular Infusion Pump (Smiths Medical International Ltd, Watford, UK).
Both studies were approved in the UK by the South Wales Research Ethics Committee and all study participants provided written informed consent. Studies were performed at Simbec Research Ltd, Merthyr Tydfil, South Wales, UK, and were conducted in accordance with the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use, good clinical practice and local regulatory requirements.
Study population
Healthy men and women, between 18 and 45 years of age, were eligible to participate in the study, provided they had an estimated CLCR rate >70 mL/min for Study 1 or >80 mL/min for Study 2 (based on the Cockcroft–Gault equation). The permitted body mass index was 20–30 kg/m2 (inclusive), with a permissible body weight of 50–80 kg for women and 60–90 kg for men. Female volunteers were required to have a negative serum pregnancy test result at screening and admission (day 1).
Subjects with any personal or family history of adverse drug reaction, hypersensitivity to daptomycin or drugs with a similar chemical structure or any serious allergy were excluded from the study. Additional exclusion criteria included serum creatine phosphokinase ≥1.5 of the upper limit of normal and any significant clinical or laboratory abnormality.
Pharmacokinetic analysis
Sample collection
Whole blood samples were collected into lithium heparin tubes. In Study 1, samples were collected before dosing, immediately after dosing and at 15 min, 30 min and 1, 1.5, 2, 4, 6, 8, 12, 24 and 36 h from the end of the dosing period. For subjects receiving the 30 min iv infusion, an additional sample was collected 15 min after the start of infusion.
In Study 2, blood samples were collected before dosing, immediately after dosing, at 15 and 30 min after the start of the 2 min iv injection and at 1, 2, 4, 6, 8, 12 and 24 h after the start of the injection on days 1 and 7. Additional samples were obtained at 36 and 48 h after the 2 min iv injection on day 7, and a trough sample was obtained before dosing on days 4 and 6. Urine samples were pooled from collections obtained pre-dosing and at the following intervals from the start of administration of the 2 min iv injection: 0–12 and 12–24 h on day 1; and 0–12, 12–24 and 24–48 h on day 7.
Plasma and urine daptomycin concentrations
Total plasma and urine daptomycin concentrations were analysed according to a validated HPLC detection method.11 The lower limit of quantification was 3 mg/L and the upper limit was 500 mg/L. The precision and sensitivity of these assays were within previously determined ranges.
Non-compartmental analysis
Relevant pharmacokinetic parameters (e.g. AUC, CL, Cmax, Tmax, t1/2 and V) for daptomycin were calculated using non-compartmental methods implemented in SAS® software (version 9.1, SAS Institute, Cary, NC, USA). The trapezoidal rule was used to calculate AUC from time zero to the last measurable concentration (AUC0–t). AUC0–∞ was estimated using the trapezoidal rule, with the terminal elimination rate constant (beta) being estimated using log-linear regression of the terminal segment of the concentration–time curve.
In Study 1, statistical analysis was carried out on log-transformed, dose-normalized pharmacokinetic parameters, using an ANOVA model suited to a two-period, two-treatment, two-sequence crossover design. Least square means were estimated and back transformed to provide point estimates and 95% confidence intervals (CIs) for the ratio of the 2 min iv injection to the 30 min iv infusion for each parameter. Period and sequence effects were evaluated at the two-sided 5% level.
In Study 2, analysis of accumulation ratio, dose proportionality, assessment of steady state and comparison of day 1 and day 7 pharmacokinetic parameters were carried out.
Compartmental analysis
Pharmacokinetic modelling used to describe the serum daptomycin concentrations was based on a two-compartment, linear disposition model. The population pharmacokinetic model was fitted using the first-order conditional estimation method with interaction, as implemented in NONMEM software (version V level 1.1).19
The parameters fitted were CL, central compartment volume of distribution (Vc), peripheral compartment volume of distribution (Vt), distribution clearance (CLd) and duration of infusion (D1). Individual pharmacokinetic parameters (e.g. CLi) were assumed to be log-normally distributed (the subscript i denotes the ith individual). The parameter was modelled as follows:
where θCL is the population mean clearance and ηiCLi are random effects reflecting the deviation of the logarithm of individual CL from the logarithm of the population mean value. ηiCLi was assumed to be normally distributed with mean zero and variance ωCL. Other pharmacokinetic parameters were similarly modelled. Inter-individual effects were assumed to be independent of each other.
Safety analysis
Treatment-emergent AEs included all AEs occurring after the first dose of study medication. AEs were categorized by the investigator as not related, unlikely to be related, possibly related or probably related to the study drug. The severity of each AE was also determined by the investigator as mild, moderate or severe. The final post-study follow-up took place between 1 and 11 days after the last dose of study medication for Study 1 and between 9 and 11 days after last dosing for Study 2.
Results
Study populations
Sixteen subjects (eight males) were enrolled in the single-dose (6 mg/kg) crossover study (Study 1). The mean age (±SD) was 26.3 ± 7.2 years, with a mean weight (±SD) of 71.98 ± 10.90 kg. Fifteen subjects were Caucasian and one was of mixed race. Fifteen subjects received both the 2 min iv injection and the 30 min iv infusion and did not experience any significant AEs. One subject received only the 2 min iv injection and was excluded from the safety analyses for the infusion and from all pharmacokinetic analyses (details in the safety analysis).
For Study 2, 24 subjects (21 males) were randomized to receive 6 mg/kg daptomycin (n = 12), 4 mg/kg daptomycin (n = 8) or placebo (n = 4) administered as a 2 min iv injection once daily for 7 days. All subjects were Caucasian. The mean age and weight (±SD) of subjects were: 29.3 ± 8.6 years and 74.79 ± 13.92 kg, respectively, for the 6 mg/kg daptomycin group; 27.8 ± 6.3 years and 81.99 ± 1.14 kg, respectively, for the 4 mg/kg daptomycin group; and 29.8 ± 7.3 years and 78.13 ± 6.60 kg, respectively, for the placebo group. The pharmacokinetic population consisted of the 20 subjects receiving daptomycin, and all subjects were included in the safety analyses.
Pharmacokinetic analysis
Comparison of the daptomycin 2 min iv injection and 30 min iv infusion (Study 1)
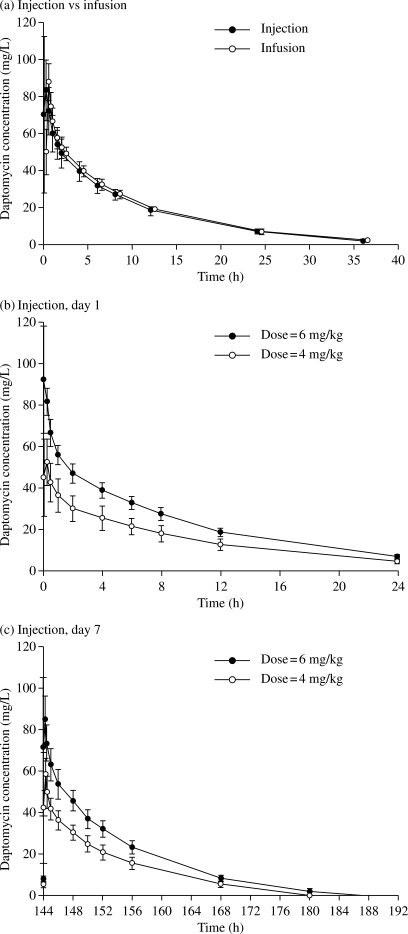
The mean plasma concentration–time profiles following a single 6 mg/kg dose of daptomycin were similar, whether daptomycin was administered as a 2 min iv injection or as a 30 min iv infusion (Figure 1a).
Figure 1.
Mean daptomycin concentration–time plots for daptomycin administered as a 2 min iv injection or as a 30 min iv infusion (Study 1; a), and following single and multiple doses of the daptomycin 2 min iv injection (Study 2; b and c). Data shown are means ± SD.
Pharmacokinetic parameters following administration of daptomycin as a 2 min iv injection or a 30 min iv infusion are summarized in Table 1. There were no significant differences in AUC or Cmax between the 2 min iv injection and the 30 min iv infusion of daptomycin, and all 95% CIs fell within the commonly used 80%–125% equivalence range. All other pharmacokinetic parameters were similar for the two regimens, including small values for mean V.
Table 1.
Comparison of pharmacokinetic parameters in healthy adult volunteers following a single 6 mg/kg dose of daptomycin administered as a 2 min iv injection relative to a 30 min iv infusion (Study 1)
| 2 min iv injection n = 15 mean (SD) | 30 min iv infusion n = 15 mean (SD) | 95% CI | |
|---|---|---|---|
| CL (L/h/kg) | 0.0089 (0.0012) | 0.0083 (0.0008) | NA |
| t1/2 (h) | 8.7 (1.0) | 8.7 (0.9) | NA |
| V (L/kg) | 0.113 (0.014) | 0.105 (0.012) | NA |
| Cmax (mg/L) | 94.7 (22.6) | 88.4 (12.4) | 0.9588–1.1719 |
| AUC0–t (mg·h/L) | 626.5 (103.4) | 669.6 (69.1) | 0.8709–1.0055 |
| AUC0–∞ (mg·h/L) | 691.4 (96.0) | 725.2 (63.3) | 0.9007–1.0117 |
AUC0–t, area under the plasma concentration–time curve from time zero to the last measurable concentration; NA, not applicable; V, volume of distribution based on the terminal phase.
The table shows the arithmetic means of non-transformed values, except for t1/2, where the harmonic mean is shown.
CIs are for the ratio of the geometric means derived from the ANOVA of log-transformed values.
Parameters were not dose-normalized.
Daptomycin pharmacokinetics following single and multiple doses of the 2 min iv injection (Study 2)
The mean plasma concentration–time profiles following single and multiple doses of the daptomycin 2 min iv injection are shown in Figure 1(b and c); individual pharmacokinetic parameter estimates are summarized in Table 2. Peak plasma concentrations were observed at the first or second sampling time (2 or 15 min after the start of the 2 min iv injection). Mean plasma concentration–time profiles for the 6 mg/kg daptomycin and 4 mg/kg daptomycin treatment groups were clearly separable. For each dose of daptomycin, all pharmacokinetic parameters were similar on day 1 and on day 7, with the exception of a small increase in Tmax on day 7 compared with day 1. Steady-state concentrations of daptomycin were achieved by the third daily dose for both treatment groups (data not shown).
Table 2.
Pharmacokinetic parameters following a single dose or multiple doses of the daptomycin 2 min iv injection in healthy adult volunteers (Study 2)
| Day 1 |
Day 7 |
|||
|---|---|---|---|---|
| daptomycin 6 mg/kg n = 12 mean (SD) | daptomycin 4 mg/kg n = 8 mean (SD) | daptomycin 6 mg/kg n = 12 mean (SD) | daptomycin 4 mg/kg n = 8 mean (SD) | |
| AUC0–∞ (mg·h/L) | 690.37 (68.83) | 468.40 (98.90) | NA | NA |
| AUC0–tau (mg·h/L) | NA | NA | 701.08 (81.96) | 475.24 (70.97) |
| Cmax (mg/L) | 97.49 (17.30) | 56.80 (8.32) | 91.83 (17.88) | 62.83 (11.31) |
| Tmax (h)a | 0.03 (0.03–0.25) | 0.14 (0.03–0.25) | 0.25 (0.03–0.25) | 0.25 (0.03–0.25) |
| t1/2 (h) | 8.43 (0.63) | 9.08 (0.94) | 8.65 (0.63) | 8.93 (1.05) |
| CL (L/h/kg) | 0.0088 (0.0009) | 0.0090 (0.0025) | 0.0087 (0.001) | 0.0086 (0.001) |
| V (L/kg) | 0.106 (0.011) | 0.116 (0.031) | 0.107 (0.011) | 0.109 (0.011) |
| %Fe0–tau | 56.74 (12.25) | 54.31 (12.30) | 65.06 (9.81) | 67.52 (12.66) |
AUC0–tau, area under the plasma concentration–time curve over the dosing interval; %Fe0–tau, percentage of daptomycin excreted unchanged in the urine over 24 h; NA, not applicable.
Means are arithmetic means of non-transformed values.
aMedian (range).
Single-dose pharmacokinetics (measured on day 1) and multiple-dose pharmacokinetics (measured on day 7) showed dose proportionality between the 6 mg/kg daptomycin and 4 mg/kg daptomycin doses. All 95% CIs, for the ratio of means of the pharmacokinetic parameters, fell within the 80%–125% equivalence range with the exception of dose-normalized Ae0–tau on days 1 and 7 and dose-normalized Cmax on day 1 (Table 3). For both treatment groups, CL was unchanged between day 1 and day 7. A small accumulation of daptomycin with repeated doses was indicated by the ratio, for day 1 versus day 7, of >1 for both AUC0–tau and Ae0–tau [Table S1, available as Supplementary data at JAC Online (http://jac.oxfordjournals.org/)].
Table 3.
Ratio of geometric mean pharmacokinetic parameters for the 6 mg/kg (n = 12) and 4 mg/kg (n = 8) doses of daptomycin administered as a 2 min iv injection to healthy adult volunteers (Study 2)
| Ratio of 6 mg/kg:4 mg/kg daptomycin (95% CI) |
||
|---|---|---|
| day 1 | day 7 | |
| AUC0–tau (dose-normalized) | 1.02 (0.87–1.2) | 0.99 (0.87–1.12) |
| CL | 1.00 (0.85–1.18) | 1.01 (0.9–1.15) |
| Cmax (dose-normalized) | 1.14 (0.97–1.3) | 0.97 (0.82–1.16) |
| Ae0–tau (dose-normalized) | 0.95 (0.72–1.25) | 0.88 (0.69–1.11) |
Ae0–tau, cumulative amount of unchanged daptomycin excreted in urine; AUC0–tau, area under the plasma concentration–time curve over the dosing period.
Compartmental pharmacokinetics of daptomycin
Pharmacokinetic parameters were estimated precisely and diagnostic plots from the daptomycin pharmacokinetic model showed a good fit of the final model to the observed daptomycin plasma concentrations [Figure S1, available as Supplementary data at JAC Online (http://jac.oxfordjournals.org/)]; population parameter estimates are presented in Table S2 [available as Supplementary data at JAC Online (http://jac.oxfordjournals.org/)]. Additional analyses were conducted to compare Cmax predicted by the above model for the 2 min iv injection with that of the 30 min iv infusion of 6 mg/kg daptomycin. The predicted Cmax after administration of a single 6 mg/kg daptomycin dose as 2 min iv injection and 30 min iv infusion were 86.6 mg/L and 76.4 mg/L, respectively.
In order to determine whether, in patients with varying degrees of renal impairment, renal function affected the differences in peak daptomycin exposure between the two regimens, Cmax was predicted based on clearance from the current pharmacokinetic model re-parameterized using the previously described relationship between daptomycin CL with estimated CLCR:12
with all other pharmacokinetic parameters unchanged. The predicted Cmax values (estimated at 0 h post-dose) for subjects with CLCR of 80, 50 and 30 mL/min were 86.57, 86.62 and 86.66 mg/L, respectively, for the 2 min iv injection and 76.58, 77.13 and 77.5 mg/L, respectively, for the 30 min iv infusion. These data suggest a small (<15%) increase in Cmax for the 2 min iv injection compared with the 30 min iv infusion, irrespective of the renal function status of the patients.
Safety and tolerability
Safety of the 2 min injection versus 30 min infusion in a single-dose, crossover trial (Study 1)
Treatment with daptomycin was well tolerated with no consistent differences between treatment groups in the type of AEs reported. A total of 21 AEs were reported by 9 of 16 subjects. Nineteen AEs were of mild severity and no serious or severe AEs or deaths were reported during the study. Six subjects reported AEs that were considered to be possibly related to the study medication, four subjects following administration of the daptomycin 2 min iv injection and two subjects following administration of the daptomycin 30 min iv infusion (Table 4). Local tolerability reactions were mild tenderness (one subject in the 2 min iv injection group and two subjects in the 30 min iv infusion group) and pain (one subject in the 30 min iv infusion group).
Table 4.
Adverse events possibly or probably related to study drug following a 6 mg/kg dose of daptomycin administered as a 2 min iv injection or as a 30 min iv infusion (Study 1)
| Adverse event (system organ class) | Subjects with at least one adverse event, n (%) |
|
|---|---|---|
| 2 min iv injection n = 16 | 30 min iv infusion n = 15 | |
| Any adverse event | 4 (25) | 2 (13) |
| Gastrointestinal disorders | 1 (6) | 0 |
| nausea | 1 (6) | 0 |
| General disorders and administration-site conditions | 1 (6) | 0 |
| fatigue | 1 (6) | 0 |
| Infections and infestations | 1 (6) | 2 (13) |
| urinary tract infection | 1 (6) | 2 (13) |
| Nervous system disorders | 1 (6) | 0 |
| headache | 1 (6) | 0 |
One subject discontinued prematurely due to an AE (anaemia) not related to study medication after completing the 2 min iv injection treatment period and before receiving the 30 min iv infusion. The anaemia was mild and resolved after 3 weeks. No other clinically significant haematological changes were reported for any other subject during the study.
Safety after single and multiple doses of 6 mg/kg daptomycin, 4 mg/kg daptomycin or placebo administered as a 2 min iv injection once daily for 7 days (Study 2)
No clinically relevant differences in AEs and local tolerability were observed between daptomycin-treated and placebo-treated subjects. A total of 25 AEs were reported by 14 of 24 subjects enrolled on the multiple-dose study. The majority of AEs were of mild intensity, and there were no serious or other significant AEs. A total of five subjects treated with daptomycin and four subjects treated with placebo reported AEs that were considered to be possibly related to the study medication (Table 5). No AE led to withdrawal from the study. One subject in the 6 mg/kg daptomycin group experienced first-degree atrioventricular block, associated with a congenital wandering pacemaker, and not considered related to daptomycin treatment.
Table 5.
Adverse events possibly or probably related to study drug following multiple doses of daptomycin 2 min iv injection or placebo (Study 2)
| Adverse event (system organ class) | Subjects with at least one adverse event, n (%) |
||
|---|---|---|---|
| daptomycin 6 mg/kg n = 12 | daptomycin 4 mg/kg n = 8 | placebo n = 4 | |
| Any adverse event | 3 (25) | 2 (25) | 4 (100) |
| Gastrointestinal disorders | 0 | 1 (13) | 1 (25) |
| flatulence | 0 | 1 (13) | 0 |
| nausea | 0 | 0 | 1 (25) |
| Infections and infestations | 0 | 0 | 1 (25) |
| upper respiratory tract infection | 0 | 0 | 1 (25) |
| Musculoskeletal, connective tissue and bone disorders | 0 | 1 (13) | 0 |
| pain in extremity | 0 | 1 (13) | 0 |
| Nervous system disorders | 3 (25) | 1 (13) | 2 (50) |
| dizziness | 1 (8) | 0 | 0 |
| dizziness postural | 1 (8) | 0 | 0 |
| headache | 1 (8) | 0 | 1 (25) |
| lethargy | 0 | 1 (13) | 0 |
| paraesthesia | 0 | 0 | 1 (25) |
The incidence of local injection-site reactions was low and all reactions were generally mild and transient, resolving within 1 h. Nine subjects experienced erythema: two subjects in the 6 mg/kg daptomycin group; five subjects in the 4 mg/kg daptomycin group; and two subjects in the placebo group.
Discussion
These studies demonstrate that daptomycin exposure (including AUC and Cmax) is similar, whether it is administered as a 2 min iv injection or the currently approved 30 min iv infusion, and is consistent with the results of previous studies with the 30 min iv infusion in healthy volunteers.10,14,17,20 In addition, the percentage of daptomycin excreted unchanged in the urine over 24 h (measured on day 7) was within the 34%–68% range of previously reported studies,10,17,20 confirming renal excretion as the major elimination pathway for daptomycin.
For additional rigor, and because it is often difficult to capture true Cmax from observed concentration–time data following rapid iv injection, pharmacokinetic modelling was also employed. This predicted a Cmax slightly (<15%) higher following the 2 min iv injection of daptomycin compared with the approved 30 min iv infusion regimen, irrespective of modelled differences in renal function. This potential increase in Cmax is not expected to change the safety profile of the currently approved doses of daptomycin. The pharmacokinetic, safety and tolerability profiles of daptomycin have been investigated in clinical trials, with single daily daptomycin doses of up to 12 mg/kg, exposing subjects to substantially higher Cmax than the levels observed from the 6 mg/kg daptomycin 2 min iv injection. High-dose daptomycin (8, 10 and 12 mg/kg) administered as a 30 min iv infusion,10 resulted in Cmax values equivalent to 112%, 137% and 174% of that observed with the 6 mg/kg 2 min iv injection in Study 1, respectively. Furthermore, no significant AEs were observed in subjects receiving these high doses once daily for up to 14 days.10 Indeed, the present studies suggest that daptomycin administered as a 2 min iv injection has a similar safety profile to that of the 30 min iv infusion, with no new or unexpected safety concerns. The majority of treatment-emergent AEs were mild and not considered to be related to daptomycin treatment, and local tolerability reactions were similar between daptomycin-treated and placebo-treated subjects.
As a concentration-dependent bactericidal antibiotic, the efficacy of daptomycin is pharmacodynamically best correlated with the AUC/MIC or Cmax/MIC ratio.21 Given that AUCs were similar following the different modes of administration, and that Cmax was predicted to be slightly higher with the 2 min iv injection, the efficacy of the 2 min daptomycin iv injection is expected to be similar to that of the standard 30 min iv infusion.
The daptomycin 2 min iv injection has the potential to confer a number of benefits in the management of patients with serious Gram-positive infections. As well as simplifying the dosing schedule for patients receiving multiple medications via catheter, the reduced administration volume gives the physician more scope in managing the patient's fluid balance, which may be a particular concern for patients in intensive care units.22 Additionally, the increased risk of catheter-related bloodstream infections associated with the use of multilumen catheters23 suggests that drugs that can be administered relatively rapidly have the potential to decrease the need for such catheters, thereby reducing the risk of infection.
Patients with serious Gram-positive infections are increasingly treated in the outpatient setting.15,16 Treating patients with serious infections, such as MRSA, as outpatients, reduces the risk of spreading infections to other hospital patients. Agents that can be administered by slow iv injection may be advantageous in this context, because they obviate the need for infusion devices,18 which may incur additional costs. Indeed, short injections have been shown to be one of the most cost-effective methods of administering iv drugs in the outpatient setting,24 and are more convenient for patients in that they minimize the degree of disruption to everyday activities.
These data indicate that daptomycin, administered as a 2 min iv injection once daily over 7 days, has a similar safety, tolerability and pharmacokinetic profile to that of the 30 min iv infusion. The 2 min iv injection may, therefore, offer an alternative method of administration to the currently approved 30 min iv infusion. This could contribute towards more streamlined management of seriously ill patients in hospital and simplify treatment administration for patients and caregivers, thus facilitating the potential use of daptomycin in the outpatient setting. Additional studies in patients are warranted to confirm the promising results observed in healthy volunteers.
Funding
The studies presented herein were funded by Novartis Pharma AG and were conducted in preparation for submission of the daptomycin 2 min iv injection to regulatory authorities. Writing support (by Ruthline Laylor of Chameleon Communications International) was funded by Novartis Pharma AG.
Transparency declarations
A. C., S. R., J. L. and R. L. C. are employees of Novartis Pharma AG, and as such own stock options with the company. No other conflicts of interest to declare.
In addition to the writing of this article, the role of the authors was limited to analysis and interpretation of the data arising from the presented randomized clinical trials. The authors had no direct role in the design or execution of the work described.
Writing support for the preparation of this manuscript was provided by Ruthline Laylor, of Chameleon Communications International.
Supplementary data
Acknowledgements
Preliminary analysis of the current studies was presented at the Forty-sixth Interscience Conference on Antimicrobial Agents and Chemotherapy, San Francisco, CA, USA, 2006 (Ahmad QI, Mankowski M, Girish SR. Safety and tolerability of daptomycin iv bolus injections in healthy adult volunteers. Poster A-1948).
We would like to thank the study investigator Dr Peter Dewland of Simbec Research Ltd, Merthyr Tydfil, South Wales, UK. In addition, we would like to thank Ruthline Laylor, of Chameleon Communications International, who provided writing support in the preparation of this manuscript.
References
- 1.Cubist Pharmaceuticals. Cubicin Prescribing Information. Lexington, MA, USA: Cubist Pharmaceuticals, Inc.; 2007. [Google Scholar]
- 2.Novartis Europharm Ltd. Cubicin Summary of Product Characteristics. Horsham, UK: Novartis Europharm Ltd; 2008. [Google Scholar]
- 3.Holmes RL, Jorgensen JH. Inhibitory activities of eleven antimicrobial agents and bactericidal activities of vancomycin and daptomycin against invasive methicillin-resistant Staphylococcus aureus (MRSA) from 1999 through 2006. Antimicrob Agents Chemother. 2008;52:757–60. doi: 10.1128/AAC.00945-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sader HS, Streit JM, Fritsche TR, et al. Antimicrobial activity of daptomycin against multidrug-resistant Gram-positive strains collected worldwide. Diagn Microbiol Infect Dis. 2004;50:201–4. doi: 10.1016/j.diagmicrobio.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Sader HS, Fritsche TR, Streit JM, et al. Daptomycin in vitro activity tested against Gram-positive strains collected from European and Latin American medical centers in 2003. J Chemother. 2005;17:477–83. doi: 10.1179/joc.2005.17.5.477. [DOI] [PubMed] [Google Scholar]
- 6.Sader HS, Fritsche TR, Jones RN. Antimicrobial activity of daptomycin tested against clinical strains of indicated species isolated in North American medical centers (2003) Diagn Microbiol Infect Dis. 2005;53:329–32. doi: 10.1016/j.diagmicrobio.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Sader HS, Streit JM, Fritsche TR, et al. Antimicrobial susceptibility of Gram-positive bacteria isolated from European medical centres: results of the Daptomycin Surveillance Programme (2002–2004) Clin Microbiol Infect. 2006;12:844–52. doi: 10.1111/j.1469-0691.2006.01550.x. [DOI] [PubMed] [Google Scholar]
- 8.Sader HS, Watters AA, Fritsche TR, et al. Daptomycin antimicrobial activity tested against methicillin-resistant staphylococci and vancomycin-resistant enterococci isolated in European medical centers (2005) BMC Infect Dis. 2007;7:29. doi: 10.1186/1471-2334-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sader HS, Watters AA, Fritsche TR, et al. Activity of daptomycin and selected antimicrobial agents tested against Staphylococcus aureus from patients with bloodstream infections hospitalized in European medical centers. J Chemother. 2008;20:28–32. [PubMed] [Google Scholar]
- 10.Benvenuto M, Benziger DP, Yankelev S, et al. Pharmacokinetics and tolerability of daptomycin at doses up to 12 milligrams per kilogram of body weight once daily in healthy volunteers. Antimicrob Agents Chemother. 2006;50:3245–9. doi: 10.1128/AAC.00247-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dvorchik BH, Brazier D, DeBruin MF, et al. Daptomycin pharmacokinetics and safety following administration of escalating doses once daily to healthy subjects. Antimicrob Agents Chemother. 2003;47:1318–23. doi: 10.1128/AAC.47.4.1318-1323.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dvorchik B, Arbeit RD, Chung J, et al. Population pharmacokinetics of daptomycin. Antimicrob Agents Chemother. 2004;48:2799–807. doi: 10.1128/AAC.48.8.2799-2807.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arbeit RD, Maki D, Tally FP, et al. The safety and efficacy of daptomycin for the treatment of complicated skin and skin-structure infections. Clin Infect Dis. 2004;38:1673–81. doi: 10.1086/420818. [DOI] [PubMed] [Google Scholar]
- 14.Fowler VG, Jr, Boucher HW, Corey GR, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med. 2006;355:653–65. doi: 10.1056/NEJMoa053783. [DOI] [PubMed] [Google Scholar]
- 15.Bernard L, El-Hajj L, Pron B, et al. Outpatient parenteral antimicrobial therapy (OPAT) for the treatment of osteomyelitis: evaluation of efficacy, tolerance and cost. J Clin Pharm Ther. 2001;26:445–51. doi: 10.1046/j.1365-2710.2001.00380.x. [DOI] [PubMed] [Google Scholar]
- 16.Esposito S, Leone S, Noviello S, et al. Outpatient parenteral antibiotic therapy for bone and joint infections: an Italian multicenter study. J Chemother. 2007;19:417–22. doi: 10.1179/joc.2007.19.4.417. [DOI] [PubMed] [Google Scholar]
- 17.Wise R, Gee T, Andrews JM, et al. Pharmacokinetics and inflammatory fluid penetration of intravenous daptomycin in volunteers. Antimicrob Agents Chemother. 2002;46:31–3. doi: 10.1128/AAC.46.1.31-33.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nathwani D, Morrison J. Parenteral therapy in the outpatient or home setting: evidence, evaluation and future prospects. J Infect. 2001;42:173–5. doi: 10.1053/jinf.2001.0823. [DOI] [PubMed] [Google Scholar]
- 19.Beal SL, Sheiner LB, Boeckmann AJ. NONMEM Users Guide. San Francisco, CA, USA: NONMEM Project Group, University of California; 1994. [Google Scholar]
- 20.Dvorchik B, Damphousse D. Single-dose pharmacokinetics of daptomycin in young and geriatric volunteers. J Clin Pharmacol. 2004;44:612–20. doi: 10.1177/0091270004265646. [DOI] [PubMed] [Google Scholar]
- 21.Safdar N, Andes D, Craig WA. In vivo pharmacodynamic activity of daptomycin. Antimicrob Agents Chemother. 2004;48:63–8. doi: 10.1128/AAC.48.1.63-68.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steven WJ. Fluid balance and critical aspects of ICU care. Nursing 2008 Critical Care. 2008;3:13–21. [Google Scholar]
- 23.Pawar M, Mehta Y, Kapoor P, et al. Central venous catheter-related blood stream infections: incidence, risk factors, outcome, and associated pathogens. J Cardiothorac Vasc Anesth. 2004;18:304–8. doi: 10.1053/j.jvca.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 24.Schleis TG, Tice AD. Selecting infusion devices for use in ambulatory care. Am J Health Syst Pharm. 1996;53:868–77. doi: 10.1093/ajhp/53.8.868. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.