Abstract
Purpose
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in the United States but is often under-treated. COPD often overlaps with other conditions such as hypertension and osteoporosis, which are less morbid but which may be treated more aggressively. We evaluated the prevalence of these comorbid conditions and compared testing, patient knowledge, and management in a national sample of patients with COPD.
Methods and Methods
A survey was administered by telephone in 2006 to 1,003 COPD patients to evaluate the prevalence of comorbid conditions, diagnostic testing, knowledge, and management using standardized instruments. The completion rate was 87%.
Results
Among 1,003 patients with COPD, 61% reported moderate or severe dyspnea and 41% a prior hospitalization for COPD. The most prevalent comorbid diagnoses were hypertension (55%), hypercholesterolemia (52%), depression (37%), cataracts (31%) and osteoporosis (28%). Only 10% of respondents knew their FEV1 (95% CI: 8, 12%) compared to 79% who knew their blood pressure (95% CI: 76%, 83%). Seventy-two percent (95% CI: 69%, 75%) reported taking any medication for COPD – usually a short-acting bronchodilator – whereas 87% (95% CI: 84%, 90%) of patients with COPD and hypertension were taking an antihypertensive medication and 72% (95% CI: 68%, 75%) of patients with COPD and hypercholesterolemia were taking a statin.
Conclusion
Although most of these COPD patients in this national sample were symptomatic and many had been hospitalized for COPD, COPD self-knowledge was low and COPD was undertreated compared to generally asymptomatic, less morbid conditions such as hypertension.
Keywords: chronic obstructive pulmonary disease, emphysema, chronic bronchitis, asthma, comorbidities
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is currently the fourth leading cause of death in the United States (US) and is projected to be the third most common cause of death by the year 2020.1 In 2004, 120,000 persons in the US died from COPD 2 – an increase of 67% from 1980 3 and more than twice the number that died from congestive heart failure.2 The number of patients diagnosed by a physician as having COPD in the US increased from approximately 7 million in 1980 to 12 million in 2004 – higher than the prevalence of both stroke and congestive heart failure.4
COPD is a leading cause of hospitalizations in older adults 5 and accounted for 15.4 million physician office visits in the US in 2003 – about the same as coronary heart disease, stroke and congestive heart failure combined.2 The cost of COPD care was approximately $37.2 billion in 2004, including $20.9 billion in direct healthcare expenditures, $7.4 billion in indirect morbidity costs and $8.9 billion in indirect mortality costs.6 Morbidity, mortality and cost of COPD continue to rise.7
Patients with COPD may have a worse prognosis than patients with other commonly treated conditions. For example, 15-year cumulative incidence of fatal coronary heart disease in NHANES II was 5.1% and 3.0% among men and women with hypercholesterolemia, respectively, and 5.0% and 3.4% among men and women with hypertension, respectively.8 By comparison, 22-year cumulative incidence of fatal COPD among NHANES I participants with moderate-to-severe airflow obstruction based on pre-bronchodilator measures only was 7.8% and all-cause mortality was 51%.9 Post-bronchodilator measures necessary for the diagnosis of COPD were not available in NHANES I; COPD mortality is likely to have been higher still among those with actual COPD.
COPD patients may be predisposed to developing muscle weakness,10, 11 osteoporosis,12, 13 depression,14, 15 and possibly cardiovascular disease,16–20 and some studies suggest that these co-morbidities contribute to mortality in COPD.21 While co-morbidities appear to be common in COPD, the reported prevalence varies tremendously in different studies 22–25 and national data are lacking. We therefore interviewed a national sample of patients with COPD to describe comorbid conditions in COPD and to compare testing, self-knowledge, and management for COPD with prevalent but less morbid coexisting diagnoses among these COPD patients.
METHODS
Participants were drawn from a national sample of 4,003 households in which one or more persons reported a diagnosis of a form of COPD. COPD was ascertained by the questionnaire item, “Have you ever been diagnosed by a physician as having: emphysema; chronic obstructive pulmonary disease (COPD); [or] alpha-one antitrypsin deficiency.” COPD patients with a co-diagnosis of asthma were not excluded due to the overlap of these two conditions in clinical practice. The sampling frame was derived from an on-going series of national surveys identifying households with members afflicted by various disease conditions. The use of this commercial compiled list increased the likelihood that each contacted household included a person with COPD. The list excluded households that had previously indicated that they were not willing to participate in surveys. The survey was conducted by Schulman, Ronca and Bucuvalas, Inc (SRBI, New York, NY) and performed between 12/29/05 and 2/17/06. Participants were interviewed using an established computer-assisted telephone interview approach. The response rate (number interviewed/[valid telephone numbers – deaths – no contacts]) was 52% and the completion rate (number interviewed/eligible units contacted) was 87%.
Questionnaire Items
Participants were asked about the diagnosis and severity of COPD using previously validated questionnaire items, as available. Dyspnea severity was measured by the modified Medical Research Council (MRC) Dyspnea index.26 COPD-related items were used as previously described.27 Participants were asked about physician diagnoses of comorbid conditions, in addition to symptoms that are considered diagnostic (e.g., for heartburn and reflux28) and medication use. A panel of COPD experts including physicians, patients, and representatives from COPD organizations helped draft the questionnaire. Validation of the responses was beyond the scope of the current study.
Statistical Analysis
Data are presented as proportions and means with standard deviations (SD) or medians with interquartile ranges (IQR), as appropriate. One-sample 95% confidence intervals (CI) were calculated for binomial data using the normal-theory method. Associations between categorical factors were tested with the chi-squared test and Mantel-Hanzel test for trend, as appropriate. All p-values were two-tailed, with P<0.05 considered statistically significant. Analyses were performed using SAS 9.1 (SAS Institute, Cary, NC).
RESULTS
The characteristics of the 1,003 patients who responded to the survey, stratified by gender, are shown in Table 1. The mean age (± SD) was 61±10 and 58% were women. Respondents lived mostly in the Midwest and the South of the United States, and were predominantly white. Half had no education beyond high school. Ninety-five percent noted a history of daily cigarette use and 47% of women and 39% of men smoked cigarettes regularly at the time of the survey. A co-diagnosis of asthma was common, particularly among women.
Table 1.
Characteristics of participants in a national sample of 1,003 patients with chronic obstructive pulmonary disease.
| Women | Men | P-value | |
|---|---|---|---|
| N=581 (58%) | N=422 (42%) | ||
| Age category (%), years | <0.001 | ||
| 40–49 | 20 | 10 | |
| 50–59 | 36 | 29 | |
| 60–69 | 26 | 35 | |
| 70 and over | 18 | 26 | |
| Region (%) | 0.86 | ||
| Northeast | 12 | 11 | |
| Midwest | 30 | 29 | |
| South | 36 | 28 | |
| West | 22 | 22 | |
| Race/Ethnicity (%) | 0.85 | ||
| White | 88 | 89 | |
| African American | 6 | 5 | |
| Hispanic | 3 | 2 | |
| Other | 3 | 4 | |
| Educational attainment | 0.91 | ||
| No high school degree | 13 | 17 | |
| High school degree | 38 | 34 | |
| Some college | 37 | 31 | |
| College graduate | 12 | 18 | |
| Work status | <0.001 | ||
| Fulltime | 12 | 21 | |
| Part-time or unemployed | 16 | 12 | |
| Disabled | 34 | 20 | |
| Retired | 32 | 47 | |
| Other | 6 | 0 | |
| Gross household income in 2004 | <0.001 | ||
| $15,000 or less | 41 | 23 | |
| $15,001–$25,000 | 18 | 21 | |
| $25,001–$35,000 | 16 | 18 | |
| $35,001–$50,000 | 13 | 17 | |
| $50,001 or above | 4 | 6 | |
| Ever smoker (%) | 93 | 96 | 0.04 |
| Current smoking (%) | 47 | 39 | 0.01 |
| Packyears (mean ± SD) | 32 ± 13 | 37 ± 13 | 0.32 |
| Concurrent diagnosis of asthma (%) | 62 | 37 | <0.001 |
| Symptoms every/most days for three consecutive months or more in past year (%) | |||
| Coughed | 66 | 60 | 0.06 |
| Brought up phlegm | 56 | 56 | 0.99 |
| Current degree of dyspnea (%), MRC Scale | 0.43 | ||
| None (0) | 2 | 4 | |
| I only get breathless after strenuous exercise (1) | 9 | 15 | |
| I get breathless when hurrying on level ground or walking up a slight incline (2) | 23 | 26 | |
| I walk slower than people my own age (3) | 13 | 10 | |
| I have to stop for breath when walking on level ground at my own pace (3) | 13 | 14 | |
| I have to stop for breath after walking a few minutes on level ground (4) | 30 | 23 | |
| I am too breathless to leave the house (5) | 10 | 8 | |
| Health status (%) | 0.001 | ||
| Excellent | 1 | 3 | |
| Very good | 7 | 8 | |
| Good | 21 | 31 | |
| Fair | 38 | 31 | |
| Poor | 32 | 28 | |
| COPD hospitalization ever (%) | 44 | 38 | 0.09 |
| Number of COPD hospitalizations in last 5 years | |||
| 1 | 16 | 25 | 0.47 |
| 2–4 | 44 | 54 | |
| 5 or more | 31 | 18 | |
| Health Insurance* | |||
| Government | |||
| Medicare | 48 | 48 | 0.95 |
| Medicaid | 22 | 10 | <0.001 |
| Veterans Administration | 4 | 17 | <0.001 |
| Employer-based | 33 | 37 | 0.01 |
| Self-financed | 15 | 13 | 0.43 |
| None | 11 | 14 | 0.39 |
| Insurance coverage of drug costs | 0.26 | ||
| Most or all | 62 | 68 | |
| Some, little or none | 34 | 29 | |
More than one response was permitted.
COPD patients in the survey were generally symptomatic and made extensive use of the healthcare system. Sixty-one percent reported moderate or severe dyspnea on exertion (MRC Dyspnea Index 3 or more), 63% described chronic cough, 55% chronic sputum production, and 55% at least one bronchitic episode per year. Forty-one percent reported being hospitalized for a COPD exacerbation and, over the past year, 30% had visited doctors 3–5 times, 22% 6–10 times and 33% over 10 times.
Comorbid Conditions
Table 2 shows the frequencies of comorbid diagnoses and non-respiratory symptoms reported by the 1,003 patients with COPD stratified by gender. Hypertension (55%) and hypercholesterolemia (52%) were the most prevalent comorbidities, followed in frequency by depression, cataracts and osteoporosis. Sleep apnea and diabetes each occurred in about a quarter of COPD patients. Twenty-two percent reported angina, 19% a history of myocardial infarction, and 14% a history of a cerebrovascular event (with overlap). Eleven percent reported chronic kidney disease and 6% congestive heart failure. Of the 6% with cancer, colon (0.7%), prostate (0.6%), lung (0.5%) and breast (0.4%) cancers were most common. The prevalence of comorbid conditions was generally similar among women and men, except for depression, osteoporosis and cardiovascular disease.
Table 2.
Prevalence of comorbid diagnoses and symptoms among a national sample of patients with chronic obstructive pulmonary disease.
| Percent of COPD Patients Reporting Condition | |||
|---|---|---|---|
| Women | Men | P-value | |
| N=581 | N=422 | ||
| Physician diagnosis | |||
| Hypertension | 53 | 57 | 0.15 |
| Hypercholesterolemia | 54 | 49 | 0.14 |
| Depression | 44 | 27 | <0.001 |
| Cataracts | 31 | 32 | 0.65 |
| Osteoporosis | 39 | 12 | <0.001 |
| Sleep Apnea | 25 | 28 | 0.28 |
| Diabetes | 25 | 26 | 0.78 |
| Angina | 20 | 24 | 0.23 |
| Heart attack | 14 | 27 | <0.001 |
| Stroke | 16 | 11 | 0.01 |
| Glaucoma | 7 | 7 | 0.86 |
| Congestive heart failure | 7 | 3 | 0.01 |
| Cancer | 6 | 4 | 0.47 |
| Symptoms | |||
| Joint pain | 77 | 66 | <0.001 |
| Heartburn or acid reflux | 68 | 60 | 0.02 |
| Sinus problems more than 1–2 times/year | 65 | 51 | <0.001 |
| Erectile dysfunction | -- | 37 | -- |
Symptoms of joint pain, GERD and sinus problems were highly prevalent (Table 2) and were more commonly reported by women than by men.
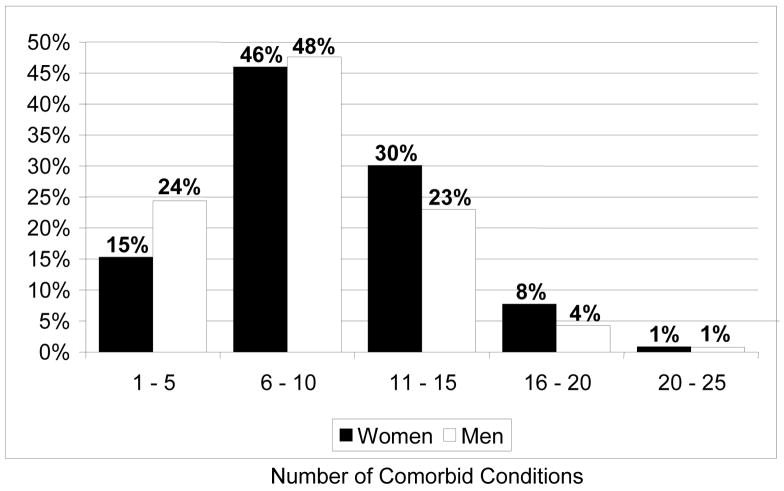
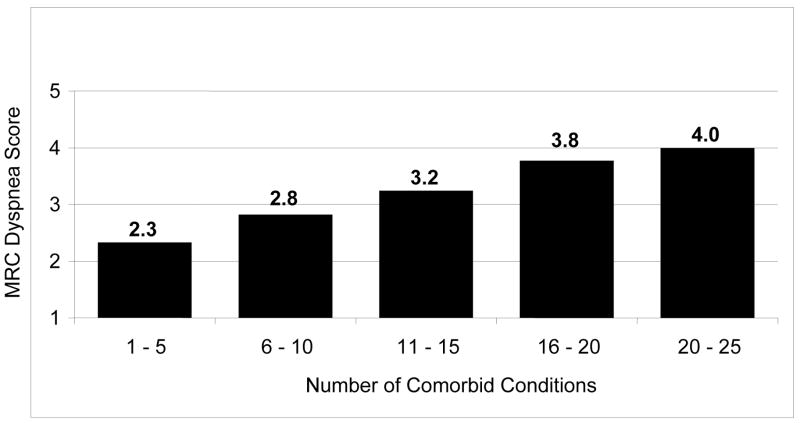
The median number of comorbid conditions among these patients with COPD was 9 (interquartile range [IQR], 6, 12). The frequency distribution of the total number of comorbidities is shown in Figure 1. The mean MRC Dyspnea Index increased monotonically with the number of comorbid conditions from 2.3 among those with 1–5 comorbid conditions to 4 among those with 20 or more comorbid conditions (Figure 2).
Figure 1.
Figure 2.
Diagnostic Testing for COPD and Comorbid Conditions
Eighty-two percent reported undergoing spirometry in the prior year, while 77% had a chest X-ray and 45% computerized axial tomography (CT) scan. Sixty-nine percent had undergone cardiac stress testing and 24% reported a prior cardiac catheterization. Overall 22% underwent bone densitometry, 21% a sleep study, and 7% a carotid ultrasound.
Self-Knowledge of COPD and Comorbid Conditions
Of the 55% of COPD patients who reported hypertension, 79% knew their blood pressure (95% CI: 76%, 83%). Of the 52% of COPD patients who reported hypercholesterolemia, 37% knew their cholesterol level (95% CI: 32%, 42%). In contrast, of the 1,003 COPD patients surveyed, only 10% reported knowing their FEV1 or percent predicted FEV1 (95% CI: 8, 12%). There was no difference in knowledge of FEV1 by gender (P=0.47)
COPD Management
Despite the severity of symptoms and frequency of health-care utilization reported by most COPD patients in this survey, 72% (95% CI: 69%, 75%) reported taking any regular medication for COPD (Table 3). Most commonly, this medication was a short-acting bronchodilator (55% of COPD patients). Twenty-six percent of COPD patients reported use of combination long-acting beta agonist and inhaled corticosteroid, and 15% reported use of a long-acting inhaled anticholinergic. Forty percent reported daily nebulizer use, 35% used oxygen daily, and 15% had participated in pulmonary rehabilitation. Sixty-five percent reported receiving influenza vaccination over the past year.
Table 3.
Prevalence of medication use for chronic obstructive pulmonary disease and for comorbid diagnoses and symptoms among a national sample of patients with chronic obstructive pulmonary disease.
| Percent of COPD patients with condition taking medication* | |||
|---|---|---|---|
| Women | Men | P-value | |
| N=581 | N=422 | ||
| Medication (any) for COPD (%) | 74 | 69 | 0.10 |
| Among patients without diagnosis of asthma | 66 | 63 | 0.45 |
| Among patients with diagnosis of asthma | 79 | 79 | 0.89 |
| Comorbid diagnoses | |||
| Medication (any) for hypertension* (%) | 87 | 86 | 0.63 |
| Statin for hypercholesterolemia* (%) | 68 | 76 | 0.05 |
| Medication (any) for depression* (%) | 72 | 64 | 0.13 |
| Medication (any) for osteoporosis* (%) | 63 | 45 | 0.02 |
| Continuous positive airway pressure for obstructive sleep apnea* (%) | 48 | 45 | 0.57 |
| Medication for diabetes mellitus* (%) | |||
| Insulin | 28 | 44 | 0.01 |
| Oral hypoglycemic | 67 | 68 | 0.88 |
| Medication for coronary artery disease* (%) | |||
| Aspirin | 52 | 72 | <0.001 |
| Other cardiac medication | 61 | 45 | <0.001 |
| Medication for stroke* (%) | |||
| Aspirin | 50 | 67 | 0.07 |
| Warfarin | 34 | 38 | 0.64 |
| Medication (any) for glaucoma* (%) | 55 | 52 | 0.78 |
| Comorbid symptoms | |||
| Medications for joint pain* (%) | <0.001 | ||
| Prescription analgesic only | 45 | 32 | |
| Over-the-counter analgesic only | 19 | 17 | |
| Both | 10 | 8 | |
| Regular medication (any) for heartburn or acid reflux* (%) | 68 | 57 | 0.004 |
| Medication (any; more than 1–2 times/year) for sinus problems* (%) | 68 | 64 | 0.29 |
Among those reporting comorbid condition (the prevalence of comorbid conditions is listed in Table 2).
The proportion taking any regular medication was higher among COPD patients with a co-diagnosis of asthma than among those with COPD only (79% vs. 64%, respectively; P<0.001). There were no significant differences in treatment for COPD by gender.
Management of Comorbid Conditions
Table 3 also shows medication use for comorbid conditions stratified by gender. Figure 3 presents the distribution of the total number of non-inhaler prescription medications taken by COPD patients per day.
Figure 3.
* Inhaled and nebulized treatments were not included in these totals.
Eighty seven percent (95% CI: 84%, 90%) of patients with COPD and hypertension were taking an antihypertensive medication. The proportion of COPD patients with hypertension who took antihypertensive medications was significantly greater than the proportion of COPD patients who took COPD medications. Seventy two percent (95% CI: 68%, 75%) of patients with COPD and hypercholesterolemia were taking a statin, which was similar to the proportion of COPD patients who took any COPD medication and far greater than the proportion who took a long-acting bronchodilator (41%; 95% CI: 38%, 44%).
Twelve percent of surveyed patients reported having no healthcare insurance, 30% of those with health insurance reported having no, little or only some medication coverage, and about a third described co-pay amounts as moderate or large. Lack of or inadequate health insurance coverage appeared to have a substantial negative impact on COPD patients’ use of likely necessary health services (Figure 4).
Figure 4.
Percent of participants who answered in the affirmative to the question: “During the past twelve months, as a result of costs or lack of coverage have you…?”
DISCUSSION
This national survey of patients with diagnosed COPD suggested that comorbid diagnoses of hypertension, hypercholesterolemia, depression and osteoporosis occur frequently in patients with COPD. Although this was a COPD survey and despite similar amounts of clinical testing, COPD patients’ knowledge of their cholesterol levels and blood pressure far exceeded their knowledge of their FEV1. COPD was under-treated compared to other conditions such as hypertension, which is generally asymptomatic and causes fewer hospitalizations and deaths than COPD.2
Several regional studies have examined the prevalence of comorbidities in COPD,24, 25, 29, 30 with prevalences of cardiac disease ranging from 13 to 71%, of arthritis from 10 to 36%, of diabetes from 2 to 22% and cancer from 4 to 15%. The present study showed, in general, higher prevalences of most comorbid conditions than many of the prior studies. Possible sources of variation in estimates across studies include differing severity of COPD, differing methods of ascertaining co-morbidities (e.g., direct inquiry vs. interrogating administrative databases, etc.), and differing definitions. Notably, most of the prior studies performed chart or administrative data reviews rather than the direct patient survey performed here and none were national or representative samples.
The high prevalence of comorbidity in COPD is likely multifactorial, and associated with age, multisystem impact of tobacco exposure and pathogenic features associated with or as a result of primary lung pathophysiology. The frequency of comorbid conditions in COPD patients in part probably reflects the age of the COPD population. According to the National Health Interview Survey in 2003–2004, 28% of men and 16% of women over age 65 reported having cardiac disease, 48% of men and 54% of women reported hypertension, 20% of men and 18% of women reported diabetes and 44% of men and 55% of women described having arthritis.31 However, 95% of COPD patients have a smoking history and smoking is a major risk factor for a large number of other diseases including coronary artery disease, cerebrovascular and peripheral vascular disease, lung cancer and other malignancies, erectile dysfunction, cataracts, osteoporosis, peptic ulcer disease and the metabolic syndrome.32 Recent investigations have documented associations of comorbid conditions with COPD independent of common risk factors such as tobacco exposure.10, 33–35 Speculation on the mechanisms behind such associations include common genetic mechanisms resulting in synchronous pathology in multiple organ systems, systemic effects related to the pulmonary and systemic vasculature or a systemic inflammatory response linked to the lung parenchymal and airway inflammatory processes in COPD.
Medications may also contribute to the development of comorbidities in COPD. Bronchodilators may contribute to tachyarrhythmias and tremors, although recent randomized clinical trials of long-acting β-agonists suggest that these effects probably do not translate into increased cardiovascular mortality.33, 34 Inhaled anticholinergics affect intra-ocular pressure and bladder function and might have cardiovascular effects.34–36 Inhaled corticosteroids predispose to cataracts and skin bruising, and may increase osteoporosis and risk of pneumonia.33 Systemic corticosteroids, often over-utilized in COPD care,27 could contribute to diabetes, hypertension, osteoporosis, muscle dysfunction, and adrenal insufficiency.
Numerous studies have suggested that comorbidities are a common cause of or contributor to COPD hospitalizations.40 In the Lung Health Study, a study of mild COPD, 12.8% of the 5,887 smokers were hospitalized with 42% due to cardiovascular events compared with 14% due to pulmonary complications.41 In a Kaiser Permanente study of over 45,000 COPD patients, heart failure was the leading cause of hospitalization, followed by myocardial infarction and stroke.21 Kinnuen et al found that co-morbidities were associated with the increased duration of COPD hospitalizations; the mean length-of-stay in patients without co-morbidity was 7.7 days compared to 10.5 days if a concurrent disease was present.42 Most studies evaluating cause of death in COPD suggest that COPD patients are more likely to die of co-morbid conditions rather than from their COPD,43–46 with most deaths from cardiovascular disease or malignancy, although this varies with severity of COPD.
A striking finding in our study was that COPD patients demonstrated much better recall of their blood pressure and cholesterol than of their FEV1. While this is not surprising in the context of the greater public education regarding hypertension and hypercholesterolemia than about COPD, the fact that lung function is a stronger independent predictor of survival than blood pressure or cholesterol level – not just among patients with COPD but in the general elderly population 47 also – suggests the irony of this observation and suggests the need for more public education about COPD. The National Institutes of Health has recently initiated a major initiative, called the Learn More, Breathe Better Campaign, to increase awareness of and understanding about COPD.48
COPD was less commonly treated than less symptomatic and less morbid conditions such as hypertension and hypercholesterolemia despite the increasing number of proven medications for the treatment of COPD. Recent randomized clinical trials show the effectiveness of long-acting β-agonists, long-acting anticholinergics and long-acting β-agonist-inhaled corticosteroid combinations for long-term bronchodilation, improvement in quality-of-life, and prevention of exacerbations,33, 36 although definitive evidence for their effects on change in lung function and mortality requires further testing in randomized clinical trials.
The diagnosis of COPD in this study was not validated in the patient surveys but was based on patient report. On the other hand, almost all patients had a substantial smoking history and most had prominent symptoms of chronic dyspnea. The prevalence of overlap with asthma, particularly among women, reflected real-world clinical practice and diagnostic challenges. Previous studies have documented a gender discrepancy in the diagnosis of asthma compared to COPD in which women are preferentially diagnosed with asthma given the same clinical history.49 Notably, the underuse of COPD medications was more marked in COPD patients without a co-diagnosis of asthma compared to those with a co-diagnosis of asthma. Comorbid diagnoses were also not validated, although the high prevalence of appropriate medication use for these diagnoses suggested that they were accurate. The survey was performed in a national sample but the sample was not representative, potentially limiting the generalizability of the results. The sampling frame might have increased the estimated prevalence of comorbidities and the reported use of all medications compared to a representative sample.
In summary, comorbidities are common in COPD and likely add to the complexity and cost of care. While patients with COPD take a large number of medications, relatively few of these medications are for COPD. This discrepancy may relate to poor physician and patient knowledge about COPD,27 or may reflect the more limited evidence base for COPD compared to other leading causes of death. While advances in COPD pathophysiology and clinical research are needed to have a full impact, better education and optimal use of existing therapeutic strategies is warranted to improve symptoms and reduce hospitalizations in patients with COPD.
Acknowledgments
We acknowledge and thank the COPD Foundation, which commissioned the survey, and the firm of Schulman, Ronca and Bucuvalas, Inc (SRBI), which administered the survey, performed initial data analyses and assisted with some aspects of the initial manuscript preparation.
Funding sources: The COPD Foundation and National Institutes of Health HL077612 and HL075476
Footnotes
Conflict of Interest Statement:
R. Graham Barr, MD, DrPH: none.
Bartolome R. Celli, MD: research grants from Glaxo Smith Kline (GSK), Boehringer Ingelheim (BI), Forrest Medical, Astra Zeneca; advisory board payments from GSK, BI, Almirall, Astra Zeneca; speakers fees from GSK, BI, Astra Zeneca, Almirall.
David Mannino, MD: research funding from GSK, Pfizer and Novartis; consultant or speakers fees from GSK, Pfizer, BI, Astra-Zeneca, Dey and Sepracor.
Thomas Petty, MD: none
Stephen I. Rennard, MD: research grants from Almirall, Lorillard, Centocor, Novartis, GSK, Philip Morris, Institute for Science and Health, Roche; consultancy and advisory board payments from Abbott, Johnson & Johnson, Almirall, Novartis, Altana, Roche, Anthera, Quintiles, GSK, Targegen; speakers fees from Adams, Novartis, AstraZeneca, Pfizer
Frank C. Sciurba, MD: consultancy for Astra Zeneca, BI, Dey, GSK, Novartis, Pfizer, PneumRX, Respironics, Schering and Sepracor.
James K. Stoller, MD, MS: consultancy for Talecris Biotherapeutics, BI; speaker for Grifols, Baxter, CSL-Behring, Pfizer, Talecris.
Byron M. Thomashow, MD: speakers fees and consultancy for BI, Pfizer and GSK.
Gerard M. Turino, MD: research grant from BI; consultancy for Talecris Corporation
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Petty TL. Definition, epidemiology, course, and prognosis of COPD. Clin Cornerstone. 2003;5(1):1–10. doi: 10.1016/s1098-3597(03)90003-2. [DOI] [PubMed] [Google Scholar]
- 2.National Heart Lung Blood Institute Factbook FY-2006. Bethesda, MD: NIH/NHLBI; 2007. [Google Scholar]
- 3.Hoyert DL, Arias E, Smith BL, Murphy SL, Kochanek KD. Death: Final Data for 1999. National Vital Statistics Reports 2001. Hyattsville, MD: National Center for Health Statistics; 2001. US Dept of Health and Human Services publication (PHS) 2001-1120; 2001. [Google Scholar]
- 4.Schiller JS, Adams PF, Nelson ZC. Summary health statistics for the U.S. population: National Health Interview Survey, 2003. Vital Health Stat 10. 2005 Apr;(224):1–104. [PubMed] [Google Scholar]
- 5.Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002 May;121(5 Suppl):121S–126S. doi: 10.1378/chest.121.5_suppl.121s. [DOI] [PubMed] [Google Scholar]
- 6.Morbidity and Mortality Chartbook. National Heart Lung and Blood Institute; 2004. [Google Scholar]
- 7.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997 May 24;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 8.Mensah GA, Brown DW, Croft JB, Greenlund KJ. Major coronary risk factors and death from coronary heart disease: baseline and follow-up mortality data from the Second National Health and Nutrition Examination Survey (NHANES II) American Journal of Preventive Medicine. 2005;29(5 Suppl 1):68–74. doi: 10.1016/j.amepre.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 9.Mannino DM, Buist AS, Petty TL, Enright PL, Redd SC. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow-up study. Thorax. 2003;58:388–393. doi: 10.1136/thorax.58.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wouters EF, Creutzberg EC, Schols AM. Systemic effects in COPD. Chest. 2002 May;121(5 Suppl):127S–130S. doi: 10.1378/chest.121.5_suppl.127s. [DOI] [PubMed] [Google Scholar]
- 11.Skeletal muscle dysfunction in chronic obstructive pulmonary disease. A statement of the American Thoracic Society and European Respiratory Society. Am J Respir Crit Care Med. 1999 Apr;159(4 Pt 2):S1–40. doi: 10.1164/ajrccm.159.supplement_1.99titlepage. [DOI] [PubMed] [Google Scholar]
- 12.de Vries F, van Staa TP, Bracke MS, Cooper C, Leufkens HG, Lammers JW. Severity of obstructive airway disease and risk of osteoporotic fracture. Eur Respir J. 2005 May;25(5):879–884. doi: 10.1183/09031936.05.00058204. [DOI] [PubMed] [Google Scholar]
- 13.Jorgensen NR, Schwarz P, Holme I, et al. The prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross sectional study. Respiratory Medicine. 2007 Jan;101(1):177–185. doi: 10.1016/j.rmed.2006.03.029. [DOI] [PubMed] [Google Scholar]
- 14.Himelhoch S, Lehman A, Kreyenbuhl J, Daumit G, Brown C, Dixon L. Prevalence of chronic obstructive pulmonary disease among those with serious mental illness. Am J Psychiatry. 2004 Dec;161(12):2317–2319. doi: 10.1176/appi.ajp.161.12.2317. [DOI] [PubMed] [Google Scholar]
- 15.Norwood R, Norwood R. Prevalence and impact of depression in chronic obstructive pulmonary disease patients. Current Opinion in Pulmonary Medicine. 2006 Mar;12(2):113–117. doi: 10.1097/01.mcp.0000208450.50231.c6. [DOI] [PubMed] [Google Scholar]
- 16.Sin DD, Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003 Mar 25;107(11):1514–1519. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- 17.Schunemann HJ, Dorn J, Grant BJ, Winkelstein W, Jr, Trevisan M. Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. Chest. 2000 Sep;118(3):656–664. doi: 10.1378/chest.118.3.656. [DOI] [PubMed] [Google Scholar]
- 18.Friedman GD, Klatsky AL, Siegelaub AB. Lung function and outcome of myocardial infarction. N Engl J Med. 1976 Dec 2;295(23):1323. doi: 10.1056/NEJM197612022952324. [DOI] [PubMed] [Google Scholar]
- 19.Curkendall SM, Lanes S, de Luise C, et al. Chronic obstructive pulmonary disease severity and cardiovascular outcomes. European Journal of Epidemiology. 2006;21(11):803–813. doi: 10.1007/s10654-006-9066-1. [DOI] [PubMed] [Google Scholar]
- 20.Curkendall SM, DeLuise C, Jones JK, et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada. Annals of Epidemiology. 2006 Jan;16(1):63–70. doi: 10.1016/j.annepidem.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Holguin F, Folch E, Redd SC, Mannino DM. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest. 2005 Oct;128(4):2005–2011. doi: 10.1378/chest.128.4.2005. [DOI] [PubMed] [Google Scholar]
- 22.van Manen JG, Bindels PJ, CJ IJ, van der Zee JS, Bottema BJ, Schade E. Prevalence of comorbidity in patients with a chronic airway obstruction and controls over the age of 40. J Clin Epidemiol. 2001 Mar;54(3):287–293. doi: 10.1016/s0895-4356(01)00346-8. [DOI] [PubMed] [Google Scholar]
- 23.Mapel DW, Dedrick D, Davis K. Trends and cardiovascular co-morbidities of COPD patients in the Veterans Administration Medical System, 1991–1999. Copd. 2005 Mar;2(1):35–41. doi: 10.1081/copd-200050671. [DOI] [PubMed] [Google Scholar]
- 24.Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005 Oct;128(4):2099–2107. doi: 10.1378/chest.128.4.2099. [DOI] [PubMed] [Google Scholar]
- 25.Sidney S, Sorel M, Quesenberry CP, Jr, DeLuise C, Lanes S, Eisner MD. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest. 2005 Oct;128(4):2068–2075. doi: 10.1378/chest.128.4.2068. [DOI] [PubMed] [Google Scholar]
- 26.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999 Jul;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: the COPD Resource Network Needs Assessment Survey. Am J Med. 2005 Dec;118(12):1415. doi: 10.1016/j.amjmed.2005.07.059. [DOI] [PubMed] [Google Scholar]
- 28.Kahrilas PJ. Gastroesophageal reflux disease. JAMA. 1996 Sep 25;276(12):983–988. [PubMed] [Google Scholar]
- 29.Wijnhoven HA, Kriegsman DM, Hesselink AE, de Haan M, Schellevis FG. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir Med. 2003 May;97(5):468–475. doi: 10.1053/rmed.2002.1463. [DOI] [PubMed] [Google Scholar]
- 30.Yeo J, Karimova G, Bansal S. Co-morbidity in older patients with COPD--its impact on health service utilisation and quality of life, a community study. Ageing. 2006 Jan;35(1):33–37. doi: 10.1093/ageing/afj002. [DOI] [PubMed] [Google Scholar]
- 31.Adams PF, Barnes PM. Summary health statistics for the U.S. population: National Health Interview Survey, 2004. Vital Health Stat 10. 2006 Aug;(229):1–104. [PubMed] [Google Scholar]
- 32.The 2004 United States Surgeon General’s Report: The Health Consequences of Smoking. N S W Public Health Bull. 2004 May–Jun;15(5–6):107. [PubMed] [Google Scholar]
- 33.Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007 Feb 22;356(8):775–789. doi: 10.1056/NEJMoa063070. [DOI] [PubMed] [Google Scholar]
- 34.Wedzicha JA, Calverley PM, Seemungal TA, et al. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. American Journal of Respiratory & Critical Care Medicine. 2008;177(1):19–26. doi: 10.1164/rccm.200707-973OC. [DOI] [PubMed] [Google Scholar]
- 35.Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994;272(19):1497–1505. [PubMed] [Google Scholar]
- 36.Barr RG, Bourbeau J, Camargo CA, Jr, Ram FSF. Inhaled tiotropium for stable chronic obstructive pulmonary disease: a meta-analysis. Thorax. 2006;61:854–862. doi: 10.1136/thx.2006.063271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agusti AG, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003 Feb;21(2):347–360. doi: 10.1183/09031936.03.00405703. [DOI] [PubMed] [Google Scholar]
- 38.Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: Role of comorbidities. Eur Respir J. 2006 Dec;28(6):1245–1257. doi: 10.1183/09031936.00133805. [DOI] [PubMed] [Google Scholar]
- 39.Walter RE, Wilk JB, Larson MG, et al. Systemic Inflammation and COPD: The Framingham Heart Study. 2008;133:19–25. doi: 10.1378/chest.07-0058. [DOI] [PubMed] [Google Scholar]
- 40.Fabbri LM, Luppi F, Beghe B, Rabe KF. Complex chronic comorbidities of COPD. 2008;31:204–212. doi: 10.1183/09031936.00114307. [DOI] [PubMed] [Google Scholar]
- 41.Anthonisen NR, Connett JE, Enright PL, Manfreda J. Hospitalizations and mortality in the Lung Health Study. Am J Respir Crit Care Med. 2002 Aug 1;166(3):333–339. doi: 10.1164/rccm.2110093. [DOI] [PubMed] [Google Scholar]
- 42.Kinnunen T, Saynajakangas O, Tuuponen T, Keistinen T. Impact of comorbidities on the duration of COPD patients’ hospital episodes. Respir Med. 2003 Feb;97(2):143–146. doi: 10.1053/rmed.2003.1438. [DOI] [PubMed] [Google Scholar]
- 43.Huiart L, Ernst P, Suissa S. Cardiovascular morbidity and mortality in COPD. Chest. 2005 Oct;128(4):2640–2646. doi: 10.1378/chest.128.4.2640. [DOI] [PubMed] [Google Scholar]
- 44.Hansell AL, Walk JA, Soriano JB. What do chronic obstructive pulmonary disease patients die from? A multiple cause coding analysis. Eur Respir J. 2003 Nov;22(5):809–814. doi: 10.1183/09031936.03.00031403. [DOI] [PubMed] [Google Scholar]
- 45.Mannino DM, Brown C, Giovino GA. Obstructive lung disease deaths in the United States from 1979 through 1993. An analysis using multiple-cause mortality data. Am J Respir Crit Care Med. 1997 Sep;156(3 Pt 1):814–818. doi: 10.1164/ajrccm.156.3.9702026. [DOI] [PubMed] [Google Scholar]
- 46.Camilli AE, Robbins DR, Lebowitz MD. Death certificate reporting of confirmed airways obstructive disease. Am J Epidemiol. 1991 Apr 15;133(8):795–800. doi: 10.1093/oxfordjournals.aje.a115958. [DOI] [PubMed] [Google Scholar]
- 47.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279(8):585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 48. [Accessed February 3, 2008];Learn More, Breathe Better Campaign. http://www.nhlbi.nih.gov/health/public/lung/copd/index.htm.
- 49.Chapman KR, Tashkin DP, Pye DJ. Gender bias in the diagnosis of COPD. Chest. 2001;119:1691–1695. doi: 10.1378/chest.119.6.1691. [DOI] [PubMed] [Google Scholar]