Abstract
This study, conducted in Columbus, Ohio, identified the predictors of current (past 30 day) illicit use of pharmaceutical opioids among young individuals (n=402) with a history of MDMA/ecstasy use who were recruited in 2002–2003 using respondent-driven sampling. To be eligible, participants had to be 18–30 years old, not involved in a drug abuse treatment, and report MDMA/ecstasy use at least once in the past 6 months. About 81% reported lifetime, and more than 31% reported current illicit use of pharmaceutical opioids. Logistic regression analysis revealed that illicit use of pharmaceutical tranquilizers and pharmaceutical stimulants were the strongest predictors of illicit use of pharmaceutical opioids. Risk of pharmaceutical opioid use was also greater among those who had higher levels of depressive symptoms and reported current use of hallucinogens and inhalants. Our findings suggest that the non-medical use of pharmaceutical opioids is a part of polydrug use practices that often incorporate illicit use of other prescription drugs. The observed relationship between depressive symptoms and illicit use of pharmaceutical opioids may have important implications for prevention programming and should be examined in future research.
Keywords: substance abuse, pharmaceutical opioids, pharmaceutical drugs, MDMA/ecstasy, depression, young adults
1. Introduction
Illegal use of pharmaceutical drugs has been identified as one of the fastest growing forms of drug abuse in the U.S., with pain relievers showing the highest prevalence rates of non-medical use among all other therapeutic classes of prescription drugs (SAMHSA, 2006). According to the National Survey of Drug Use and Health, in 2004 approximately 2.4 million people aged 12 years or older initiated illicit use of prescription opioids, which exceeded the numbers of new marijuana users (2.1 million) (SAMHSA, 2006). Similar to other drugs of abuse, rates of non-medical use of pharmaceutical opioids are higher among young adults than any other age group. In 2006, 25.5% of individuals between ages 18 and 25 reported lifetime, and 4.9% past month, illicit use of pharmaceutical opioids (SAMHSA, 2007).
Consistent with the increasing trend of non-medical use, U.S. population-based community surveys have shown that rates of past-year prevalence of prescription opioid abuse and dependence more than doubled between 1991–1992 and 2001–2002 (McCabe, Cranford, & West, 2008). The Treatment Episode Data Set has also shown significant increases in treatment admissions involving pharmaceutical opioids, especially among people between 20 and 30 years of age (SAMHSA, 2004b). However, National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data suggest that in 2001–2002, only about 16% of those with past-year pharmaceutical opioid abuse and about 59.5% of those with past-year dependence disorder, utilized substance abuse treatment (McCabe et al., 2008).
To develop appropriate prevention and treatment programs, more research is needed to understand the population of illicit users of pharmaceutical opioids (Zacny et al., 2003). Research has shown that non-medical users of pharmaceutical opioids are very diverse in terms of socio-demographic characteristics, drug use trajectories, and patterns of other drug use. For example, a recent study in South Florida described a trend of significant “invasion” of prescription drugs, including pharmaceutical opioids, into the local club drug subculture (Kurtz, Inciardi, Surratt, & Cottler, 2005). Prescription drug abuse has also been documented among drug-involved street-based sex workers (Surratt, Inciardi, & Kurtz, 2006). A study based on the National Addictions Vigilance Intervention and Prevention Program that used a sample of 3,821 individuals, identified six groups of illicit pharmaceutical opioids users that differed in terms drug use practices, social and demographic characteristics, and recent medical and psychological problems (Green & Butler, 2008). A study based on qualitative data collected for the Ohio Substance Abuse Monitoring Network also identified several distinct groups of users, including a group of new generation users, all between 19 and 23 years of age, who displayed two distinct patterns of non-medical use of pharmaceutical opioids. A group of “heavy” users developed more destructive patterns of use, became addicted to pharmaceutical opioids, and eventually transitioned to heroin. A group of “occasional” users differed from young “heavy” users and other groups in that they reported less social dysfunction and traumatic experiences while growing up, and were better adjusted in their current social situations (Daniulaityte, Carlson, & Kenne, 2006).
Previous research has shown that illicit use of pharmaceutical opioids and other prescription drugs is strongly associated with other drug use behaviors (Boyd, Esteban McCabe, & Teter, 2006; Inciardi, Surratt, Martin, & Gealt, 2004; McCabe, Boyd, & Teter, 2005; McCabe, Teter, & Boyd, 2005; McCabe, Teter, Boyd, Knight, & Wechsler, 2005; Sung, Richter, Vaughan, Johnson, & Thom, 2005). Furthermore, data obtained from the NESARC show that the majority (about 74%) of individuals with past year pharmaceutical opioid use disorder also met DSM-IV criteria for an additional past-year substance use disorder (McCabe et al., 2008).
This study aims to identify the socio-demographic and drug-related predictors of illicit use of pharmaceutical opioids among 402 young adults recruited for a longitudinal study of MDMA/ecstasy use in Columbus, Ohio. The study described here uses data collected through the baseline structured questionnaire.
2. Methods
The 402 participants in this study were recruited between May 2002 and June 2003 in the Columbus, Ohio, area to participate in a natural history study examining MDMA/ecstasy and other drug use practices among young adults (Carlson, Wang, Falck, & Siegal, 2005). To be eligible for the study, participants had to be between 18 and 30 years old, Ohio residents, not involved in formal drug treatment within the past 30 days, able to provide an address and telephone number for follow-up interview-contact information, and report having used MDMA/ecstasy at least once in the past 6 months. In addition, subjects who reported having used MDMA/ecstasy within 3 days prior to the baseline questionnaire were rescheduled to help minimize the potential effects of the post-MDMA use wash-out period affecting the interview (Curran & Travill, 1997).
Participants were recruited using respondent-driven sampling (RDS), a modified form of snowball or chain-referral sampling. In RDS, a financial reward is given to a participant for each potentially-eligible peer that he/she refers. To impose a form of rationing on recruitment, a limited number (e.g., 3) of referral coupons is used. This strategy helps prevent the emergence of semi-professional recruiters and to reduce the effects of volunteerism (Heckathorn, 1997; Heckathorn, Semaan, Broadhead, & Hughes, 2002). Sampling “seeds” were identified at dance clubs, music festivals, raves, on the streets, and other venues as well as through the networks of consultants. We attempted to diversify the “seeds” in terms of gender, ethnicity, age, and experience with MDMA/ecstasy to speed up the recruitment process and the convergence of sample compositions (Wang et al., 2005). Each respondent was given $15 for an eligible peer refereed to the project.
Informed consent was obtained from participants following a protocol that was approved by the University’s Institutional Review Board. Participants were compensated $50 for the time they spent responding to the 2–3 hour baseline interview. The baseline questionnaire was largely interviewer-administered and covered a variety of topics including, but not limited to, socio-demographic and drug use characteristics, adverse consequences associated with drug use, treatment history, and depressive symptoms measured using the Beck Depression Inventory (BDI-II). The BDI-II measures the severity of symptoms of depression that have occurred in the 2 weeks prior to its administration (Beck, Steer, & Brown, 1996). The instrument consists of 21 items, and scores can range from 0 to 63, with higher scores reflecting a greater severity of symptoms.
Statistical analysis was conducted using SPSS. Univariate statistics were used to describe socio-demographic and drug use characteristics. Logistic regression analysis was used to identify factors related to illicit use of pharmaceutical opioids. Prior 30 day use of marijuana was measured as: 0–“no use;” 1–“non-daily use;” 2–“daily use.” Prior 30 day use of cocaine (including crack), heroin, methamphetamine, pharmaceutical stimulants, pharmaceutical tranquilizers, hallucinogens (LSD and psilocybin mushrooms), and inhalants (amyl and butyl nitrites, others) were measured as: 0–“no use;” 1–“use.” Alcohol use was measured by the number of days of “drunkenness” in the previous 30 days (0–“none;” 1–“≤mean days (9 or less);” 2–“>mean days (10 or more)”).
3. Results
The majority of the participants were White, and almost 11% were African American. About 35% were females, and the majority were between 18 and 25 years old (Table 1). More than half reported they were currently enrolled in school (204 in college and 10 in high school). About 17% of the study participants had been to a professional substance abuse treatment program at least once in their lifetime. The majority of the sample had BDI-II scores suggesting none or minimal depressive symptomatology, and about 15% of the sample had BDI-II scores indicating moderate or severe depressive symptoms (Table 1).
Table 1.
Characteristics of the study participants, N=402.
| Variable | n (%) |
|---|---|
| Gender | |
| Men | 258 (64.2) |
| Women | 144 (35.8) |
| Ethnicity | |
| White | 330 (82.1) |
| African American | 43 (10.7) |
| Other | 29 (7.2) |
| Age | |
| 18–19 | 146 (36.3) |
| 20–25 | 222 (55.2) |
| 26–30 | 34 (8.5) |
| Education | |
| School enrollment | 204 (50.7) |
| Not in school | 198 (49.3) |
| Treatment | |
| Never | 332 (82.6) |
| At least once | 70 (17.4) |
| Depression (BDI Scores) | |
| None or minimal (0–19) | 343 (85.5) |
| Moderate or severe (20+) | 58 (14.5) |
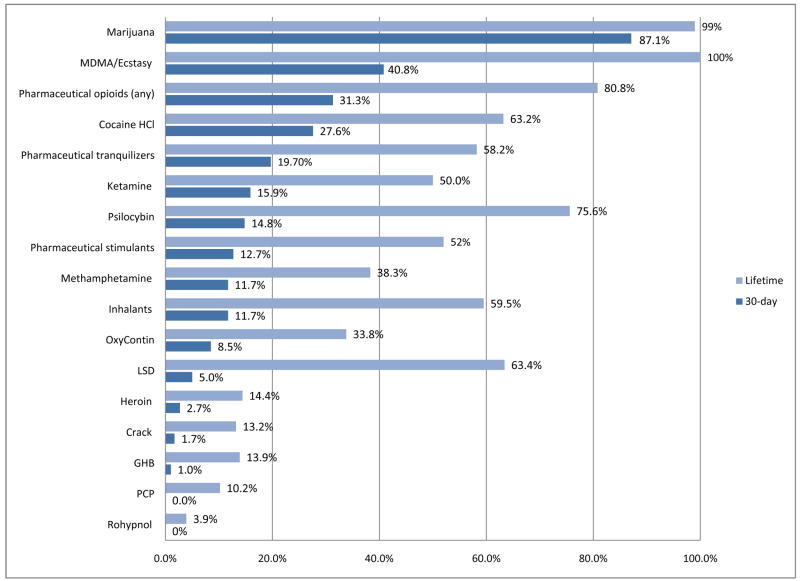
Lifetime and prior 30 day drug use characteristics are presented in Figure 1. About 81% of the sample reported lifetime non-medical use of any pharmaceutical opioid (e.g., Vicodin®, OxyContin®, etc.), and 31% reported current use (within 30 days prior to the study). Overall, illicit use of other drugs was common among the study participants. The majority of the sample (about 87%) reported marijuana use in the 30 days prior to the interview, and 53% were daily marijuana users (20+ days in the past 30 days). About 87% reported drinking alcohol to the point of intoxication at least once in the past 30 days, and 27% of the sample reported getting drunk on 10 or more days. Nearly half of the sample had used MDMA/ecstasy on 10 or fewer occasions in their lifetime, 17.2% reported using on 21–50 occasions, and about 15% reported using MDMA/ecstasy on more than 50 occasions.
Figure 1.
Prevalence of lifetime and current (past 30 day) use of illicit drugs, N=402.
Results of the logistic regression are presented in Table 2. The Hosmer-Lemeshow test (X2 =5.42, df=8, p=0.71) suggests that the model fits the data well. Five of the 17 variables showed significant association with pharmaceutical opioid use (p≤0.05).
Table 2.
Logistic regression analysis: Predictors of illicit use of pharmaceutical opioids in past 30 days.
| Variable | Odds ratio | 95% CI | p value |
|---|---|---|---|
| Age | 0.95 | 0.85 – 1.07 | 0.402 |
| Male (vs. female ) | 1.34 | 0.77 – 2.33 | 0.299 |
| Ethnicity (vs. White) | |||
| African American | 0.31 | 0.10 – 1.01 | 0.052 |
| Other ethnicity | 1.33 | 0.52 – 3.41 | 0.549 |
| School enrollment (vs. not in school) | 0.75 | 0.41 – 1.37 | 0.345 |
| Treatment history (vs. never in treatment) | 0.83 | 0.43 – 1.63 | 0.591 |
| Depressive symptoms (BDI scores ‘≥20’ vs. ‘<20’) | 2.15 | 1.04 – 4.44 | 0.039 |
| Marijuana use past 30 days (vs. 0 days) | |||
| > 20 days | 2.07 | 0.84 – 5.12 | 0.114 |
| 1–20 days | 1.54 | 0.60 – 3.95 | 0.365 |
| Drunk past 30 days (vs. 0 days) | |||
| 10 or more days | 1.32 | 0.55 – 3.12 | 0.535 |
| 1–9 days | 0.89 | 0.40 – 1.97 | 0.766 |
| Other drug use past 30 days (vs. no use) | |||
| Heroin | 2.22 | 0.53 – 9.24 | 0.275 |
| Cocaine | 1.48 | 0.80 – 2.70 | 0.210 |
| Methamphetamine | 0.71 | 0.29 – 1.71 | 0.440 |
| Ketamine | 0.75 | 0.34 – 1.66 | 0.472 |
| Prescription tranquilizers | 6.43 | 3.36 – 12.31 | <0.001 |
| Prescription stimulants | 2.90 | 1.33 – 6.32 | 0.007 |
| LSD and psilocybin | 2.02 | 1.03 – 3.94 | 0.040 |
| Inhalants | 2.26 | 1.01 - 5.06 | 0.048 |
| Lifetime MDMA use (vs. 1–10 occasions) | |||
| > 50 occasions | 0.77 | 0.33 – 1.82 | 0.551 |
| 21–50 occasions | 1.95 | 0.96 – 3.97 | 0.065 |
| 11–20 occasions | 1.20 | 0.59 – 2.43 | 0.617 |
Hosmer-Lemeshow Test: X2 =5.42, df=8, p=0.712
The odds of pharmaceutical opioid use among those who also reported illicit use of pharmaceutical tranquilizers (e.g., Xanax®, Valium®) was much higher, compared with those who did not use tranquilizers (OR=6.43, 95% CI: 3.36–12.31). The odds of pharmaceutical opioid use was also higher among those who reported illicit use of pharmaceutical stimulants (e.g., Ritalin®, Adderall®) in the 30 days prior to the study, compared with those who did not use stimulants (OR=2.90, 95% CI: 1.33–6.32). Increased risk of using pharmaceutical opioids was also associated with use of hallucinogens (OR=2.02, CI: 1.03–3.94) and inhalants (OR=2.26, CI: 1.01–5.06). African Americans had a lower risk of pharmaceutical opioid use than Whites, although the association was marginally significant (OR=0.31, CI: 0.10–1.01). In addition, participants who had moderate or severe depressive symptoms (BDI-II scores ≥ 20) were more likely to use pharmaceutical opioids than otherwise (OR=2.15, CI: 1.04–4.44). No statistically significant association was found between illicit use of pharmaceutical opioids and the use of alcohol, marijuana, and other drugs, including heroin, cocaine, methamphetamine, or ketamine. There was no statistically significant association between illicit use of pharmaceutical opioids and lifetime occasions of MDMA use.
4. Discussion and Conclusions
The study found high rates of non-medical use of pharmaceutical opioids among participants recruited for a natural history study of MDMA/ecstasy users, with more than 80% reporting lifetime use. In terms of lifetime and past 30 day use, pharmaceutical opioids were the third most commonly used illicit drugs after marijuana and MDMA/ecstasy. Our findings suggest that the non-medical use of pharmaceutical opioids is a part of polydrug use practices that often include illicit use of other prescription drugs. These results are consistent with data obtained by the Ohio Substance Abuse Monitoring Network showing a common trend of illicit use of pharmaceutical opioids in conjunction with benzodiazepines and other pharmaceutical drugs (Daniulaityte et al., 2006). The finding that hallucinogen use and use of inhalants were linked to non-medical use of pharmaceutical opioids is intriguing, although difficult to explain.
There was no statistically significant association between pharmaceutical opioid and heroin use among the study participants. In contrast, prior studies have suggested that non-medical use of pharmaceutical opioids is quite common among heroin users, and pharmaceutical opioids abuse sometimes may lead to initiation of heroin use (Daniulaityte et al., 2006; Ohio Substance Abuse Monitoring Network, 2006, June; Siegal, Carlson, Kenne, & Swora, 2003). The lack of a statistically meaningful association between heroin and pharmaceutical opioids use observed in the current study may be related to the fact that very low rates of heroin use were reported among the study participants.
The relationship between depressive symptoms and increased risk of non-medical opioid use is consistent with findings from other studies suggesting high rates of depression and psychosocial distress among illicit users of pharmaceutical opioids (Kurtz et al., 2005; Passik, Hays, Eisner, & Kirsh, 2006). Earlier research has also shown a significant association between psychiatric morbidity and illicit use of pharmaceutical opioids among chronic pain patients (Wasan et al., 2007). Furthermore, other studies found that depression and other psychiatric disorders are strongly linked to legitimate use of prescribed pharmaceutical opioids in the general population (Sullivan, Edlund, Zhang, Unutzer, & Wells, 2006). Prior research has also suggested that higher rates of opioid abuse problems among users of prescribed opioids may be partly mediated by depressive and anxiety disorders (Edlund, Sullivan, Steffick, Harris, & Wells, 2007). Overall, the NESARC data suggest that mood and anxiety disorders have a stronger association with prescription drug use disorders than most other drug use disorders, such as marijuana, cocaine, amphetamine, hallucinogen and inhalant/solvent (Conway, Compton, Stinson, & Grant, 2006). Prior qualitative research has also shown that pharmaceutical opioids and other prescription drugs are sometimes used to self-medicate psychosocial stress related to life adversities and poor health (Daniulaityte et al., 2006; Quintero, Peterson, & Young, 2006). However, it is important to note that this study’s cross-sectional design and methods used to assess depressive symptoms precludes determining whether depressive symptomatology was primary or secondary to illicit use of pharmaceutical opioids. Of note, our prior findings have shown that current illicit use of opioids, including heroin, was a statistically significant predictor of increases in BDI-II scores over a 24 month period, controlling for other covariates (Falck, Wang, & Carlson, 2008).
Ethnic differences in pharmaceutical opioid use among MDMA/ecstasy users recruited in Columbus, Ohio, were not statistically significant. Most prior studies have shown higher rates of illicit use of pharmaceutical opioids among whites than other ethnic groups in the US (McCabe, Teter, Boyd, Knight et al., 2005; Simoni-Wastila, Ritter, & Strickler, 2004). Prior research has also shown that similar ethnic differences exist in legitimate access to pharmaceutical opioids: ethnic minorities have lower chances than whites of receiving opioid medications for pain management, and pharmacies in minority urban areas may carry insufficient supplies of pharmaceutical opioids (Green, Ndao-Brumblay, West, & Washington, 2005; Tamayo-Sarver, Hinze, Cydulka, & Baker, 2003). The fact that in our study the association between race and illicit use of pharmaceutical opioids was not statistically significant may be partially related to the sample characteristics. As has been indicated previously, MDMA/ecstasy use was an eligibility criterion for participation. According to prior research, MDMA/ecstasy use in Ohio has been more common among whites than other ethnic or racial groups (Daniulaityte, Siegal, Carlson, Kenne, Starr, & DeCamp, 2004; Ohio Substance Abuse Monitoring Network, 2001, January; Ohio Substance Abuse Monitoring Network, 2001, June). As a result, African Americans who met eligibility criteria and were recruited for the study may have had many similarities with whites in terms of drug use patterns and networks.
The study did not find any gender differences in the illicit use of pharmaceutical opioids. Prior research has shown mixed results regarding differences in male and female use of pharmaceutical drugs. For example, a study based on 1991 National Household Survey on Drug Abuse, found that women were at increased risk for non-medical use of pharmaceutical opioids (Simoni-Wastila et al., 2004). In contrast, another study that was conducted in 2001 and used a nationally representative sample of 10,904 college students, found that gender was not significantly related to the nonmedical use of pharmaceutical opioids (McCabe, Teter, Boyd, Knight et al., 2005). In a study conducted among MDMA/ecstasy users in Miami, Florida, males had higher rates of illicit use of pharmaceutical opioids and other prescription drugs than females (Kurtz et al., 2005). These differences in findings related to gender may be due to local and age-related variations in patterns of pharmaceutical drug use, which highlights the importance of local assessments of drug use patterns and trends.
Since the main focus of this research project was Ecstasy use and associated behaviors, the study did not collect extensive information on patterns and motivation of illicit use of pharmaceutical opioids. However, our prior qualitative study conducted with 24 users in central Ohio suggested that initiation and continued illicit use of pharmaceutical opioids were linked to a number of different reasons, including self-medication of emotional and physical pain, recreation, social influences, legitimate medical prescriptions for chronic pain management, and easy access to pharmaceutical opioids (Daniulaityte et al., 2006). However, more extensive studies are needed to obtain a better understanding of patterns, motivations, social setting, and sources of non-medical use of pharmaceutical opioids.
This study has limitations which affect the generalizability of its results. First, the sample was not a random one, although respondent-driven sampling is recognized as one of the best methods to recruit active illicit drug users (Heckathorn, 1997; Wang et al., 2005). However, it is important to recognize that the sample was recruited to represent a population of MDMA users, and so caution should be used when generalizing the findings to a much broader population of young, polydrug users. Second, the study relies, in part, on participants’ self-reports of their non-medical drug use. Although self-reports of drug use have limitations, there is evidence to suggest that such reports can be valid and reliable (Adair, Craddock, Miller, & Turner, 1995; Darke, 1998). Our findings indicate that the non-medical use of pharmaceutical opioids is a part of polydrug use practices that often incorporate abuse of other prescription drugs. The observed relationship between depressive symptoms and illicit use of pharmaceutical opioids may have important implications for prevention programming and should be examined in future research.
Acknowledgments
Financial support was provided by the National Institute on Drug Abuse, Grant Number R01 DA14488 (R.G. Carlson, PI). The views expressed in this paper do not necessarily reflect those of the National Institute on Drug Abuse or any other governing agency.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adair EB, Craddock SG, Miller HG, Turner CF. Assessing consistency of responses to questions on cocaine use. Addiction (Abingdon, England) 1995;90(11):1497–1502. doi: 10.1046/j.1360-0443.1995.901114978.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Boyd CJ, Esteban McCabe S, Teter CJ. Medical and nonmedical use of prescription pain medication by youth in a Detroit-area public school district. Drug and Alcohol Dependence. 2006;81(1):37–45. doi: 10.1016/j.drugalcdep.2005.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: a latent class analysis. Drug and Alcohol Dependence. 2005;79(2):167–179. doi: 10.1016/j.drugalcdep.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry. 2006;67(2):247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Curran HV, Travill RA. Mood and cognitive effects of +/−3,4-methylenedioxymethamphetamine (MDMA, ‘ecstasy’): week-end ‘high’ followed by mid-week low. Addiction (Abingdon, England) 1997;92(7):821–831. [PubMed] [Google Scholar]
- Daniulaityte Raminta Siegal, Harvey A, Carlson RG, Kenne, Starr Deric R, Sanford DeCamp Brad. Qualitative epidemiologic methods can improve local prevention programming among adolescents. Journal of Alcohol and Drug Education. 2004;48:73–83. [Google Scholar]
- Daniulaityte R, Carlson RG, Kenne DR. Initiation to pharmaceutical opioids and patterns of misuse: Preliminary qualitative findings obtained by the Ohio Substance Abuse Monitoring Network. Journal of Drug Issues. 2006;36:787–808. [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug and Alcohol Dependence. 1998;51(3):253–63. doi: 10.1016/s0376-8716(98)00028-3. discussion 267–8. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Sullivan M, Steffick D, Harris KM, Wells KB. Do users of regularly prescribed opioids have higher rates of substance use problems than nonusers? Pain Medicine (Malden, Mass) 2007;8(8):647–656. doi: 10.1111/j.1526-4637.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- Falck RS, Wang J, Carlson RG. Depressive symptomatology in young adults with a history of MDMA use: a longitudinal analysis. Journal of Psychopharmacology (Oxford, England) 2008;22(1):47–54. doi: 10.1177/0269881107078293. [DOI] [PubMed] [Google Scholar]
- Green TC, Butler SF. A latent class analysis of prescription opioid abuse in the National Addictions Vigilance Intervention and Prevention Program (NAVIPPRO™). Paper presentation at the College on Problems of Drug Dependence Conference; San Juan, Puerto Rico. June 19, 2008.2008. [Google Scholar]
- Green CR, Ndao-Brumblay SK, West B, Washington T. Differences in prescription opioid analgesic availability: comparing minority and white pharmacies across Michigan. The Journal of Pain : Official Journal of the American Pain Society. 2005;6(10):689–699. doi: 10.1016/j.jpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden population. Social Problems. 1997;44:174–199. [Google Scholar]
- Heckathorn DD, Semaan S, Broadhead RS, Hughes JJ. Extensions of respondent-driven sampling: A new approach to the study of injection drug users aged 18–25. AIDS Behavior. 2002;6:55–67. [Google Scholar]
- Inciardi JA, Surratt Hilary L Martin, Steven S, Gealt R. Prevalence of narcotic analgesic abuse among students: individual or polydrug abuse? Archives of Pediatrics and Adolescent Medicine. 2004;158:498–499. doi: 10.1001/archpedi.158.5.498-b. [DOI] [PubMed] [Google Scholar]
- Kurtz SP, Inciardi JA, Surratt HL, Cottler L. Prescription drug abuse among ecstasy users in Miami. Journal of Addictive Diseases : The Official Journal of the ASAM, American Society of Addiction Medicine. 2005;24(4):1–16. doi: 10.1300/j069v24n04_01. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Teter CJ. Illicit use of opioid analgesics by high school seniors. Journal of Substance Abuse Treatment. 2005;28(3):225–230. doi: 10.1016/j.jsat.2004.12.009. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, West BT. Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: Results from two national surveys. Addictive Behaviors. 2008;33(10):1297–1305. doi: 10.1016/j.addbeh.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Illicit use of prescription pain medication among college students. Drug and Alcohol Dependence. 2005;77(1):37–47. doi: 10.1016/j.drugalcdep.2004.07.005. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ, Knight JR, Wechsler H. Nonmedical use of prescription opioids among U.S. college students: prevalence and correlates from a national survey. Addictive Behaviors. 2005;30(4):789–805. doi: 10.1016/j.addbeh.2004.08.024. [DOI] [PubMed] [Google Scholar]
- Ohio Substance Abuse Monitoring Network. Surveillance of drug trends in the state of Ohio: June 2000 - January 2001. Columbus, OH: Ohio Department of Alcohol and Drug Addiction Services, Wright State University and the University of Akron; 2001. Jan, [Google Scholar]
- Ohio Substance Abuse Monitoring Network. Surveillance of drug trends in the state of Ohio: January 2001 - June 2001. Columbus, OH: Ohio Department of Alcohol and Drug Addiction Services, Wright State University and the University of Akron; 2001. Jun, [Google Scholar]
- Ohio Substance Abuse Monitoring Network. Young Heroin Users and Treatment Experiences in Ohio: A Targeted Response Initiative, January 2006 - June 2006. Columbus, OH: Ohio Department of Alcohol and Drug Addiction Services, Wright State University and the University of Akron; 2006. Jun, [Google Scholar]
- Passik SD, Hays L, Eisner N, Kirsh KL. Psychiatric and pain characteristics of prescription drug abusers entering drug rehabilitation. Journal of Pain & Palliative Care Pharmacotherapy. 2006;20(2):5–13. [PubMed] [Google Scholar]
- Quintero G, Peterson J, Young B. An exploratory study of socio-cultural factors contributing to prescription drug misuse among college students. Journal of Drug Issues. 2006;36(4):903–931. [Google Scholar]
- SAMHSA Substance Abuse and Mental Health Services Administration. Treatment admissions involving narcotic painkillers: 2002 update. [(Accessed June 5, 2008)];The DASIS Report. 2004 July 23; Available at http://www.oas.samhsa.gov/factsDASIS.htm.
- SAMHSA. Nonmedical Users of Pain Relievers: Characteristics of Recent Initiates. The NSDUH Report. [(Accessed June 5, 2008)];Office of Applied Studies. 2006 Available at http://www.oas.samhsa.gov/2k6/pain/pain.pdf.
- SAMHSA. Results From the 2006 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies; 2007. [Google Scholar]
- Siegal HA, Carlson RG, Kenne DR, Swora MG. Probable relationship between opioid abuse and heroin use. American Family Physician. 2003;67(5):942–945. [PubMed] [Google Scholar]
- Simoni-Wastila L, Ritter G, Strickler G. Gender and other factors associated with the nonmedical use of abusable prescription drugs. Substance use & Misuse. 2004;39(1):1–23. doi: 10.1081/ja-120027764. [DOI] [PubMed] [Google Scholar]
- Sullivan MD, Edlund MJ, Zhang L, Unutzer J, Wells KB. Association between mental health disorders, problem drug use, and regular prescription opioid use. Archives of Internal Medicine. 2006;166(19):2087–2093. doi: 10.1001/archinte.166.19.2087. [DOI] [PubMed] [Google Scholar]
- Sung HE, Richter L, Vaughan R, Johnson PB, Thom B. Nonmedical use of prescription opioids among teenagers in the United States: trends and correlates. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine. 2005;37(1):44–51. doi: 10.1016/j.jadohealth.2005.02.013. [DOI] [PubMed] [Google Scholar]
- Surratt HL, Inciardi JA, Kurtz SP. Prescription opioid abuse among drug-involved street-based sex workers. Journal of Opioid Management. 2006;2(5):283–289. doi: 10.5055/jom.2006.0042. [DOI] [PubMed] [Google Scholar]
- Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. American Journal of Public Health. 2003;93(12):2067–2073. doi: 10.2105/ajph.93.12.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Carlson RG, Falck RS, Siegal HA, Rahman A, Li L. Respondent-driven sampling to recruit MDMA users: a methodological assessment. Drug and Alcohol Dependence. 2005;78(2):147–157. doi: 10.1016/j.drugalcdep.2004.10.011. [DOI] [PubMed] [Google Scholar]
- Wasan AD, Butler SF, Budman SH, Benoit C, Fernandez K, Jamison RN. Psychiatric history and psychologic adjustment as risk factors for aberrant drug-related behavior among patients with chronic pain. The Clinical Journal of Pain. 2007;23(4):307–315. doi: 10.1097/AJP.0b013e3180330dc5. [DOI] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: position statement. Drug and Alcohol Dependence. 2003;69(3):215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]